
 | International Journal of Mental Health Promotion |  |
DOI: 10.32604/IJMHP.2021.011568
ARTICLE
Loneliness in Older Chilean People: Importance of Family Dysfunction and Depression
1School of Medicine, Faculty of Medicine, Pontificia Universidad Católica de Chile, Member of “Centro UC Estudios de Vejez y Envejecimiento”, Centre for the Study of Ageing, Santiago, 8330033, Chile
2Institute of Sociology, Pontificia Universidad Católica de Chile, Member of “Centro UC Estudios de Vejez y Envejecimiento”, Centre for the Study of Ageing, Santiago, 7820436, Chile
3School of Medicine, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, 8330033, Chile
*Corresponding Author: Marcela Carrasco. Email: mcarras@med.puc.cl
Received: 16 May 2020; Accepted: 06 July 2020
Abstract: Loneliness is considered a public health problem that negatively affects wellbeing, especially in the older population. In Latin-American countries, most of the older population live with their family. Although this is thought to diminish feelings of loneliness, there is scarce data to support this. The objective of this study is to determine the prevalence of loneliness and evaluate its association with objective social networks, family functioning and perception of social support, in a sample of older people from Santiago, Chile. A survey was conducted of a representative sample of community older people (60–97 years) from Santiago, Chile, using the UCLA abbreviated scale of loneliness. Logistic regression was performed to test the variables related to the loneliness of older people. A total of 1,217 older people were interviewed. 88% were living with at least one person at home and 92% had living children. Using the UCLA abbreviated scale, 45% were found to perceive feelings of loneliness at least some of the time. Logistic regression showed significant association between loneliness and family dysfunction; depressive symptoms; living alone; not having a partner (widowed, separated or single); having little contact with relatives and friends; feeling a lack of social support; and sensation of poor self-efficacy. Loneliness is a prevalent public health problem in this older Latin-American community. Living accompanied does not protect against loneliness, particularly in vulnerable groups such as those with depression, or when there are family conflicts. The high prevalence of loneliness strongly conveys the need for public health policies to address loneliness in older people.
Keywords: Ageing; family relations; loneliness; social support
The population is ageing around the world. However, regions such as Latin America are experiencing an accelerated process, in contrast to now industrialized countries where the process took place more gradually. For example, to double the proportion of people aged 65 and over, the USA and France took more than 60 and 100 years respectively. In contrast, Chile is estimated to double this value in only 24 years [1]. This ageing population poses new challenges, such as promoting wellbeing in the years gained, with different social and health support.
Social participation is key for successful ageing. Often, older people give greater importance to it than to physical health [2,3]. However, both determinants seem to be strongly linked: health can hinder social integration and social relationships can affect health in a beneficial or prejudicial way [4].
Loneliness is a subjective experience of dissatisfaction due to lack of significant human relationships or a perception of discrepancy between desired human relationships versus reality [5,6]. Loneliness must also be distinguished from social isolation, which refers to number of social contacts and level of social integration. Therefore, even when social isolation is not present loneliness may occur, as social contact may be plentiful but unsatisfactory [5].
The estimated prevalence of loneliness varies and has been reported to be as high as 49%, depending on the population studied [5,7]. Loneliness has been associated to different aspects, such as: older age [8–10], poorer health [11], depression [12,13], and social, economic and cultural aspects [8,14]. Although there are many studies internationally, to our knowledge the only study regarding a Latin American population is from older Latin-American people living in the USA [15]. Older people in Latin America live a different reality from that of developed countries. For instance, there is greater poverty and inequality; less access to health; and a weaker social security system [1]. This means conclusions of loneliness studies from other regions may not be extrapolated to Latin America and that this study gives us new and interesting insight regarding this population.
The aim of this study is to determine the prevalence of loneliness in older people in Santiago, Chile, and to analyse possible association with objective social networks, family functioning, perception of social support, physical and mental health, controlling for sociodemographic factors, all of which are important aspects in successful ageing.
This study is based on data from the survey “Stressful events that occur while growing old: how family relationships and social resources impact elderly people’s wellbeing” of the FONDECYT project N° 1120331. The survey was face-to-face and conducted in Autumn 2013 (April to June). The target population was all people aged 60 or over who lived in the city of Santiago de Chile, in their private homes, and who could answer a survey by themselves. The final sample was composed of a total of 1,217 senior citizens, with a sampling error of 4%. Nursing home residents were excluded, as well as individuals with suspicion of cognitive impairment.
The sample design consisted of a multistage random sampling. First, using systematic randomization, geographic blocks of the city of Santiago were selected. Second, private housing was randomly selected from the selected blocks. Third, in the selected residences, all older people were listed and then randomly selected using a Kish grid. Respondents did not receive monetary incentives to participate in the study.
All respondents gave informed consent. The project had an ethical follow-up at all stages, being approved by the Ethical Committee of the Pontificia Universidad Católica de Chile, following the ethical standards laid down in the Declaration of Helsinki, 2008.
The survey was constructed by professionals of the research team, and was composed of six sections: a) Socio-demographic factors (sex, age, education, marital status, number of children), b) Loneliness and wellbeing (general satisfaction and positive or negative emotions), c) Family structure and functioning (household composition, quality of family relationships), d) social participation and social support and e) Personal conditions (self-efficacy, functional capacity, depressive symptoms).
Loneliness was used as the outcome variable, using the revised UCLA Three-Item Loneliness Scale, which has shown performance comparable with the original version [16]. The scale is composed of three questions: i) How often do you feel that you lack companionship? ii) How often do you feel left out? iii) How often do you feel isolated from others? The possible responses were hardly ever, some of the time, or often. The scale was then dichotomised: in cases in which the answer was “hardly ever” for all three questions, the answers were re-coded as “without loneliness” and those who answered “some of the time” or “often” in at least one question as “with loneliness” [11].
Principal component analysis supported construct validity of the index in the Chilean sample, finding that 78% of the loneliness variance was explained by the three items, with a factor loading of 0.80 for the item “how often do you feel that you lack companionship” and a 0.92 for the other two items. The alpha coefficient of Cronbach was 0.84.
To measure family structure and functioning, the following variables were selected. Firstly, the Household Composition variable (to live accompanied or alone) and secondly, number of children (current living children: “How many living children do you have?”).
In addition, the Scale of Family Functioning: APGAR [17,18] was selected: APGAR is a five-item scale of family functioning: Adaptability, Partnership, Growth, Affection, and Resolve. The range of answers corresponds to a 3-point scale, ranging from 0 (hardly ever), 1 (sometimes) and 2 (almost always). The summated scale ranges from 0 (low) to 10 (greater degree of satisfaction with family functioning). It is coded into three levels: Serious dysfunction (0 to 3 points), minor dysfunction (4 to 6 points) and good family functioning (7 to 10 points). In analysis of the main components, this scale behaved in a unidimensional way, with 68% of variance explained by the five items. The factor loading varied from 0.77 for “Do you feel satisfied with the way in which you can ask your family for help when something worries you?” to 0.87 for “Do you feel satisfied with the way in which your family talk and share problems with you?” The scale had a high level of internal consistency, with an alpha coefficient of Cronbach of 0.88.
In addition, the eight-item Medical Outcomes Study Social Support Survey (MOS) [19] was used to measure two dimensions of social support: instrumental and emotional. The survey investigated the perception of potential available support in eight hypothetical cases with three possible answers (always = 1; sometimes = 2; never = 3); giving a range of 8 to 24 points (from less to greater support). In the principal component analysis, the scale behaved in a unidimensional way, with 70% explained variance; an alpha coefficient of Cronbach of 0.938; and factor loading from 0.79 for “… love and make you feel wanted?” to 0.86 for “…to take you to the doctor if you need it?”
Amongst significant activities, two were selected: frequency with which the individual visits or receives visits from relatives or friends, and frequency with which the individual participates in religious activities, social organisations, or in courses and workshops. In both cases, possible answers were: Many times a week, once a week, once a month and less frequent/never. Posteriorly, answers were classified into two categories: Once a month or less frequent/never, versus once or many times a week. These two activities have been significantly associated to subjective well-being in previous studies on older people carried out in Chile [20,21].
In the personal conditions section, two variables were chosen: self-efficacy and health status. Chen’s Self-Efficacy Scale [22], which measures a person’s capacity to cope when facing new and difficult tasks, was used as a scale composed of eight items with a range of answers corresponding to a Likert scale of three options (almost never/never, sometimes, almost always/always), giving a range of 8–24 points. According to the principal component analysis, the scale was unidimensional with 73% of variance explained by the eight items; factor loading between 0.78 for “Do you think you would be able to achieve most of the goals you propose?” to 0.88 for “Do you think you would be able to overcome many challenges successfully?”; and Cronbach’s alpha of 0.945.
Health status was evaluated with self-rated perception of health, an indicator broadly used as a predictor of global health which is associated to morbidity, use of services and mortality [23]. This self-perception was evaluated using the question “Do you consider your health: Excellent, good, regular or bad?” which was then categorized into three groups: bad, regular and excellent/good.
The last variable selected was depressive symptoms, measured using the Abbreviated Screening Scale of Depression Yesavage GDS-5, a questionnaire of five dichotomous questions (Yes/No) validated in Chile [24]. A score higher or equal to 2 suggests depression. The scale behaved in a unidimensional way with a Cronbach’s alpha coefficient of 0.646.
Finally, the following socio-demographic variables were selected: gender, age (60–74, 75 and more), education (primary: Eight or less years of education, secondary: From nine to 12 years of education, higher: At least one year of university or professional studies), and marital status (single, married/cohabitant, separated/divorced, widower).
Data was analyzed using STATA 14 software. First, we conducted a descriptive analysis of the variables (percentages, means, and standard deviations). Then, we performed a logistic regression to test the variables related to the loneliness to the older people. Logistic regression models were calculated with the dichotomous dependent variable of loneliness (0 = without loneliness; 1 = with loneliness). Stepwise models were calculated which allowed continuous evaluation of how the models changed while the variables were being incorporated step by step. First, the variables of family structure, family functioning and the undertaking of significant activities were included. These constitute social factors, which are more likely to be associated with the feeling of loneliness. In a second model, the variables of self-efficacy, and mental/physical health were added. Finally, the socio-demographic variables were incorporated (sex, age, education and marital status). Goodness of fit was assessed using the Hosmer–Lemeshow test and pseudo-R2.
The characteristics of the sample were: 63% women with a mean age of 71.0 years (SD = 7.512). Only 11% had completed higher education, just over half of the participants were married (53%) and near one quarter widowed (26%). Almost all respondents said that they had living children (92%), with an average number of three children (SD = 1.846). The majority were living with at least one person at home (88%) and perceived their family functioning as quite positive (81%). There was a high valorization of the availability of support with a mean of 21.4 points in the MOS scale (SD = 4.334).
With regards to participation in significant activities, over half of the participants mentioned frequently (once or many times a week) meeting with relatives or friends (60%), whilst the participation in religious activities, social organizations, or courses/workshops reached 42%. In terms of personal conditions, perception of self-efficacy was high, with a mean of 20.0 (SD = 4.183) in the Chen scale and 49% perceiving their health as excellent/good or very good health. Finally, more than one third (34%) had a positive GDS-5 screening, suggesting depression.
Loneliness: 45% of the sample were classified with some level of loneliness and 55% without. The analysis by item showed that 13.4% of the sample answered “often” to at least one of the three items of the UCLA abbreviated loneliness scale, and 4.3% to all three items (severe loneliness). The average score of this three-item scale was 4.176 (SD = 1.690), ranging between 3 and 9. In other words, even though almost half felt lonely at least some of the time, for most of them it was not severe. The distribution of each independent variable and its association with loneliness, analyzed in a dichotomous way, is shown in Tab. 1.
Table 1: Independent variables and loneliness scale (Sample = 1217 cases)
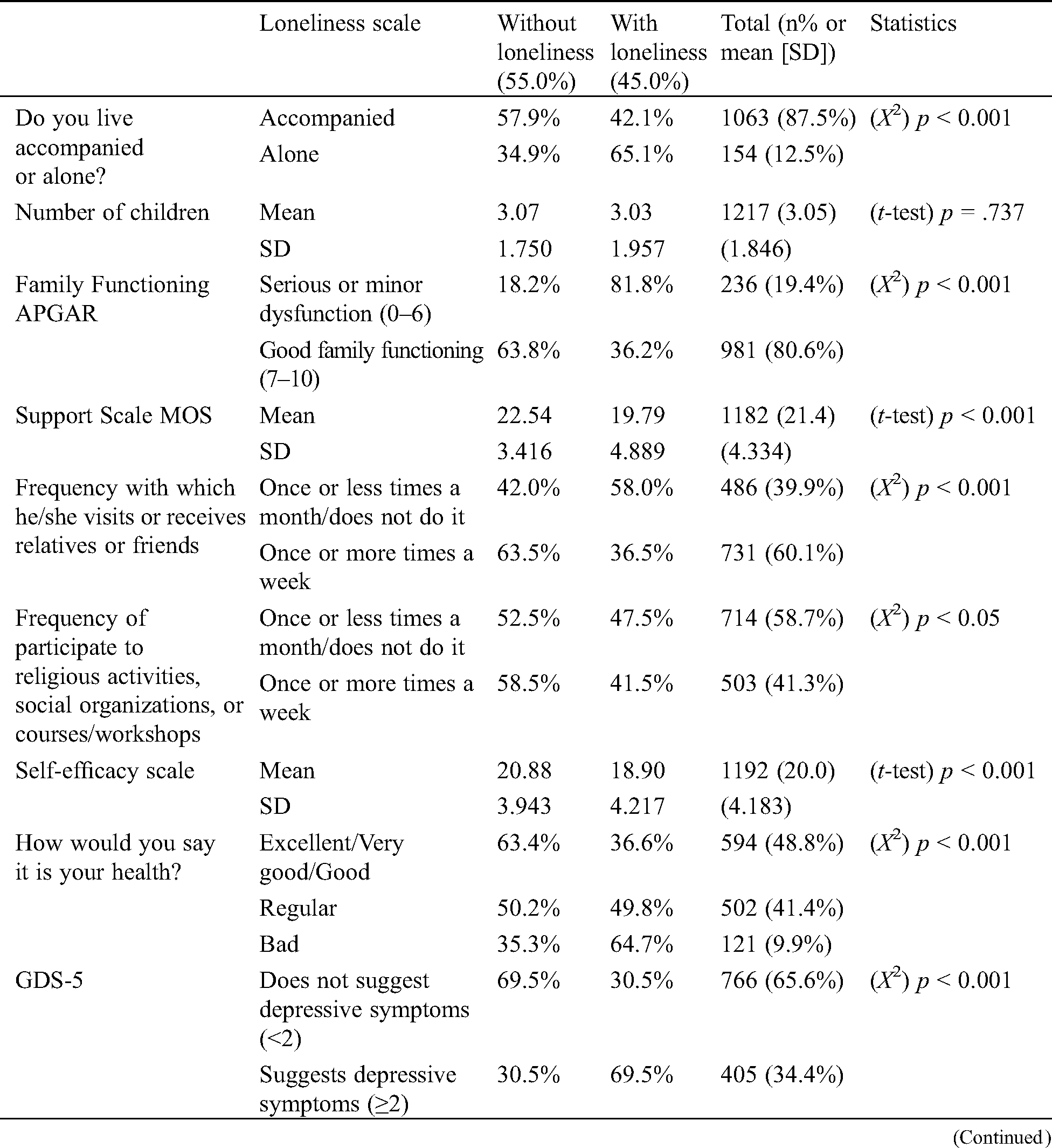

Older people living alone reported more loneliness (X2 (1) = 22.2, p < 0.001) whereas number of children was not significant (t = 0.335, p = 0.737). Presence of family dysfunction was significantly associated to more loneliness (X2 (1) = 159.7, p < 0.001), and the greater the perceived availability of support the lower perception of loneliness (t = 11.2, p < 0.001). In terms of participation in significant activities, having frequent contact with relatives or friends and participate (at least once a week) to religious activities, social organizations, or courses/workshops reduced loneliness (X2 (1) = 54.1, p < 0.001 and (X2 (1) = 4.190, p = 0.05, respectively).
Greater loneliness was found in those with lower self-efficacy (t = –8.000, p < 0.001) and in those with poor self-reported health (X2 (2) = 39.9, p < 0.001). Also, people who were classified with depressive symptoms reported more loneliness (X2 (1) = 162.0, p < 0.001).
Finally, loneliness was more prevalent among female gender (X2 (1) = 13.5, p < 0.001) and lower educational level (X2 (2) = 14.98, p < 0.001), in contrast to being married or cohabiting (X2 (3) = 65.3, p < 0.001). Age was not significant (X2 (1) = 0.764, p = 0.382).
Multivariate logistic regression models were constructed for the probability of loneliness occurrence (Tab. 2). As previously mentioned, family variables and significant activities were included in the first model. In the second, personal conditions (self-efficacy and health) were included, and in the third model the socio-demographic variables. All models were significant (Model 1: X2 (6) = 225.4, p < 0.001; Model 2: X2 (10) = 315.5, p < 0.001 and Model 3: X2 (17) = 352.4, p < 0.001). The Hosmer–Lemeshow goodness-of-fit test showed that all models fit the data well, with the third model having the best fit, explaining 26% of the variance.
Table 2: Loneliness Logistic Regression (dichotomous variable 0=without loneliness 1= with loneliness)
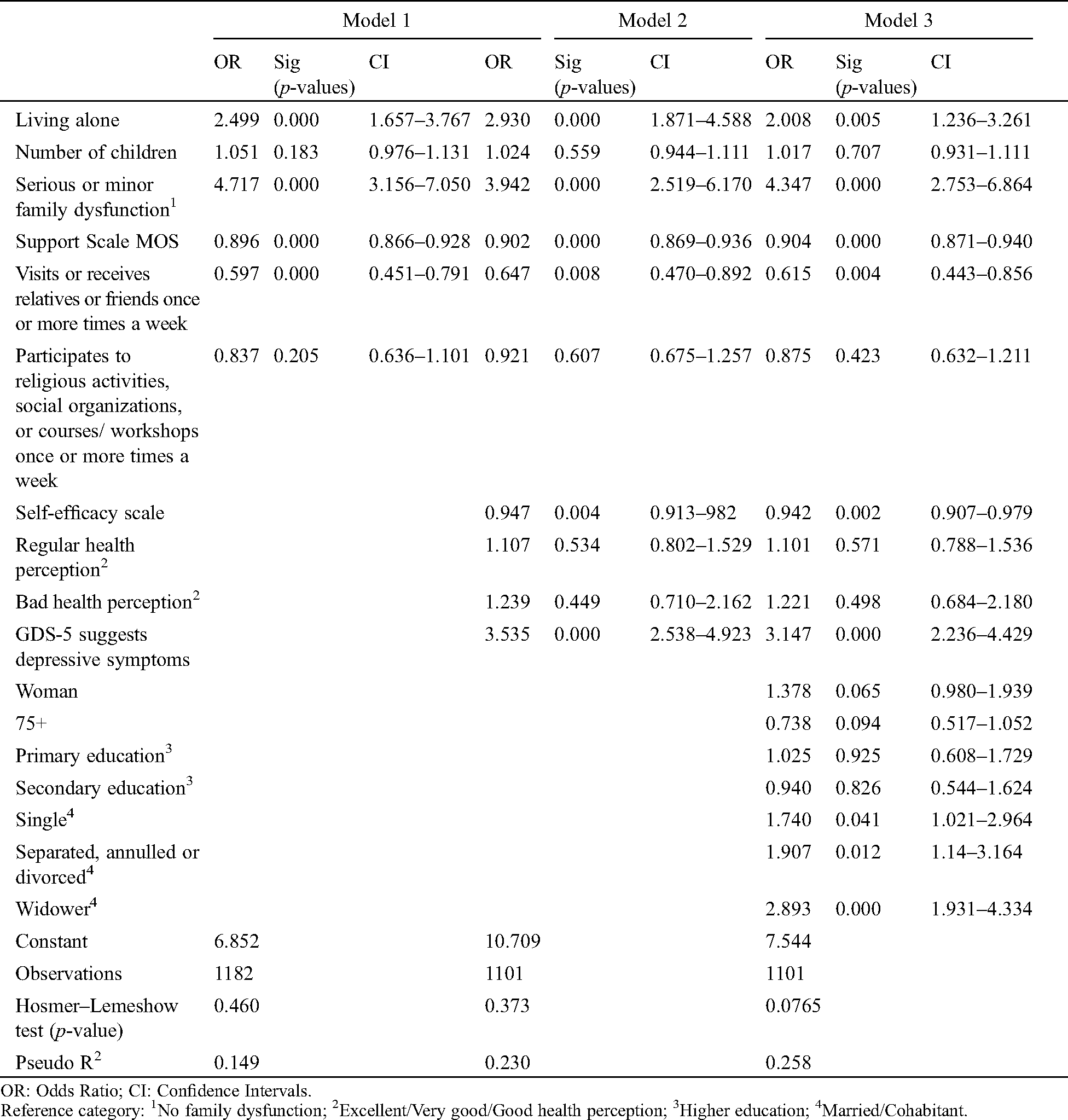
In the final model, it was observed that the greatest chances to feel lonely were associated to the presence of family dysfunction (OR = 4.734, p < 0.001) and the presence of depressive symptoms (OR = 3.147, p < 0.001).
Other significant but less relevant variables in the model were related to objective loneliness measured as living alone (OR = 2.008, p < 0.01) and living without a partner: either being single (OR = 1.740, p < 0.05), separated (OR = 1.907, p < 0.05), and especially a widower (OR = 2.893, p < 0.001). On the other hand, the greater the perceived potential support, the lower the chances of loneliness (OR = 0.904, p < 0.001). This was also the case for frequent contact with relatives and friends (OR = 0.615, p < 0.01). Finally, people with higher perception of self-efficacy reported less loneliness (OR = 0.942, p < 0.01).
Loneliness in the older population is a growing, worldwide public health problem that negatively impacts wellbeing [5,11]. In this Latin-American sample of older people there was a high overall prevalence of loneliness (45%), although the prevalence of severe loneliness only reached 4.3%.
The most remarkable finding in our population, which had low objective isolation, was the strong relation between loneliness and family dysfunction, suggesting that when family dysfunction is present, it may outweigh the protective benefits of living accompanied. This powerfully supports the hypothesis that the quality of social contacts, such as the level of friendliness, trust and companionship of relationships, has more influence on loneliness than quantity [10]. Similarly, a previous study links quality of relationship between spouses to loneliness [25], however does not evaluate the effect of family functioning or presence of conflict.
In line with the literature, we found an association of loneliness with objective social isolation, measured as living alone; not having a partner (widowed, separated or single); and having little contact with relatives and friends [8,26,27]. However, in our sample social isolation was rare: only 13% were living alone, more than 90% had living children (three on average) and more than half had visits from friends/family at least every week, assumed as representing relatively better quality relationships [26–28]. These factors, which are expected to be protective against loneliness [29], are much more prevalent than in other populations [28,30]. Despite this, the prevalence of loneliness is not better than in other populations, even in terms of severe loneliness, which reinforces the importance of the quality of bonds over quantity of contact [10].
The high prevalence of loneliness in this sample may also be linked to cultural aspects. It is known that Latins tend to have high expectations of family relationships, amplifying the difference between desired and actual relationships [31,32]. Moreover, in contrast to Anglo-Saxon cultures in which living alone is more of a sign of independence, Latin-Americans associate living alone with feelings of abandonment [14,15]. Additionally, as in many other developing countries, families provide most of the care for older people informally, satisfying the needs that are not sufficiently covered by the formal system of social protection [1]. This could be a source of conflict and caregiver overload, related to the association of loneliness found with poor perception of self-efficacy [8]. In addition, Chile has one of the highest rates of depression in Latin America [33] and there is a strong association with loneliness in our population. Depression has been systematically associated with loneliness, however the relationship between the two remains unclear. In some studies, loneliness increases depression [13] but in others loneliness may cause anxiety rather than depression itself [34].
No association was shown with gender nor age. Literature describes increased loneliness in women due to factors such as being widowed, suffering depression or being at an economic disadvantage [10,11,14,35]. Greater age has also frequently been associated with loneliness [9,10,27,30,36] due to many factors such as negativity linked to acceptance of irreversible aspects of ageing; less social support due to a higher probability of death of loved ones; and physical and health limitations which hinder social situations [10,35]. Many studies have demonstrated a U-shaped relationship between age and loneliness over a lifetime [10]. However, our study is in line with other reports that show no higher risk of loneliness with increasing age [28,37,38], one of which also studied a Latin-American population but living in the USA [15].
It is important to note that, as described in the method of the study, the revised UCLA scale used to measure the prevalence of loneliness was dichotomised as “without loneliness” for “hardly ever” in all three questions, and “with loneliness” when people answered “some of the time” or “often” in at least one question [11]. The reason for this classification was that the scale did not have a normal distribution, because close to half of the sample answered “hardly ever” for the three questions. Although this classification could be seen as a risk for concealing important results, in this study an exploratory bivariate analysis showed that the discrimination was higher when the scale was dichotomized.
This study has the strength of being the first, to our knowledge, to analyses a representative sample of urban Latin–American older people living in their country of origin. The study allowed control of the effects of social isolation, depressive symptoms, social support and health determinants. However, due to the study’s transversal design, results could only refer to associations and not to causality. Moreover, the scales used to measure self-efficacy, health and functional capacity were based on each individual’s perceptions, and therefore not diagnostic as in the case of the depression or cognitive impairment scales. As a consequence, results could only suggest associations of each factor analysed. More longitudinal studies are needed to study the causality relationships in loneliness.
In conclusion, as the population grows older, the interest in studying the variables associated to ageing and well-being in the older population increases. Loneliness is a complex and multifactorial condition which is deeply influenced by culture, social determinants and health. The development of public policies addressing its potentially modifiable aspects should be encouraged. Our study suggests that focusing on improving social support to families living with older people and treating depression may have a positive impact on the quality of life of older people.
Acknowledgement: None to declare.
Funding Statement: This investigation was supported by the FONDECYT (National Fund for Scientific and Technological Development) Project No. 1120331 and Project No. 1171071, subsidised by the Chilean state through by the ANID (Agencia Nacional de Investigación y Desarrollo).
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
1. Huenchuan, S. (2013). Ageing, solidarity and social protection in Latin America and the Caribbean. Time to advance toward equality. Economic Commission for Latin America and the Caribbean (CEPAL). Santiago, Chile: United Nations (in Spanish). https://repositorio.cepal.org/bitstream/handle/11362/2617/1/LCG2553P_es.pdf. [Google Scholar]
2. Depp, C. A., Jeste, D. (2006). Definitions and predictors of successful aging: A comprehensive review of larger quantitative studies. American Journal of Geriatric Psychiatry, 14(1), 6–20. DOI 10.1097/01.JGP.0000192501.03069.bc. [Google Scholar] [CrossRef]
3. Fernández-Ballesteros, R., Garcia, L. F., Abarca, D., Blanc, E., Efklides, A. et al. (2010). The concept of ‘ageing well’ in ten Latin American and European countries. Ageing and Society, 30(1), 41–56. DOI 10.1017/S0144686X09008587. [Google Scholar] [CrossRef]
4. Fratiglioni, L., Paillard-Borg, S., Winblad, B. (2004). An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurology, 3(6), 343–353. DOI 10.1016/S1474-4422(04)00767-7. [Google Scholar] [CrossRef]
5. Victor, C., Scambler, S., Bond, J., Bowling, A. (2000). Being alone in later life: loneliness, social isolation and living alone. Reviews in Clinical Gerontology, 10(4), 407–417. DOI 10.1017/S0959259800104101. [Google Scholar] [CrossRef]
6. Peplau, L. A., Perlman, D. (1982). Perspectives on loneliness, loneliness: A sourcebook of current theory, research, and therapy. New York: John Wiley and Sons. [Google Scholar]
7. Holmen, K., Ericsson, K., Winblad, B. (1994). Loneliness and living conditions of the oldest old. Scandinavian Journal of Social Medicine, 22(1), 15–19. DOI 10.1177/140349489402200103. [Google Scholar] [CrossRef]
8. Cohen-Mansfield, J., Hazan, H., Lerman, Y., Shalom, V. (2016). Correlates and predictors of loneliness in older-adults: A review of quantitative results informed by qualitative insights. International Psychogeriatrics, 28(4), 557–576. DOI 10.1017/S1041610215001532. [Google Scholar] [CrossRef]
9. Hazer, O., Boylu, A. (2010). The examination of the factors affecting the feeling of loneliness of the elderly. Procedia—Social and Behavioral Sciences, 9, 2083–2089. DOI 10.1016/j.sbspro.2010.12.450. [Google Scholar] [CrossRef]
10. Pinquar, M., Sorensen, S. (2010). Influences on loneliness in older adults: A meta-analysis. Basic and Applied Social Psychology, 23(4), 245–266. DOI 10.1207/S15324834BASP2304_2. [Google Scholar] [CrossRef]
11. Perissinotto, C. M., Stijacic, C. I., Covinsky, K. E. (2012). Loneliness in older persons: A predictor of functional decline and death. Archives of Internal Medicine, 172(14), 1078–1083. DOI 10.1001/archinternmed.2012.1993. [Google Scholar] [CrossRef]
12. Aylaz, R., Aktürk, U., Erci, B., Öztürk, H., Aslan, H. (2012). Relationship between depression and loneliness in elderly and examination of influential factors. Archives of Gerontology and Geriatrics, 55(3), 548–554. DOI 10.1016/j.archger.2012.03.006. [Google Scholar] [CrossRef]
13. Cacioppo, J. T., Hughes, M. E., Waite, L. J., Hawkley, L. C., Thisted, R. A. (2006). Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychology and Aging, 21(1), 140–151. DOI 10.1037/0882-7974.21.1.140. [Google Scholar] [CrossRef]
14. Dykstra, P. A. (2009). Older adult loneliness: myths and realities. European Journal of Ageing, 6(2), 91–100. DOI 10.1007/s10433-009-0110-3. [Google Scholar] [CrossRef]
15. Gerst-Emerson, K., Shovali, T. E., Markides, K. S. (2014). Loneliness among very old Mexican Americans: findings from the Hispanic established populations epidemiologic studies of the elderly. Archives of Gerontology and Geriatrics, 59(1), 145–149. DOI 10.1016/j.archger.2014.01.007. [Google Scholar] [CrossRef]
16. Hughes, M. E., Waite, J., Hawkley, L. C., Cacioppo, J. T. (2016). A short scale for measuring loneliness in large surveys: results from two population-based studies. Research on Aging, 26(6), 655–672. DOI 10.1177/0164027504268574. [Google Scholar] [CrossRef]
17. Smilkstein, G. (1978). The family APGAR: a proposal for a family function test and its use by physicians. The Journal of Family Practice, 6(6), 1231–1239. [Google Scholar]
18. Orpinas, P., Rico, A., Martinez, L. (2013). Family APGAR. World Health Organization, Pan American Health Organization. Latino families and youth: a compendium of assessment tools. http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=23171&Itemid=. [Google Scholar]
19. Moser, A., Stuck, A. E., Silliman, R. A., Ganz, P. A., Clough-Gorr, K. M. (2012). The eight-item modified medical outcomes study social support survey: psychometric evaluation showed excellent performance. Journal of Clinical Epidemiology, 65(10), 1107–1116. DOI 10.1016/j.jclinepi.2012.04.007. [Google Scholar] [CrossRef]
20. Herrera, M. S., Barros, C., Fernández, M. B. (2011). Predictors of quality of life in old age: A multivariate study in Chile. Journal of Population Ageing, 4(3), 121–139. DOI 10.1007/s12062-011-9043-7. [Google Scholar] [CrossRef]
21. Herrera, M. S., Elgueta, R., Fernández, M. B. (2014). Social capital, social participation and life satisfaction among Chilean older adults. Revista de Saúde Pública, 48(5), 739–749. [Google Scholar]
22. Chen, G., Gully, S. M., Eden, D. (2016). Validation of a new general self-efficacy scale. Organizational Research Methods, 4(1), 62–83. DOI 10.1177/109442810141004. [Google Scholar] [CrossRef]
23. Idler, E. L., Benyamini, Y. (1997). Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health and Social Behavior, 38(1), 21–37. DOI 10.2307/2955359. [Google Scholar] [CrossRef]
24. Hoyl, T., Valenzuela, E., Marin, P. P. (2000). Depression in the aged: preliminary evaluation of the effectiveness, as a screening instrument, of the 5-item version of the Geriatric Depression Scale. Revista Médica de Chile, 128(11), 1199–1204. [Google Scholar]
25. Ayalon, L., Shiovitz-Ezra, S., Palgi, Y. (2013). Associations of loneliness in older married men and women. Aging & Mental Health, 17(1), 33–39. DOI 10.1080/13607863.2012.702725. [Google Scholar] [CrossRef]
26. Hawkley, L. C., Hughes, M. E., Waite, L. J., Masi, C. M., Thisted, R. A. et al. (2008). From social structural factors to perceptions of relationship quality and loneliness: the Chicago health, aging, and social relations study. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 63(6), S375–S384. DOI 10.1093/geronb/63.6.S375. [Google Scholar] [CrossRef]
27. Routasalo, P. E., Savikko, N., Tilvis, R. S., Strandberg, T. E., Pitkälä, K. H. (2006). Social contacts and their relationship to loneliness among aged people-a population-based study. Gerontologia, 52(3), 81–187. [Google Scholar]
28. Heylen, L. (2010). The older, the lonelier? Risk factors for social loneliness in old age. Ageing and Society, 30(7), 1177–1196. DOI 10.1017/S0144686X10000292. [Google Scholar] [CrossRef]
29. Seeman, T. E. (2016). Health promoting effects of friends and family on health outcomes in older adults American. Journal of Health Promotion, 14(6), 362–370. DOI 10.4278/0890-1171-14.6.362. [Google Scholar] [CrossRef]
30. Savikko, N., Routasalo, P., Tilvis, R. S., Strandberg, T. E., Pitkälä, K. (2005). Predictors and subjective causes of loneliness in an aged population. Archives of Gerontology and Geriatrics, 41(3), 223–233. DOI 10.1016/j.archger.2005.03.002. [Google Scholar] [CrossRef]
31. Ross, C. E., Mirowsky, J., Cockerham, W. C. (1983). Social class, Mexican culture, and fatalism: their effects on psychological distress. American Journal of Health Promotion, 11(4), 383–399. [Google Scholar]
32. Wilmoth, J. M. (2001). Living arrangements among older immigrants in the United States. Gerontologist, 41(2), 228–238. DOI 10.1093/geront/41.2.228. [Google Scholar] [CrossRef]
33. Marin, P. P., Albala, C., Pelaez, M., Lera, L., Garcia, C. (2003). Prevalence of depression in four Latin-American cities: results of the SABE Project. International Psychogeriatrics, 15(4), 187. DOI 10.1017/S1041610203009633. [Google Scholar] [CrossRef]
34. Domènech-Abella, J., Mundó, J., Maria, H. J., Rubio-Valera, M. (2019). Anxiety, depression, loneliness and social network in the elderly: Longitudinal associations from the Irish Longitudinal Study on Ageing (TILDA). Journal of Affective Disorders, 246, 82–88. DOI 10.1016/j.jad.2018.12.043. [Google Scholar] [CrossRef]
35. Losada, A., Márquez-González, M., García-Ortiz, L., Gómez-Marcos, M. A., Fernández-Fernández, V. et al. (2012). Loneliness and mental health in a representative sample of community-dwelling Spanish older adults. Journal of Psychology, 146(3), 277–292. DOI 10.1080/00223980.2011.582523. [Google Scholar] [CrossRef]
36. Fry, P. S., Debats, D. L. (2016). Self-efficacy beliefs as predictors of loneliness and psychological distress in older adults. International Journal of Aging and Human Development, 55(3), 233–269. DOI 10.2190/KBVP-L2TE-2ERY-BH26. [Google Scholar] [CrossRef]
37. Theeke, L. A. (2009). Predictors of loneliness in US adults over age sixty-five. Archives of Psychiatric Nursing, 23(5), 387–396. DOI 10.1016/j.apnu.2008.11.002. [Google Scholar] [CrossRef]
38. Palgi, Y., Shrira, A., Ben-Ezra, M., Shiovitz-Ezra, S., Ayalon, L. (2012). Self-and other-oriented potential lifetime traumatic events as predictors of loneliness in the second half of life. Aging & Mental Health, 16(4), 423–430. DOI 10.1080/13607863.2011.638903. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |