
 | International Journal of Mental Health Promotion | 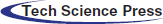 |
DOI: 10.32604/IJMHP.2021.013072
ARTICLE
Community Workers’ Social Support and Sleep Quality during the Coronavirus Disease 2019 (COVID-19): A Moderated Mediation Model
1Center of Student Development Research and Guidance, Huazhong University of Science and Technology, Wuhan, 430074, China
2School of Educational Science, Central China Think Tank, Huazhong University of Science and Technology, Wuhan, 430074, China
3College of Life Science and Technology, Huazhong University of Science and Technology, Wuhan, 430074, China
4Department of Orthodontics, Shanghai Xuhui District Dental Disease Prevention and Control Institute, Shanghai, 200032, China
5Department of Oral and Cranio-maxillofacial Surgery, Ninth People’s Hospital, Shanghai Jiaotong University School of Medicine, Shanghai Key Laboratory of Stomatology & Shanghai Research Institute of Stomatology, National Clinical Research Center of Stomatology, Shanghai, 200011, China
*Corresponding Authors: Yan Zhang. Email: zhangyan1981@hust.edu.cn; Yufei Xie. Email: xieyufei9@163.com
Received: 25 July 2020; Accepted: 30 December 2020
#Caihong Yang and Yan Ge are co-first authors
Abstract: To explore the relationship between social support and sleep quality of community workers in Wuhan during the coronavirus disease 2019 (the COVID-19 infection epidemic), this research constructed a mediating effect model to explore the mediating psychological mechanism of social support influencing sleep quality of front-line community workers. A total of 500 front-line community workers in Wuhan were investigated. We used the perceived social support scale (PSSS), the Connor-Davidson Resilience Scale (CD-RISC), the perceived stress scale (PSS), and the Pittsburgh sleep quality index (PSQI) to measure social support, psychological resilience, perceived stress and sleep quality. Specifically, the higher the PSQI, the worse the sleep quality. Pearson correlation structural equation model was used to analyze the relationship between these factors. The results showed that: (1) There was a significant negative correlation between social support, psychological resilience, and perceived stress of community workers and PSQI, that means, the higher the level of social support, psychological resilience, and perceived stress, the higher the sleep quality. (2) Social support positively predicted psychological resilience and perceived stress, and perceived stress negatively predicted PSQI. (3) Social support can affect sleep quality through the mediating role of psychological resilience and perceived stress, and the mediating role includes two paths: the single mediating role of perceived stress and the chain mediating role of psychological resilience-perceived stress. (4) Gender moderates the relationship between social support and perceived stress, and the influence of social support on perceived stress of women is higher than that of men. Gender moderates the relationship between psychological resilience and PSQI, and only women’s psychological resilience had a negatively predictive effect on PSQI, while men did not, which means that psychological resilience of female frontline community workers can positively predict sleep quality. This research reveals the relationship between social support and sleep quality and its mechanism and verifies that social support can indirectly affect physical health through psychological resilience and perceived stress. It provides reference suggestions and intervention guidance for improving the sleep quality of community workers.
Keywords: COVID-19; social support; sleep quality; psychological resilience; perceived stress; mediating effect; community workers
The coronavirus disease 2019 (COVID-19) has been declared a global public health emergency (PHEIC) by WHO. To counter the rapid spread of the COVID-19 infection epidemic, strict prevention and control measures, such as strict quarantines, have been instituted. Everyone feels they are in danger, and their mental health and sleep quality have been greatly challenged. Front-line staff is closest to the threat posed by the coronavirus disease.
Some studies have shown that earthquakes, SARS, and Ebola outbreaks will affect the mental health of the residents at that time [1–3]. For example, compared with the community samples, SARS survivors had significantly more distress and poor quality of life [4]. PTSD was associated with higher scores of coping efforts (including self-distraction, behavioral disengagement, social support, venting, planning, and self-blame), but not with direct exposure factors (such as contact with suspected SARS patients or working in a hot room/tent) [5]. The post-earthquake stress response is very high and unstable within one month after the earthquake, which indicates that psychological first aid is necessary for post-traumatic events [6].
Studies have shown that better social support is negatively correlated with post-traumatic stress, perception of SARS related stress and important buffering of negative effects [7]. The improved social support experienced by pregnant women during SARS has buffered the stress associated with the outbreak [8]. Post-earthquake psychological related research shows that increasing children’s social support can reduce PTSD symptoms [6]. Studies have shown that among front-line medical staff, perceived stress and sleep quality are impacted by the epidemic, and perceived social support can buffer the effects of perceived stress on sleep quality; however, social support does not directly affect sleep quality [9]. In addition to front-line medical staff, the dangers and pressures faced by front-line community workers are often overlooked. In this epidemic, countless community workers across the country are working actively on the front lines to address the needs of different families and taking every precaution to prevent the spread of the virus. They need and deserve more attention and support.
This research focuses on the mediating effects of these community workers’ psychological resilience and perceived stress on the impact of social support on sleep quality. In this survey, the interviewees were all new coronavirus front-line community workers, and their perceived stress was considered to be mental stress and negative emotions mainly caused by the epidemic.
1.1 Social Support and Sleep Quality
Sleep quality is a key indicator of health. For community workers, good sleep quality can not only help them better treat the public but also maintain the best state of their immune system to prevent infection [10]. Mental health and sleep are also affected by many social and cultural factors [9]. Social support refers to the care and support from others [11]. Social support can be classified into two types: one is objective, practical or visible support, including direct material support and social networks; the other is subjective, experienced or emotional support, which refers to individual feelings, such as emotional experiences and/or degree of satisfaction with being respected, supported, and understood in society [10]. However, objective social support and subjectively perceived support from others have different effects on health [3,4]. This research focuses on the subjectively perceived social support, that means the effective emotional support and help from relatives, friends, leaders, and colleagues in life, and the impact on mental and physical health.
Previous studies have found that adequate social support has a positive impact on mental health and sleep function [12]. During the COVID-19 infection epidemic, the level of social support of medical staff was positively correlated with sleep quality [9]. It is found that for women, the social support of family members is significantly related to their sleep quality [9]. Research on infertile women found that social support plays a moderating role between sleep quality and anxiety and depression [10]. Studies on sleep quality of the elderly have found that social support from being close to others can significantly improve sleep quality [13]. There is a significant positive correlation between sleep quality and social support in the elderly [14]. Based on this, we propose hypothesis 1: There is a significant correlation between social support and sleep quality.
1.2 The Mediating Role of Psychological Resilience
The research found that there is a significant correlation between social support and psychological resilience [15–22]. Psychological resilience (PR) is an evaluation of personal stress coping ability. High psychological resilience can make people better recover from stress events and improve their mental health under pressure. Individuals with a high sense of social support are more likely to recover from negative events when facing stressful events because they feel more support and experience more emotional support. This may be the reason why social support is positively correlated with psychological resilience. Everyone’s psychological resilience is constantly changing under the influence of external and internal factors [23]. Effective social support can help people cope with the crisis and enhance their adaptability to change [24]. The results show that psychological resilience is positively correlated with perceived social support [15,16,22].
Similarly, the research also found a significant positive correlation between sleep quality and psychological resilience [25]. Studies have found that improving psychological resilience indirectly improves sleep quality [26]. Training emotional psychological resilience can improve sleep quality [27,28].
According to the stress-buffering theory of social support. Protective effects of good social support foster resilience; meanwhile, resilience also enhances people’s ability to cope with stress [29]. Therefore, we propose hypothesis 2: Psychological resilience plays a mediating role between social support and sleep quality.
1.3 The Mediating Role of Perceived Stress
The COVID-19 infection epidemic is an acute stress event. Studies have found that stress leads to abnormal decreases in hormones such as cortisol and progesterone. Corticosteroids may play a negative role in reducing the negative emotions of patients through corticosteroids [30]. The results showed that the degree of psychological distress of medical staff was great, including the symptoms of post-traumatic stress disorder (PTSD) [31]. Residents living in Ebola virus outbreak areas reported more somatization and anxiety symptoms, dysfunction, and/or Ebola-related concerns [2].
It is found that social support is negatively correlated with perceived stress [32–35]. Social support was negatively correlated with post-traumatic stress disorder (PTSD) [36,37]. The quality of perceived social support, rather than quantity, reduces blood pressure’s response to stress [38]. Perceived stress can lead to a decline in health and well-being. Conversely, health problems and unhappiness can also lead people to think that environmental stress is extremely high [39].
Also, the research found that there was a significant correlation between perceived stress and sleep quality [40–45]. There was a significant negative correlation between perceived stress and sleep quality [46–48]. There was a significant positive correlation between stress perception and fatigue [49].
On the contrary, other studies have found that sleep quality is significantly positively correlated with stress perception [48,50], for example, occupational stress positively predicts sleep quality [51]. The level of stress management was positively correlated with sleep quality [52]. Mindfulness-based decompression significantly improves sleep quality [53,54]. Based on this, we propose hypothesis 3: Perceived stress mediates social support and sleep quality.
1.4 The Chain Intermediary between Psychological Resilience and Stress Mediates
Previous studies have found that psychological resilience is negatively correlated with perceived stress [34,55–59]. Psychological resilience significantly negatively predicted perceived stress [39,60,61]. Perceived stress can regulate the protective effect of psychological resilience on suicide [62].
It is found that psychological resilience is related to stressful life events. When more stress events affect individuals, psychological resilience can cushion perceived stress; but when stress is not chronic, psychological resilience can’t cushion stress [63]. It is found that acute stress is significantly correlated with cognitive emotion regulation, social support, and resilience. Social support and resilience have multiple mediating effects on acute stress response [64].
Primarily, According to the stress-buffering theory of social support [24,29]. Protective effects of good social support foster resilience; meanwhile, resilience also enhances people’s ability to cope with stress [65]. The level of perceived stress is tightly related to sleep quality since the stress system serves as effectors on the wake-sleep centers of the brain [66]; therefore, sleep quality is added to the model, supposed to be affected by the level of perceived stress. Secondly, according to the main-effect theory of social support [29], social support is hypothesized to be directly associated with sleep quality in the model. Therefore, this research further proposes Hypothesis 4: Psychological resilience and perceived stress play a chain mediating role between social support and sleep quality.
1.5 The Moderating Effect of Gender on Mediating Effect
Researchers have used different methods to measure psychological resilience and found that men have stronger psychological resilience than women [67]. On the contrary, the research of the elderly found that the psychological resilience level of elderly women was higher than that of elderly men [68]. In addition, the research found that the sleep quality of adult women is worse than that of adult men [69]. Based on this, this research will further examine the gender moderating effect on mediating role after testing the mediating effect. To sum up, by combing and analyzing the existing literature, this paper discusses the relationship between social support and sleep quality, gender differences, and its mechanism to improve the sleep quality of front-line community workers in Wuhan During the COVID-19 infection epidemic.
The four variables, social support, psychological resilience, perceived stress, and sleep quality, and their interaction can be analyzed by structural equation modeling (SEM), which is a multivariate analysis method to determine the structural relationship between the measured variables. Therefore, this observational research aims to determine the impact of social support on the sleep quality of front-line community workers in Wuhan by using SEM. This research mainly analyzes the direct impact of social support on sleep quality, and the mediating role of different psychological states in the impact of social support on sleep quality, and builds a hypothetical model as shown in Fig. 1.
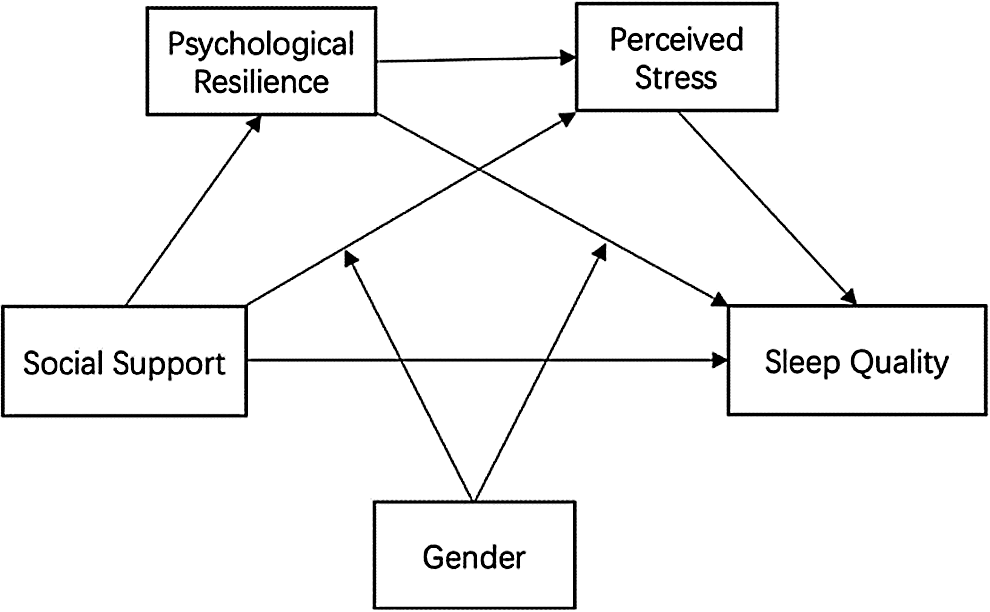
Figure 1: Hypothesis model
2.1 Participants and Procedure
The study was designed in accordance with the tenets of the Declaration of Helsinki. Approval from the ethical authority of School of Educational Science, Huazhong University of Science and Technology was granted. Confidentiality was ensured by placing anonymous codes on the self-report questionnaires, and subjects signed a statement providing informed consent.
Using the Questionnaire Star platform (Wenjuanxing, http://www.wjx.cn), there are 500 front-line community workers in Wuhan, including 322 males and 178 females with an average age of 38.7 ± 10.3 years. After completing the questionnaire, some interviews were conducted with these community workers to understand the nature and content of their work. We learned that their tasks included door-to-door investigation of febrile patients, reporting of the epidemic situation, sending confirmed and suspected patients to hospitals, and solving the household chores of isolated residents, such as delivering vegetables, buying medicine, and disinfecting public places in the community. As a matter of fact, one person took many positions.
The perceived social support scale (PSSS) [17]. It contains 12 items and includes three subscales: family support, friend support, and other support. For example: “I can get emotional help and support from my family when I need it” (family support); “my friends can really help me” (friend support); some people (leaders, relatives, colleagues) will support me when I encounter problems. The higher the score, the higher the level of social support (1 = strongly opposed, 7 = strongly agreed). In this research, the Cronbach α coefficient of the scale was 0.963.
The Connor-Davidson Resilience Scale (CD-RISC) was originally developed by Connor and Davidson [15,70]. After that, Campbell sills and Stein (2007) revised the CD-RISC. The revised version contained 10 items, with 5 grades of score: 1 for “never,” 5 for “always.” The score of 10 items was added up to get the score of psychological resilience. In this research, the Cronbach α coefficient of the scale was 0.943.
The perceived stress scale (PSS) was used to evaluate the perceived stress [40,71]. In order to measure the perceived stress more comprehensively, 10 items were randomly selected from the perceived stress scale. In this research, the Cronbach α coefficient of the scale was 0.878.
The Pittsburgh sleep quality index (PSQI) was compiled by Buysse et al. [13]. There were 18 self-rated items on the scale. Seven components of sleep quality were measured: subjective sleep quality, sleep time, the amount of sleep, sleep efficiency, sleep disorders, hypnotics, and daytime dysfunction. The higher the score, the worse the sleep quality. In this research, the Cronbach α coefficient of the scale was 0.917.
SPSS 25.0 and Process Syntax were used to perform the regression analysis and construct the predicted moderated mediation model. All data were expressed as the mean ± standard deviation (SD), median (interquartile range), or number (frequency). The data of social support, resilience, perceived stress and PSQI showed a non-normal distribution, so we normalized the data using Cumulative Relative Frequency Distribution method and standardization method. After normalization, the data of PSQI showed the normal distribution, p > 0.05, skewness = 0.089 ± 0.109, kurtosis = −0.237 ± 0.218; the data of perceived stress showed the normal distribution, p > 0.05, skewness = −0.080 ± 0.109, kurtosis = −0.257 ± 0.218. However, the data of social support still did not obey the normal distribution, p < 0.05, skewness = −0.242 ± 0.109, kurtosis = −0.498 ± 0.218; the data of psychological resilience also did not obey the normal distribution, p < 0.05, skewness = −0.326 ± 0.109, kurtosis = −0.545 ± 0.218. Therefore, we use the method of nonparametric test in the follow-up statistics. Non-parametric test was used to compare the psychological resilience and social support of different gender groups separately. Pearson correlation was used to analyze the correlation among social support, psychological resilience, perceived stress and PSQI. All the tests were bilateral, and the significance level was α = 0.05.
The possible multicollinearity was quantified using the variance infiltration factor (VIF). This parameter indicates how much the variance of a given covariable is increased compared to complete absence of correlation (orthogonality) and is generally agreed to indicate potential model instability if higher than five. In order to detect potentially influential multicollinearity between social support, psychological resilience and perceived stress in the constructed models we calculated the variance inflation factor (VIF). We used linear regression analysis for collinearity diagnosis, with PSQI as the dependent variable and social support, resilience and persistent stress as independent variables. The results showed that the VIF of social support = 1.617; the VIF of persistent stress = 1.568; the VIF of psychological resistance = 1.927. It shows that there is no serious multicollinearity problem in our data.
3.1 Control and Inspection of Common Method Deviation
In this research, Haman single factor method was used to test the common method bias. All items of social support, resilience, perceived stress and sleep quality index were analyzed without rotation to determine the minimum number of factors necessary for variable variation. The results showed that there were 18 factors with eigenvalues greater than 1, and the variance explained by the first factor was 34.87%, less than the critical standard of 40%, indicating that there was no serious common method deviation in this research.
The results of the correlation analysis are shown in Tab. 1. The sleep quality index (PSQI) of front-line social workers was significantly negatively correlated with social support, psychological resilience, and perceived stress (p < 0.001); there was a significant positive correlation between social support, psychological resilience, and perceived stress (p < 0.001). In this research, the relationship between the variables is relatively close, and the absolute value of the correlation coefficient is between 0.260 and 0.597, which is suitable for further analysis.
Table 1: Correlation Analysis of social support, psychological resilience, perceived stress and PSQI (n = 500)
3.3 Two Independent Samples Nonparametric Test of Psychological Resilience and Social Support
Two independent samples nonparametric test was conducted on the psychological resilience of subjects of different genders, and Mann-Whitney U test was used. The results showed that the level of psychological resilience of males was significantly higher than that of females (p < 0.001).
Similarly, two independent samples nonparametric test was conducted on the social support of subjects of different genders, and Mann-Whitney U test was used. The results showed that the level of social support of males was also significantly higher than that of females (p = 0.031).
3.4 The Relationship between Perceived Stress, Gender and Contact History of Front-Line Community Workers
Then, we conducted a one-way ANOVA analysis on the relationship between perceived stress of front-line community workers and gender and contact history. Before the analysis of variance, the homogeneity test of variance is carried out. In Levene’s test, F(1, 498) = 0.982, p = 0.322, indicating homogeneity of variance and analysis of variance can be carried out.
Taking the perceived stress of community workers as dependent variables, the perceived stress scores of different genders and contact history were analyzed by one-way ANOVA. The results showed that the main effect of contact history on perceived stress was significant, F(1, 498) = 16.859, p = 0.004, η2p = 0.033; the main effect of gender on perceived stress was significant, F(1, 498) = 8.550, p = 0.650, η2p = 0.017; the interaction between gender and contact history was significant F(1, 498) = 2.774, p = 0.096, η2p = .006. Further simple effect analysis showed that for male front-line community workers, the stress they perceived when they had contact history (M = 30.950, SD = 0.795) was significantly lower than that of those without contact history (M = 33.872, SD = 0.457), F(1, 130) = 10.162, p = 0.002; for female front-line community workers, the stress they felt when they had contact history (M = 8.325, SD = 0.454) was also significantly lower than that of the people without contact history (M = 6.541, SD = 0.261), F(1, 130) = 11.576, p < 0.001. This shows that, for both male and female front-line community workers, compared with those with contact history, the front-line community workers without contact history feel a lower stress level. See Tab. 2.
Table 2: One-way ANOVA of perceived stress, gender and contact history

3.5 Relationship between Sleep Quality Index (PSQI) and Gender, Contact History of Front-Line Community Workers
Next, we analyzed the relationship between sleep quality index (PSQI) and gender and contact history of front-line community workers by one-way ANOVA. Before the analysis of variance, the homogeneity test of variance is carried out. In Levene’s test, F(1, 498) = 0.510, p = 0.476, indicating homogeneity of variance and analysis of variance can be carried out.
Taking the PSQI of front-line community workers as a dependent variable, the single factor analysis of variance was conducted on the PSQI of different gender and contact history. The results showed that the main effect of contact history on PSQI was significant, F(1, 498) = 8.238, p = 0.004, η2p = 0.016; however, the main effect of gender on PSQI was not significant, F(1, 498) = 0.207, p = 0.650, η2p < .001; the interaction between gender and contact history on PSQI was not significant, F(1, 498)= 0.071, p = 0.791, η2p < .001. Further simple effect analysis showed that for male first-line community workers, PSQI (M = 8.325, SD = 0.454) with contact history was significantly higher than that without contact history (M = 6.541, SD = 0.261), F(1, 130) = 11.576, p < 0.001; while for female community workers, there was no significant difference in their sleep quality. This shows that for male front-line community workers, contact history has an impact on sleep quality, compared with community workers without contact history, front-line community workers with contact history have poorer sleep quality, while women do not have this difference. See Tab. 3.
Table 3: One-way ANOVA of sleep quality index (PSQI), gender and contact history

3.6 Verification of Multiple Mediation Model
In order to effectively control the measurement error, the structural equation modeling method is used to test the multiple mediating effects. Firstly, after controlling gender, age, and working years, the total effect of social support on sleep quality index was tested, and the path coefficient was significant (β = −0.260, t = −6.004, SE = 0.043, p < 0.001). Secondly, the mediating variables, psychological resilience, and perceived stress are added to the model to obtain the mediating model shown in Fig. 2. The results show that (see Tab. 4), social support can significantly positively predict psychological resilience; when social support and psychological resilience predict perceived stress at the same time, social support and psychological resilience have a significant positive predictive effect; when the three predict the sleep quality of individuals at the same time, perceived stress can significantly predict individual sleep quality, while social support and psychological resilience have no significant predictive effect on sleep quality. This indicates that psychological resilience and perceived stress play a completely mediating role in the influence of social support on sleep quality.
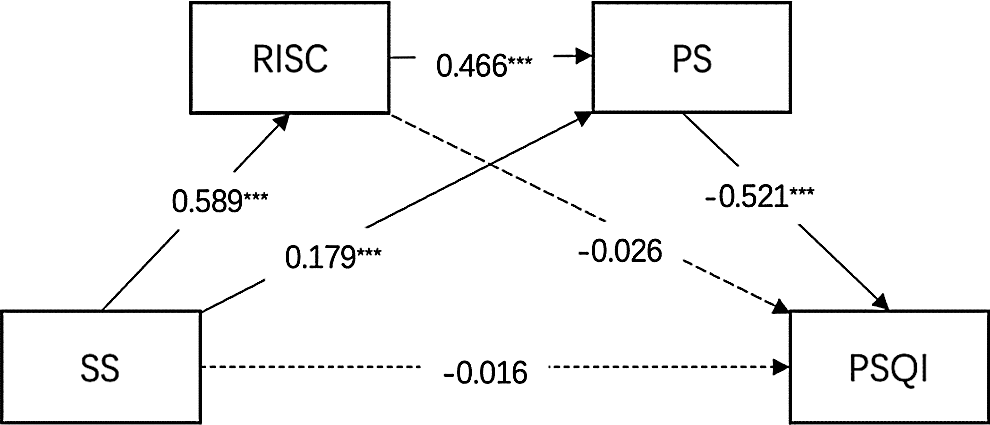
Figure 2: Mediating model and gender differences (n = 500). Note: ***p < 0.001, *p < 0.05. All the original continuous variable data are standardized. The data are standardized path coefficient. Variables include social support (SS), psychological resilience (RISC), perceived stress (PS), and Pittsburgh sleep Quality Index (PSQI) of community workers (with standardized beta weighting)
Table 4: Psychological resilience and perceived stress chain mediators. Regression analysis of the relationship between variables in the model (n = 500)

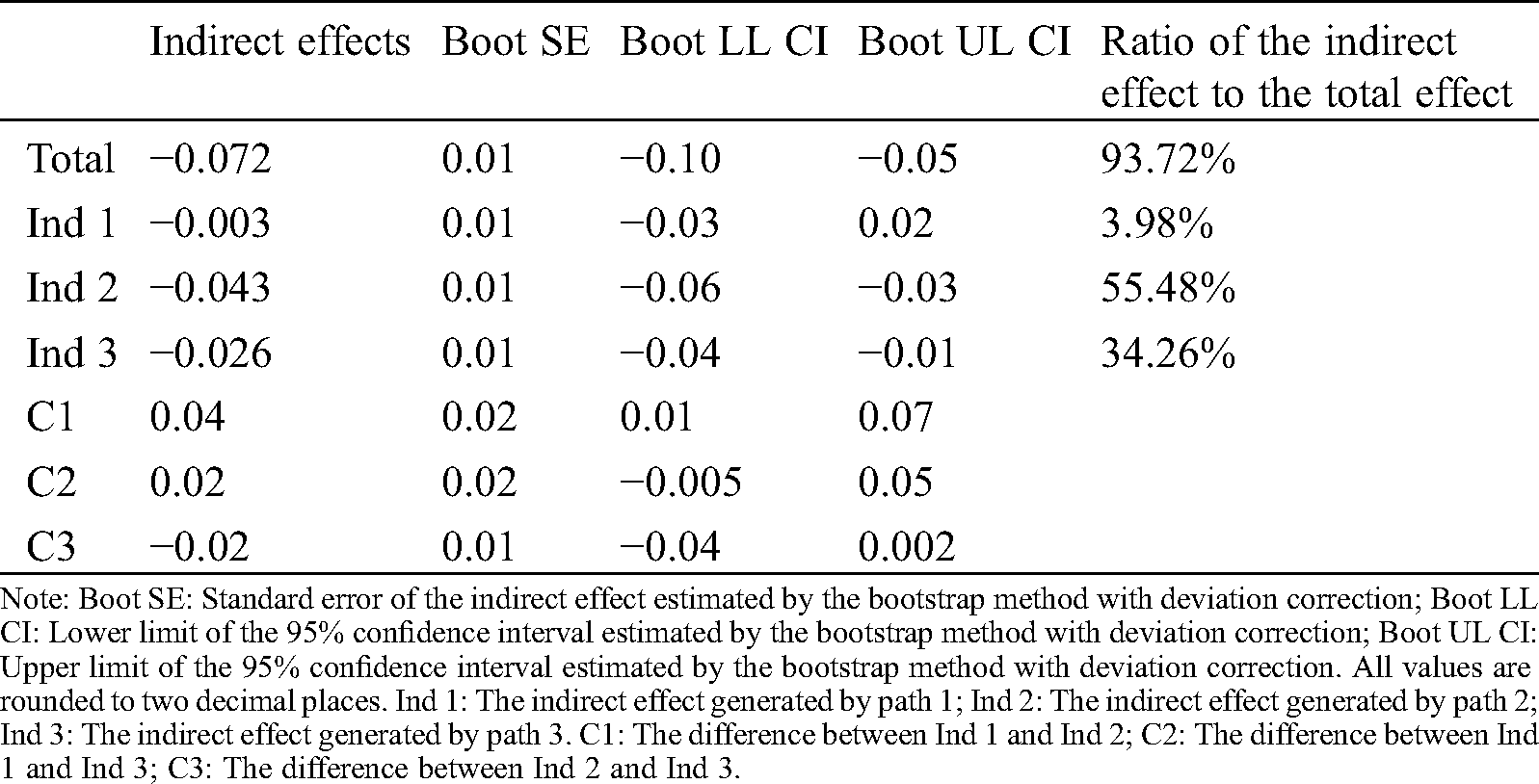
Next, the results of the direct test of mediating effect (see Tab. 5) showed that the bootstrap 95% confidence interval of the total indirect effects of psychological resilience and perceived stress did not contain 0 value, indicating that the two mediators had a significant mediating effect between social support and sleep quality. The mediating effect is composed of three indirect effects: First, the indirect effect produced by the path of social support → psychological resilience → sleep quality, with a confidence interval of 0, indicating that the indirect effect produced by this pathway is not significant; second, the confidence interval of the indirect effect produced by the path of social support → perceived stress → sleep quality does not contain 0 value, indicating the perceived Stress has a significant indirect effect (−0.043, 55.48%) between social support and sleep quality; third, the confidence interval of indirect effect 3 produced by the path of social support → psychological resilience → perceived stress → sleep quality does not contain 0 value, indicating that the indirect effect produced by this pathway (−0.026, 34.26%) also reaches a significant level.
Table 5: Analysis of mediating role
3.7 The Moderating Effect of Gender on the Relationship between Social Support and Perceived Stress
According to the results of previous studies, there are significant differences in perceived stress between males and females. Based on this, this research examined whether the mediating effects of psychological resilience and perceived stress have cross-gender consistency. In order to reduce multicollinearity, all variables are standardized. First, we use perceived stress as a dependent variable to test whether gender has a moderating effect on the relationship between social support and perceived stress. The results showed that social support and gender had no significant predictive effect on perceived stress (β = 0.129, t = 1.484, SE = 0.086, p = 0.138). There was no interaction effect between gender and social support.
Secondly, the moderating role of gender is shown in Tab. 6. After adding gender into the model, the multiplicative term of social support and gender had a significant positive predictive effect on perceived stress (β = 0.163, t = 2.082, p = 0.038). It shows that gender plays a moderating role in the relationship between social support and perceived stress. The moderating effect is shown in Tab. 6 and Fig. 3. Further simple slope analysis showed that: For male subjects, social support had a significant positive predictive effect on perceived stress, simple slope = 0.122, t = 2.262, SE = 0.052, p = 0.019; for female subjects, social support had a significant positive predictive effect on perceived stress, simple slope = 0.285, t = 4.091, SE = 0.070, p < 0.001. Compared with male subjects, female subjects’ social support has a stronger positive predictive effect on perceived stress, and the predictive effect of social support on perceived stress shows an upward trend. See Tab. 7 and Fig. 4.
Table 6: Test of moderating effect (n = 500)
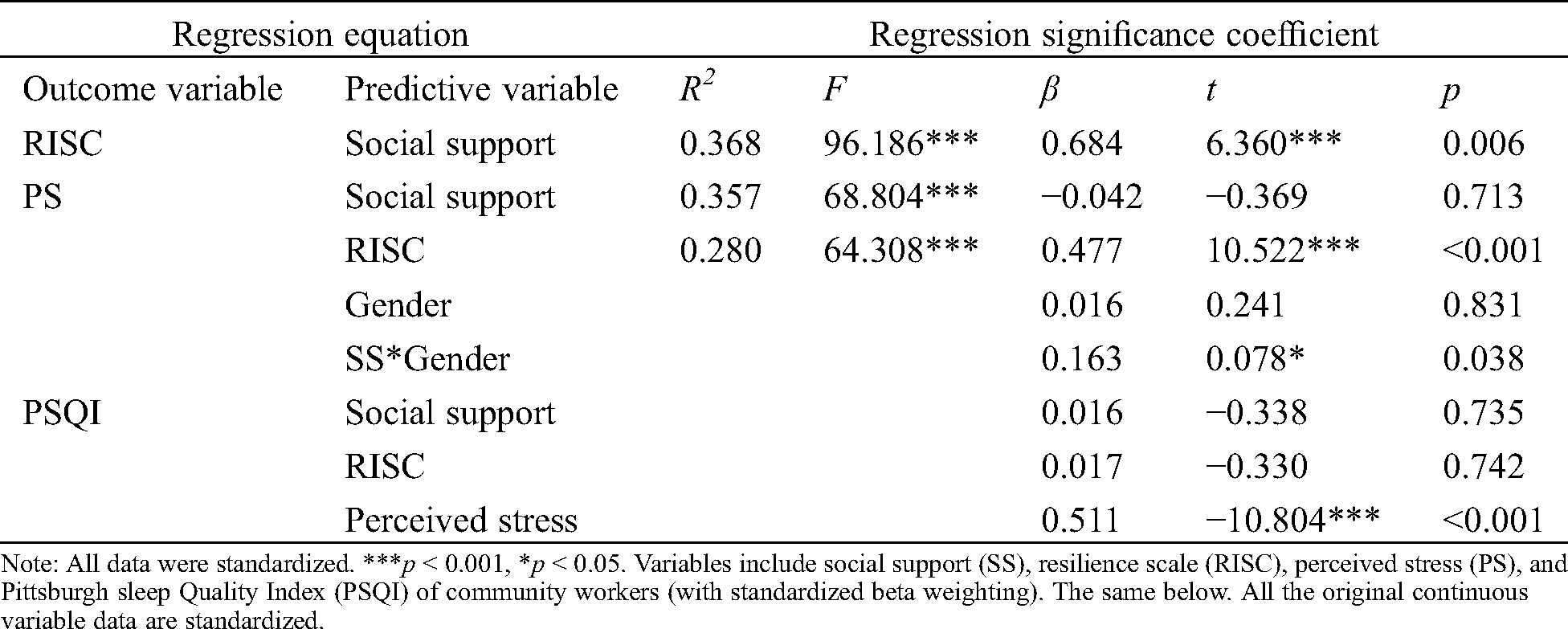
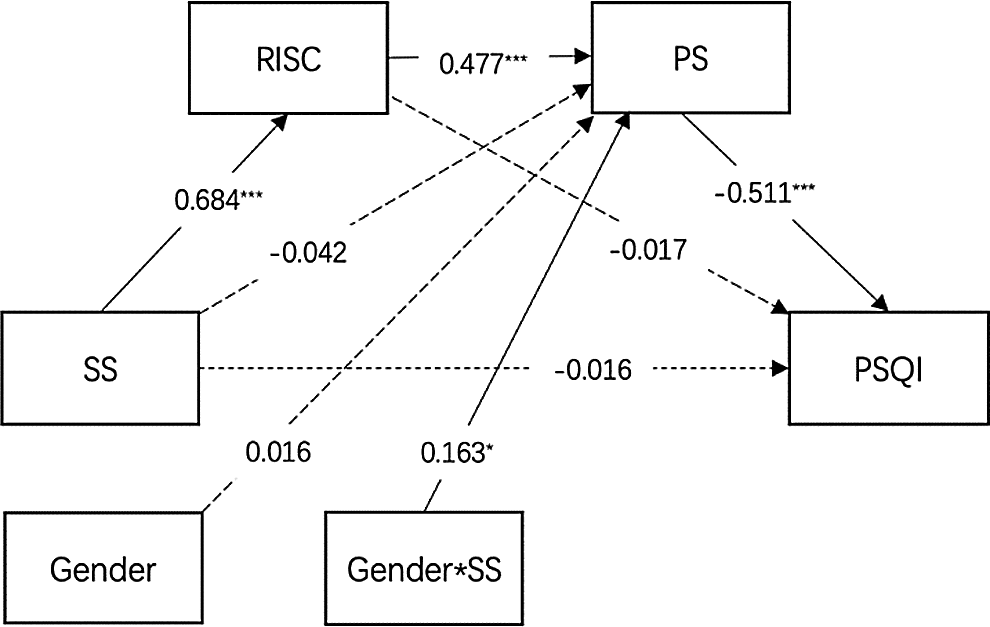
Figure 3: The moderating effect of gender on the relationship between social support and perceived stress. Note: All data were standardized. ***p < 0.001, *p < 0.05. Variables include social support (SS), psychological resilience (RISC), perceived stress (PS), and Pittsburgh sleep Quality Index (PSQI) of community workers (with standardized beta weighting)
Table 7: The moderating effect of gender on mediating variables
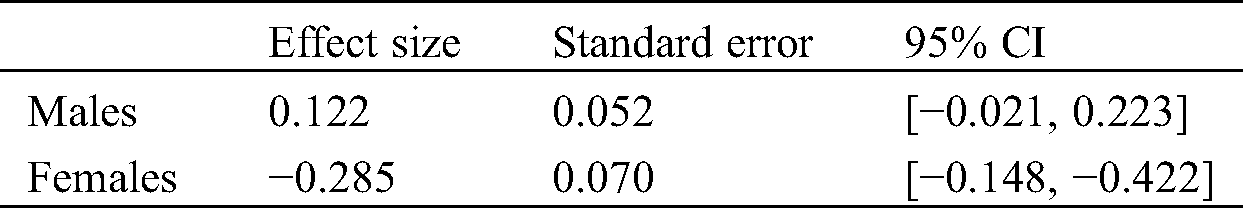

Figure 4: The moderating effect of gender on the relationship between social support and perceived stress
3.8 The Moderating Effect of Gender on the Relationship between Psychological Resilience and PSQI
According to the results of previous studies, there are significant differences in psychological resilience between males and females. Based on this, this research examined whether the mediating effects of psychological resilience and Pittsburgh sleep Quality Index (PSQI) have cross-gender consistency. Firstly, we use PSQI as a dependent variable to test whether gender has a moderating effect on the relationship between psychological resilience and PSQI. The results showed that psychological resilience and gender had no significant predictive effect on PSQI (β = −0.186, t = −2.001, SE = 0.093, p = 0.046). There was a significant interaction effect between gender and psychological resilience.
Secondly, the moderating role of gender is shown in Tab. 8. After adding gender into the model, the multiplicative term of psychological resilience and gender had a significant positive predictive effect on PSQI (β = −0.233, t = −1.979, p = 0.048). It shows that gender plays a moderating role in the relationship between psychological resilience and PSQI. The moderating effect is shown in Tab. 8 and Fig. 5. Further simple slope analysis showed that: for male subjects, psychological resilience had no significant predictive effect on PSQI, simple slope = 0.034, t = 0.549, SE = 0.062, p = 0.583; for female subjects, psychological resilience had a significant negative predictive effect on Pittsburgh sleep Quality Index (PSQI), simple slope = −0.163, t = −1.870, SE = 0.087, p = 0.042. Compared with male subjects, female subjects’ psychological resilience has a stronger negative predictive effect on PSQI. Moreover, the relationship between psychological resilience and PSQI shows a downward trend. See Tab. 9 and Fig. 6.
Table 8: Test of moderating effect (n = 500)
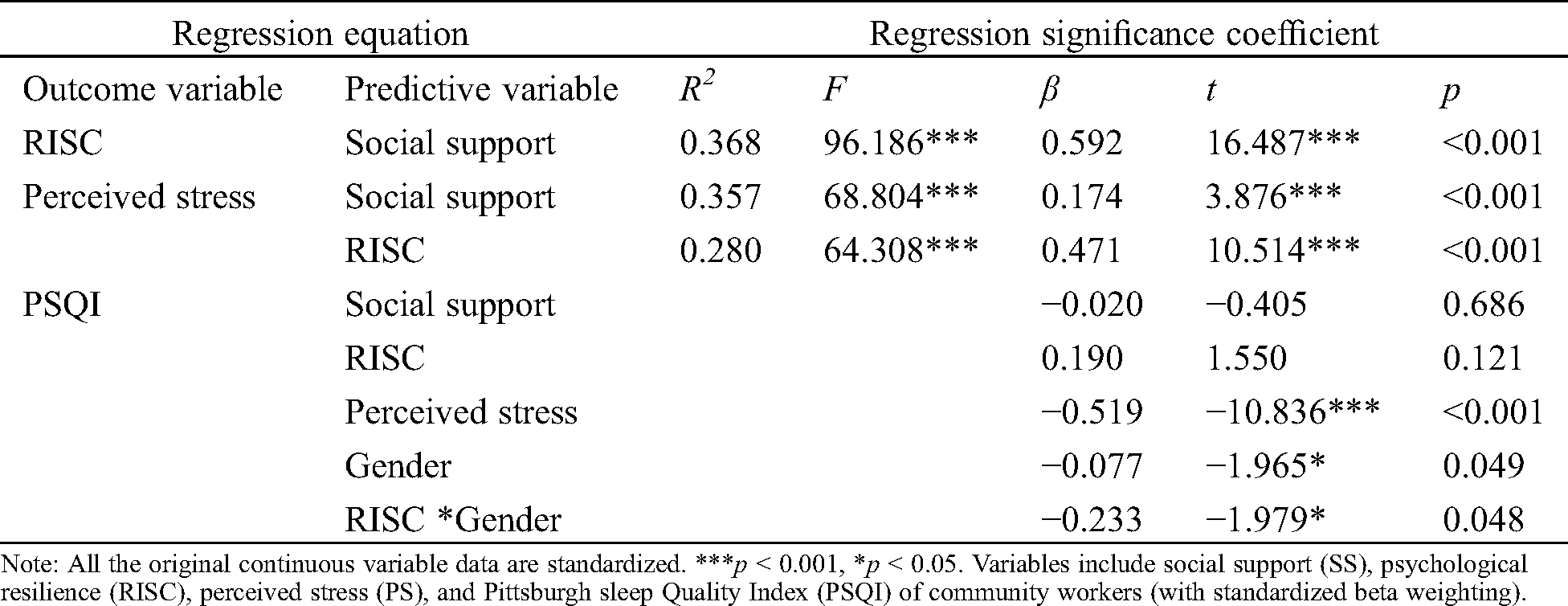

Figure 5: The moderating effect of gender on the relationship between psychological resilience and PSQI. Note: All the original continuous variable data are standardized. ***p < 0.001, *p < 0.05
Table 9: The moderating effect of gender on mediating variables
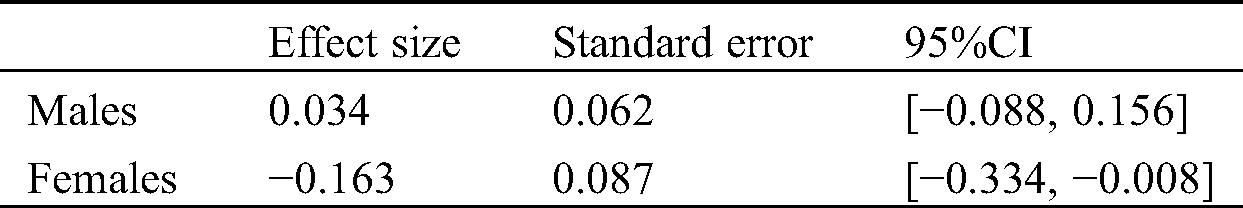

Figure 6: The moderating effect of gender on the relationship between psychological resilience and PSQI
4.1 Social Support and Sleep Quality of Community Workers
The purpose of this research was to explore the relationship between social support and sleep quality in Wuhan during the epidemic period. The results showed that there was a significant positive correlation between social support and sleep quality, which verified hypothesis 1. This result is consistent with the existing research results [9]. It can be seen that physical and mental health and security, and then have a higher quality of sleep. Therefore, for the physical and mental health of front-line community workers, especially their sleep quality under the epidemic situation, social support plays an important role; the support from family, friends, and leaders, as well as the respect, support and, care from families, friends, and colleagues may promote the improvement of sleep quality to a certain extent. The previous study found that positive attitudes and strong social and family support may help to resist acute stress [72]. This is consistent with the stress-buffering theory of social support [24,29].
4.2 The Mediating Role of Psychological Resilience and Perceived Stress
This research found that the mediating role of psychological resilience between social support and sleep quality is not significant, hypothesis 2 has not been verified. However, the results of correlation analysis show that there is a significant positive correlation between psychological resilience and social support, which may be due to the fact that individuals will have more psychological resources to deal with stressful events when they feel more social support and get more respect and support. Therefore, they are more likely to recover from the stress events faster and show higher psychological resilience [15–22]. The results of correlation analysis also found that there is a significant positive correlation between psychological resilience and sleep quality, which may be due to the fact that individuals with high psychological resilience can better face the stressful events in life and better deal with the impact of negative emotions. Therefore, the mental health level is relatively high, and the sleep quality may be improved, which is consistent with the existing research [15–22]. The community work has certain risks, and even directly contacts with the confirmed patients or suspected patients. Compared with the general work, the possibility of exposure to the risk is high. The results showed that the degree of psychological distress of medical staff was great, including the symptoms of post-traumatic stress disorder (PTSD) [31]. In this special situation, social support, as one of the important sources of strength, will inevitably have an impact on the psychological and physical health of front-line community workers. Therefore, the improvement of psychological resilience is helpful to improve their sleep quality and promote their physical and mental health.
This research also found that perceived stress played a mediating role between social support and sleep quality, which verified hypothesis 3. This research explored the relationship between these three variables and confirmed that social support is an important factor affecting sleep quality, and it also increases the mediating factor of social support on sleep quality. However, this is not consistent with the research results of high social support promoting perceived stress [32–35]. But it is consistent with the research that perceived stress has a positive effect on sleep quality [48,50]. The reason for the inconsistency with the existing research results may be due to the particularity of the COVID-19 infection epidemic. During the outbreak of the COVID-19 infection epidemic, the risk of illness is much higher than that before the outbreak of the COVID-19 infection epidemic. Especially for Wuhan residents, people are in danger. Their mental health and pressure may not be consistent with those before the outbreak of the COVID-19 infection epidemic, and the perceived stress baseline is higher than that before the COVID-19 infection epidemic. Moreover, due to the sudden outbreak of the epidemic, the pressure generated is severe.
In addition, this research examined the chain mediating role of psychological resilience and perceived stress between social support and sleep quality of community workers during the COVID-19 infection epidemic. The perceived social support of community workers can indirectly predict sleep quality through the chain mediation of psychological resilience perceived stress, which verifies Hypothesis 4. This is inconsistent with the previous results that psychological resilience helps to reduce perceived stress. Previous studies have found that psychological resilience is significantly negatively correlated with perceived stress [34,55–59]. However, this research found a significant positive correlation between psychological resilience and perceived stress. The reason may be that in a special period such as the COVID-19 infection epidemic, the perceived stress level of residents is higher than that before the outbreak of the COVID-19 infection epidemic, especially the front-line community workers in Wuhan have a high chance to be exposed to confirmed patients or suspected patients and face a great risk of infection. Previous studies can explain this phenomenon. Studies have found that psychological resilience is related to stressful life events. When more stress events affect individuals, psychological resilience can cushion perceived stress; but when stress is not chronic stress, psychological resilience can not cushion stress [63]. However, the COVID-19 infection epidemic is an acute stress event. Studies have found that stress leads to abnormal decreases in hormones such as cortisol and progesterone. Corticosteroids may play a negative role in reducing the negative emotions of patients through corticosteroids [30].
The results showed that the level of psychological resilience of males was significantly higher than that of females. Similarly, the results showed that the level of perceived stress of males was significantly higher than that of females.
In addition, this study found that there is an interaction between gender and contact history in terms of sleep quality. Specifically, for male front-line community workers, their sleep quality will be affected by contact history. Male front-line community workers with contact history have worse sleep quality, while female front-line community workers have no such difference. Therefore, we should pay more attention to the male front-line social workers who have contact history in the later stage of psychological guidance or counseling for such groups. In addition, the results showed that the level of psychological resilience of males was significantly higher than that of females. Similarly, the results showed that the level of perceived stress of males was significantly higher than that of females.
In the model of this study, gender moderates the relationship between social support and perceived stress, and the influence of social support on perceived stress of women is higher than that of men. In addition, gender moderates the relationship between psychological resilience and PSQI, and only women’s psychological resilience had a negatively predictive effect on PSQI, while men did not, which means that psychological resilience of female frontline community workers can positively predict sleep quality. The mediating effect of gender differences may be due to the lower resilience of women than men [67], for example, women are less likely to recover from stressful events than men. This is consistent with the results of previous studies [67], and the same results were obtained in this research.
In conclusion, during the COVID-19 infection epidemic, there are two ways to influence the sense of social support on the physical health of front-line community workers in Wuhan city. Social support is an environmental variable to improve sleep quality, and social support acts on sleep quality through the chain mediation of psychological resilience and perceived pressure. This research reveals that under the COVID-19 infection epidemic, for the community workers working in the front line, we should pay attention to improve their social support, improve their psychological resilience, reduce their perceived pressure so as to improve their sleep quality and promote their mental and physical health.
This research has the following limitations. Firstly, this survey focuses on the relationship between social support and sleep quality during the period of the COVID-19 infection epidemic, as well as the mediating role of psychological resilience and perceived stress, without considering the long-term impact of social support before the occurrence of the COVID-19 infection epidemic; secondly, in the analysis of perceived stress and sleep quality, various sources of stress are not taken into account; thirdly, the relationship between perceived stress and sleep quality is analyzed, which is cross-sectional research, only using the form of a questionnaire survey, so long-term follow-up experiments and more field studies are needed to verify the experimental results.
1. During the period of the COVID-19 infection epidemic, there was a significant positive correlation between social support and sleep quality of community workers.
2. Psychological resilience and perceived stress play a mediating role between social support and sleep quality, and the mediation includes two paths: the single mediating role of perceived stress and the chain mediating role of psychological resilience and perceived stress.
3. Gender moderates the relationship between social support and perceived stress, and the influence of social support on perceived stress of women is higher than that of men. Gender moderates the relationship between psychological resilience and PSQI, and only women’s psychological resilience had a negatively predictive effect on PSQI, while men did not, which means that psychological resilience of female frontline community workers can positively predict sleep quality.
Acknowledgement: We thank all participants for their time and interest as well as the editor and reviewers for their valuable feedback.
Funding Statement: This study was supported and granted by the “National Social Science Fund Emergency Management System Construction Research Special Project (20VYJ040),” “Central China Think Tank Special Key Projects (2020HZZK031),” “Key Projects of Educational Science Planning of Hubei Province (2019CFB425)” and “Ministry of Education of Humanities and Social Sciences Research Fund (19YJA880082)” to YZ.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Ko, C., Yen, C., Yen, J., Yang, M. (2006). Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry and Clinical Neurosciences, 60(4), 397–403. DOI 10.1111/j.1440-1819.2006.01522.x. [Google Scholar] [CrossRef]
2. Jose, R., Holman, E. A., Silver, R. C. (2017). The importance of the neighborhood in the 2014 Ebola Outbreak in the United States: Distress, worry, and functioning. Health Psychology, 36(12), 1181–1185. DOI 10.1037/hea0000518. [Google Scholar] [CrossRef]
3. Almutairi, A. F., Adlan, A. A., Balkhy, H. H., Abbas, O. A., Clark, A. M. (2018). “It feels like I’m the dirtiest person in the world.”. Journal of Infection and Public Health, 11(2), 187–191. DOI 10.1016/j.jiph.2017.06.011. [Google Scholar] [CrossRef]
4. Cheng, S. K. W., Sheng, B., Lau, K. K., Wong, C. W., Ng, Y. K. et al. (2004). Adjustment outcomes in Chinese patients following one-month recovery from severe acute respiratory syndrome in Hong Kong. Journal of Nervous and Mental Disease, 192(12), 868–871. DOI 10.1097/01.nmd.0000147169.03998.dc. [Google Scholar] [CrossRef]
5. Sim, K., Chong, P. N., Chan, Y. H., Soon, W. S. W. (2004). Severe acute respiratory syndrome-related psychiatric and posttraumatic morbidities and coping responses in medical staff within a primary health care setting in Singapore. Journal of Clinical Psychiatry, 65(8), 1120–1127. DOI 10.4088/JCP.v65n0815. [Google Scholar] [CrossRef]
6. Cheng, J., Liang, Y. M., Zhou, Y. Y., Eli, B., Liu, Z. K. (2019). Trajectories of PTSD symptoms among children who survived the Lushan earthquake: A four-year longitudinal study. Journal of Affective Disorders, 252, 421–427. DOI 10.1016/j.jad.2019.04.047. [Google Scholar] [CrossRef]
7. Lau, J., Yang, X., Tsui, H., Pang, E., Wing, Y. (2006). Positive mental health-related impacts of the SARS epidemic on the general public in Hong Kong and their associations with other negative impacts. Journal of Infection, 53(2), 114–124. DOI 10.1016/j.jinf.2005.10.019. [Google Scholar] [CrossRef]
8. Lee, D. T. S., Sahota, D., Leung, T. N., Yip, A. S. K., Lee, F. F. Y. et al. (2006). Psychological responses of pregnant women to an infectious outbreak: A case-control study of the 2003 SARS outbreak in Hong Kong. Journal of Psychosomatic Research, 61(5), 707–713. DOI 10.1016/j.jpsychores.2006.08.005. [Google Scholar] [CrossRef]
9. Xiao, H., Zhang, Y., Kong, D., Li, S., Yang, N. (2020). The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Medical Science Monitor, 26, e923549. [Google Scholar]
10. Cui, Y., Li, D., Zhou, B., Lin, Y., Zeng, Y. (2020). Mediating role of social support between sleep quality, anxiety and depressive symptoms in Chinese women undergoing in vitro fertilization treatment. SAGE Open Medicine, 8(1), 205031212093016. DOI 10.1177/2050312120930163. [Google Scholar] [CrossRef]
11. Pow, J., King, D. B., Stephenson, E., DeLongis, A. (2017). Does social support buffer the effects of occupational stress on sleep quality among paramedics? A daily diary study. Journal of Occupational Health Psychology, 22(1), 71–85. DOI 10.1037/a0040107. [Google Scholar] [CrossRef]
12. Chung, J. (2017). Social support, social strain, sleep quality, and actigraphic sleep characteristics: Evidence from a national survey of US adults. Sleep Health, 3(1), 22–27. DOI 10.1016/j.sleh.2016.10.003. [Google Scholar] [CrossRef]
13. Stafford, M., Bendayan, R., Tymoszuk, U., Kuh, D. (2017). Social support from the closest person and sleep quality in later life: Evidence from a British birth cohort study. Journal of Psychosomatic Research, 98, 1–9. DOI 10.1016/j.jpsychores.2017.04.014. [Google Scholar] [CrossRef]
14. Pan, K. C., Hung, S. Y., Chen, C. I., Lu, C. Y., Shih, M. L. et al. (2019). Social support as a mediator between sleep disturbances, depressive symptoms, and health-related quality of life in patients undergoing hemodialysis. PLoS One, 14(4), e0216045. DOI 10.1371/journal.pone.0216045. [Google Scholar] [CrossRef]
15. Zhang, D., Wang, R., Zhao, X., Zhang, J., Jia, J. et al. (2020). Role of resilience and social support in the relationship between loneliness and suicidal ideation among Chinese nursing home residents. Aging & Mental Health, 1–11. DOI 10.1080/13607863.2020.1786798. [Google Scholar] [CrossRef]
16. Yaşar, Ö., Vural-Batık, M., Özdemir, Ş. (2020). Investigating resilience, perceived social support and trait anxiety levels of mothers of school-age children who stutter. CoDAS, 32(2), 299. DOI 10.1590/2317-1782/20192019093. [Google Scholar] [CrossRef]
17. Xiang, Y., Dong, X., Zhao, J. (2020). Effects of envy on depression: The mediating roles of psychological resilience and social support. Psychiatry Investigation, 17(6), 547–555. DOI 10.30773/pi.2019.0266. [Google Scholar] [CrossRef]
18. Xi, Y., Yu, H., Yao, Y., Peng, K., Wang, Y. et al. (2020). Post-traumatic stress disorder and the role of resilience, social support, anxiety and depression after the Jiuzhaigou earthquake: A structural equation model. Asian Journal of Psychiatry, 49, 101958. DOI 10.1016/j.ajp.2020.101958. [Google Scholar] [CrossRef]
19. Tyler, C. M., Henry, R. S., Perrin, P. B., Watson, J. Villaseñor, T. et al. (2020). Structural equation modeling of Parkinson’s Caregiver social support, resilience, and mental health: A strength-based perspective. Neurology Research International, 2020, 1–8. DOI 10.1155/2020/7906547. [Google Scholar] [CrossRef]
20. Ruisoto, P., Contador, I., Fernández-Calvo, B., Serra, L., Jenaro, C. et al. (2020). Mediating effect of social support on the relationship between resilience and burden in caregivers of people with dementia. Archives of Gerontology and Geriatrics, 86, 103952. DOI 10.1016/j.archger.2019.103952. [Google Scholar] [CrossRef]
21. Huang, Y., Wu, R., Wu, J., Yang, Q., Zheng, S. et al. (2020). Psychological resilience, self-acceptance, perceived social support and their associations with mental health of incarcerated offenders in China. Asian Journal of Psychiatry, 52, 102166. DOI 10.1016/j.ajp.2020.102166. [Google Scholar] [CrossRef]
22. Wang, Y., Zhao, Y., Xie, S., Wang, X., Chen, Q. et al. (2019). Resilience mediates the relationship between social support and quality of life in patients with primary glaucoma. Frontiers in Psychiatry, 10, 668. DOI 10.3389/fpsyt.2019.00022. [Google Scholar] [CrossRef]
23. Burnette, C. B., Kwitowski, M. A., Trujillo, M. A., Perrin, P. B. (2019). Body appreciation in lesbian, bisexual, and queer women: Examining a model of social support, resilience, and self-esteem. Health Equity, 3(1), 238–245. DOI 10.1089/heq.2019.0003. [Google Scholar] [CrossRef]
24. Putnam, M. (2018). Loneliness, resilience and social support. Journal of Gerontological Social Work, 61(6), 583. DOI 10.1080/01634372.2018.1499181. [Google Scholar] [CrossRef]
25. Li, T., Cui, C., Li, Y., Wang, L. (2020). The impacts of resilience on the association between illness uncertainty and sleep quality among Chinese women with systemic lupus erythematosus. Clinical Rheumatology, 39(5), 1609–1616. DOI 10.1007/s10067-019-04898-3. [Google Scholar] [CrossRef]
26. Li, Y., Gu, S., Wang, Z., Li, H., Xu, X. et al. (2019). Relationship between stressful life events and sleep quality: Rumination as a mediator and resilience as a moderator. Frontiers in Psychiatry, 10, 98. DOI 10.3389/fpsyt.2019.00348. [Google Scholar] [CrossRef]
27. FEI, Y. (2019). Effects of emotional resilience training on nurses’ perceived stress, positive and negative emotions and sleep quality. Revista Argentina De Clinica Psicologica, 28(2), 199–209. [Google Scholar]
28. Chang, L. Y., Wu, C. C., Yen, L. L., Chang, H. Y. (2019). The effects of family dysfunction trajectories during childhood and early adolescence on sleep quality during late adolescence: Resilience as a mediator. Social Science & Medicine, 222, 162–170. DOI 10.1016/j.socscimed.2019.01.010. [Google Scholar] [CrossRef]
29. House, J., Landis, K., Umberson, D. (1988). Social relationships and health. Science, 241(4865), 540–545. DOI 10.1126/science.3399889. [Google Scholar] [CrossRef]
30. Crowley, S. K., O’Buckley, T. K., Schiller, C. E., Stuebe, A., Morrow, A. L. et al. (2016). Blunted neuroactive steroid and HPA axis responses to stress are associated with reduced sleep quality and negative affect in pregnancy: A pilot study. Psychopharmacology, 233(7), 1299–1310. DOI 10.1007/s00213-016-4217-x. [Google Scholar] [CrossRef]
31. Reynolds, D. L., Garay, J. R., Deamond, S. L., Moran, M. K., Gold, W. et al. (2008). Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiology and Infection, 136(7), 997–1007. DOI 10.1017/S0950268807009156. [Google Scholar] [CrossRef]
32. Smeds, M. R., Janko, M. R., Allen, S., Amankwah, K., Arnell, T. et al. (2020). Burnout and its relationship with perceived stress, self-efficacy, depression, social support, and programmatic factors in general surgery residents. American Journal of Surgery, 219(6), 907–912. DOI 10.1016/j.amjsurg.2019.07.004. [Google Scholar] [CrossRef]
33. Lovell, B., Wetherell, M. A. (2019). Affiliate stigma, perceived social support and perceived stress in caregivers of children with autism spectrum disorder: A multiple mediation study. Archives of Psychiatric Nursing, 33(5), 31–35. DOI 10.1016/j.apnu.2019.08.012. [Google Scholar] [CrossRef]
34. Catabay, C. J., Stockman, J. K., Campbell, J. C., Tsuyuki, K. (2019). Perceived stress and mental health: The mediating roles of social support and resilience among black women exposed to sexual violence. Journal of Affective Disorders, 259, 143–149. DOI 10.1016/j.jad.2019.08.037. [Google Scholar] [CrossRef]
35. Yeung, N. C. Y., Lu, Q. (2018). Perceived stress as a mediator between social support and posttraumatic growth among Chinese American breast cancer survivors. Cancer Nursing, 41(1), 53–61. DOI 10.1097/NCC.0000000000000422. [Google Scholar] [CrossRef]
36. Huang, J., Wang, X., Li, W., An, Y. (2019). The relationship between conscientiousness and posttraumatic stress disorder among young Chinese firefighters: The mediating effect of perceived social support. Psychiatry Research, 273, 450–455. DOI 10.1016/j.psychres.2019.01.053. [Google Scholar] [CrossRef]
37. Goussé, V., Czernecki, V., Denis, P., Stilgenbauer, J. L., Deniau, E. et al. (2016). Impact of perceived stress, anxiety-depression and social support on coping strategies of parents having a child with Gilles de la Tourette syndrome. Archives of Psychiatric Nursing, 30(1), 109–113. DOI 10.1016/j.apnu.2015.08.017. [Google Scholar] [CrossRef]
38. Howard, S., Creaven, A. M., Hughes, B. M., O’Leary, É. D., James, J. E. (2017). Perceived social support predicts lower cardiovascular reactivity to stress in older adults. Biological Psychology, 125, 70–75. DOI 10.1016/j.biopsycho.2017.02.006. [Google Scholar] [CrossRef]
39. Moore, R. C., Eyler, L. T., Mausbach, B. T., Zlatar, Z. Z., Thompson, W. K. et al. (2015). Complex interplay between health and successful aging: Role of perceived stress, resilience, and social support. American Journal of Geriatric Psychiatry, 23(6), 622–632. DOI 10.1016/j.jagp.2014.08.004. [Google Scholar] [CrossRef]
40. Zhao, X., Lan, M., Li H., Yang, J. (2020). Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: A moderated mediation model. Sleep Medicine, 10.1016/j.sleep.2020.05.021. [Google Scholar] [CrossRef]
41. Zaidel, C., Musich, S., Karl, J., Kraemer, S., Yeh, C. S. (2020). Psychosocial factors associated with sleep quality and duration among older adults with chronic pain. Population Health Management, 3(1), S526. DOI 10.1089/pop.2019.0165. [Google Scholar] [CrossRef]
42. Silva, K. K. M. D., Martino, M. M. F. D., Bezerra, C. M. B., Souza, Â. M. L. D., Silva, D. M. D. et al. (2020). Stress and quality of sleep in undergraduate nursing students. Revista Brasileira de Enfermagem, 73(Suppl 1), 155. DOI 10.1590/0034-7167-2018-0227. [Google Scholar] [CrossRef]
43. Najem, J., Saber, M., Aoun, C., El Osta, N., Papazian, T. et al. (2020). Prevalence of food addiction and association with stress, sleep quality and chronotype: A cross-sectional survey among university students. Clinical Nutrition, 39(2), 533–539. DOI 10.1016/j.clnu.2019.02.038. [Google Scholar] [CrossRef]
44. Deng, X., Liu, X., Fang, R. (2020). Evaluation of the correlation between job stress and sleep quality in community nurses. Medicine, 99(4), e18822. DOI 10.1097/MD.0000000000018822. [Google Scholar] [CrossRef]
45. Li, X., Gao, X., Liu, J. (2019). Cross-sectional survey on the relationship between occupational stress, hormone levels, and the sleep quality of oilfield workers in Xinjiang, China. International Journal of Environmental Research and Public Health, 16(18), 3316. DOI 10.3390/ijerph16183316. [Google Scholar] [CrossRef]
46. Gao, M., Hu, J., Yang, L., Ding, N., Wei, X. et al. (2019). Association of sleep quality during pregnancy with stress and depression: A prospective birth cohort study in China. BMC Pregnancy and Childbirth, 19(1), 86. DOI 10.1186/s12884-019-2583-1. [Google Scholar] [CrossRef]
47. Bavafa, A., Khazaie, H., Khaledi-Paveh, B., Rezaie, L. (2019). The relationship of severity of symptoms of depression, anxiety, and stress with sleep quality in earthquake survivors in Kermanshah. Journal of Injury and Violence Research, 11(2), 225–232. [Google Scholar]
48. Hrozanova, M., Moen, F., Pallesen, S. (2019). Unique predictors of sleep quality in junior athletes: The protective function of mental resilience, and the detrimental impact of sex, worry and perceived stress. Frontiers in Psychology, 10, 674. DOI 10.3389/fpsyg.2019.01256. [Google Scholar] [CrossRef]
49. Abshire, M., Russell, S. D., Davidson, P. M., Budhathoki, C., Han, H. R. et al. (2018). Social support moderates the relationship between perceived stress and quality of life in patients with a left ventricular assist device. Journal of Cardiovascular Nursing, 33(5), E1–E9. DOI 10.1097/JCN.0000000000000487. [Google Scholar] [CrossRef]
50. Zhang, H., Zhang, Q., Gao, T., Kong, Y., Qin, Z. et al. (2019). Relations between stress and quality of life among women in late pregnancy: The parallel mediating role of depressive symptoms and sleep quality. Psychiatry Investigation, 16(5), 363–369. DOI 10.30773/pi.2019.02.14. [Google Scholar] [CrossRef]
51. Yook, Y. S., Sanada, K. (2019). Firefighters’ occupational stress and its correlations with cardiorespiratory fitness, arterial stiffness, heart rate variability, and sleep quality. PLoS One, 14(12), e0226739. DOI 10.1371/journal.pone.0226739. [Google Scholar] [CrossRef]
52. Linares, J. J. G., Pérez-Fuentes, M., Jurado, M. M. M., Ruiz, N. F. O., Márquez, M. M. S. et al. (2019). Sleep quality and the mediating role of stress management on eating by nursing personnel. Nutrients, 11(8), 1731. DOI 10.3390/nu11081731. [Google Scholar] [CrossRef]
53. Chen, T. L., Chang, S. C., Hsieh, H. F., Huang, C. Y., Chuang, J. H. et al. (2020). Effects of mindfulness-based stress reduction on sleep quality and mental health for insomnia patients: A meta-analysis. Journal of Psychosomatic Research, 135, 110144. DOI 10.1016/j.jpsychores.2020.110144. [Google Scholar] [CrossRef]
54. Liu, H., Gao, X., Hou, Y. (2019). Effects of mindfulness-based stress reduction combined with music therapy on pain, anxiety, and sleep quality in patients with osteosarcoma. Brazilian Journal of Psychiatry, 41(6), 540–545. DOI 10.1590/1516-4446-2018-0346. [Google Scholar] [CrossRef]
55. Lehrer, H. M., Steinhardt, M. A., Dubois, S. K., Laudenslager, M. L. (2020). Perceived stress, psychological resilience, hair cortisol concentration, and metabolic syndrome severity: A moderated mediation model. Psychoneuroendocrinology, 113, 104510. DOI 10.1016/j.psyneuen.2019.104510. [Google Scholar] [CrossRef]
56. Canale, N., Marino, C., Griffiths, M. D., Scacchi, L., Monaci, M. G. et al. (2019). The association between problematic online gaming and perceived stress: The moderating effect of psychological resilience. Journal of Behavioral Addictions, 8(1), 174–180. DOI 10.1556/2006.8.2019.01. [Google Scholar] [CrossRef]
57. Thurston, I. B., Hardin, R., Kamody, R. C., Herbozo, S., Kaufman, C. (2018). The moderating role of resilience on the relationship between perceived stress and binge eating symptoms among young adult women. Eating Behaviors, 29, 114–119. DOI 10.1016/j.eatbeh.2018.03.009. [Google Scholar] [CrossRef]
58. Kim, J. I., Park, H., Kim, J. H. (2018). The mediation effect of PTSD, perceived job stress and resilience on the relationship between trauma exposure and the development of depression and alcohol use problems in Korean firefighters: A cross-sectional study. Journal of Affective Disorders, 229, 450–455. DOI 10.1016/j.jad.2017.12.055. [Google Scholar] [CrossRef]
59. Hong, F., Tarullo, A. R., Mercurio, A. E., Liu, S., Cai, Q. et al. (2018). Childhood maltreatment and perceived stress in young adults: The role of emotion regulation strategies, self-efficacy, and resilience. Child Abuse & Neglect, 86, 136–146. DOI 10.1016/j.chiabu.2018.09.014. [Google Scholar] [CrossRef]
60. Thompson, G., Wrath, A., Trinder, K., Adams, G. C. (2018). The roles of attachment and resilience in perceived stress in medical students. Canadian Medical Education Journal, 9(4), e69–e77. DOI 10.36834/cmej.43204. [Google Scholar] [CrossRef]
61. Sarrionandia, A., Ramos-Díaz, E., Fernández-Lasarte, O. (2018). Resilience as a mediator of emotional intelligence and perceived stress: A cross-country study. Frontiers in Psychology, 9, 629. DOI 10.3389/fpsyg.2018.02653. [Google Scholar] [CrossRef]
62. Chen, Y. L., Kuo, P. H. (2020). Effects of perceived stress and resilience on suicidal behaviors in early adolescents. European Child & Adolescent Psychiatry, 29(6), 861–870. DOI 10.1007/s00787-019-01401-w. [Google Scholar] [CrossRef]
63. García-León, M. D. Á., Pérez-Mármol, J. M., Gonzalez-Pérez, R., García-Ríos, M. D. C., Peralta-Ramírez, M. D. I. (2019). Relationship between resilience and stress: Perceived stress, stressful life events, HPA axis response during a stressful task and hair cortisol. Physiology & Behavior, 202, 87–93. DOI 10.1016/j.physbeh.2019.02.001. [Google Scholar] [CrossRef]
64. Cai, W., Pan, Y., Zhang, S., Wei, C., Dong, W. et al. (2017). Relationship between cognitive emotion regulation, social support, resilience and acute stress responses in Chinese soldiers: Exploring multiple mediation model. Psychiatry Research, 256, 71–78. DOI 10.1016/j.psychres.2017.06.018. [Google Scholar] [CrossRef]
65. Ozbay, F., Johnson, D. C., Dimoulas, E., Morgan, C. A., Charney, D. et al. (2007). Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry (Edgmont), 4(5), 35–40. [Google Scholar]
66. Chrousos, G. P. (2009). Stress and disorders of the stress system. Nature Reviews Endocrinology, 5(7), 374–381. DOI 10.1038/nrendo.2009.106. [Google Scholar] [CrossRef]
67. Pulido-Martos, M., Fernández-Sánchez, M. D., Lopez-Zafra, E. (2020). Measurement invariance across gender and age in the Connor–Davidson Resilience Scale (CD-RISC) in a Spanish general population. Quality of Life Research, 29(5), 1373–1384. DOI 10.1007/s11136-019-02389-1. [Google Scholar] [CrossRef]
68. Meng, M., He, J., Guan, Y., Zhao, H., Yi, J. et al. (2019). Factorial invariance of the 10-item connor-davidson resilience scale across gender among Chinese elders. Frontiers in Psychology, 10, 43. DOI 10.3389/fpsyg.2019.01237. [Google Scholar] [CrossRef]
69. Madrid-Valero, J. J., Martínez-Selva, J. M., Ribeiro do Couto, B., Sánchez-Romera, J. F., Ordoñana, J. R. (2017). Age and gender effects on the prevalence of poor sleep quality in the adult population. Gaceta Sanitaria, 31(1), 18–22. DOI 10.1016/j.gaceta.2016.05.013. [Google Scholar] [CrossRef]
70. Zhang, M., Zhang, J., Zhang, F., Zhang, L., Feng, D. (2018). Prevalence of psychological distress and the effects of resilience and perceived social support among Chinese college students: Does gender make a difference? Psychiatry Research, 267, 409–413. DOI 10.1016/j.psychres.2018.06.038. [Google Scholar] [CrossRef]
71. Wu, Z. H., Stevens, R. G., Tennen, H., North, C. S., Grady, J. J. et al. (2015). Sleep quality among low-income young women in Southeast Texas predicts changes in perceived stress through hurricane Ike. Sleep, 38(7), 1121–1128. DOI 10.5665/sleep.4826. [Google Scholar] [CrossRef]
72. Su, T., Lien, T., Yang, C., Su, Y., Wang, J. et al. (2007). Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. Journal of Psychiatric Research, 41(1–2), 119–130. DOI 10.1016/j.jpsychires.2005.12.006. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |