
Mental Health Promotion
 | International Journal of Mental Health Promotion |  |
DOI: 10.32604/IJMHP.2021.015033
ARTICLE
Acceptability and Feasibility of YouthCHAT to Detect Psychosocial Problems in Young People with Congenital Heart Disease
1Department of Psychological Medicine, Faculty of Medical and Health Sciences, University of Auckland, Auckland, 1023, New Zealand
2Adult Congenital Heart Disease Service, Paediatric and Congenital Cardiology, Starship Hospital, Auckland, 1023, New Zealand
3Department of General Practice and Primary Health Care, University of Auckland, Auckland, 1023, New Zealand
*Corresponding Author: Hiran Thabrew. Email: h.thabrew@auckland.ac.nz
Received: 19 November 2020; Accepted: 09 March 2021
Abstract: Objective: Young people with congenital heart disease (CHD) are at increased risk of psychosocial issues, including anxiety and depression that can affect their medical care and quality of life. This open trial investigated the acceptability, feasibility and preliminary effectiveness of YouthCHAT, a tablet-based screener, designed to identify similar issues to a face to face psychosocial assessment, with young people who have CHD. Methods: YouthCHAT was administered to 44 such young people aged 15–25 years attending a specialist outpatient clinic at a New Zealand tertiary hospital. Key outcomes were (i) acceptability and (ii) feasibility of YouthCHAT, assessed via feedback from young people and clinicians and (iii) detection rates for each domain of YouthCHAT, measured by mental health or lifestyle issue being ‘present’ or ‘absent’. Results: YouthCHAT was quick to complete (mean 9 min and 7 s) and well-received by young people (overall rating 7 out of 10) and clinicians. Rates of anxiety, substance use and other issues were similar to those in a previous study of young people with mixed long-term physical conditions. However, rates of depression (41%) and life stresses (98%) were notably higher. Conclusions: Although further research is required, our results provide initial evidence that YouthCHAT is a viable and acceptable psychosocial screener with which to improve the holistic care of young people with CHD.
Keywords: Screening; adolescent; anxiety; depression; congenital heart disease
Advances in the medical and surgical care of individuals with congenital heart disease (CHD) have resulted in improved long-term survival, with over 90% of children born with CHD expected to reach adulthood [1]. Yet, these individuals still face uncertainty in their future as well as unique challenges across physical, medical, social and emotional domains [2]. Illness and treatment-related stresses, readjustment to usual life following hospital treatment and family pressures can lead to increased risk of psychosocial problems for young people, particularly anxiety and depression [3–7]. These issues can in turn impact medical treatment adherence, psychological safety (including self-harm and suicide) and longer-term social functioning and economic productivity [8,9].
Routine psychological assessment of young people with CHD has been encouraged to facilitate early intervention [10,11]. However, due to the wide range of issues that need to be monitored, individual psychometric instruments for identifying anxiety (e.g., the Generalized Anxiety Disorder—7 item scale (GAD-7) [12], depression (e.g., the Patient Health Questionnaire—9 items (PHQ-9) [13], family functioning (e.g., the Psychosocial Assessment Tool (PAT) [14] and other clinical issues are individually insufficient and cumbersome to administer in bulk [15]. Additionally, limited clinician confidence, time and financial constraints also contribute to psychosocial problems being sub-optimally addressed in this group of young people [3]. The most common way in which psychosocial screening of young people is currently conducted within pediatric settings is using a face-to-face interview called the HEEADSSS (Home, Education, Eating, Activities, Drugs and Alcohol, Sexuality, Suicide and Depression, Safety) assessment [16]. As the mnemonic suggests, this assessment includes questions about corresponding areas of a young person’s life and can take anywhere from 10 to 60 min to complete depending on the number of identified issues.
Recently, a composite electronic psychosocial screener called YouthCHAT has been developed by our team in New Zealand and shown to be acceptable to young people and to be quicker to complete than face-to-face HEEADSSS assessment in a high school setting [17], preferable for disclosing sensitive issues and feasible to use in a general pediatric clinic [18]. This study was undertaken to evaluate the potential for YouthCHAT to support routine and opportunistic screening of young people with CHD when attending medical appointments at a congenital cardiology outpatient clinic. Primary aims of the study were to evaluate the (i) acceptability of YouthCHAT to young people with CHD and (ii) feasibility of using YouthCHAT in a CHD outpatient clinic setting. A secondary aim was to identify detection rates for each domain of YouthCHAT, measured by mental health or lifestyle issue being ‘present’ or ‘absent’.
This study employed a pragmatic and primarily quantitative design.
Between July 2018 and March 2019, young people aged 15–25 years with CHD attending a specialist outpatient clinic at Starship Hospital (a tertiary hospital in Auckland, New Zealand), who could speak English, use an iPad and provide informed consent (or assent with paired parental consent if under 16 years of age) were invited to participate in the study via flyers disseminated by clinic staff, hence this was a purposive sample. Invited youth participants were approached in clinic by a research assistant before their medical appointments with participant information and consent sheets and a verbal explanation of the study. Clinical staff who reviewed the YouthCHAT results with their young patients were also invited to participate in the study. Those who consented completed an online survey following their consultation with the young person.
Enrolled participants completed YouthCHAT screening on an iPad individually in a consulting room prior to their medical appointments. After the consultation with their cardiac health provider they completed a paper survey to report on YouthCHAT acceptability and utility. YouthCHAT scoring and timing data were collected electronically and securely stored on a central database. Clinicians received YouthCHAT results on their clinic computer at the point of care and discussed them with participants during their medical appointment. Feedback on clinicians’ experience was collected via an electronic survey using SurveyMonkey®.
The intervention is YouthCHAT, the youth version of the electronic Case-Finding and Help Assessment Tool, a self-reported, tablet-based screener. It consists of up to 72 questions, the exact number answered depending on positive responses to gate-keeper questions in each of 13 domains: smoking, drinking, recreational drug use, problematic gambling, depression, anxiety, sexual health, eating and conduct issues, stress, exposure to abuse, anger management and physical activity [19]. Broadly matched to the areas of HEEADSSS (Home, Education, Eating, Activities, Drugs and Alcohol, Suicide and Depression, Sexuality and Safety) assessment [17].
YouthCHAT includes three well-known and validated screens: for substance abuse (Substances and Choices Scale, SACS), depression (Patient Health Questionnaire—Adolescent Version, PHQ-A) and anxiety (Generalized Anxiety Disorder scale—7 item, GAD-7) with which severity of these issues can be identified. These are validated screening tools. The scores are calculated electronically and provided to the clinician in the summary report including a severity rating for each score range (for example, a PHQ-A score of 15–19 indicates moderately severe depression).
Response options for answers to each question are in the form of yes/no, or Likert scales relevant to the domain (such as ‘not at all’, ‘for several days’, ‘more than half the days’ or ‘nearly every day’ in the past two weeks). For each identified positive domain, a ‘help’ question enables users to communicate whether they would prefer assistance at the time, later or not at all. Previous studies have shown that YouthCHAT is twice as fast as HEEADSSS assessment (mean 8 min 57 s vs. 17 min 22 s; mean difference 8 min 25 s) and that it detects more issues overall on comparable domains [17].
Primary outcomes’ measures were self-reported acceptability and feasibility of YouthCHAT use within an outpatient setting, assessed via feedback from young people and clinicians and the time taken to complete YouthCHAT screening. Young people were asked for overall ratings of the screener and its helpfulness with discussing psychosocial issues with clinicians, specific concerns about included questions, and items regarding YouthCHAT with checkboxes to tick if they agreed with the statements. Clinicians were asked about their usual methods of psychosocial screening, their overall impressions of YouthCHAT and for more detailed open-ended feedback regarding what they liked and did not like about it. Secondary outcome measures were detection rates for each module of YouthCHAT, i.e., mental health or lifestyle issues being ‘present’ or ‘absent’.
All 44 screens were included in data analysis and there were no missing data. Quantitative data were collected through the YouthCHAT database and were processed using Microsoft Excel. Analyses included basic descriptive statistics (e.g., number of youths screened, YouthCHAT summary data and demographic characteristics of the sample). Qualitative data were analyzed using a general inductive approach [20]. Data were independently evaluated, then cross-coded by two researchers (HT and HK) to identify key themes and subthemes, with any disagreements being resolved by consensus.
The study protocol was registered with the Australian and New Zealand Clinical Trials Network Registry ANZCTR in July 2017 (ACTRN12616001243404p.) and received approval as an extension of the previous hospital-based study [18] from the New Zealand Health and Disability Ethics Committee (Reference: 16/CEN/137).
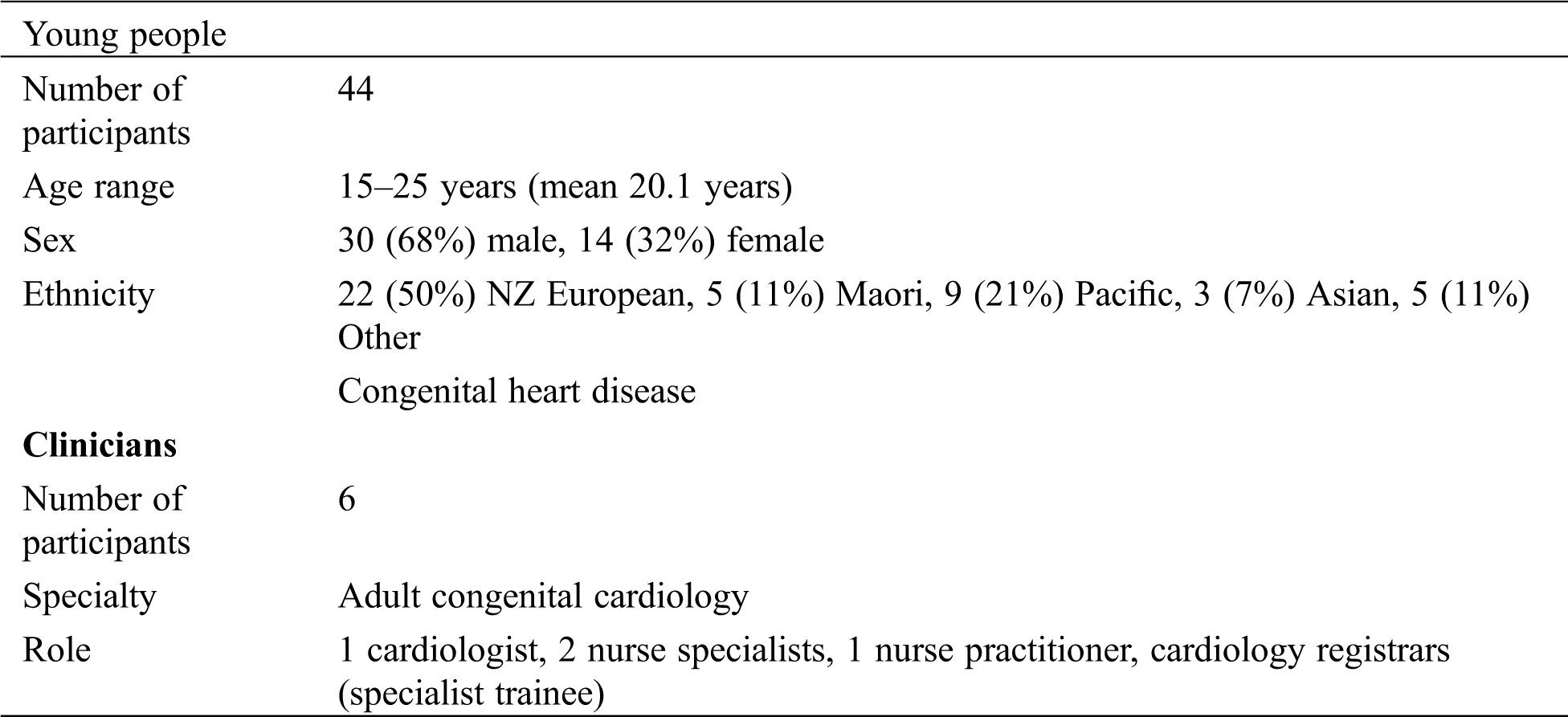
3.1 Participant Characteristics
A total of 58 young people with CHD were invited to participate. Of these, 44 provided consent and all (100%) completed YouthCHAT screening and 26 (59%) completed follow-up questionnaires during their congenital cardiology outpatient visit. Although information regarding the age, sex and ethnicity of these young people was collected, their education level, employment experience and health literacy status was not obtained. Out of the non-participants, thirteen said they either were not interested in the study (without giving any specific reason) and one said that they did not have time. Six clinicians participated in the study and four (67%) completed the online feedback survey. Of those surveyed, one was a cardiologist, two were nurse specialists and one was a nurse practitioner. The two clinicians who did not complete surveys were registrars (specialist trainees) who had completed their clinical rotation before survey invitations were dispatched. Information regarding the role and specialty of clinicians was collected, however information regarding their sex and number of years of experience of clinicians was not obtained. Further details of participant characteristics are provided in Tab. 1.
Table 1: Participant characteristics
3.2 Time Taken to Complete YouthCHAT
Young people completed YouthCHAT in an average of 9 min and 7 s (range 4 min and 44 s to 44 min and 49 s), and a median of 7 min and 29 s (IQR = 6 min and 40 s–9 min and 36 s).
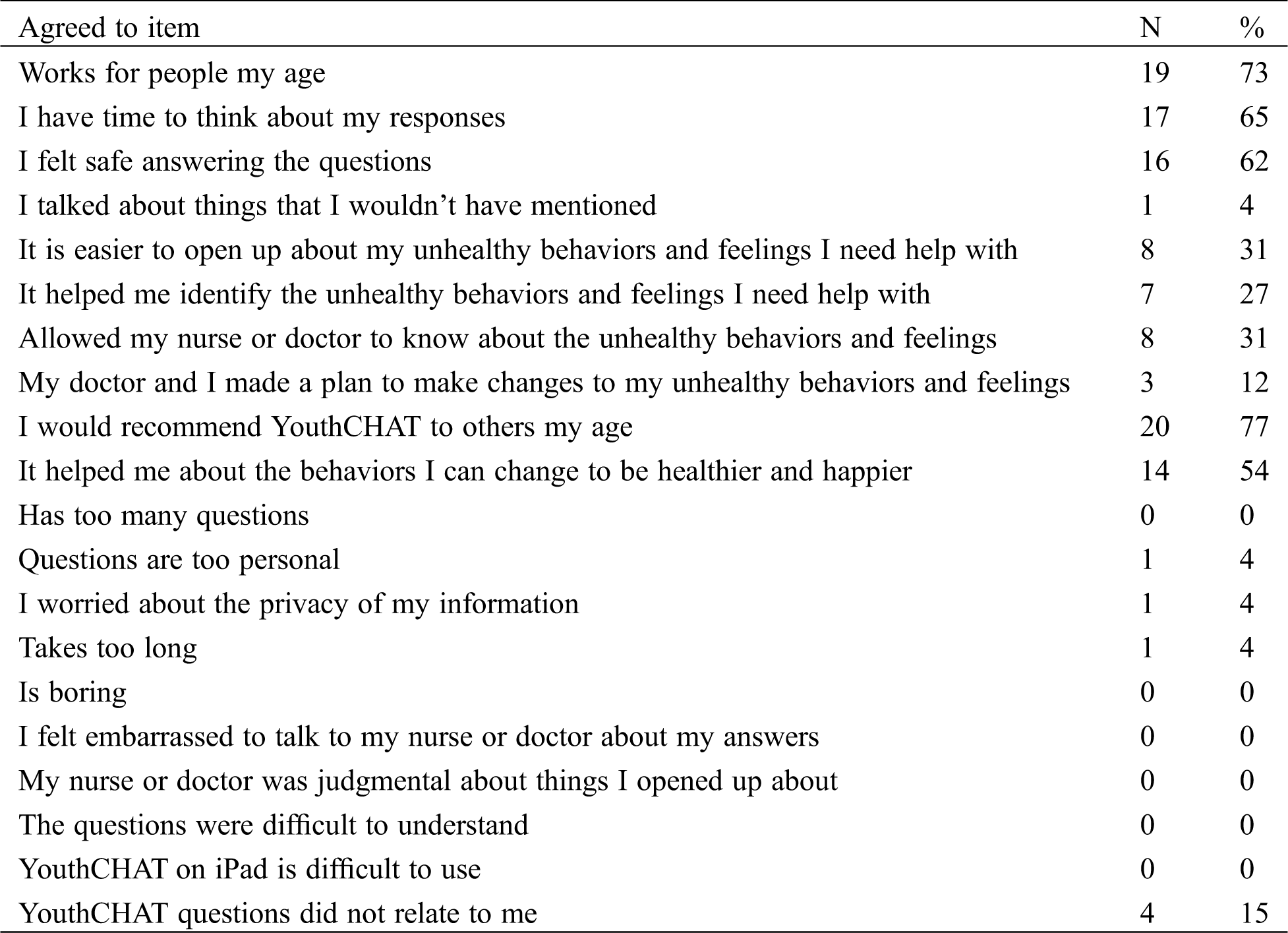
3.3 Feedback from Young People with Congenital Heart Disease
Young people gave YouthCHAT a rating of 7.0 (range 3–10) on a 10-point scale from ‘lame’ (0) to ‘awesome’ (10) and said that it had been helpful for discussing psychosocial issues with their clinician at a rating of 4.4 (range 1–10) on a 10 point scale from ‘helpful’ (10) to ‘not helpful at all’ (0). Most (N = 25, 96%) young people denied disliking any YouthCHAT questions. One person (4%) out of the young people said they did not like answering questions on worrying and exercise. Optional statements regarding YouthCHAT were acknowledged in a dichotomous manner (agree/disagree) at the rates shown in Tab. 2.
Table 2: Acceptability of YouthCHAT to young people
As shown in Tab. 3, the most common issues identified by young people were concerns about life stresses (N = 42; 98%), eating and weight (N = 38; 86%), sexual activity/identity (N = 31; 72%), drinking (N = 27; 61%), depression (N = 18; 41%) and physical inactivity (N = 16; 38%). Positive screens for eating problems were primarily related to dissatisfaction with body shape or weight and serious eating disordered behaviour.
Table 3: Rates of issues among young people identified by YouthCHAT
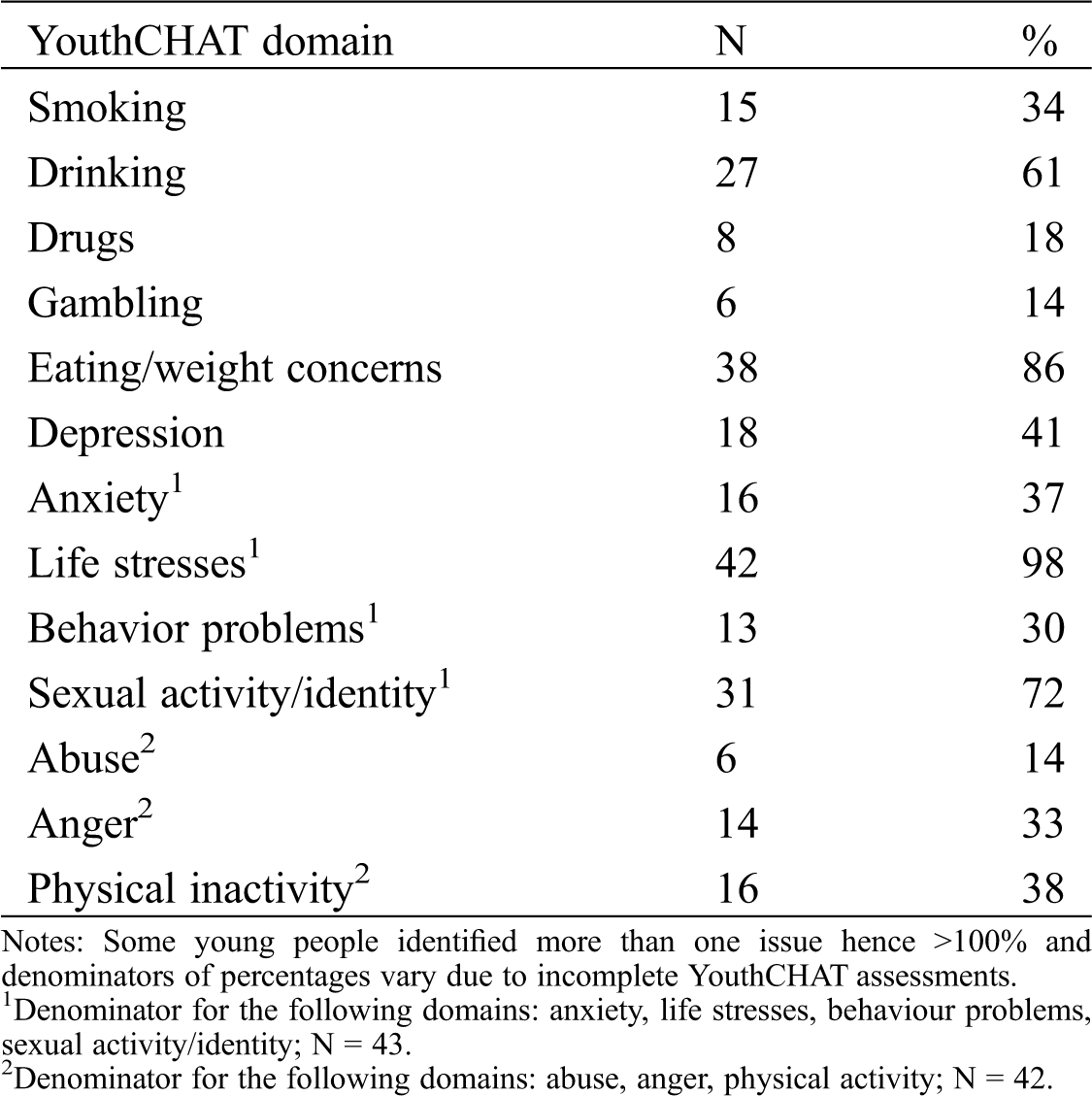
Types of stress experienced by individuals were related to issues at home, school or work, issues with relationships with specific people in their life, being bullied, violence, an upsetting event and money. Eighteen individuals were identified as having symptoms of depression via the PHQ-A. Of these, 12 were rated subthreshold, one was rated mild, one was rated moderate, three were rated moderate-severe and one was rated severe in intensity. Sixteen individuals were identified as having anxiety via the GAD-7. Of these, three were rated subthreshold, 12 were rated mild and one was rated moderate in intensity. Twenty-nine individuals were identified as having substance use problems via the SACS. Of these, 17 were rated subthreshold and 12 were rated as having a low level of problems that required further assessment. Despite YouthCHAT identifying a range of psychosocial issues, only four (9%) young people said that they wanted help that day, 11 (25%) said that they wanted help later and the remainder (66%) said they did not want help at all. The latter category included two young people with moderately severe to severe symptoms of depression who reported suicidal ideation and were flagged as being of immediate concern. They were provided with face to face follow-up by the in-hospital pediatric consult liaison.
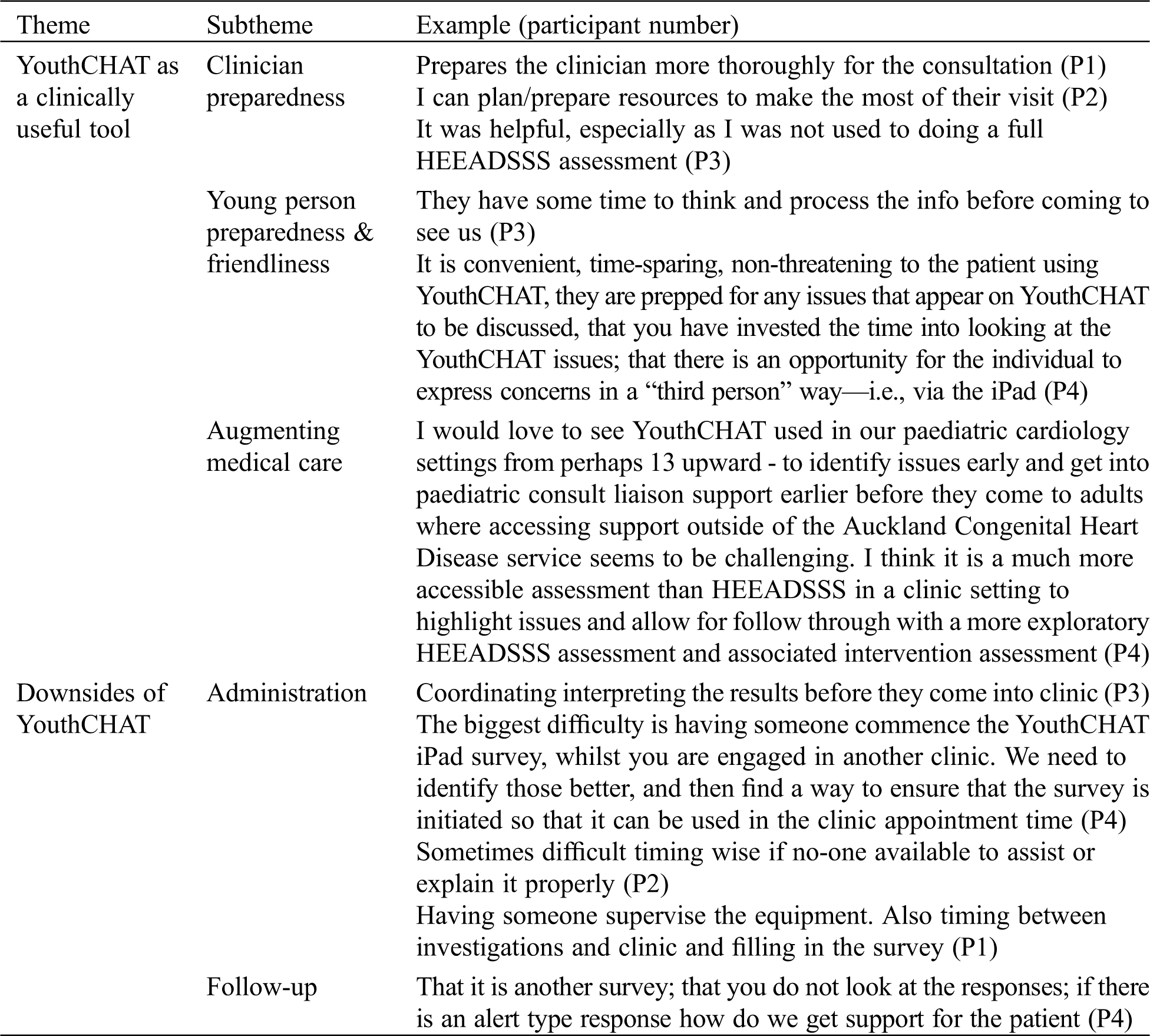
Clinicians reported they rarely (N = 2; 50%) or sometimes (N = 2; 50%) conducted intermittent HEEADSSS assessments in an outpatient clinic setting depending to perceived need. Feedback regarding YouthCHAT was generally positive, with all clinicians rating the discussion of psychosocial issues raised by YouthCHAT as ‘very acceptable’ and denying that young people overtly objected to any of the questions. Three clinicians rated YouthCHAT as a ‘very useful’ screener, ‘very useful’ for identifying whether young people were ready to make changes in their behavior and ‘very useful’ for initiating conversation with young people about psychosocial issues. One clinician rated YouthCHAT as ‘neither useful nor un-useful’ for identifying psychosocial issues, ‘neither useful for un-useful’ for identifying whether young people were ready to make changes in their behavior and ‘useful’ for initiating conversation with young people about these issues. Three clinicians said that they would be ‘very likely’ and one clinician said they would be ‘likely’ to use YouthCHAT regularly if it was available in their clinic. Key themes, subthemes and examples of clinician feedback are presented in Tab. 4.
Table 4: Feedback from clinicians
YouthCHAT appears to be an acceptable and efficient means of undertaking electronic psychosocial screening of young people within an adult congenital cardiac clinic setting. It is also acceptable to clinicians, helping them prepare for consultations and address information regarding their patients’ psychosocial wellbeing, without any apparent delay in seeing patients. The time taken for its use in this study was comparable with a previous hospital-based study [18] and high school-based study [17], suggesting that YouthCHAT can be used to efficiently undertake psychosocial screening in multiple settings.
Previous research with a younger group (mean age 14.9 years) has demonstrated the acceptability and effectiveness of YouthCHAT for individuals with mixed long-term physical conditions (LTPC) [18]. Although the somewhat older group in this study (mean age 20.1 years) reported similar overall ratings for YouthCHAT, they reported slightly lower rating of 4.4 vs. 5.2 out of 10 for helpfulness with discussing psychosocial issues with clinicians. This may reflect their greater confidence in directly addressing these issues (albeit only when asked). The limited proportion of young people with positive screens who elected to receive further assistance while using YouthCHAT is concordant with previous evidence that 75% of young people are reluctant to seek professional help for mental health problems [21]. However, it is also one of the key reasons why clinical follow-up is required when undertaking electronic screening. Although young people have been found to prefer electronic screening as it makes them feel more in control, to have greater input into their care and to disclose sensitive information [22], they are more likely to accept help when they experience significant distress, positive attitudes toward counselling [23] or they have attachment anxiety [24]; and less likely to do so when they have greater levels of stigma [25], lower levels of emotional openness [26] and greater levels of suicidal ideation [27]. YouthCHAT is probably best considered a prelude to more in-depth, targeted screening by an empathic clinician who can collaboratively discern whether immediate or delayed follow-up is necessary and at a minimum, note any positive YouthCHAT findings in the young person’s clinical record.
Rates of self-identified issues in young people with CHD were broadly similar to those with mixed LTPC with a couple of notable differences. First, the young people with CHD who took part in this study reported higher levels of depression (41%) than those of a younger mean age with mixed long-term physical conditions (13%) [18] and those of a similar mean age in the general population (18%) [28]. Second, they identified significantly greater rates of life stresses (98%) compared with those with mixed LTPC (33%) [18] and those at high school (27%) [17]. Although based on small numbers, these findings suggest that young people with CHD may face an even greater psychosocial burden than those with other LTPC, let alone those without physical illness. Whether the higher rate of life stresses are related to the nature of experienced symptoms, endured clinic attendance and procedures or other factors is currently unclear. However, they suggest that regular psychosocial screening would be useful to facilitate earlier intervention and prevention of secondary issues, including self-harm and suicide.
Strengths of this study include it being, to our knowledge, one of the first studies to examine the use of electronic screening with young people who have CHD in a naturalistic setting; extension of previous research findings to demonstrate the acceptability of YouthCHAT with an older population that includes both adolescents and young adults; and the lack of missing data from young people. The main limitation of this study is its relatively small sample size. Despite this, our findings are likely to be representative of the truth, given the identification of similar rates of physical inactivity, anger, abuse and anxiety during previous YouthCHAT studies [17,18] and similar rates of substance abuse being identified during previous studies of this clinical population [6,29]. Additional limitations include the study not being powered to conduct subgroup analyses to better understand the needs of young people of different gender and ethnicity, optional statements regarding the use of YouthCHAT not being completed by all participants and not all clinicians completing feedback surveys.
Further research is required to confirm the findings of this study with a larger group of young people with CHD, including those of different gender and ethnicities (especially in a New Zealand context, Maori and Pacific Island young people who are known to have higher rates of most psychosocial issues) [28]. Additional examination of systemic factors is also required to pave the way for routine implementation of YouthCHAT within a hospital setting. Given that tertiary congenital cardiac services are currently only available in Auckland city, it is important to evaluate the feasibility of using YouthCHAT in less specialist settings to promote equity of access to psychosocial screening. Providing more intensive training to clinical staff on responding to psychosocial issues may increase the likelihood of young people feeling comfortable discussing sensitive information with clinicians. Exploration of the impact of screening on mental and physical healthcare and the development of mechanisms to make results directly available to young people will ensure that YouthCHAT augments holistic healthcare while supporting young people to be in charge of their health.
Acknowledgement: We thank Margot Darragh, Research Fellow for YouthCHAT, Jim Warren, Professor of Health Informatics, University of Auckland, Lois Ravuri and the Adult Congenital Heart Disease Team from Auckland Hospital for their contributions to this project.
Authors’ Contributions: The study was conceptualized by HT, VGH and FG. Data analysis was undertaken by HT and HK. The paper was written and reviewed by all authors.
Funding Statement: This work was supported by the Starship Foundation, New Zealand (Grant No. SF 1343).
Conflicts of Interest: Felicity Goodyear-Smith is the primary developer of Youth version, Case-finding and Help Assessment Tool. None of the other authors have any conflicts of interest to declare.
1. Moons, P., Bovijn, L., Budts, W., Belmans, A., Gewillig, M. (2010). Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation, 122(22), 2264–2272. DOI 10.1161/CIRCULATIONAHA.110.946343. [Google Scholar] [CrossRef]
2. Lui, G. K., Saidi, A., Bhatt, A. B., Burchill, L. J., Deen, J. F. et al. (2017). Diagnosis and management of noncardiac complications in adults with congenital heart disease: A scientific statement from the American Heart Association. Circulation, 136(20), e348–e392. DOI 10.1161/CIR.0000000000000535. [Google Scholar] [CrossRef]
3. Kovacs, A. H., Saidi, A. S., Kuhl, E. A., Sears, S. F., Silversides, C. et al. (2009). Depression and anxiety in adult congenital heart disease: Predictors and prevalence. International Journal of Cardiology, 137(2), 158–164. DOI 10.1016/j.ijcard.2008.06.042. [Google Scholar] [CrossRef]
4. Latal, B., Helfricht, S., Fischer, J. E., Bauersfeld, U., Landolt, M. A. (2009). Psychological adjustment and quality of life in children and adolescents following open-heart surgery for congenital heart disease: A systematic review. BioMed Central Pediatrics, 9(1), 6. DOI 10.1186/1471-244X-9-6. [Google Scholar] [CrossRef]
5. O’Donovan, C. E., Painter, L., Lowe, B., Robinson, H., Broadbent, E. (2016). The impact of illness perceptions and disease severity on quality of life in congenital heart disease. Cardiology in the Young, 26(1), 100–109. DOI 10.1017/S1047951114002728. [Google Scholar] [CrossRef]
6. Westhoff-Bleck, M., Briest, J., Fraccarollo, D., Hilfiker-Kleiner, D., Winter, L. et al. (2016). Mental disorders in adults with congenital heart disease: Unmet needs and impact on quality of life. Journal of Affective Disorders, 204, 180–186. DOI 10.1016/j.jad.2016.06.047. [Google Scholar] [CrossRef]
7. Berant, E., Mikulincer, M., Shaver, P. R. (2008). Mothers’ attachment style, their mental health, and their children’s emotional vulnerabilities: A 7-year study of children with congenital heart disease. Journal of Personality, 76(1), 31–66. DOI 10.1111/j.1467-6494.2007.00479.x. [Google Scholar] [CrossRef]
8. Ferro, M. A., Rhodes, A. E., Kimber, M. (2017). Suicidal behaviour among adolescents and young adults with self-reported chronic illness. Canadian Journal of Psychiatry, 62(12), 845–853. DOI 10.1177/0706743717727242. [Google Scholar] [CrossRef]
9. Smith, J. P., Smith, G. C. (2010). Long-term economic costs of psychological problems during childhood. Social Science & Medicine, 71(1), 110–115. DOI 10.1016/j.socscimed.2010.02.046. [Google Scholar] [CrossRef]
10. Foster, E., Graham, T. P., Driscoll, D. J., Reid, G. J., Reiss, J. G. et al. (2001). Task force 2: Special health care needs of adults with congenital heart disease. Journal of the American College of Cardiology, 37(5), 1176–1183. DOI 10.1016/S0735-1097(01)01277-3. [Google Scholar] [CrossRef]
11. Gurvitz, M., Burns, K. M., Brindis, R., Broberg, C. S., Daniels, C. J. et al. (2016). Emerging research directions in adult congenital heart disease: A report from an NHLBI/ACHA working group. Journal of the American College of Cardiology, 67(16), 1956–1964. DOI 10.1016/j.jacc.2016.01.062. [Google Scholar] [CrossRef]
12. Spitzer, R. L., Kroenke, K., Williams, J. B., Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. DOI 10.1001/archinte.166.10.1092. [Google Scholar] [CrossRef]
13. Kroenke, K., Spitzer, R. L. (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatry Annals, 32(9), 509–515. DOI 10.3928/0048-5713-20020901-06. [Google Scholar] [CrossRef]
14. Kazak, A. E., Prusak, A., McSherry, M. (2001). The Psychosocial Assessment Tool (PATPilot data on a brief screening instrument for identifying high risk families in pediatric oncology. Family, Systems and Health, 19(3), 303–317. DOI 10.1037/h0089454. [Google Scholar] [CrossRef]
15. Thabrew, H., McDowell, H., Given, K., Murrell, K. (2017). Systematic review of screening instruments for psychosocial problems in children and adolescents with long-term physical conditions. Global Pediatric Health, 4(5), 2333794X17690314. DOI 10.1177/2333794X17690314. [Google Scholar] [CrossRef]
16. Goldenring, J. M., Rosen, D. S. (2004). Getting into adolescent heads: An essential update. Contemporary Pediatrics, 21(1), 64–92. [Google Scholar]
17. Thabrew, H., Silva, S., Darragh, M., Goldfinch, M., Meads, J. et al. (2019). Comparison of YouthCHAT, an electronic composite psychosocial screener, with a clinician interview assessment for young people: Randomized trial. Journal of Medical Internet Research, 21(12), e13911. DOI 10.2196/13911. [Google Scholar] [CrossRef]
18. Thabrew, H., Goodyear, S. F. (2020). Youth version, case-finding and help assessment tool (YouthCHATAn electronic, psychosocial screener for young people with long-term physical conditions. Journal of Paediatrics and Child Health, 56(1), 102–106. DOI 10.1111/jpc.14503. [Google Scholar] [CrossRef]
19. Goodyear-Smith, F., Martel, R., Darragh, M., Warren, J., Thabrew, H. et al. (2017). Screening for risky behaviour and mental health in young people: The YouthCHAT programme. Public Health Reviews, 38(1), 20. DOI 10.1186/s40985-017-0068-1. [Google Scholar] [CrossRef]
20. Thomas, D. R. (2006). A general inductive approach for analyzing qualitative evaluation data. American Journal of Evaluation, 27(2), 237–246. DOI 10.1177/1098214005283748. [Google Scholar] [CrossRef]
21. Mariu, K. R., Merry, S. N., Robinson, E. M., Watson, P. D. (2012). Seeking professional help for mental health problems, among New Zealand secondary school students. Clinical Child Psychology and Psychiatry, 17(2), 284–297. DOI 10.1177/1359104511404176. [Google Scholar] [CrossRef]
22. Bradford, S., Rickwood, D. (2015). Young people’s views on electronic mental health assessment: Prefer to type than talk? Journal of Child and Family Studies, 24(5), 1213–1221. DOI 10.1007/s10826-014-9929-0. [Google Scholar] [CrossRef]
23. Cramer, K. M. (1999). Psychological antecedents to help-seeking behavior: A reanalysis using path modeling structures. Journal of Counseling Psychology, 46(3), 381–387. DOI 10.1037/0022-0167.46.3.381. [Google Scholar] [CrossRef]
24. Vogel, D. L., Wei, M. (2005). Adult attachment and help-seeking intent: The mediating roles of psychological distress and perceived social support. Journal of Counseling Psychology, 52(3), 347–357. DOI 10.1037/0022-0167.52.3.347. [Google Scholar] [CrossRef]
25. Clement, S., Schauman, O., Graham, T., Maggioni, F., Evans-Lacko, S. et al. (2015). What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine, 45(1), 11–27. DOI 10.1017/S0033291714000129. [Google Scholar] [CrossRef]
26. Komiya, N., Good, G. E., Sherrod, N. B. (2000). Emotional openness as a predictor of college students’ attitudes toward seeking psychological help. Journal of Counselling Psychology, 47(1), 138–143. DOI 10.1037/0022-0167.47.1.138. [Google Scholar] [CrossRef]
27. Carlton, P. A., Deane, F. P. (2000). Impact of attitudes and suicidal ideation on adolescents’ intentions to seek professional psychological help. Journal of Adolescence, 23(1), 35–45. DOI 10.1006/jado.1999.0299. [Google Scholar] [CrossRef]
28. Slade, T., Johnston, A., Oakley Browne, M. A., Andrews, G., Whiteford, H. (2007). National Survey of Mental Health and Wellbeing: Methods and key findings. Australian and New Zealand Journal of Psychiatry, 43(7), 594–605. DOI 10.1080/00048670902970882. [Google Scholar] [CrossRef]
29. BPAC (2010). Depression in young people. https://bpac.org.nz/BPJ/2010/January/docs/bpjse_young_depression.pdf. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |