
 | International Journal of Mental Health Promotion | 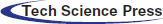 |
DOI: 10.32604/ijmhp.2022.017685
ARTICLE
Perceived Stress and Coping Styles among the General Population in Saudi Arabia during COVID-19 Pandemic
1Department of Medicine, Faculty of Medicine, King Abdulaziz University, Jeddah, 21589, Saudi Arabia
2Department of Medicine, Division of Psychiatry, Rabigh Faculty of Medicine, King Abdulaziz University, Jeddah, 25732, Saudi Arabia
3Department of Family Medicine, Faculty of Medicine, King Abdulaziz University, Jeddah, 21589, Saudi Arabia
*Corresponding Author: Saeed S. Shaaban. Email: saeedalfehri@gmail.com
Received: 30 May 2021; Accepted: 20 September 2021
Abstract: This article examines the stress levels, coping responses, and influence of adaptive and maladaptive coping styles on stress in Saudi Arabia during the COVID-19 pandemic. An online cross-sectional survey was distributed to the attendees of a pandemic-related awareness webinars. The questionnaire assessed demographic and clinical characteristics, coping strategies (the brief COPE inventory), and stress levels (the Perceived Stress Scale). A multivariate linear regression analysis was conducted to assess the predictors of stress. The highest adaptive and maladaptive coping styles were reported for religion and self-distraction. Certain groups were independently more vulnerable to experience stress, including young- and middle-aged adults, females, students, and those with a low-to-middle income, with a personal or familial history of mental conditions, and living with someone with COVID-19 in their close circle. Higher levels of stress were also predicted by lower levels of using positive coping styles, particularly positive reframing, planning, and returning to religion, and higher levels of negative coping styles, such as venting, self-blame, and denial. Future psychotherapeutic interventions through the media and digital solutions are warranted to mitigate and manage stress by targeting vulnerable groups, promoting active coping styles, and discouraging negative coping strategies.
Keywords: Anxiety; coronavirus; public health; pandemic; mental health; chronic illness
The novel coronavirus disease 2019 (COVID-19) was first reported in Wuhan, China, in December 2019 [1], and was classified by the World Health Organization (WHO) as a public health emergency of international concern on January 30, 2020 [2,3]. As the virus continues to spread worldwide, more than 200 countries have been affected, with confirmed cases reaching 61.8 million worldwide [4]. This surge of cases has led to public fear regarding the disease and increasing stress levels [5,6].
The Kingdom of Saudi Arabia experienced its first COVID-19 case on March 03, 2020 [7]. Since then, there have been 356,911 confirmed cases and 5,870 deaths as of November 29, 2020 [4]. Consequently, the Saudi government suspended international and national flights, banned gathering in public places, switched schools to remote teaching, and implemented a strict curfew. These drastic measures were implemented to minimize the spread of COVID-19, and they have profoundly affected lifestyles and social interactions.
As the pandemic continues to impact people’s lives, issues of mental health and wellbeing need special attention [8,9]. As seen among those affected by the severe acute respiratory syndrome (SARS) in 2003 [10,11], major negative life events can impact mental health. The COVID-19 pandemic has caused similar increases in stress and anxiety [12–14]. In Saudi Arabia, a recent publication reported that 40% of the sample population were stressed during the pandemic, with 7% exhibiting severe stress levels [15].
Limited studies have been done detailing the coping styles for dealing with the COVID-19 pandemic. Nonetheless, understanding the coping styles will help provide relevant clinical knowledge to manage these issues. In China, Wang and his colleagues demonstrated that individuals with negative coping styles had a higher psychological distress level [16].
In this study, we aimed to examine the coping strategies and determine the perceived stress levels related to the COVID-19 pandemic in a sample from Saudi Arabia. Additionally, we explored the sociodemographic and health variables within the population that may impact stress levels. We hypothesized that the perceived stress levels among the Saudi Arabia participants are moderate and that sociodemographic and health variables impacted these levels. Furthermore, we postulated that positive and negative coping mechanisms are significant predictors of changes in stress levels.
A cross-sectional study was carried out during May 2020. A three-part questionnaire was distributed to attendees of daily, open access pandemic-related public awareness webinars held for two weeks and organized by the center of health promotion at King Abdulaziz University. All participants provided written informed consent. This Institutional Review Board (IRB) of King Abdulaziz University Hospital approved this study (Reference No. 310–20).
2.2 Measurements and Instruments
The questionnaire comprised three parts: sociodemographic data, the brief COPE inventory, and the Perceived Stress Scale (PSS).
We collected general sociodemographic data such as gender, age, nationality, city of residence, monthly income, education, and marital status. Additionally, we sought other social and health variables that may have affected participants’ levels of stress and coping styles during the pandemic, including the presence of physical or mental health conditions, current use of psychotropic medications, being a caregiver of or living with an older person, being a caregiver of or living with someone who has a chronic illness, and having a family history of mental illness.
The Brief COPE is a 28-item self-administered inventory containing 14 subscales of two items that assess individuals’ stress coping in daily life. The subscales include eight adaptive coping styles: active coping, planning, positive reframing, acceptance, humor, religion, emotional support, and instrumental support. It also comprises six maladaptive coping styles: self-distraction, denial, venting, substance use, behavioral disengagement, and self-blame [17]. Participants were asked to rate each question on a 4-point Likert scale ranging from 1 (I do not do this at all) to 4 (I do this a lot). This scale was validated in Arabic, and the internal consistency of the 14 dimensions assessed using Cronbach’s alpha coefficient, which was between α = 0.63 and α = 0.94. Additionally, the expected divergent validity results had good construct validity [18].
2.2.3 Perceived Stress Scale (PSS)
The PSS is a 10-item self-administered questionnaire designed to determine how unpredictable, uncontrollable, and overloaded respondents find their lives. It contains four positively stated items and six negatively stated items. Participants were asked to rate each question on a 5-point Likert scale ranging from 0 (never) to 4 (very often). The scores were calculated by reversing the responses to the four positively stated items (items 4, 5, 7, and 8) and then summing the scores of all scale items. The total scores were from “0–13” indicating low stress, “14–26” indicating moderate stress, and “27–40” indicating high perceived stress. The reliability and validity of the Arabic version of the PSS were evaluated and had a Cronbach’s alpha coefficient of 0.80. The test-retest reliability had an intra-correlation coefficient of 0.90 [19].
SPSS version 26 (IBM, New York, USA) was used for the data analysis. Frequencies and percentages were used to describe categorical data, and continuous data were expressed as mean ± standard deviation (minimum and maximum). The Shapiro-Wilk test was used to evaluate normal data distribution; the data were not normally distributed (P < 0.0001 for all scores). Significance was determined using the Kruskal- Wallis H (KWH) test between more than two groups and the Mann-Whitney (MW) test between two groups. Composite adaptive and maladaptive coping scores were calculated by summing their relevant subscales. The effect of coping strategies on participants’ perceived stress was investigated using a multivariate linear regression analysis in UNIANOVA. The total PSS score was the dependent variable, and coping strategies were independent variables. The results were adjusted for the significant demographic and clinical factors obtained from the univariate analyses (KWH and MW tests). Statistical significance was considered at P < 0.05 (2-tailed).
3.1 Demographic and Clinical Characteristics
In total, 5,514 participants participated in this research. The largest group in each category were 18–25 years, Western region, female, Saudi, students, single, college (educational level), and < SAR 3000 (monthly income) (Table 1).
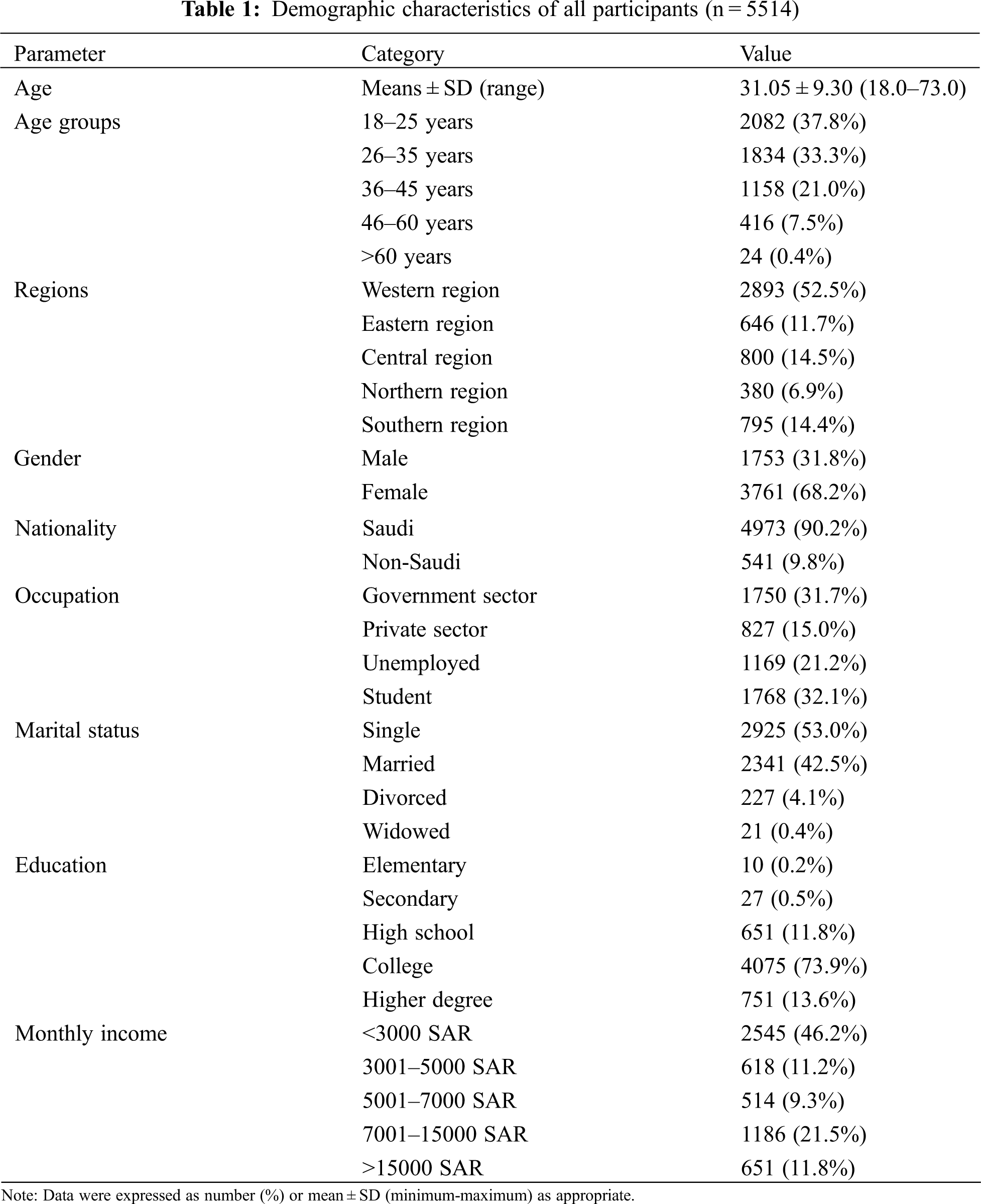
In this study, 9.6% of participants suffered from chronic medical conditions such as diabetes mellitus and hypertension; 4.7% were previously diagnosed with mental health conditions; 1.6% were currently taking psychiatric medications; 28.4% were currently living with someone experiencing chronic medical conditions; 13.1% had family members currently experiencing mental conditions; 21.4% were currently living with someone over the age of 60 years; and 33.8% were having a child or more currently under the age of 18 years. Of the participants, 21.0% had someone in their close circle diagnosed with COVID-19 (Fig. 1).
Figure 1: Clinical characteristics of all participants (n = 5514). Data are expressed as percentages
3.2 Outcomes of Coping Strategies and the Perceived Stress
The mean ± SD composite adaptive coping score was 41.95 ± 8.86 (range 16–64), while the mean maladaptive coping score was 20.85 ± 5.29 (range 12–48). A summary of the mean scores of the COPE scale is depicted in Fig. 2. Of the eight adaptive coping styles studied (Fig. 2A), the most frequently used strategies were religion (6.64), acceptance (6.46), positive reframing (5.82), active coping (5.81), planning (5.79), instrumental support (4.26), and emotional support (4.16); the least used was humor (3.01). Of the six maladaptive coping styles studied (Fig. 2B), the most frequently used strategies were self-distraction (4.88), venting (4.02), self-blame (3.41), denial (3.35), behavioral disengagement (3.15), and substance use (2.06). Regarding the total PSS score, the mean ± SD score among all participants was 17.21 ± 6.89. Most participants reported moderate stress (61.5%), followed by low stress (29.5%), while participants who reported high stress were only at 9.0% (Fig. 2C).
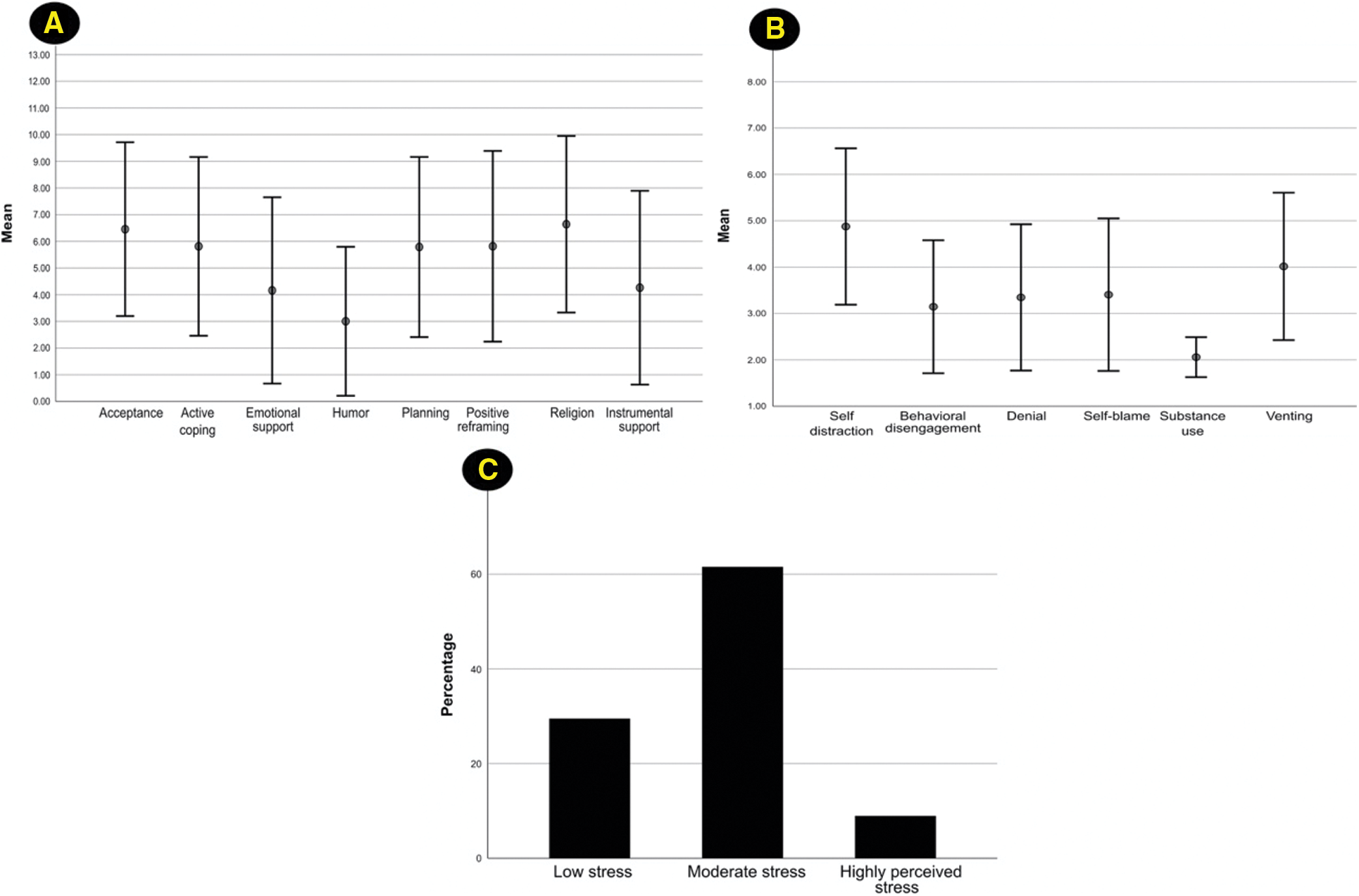
Figure 2: The results of coping and stress scores. The mean scores of the coping subscales are illustrated in Panel A (adaptive coping) and Panel B (maladaptive coping). Error bars represent the standard deviation. Panel (C) depicts the percentage of participants with different stress levels based on the Perceived Stress Scale score (n = 5514)
3.3 Demographic and Clinical Differences in the Perceived Stress Scale Score
There was a significant difference in perceived stress score among age groups, regions, gender, occupation, marital status, and monthly income. The perceived stress score was highest among participants aged 18–25 years: in the Eastern Region, female, students, single elementary education, and with a monthly income of <3000 SAR (Table 2).
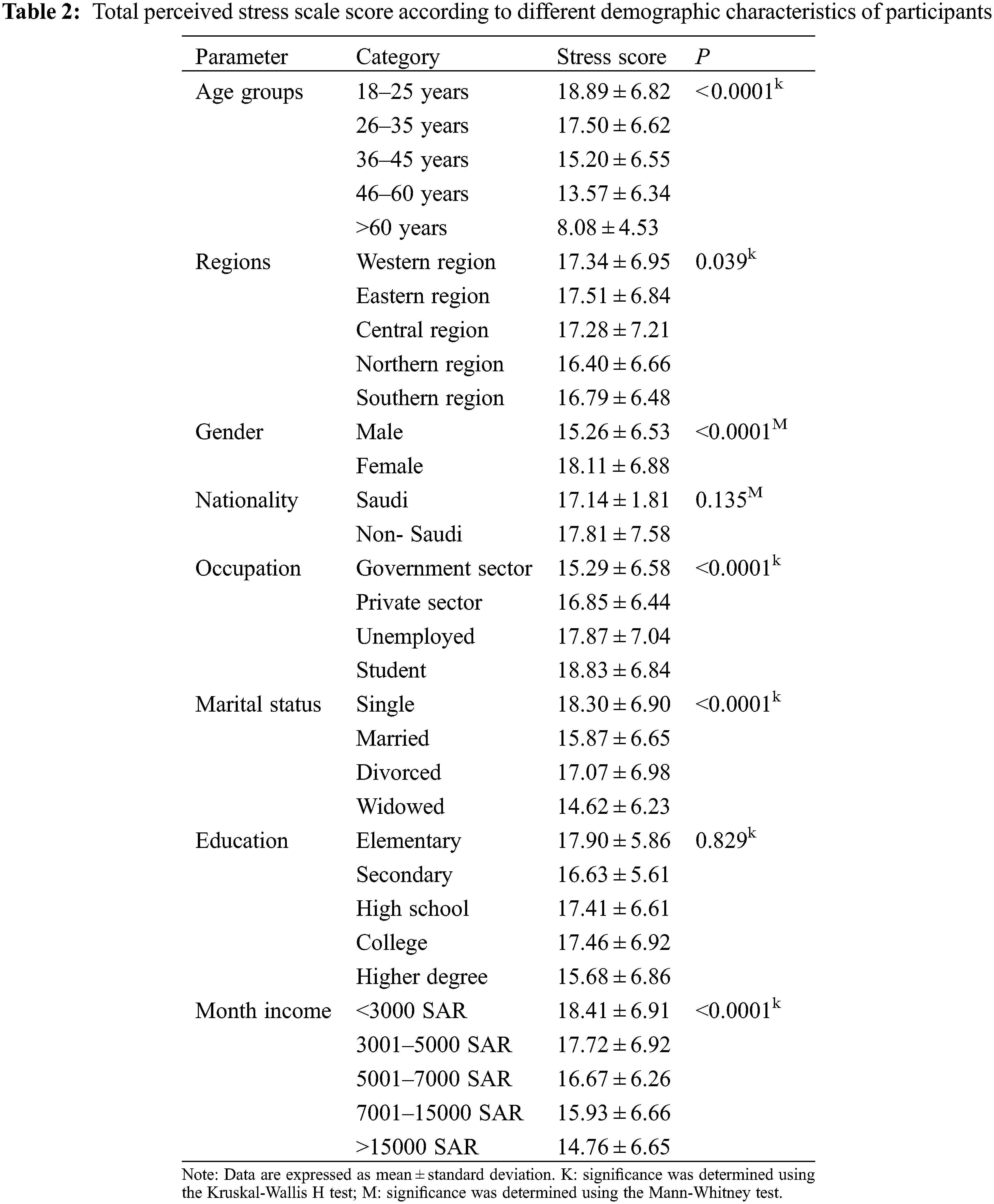
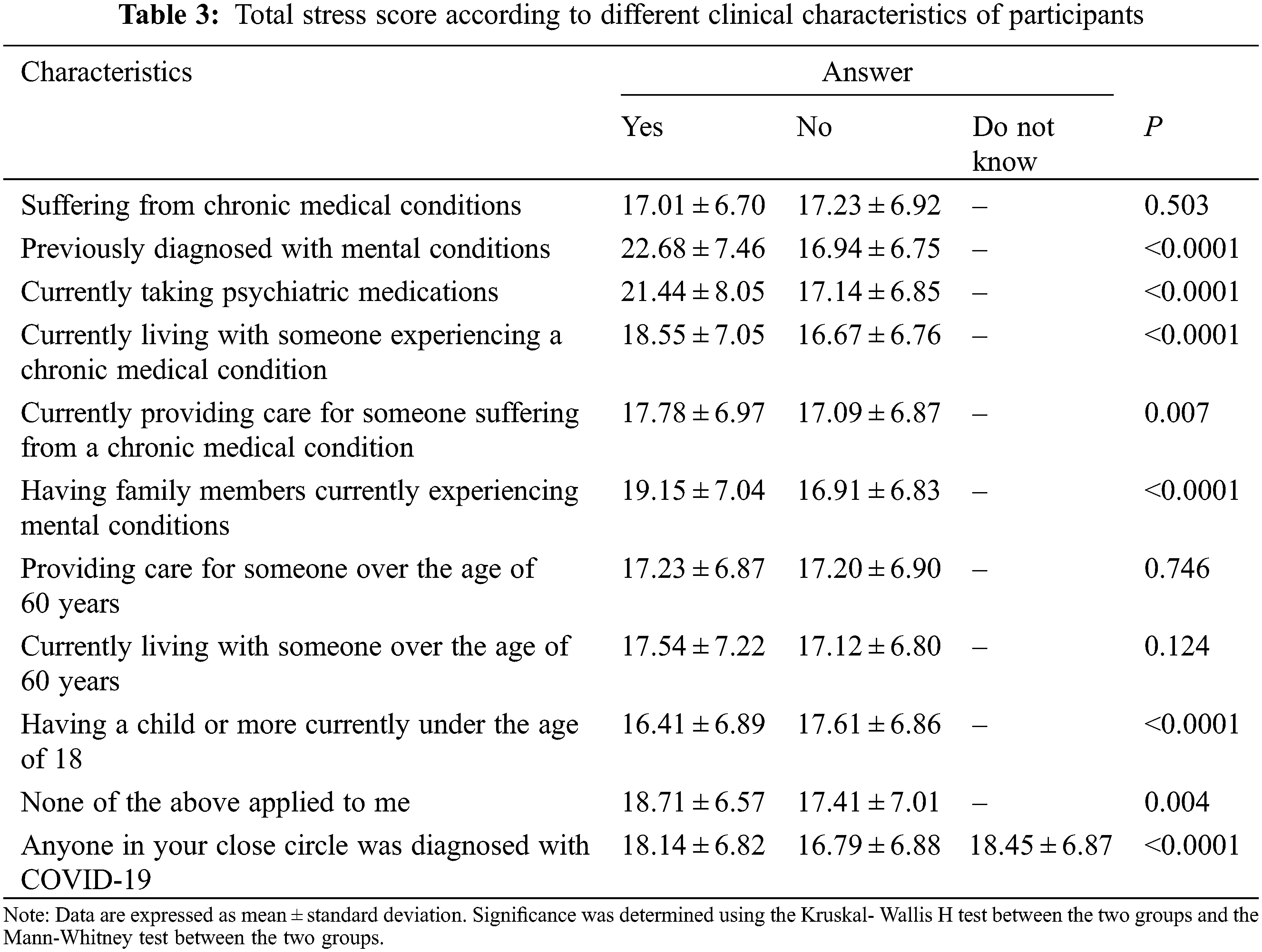
The PSS score was significantly higher for those previously diagnosed with a mental condition, currently taking psychiatric medications, currently living with someone experiencing chronic medical conditions, currently providing care for someone suffering from chronic medical conditions, having family members currently experiencing mental conditions, having a child or more currently under the age of 18, to whom none of the options applied, and having someone in one’s close circle diagnosed with COVID-19 (Table 3).
3.4 The Results of the Multivariate Regression Analysis
The multivariate analysis included the significantly associated demographic and clinical factors with the PSS scores and the composite scores of adaptive and maladaptive coping (Table 4). Predictor variables significantly influenced the perceived stress, F(40, 1) = 68.80, P < 0.0001, and they accounted for 30.3% of the variation in the perceived stress of the participants (R2 = 0.306, adjusted R2 = 0.303). Young and middle-aged adults, females, students, and individuals with low or middle monthly income levels had higher stress levels. The clinical predictors of high stress included having a personal or familial history of mental conditions (β = 2.98 and β = 0.92, respectively, P < 0.001 for both), living with someone with a chronic medical condition (β = 0.91, P < 0.001), and having someone with COVID-19 in the close circle (β = 0.75, P < 0.001). Higher stress scores were predicted by employing adaptive coping mechanisms less frequently (β = −0.23, P < 0.001) and maladaptive mechanisms more frequently (β = 0.63, P < 0.001).
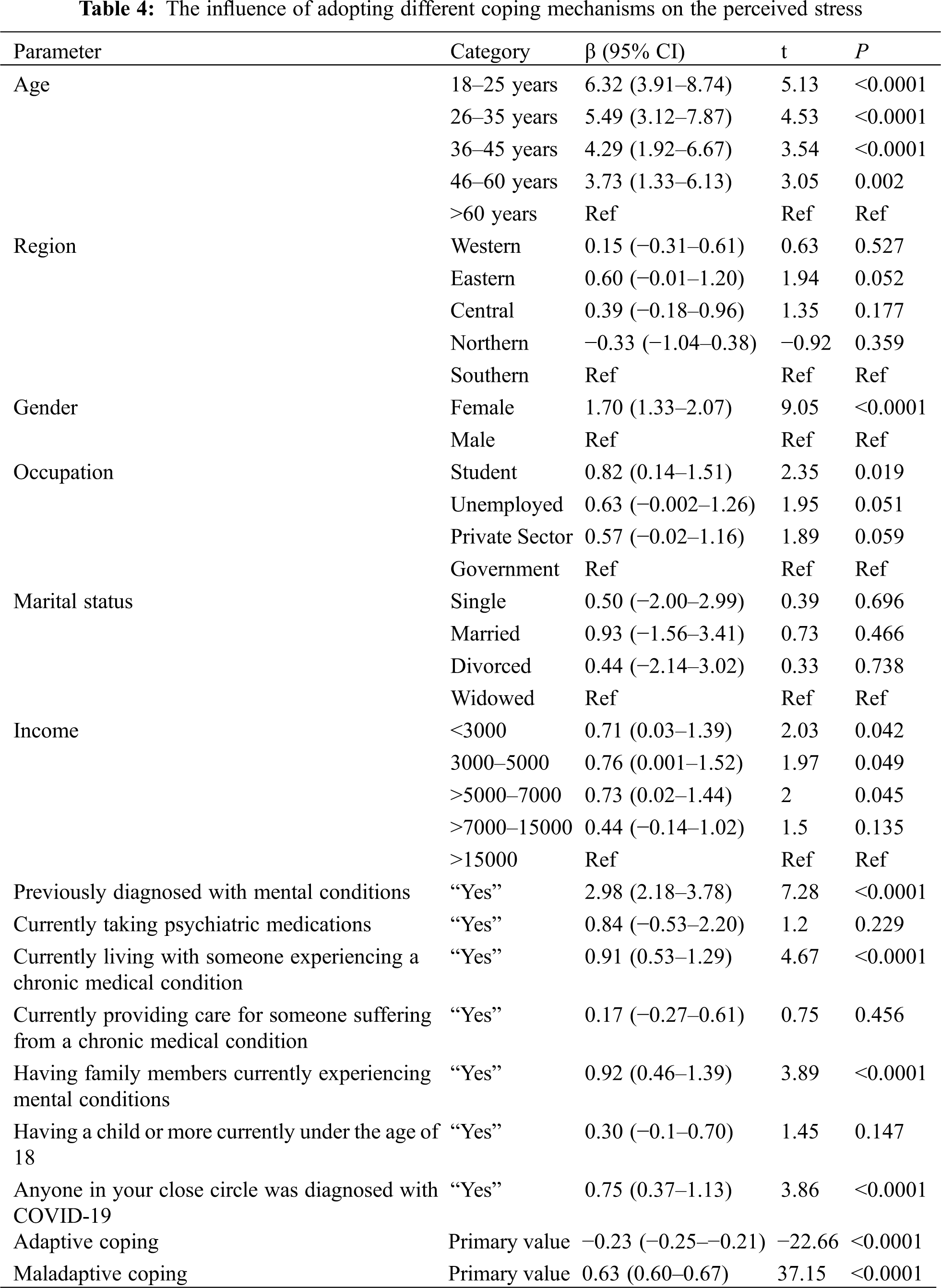
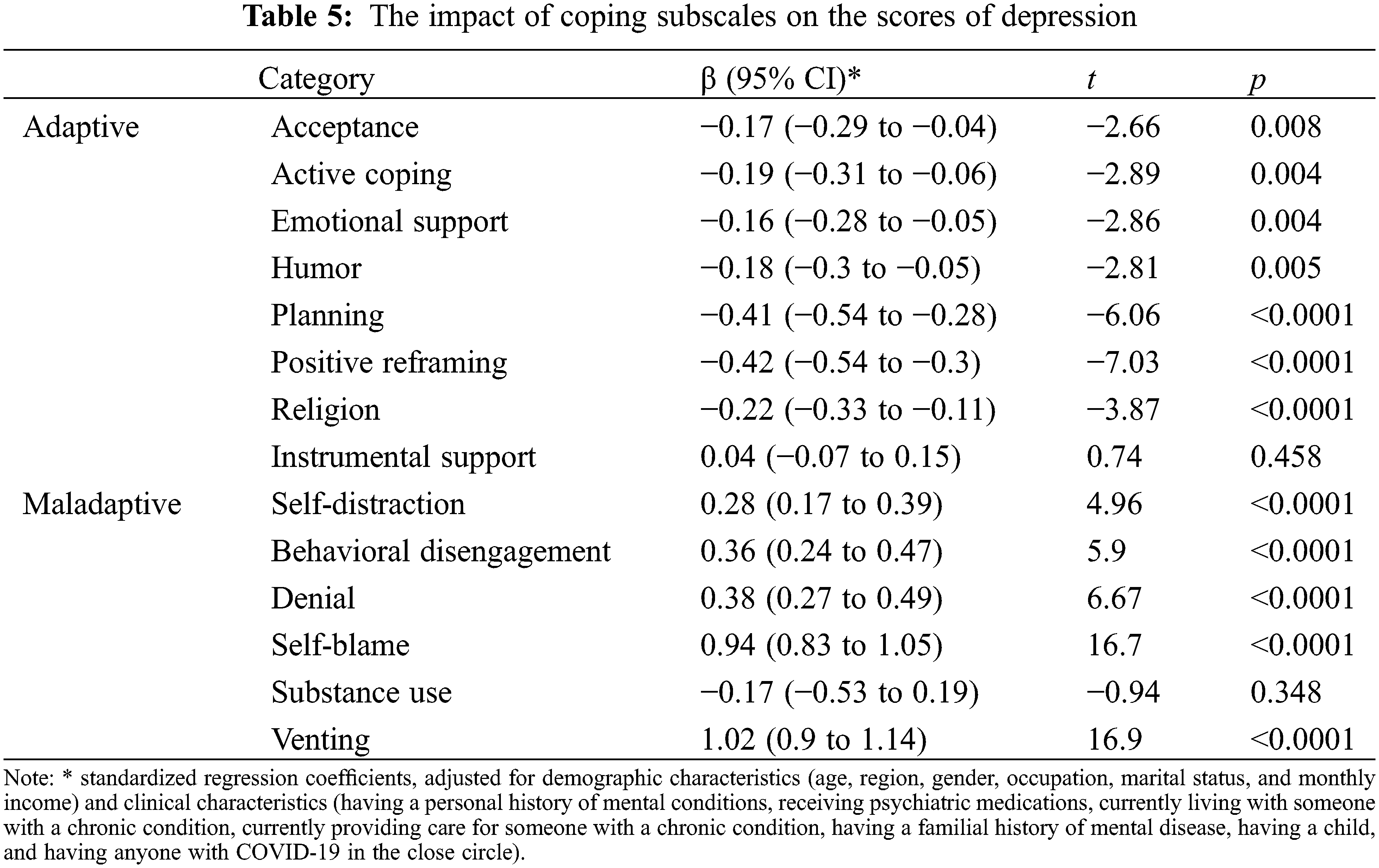
To further analyze the subscales of coping strategies as predictors of stress, the composite scores of coping were replaced with the subscales of coping mechanisms (n = 14) in the regression model, and the analysis was adjusted for demographic and clinical characteristics. Low stress scores were predicted by more frequent use of positive reframing (β = −0.42, P < 0.0001), planning (β = −0.41, P < 0.0001), returning to religion (β = −0.22, P < 0.0001), active coping (β = −0.19, P = 0.004), seeking emotional support (β = −0.16, P = 0.004), humor (β = −0.18, P = 0.005), and acceptance (β = −0.17, P = 0.008). Conversely, higher scores of venting (β = 1.02, P < 0.0001), self-blame (β = 0.94, P < 0.0001), being in denial (β = 0.38, P < 0.0001), behavioral disengagement (β = 0.36, P < 0.0001), and self-distraction (β = 0.28, P < 0.0001) were significant predictors of higher stress (Table 5).
Consistent with previous literature by Casagrande et al. and Huang et al. [8,13], 70% of the participants in this study reported moderate to high levels of stress during the pandemic. However, the mean score reported by Halayem et al. was higher than that of our study (28.8 vs. 17.2) [20]. This might be because their study’s sample population consisted of physicians in public hospitals.
Our findings indicated that a point increase in the composite adaptive coping score corresponded to a 0.23 decrease in the PSS-10 score, and all the subscales of positive coping (except the instrumental support) predicted lower stress scores. The most used coping styles were religion, acceptance, and positive reframing for the adaptive category, while positive reframing, planning, and returning to religion were the most influential coping strategies for reducing stress scores. Given that Saudi Arabia is a religious country and religion is an accepted method in dealing with stress, this finding was not surprising. Prior studies have noted the importance of religion as a coping style and found that religious behaviors and beliefs were associated with better mental health and greater ability to cope [21,22]. Although using humor seems to be common in Saudi Arabia, especially during difficult times, all the previous studies reported humor as the least used coping style [23]. A possible explanation for this might be the phrasing of questions in the Arabic language, which could be misinterpreted, and a lack of humor appreciation as a coping style.
In contrast, an increase of one in the maladaptive composite score corresponded to a 0.63-point increase in the PSS-10 score, and all the maladaptive coping subscales (except substance use) predicted changes in stress. Self-distraction, venting, and self-blame were the most commonly used strategies in the maladaptive category, which is similar to the findings of Umucu and Lee, who studied stress related to COVID-19 in the US [24]. The similarity of the results might be due to the universal messages from the WHO, and local ministries of health. Unsurprisingly, substance use was the least used maladaptive coping style, and it did not predict changes in stress levels. This can be attributed to the legal status of substance use in the country, including the alcohol ban, which may lead to underreporting. Another possibility is that substance use is considered a sin in Islam.
The analysis confirmed that the younger population, female participants, students, and those in the low- and middle-income categories had an increased risk of high stress levels. This result is in line with previous studies that looked for the predisposing factors of the psychological impact of the COVID-19 pandemic and SARS survivors [25]. Consistent with our findings, females were more likely to experience stress during the COVID-19 pandemic, as revealed in India, and China [26,27]. Another important finding was that most of the participants who reported higher levels of stress were students, who are likely to experience uncertainty around exams and switching to remote learning during the COVID-19 pandemic. Low monthly incomes were also positively associated with higher stress levels. However, a large segment of our population comprised students, who tend to have a low income, which explains the correlation. Nevertheless, our findings were consistent with those of a previous study by Park et al. [28].
Certain clinical characteristics were investigated to determine their impact on stress levels during the COVID-19 pandemic. For example, individuals who were found to have high stress levels reported that a person close to them had been diagnosed with the virus. This finding was expected, as those with closer proximity to an infected patient might worry more about their social interactions and feel more stressed about carrying and spreading the disease. Furthermore, consistent with the literature, this research found that participants diagnosed with mental health conditions reported higher levels of stress. This could be attributed to being locked in, increased feelings of isolation, and the inability to reach their primary psychiatrist for follow-up or medication. This supports the results of Hao et al. [29], who demonstrated that psychiatric patients experienced more worries and had more intense suicidal ideation compared to the healthy control group. Moreover, they experienced a more negative psychological impact due to stricter lockdown or curfew measures.
Suffering from chronic physical medical conditions did not correlate with increased stress levels. This was surprising as chronic medical conditions predict poorer COVID-19 outcomes. Additionally, this finding is contrary to a previous study by Ozamiz-Etxebarria et al. [30], which found significantly higher stress responses to the COVID-19 pandemic among persons with medical comorbidities. This study’s finding could be attributed to the safety felt because of the lockdown and strict curfew regulations from the beginning of the pandemic. However, living with someone with a chronic medical condition correlated with higher levels of stress. This could be because they are more fearful of interacting with their social groups due to the fear of acquiring the disease and spreading it to their household members.
Several limitations should be considered in this study. First, this is a self-report, cross-sectional study that reflects the coping styles and stress levels of the population at a particular time. It was not possible to compare the results to levels of stress before the pandemic. Second, the results’ generalizability is limited by the recruitment method as the questionnaire was distributed to attendees of pandemic-related public awareness webinars. As a result, the participants were interested in knowing more about COVID-19, reflecting more concerns about the pandemic. Finally, it is beyond this study’s scope to find a causal relationship between stress levels and the use of coping styles.
Stress represents a significant problem during the outbreaks of infectious diseases, and COVID-19 is no exception. The current study’s findings demonstrated that more than two-thirds of a sample from the general population in Saudi Arabia had moderate to severe stress due to the pandemic. Religion and acceptance were the most used adaptive coping styles, whereas self-distraction and venting were frequently employed negative coping approaches. Stress was higher among distinct demographic groups and specific clinical characteristics. Furthermore, using positive coping styles less frequently, and negative coping strategies more frequently, were independently associated with higher stress. The present study’s findings will help mental health care workers direct their services most suitably by understanding how the public manages this unique situation.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Lu, R., Zhao, X., Li, J., Niu, P., Yang, B. et al. (2020). Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. The Lancet, 395(10224), 565–74. DOI 10.1016/S0140-6736(20)30251-8. [Google Scholar] [CrossRef]
2. Lai, C. C., Shih, T. P., Ko, W. C., Tang, H. J., Hsueh, P. R. (2020). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19The epidemic and the challenges. International Journal of Antimicrobial Agents, 55, 105924. DOI 10.1016/j.ijantimicag.2020.105924. [Google Scholar] [CrossRef]
3. WHO (2020). Novel Coronavirus (2019-nCoV): Situation report 11. https://apps.who.int/iris/handle/10665/330776. [Google Scholar]
4. WHO (2020). Weekly epidemiological update-1 December 2020. https://www.who.int/publications/m/item/weekly-epidemiological-update---1-december-2020. [Google Scholar]
5. Bao, Y., Sun, Y., Meng, S., Shi, J., Lu, L. (2020). 2019-nCoV epidemic: Address mental health care to empower society. The Lancet, 395, e37–8. DOI 10.1016/S0140-6736(20)30309-3. [Google Scholar] [CrossRef]
6. Liang, L., Ren, H., Cao, R., Hu, Y., Qin, Z. et al. (2020). The effect of COVID-19 on youth mental health. Psychiatric Quarterly, 91(3), 841–52. DOI 10.1007/s11126-020-09744-3. [Google Scholar] [CrossRef]
7. https://apps.who.int [Internet]. Novel Coronavirus (2019-nCoV): Situation report 43: WHO; 2020. (2020). [cited: 20/5/2020] Available from: https://apps.who.int/iris/handle/10665/331354. [Google Scholar]
8. Casagrande, M., Favieri, F., Tambelli, R., Forte, G. (2020). The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Medicine, 75, 12–20. DOI 10.1016/j.sleep.2020.05.011. [Google Scholar] [CrossRef]
9. Zandifar, A., Badrfam, R. (2020). Iranian mental health during the COVID-19 epidemic. Asian Journal of Psychiatry, 51, 101990. DOI 10.1016/j.ajp.2020.101990. [Google Scholar] [CrossRef]
10. Nickell, L. A., Crighton, E. J., Tracy, C. S., Al-Enazy, H., Bolaji, Y. et al. (2004). Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. Canadian Medical Association Journal, 170(5), 793–798. DOI 10.1503/cmaj.1031077. [Google Scholar] [CrossRef]
11. Cheng, S. K. W., Wong, C. W., Tsang, J., Wong, K. C. (2004). Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS). Psychological Medicine, 34(7), 1187–1195. DOI 10.1017/S0033291704002272. [Google Scholar] [CrossRef]
12. Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L. et al. (2020). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity, 87, 40–48. DOI 10.1016/j.bbi.2020.04.028. [Google Scholar] [CrossRef]
13. Huang, Y., Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research, 288, 112954. DOI 10.1016/j.psychres.2020.112954. [Google Scholar] [CrossRef]
14. Moghanibashi-Mansourieh, A. (2020). Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian Journal of Psychiatry, 51, 102076. DOI 10.1016/j.ajp.2020.102076. [Google Scholar] [CrossRef]
15. Al-Hanawi, M. K., Mwale, M. L., Alshareef, N., Qattan, A. M. N., Angawi, K. et al. (2020). Psychological distress amongst health workers and the general public during the COVID-19 pandemic in Saudi Arabia. Risk Management and Healthcare Policy, 13, 733–742. DOI 10.2147/RMHP.S264037. [Google Scholar] [CrossRef]
16. Wang, H., Xia, Q., Xiong, Z., Li, Z., Xiang, W. et al. (2020). The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: A web-based survey. PLoS One, 15(5), e0233410. DOI 10.1371/journal.pone.0233410. [Google Scholar] [CrossRef]
17. Carver, C. S. (1997). You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine, 4(1), 92–100. DOI 10.1207/s15327558ijbm0401_6. [Google Scholar] [CrossRef]
18. Nawel, H., Elisabeth, S. (2015). Adaptation and validation of the Tunisian version of the brief COPE scale. European Journal of Health Psychology, 17, 783. [Google Scholar]
19. Almadi, T., Cathers, I., Hamdan, M. A. M., Chow, C. M. (2012). An arabic version of the perceived stress scale: Translation and validation study. International Journal of Nursing Studies, 49(1), 84–89. DOI 10.1016/j.ijnurstu.2011.07.012. [Google Scholar] [CrossRef]
20. Halayem, S., Sayari, N., Cherif, W., Cheour, M., Damak, R. (2020). How Tunisians physicians of public health hospitals deal with COVID-19 pandemic? Perceived stress and coping strategies. Psychiatry and Clinical Neurosciences, 74(9), 496–497. DOI 10.1111/pcn.13097. [Google Scholar] [CrossRef]
21. Koenig, H. G., Larson, D. B., Larson, S. S. (2001). Religion and coping with serious medical illness. Annals of Pharmacotherapy, 35(3), 352–359. DOI 10.1345/aph.10215. [Google Scholar] [CrossRef]
22. Shaheen, A., Ahwal, M., Al Zaben, F., Sehlo, M. G., Khalifa, D. A. et al. (2016). Religious beliefs, practices, and health in colorectal cancer patients in Saudi Arabia. Psychooncology, 25(3), 292–299. DOI 10.1002/pon.3845. [Google Scholar] [CrossRef]
23. Alosaimi, F. D., Alawad, H. S., Alamri, A. K., Saeed, A. I., Aljuaydi, K. A. et al. (2018). Stress and coping among consultant physicians working in Saudi Arabia. Annals of Saudi Medicine, 38(3), 214–224. DOI 10.5144/0256-4947.2018.214. [Google Scholar] [CrossRef]
24. Umucu, E., Lee, B. (2020). Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabilitation Psychology, 65(3), 193–198. DOI 10.1037/rep0000328. [Google Scholar] [CrossRef]
25. Mak, I. W. C., Chu, C. M., Pan, P. C., Yiu, M. G. C., Ho, S. C. et al. (2010). Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. General Hospital Psychiatry, 32(6), 590–598. DOI 10.1016/j.genhosppsych.2010.07.007. [Google Scholar] [CrossRef]
26. Wilson, W., Raj, J. P., Rao, S., Ghiya, M., Nedungalaparambil, N. M. et al. (2020). And depression among healthcare workers managing COVID-19 pandemic in India : A nationwide observational study. Indian Journal of Psychological Medicine, 42(4), 353–358. DOI 10.1177/0253717620933992. [Google Scholar] [CrossRef]
27. Yan, S., Xu, R., Stratton, T. D., Kavcic, V., Luo, D. et al. (2021). Sex differences and psychological stress: Responses to the COVID-19 pandemic in China. BMC Public Health, 21(1), 79. DOI 10.1186/s12889-020-10085-w. [Google Scholar] [CrossRef]
28. Park, C. L., Russell, B. S., Fendrich, M., Finkelstein-Fox, L., Hutchison, M. (2020). Americans’ COVID-19 stress, coping, and adherence to CDC guidelines. Journal of General Internal Medicine, 35(8), 2296–2303. DOI 10.1007/s11606-020-05898-9. [Google Scholar] [CrossRef]
29. Hao, F., Tan, W., Jiang, L., Zhang, L., Zhao, X. et al. (2020). Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain, Behavior, and Immunity, 87, 100–106. DOI 10.1016/j.bbi.2020.04.069. [Google Scholar] [CrossRef]
30. Ozamiz-Etxebarria, N., Dosil-Santamaria, M., Picaza-Gorrochategui, M., Idoiaga-Mondragon, N. (2020). Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the Northern Spain. Cadernos de Saúde Pública, 36(4), e00054020. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |