
 | International Journal of Mental Health Promotion |  |
DOI: 10.32604/ijmhp.2022.022522
ARTICLE
Nonprecsion (Standard) Psychosocial Interventions for the Treatment of Mental Disorders
Department of Psychology, Yale University, New Haven, Connecticut, 06520-8205, USA
*Corresponding Author: Alan E. Kazdin. Email: alan.kazdin@yale.edu
Received: 14 March 2022; Accepted: 11 April 2022
Abstract: Advances in precision treatment promise to greatly improve the extent to which therapies for mental disorders are better matched to patient characteristics. At the same, we need to ensure that more readily disseminable and available nonprecison treatments are further developed as well. These treatments refer to standardized interventions that do not have to be individualized and are more readily available. Impetus for this call stems from the treatment gap, namely, the huge difference in the proportion of individuals who are in need of mental health services and who actually receive any form of treatment. The prevalence rates for mental disorders worldwide are high and in low-, middle-, and high-income countries and the vast majority of individuals in need of services receive none. To address the need, we need interventions that can reach large numbers of individuals and especially target those individuals least likely to receive services. Standardized treatments that can be widely applied may be in a better position at present to reach people in need who otherwise receive no care.
Keywords: Treatment of mental disorders; nonprecision treatment; closing the treatment gap
Precision medicine reflects advances that integrate improved methods of diagnosis, assessment, and treatment. The promise of better matching treatments with characteristics of individual patients has already seen gains in many areas of medicine. Advances have extended to psychotherapy with the similar goal of matching patients to treatments for which they are especially well suited. While advances are made in precision interventions, it is critical not to lose sight of the pivotal role of nonprecision interventions as well. These are evidence-based treatments that have been well studied but are not tailored in a way that is the focus of precision care. This sounds like a retreat from moving forward toward increased precision. Yet, there are separate roles for precision and more standard interventions and it is important to underscore the latter of these in the context of mental health care. The present article conveys the continued, and indeed accelerated need, for standardized (nonprecision) interventions that can be extended for the treatment of mental disorders. There is no necessary conflict with advancing both precision and standard interventions that are not individualized. Indeed, they serve different needs and purposes at the present time as will be elaborated here.
Precision interventions refer to care in which the treatment is tailored or customized to the individualized client. The interventions draw from data about the patient’s characteristics and how these relate to clinical outcomes. The importance of the characteristics of the individual patient was nicely summarized by the Greek physician, Hippocrates (c. 460 BC-c. 370 BC) who is credited with saying, “It is far more important to know what sort of person the disease has than what sort of disease the person has” [1]. In keeping with that, precision interventions are sometimes referred to as personalized and person-centered rather than disorder-centered care.
Precision medicine is the most familiar area in which efforts are made to identify individualized care. Advances are evident for a variety of conditions and diseases [2,3]. These advances have been facilitated by drawing on analyses of biomarkers and clinical profiles and the use of “big data,” artificial intelligence, predictive analytics, and machine learning, among other tools, to help in decision making and matching patients and treatments. Efforts to provide precision care have extended to many areas including nutrition, learning, pharmacotherapy, dentistry, gerontology, nursing care, law and policy, agriculture, forestation, advertising and marketing, and of course, dating, as in courtship and finding a mate, rather than in forensics or anthropology.
Precision psychotherapy and the treatment of mental disorders is another such area and has advanced as well [4–6]. Impetus has stemmed from several factors including findings that:
• in controlled studies that compare various psychotherapies, on average the outcomes often are no different;
• within a given treatment condition, there is considerable variation in client outcomes;
• the initial treatment individuals receive often is not helpful and patients have to pursue multiple treatments before reaching one that has helped with their psychiatric disorder;
• clients from and within different cultures are likely to have preferences or personal characteristics that make a given treatment much more compatible with their views; and
• treatments differ in their feasibility in administration for different clients [7–11].
These findings support the view that greater precision is needed in matching treatments to individual clients. Now several models (e.g., conceptual, statistical) and measures to operationalize them are being explored [4,12,13].
To sure, there are many challenges related to fine-grained assessment and diagnosis that provide the data for decision making, the optimal models used to integrate the data, actual testing to evaluate whether precision therapies are invariably better than standardized treatment, extending the models to clinical practice, and others. Even so, addressing the many challenges is part of an ongoing process well underway. No doubt more precise forms of therapy will be increasingly evaluated in controlled trials to test whether or the extent to which they improve on standard (nonprecision) care and then in tests of the optimal ways of disseminating precision methods to clinical practice. The progress, benefits, and promise of precision psychotherapy are to be celebrated, even though it may be a while before the benefits are routinely applied in clinical settings.
The importance of precise interventions is often underscored by citing the lay cliché that “one size does not fit all” [2,14–18]. The “one size” is a reference to standard care currently in practice. We are very familiar with the cliché in the context of clothing where it emerged and meaning, of course, that any garment designed to fit all or most people is not likely to fit many people very well. And, in the context of psychotherapy, the cliché indeed still applies. One form or a standard (nonprecision) version of therapy cannot be expected to be effective for everyone. There is an obvious way in which that cannot be argued, but there is another side that challenges the cliché in light of what we know about the prevalence of mental illness and the paucity of psychosocial treatments actually provided to people in need of services. Consider what might be called the case for standardized (nonprecision) treatments.
The treatment gap refers to the difference in the proportion of people who have disorders or a specific disorder (prevalence) and the proportion of those individuals who receive care [19,20]. In the context of mental health, considerable evidence has addressed and documented the gap worldwide and for various disorders and age groups [21–25].
2.1 Prevalence of Mental Disorders
The initial facet relevant to the treatment gap is the prevalence of mental disorders. Two common metrics are prevalence at a given period of time (often within the past year) and over the course of one’s life. For example, a series of studies has been ongoing as part of the World Mental Health Survey, an initiative from the World Health Organization (WHO), that periodically assesses mental disorders, substance use, and behavioral problems in multiple countries (see https://www.hcp.med.harvard.edu/wmh/). In one report, 12-month and lifetime prevalence were evaluated among 28 countries (e.g., United States, Mexico, Nigeria, South Africa, France, Ukraine, Japan, New Zealand) from multiple regions of the world. Within a one-year period, prevalence ranged from 6.0 percent (Nigeria) to 27.0 percent (US). Lifetime prevalence ranged from a low of 12.0 percent to a high of 47.4 percent (same countries, respectively) [26]. In general, prevalence of disorders was generally higher in high-income countries than in low- and middle-income countries.
Two other large-scale surveys briefly noted, convey high prevalence rates, even though the surveys vary in many ways (e.g., countries that are sampled, type of disorder that is studied, and diagnostic system used [versions of DSM, ICD]). First, a large-scale evaluation in the European Union (EU) included data from all member states (N = 27) plus Switzerland, Iceland and Norway [27]. In a given year, 38.2 percent of the EU population suffered from a mental disorder. That corresponded to approximately 165 million people, from childhood through late adulthood.
Second, in the United States (US), from reports of the National Comorbidity Study, we have learned that 26 percent of the US population meet criteria for a psychiatric disorder within the past 12 months [28,29]. This increases to 46 percent of the population over the course of life [30]. For ease of computation, consider that approximately 25 percent of the US population experience a psychiatric disorder during a given year and 50 percent in their lifetime. From a US population of approximately 333 million, at the time of this writing, this translates to approximately 83 million and 167 million people, respectively.
Any effort to be precise about the prevalence rates must be qualified. The rates are a moving target in light of changes over time in the diagnostic criteria for many disorders, the emergence of newly defined disorders and elimination of others, and different methods of assessment (in person vs. phone interviews; retrospective vs. prospective studies) and the actual instruments (questionnaires) that the surveys use. Important to add is that the estimates from many surveys may well be conservative; some disorders (e.g., schizophrenia) as well as subsyndromal (subclinical) disorders often are omitted. In addition, some populations with high rates of mental disorder (e.g., prisoners) usually are excluded. Moreover, some evidence points to increases in the rates of disorders in the past 10–20 years [31–33]. Notwithstanding these caveats, the conclusion remains, namely, mental disorders are prevalent worldwide.
2.2 Receipt of Services for Mental Disorders
The second facet of the treatment gap pertains to the proportion of those with mental disorders and in in need of services who actually receive them. The WHO Mental Health Survey Consortium provided extensive data on this matter in surveys of over 60,000 adults in 14 countries in the Americas, Europe, Middle East, Africa, and Asia [34]. The proportion of respondents who received treatment for emotional or substance-use disorders during the previous 12 months ranged from a low of 0.8 percent (Nigeria) to a high of 15.3 percent (US). These percentages refer to those who received treatment among those in need. These numbers convey that the vast majority (99.2 percent and 84.7 percent, respectively, by subtracting the above percentages from 100 percent) of individuals in need did not receive treatment. Another review conveyed the treatment gap in relation to depression across 21 countries [35]. In high-income countries, 1 in 5 (20 percent) individuals with depression received treatment. In low- and middle-income countries, 1 in 27 (3.7 percent) received treatment. Overall, among many countries, disorders, time frames, and measures the conclusion remains that most people with a diagnosable psychiatric condition do not receive treatment.
Focusing on one country reveals within population variation as well as the larger problem of most people not receiving treatment. For example, in the US, approximately 70 percent of people in need do not receive any services [36]. Ethnic minority groups (e.g., African, Hispanic, and Native Americans) have much less access to care than do European Americans [37–39]. For example, African Americans are less likely to have access to services than are European Americans (12.5 vs. 25.4 percent), and Hispanic Americans are less likely to have adequate care than are European Americans (10.7 vs. 22.7 percent) [40]. No doubt, each country has its groups (e.g., in rural areas, indigenous people, immigrants) that are especially unlikely to receive mental health services. The lack of available services for most people and systematic disparities among those services underlie the importance of delivering services in ways that can reach many more people as well as can target special groups.
Among the small minority of individuals who do receive services, what exactly do they receive? In the WHO study, receiving services was based on asking respondents if they ever had any contact from a long list of caregivers either as an outpatient or inpatient for problems with emotions, nerves, mental health, or use of alcohol or drugs. Included were mental health professionals (e.g., psychiatrist, psychologist), general medical or other professionals (e.g., general practitioner, occupational therapist), religious counselors (e.g., minister, sheikh), and traditional healers (e.g., herbalist, spiritualist). The list varied among countries depending on local circumstances where types of healers vary. The precise service provided by these individuals was not identified. Also, the duration of the intervention was not known, but receiving services required at least one contact. Thus, when we say that 15 percent of individuals received treatment, information is ambiguous and could be one contact with someone who has had no training in mental health.
In the US, the National Comorbidity Survey-Replication study also has provided data on who receives treatment as well as some further information about the nature of that treatment [41]. Over 9,000 individuals with psychiatric disorders answered questions about their treatment that included who the service provider was (e.g., psychiatric, family physical, social worker, spiritual advisor and others) and the type of treatment they received (e.g., self-help group, medication, hospital admission). The study evaluated whether individuals received any treatment and if so if this was minimally adequate, which was defined as receiving an intervention (e.g., medication, psychotherapy) that followed evidence-based guidelines for the specific disorder and included multiple contacts (rather than only one visit). For individuals with a psychiatric disorder, 21.5 percent received treatment from a mental health specialist; 41.7 percent received treatment if this is expanded to include contact with any health-care person, in addition to those trained in mental health. For individuals who did not meet criteria for disorder (subsyndromal disorder), 4.4 percent received treatment from a mental health specialist and 10.1 percent received treatment if this is expanded to include any contact. Overall, across the entire sample, only 32.7 percent were classified as receiving at least minimally adequate treatment. The investigators concluded that only one third of treatments provided met minimal standards of adequacy based on evidence-based treatment guidelines.
Key points summarize the state of the treatment gap. First, prevalence rates of mental disorders is high. Second, most individuals with mental disorders do not receive treatment and that applies to low-, middle-, and high-income countries. There is no single summary percentage one can provide because of variation among studies in: the disorders that are included (e.g., subsyndromal disorders, substance use and abuse, personality disorders); in what counts as treatment; the list of who is included as potential service providers (e.g., mental health professional, religious leader); and the ethnicity, culture, and country of the sample. And yet, through it all, it is clear that we are not providing treatment to the large majority of people in need of services.
Third when treatment is provided, it includes a variety of interventions administered by mental health professionals, health-care professionals in other areas (e.g., general practitioners), and by others (e.g., religious leaders, healers). This care usually refers to some contact. Yet that contact is not necessarily formalized psychological treatment or medication. Fourth and related, evidence-based treatments are used infrequently for mental disorders for the proportionately few individuals who do receive care. Epidemiological surveys have not been designed to probe in depth precisely what the interventions are, how long they are administered, and whether the persons administering the treatment are trained in use of the treatment. Yet, we know from other sources as well that evidence-based treatments are not being used for mental and substance use disorders as a general rule [42–44]. The goals for individual patients and service providers are not just to receive and provide any treatment but rather to receive and provide the best treatments and specifically those that have an evidence base. In addition to ensuring that the most well-supported interventions are provided to those who seek and receive treatment, we need to extend these treatments to the much larger group of people in need who receive no services at all.
The points about providing evidence-based treatment are obviously important but there are a variety of options. Among the key questions what treatments can reach the largest numbers of individuals in need of services. Next we consider options that vary in the extent to which they are individualized to each patient or are more general and applicable to many without such individualization.
3 Standard (Nonprecision) Treatment
3.1 Continuum of Individualization
The term “precision medicine” is often used interchangeably with “personalized medicine” [45,46]. I retain the recommended use of the National Research Council which suggests use of “precision” to not necessarily imply that the level of tailoring of treatment is at the individual (personal) level per se. The term precision medicine better addresses looking for samples and subsamples with some common set of characteristics. This is not quite individualized for every person [47,48].
With these considerations in mind, it is useful to distinguish three broad domains of interventions to better make the case for standard treatment. I refer to them as personalized, precision, and standard treatments. First, personalized interventions refers specifically to treatments that are tailored or crafted at the level of the individual patient. This would take advantage of the patient’s unique characteristics. No doubt those characteristics would draw on broader findings from precision-based interventions, but they are tailored in an even more refined way on an individual-by-individual basis. Currently this is not the main focus of treatment development.
Second, precision interventions refer to the integration of multiple sources of data to identify subgroups of individuals likely to respond to a given treatment [47,49]. Big data, artificial intelligence, and other tools I mentioned previously identify who is very likely to respond to treatment and then the treatment is applied to those individuals. The focus is not on each individual per se but subpopulations and cohorts that are likely to respond.
Third, are standard treatments. These are treatment packages (e.g., cognitively based therapy, transtreatments) that are commonly studied in randomized controlled trials of evidence-based treatments and occasionally drawn on in varying degrees in clinical practice. They are standard in the sense of including core components, often with treatment manuals that are available, and procedures that can be well specified. Any individualization that is done is based on clinical experience but is not usually formulated in any systematic way. For the standard treatments, decision making is largely disorder- or symptom-based with no formalized algorithm to dictate what treatment or components of treatment are needed for a given patient.
A disadvantage of standard treatments is that they evoke the applicable “one-size does not fit all” criticism. That is, applying a standard treatment (e.g., cognitive behavior therapy) to all (e.g., with major depression or with anxiety) is not likely to be effective for all patients. The objection is cogent but ignores two critical points. First, a top priority is to extend treatments so they reach people in need. A more standardized treatment that is nonprecision based is likely to be more readily disseminable, at least at present. Second, we all expect precision interventions to be much more effective than a standard treatment, given the one-size-fits-all concern. However, we have little evidence in the context of mental health services in research and clinical practice that a more precision-based treatment is more effective than a standard treatment for the treatment of mental disorders. Assume for a moment that such evidence accumulated. Precision-based treatments too will not be effective with everyone. Now we have the challenge of whether more precision-based treatments with their greater effectiveness (assumed not known) sacrifices in the ease reaching people in need. There is no need to pit one form of treatment against another.
I have distinguished the three domains of treatment. For purposes of presentation, it is useful to present these as distinct categories. However, the categories are only clear at the margins. Fig. 1 presents the three domains as represented by a Venn diagram.
Figure 1: Overlap of the different types of treatments
Note: For purpose of presentation delineating the three treatment types is useful, but as researches moves from standard treatment to more refined applications to subgroups and sub-subgroups who respond the treatment moves more toward precision and personalized treatment. The overlap nature of the relations means the clarity of whether treatment is standard or personalized is at the margins.
Consider that one begins studying a standard treatment. Soon one may learn a particular variable (sex, no comorbid disorders) influences the outcome so that some individuals respond well (e.g., individuals with a certain type of diagnosis or no comorbid disorders). So now the standard treatment is only applied to individuals likely to respond; other individuals receive some other treatment. That is, the standard treatment begins to be matched to a subgroup that is likely to respond. In other words, what might begin as a nonprecision or standard treatment can become increasingly more precision based. As research progresses and improved algorithms are developed, treatment decisions now might be based on finer-grained interventions-patient combinations to maximize effectiveness. That is, more sub and sub-subgroups can be distinguished so that the matching of the intervention to multiple characteristics is improved. This now moves into precision treatment and the degree of precision can increase with further knowledge about the types of persons and situations to which an intervention can be effectively applied. Treatment might move from precision to individualization too as one learns of very complex profiles to which a given treatment can be effectively applied. That is, precision treatments can move closer to personalized treatment. The treatments are not completely individualized but the subgroups are smaller and different treatments vary for those subgroups. The goal would be to improve further the matching of patients (subgroups) to treatment variations that optimize clinical outcomes.
3.2 Criteria of Interventions to Reach People in Need
A standard form of care is one in which treatment is applied to all with little or no change beyond what is usually done in relation to specific symptom profile, age, and other tacit changes clinicians carry out routinely and perhaps unsystematically and idiosyncratically. The treatment is standardized in terms of content and therapeutic-related activities and perhaps even manualized to guide the sessions. I am advocating standard treatments but not merely to continue business as usual. Indeed, with current practices, we know that most people in need receive no treatment at all. It is just that standardized (nonprecision) treatment at this point in time is much more likely to be delivered on a large-scale.
It is important to go beyond type of treatment because that facet of care does not alone guarantee closing the treatment gap. To reach many more people with clinical services, it is useful to consider key criteria that would be essential to include in any intervention, standardized or not. Table 1 provides a list of key criteria that a given intervention ought to meet. I highlight them here.

First, of course we would want to draw on evidence-based treatments. The criteria used to designate treatment as evidence based vary among multiple disciplines (e.g., psychology, psychiatry, social work), diverse professional organizations, and private and public agencies within and among countries (e.g., in the Americas, European Union). For present purposes, we can leave the variants aside. We want controlled studies (e.g., traditional randomized controlled trials, pragmatic trials) to support use of the intervention.
Second, scalability is the central criterion for overcoming the treatment gap. That we need interventions that can reach large numbers of individuals in need of services. This is distinguished from current psychosocial treatments whose use is very restricted including, its many variations (e.g., in person treatment, telepsychotherapy).
Third, reach as a criterion overlaps with, but is distinguishable from, scalability. Many groups are especially more likely to be excluded from treatment and for a variety of reasons. For example, in the US, these groups include children and adolescents, the elderly, ethnic and underrepresented group members, single-parents, victims of violence, and individuals with intellectual disabilities, of lower income, or living in rural areas. Members of these groups are even less likely to receive treatment than are individuals with none of these characteristics. Internationally, most people in low- , middle-, and high-income countries do not receive the needed services. And yet, there are some countries, as I mentioned previously, that are among the least likely to receive treatment. Scaling treatments so that more people receive them does not necessarily handle disparities in treatment within a given country and internationally among countries. Reach extends the criterion of scalability to ensure that those groups least likely to receive care are specifically targeted.
Fourth, affordability is important because cost is a major and multifaceted barrier to receiving or providing care. On the patient or receiving side, cost of individual sessions when not covered by insurance can deter people from seeking or remaining in a treatment that is otherwise available. Effective coverage (some form of insurance) is a strong determinants of whether people in need of services actually receive them [50,51].
Affordability is not merely dictated by insurance coverage. Some interventions can be recover the costs of their delivery and scaling. For example, the program referred to as Improving Access to Psychological Therapies (IAPT) in the United Kingdom is a large-scale program designed to greatly increase the availability of effective psychological treatment for depression and anxiety [52,53]. This is a government-based program within the English National Health Service and began in 2008 with programs to recruit and train therapists and in the process had extended the reach of treatment. The treatment has been extended on a large scale and demonstrated positive clinical outcomes. In relation to affordability, treatment was shown to have paid for itself (and more) in terms of government savings. Large numbers of patients were no longer receiving sick pay or receiving government benefits and these were the main sources of cost savings. In any case, providing more treatment does not invariably increase the expense of providing services. Indeed, there are often huge costs of not providing treatment (e.g., disability, emergency room visits, family and home services).
Fifth, acceptability of treatment has to do with consumer views of how appropriate, suitable, and reasonable the treatment or model of delivery is, that is, the means or procedures rather than the outcomes. Acceptability has been evaluated in the context of psychotherapy, medications, hospitalization and other-change interventions. Acceptability influences the likelihood that clients will seek, continue in, or drop out of treatment, whether clients carry out the procedures prescribed during treatment, and whether professionals (e.g., educators, therapists) actually use or implement the procedure correctly [54–57]. We know there are cultural and ethnic differences in seeking treatment, utilizing clinical services, and treatment preferences [58,59]. Thus, acceptability is not a property or characteristic of treatment per se, but a characteristic in the context of ethnic and cultural perspectives in relation to that treatment. In any case, to scale and reach people in need, the intervention needs to be acceptable, not to everyone but to large numbers.
3.3 Standard Treatments and Their Dissemination
The criteria I have outlined might be viewed as a starting point rather than an exhaustive list of all the criteria. Yet for closing the treatment gap, evidenced-based treatments that can be scaled are clearly core or minimal criteria. In an ideal world, precision interventions might meet these criteria and would become “standard care.” It will be great cause to rejoice when we have such treatments. Yet, there remains the challenge of reaching that vast majority of people with mental disorders who receive no treatment at all. The availability of precision treatment does not automatically change the plight of such individuals because the problem is not entirely or even perhaps primarily in the nature of the treatment (precision or not) but rather in scaling the treatment so it can reach the persons in need. Precision treatment will raise new challenges for clinicians in practice where novel assessments and diagnoses may be needed to guide decision making for each client. Thus, delivering these treatments may be more difficult than the standard fare clinicians currently provide. It seems that we would very much profit from an explicit emphasis advancing, developing, and establishing standard (nonprecision) interventions that can be very widely disseminated. This is not instead of precision interventions, but rather interventions that can be expected to have impact to large numbers even though (like any therapy) not everyone would benefit.
In principle, most of us favor the model of standardized or nonprecision interventions, although it sounds alien when stated that way. An obvious example of “the model” is in recent and current development of vaccinations for the COVID-19 virus. Given the need to reach many people worldwide in diverse situations (e.g., urban, rural; low-, middle-, and high-income countries), there was not much discussion of personalized or precision vaccines. We needed, as it were, nonprecision vaccines, that is, a standard intervention (vaccine and dose) that would be effective with many people and could be disseminated widely. We could say, “no one size fits all” and be correct. That is, the vaccine was not effective with everyone or equally effective among those for whom it had an effect. Indeed, some individuals are allergic to the vaccine [60]. Yet, the task was to get an effective intervention to most people in an efficient way that was scalable and could reach people with and without easy access to care. Yes, the “success” for uniform scalability, equal access, and the ability to reach to people and countries can be challenged. However the broader point is worth underscoring. Scaling the standard intervention was in fact able to reach millions of people. To be sure, precision vaccines are an important research topic in their own right and are on the horizon for various disorders [61,62]. Whenever everyone can receive a scalable precision vaccine that too, like the psychotherapy counterpart, will be cause to rejoice. In the meantime, we are fortunate to have the nonprecision versions that can reach many people (but still have problems of dissemination) and that do not have be individualized. Again, this does not mean everyone receives the benefit; it does mean we can reach many more people with a standard treatment and that treatment could make a huge difference.
I am not arguing that psychotherapy is like a vaccine or that the challenges of their dissemination are the same. I am saying that we want a standardized or nonprecision treatment that can be administered widely. It would not be expected to work with everyone which, as I noted, will also be the case with precision treatment. Yet, treatment will work for many and among those individuals who simply do not receive treatment, “one size fits all” is much better than no size at all. I am not arguing for a specific intervention, precision or nonprecision based, but only the use of interventions that can be scaled. A standard treatment package may be more likely to accomplish that at this point in time than one that can be personalized.
Let us assume that a standardized treatment is not as effective as a personalized intervention. If so, nonprecision treatment might be the considered as the first step in a stepped-care model. That is, a standardized more readily disseminable treatment may be the first choice only to be followed by a more nuanced (precision based) treatment if needed. We know from large-scale international surveys that the first treatment people receive for their mental disorder may not be seen as helpful and that clients often traverse many treatments before being helped [11]. Yet, the key task is getting treatment to people because that first treatment often does have impact for many patients. It is important to keep the context in mind. Most people in need of services for their psychiatric disorder do not receive any treatment, leaving aside the more nuanced matter of receiving evidence-based treatments.
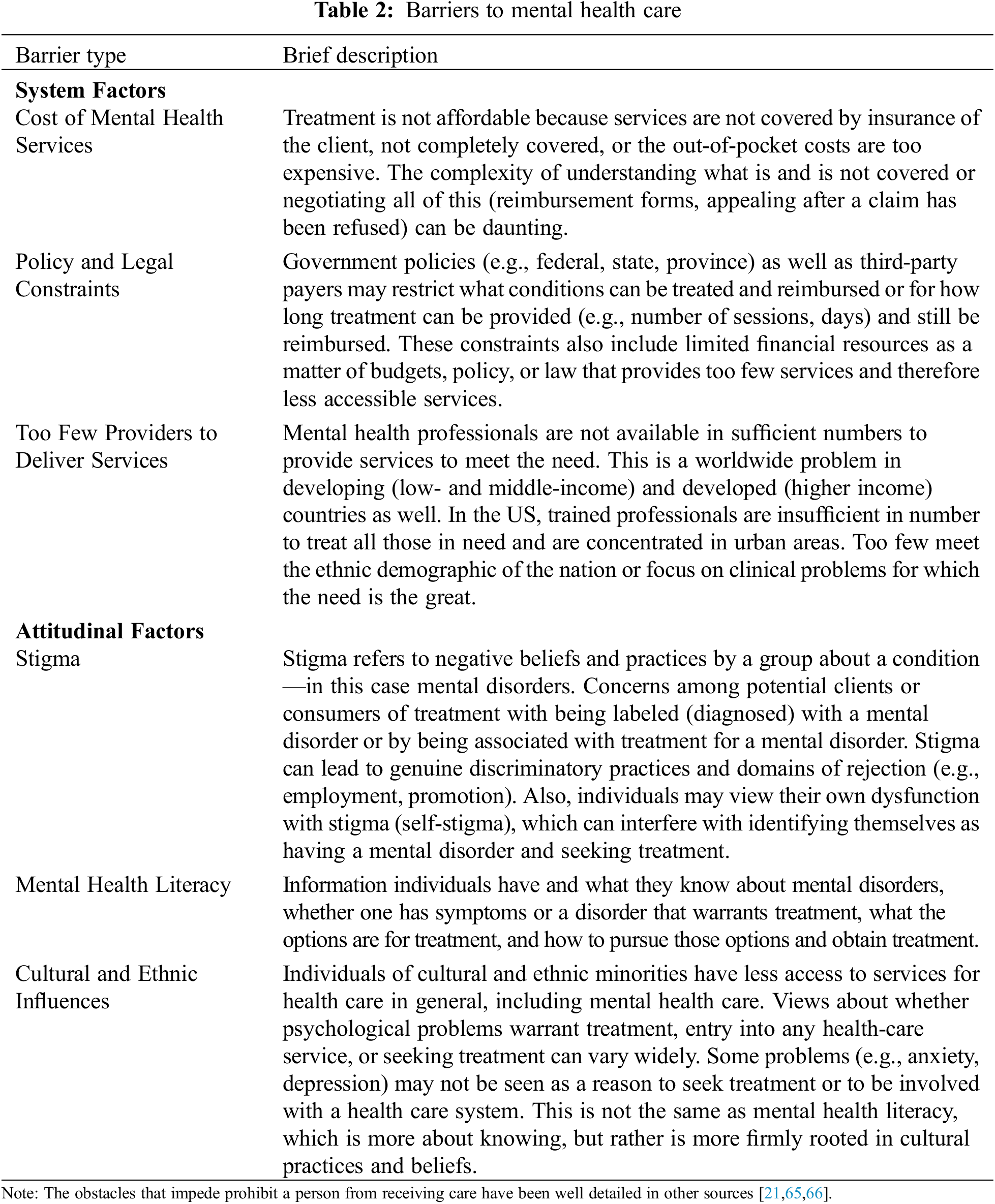
4 Obstacles to Service Delivery
I have emphasized the nature of the treatment (precision or standard) as a determinant of reaching people in need of services. Needless to say, there are other determinants of whether receive treatment. Among them is a large set of well-studied barriers to mental health treatment (see Table 2). For many individuals, even beginning the process of therapy is not perceived as worthwhile. For example, a survey in six European countries indicated that one third of individuals believed that professional mental health care is worse than or equal to no help at all for mental disorders [63]. A recent study surveyed 6 countries in the Americas and found that 43 percent of individuals with a mental disorder did not feel there was a need for treatment [64]. Thus, initial reticence in participating in treatment is rather widespread.
Assume for a moment that individuals wish to attend therapy for their mental disorders or symptoms. A key barrier in reaching such individuals is the dominant model of delivering psychotherapy. The dominant model of administering psychosocial therapies for mental disorders has three characteristics:
1. Treatment sessions are provided in person and one-to-one with a client (individual, couple, family);
2. Treatment is administered by a highly trained (e.g., master’s or doctoral level) mental health professional; and
3. Sessions are held at a clinic, private office, or health-care facility.
Access to clinical services that provide treatment in this model has been largely restricted to urban areas and to individuals who have insurance or can pay for their treatment. Interestingly, many individuals who do have access to mental health services do not seek treatment, among those who actively seek treatment, many never show up for the initial session, and among those who do show up and enter treatment, many dropout very early [67–70]. Efforts have been made to increase the initiation of treatment, attendance once one begins, remaining in treatment, and following through with prescribed practices during treatment [71–75]. However, it is unclear that such efforts have significantly improved utilization of treatment.
Other efforts to extend the reach of psychological services also have been developed. A primary example is integrated care where mental health and physical health services are provided in the same setting. Integrated care is a model of bringing together multiple resources to address the range of physical, mental health, and substance use problems and life-style practices (e.g., diet, exercise, cigarette smoking). Integrated care is an important effort to extend treatment and reduce some of barriers of seeking and obtaining mental health services [76,77]. Reducing barriers to treatment are pinitol but also need to be followed up with information about effectiveness and scalability.
I have argued for the continued and greatly extended need for standardized (nonprecision treatment) at this time, perhaps if and as we wait for precision treatments that can be scaled with equal ease as something less well tailored. I used the term nonprecision treatment to mean a standard treatment package (e.g., cognitive behavior therapy, transtreatments) that might be extended widely to people. This is not necessarily instead of precision treatment. Indeed we want to take advantage of the many areas that coalesce to improve diagnoses, collection and integration of data, artificial intelligence, machine learning and other areas that can not only improve matching clients to treatment but will no doubt improve the treatments. At this point in time, a key challenge of treatment is to reach people in need of services and reduce the prevalence and burdens of mental illness. Nonprecision treatments may not merely play a role but might play a central role insofar as these are likely candidates to reach people in need.
All options for treatment (precision, nonprecision, and variations in between) are welcome and needed. Indeed, an emphasis on the treatment side alone will not help reduce the burden of mental illness, except for the very select few who receive treatment. We are learning that better and more effective treatments alone do not seem to have impact on the prevalence of disorders [78].
We need to develop evidence-based treatments that address the criteria I have mentioned, with particular attention to scalability and reach. The delivery of treatments will need to be adapted to address constraints (e.g., health care delivery infrastructure, rural areas, and resources such as access to internet or phone services for delivery of treatment). Interventions that can be scaled and with reach to special populations may influence who is allowed to provide the interventions (e.g., lay persons, peers), expansion of the settings in which treatment is delivered (e.g., stores, beauty parlors, barbershops, public schools), the use of television, radio, and available media services, and a full panoply of available digital technologies (e.g., apps, telepsychotherapy), all of which I mentioned (in parentheses) already have precedence and with supportive evidence [79].
The use of technology may hold special promise in extending treatment. Digital mental health services refer to an array of interventions that are delivered online, via mobile devices, and other uses of technology [80,81]. Included in this is telemedicine, which refers to the use of communication and information technology to extend the reach of medical practice including assessment, diagnosis, and treatment. Telemedicine has been in use for many decades [82,83]. In relation to psychological treatments, telemedicine is a very active area of research and practice, bolstered even more in light of the recent COVID pandemic and the increased isolation and condiment of both clients and practitioners. Of course, technological developments have provided many additional ways of providing services. Using smartphones, watches, and tablets and smart clothing and various other sensors (e.g., in the car, home) provide opportunities for assessing psychological states and bringing interventions to individuals in their everyday lives [84,85].
Online delivery of treatment extends of the dominant model of therapy. For example, multiple options are available online for the treatment of anxiety and depression [80,86]. These programs often include the same core cognitive behavioral treatment sessions as used with in-person treatment (e.g., scheduling of positive activities, identifying and challenging cognitive distortions) and are divided into sessions (with video clips describing key information and assigned home- work) that patients can complete from home. There are now scores of other evidence-based self-help psychosocial interventions for a range of psychological problems [87–89]. These interventions can leap over many of the usual barriers of receiving treatment and expand on the dominant model of in-person, individual psychotherapy delivered at a clinic.
Although the goal is to reach more people who are not otherwise served, this is not invariably the case. For example, extensions of telemedicine for mental health services can increase rates of services for white patients but decrease use of services for underrepresented groups [80]. There are efforts to extend digital intervention to underrepresented and marginalized groups but more evidence is needed to establish their efficacy [90,91].
A key challenge among many technology based interventions is that the development of treatment (e.g., mobile apps) has greatly outstripped the evidence for their effectiveness. Controlled trials do not routinely follow once a mobile application has been developed. Even so, there is considerable evidence that digital variations of treatments (e.g., cognitive therapy, interpersonally psychotherapy) can be extended to populations and places that are not otherwise reached by the dominant model of treatment [81,92]. Digital mental health services hold great promise. Their scalability may be among the most salient feature.
Returning to the metaphor of clothing, it is true that one size does not fit all. However, if most people do not have clothing, that one size will go a long way in being of palpable help. It will not only fit many people, but it is also likely to be better than nothing (no clothing, no treatment). In the context of mental health services, most people in low- , middle- , and high-income countries in need of mental health services receive no treatment. It will be important to connect progress on the intervention side (precision or nonprecision treatment) with progress in delivery side to reduce the enormous treatment gap and the burdens of mental illness.
Acknowledgement: The author is grateful for the supportive environment that Yale University provides for my work.
Funding Statement: The author received no funding for this study.
Conflicts of Interest: The author declares that they have no conflicts of interest to report regarding the present study.
1. Vargas, A. J., Harris, C. C. (2016). Biomarker development in the precision medicine era: Lung cancer as a case study. Nature Reviews Cancer, 16(8), 525–537. DOI 10.1038/nrc.2016.56. [Google Scholar] [CrossRef]
2. Brandsma, C. A., van den Berge, M., Hackett, T. L., Brusselle, G., Timens, W. (2020). Recent advances in chronic obstructive pulmonary disease pathogenesis: From disease mechanisms to precision medicine. Journal of Pathology, 250(5), 624–635. DOI 10.1002/path.5364. [Google Scholar] [CrossRef]
3. Haggarty, S. J., Karmacharya, R., Perlis, R. H. (2021). Advances toward precision medicine for bipolar disorder: Mechanisms & molecules. Molecular Psychiatry, 26(1), 168–185. DOI 10.1038/s41380-020-0831-4. [Google Scholar] [CrossRef]
4. Cohen, Z. D., Delgadillo, J., DeRubeis, R. J. (2021). Personalized treatment approaches. In: Barkham, M., Lutz, W., Castonguay, L. (Eds.The Bergin and Garfield handbook of psychotherapy and behavior change (7th ed.pp. 673–703. New York: John Wiley & Sons. [Google Scholar]
5. Norcross, J. C., Cooper, M. (2021). Personalizing psychotherapy: Assessing and accommodating patient preferences. Washington DC: American Psychological Association. [Google Scholar]
6. Zilcha-Mano, S. (2019). Major developments in methods addressing for whom psychotherapy may work and why. Psychotherapy Research, 29(6), 693–708. DOI 10.1080/10503307.2018.1429691. [Google Scholar] [CrossRef]
7. Bedi, R. P. (2018). Racial, ethnic, cultural, and national disparities in counseling and psychotherapy outcome are inevitable but eliminating global mental health disparities with indigenous healing is not. Archives of Scientific Psychology, 6(1), 96–104. DOI 10.1037/arc0000047. [Google Scholar] [CrossRef]
8. Cohen, Z. D., DeRubeis, R. J. (2018). Treatment selection in depression. Annual Review of Clinical Psychology, 14(1), 209–236. DOI 10.1146/annurev-clinpsy-050817-084746. [Google Scholar] [CrossRef]
9. Cuijpers, P., Noma, H., Karyotaki, E., Vinkers, C. H., Cipriani, A. et al. (2020). A network meta-analysis of the effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression. World Psychiatry, 19(1), 92–107. DOI 10.1002/wps.20701. [Google Scholar] [CrossRef]
10. Heim, E., Mewes, R., Abi Ramia, J., Glaesmer, H., Hall, B. et al. (2021). Reporting cultural adaptation in psychological trials–The RECAPT criteria. Clinical Psychology in Europe, 3, 1–25. DOI 10.32872/cpe.6351. [Google Scholar] [CrossRef]
11. Kessler, R. C., Kazdin, A. E., Aguilar-Gaxiola, S., Al-Hamzawi, A., Alonso, J. et al. (2022). Patterns and correlates of patient-reported helpfulness of treatment for common mental and substance use disorders in the WHO World Mental Health surveys. World Psychiatry, 21(2), 272–286. [Google Scholar]
12. Barber, J. P., Solomonov, N. (2019). Toward a personalized approach to psychotherapy outcome and the study of therapeutic change. World Psychiatry, 18(3), 291–292. DOI 10.1002/wps.20666. [Google Scholar] [CrossRef]
13. Huibers, M. J., Lorenzo-Luaces, L., Cuijpers, P., Kazantzis, N. (2021). On the road to personalized psychotherapy: A research agenda based on cognitive behavior therapy for depression. Frontiers in Psychiatry, 11, 1551. DOI 10.3389/fpsyt.2020.607508. [Google Scholar] [CrossRef]
14. Bokhove, C., Muijs, D., Downey, C. (2022). The influence of school climate and achievement on bullying: Comparative evidence from international large-scale assessment data. Educational Research, 64(1). DOI 10.1080/00131881.2021.1992294. [Google Scholar] [CrossRef]
15. Hübel, C., Abdulkadir, M., Herle, M., Loos, R. J., Breen, G. et al. (2021). One size does not fit all. Genomics differentiates among anorexia nervosa, bulimia nervosa, and binge-eating disorder. International Journal of Eating Disorders, 54(5), 785–793. DOI 10.1002/eat.23481. [Google Scholar] [CrossRef]
16. Kohler, S. (2018). Precision medicine-moving away from one-size-fits-all. Quest, 14(3), 12–15. [Google Scholar]
17. Mian, A., MacGregor, A. (2017). Will the real Mr. Average please stand up? (part 1). N1-Headache. [Google Scholar]
18. Schee genannt Halfmann, S., Evangelatos, N., Schröder-Bäck, P., Brand, A. (2017). European healthcare systems readiness to shift from ‘one-size fits all’ to personalized medicine. Personalized Medicine, 14(1), 63–74. DOI 10.2217/pme-2016-0061. [Google Scholar] [CrossRef]
19. Kohn, R., Saxena, S., Levav, I., Saraceno, B. (2004). The treatment gap in mental health care. Bulletin of the World Health Organization, 82(11), 858–866. [Google Scholar]
20. Patel, V., Weiss, H. A., Chowdhary, N., Naik, S., Pednekar, S. et al. (2010). Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANASA cluster randomised controlled trial. Lancet, 376(9758), 2086–2095. DOI 10.1016/S0140-6736(10)61508-5. [Google Scholar] [CrossRef]
21. Andrade, L. H., Alonso, J., Mneimneh, Z., Wells, J. E., Al-Hamzawi, A. et al. (2014). Barriers to mental health treatment: Results from the WHO World Mental Health surveys. Psychological Medicine, 44(6), 1303–1317. DOI 10.1017/S0033291713001943. [Google Scholar] [CrossRef]
22. Becker, A. E., Kleinman, A. (2013). Mental health and the global agenda. New England Journal of Medicine, 369(1), 66–73. DOI 10.1056/NEJMra1110827. [Google Scholar] [CrossRef]
23. Merikangas, K. R., He, J. P., Burstein, M., Swendsen, J., Avenevoli, S. et al. (2011). Service utilization for lifetime mental disorders in US adolescents: Results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 50(1), 32–45. DOI 10.1016/j.jaac.2010.10.006. [Google Scholar] [CrossRef]
24. Steel, Z., Marnane, C., Iranpour, C., Chey, T., Jackson, J. W. et al. (2014). The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. International Journal of Epidemiology, 43(2), 476–493. DOI 10.1093/ije/dyu038. [Google Scholar] [CrossRef]
25. Whiteford, H. A., Degenhardt, L., Rehm, J., Baxter, A. J., Ferrari, A. J. et al. (2013). Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet, 382(9904), 1575–1586. DOI 10.1016/S0140-6736(13)61611-6. [Google Scholar] [CrossRef]
26. Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Chatterji, S., Lee, S. et al. (2009). The global burden of mental disorders: An update from the WHO World Mental Health (WMH) surveys. Epidemiology and Psychiatric Sciences, 18(1), 23–33. DOI 10.1017/S1121189X00001421. [Google Scholar] [CrossRef]
27. Wittchen, H. U., Mühlig, S., Beesdo, K. (2003). Mental disorders in primary care. Dialogues in Clinical Neuroscience, 5(2), 115–128. DOI 10.31887/DCNS.2003.5.2/huwittchen. [Google Scholar] [CrossRef]
28. Kessler, R. C., Chiu, W. T., Demler, O., Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627. DOI 10.1001/archpsyc.62.6.617. [Google Scholar] [CrossRef]
29. Kessler, R. C., McGonagle, K. A., Zhao, S., Nelson, C. B., Hughes, M. et al. (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Archives of General Psychiatry, 51(1), 8–9. DOI 10.1001/archpsyc.1994.03950010008002. [Google Scholar] [CrossRef]
30. Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R. et al. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. DOI 10.1001/archpsyc.62.6.593. [Google Scholar] [CrossRef]
31. Lebrun-Harris, L. A., Ghandour, R. M., Kogan, M. D., Warren, M. D. (2022). Five-year trends in US children’s health and well-being, 2016–2020. Journal of Pediatrics, 80(3), 433. DOI 10.1001/jamapediatrics.2022.0056. [Google Scholar] [CrossRef]
32. Martins, S. S., Sarvet, A., Santaella-Tenorio, J., Saha, T., Grant, B. F. et al. (2017). Changes in US lifetime heroin use and heroin use disorder: Prevalence from the 2001–2002 to 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry, 74(5), 445–455. DOI 10.1001/jamapsychiatry.2017.0113. [Google Scholar] [CrossRef]
33. Twenge, J. M., Joiner, T. E., Rogers, M. L., Martin, G. N. (2018). Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clinical Psychological Science, 6(1), 3–17. DOI 10.1177/2167702617723376. [Google Scholar] [CrossRef]
34. World Mental Health Survey Consortium (2004). Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA, 291(21), 2581–2590. DOI 10.1001/jama.291.21.2581. [Google Scholar] [CrossRef]
35. Thornicroft, G., Chatterji, S., Evans-Lacko, S., Gruber, M., Sampson, N. et al. (2017). Undertreatment of people with major depressive disorder in 21 countries. British Journal of Psychiatry, 210(2), 119–124. DOI 10.1192/bjp.bp.116.188078. [Google Scholar] [CrossRef]
36. Kessler, R. C., Demler, O., Frank, R. G., Olfson, M., Pincus, H. A. et al. (2005). Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine, 352(24), 2515–2523. DOI 10.1056/NEJMsa043266. [Google Scholar] [CrossRef]
37. Alegría, M., Chatterji, P., Wells, K., Cao, Z., Chen, C. N. et al. (2008). Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services, 59(11), 1264–1272. DOI 10.1176/ps.2008.59.11.1264. [Google Scholar] [CrossRef]
38. Alegría, M., Vallas, M., Pumariega, A. J. (2010). Racial and ethnic disparities in pediatric mental health. Child and Adolescent Psychiatric Clinics of North America, 19(4), 759–774. DOI 10.1016/j.chc.2010.07.001. [Google Scholar] [CrossRef]
39. McGuire, T. G., Miranda, J. (2008). New evidence regarding racial and ethnic disparities in mental health: Policy implications. Health Affairs, 27(2), 393–403. DOI 10.1377/hlthaff.27.2.393. [Google Scholar] [CrossRef]
40. Wells, K., Klap, R., Koike, A., Sherbourne, C. (2001). Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. American Journal of Psychiatry, 158(12), 2027–2032. DOI 10.1176/appi.ajp.158.12.2027. [Google Scholar] [CrossRef]
41. Wang, P. S., Lane, M., Olfson, M., Pincus, H. A., Wells, K. B. et al. (2005). Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 629–640. DOI 10.1001/archpsyc.62.6.629. [Google Scholar] [CrossRef]
42. Institute of Medicine (2001). Crossing the quality chasm: A new health system for the 21st century. Washington DC: National Academies Press. [Google Scholar]
43. Institute of Medicine (2006). Improving the quality of care for mental and substance use conditions. Washington DC: National Academies Press. [Google Scholar]
44. National Academies of Sciences, Engineering, and Medicine (2018). Crossing the global quality chasm: Improving health care worldwide. Washington DC: National Academies Press. [Google Scholar]
45. Sarhangi, N., Nikfar, S., Hasanzad, M., Larijani, B. (2021). Precision medicine path at personalized medicine research center/endocrinology and metabolism research institute: A systematic review. Journal of Diabetes & Metabolic Disorders. DOI 10.1007/s40200-020-00708-9. [Google Scholar] [CrossRef]
46. Zhang, S., Bamakan, S. M. H., Qu, Q., Li, S. (2018). Learning for personalized medicine: A comprehensive review from a deep learning perspective. IEEE Reviews in Biomedical Engineering, 12, 194–208. DOI 10.1109/RBME.2018.2864254. [Google Scholar] [CrossRef]
47. National Research Council (2011Toward precision medicine: Building a knowledge network for biomedical research and a new taxonomy of disease. Washington DC: National Academies Press. [Google Scholar]
48. Zhang, X. D. (2015). Precision medicine, personalized medicine, omics and big data: Concepts and relationships. Journal of Pharmacogenomics and Pharmacoproteomics, 6(2), e14. DOI 10.4172/2153-0645.1000e144. [Google Scholar] [CrossRef]
49. Koenig, I. R., Fuchs, O., Hansen, G., von Mutius, E., Kopp, M. V. (2017). What is precision medicine? European Respiratory Journal, 50(4), 1700391. DOI 10.1183/13993003.00391-2017. [Google Scholar] [CrossRef]
50. Hampton, M., Lenhart, O. (2022). Access to health care and mental health—Evidence from the ACA preexisting conditions provision. Health Economics, 31, 760–783. DOI 10.1002/hec.4473. [Google Scholar] [CrossRef]
51. Walker, E. R., Cummings, J. R., Hockenberry, J. M., Druss, B. G. (2015). Insurance status, use of mental health services, and unmet need for mental health care in the United States. Psychiatric Services, 66(6), 578–584. DOI 10.1176/appi.ps.201400248. [Google Scholar] [CrossRef]
52. Clark, D. M. (2012). The English improving access to psychological therapies (IAPT) program. In: McHugh, Barlow, D. H. (Eds.Dissemination and implementation of evidence-based psychological interventions, pp. 61–77. New York: Oxford University Press. [Google Scholar]
53. Clark, D. M. (2018). Realizing the mass public benefit of evidence-based psychological therapies: The IAPT program. Annual Review of Clinical Psychology, 14(1), 159–183. DOI 10.1146/annurev-clinpsy-050817-084833. [Google Scholar] [CrossRef]
54. Carter, S. L. (2007). Review of recent treatment acceptability research. Education and Training in Developmental Disabilities, 42(3), 301–316. [Google Scholar]
55. Kaltenthaler, E., Sutcliffe, P., Parry, G., Beverley, C., Rees, A. et al. (2008). The acceptability to patients of computerized cognitive behaviour therapy for depression: A systematic review. Psychological Medicine, 38(11), 1521–1530. DOI 10.1017/S0033291707002607. [Google Scholar] [CrossRef]
56. Vazquez, M., Fryling, M. J., Hernández, A. (2019). Assessment of parental acceptability and preference for behavioral interventions for feeding problems. Behavior Modification, 43(2), 273–287. DOI 10.1177/0145445517751435. [Google Scholar] [CrossRef]
57. Wierenga, C. E., Hill, L., Knatz Peck, S., McCray, J., Greathouse, L. et al. (2018). The acceptability, feasibility, and possible benefits of a neurobiologically-informed 5-day multifamily treatment for adults with anorexia nervosa. International Journal of Eating Disorders, 51(8), 863–869. DOI 10.1002/eat.22876. [Google Scholar] [CrossRef]
58. Boothe, J., Borrego, J.Jr., Hill, C., Anhalt, K. (2005). Treatment acceptability and treatment compliance in ethnic minority populations. In: Frisby, C. L., Reynolds, C. R. (Eds.Comprehensive handbook of multicultural school psychology, pp. 945–972. Hoboken, NJ: John Wiley & Sons. [Google Scholar]
59. Miranda, J., Bernal, G., Lau, A. S., Kohn, L., Hwang, W. C. et al. (2005). State of the science on psychosocial interventions for ethnic minorities. Annual Review of Clinical Psychology, 1(1), 113–142. DOI 10.1146/annurev.clinpsy.1.102803.143822. [Google Scholar] [CrossRef]
60. National Institute of Health (2022). ClinicalTrials.Gov. The safety of administering a second dose of a COVID-19 mRNA vaccine in individuals who experienced a systemic allergic reaction to an initial dose.https://www.clinicaltrials.gov/ct2/show/NCT04977479. [Google Scholar]
61. Blass, E., Ott, P. A. (2021). Advances in the development of personalized neoantigen-based therapeutic cancer vaccines. Nature Reviews Clinical Oncology, 18(4), 215–229. DOI 10.1038/s41571-020-00460-2. [Google Scholar] [CrossRef]
62. Zhou, J., Kroll, A. V., Holay, M., Fang, R. H., Zhang, L. (2020). Biomimetic nanotechnology toward personalized vaccines. Advanced Materials, 32(13), 1901255. DOI 10.1002/adma.201901255. [Google Scholar] [CrossRef]
63. ten Have, M., de Graaf, R., Ormel, J., Vilagut, G., Kovess, V. et al. (2010). Are attitudes towards mental health help-seeking associated with service use? Results from the European Study of Epidemiology of Mental Disorders. Social Psychiatry and Psychiatric Epidemiology, 45(2), 153–163. DOI 10.1007/s00127-009-0050-4. [Google Scholar] [CrossRef]
64. Orozco, R., Vigo, D., Benjet, C., Borges, G., Aguilar-Gaxiola, S. et al. (2022). Barriers to treatment for mental disorders in six countries of the Americas: A regional report from the World Mental Health surveys. Journal of Affective Disorders, 303(Suppl 3), 273–285. DOI 10.1016/j.jad.2022.02.031. [Google Scholar] [CrossRef]
65. Leijdesdorff, S., Klaassen, R., Wairata, D. J., Rosema, S., van Amelsvoort, T. et al. (2021). Barriers and facilitators on the pathway to mental health care among 12–25 year olds. International Journal of Qualitative Studies on Health and Well-Being, 16(1), 1963110. DOI 10.1080/17482631.2021.1963110. [Google Scholar] [CrossRef]
66. Sarikhani, Y., Bastani, P., Rafiee, M., Kavosi, Z., Ravangard, R. (2021). Key barriers to the provision and utilization of mental health services in low-and middle-income countries: A scope study. Community Mental Health Journal, 57(5), 836–852. DOI 10.1007/s10597-020-00619-2. [Google Scholar] [CrossRef]
67. Becker, K. D., Boustani, M., Gellatly, R., Chorpita, B. F. (2018). Forty years of engagement research in children’s mental health services: Multidimensional measurement and practice elements. Journal of Clinical Child & Adolescent Psychology, 47(1), 1–23. DOI 10.1080/15374416.2017.1326121. [Google Scholar] [CrossRef]
68. Gmeinwieser, S., Schneider, K. S., Bardo, M., Brockmeyer, T., Hagmayer, Y. (2020). Risk for psychotherapy drop-out in survival analysis: The influence of general change mechanisms and symptom severity. Journal of Counseling Psychology, 67(6), 712–722. DOI 10.1037/cou0000418. [Google Scholar] [CrossRef]
69. Krendl, A. C., Lorenzo-Luaces, L. (2021). Identifying peaks in attrition after clients initiate mental health treatment in a university training clinic. Psychological Services. https://doi.org/10.1037/ser0000469 [Google Scholar]
70. Roseborough, D. J., McLeod, J. T., Wright, F. I. (2016). Attrition in psychotherapy: A survival analysis. Research on Social Work Practice, 26(7), 803–815. DOI 10.1177/1049731515569073. [Google Scholar] [CrossRef]
71. Constantino, M. J., Castonguay, L. G., Zack, S. E., DeGeorge, J. (2010). Engagement in psychotherapy: Factors contributing to the facilitation, demise, and restoration of the therapeutic alliance. In: Castro-Blanco, D., Karver, M. S. (Eds.Elusive alliance: Treatment engagement strategies with high-risk adolescents, pp. 21–57. Washington DC: American Psychological Association. [Google Scholar]
72. Gonzalez, C., Morawska, A., Haslam, D. M. (2018). Enhancing initial parental engagement in interventions for parents of young children: A systematic review of experimental studies. Clinical Child and Family Psychology Review, 21(3), 415–432. DOI 10.1007/s10567-018-0259-4. [Google Scholar] [CrossRef]
73. Kealy, D., Seidler, Z. E., Rice, S. M., Oliffe, J. L., Ogrodniczuk, J. S. et al. (2021). Challenging assumptions about what men want: Examining preferences for psychotherapy among men attending outpatient mental health clinics. Professional Psychology: Research and Practice, 52(1), 28–33. DOI 10.1037/pro0000321. [Google Scholar] [CrossRef]
74. Mitchell, A. J., Selmes, T. (2007). Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Advances in Psychiatric Treatment, 13(6), 423–434. DOI 10.1192/apt.bp.106.003202. [Google Scholar] [CrossRef]
75. Seidler, Z. E., Rice, S. M., Oliffe, J. L., Fogarty, A. S., Dhillon, H. M. (2018). Men in and out of treatment for depression: Strategies for improved engagement. Australian Psychologist, 53(5), 405–415. DOI 10.1111/ap.12331. [Google Scholar] [CrossRef]
76. Crowley, R. A., Kirschner, N. (2015). The integration of care for mental health, substance abuse, and other behavioral health conditions into primary care: Executive summary of an American College of Physicians position paper. Annals of Internal Medicine, 163(4), 298–299. DOI 10.7326/M15-0510. [Google Scholar] [CrossRef]
77. Kazak, A. E., Nash, J. M., Hiroto, K., Kaslow, N. J. (2017). Psychologists in patient-centered medical homes (PCMHsRoles, evidence, opportunities, and challenges. American Psychologist, 72(1), 1–12. DOI 10.1037/a0040382. [Google Scholar] [CrossRef]
78. Ormel, J., Hollon, S. D., Kessler, R. C., Cuijpers, P., Monroe, S. M. (2022). More treatment but no less depression: The treatment-prevalence paradox. Clinical Psychology Review, 91(7), 102111. DOI 10.1016/j.cpr.2021.102111. [Google Scholar] [CrossRef]
79. Kazdin, A. E. (2018). Innovations in psychosocial interventions and their delivery: Leveraging cutting-edge science to improve the world’s mental health. New York: Oxford University Press. [Google Scholar]
80. Lattie, E. G., Stiles-Shields, C., Graham, A. K. (2022). An overview of and recommendations for more accessible digital mental health services. Nature Reviews Psychology, 1(2), 1–14. DOI 10.1038/s44159-021-00003-1. [Google Scholar] [CrossRef]
81. Tal, A., Torous, J. (2017). The digital mental health revolution: Opportunities and risks. Psychiatric Rehabilitation Journal, 40(3), 263–265. DOI 10.1037/prj0000285. [Google Scholar] [CrossRef]
82. Bashshur, R., Shannon, G. W. (2009). History of telemedicine: Evolution, context, and transformation. New Rochelle, NY: Mary Ann Liebert. [Google Scholar]
83. Shirzadfar, H., Lotfi, F. (2017). The evolution and transformation of telemedicine. International Journal of Biosensors & Bioelectronics, 3(4), 303–306. DOI 10.15406/ijbsbe.2017.03.00070. [Google Scholar] [CrossRef]
84. Chen, M., Ma, Y., Song, J., Lai, C. F., Hu, B. (2016). Smart clothing: Connecting human with clouds and big data for sustainable health monitoring. Mobile Networks and Applications, 21(5), 825–845. DOI 10.1007/s11036-016-0745-1. [Google Scholar] [CrossRef]
85. Sentio Solutions (2018). Feel. San Francisco: CA. https://www.myfeel.co/how-it-worksInc. [Google Scholar]
86. Spijkerman, M. P. J., Pots, W. T. M., Bohlmeijer, E. T. (2016). Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clinical Psychology Review, 45, 102–114. DOI 10.1016/j.cpr.2016.03.009. [Google Scholar] [CrossRef]
87. Amanvermez, Y., Zhao, R., Cuijpers, P., de Wit, L. M., Ebert, D. D. et al. (2022). Effects of self-guided stress management interventions in college students: A systematic review and meta-analysis. Internet Interventions, 28, 100503. DOI 10.1016/j.invent.2022.100503. [Google Scholar] [CrossRef]
88. Ma, L., Huang, C., Tao, R., Cui, Z., Schluter, P. (2021). Meta-analytic review of online guided self-help interventions for depressive symptoms among college students. Internet Interventions, 25(2), 100427. DOI 10.1016/j.invent.2021.100427. [Google Scholar] [CrossRef]
89. Taylor, H., Strauss, C., Cavanagh, K. (2021). Can a little bit of mindfulness do you good? A systematic review and meta-analyses of unguided mindfulness-based self-help interventions. Clinical Psychology Review, 89(2), 102078. DOI 10.1016/j.cpr.2021.102078. [Google Scholar] [CrossRef]
90. Li, J., Brar, A. (2022). The use and impact of digital technologies for and on the mental health and wellbeing of Indigenous people: A systematic review of empirical studies. Computers in Human Behavior, 126(2), 106988. DOI 10.1016/j.chb.2021.106988. [Google Scholar] [CrossRef]
91. Schueller, S. M., Hunter, J. F., Figueroa, C., Aguilera, A. (2019). Use of digital mental health for marginalized and underserved populations. Current Treatment Options in Psychiatry, 6(3), 243–255. DOI 10.1007/s40501-019-00181-z. [Google Scholar] [CrossRef]
92. Teachman, B. A., Silverman, A. L., Werntz, A. (2022). Digital mental health services: Moving from promise to results. Cognitive and Behavioral Practice, 29(1), 97–104. DOI 10.1016/j.cbpra.2021.06.014. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |