
 | Congenital Heart Disease | 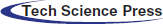 |
DOI: 10.32604/CHD.2020.011338
ARTICLE
Successful Percutaneous Closure of Atrial Septal Defect via Transjugular Approach with the Cocoon Septal Occluder
1First Department of Cardiology, Athens University, Hippokration Hospital, Athens, Greece
2Department of Pediatric Cardiology, “Agios” Lukas Clinic, Thessaloniki, Greece
*Corresponding Author: Konstantinos Toutouzas. Email: ktoutouz@gmail.com
Received: 03 May 2020; Accepted: 28 June 2020
Abstract: The percutaneous closure of ostium secundum atrial septal defects (ASD) is a well-established procedure. Currently available devices and delivery systems are designed to be used via the femoral venous route. However, an alternative approach needs to be considered in cases of congenital or acquired caval obstruction. We describe a successful transjugular closure of a moderate sized secundum ASD with the Cocoon Septal Occluder in a 37-year-old symptomatic woman with inferior vena cava (IVC) thrombosis, using a novel deployment technique to overcome difficulties, namely maintaining stable sheath position in the left atrium. Percutaneous closure of secundum ASDs via the transjugular approach is safe, feasible and effective and can be a reasonable alternative to surgical closure in patients with failed femoral venous access and not anatomically complex atrial septal defects.
Keywords: Atrial septal defect; closure devices; interventional cardiology
The percutaneous closure of ostium secundum atrial septal defects (ASD) is a well-established procedure being performed with increasing success since the initial cases were reported in 1974. Currently available devices and delivery systems are designed to be used via the femoral venous route [1]. However, an alternative approach needs to be considered in cases of congenital or acquired caval obstruction [2–6]. Transhepatic and transjugular approaches have shown to be reasonable alternatives in patients in whom femoral venous approach is not feasible.
We describe a successful transjugular closure of a moderate sized secundum ASD in a 37-year-old symptomatic woman with inferior vena cava (IVC) thrombosis, using a novel deployment technique to overcome difficulties, namely maintaining stable sheath position in the left atrium (LA).
A 37-year old woman with a history of cervical rib surgical resection due to thoracic outlet syndrome (total occlusion of the left subclavian artery and significant stenosis of both left and right subclavian veins) presented with dyspnea on exertion (NYHA II functional class) and intermittent palpitations of 4-month duration. Ten years prior to presentation, the patient had spontaneous deep vein thrombosis extending from the veins of the left lower leg up to the left common femoral vein, the etiology of which was not elucidated despite extensive imaging and laboratory investigation including thrombophilia testing. For this reason, the patient was on oral anticoagulation therapy. At the time of admission, the ECG of the patient showed sinus rhythm with right bundle branch block. Transthoracic echocardiography (TTE) showed evidence of right ventricular volume overload (dilation of right heart chambers) with no signs of pulmonary arterial hypertension, presence of a large left to right shunt at the level of the interatrial septum and normal biventricular function. The pulmonary to systemic flow ratio (QP/QS) was 2.2. Transesophageal echocardiography (TEE) confirmed the presence of a moderate sized (14 × 11 mm) isolated ostium secundum ASD with adequate rims for percutaneous closure (Fig. 1).
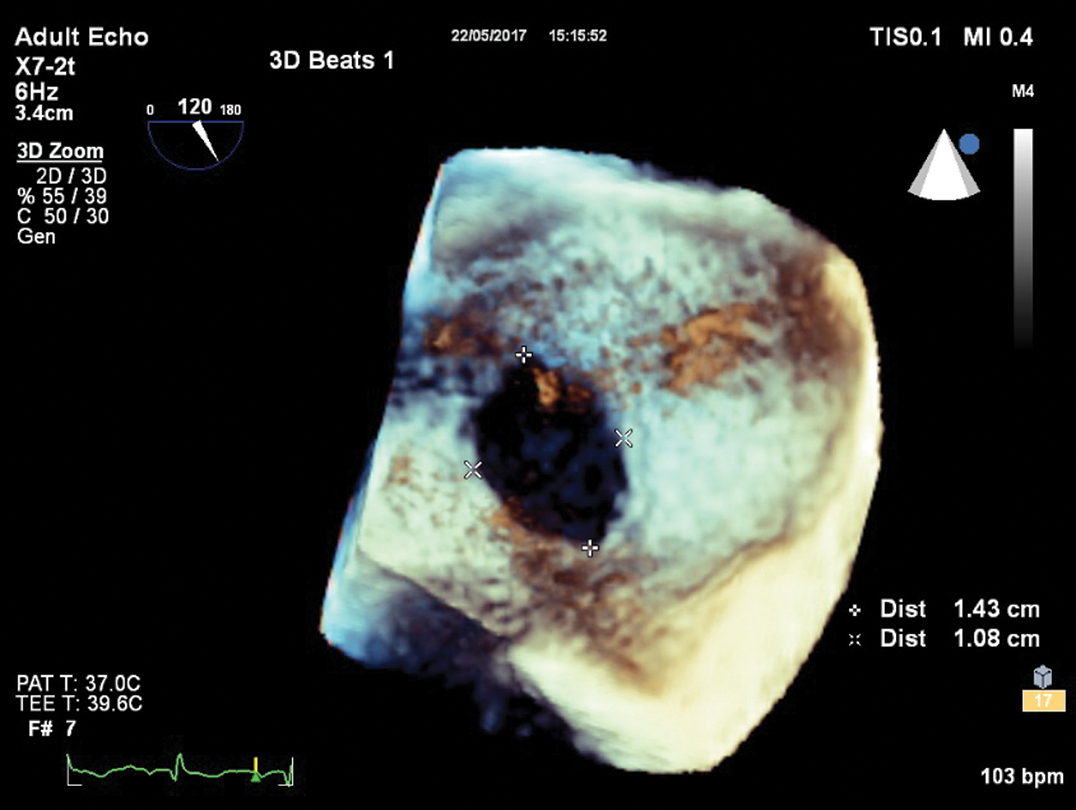
Figure 1: Mid-esophageal view of atrial septum with three-dimensional transesophageal echocardiography showing a moderate sized ostium secundum defect (15 mm × 11 mm)
Due to the past medical history of deep venous thrombosis, the patient underwent color doppler ultrasound imaging of lower extremities. On the left side, there were signs of past deep venous thrombosis with full recanalization and remnant microthrombi extending up to the left common femoral vein as well as post-thrombotic venous insufficiency. On the right side, the right femoral venous route was patent.
After interruption of oral anticoagulation therapy, bridging with low molecular weight and premedication with loading doses of aspirin (300 mg) and clopidogrel (300 mg), cardiac catheterization was performed under general anesthesia and TEE guidance. Although right femoral venous access was obtained, repeated attempts to advance the delivery sheath over the wire beyond a certain point in the IVC were unsuccessful. Manual contrast injection was performed in the femoral vein, and an obstruction of the IVC was observed and identified as thrombus. At that point, the procedure was abandoned, and the patient underwent scheduled computed tomography (CT) angiography of the abdomen and pelvis which revealed partial thrombosis of the infrarenal part of the IVC and the presence of extensive venous collaterals. With a view to proceed to ASD closure from alternative routes, the patient underwent CT angiography of neck and thorax that showed patent arterial and venous routes with no signs of obstruction.
The Heart Team decided to proceed to ASD closure via the right internal jugular vein (IJV) approach. The procedure was performed under general anesthesia and continuous TEE monitoring. After insertion of a femoral artery line for hemodynamic monitoring, a 100-U/kg bolus of heparin was administered. A 6F right IJV sheath access was introduced and a 6 Fr Cobra catheter (Cook Medical) was easily negotiated through the defect, although stable sheath position in the LA could not be maintained. Following, a 9Fr steerable sheath (Fustar Steerable Introducer sheath, Lifetech Scientific, Shenzen) was engaged to advance a 6Fr multipurpose catheter into the LA over a 0.035” 145 cm J-tip guidewire (Bard Medical). However, since a 0.035” stainless steel wire was not supporting sheath passage into the LA, a 0.035” 260 cm Amplatz super-stiff guidewire (Cook Corporation) was exchanged and introduced via the multipurpose catheter. The wire was not maintaining a stable position in any of the pulmonary veins (Fig. 2).
Figure 2: Fluoroscopy (left panel) and transesophageal echocardiography (right panel) images showing the wire in the left atrium through the atrial septal defect, unable to maintain a stable position in the pulmonary veins
Hence, with the wire pointing toward the LV inflow, the mitral valve was successfully crossed under fluoroscopy and TEE guidance and the multipurpose catheter along with the steerable sheath were advanced in the LV (Fig. 3).
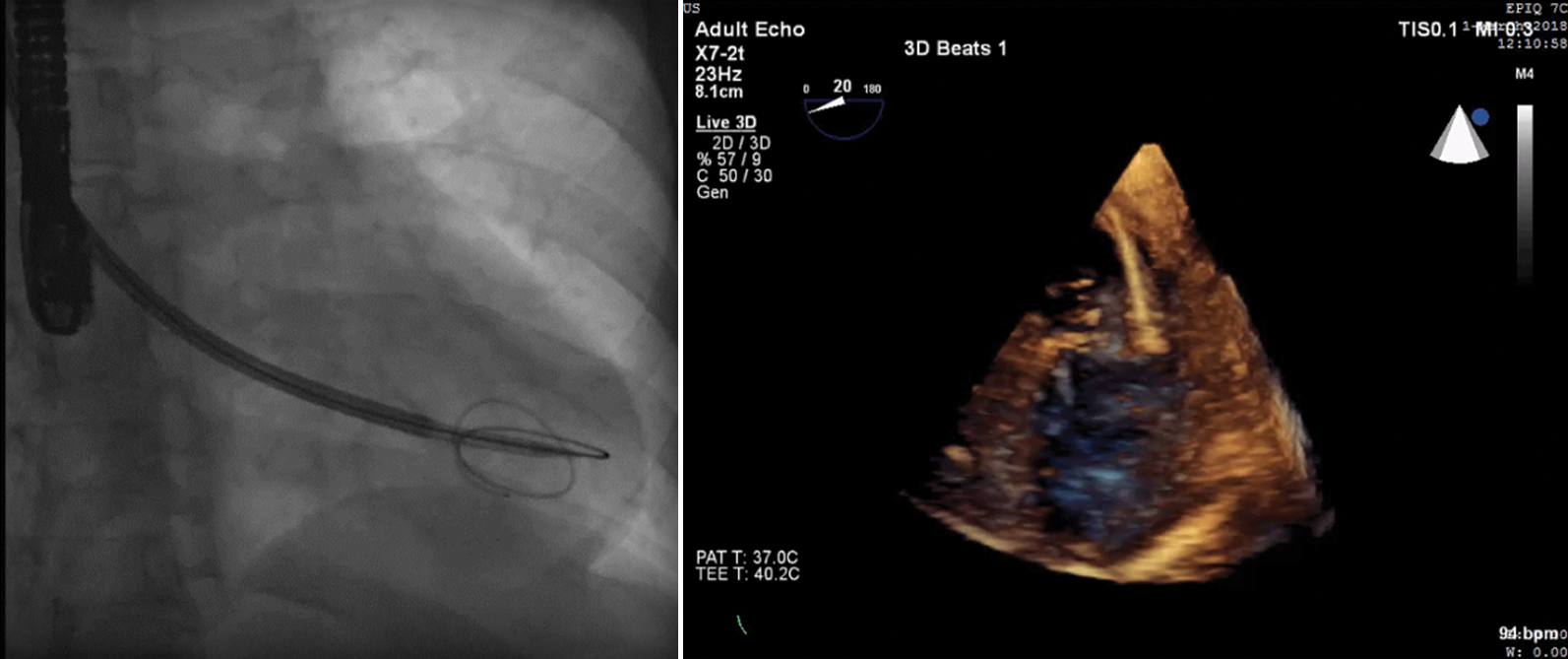
Figure 3: Fluoroscopy (left panel) and transesophageal echocardiography (right panel) images showing the 6 Fr multipurpose catheter and the Fustar Steerable Introducer sheath (Lifetech Scientific, Shenzen) advanced in the left ventricle
Then, the 6 Fr multipurpose catheter and the Lifetech sheath were removed and over the wire the Cocoon delivery sheath along with its dilator was introduced. The dilator-wire assembly was then removed from the delivery sheath, while maintaining the sheath in the high-pressure LV in order to ensure a good back-bleed and minimize the risk of air embolism. Based on TEE measurements, a 20 mm self-centering, double disk Cocoon Septal Occluder (CSO) (Vascular Innovations Co., Northaburi, Thailand) was chosen and passed through the delivery sheath [7]. The whole assembly remained in the LV for a short time (<30 seconds overall) and then was gently withdrawn toward the LV inflow. Under TEE guidance, the LA disc was released by unsheathing it in the LA just above the mitral annulus, pointing toward the LV inflow, ensuring that there was no impingement of the mitral valve apparatus (Fig. 4).
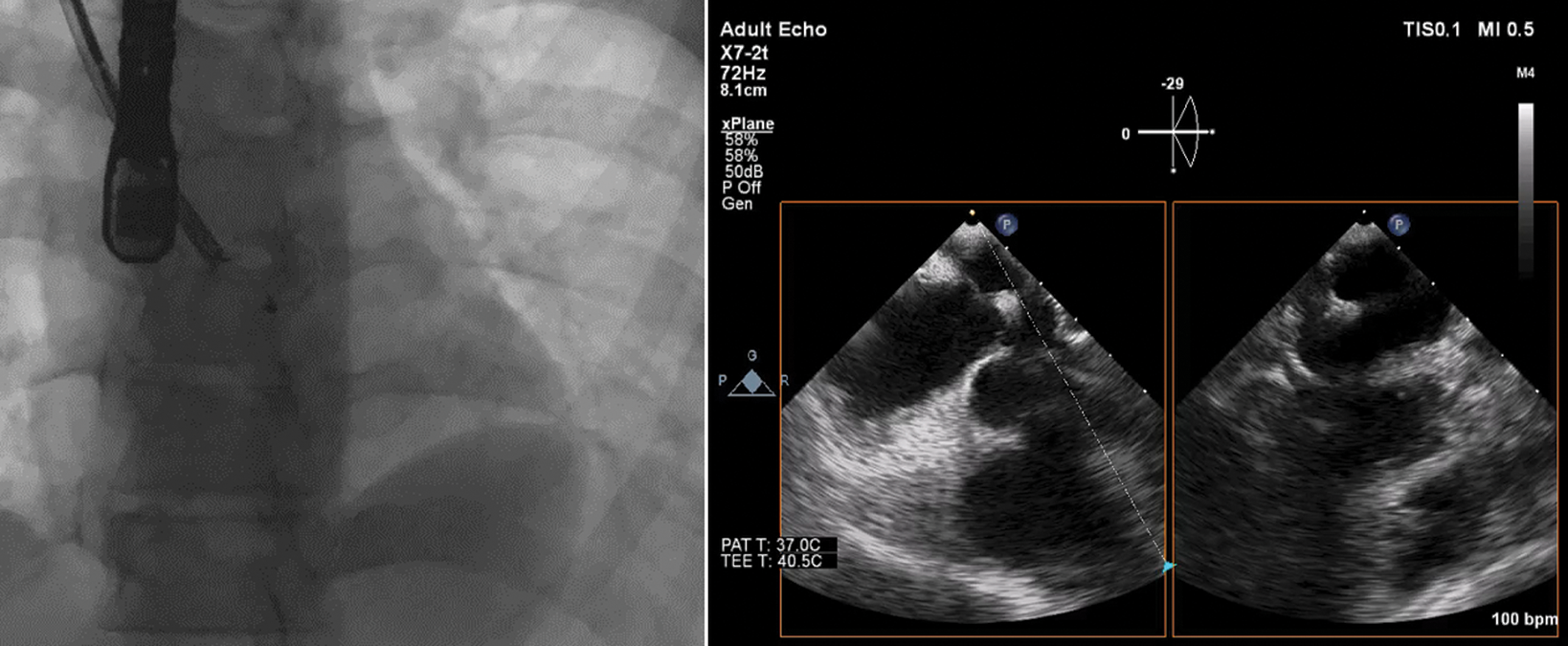
Figure 4: Fluoroscopy (left panel) and transesophageal echocardiography (right panel) images showing the withdrawal of the whole assembly (delivery sheath-device) toward the left ventricular inflow and then the release of the left atrial disc just above the mitral annulus ensuring that there was no impingement on the mitral valve apparatus
After gently withdrawing the LA disc towards the left side of the interatrial septum, the RA disc was released on the RA side. Proper alignment of the device with captured rims and no residual flow was confirmed on TEE before releasing of the device (Fig. 5). The procedure was completed without any complications with a slightly longer procedural (50 min) and fluoroscopy time (7.5 min).
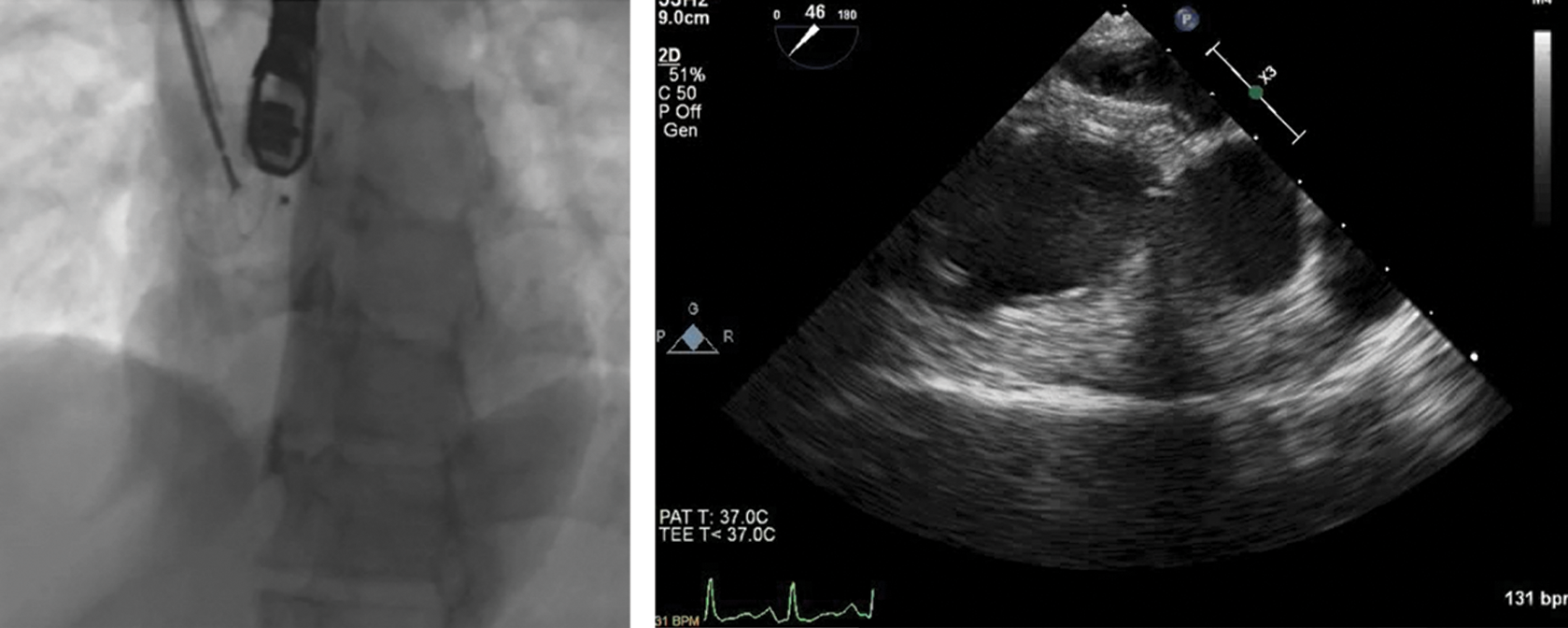
Figure 5: Fluoroscopy (left panel) and transesophageal echocardiography (right panel) images showing in situ and well-seated occluder device
The patient was discharged the following day on dual antiplatelet therapy for 6 months. At 1 year follow up, the patient remains asymptomatic, in sinus rhythm and the device is in situ and well seated with no residual shunt or valvular regurgitation on follow up TEE.
Percutaneous device closure of isolated ostium secundum ASD has evolved to become the standard of care in both pediatric and adult populations. There is a wide range of devices and delivery systems designed to be used for femoral venous access that has facilitated percutaneous closure for simple and complex ASDs. However, cases may arise where femoral venous access is not feasible as in patients with heterotaxy and interrupted IVC or IVC thrombosis.
Alternative routes for percutaneous ASD closure have been proposed [2–6]. It seems that transhepatic approach can potentially lead to a higher incidence of complications including retro- or intra- peritoneal bleeding, hemobilia, perforation of the gall bladder, pleural effusions and liver abscess or peritonitis, whereas transjugular approach is a potentially safer alternative.
Regarding the technique of ASD closure via the transjugular approach, retaining a stable wire position in the LA for sheath delivery appears to be of paramount importance for the successful closure of the defect. Previous case reports of closure through this route also mention the difficulty in maintaining a pulmonary venous wire position and the feasibility of deploying the device from a sheath pointed toward the LV inflow or LA roof [4]. Planning the procedure after as a second attempt allowed us to overcome this limitation by placing a steerable sheath in the LV. However, emphasis needs to be made on carefully unsheathing the device in the LA, after gently withdrawing the delivery sheath just above the mitral valve under fluoroscopy and TEE guidance in order to prevent any valvular dysfunction. Therefore, TEE plays a crucial role in not only assessing the size of the defect but also in tracking the wire and sheath in the LA.
In conclusion, percutaneous closure of secundum ASDs via the transjugular approach using novel deployment techniques with some modification is safe, feasible and effective and can be a reasonable alternative to surgical closure in patients with failed femoral venous access and not anatomically complex atrial septal defects.
Funding Statement: The author(s) received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Stout, K. K., Daniels, C. J., Aboulhosn, J. A., Bozkurt, B., Broberg, C. S. et al. (2019). 2018 AHA/ACC guideline for the management of adults with congenital heart disease a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation, 139(14), 637–697. DOI 10.1161/CIR.0000000000000603. [Google Scholar] [CrossRef]
2. Seshagiri, R. D., Patnaik, A. N., Srinivas, B. (2013). Percutaneous closure of atrial septal defect via transjugular approach with Blockaid device in a patient with interrupted inferior vena cava. Cardiovascular Intervention and Therapeutics, 28(1), 63–65. DOI 10.1007/s12928-012-0113-4. [Google Scholar] [CrossRef]
3. Dong, H. J., Fan, T. B., Li, B., Liang, W. J., Song, S. B. et al. (2017). Transjugular closure of secundum atrial septal defects. Journal of Cardiac Surgery, 32(2), 151–153. DOI 10.1111/jocs.12930. [Google Scholar] [CrossRef]
4. Kashour, T. S., Latroche, B., Elhoury, M. E., Galal, M. O. (2010). Successful percutaneous closure of a secundum atrial septal defect through femoral approach in a patient with interrupted inferior vena cava. Congenital Heart Disease, 5(6), 620–623. DOI 10.1111/j.1747-0803.2010.00391.x. [Google Scholar] [CrossRef]
5. Truong, Q. B., Dao, A. Q., Do, N. T., Le, M. K. (2018). Percutaneous atrial septal defect closure through femoral and transjugular approaches in patients with interrupted inferior vena cava. Journal of Cardiology Cases, 18(3), 106–109. DOI 10.1016/j.jccase.2018.05.007. [Google Scholar] [CrossRef]
6. Bhargava, R. A., Phatarpekar, A., Lanjewar, C. P., Kerkar, P. G. (2017). Modified transjugular approach for percutaneous atrial septal defect closure. Annals of Pediatric Cardiology, 10(2), 197–199. DOI 10.4103/apc.APC_167_16. [Google Scholar] [CrossRef]
7. Thanopoulos, B. D., Biasco, L., Dardas, P., De Backer, O., Avraamides, P. et al. (2014). Catheter closure of atrial septal defects using the Cocoon septal occluder: preliminary results of a European multicenter study. International Journal of Cardiology, 177(2), 418–422. DOI 10.1016/j.ijcard.2014.09.006. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |