
 | Congenital Heart Disease | 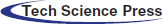 |
DOI: 10.32604/CHD.2020.013078
ARTICLE
Impact of the COVID-19 Pandemic on Health-Related Concerns, Quality of Life and Psychological Adjustment in Young Adults with Congenital Heart Disease
1Child Development Center, University Children’s Hospital Zurich, Zurich, Switzerland
2Department of Neonatology and Pediatric Intensive Care, University Children’s Hospital Zurich, Zurich, Switzerland
3Children’s Research Center, University Children’s Hospital Zurich, Zurich, Switzerland
4Department of Psychosomatics and Psychiatry, University Children’s Hospital Zurich, Zurich, Switzerland
5Division of Child and Adolescent Health Psychology, Department of Psychology, University of Zurich, Zurich, Switzerland
6Clienia Schlössli, Oetwil am See, Switzerland
7Department of Cardiology, University Heart Center, University Hospital Zurich, Zurich, Switzerland
*Corresponding Author: Matthias Greutmann. Email: matthias.greutmann@usz.ch
Received: 25 July 2020; Accepted: 25 August 2020
Background: The risk for a severe disease course in case of infection with SARS-CoV-2 in young adults with congenital heart disease is largely unknown, potentially leading to uncertainty and anxiety among affected patients. This study aims to investigate health-related concerns, health-related quality of life and psychological adjustment in patients with congenital heart disease compared to healthy peers during the COVID-19 pandemic. Methods: One-hundred patients with congenital heart disease and 50 controls (M = 29.7, SD = 3.8 years) were recruited. They completed an online survey including the assessment of health-related concerns regarding COVID-19, the 12-item Short Form Health Survey and the Brief Symptom Inventory. Results: Patients considered COVID-19 to be a more serious issue (Generalized odds ratio [GenOR] = 1.67, p = 0.04), were more concerned about becoming infected (GenOR = 2.93, p < 0.001) and expressed more fear about leaving their homes (GenOR = 1.81, p = 0.004) while general anxiety symptoms were not different between groups (p = 0.23). Patients relied more on family and friends for support (30% vs. 2% in controls, p < 0.001) and reported better compliance with protective measures (p = 0.03). Mental health-related quality of life and psychological adjustment were not different between groups (p = 0.17 and p = 0.68, respectively). Physical health-related quality of life was lower in patients compared to controls (p = 0.03). Conclusions: Young adults with congenital heart disease in Switzerland are more concerned about their health during the COVID-19 pandemic compared to healthy peers. These concerns, however, do not translate into generally impaired mental well-being. The impact of the easing of lockdown measures on long-term anxiety levels and quality of life requires further study.
Keywords: COVID-19; congenital heart disease; health-related concerns; psychological adjustment; quality of life
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) causing the coronavirus disease 2019 (COVID-19) has rapidly spread around the globe and was declared a pandemic by the World Health Organization on March 11th 2020 [1]. In the general population, high levels of worries and concerns in relation to COVID-19 have been reported in a number of studies, including concerns of contracting the virus, family and friends becoming infected, supply shortages, and potential negative consequences for society and the economy as a whole [2–4]. Furthermore, increased levels of psychological distress and poorer mental health during the pandemic have been reported [2,5–7].
While advanced age is the most important determinant of a severe disease course in case of COVID-19, preexisting cardiovascular disease has been identified as an important additional risk factor [8]. Due to the lack of data, it remains, however, largely unknown to what extent young adults with congenital heart disease are at increased risk for a severe disease course in case of infection with SARS-CoV-2 [9–11]. This uncertainty may lead to higher levels of concerns among these patients. Thus, the aim of this study is to assess the impact of the COVID-19 pandemic on health-related concerns, health-related quality of life and psychological adjustment in young adults with congenital heart disease compared to healthy peers.
Patients with congenital heart disease and healthy controls were recruited from a previous study on health-related quality of life in young adults with congenital heart diseases conducted in 2015 [12]. In short, 300 patients between 18 and 30 years of age without severe neurological impairments, comorbid genetic syndromes, severe psychiatric diagnoses and who were fluent in German were eligible for the study in 2015 and were approached when attending the cardiac outpatient clinic at the University Hospital Zurich, Switzerland. Of those, 188 completed the questionnaires on health-related quality of life and psychological adjustment. Patients were asked to identify healthy peers as controls. A total of 139 age- and sex-matched healthy controls completed the study-specific questionnaires.
For the current study, those patients and controls who had completed the questionnaires in the study in 2015 were invited to complete an online questionnaire on the impact of the COVID-19 pandemic on their life. Data were collected between April 17th and May 10th 2020, while partial lockdown measures to halt the spread of the COVID-19 pandemic were implemented in Switzerland. These included school closure, closure of non-essential services and retail, and reduction of public transport services.
Patients who participated in the COVID-19 survey did not differ from non-participating patients with regard to sex (p = 0.99) and educational level (p = 0.27). Participating patients were older than non-participating patients (difference = 1.08 years; p = 0.05). Medical characteristics (i.e., complexity of the underlying heart defect) were not different between participating and non-participating patients (all p > 0.05). Healthy controls who participated in the COVID-19 survey did not differ from non-participating controls with regard to sex (p = 0.99) and educational level (p = 0.54). Participating controls were older than non-participating controls (difference = 1.35 years; p = 0.04). Health-related quality of life and psychological adjustment were not different between participants and non-participants, neither in patients nor in controls (all p > 0.05).
This study was approved by the ethical committee of the Canton of Zurich, Switzerland (PB_2020-00030) and written informed consent was obtained from all participants.
2.2 Assessment of Health-Related Concerns During the COVID-19 Pandemic, and Quality of Life and Psychological Adjustment Prior to and During the Pandemic
Concerns related to COVID-19 and the associated measures to halt its spread were assessed as the level of agreement with various statements on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree; Fig. 1). Similarly, the perceived likelihood of becoming infected, the level of compliance with protective measures (e.g., hand disinfection, social distancing) and the perceived effectiveness of these measures were assessed on a 5-point Likert scale.
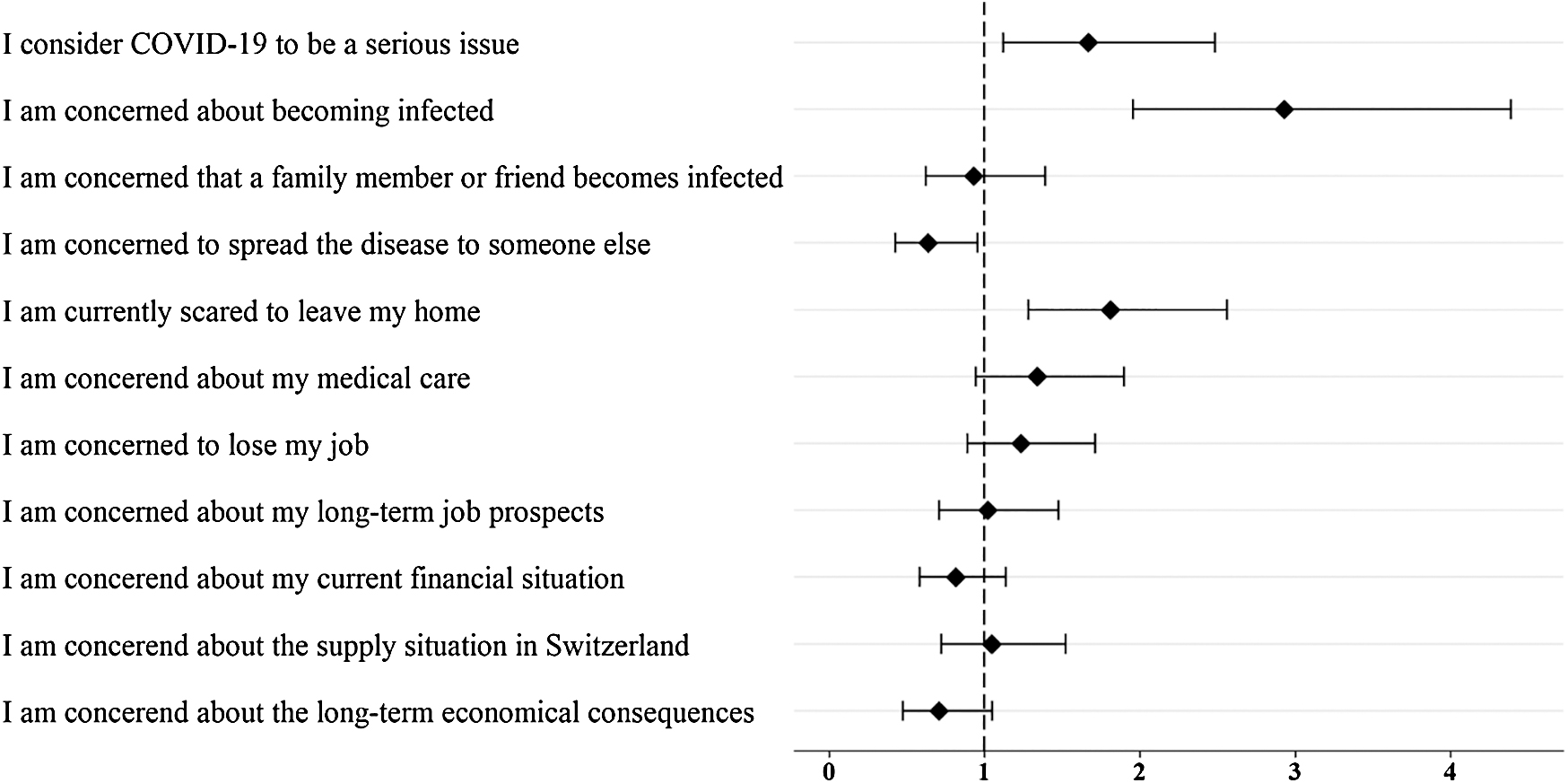
Figure 1: Health-related concerns during COVID-19 pandemic in young adults with congenital heart disease. Generalized odds ratios (and 95% confidence intervals) for a higher level of agreement with statements on concerns related to COVID-19 in patients than in healthy peers. The dashed line indicates equal levels of concern in patients and controls
Health-related quality of life was assessed with the 36-item Short From Health Survey (SF-36) [13] in the study in 2015 and a validated short-form during the pandemic (SF-12) [13,14]. Both forms provide a physical and a mental summary score. Higher scores reflect better health-related quality of life.
Psychological adjustment was assessed with the Symptom Checklist-27 (SCL-27) [15] in the study in 2015. The global severity index was used for further analyses. Higher scores reflect poorer psychological adjustment. During the pandemic, the 18-item Brief Symptom Inventory (BSI-18) [16] was applied and the global severity index and the three subscales, depressive symptoms, anxiety and somatization were used for further analyses. Higher scores reflect poorer psychological adjustment. Patients’ medical characteristics were obtained from chart review.
Descriptive statistics include mean and standard deviations for continuous and numbers and percentages of totals for categorical data. Generalized odds ratios (GenOR) were used to express the level of concerns related to COVID-19 in patients with congenital heart disease relative to controls [17]. Health-related quality of life and psychological adjustment were compared between groups using linear regression. The potential impact of sex, educational level, heart disease complexity and cardiac events since 2015 on concerns related to COVID-19, health-related quality of life and psychological adjustment were investigated with linear and ordinal regression models for continuous and categorical outcomes, respectively. All analyses were performed using R statistical software [17–19].
3.1 Participant Characteristics
A total of 100 patients and 50 controls completed the questionnaire (participation rate: 46% of the cohort in 2015). Socio-demographic characteristics of patients and controls are shown in Tab. 1.
Table 1: Socio-demographic characteristics of patients with congenital heart disease and healthy peers
Among patients, disease complexity was mild in 27%, moderate in 43% and severe in 30% (including 8 patients after Fontan palliation, 2 patients with unrepaired cyanotic defects/Eisenmenger syndrome and 1 patient with overt heart failure). Since 2015, 19% of all patients had experienced an adverse cardiac event (i.e., reintervention or reoperation, cardiac arrhythmia, heart failure or endocarditis).
3.2 Health-Related Concerns During the COVID-19 Pandemic
Fig. 1 illustrates the level of concerns regarding COVID-19 in patients with congenital heart disease relative to controls. Compared to healthy peers, patients perceived COVID-19 to be a more serious issue (GenOR = 1.67, p = 0.04), were more concerned about becoming infected (GenOR = 2.93, p < 0.001) and expressed more fear about leaving their homes (GenOR = 1.81, p = 0.004). None of the other statements differed between patients and controls (GenOR 0.64 to 1.34, all p > 0.05, p-values adjusted for false discovery rate).
The perceived likelihood of becoming infected was not different between patients and controls (p = 0.79), with 12% of patients and 19% of controls perceiving it to be ‘likely’ or ‘very likely’ to become infected. Patients reported better compliance with recommended protective measures than controls (p = 0.03), with the level of compliance being high in both groups (80% and 70% in patients and controls reporting to comply ‘well’ or ‘very well’). The perceived effectiveness of the recommended measures to halt the spread of the disease was not different between groups (p = 0.22), with 85% of patients and 78% of controls perceiving the measures to be ‘effective’ or ‘very effective’. One third of the patients reported to rely on support from family members or friends for tasks outside their homes, e.g., grocery shopping (30% vs. 2% in controls, p < 0.001). Neither sex and educational level nor disease complexity and adverse cardiac events since 2015 were associated with any of these results.
3.3 Health-Related Quality of Life and Psychological Adjustment Prior to and During the COVID-19 Pandemic
Tab. 2 presents data of health-related quality of life and psychological adjustment prior to (i.e., in 2015) and during the COVID-19 pandemic. Physical health-related quality of life was not different between groups prior to the pandemic but significantly lower in patients during the pandemic (p = 0.74 and p = 0.03, respectively). Mental health-related quality of life was not different between patients and controls, neither prior to nor during the COVID-19 pandemic (p = 0.52 and p = 0.17, respectively).
Table 2: Physical and mental health-related quality of life and psychological adjustment prior to and during the COVID-19 pandemic in young adults with congenital heart disease and healthy controls
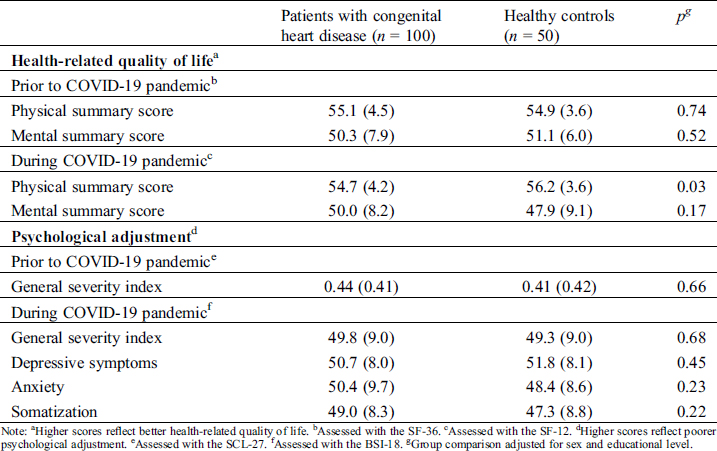
Psychological adjustment as assessed with the general severity index was not different between groups, neither prior to nor during the COVID-19 pandemic (p = 0.66 and p = 0.68, respectively). Depressive symptoms, anxiety and somatization were not different between groups during the pandemic (all p > 0.05).
Our results demonstrate that compared to healthy peers, young adults with congenital heart disease are more concerned about their health during the COVID-19 pandemic—independent of disease complexity. Neither mental health-related quality of life nor psychological adjustment is impaired in patients compared to healthy peers during the pandemic.
Patients with congenital heart disease are more concerned about becoming infected and leaving their homes during the ongoing COVID-19 pandemic and, generally, consider the disease to be a more serious issue compared to healthy peers. Presumably, these concerns prompt patients to comply better with protective measures to halt the spread of the disease (e.g., washing hands, social distancing) and to rely more strongly on family and friends for tasks outside their homes (e.g., grocery shopping). These findings parallel those of several studies in the general population, reporting that higher levels of COVID-19-related fear and feeling personally at risk by the disease are predictive of increased engagement in protective behaviors [20–22]. Notably, the increased health concerns and engagement in protective measures in patients with congenital heart disease are not the expression of a generally increased level of anxiety symptoms or a biased perception of infection likelihood and the effectiveness of the measures to prevent the spread of COVID-19.
Importantly, the increased health-related concerns of young adults with congenital heart disease do not translate into impaired mental health-related quality of life or poor psychological adjustment compared to healthy peers. This is in line with a study in young adults in Italy, reporting COVID-19-related worries and concerns for relatives and the public in general but not for oneself to be associated with psychological maladjustment [2].
Physical health-related quality of life was lower in patients with congenital heart disease compared to healthy peers during the pandemic. Reduced physical health-related quality of life has been reported previously in an overlapping cohort [12] and in other cohorts of young adults with congenital heart disease e.g., [23,24]. Notably, group differences in physical health-related quality of life during the COVID-19 pandemic in the current study are driven by high levels in controls rather than low levels in patients. Whether this, indeed, is related to the COVID-19 pandemic needs further investigation.
Importantly, the impact of the COVID-19 pandemic on health-related concerns and quality of life in young adults with congenital heart disease may change as lock-down measures are continuously eased: Patients will be asked to return to their workplace and adherence to preventive and protective measures (e.g., social distancing at workplace, avoidance of public transport) may become more difficult. Longitudinal studies are required to assess these aspects. To date, empirical data on the potential risk of COVID-19 for adults with congenital heart disease is very limited and, thus, clear risk stratification criteria are lacking. Counselling of individual patients is largely based on extrapolation from patient series with acquired heart disease and from expert opinion [8–11]. Likely, this lack of solid data increases the uncertainty among patients and treating physicians regarding their risk for a severe disease course. Several multicenter studies are currently underway that aim to assess the risk of COVID-19 for adults with congenital heart disease. Results from these studies are eagerly awaited for better risk stratification and counselling of patients.
The employment of short-form instruments during the COVID-19 assessment limits the investigation of the longitudinal development of health-related quality of life and psychological adjustment since 2015. This study was conducted in Switzerland, where lock-down measures were less strict compared to many other countries, e.g., schools were closed and orders of social distancing were issued but home confinement was not implemented. The results may, thus, not be readily generalizable to other countries with different situations during the COVID-19 pandemic.
Young adults with congenital heart disease in Switzerland are more concerned about their health during the COVID-19 pandemic compared to healthy peers. This, however, does not translate into impaired mental well-being. Studies that identify young patients with congenital heart disease at high risk for a complicated disease course in case of COVID-19 are urgently needed, as this will allow tailored counselling of individual patients and, hence, may reduce concerns in patients at low risk in case of COVID-19.
Acknowledgement: We thank Ladina Schlosser, Barbara Schnider, Dominique Eichelberger, Melanie Ehrler, Nadja Naef, and Peter Brugger for their input and support. We thank all the participants for their time and support of our research.
Data Sharing: The approval granted by the ethical committee does not allow the publication of the raw data online. If readers would like to re-analyze the data set (for different purposes), additional ethical approval (on an individual user and purpose basis) will be required. The authors are happy to support additional ethical approval applications from researchers for access to this data set.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. World Health Organization. (2019). Coronavirus disease 2019. https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
2. Germani, A., Buratta, L., Delvecchio, E., Mazzeschi, C. (2020). Emerging adults and COVID-19: the role of individualism-collectivism on perceived risks and psychological maladjustment. International Journal of Environmental Research and Public Health, 17(10), 3497. DOI 10.3390/ijerph17103497.
3. Stokes, D. C., Andy, A., Guntuku, S. C., Ungar, L. H., Merchant, R. M. (2020). Public priorities and concerns regarding COVID-19 in an online discussion forum: longitudinal topic modeling. Journal of General Internal Medicine, 35(7), 2244–2247. DOI 10.1007/s11606-020-05889-w.
4. Nelson, L. M., Simard, J. F., Oluyomi, A., Nava, V., Rosas, L. G. et al. (2020). US public concerns about the COVID-19 pandemic from results of a survey given via social media. JAMA Internal Medicine, 180(7), 1020–1022. DOI 10.1001/jamainternmed.2020.1369.
5. Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B. et al. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry, 33(2), e100213. DOI 10.1136/gpsych-2020-100213.
6. Wang, H., Xia, Q., Xiong, Z., Li, Z., Xiang, W. et al. (2020). The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: a web-based survey. PLoS One, 15(5), e0233410. DOI 10.1371/journal.pone.0233410.
7. Mazza, C., Ricci, E., Biondi, S., Colasanti, M., Ferracuti, S. et al. (2020). A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. International Journal of Environmental Research and Public Health, 17(9), 3165. DOI 10.3390/ijerph17093165.
8. Yang, J., Zheng, Y., Gou, X., Pu, K., Chen, Z. F. et al. (2020). Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. International Journal of Infectious Diseases, 94, 91–95. DOI 10.1016/j.ijid.2020.03.017.
9. Radke, R. M., Frenzel, T., Baumgartner, H., Diller, G. P. (2020). Adult congenital heart disease and the COVID-19 pandemic. Heart (British Cardiac Society), 106(17), 1302–1309.
10. Tan, W., Aboulhosn, J. (2020). The cardiovascular burden of coronavirus disease 2019 (COVID-19) with a focus on congenital heart disease. International Journal of Cardiology, 309, 70–77. DOI 10.1016/j.ijcard.2020.03.063.
11. Feinberg, J. L., Cecchin, F., Gonzalez, A., Johnson, E., Halpern, D. G. (2020). Managing the adult congenital heart disease patient in the COVID-19 pandemic—a New York perspective. Congenital Heart Disease, 15(3), 141–146.
12. Rometsch, S., Greutmann, M., Latal, B., Bernaschina, I., Knirsch, W. et al. (2019). Predictors of quality of life in young adults with congenital heart disease. European Heart Journal - Quality of Care & Clinical Outcomes, 5(2), 161–168. DOI 10.1093/ehjqcco/qcy046.
13. Morfeld, M., Kirchberger, I., Bullinger, M. (2011). Fragebogen zum Gesundheitszustand (SF-36). 2nd Edition. Bern, Switzerland: Hogrefe.
14. Wirtz, M. A., Morfeld, M., Glaesmer, H., Brähler, E. (2018). Konfirmatorische Prüfung der Skalenstruktur des SF-12 Version 2.0 in einer deutschen bevölkerungs-repräsentativen Stichprobe. Diagnostica, 64(2), 84–96. DOI 10.1026/0012-1924/a000194.
15. Hardt, J., Egle, U. T., Kappis, B., Hessel, A., Brähler, E. (2004). Die Symptom-Checkliste SCL-27- Ergebnisse einer deutschen Repräsentativbefragung [Symptom Checklist SCL-27]. PPmP-Psychotherapie, Psychosomatik, Medizinische Psychologie, 54(5), 214–223. DOI 10.1055/s-2003-814786.
16. Franke, G. H. (2017). Mini-SCL-mini-symptom-checklist. Bern, Switzerland: Hogrefe.
17. O’Brien, R. G., Castelloe, J. (2006). Exploiting the link between the Wilcoxon-Mann-Whitney test and a simple odds statistic. Proceedings of the Thirty-First Annual SAS Users Group International Conference. ASA Section on Statistical Consulting, Cary, NC: SAS Institute, pp, 2192–2198.
18. R Core Team. (2018). R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/.
19. Wickham, H. (2016). ggplot2: elegant graphics for data analyses. New York: Springer.
20. Yıldırım, M., Geçer, E., Akgül, Ö. (2020). The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Psychology, Health & Medicine, 1–9. DOI 10.1080/13548506.2020.1776891.
21. Harper, C. A., Satchell, L. P., Fido, D., Latzman, R. D. (2020). Functional fear predicts public health compliance in the COVID-19 pandemic. International Journal of Mental Health and Addiction, 395, 1–14. DOI 10.1007/s11469-020-00281-5.
22. Dryhurst, S., Schneider, C. R., Kerr, J., Freeman, A. L., Recchia, G. et al. (2020). Risk perceptions of COVID-19 around the world. Journal of Risk Research, 1–13. DOI 10.1080/13669877.2020.1758193.
23. Gratz, A., Hess, J., Hager, A. (2009). Self-estimated physical functioning poorly predicts actual exercise capacity in adolescents and adults with congenital heart disease. European Heart Journal, 30(4), 497–504. DOI 10.1093/eurheartj/ehn531.
24. Farr, S. L., Oster, M. E., Simeone, R. M., Gilboa, S. M., Honein, M. A. (2016). Limitations, depressive symptoms, and quality of life among a population-based sample of young adults with congenital heart defects. Birth Defects Research Part A: Clinical and Molecular Teratology, 106(7), 580–586. DOI 10.1002/bdra.23498.
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |