
 | Congenital Heart Disease |  |
DOI: 10.32604/CHD.2020.013127
ARTICLE
Mid-Term Outcome of Surgical Treatment in Pediatric Patients with Ebstein’s Anomaly: A Single-Center Cohort Study
Pediatric Cardiac Center, Department of Cardiac Surgery, State Key Laboratory of Cardiovascular Disease, National Center for Cardiovascular Disease, Fuwai Hospital, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing, 100037, China
*Corresponding Author: Qiang Wang. Email: wqcory@126.com
Received: 27 July 2020; Accepted: 15 August 2020
Abstract: Background: Ebstein’s anomaly (EA) is a malformation of the tricuspid valve (TV) and myopathy of the right ventricle (RV). Surgery is now the main treatment for the defect. Objective: To summarize our surgical results and experience based on patients with EA who were under 7 years of age and treated with different surgical treatments. Design: Single-center cohort study of Ebstein’s anomaly. Setting: China. Participants: 80 patients under 7 years old who were diagnosed of EA and underwent different surgical treatments were consecutively enrolled in our research from January 2010 to December 2019. Results: The median age of the 80 patients at the time of surgery was 3.63 years. Sixty-four (80.00%) patients underwent biventricular repair while 13 (16.25%) underwent 1.5-ventricle repair. With the median follow-up 27.50 months, the mid-term survival of the total cohort, 1.5-ventricular repair and biventricular repair was 82.35%, 91.67% and 100%, respectively. The mid-term freedom from reoperation rate was 97.50%, 92.31% and 98.44%, respectively. Mild, moderate and severe TR before surgery occurred in 6 (7.50%), 18 (22.50%) and 56 (70.00%), respectively. The early outcomes of 78 patients were 65 (83.33%), 11 (14.11%) and 2 (2.56%); the mid-term outcomes of 72 patients were 49 (68.06%), 19 (26.38%) and 4 (5.56%). Both early and mid-term valve regurgitations were significantly decreased (p < 0.001) compared with preoperative condition. No more severe regurgitation occurred (p = 0.404), though some early mild regurgitation became acceptable moderate regurgitation during mid-term follow-up (p = 0.036). Conclusion: The overall effect of surgical treatment for EA was good, and most patients could receive biventricular repair at an early stage. The reoperation rate and mid-term mortality were both low and TR was significantly improved.
Keywords: Ebstein’s anomaly; surgical methods; whole-valve technique; cone technique
Ebstein’s anomaly (EA) is a malformation of the tricuspid valve (TV) and myopathy of the right ventricle (RV) [1]. The incidence is 1 per 200,000 live births and it accounts for 1% of congenital heart disease [2]. The core and critical distinguishing characteristic of EA from other congenital regurgitant lesions is the degree of apical displacement of the septal leaflet (≥ 8 mm/m2 body surface area) [3]. The pathological characteristics of each EA patient is different, which makes the surgical management complex and individualized, especially when it is treated with tricuspid valvuloplasty. A number of univentricular palliation and biventricular repair methods, including various modifications of techniques, have been described [4–5]. Studies on surgical outcomes in patients with EA often include a majority of adults; consequently, long-term outcomes of biventricular repair are generally good. However, there are few studies on young children with large sample sizes. We therefore conducted a retrospective study on Chinese EA patients who were under 7 years of age and treated with different surgical treatments based on the recent 10-year data of our institution. The large-sample sized cohort study was of great significance to understand the status quo of diagnosis and summarize our surgical experience for such disease in China.
2.1 Patient Selection and Data Collection
Eighty patients under 7 years old who were diagnosed with EA and underwent different surgical treatments were consecutively enrolled in our research from January 2010 to December 2019. The diagnosis mainly relied on echocardiography and transesophageal ultrasound and was confirmed during the intraoperative probe. The diagnostic criterion was apical displacement of the TV from the atrioventricular ring >0.8 cm/m2 body surface area [6]. Children with other complex congenital heart diseases, including pulmonary atresia, tetralogy of Fallot and corrected transposition of the great arteries were excluded. Demographic data and clinical characteristics included sex, age, weight, body length, cardiac functional class, presence of cyanosis, Carpentier type, associated cardiac anomalies, the presence of preoperative arrhythmias, prior cardiac operations and preoperative degree of tricuspid regurgitation (TR). Surgical procedures and postoperative parameters, including cardiopulmonary bypass (CPB) time, aortic cross clamp time, mechanical ventilation time, intensive care unit (ICU) stay, complications, mortality, cause of death, and TV and RV function, when available, were also comprehensively evaluated. Patients’ records and postoperative follow-up were conducted through our outpatient service and over the telephone.
The surgical criteria included: presence of symptoms or worsening functional class, cyanosis, paradoxical embolism, progressive RV dilation or RV systolic dysfunction, asymptomatic EA patients with massive TR. In general, surgical procedures can be divided into three categories, biventricular repair, 1.5-ventricle repair or univentricular palliation. The decision for the type of repair was based on the ratio of the atrialized right ventricle (aRV) to the functional right ventricle (fRV), the size of the TV annulus and the size of the pulmonary artery in addition to the severity of TR. Biventricular repair was performed in patients with a retained RV function and an acceptable anatomy and fRV in the absence of severe pulmonary valve stenosis or atresia. Due to the lack of preoperative quantitative evaluation, most of the decisions for 1.5-ventricle repair were made by the surgeon during the operation. In patients with extensive RV failure, severe TR and/or the presence of other relevant cardiac comorbidities, e.g., PA, a univentricular palliation was the intended surgical strategy.
There are some evaluation criteria that can help us understand the preoperative condition and postoperative recovery of patients. Cyanosis was determined when the increasing level of deoxyhemoglobin in the blood resulted in a purplish appearance of the skin mucous membrane. The severity of EA was evaluated by echocardiography and transesophageal echocardiography and determined by the internationally recognized Carpentier type. Early outcome mainly referred to death or reoperation within 30 days after surgery or before hospital discharge. Mid-term outcome mainly referred to death or reoperation within one to five years after surgery.
Descriptive statistics for the 80 patients are reported. Data are presented as means ± standard deviations (SDs) for continuous data with a normal distribution, as medians (25th percentile, 75th percentile) for continuous data with a nonnormal distribution, or as numbers and percentages for categorical variables, as appropriate. Freedom from reoperation and cumulative survival rates were analyzed according to the Kaplan-Meier test. There was insufficient incidence of deaths and reoperations to perform an analysis to identify risk factors for early mortality. Differences in the frequency of TR at preoperative, early and mid-term follow-up examinations were performed using the chi-square test and Fisher test. Statistical significance was defined as p < 0.05 with two-tailed distributions. All statistical analyses were performed with SPSS version 22.0 software (SPSS, Inc., Chicago, IL, USA) and GraphPad Prism version 5.0 software (GraphPad Software, Inc., La Jolla, CA, USA).
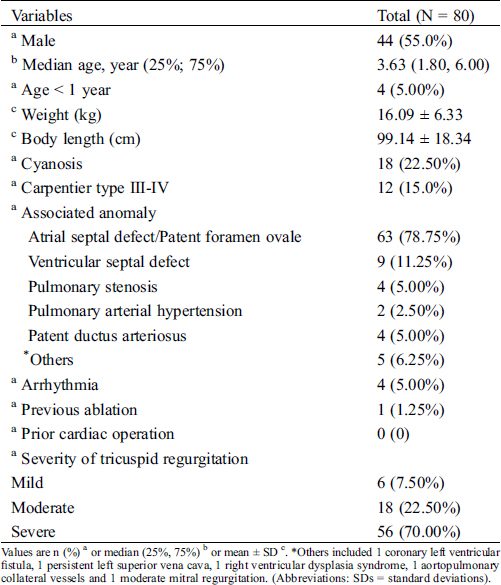
The demographic data and clinical characteristics of the patients are summarized in Tab. 1. The youngest patient who underwent biventricular repair was 3 months old, while the youngest patient who underwent 1.5-ventricle repair was 8 months old.
Table 1: Demographic data and clinical characteristics
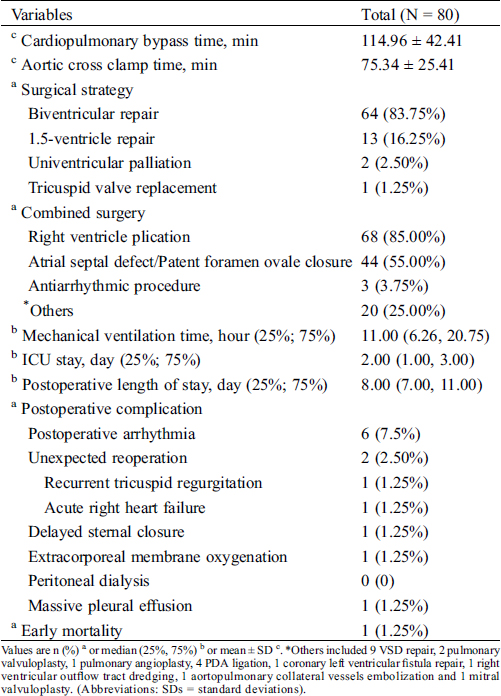
3.2 Surgical Procedures and Postoperative Data
The surgical procedures performed and postoperative data are presented in Tab. 2. Of the 80 patients, two (2.50%) patients underwent the Glenn procedure instead of radical surgery because of tricuspid orifice stenosis and right ventricle dysplasia at the age of 1.6 and 5 years old. Tricuspid valve replacement (TVR, 29#, Medtronic, Bio-valve) was performed for one (1.25%) patient because of severe tricuspid valve dysplasia. Two (2.50%) patients underwent unexpected reoperation, one of them underwent rerepair because of recurrent TR on the 6th day postoperatively, while the other underwent 1.5 ventricular repair on the 6th day postoperatively. The early mortality was 1.25%, and 1 patient’s venous pressure increased and blood pressure decreased after biventricular repair. The Glenn procedure and extracorporeal membrane oxygenation were then performed, but the patient consistently could not maintain spontaneous breathing after surgery because of poor right heart function and passed away on the 38th day after the operation.
Table 2: Surgical procedures and postoperative data
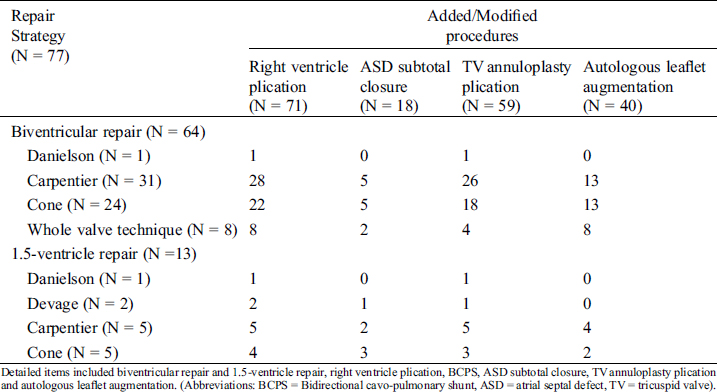
The detailed surgical strategies are shown in Tab. 3. Regular methods of EA surgical correction included the Danielson procedure, Devage procedure, Carpentier procedure, cone procedure, and whole-valve technique. The main procedures applied in our center were as follows. 1) Danielson procedure: lateral aRV plication, and the lobes were raised to the level of the normal valve ring. 2) Devage procedure: plication with 1 or 2 mattress sutures from the junction of the anterior and posterior lobe to the junction of the septal and posterior lobe, whereby the apical aspects of the septal and anterior leaflets would effectively create a bicuspid valve. 3) Carpentier procedure: most of the anterior valve and adjacent part of posterior valve were detached and sutured at the level of the normal tricuspid valve ring, longitudinal aRV plication, such that the TV became a single valve structure dominated by the anterior valve. 4) Cone procedure: all three lobes were cut off at the root of the lobe, the adhesion of the subvalve tissue was released, and the three lobes were then structured to be a cone-like body, clockwise rotated and sutured into the normal valve ring. 5) Whole-valve technique: an optimized and improved technique based on the cone procedure in our center. In the case of tricuspid dysplasia, the free margin of each lobe is actively widened with fresh autologous pericardium to ensure sufficient alignment between the lobes. Among the 13 patients, 4 received the intended bidirectional cavopulmonary shunt (BCPS) as a preoperative plan, the other 9 received unplanned BCPS because of poor RV function during the operation. Other modified techniques based on regular methods, including right ventricle plication, TV annuloplasty plication and autologous leaflet augmentation, prosthetic ring or artificial chordae, were not used in the enrolled patients. ASD subtotal closure was also considered in the research.
Table 3: Detailed surgical strategy
3.4 Follow-Up and Mid-Term Outcome
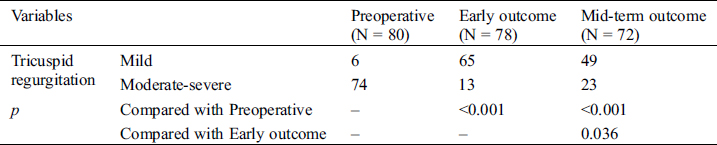
The median follow-up of the 80 patients was 27.50 (10.25, 56.75) months, with 3 patients’ loss to follow-up after discharge, and the effective follow-up rate was 96.25%. The survival curve and the freedom from reoperation curve is shown in Figs. 1a and 1b. One early death occurred after 1.5 ventricular repair on the 38th day after the operation, as mentioned above. One late death occurred in the 6th year after the Glenn procedure because of RV dysplasia. Except for 2 patients who received tricuspid valve re-repair and the Glenn procedure on the 6th day and the 4th day after surgery, no patients received reoperation to date. Of the 6 cases with arrhythmia in the early postoperative period, 1 patient had atrioventricular block of the second degree, 3 had untreated transient ventricular tachycardia, and 2 improved spontaneously after discharge. Other clinically important complications, including right ventricular outflow tract obstruction, left ventricular outflow tract obstruction or TV stenosis, were not observed either before or after surgical repair. Preoperative, predismissal, and mid-term findings observed for TR are summarized in Fig. 2a. Preoperative, predismissal, and mid-term findings observed for TR with whole-valve technique, cone procedure and Carpentier procedure are summarized in Figs. 2b, 2c and 2d, respectively. When comparing preoperative, dismissal and mid-term echocardiograms, we divided the cases into two groups (mild group vs. moderate-severe group) and found that both dismissal and mid-term degrees of TR were significantly decreased (Tab. 4, p < 0.001). Compared with the early outcome, the moderate-severe TR degree increased in the mid-term group (Tab. 4, p = 0.036). However, when separately comparing the mild TR group with the severe TR group (2 severe TR in early outcome group, 4 in severe TR mid-term outcome group), we found that no significant severe TR occurred (p = 0.404). It could be speculated that some early mild TR cases had become acceptable moderate TR.
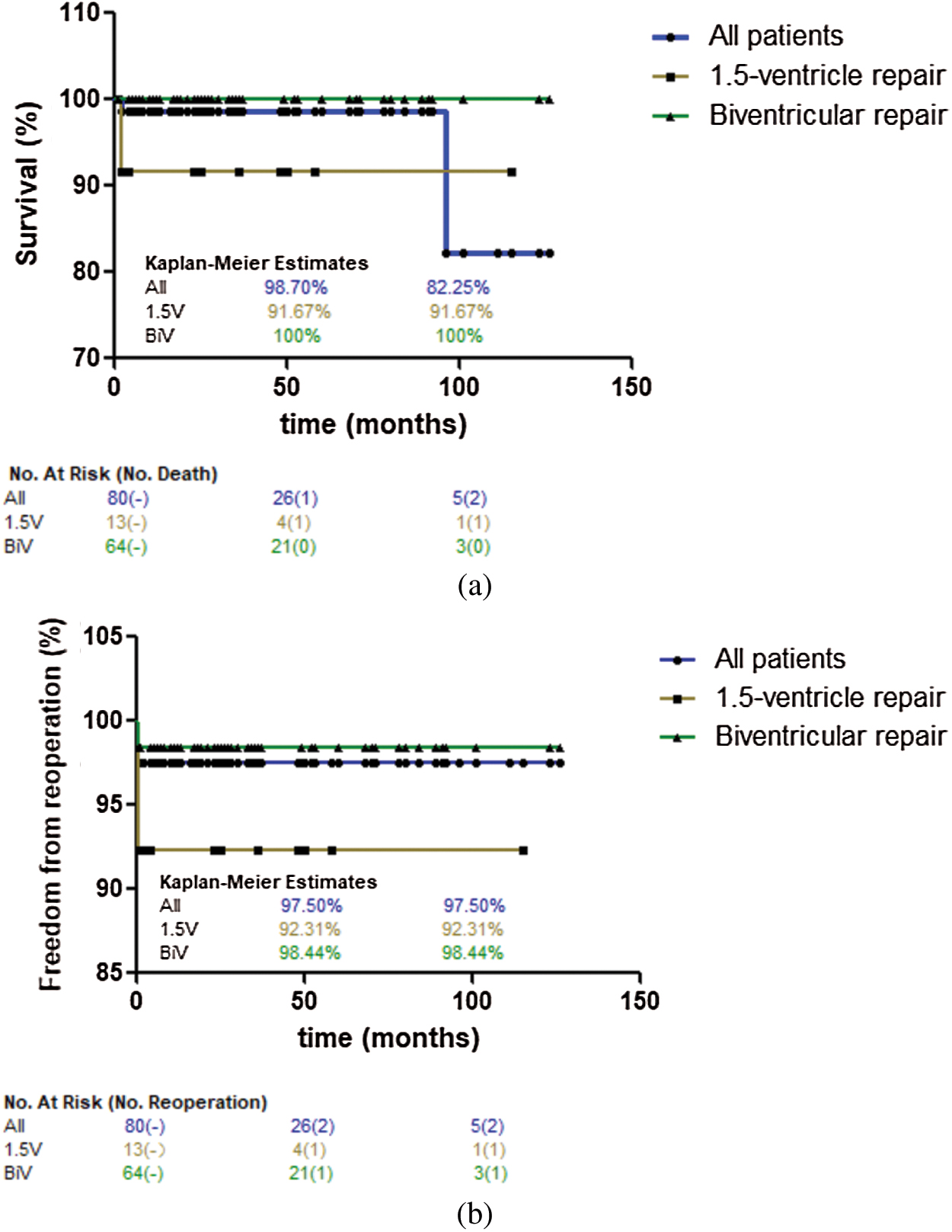
Figure 1: Mid-term survival and freedom from reoperation. (a): Mid-term survival. All patients (blue line, N = 80), patients underwent 1.5 ventricular repair (yellow line, 2 patients who only underwent Glenn procedure were excluded, N = 13), patients underwent biventricular repair (green line, 1 patient who underwent tricuspid valve replacement was excluded, N = 64). (b): Freedom from reoperation. All patients (blue line, N = 80), patients underwent 1.5 ventricular repair (yellow line, 2 patients who only underwent Glenn procedure were excluded, N = 13), patients underwent biventricular repair (green line, 1 patient who underwent tricuspid valve replacement was excluded, N = 64)
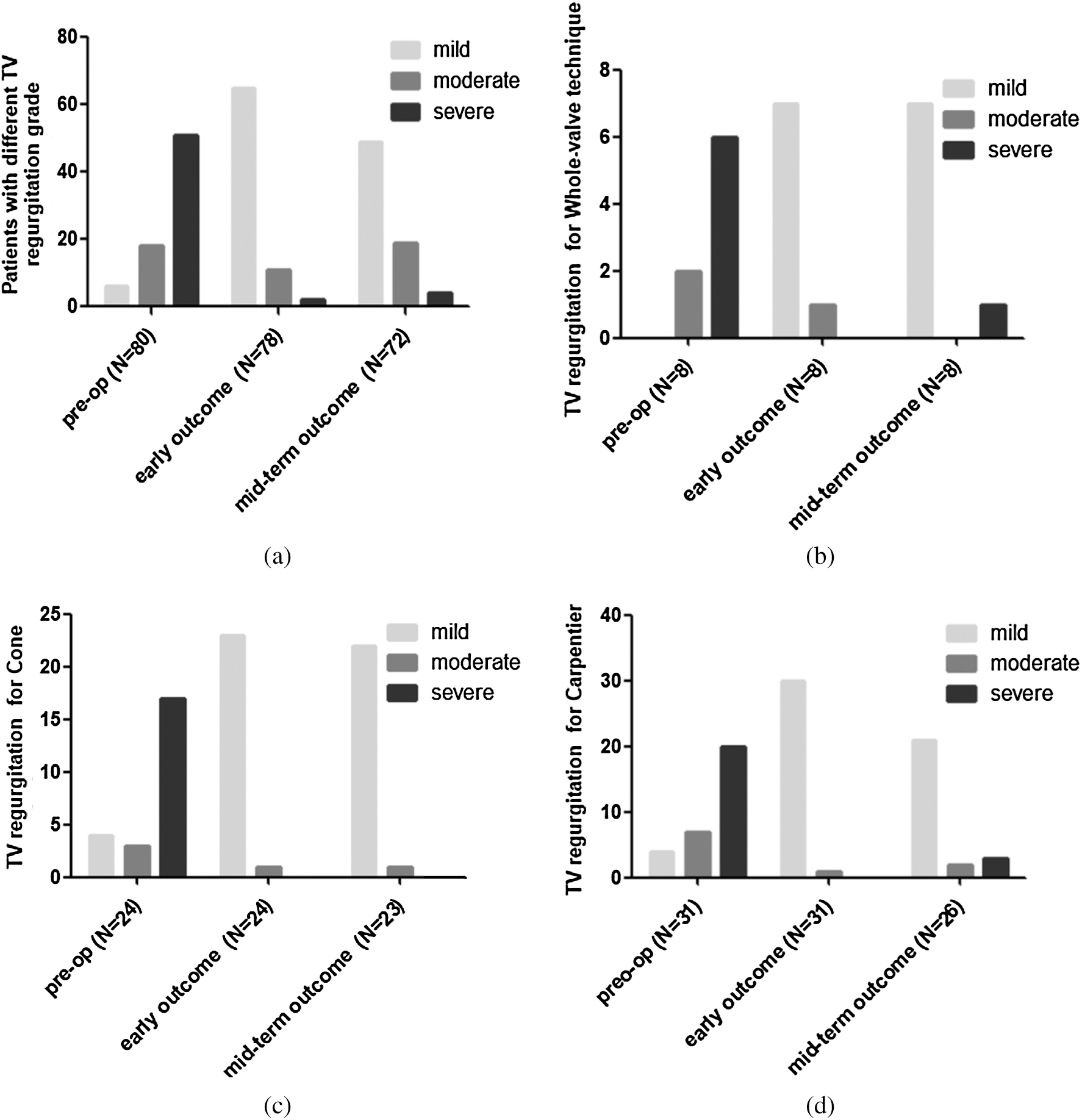
Figure 2: Paired comparisons of echocardiographic changes after surgical repair. (a): Paired comparisons after surgical repair. (b): Paired comparisons after Whole-valve technique repair. (c): Paired comparisons after Cone repair. (d): Paired comparisons after Carpentier repair. (Early outcome mainly pointed out the results of the last review before discharge from hospital, mid-term outcome pointed out the results of the last review in our or local hospital, pre-op = preoperative result, TV = tricuspid valve)
Table 4: Comparison of mild and moderate-severe tricuspid regurgitation between preoperative, early and mid-term echocardiograms
Among the patients diagnosed with EA under 7 years old in our study, 6 (7.50%) were younger than 1 year old, and 19 (23.75%) were between 1 and 2 years old. Twelve (15.00%) cases were serious Carpentier type III-IV. Compared to previously reported studies, the proportion of biventricular repair was high but the proportion of 1.5-ventricle repair and univentricular palliation rather low in our center. The overall effect of surgical treatment was good, and the overall outcome of the operations was worthy of recognition. The rates of mid-term mortality and reoperation were both very low. TR was significantly improved. Serious mid-term complications did not occur except for 6 cases of untreated arrhythmia.
Traditional indications for surgery included symptoms of cyanosis, fatigue, paradoxical embolism, decreasing exercise performance (preferably documented by exercise testing), progressive RV enlargement, progressive RV dilation or reduction of systolic function by echocardiography and/or appearance of atrial or ventricular arrhythmias [7]. But as Dr. Dearani mentioned [8], the timing of operation for Ebstein’s anomaly continues to be controversial, particularly with an asymptomatic patient who has normal exercise tolerance. If the results of anatomical repair such as cone procedure are proven durable and if the functional RV improves, there may be a paradigm shift toward earlier operation. In addition to the preceding guideline, our surgical indications also include asymptomatic EA patients with massive TR, with or without RV dysfunction. We tend to surgical treatment in an earlier period with appropriate anatomical repair, because the RV function may be preserved now but will be impaired gradually. Dr. Dearani indicated [7] that the operation should occur in early childhood as long as the surgical team can provide a reproducible and predictable satisfactory tricuspid repair. Their cone repair rate in children approached 100%, and the risk of operation was <1%, as reported in a large sample-size retrospective study [9]. Similar results could be drawn in our research. The overall survival was 98.71% at 4 years and 82.35% at 8 years, and none of the patients who received biventricular repair have died to date.
4.3 Experience of Surgical Intervention
The original method from the 1960s was to uplift the descending valve, including the Hardy technique and Danielson technique [10]. In the 1990s, the Carpentier technique [11] and subsequent Quaegebeur technique [12] incorporated surgical delamination of the anterior leaflet with annular reattachment to optimize monocusp mobility for ventricular septal coaptation. Since 2007, the cone reconstruction [13] technique has become one of the most widely recognized surgical procedures for EA. It is an extension of the previous technique in that septal and inferior leaflet tissues were mobilized, after which the sides of all mobilized leaflets were connected in a manner to create 360 degrees of leaflet tissue. Near-anatomic repair could be achieved when the newly constructed “cone” was reattached to the true annulus. After that, many other studies have reported their modified cone technique and achieved good results, including ringed annuloplasty, closure of leaflet fenestration, Sebening stitch, and artificial chordae among others [9]. During the same period, our concept of biventricular repair has constantly been updated. The Cone technique was increasingly used instead of the Carpentier technique. According to our research, although there was no significant difference in survival rate and free from reoperation rate between the two procedures, the mid-term TR effect of cone surgery was better than that of Carpentier surgery. However, during our clinical treatment and subsequent re-examination, we found that with the cone technique, some patients still showed different degrees of TR and RV enlargement at the later stage, even though the initial postoperative effect was good, especially for those with severe tricuspid dysplasia. From January 2018, we began our modified method named the “whole-valve technique”. Our experiences are as follows: 1) all the clingy leaflets of the tricuspid valve sufficiently dissociated from the right ventricular wall to guarantee effective closure of the detached part of the anterior and posterior leaflets; 2) in the cases of tricuspid valve dysplasia, fresh pericardial tablets were actively used for splicing the detached part of each leaflet; and 3) new leaflets were sutured to the plication of the true tricuspid annulus. To date, a total of 8 cases of this technique have been performed, and the 2-year follow-up was satisfactory, including 2 Carpentier type IV cases. No additional Glenn procedure has been performed, and more cases and longer follow-up times will receive further attention. In addition, the modified Devage procedure, also named the “play it where it lies” technique [14], was performed in 2 patients, both of whom underwent the intended Glenn procedure and had moderate TR at the latest reexamination. In our opinion, with regard to the choice of surgical procedure, the “play it where it lies” technique should be chosen with caution. Due to the small number of cases, we were unable to summarize the effective TVR experience and indications for young children.
4.4 When Should We Perform BCPS?
BCPS is applied selectively in patients to unload RV volume in the setting of severe RV dysfunction. Studies have shown that BDPS decreases the volume of the enlarged, dysfunctional right ventricle by 35–45% (depending on the patient’s age), providing substantial preload to the underfilled left ventricle and reducing the hemodynamic stress on a complex TV repair [7]. A multicenter retrospective study [15] from the Netherlands reported that between 1980 and 2013, 63 children (0–112 months) underwent 109 operations. Two of 37 biventricular repair patients received 1.5-ventricle repair at 11 and 105 months after surgery. Five 1.5-ventricle repair patients received BCPS in the first surgery. The other 21 patients underwent univentricular palliation surgery due to extensive RV failure, severe TR or the presence of significant other cardiac abnormalities. In terms of this study, 7 1.5-ventricle repair cases were performed in 109 operations (6.4%), and the rate of 1.5-ventricle repair was rather low compared with our research. In our center, the rate of 1.5-ventricular repair was approximately 16.9%, which was higher than that reported in the Netherlands, yet it was significantly lower compared with the 30% at the Mayo Clinic, USA [9] and the more than 50% at Shanghai Children’s Medical Center, China [16]. The study from Shanghai Children’s Medical Center also suggested that the BCPS procedure should be presented when a preoperatively severely dilated RV (aRV > 50%) with the anterior leaflet causes significant RV outflow tract obstruction, outstanding TV morphologic abnormity, and hemodynamic instability after separation from cardiopulmonary bypass, regardless of the presence of RV failure or severe cyanosis. According to Dr Dearani’s latest study [1], BCPS is generally feasible, as pulmonary hypertension is rare in EA, but should be used with caution because it may increase left ventricular (LV) end-diastolic pressure in the setting of moderate to severe LV dysfunction. Indications for BCPS in adults include both heart failure indications (RV end-diastolic volume >250 mL/m, RV ejection fraction <25%, D-shaped left ventricle, postrepair right atrial pressure to left atrial pressure ratio > 1.5:1, and postrepair cardiac output depression) and no indications of heart failure (complex TV repair tension reduction and postrepair TV stenosis with a mean gradient > 8–10 mmHg). BCPS contraindications related to pulmonary hypertension include a mean pulmonary artery pressure >20 mmHg, pulmonary arteriolar resistance >4 Woods units, and elevated left heart pressure (LV end diastolic pressure or left atrial pressure >12 mmHg). In our opinion, BCPS should be actively prepared when the tricuspid valve orifice is smaller than normal or the proportion of aRV is larger than that of fRV. In addition, ASD subtotal closure is a good method to unload RV. Although saturation was sacrificed to some extent, the mid-term prognosis of the TV and RV was not affected according to our follow-up.
This study is limited by its retrospective nature. Our center does not have many cases in univentricular palliation such as Starnes procedure, as most of the patients were older children (more than 1 year old) when sent to our center, who were more suitable for radical surgery. More arguments of RV function should be provided to assess the patient’s preoperative condition and postoperative recovery. Due to the low number of deaths and reoperations, reliable analysis to identify risk factors could not be performed.
The overall effect of surgical treatment for EA was good, and most patients could receive biventricular repair at an early stage. The reoperation rate and mid-term mortality were both low and TR was significantly improved.
Acknowledgement: The surgical database of Fuwai Hospital in Beijing, China, was studied retrospectively. The study protocol was approved by the Institutional Review Board of Fuwai Hospital. The requirement to obtain informed consent was waived because of the retrospective nature of the study.
Author Contributions: Jiachen Li: drafting article, critical revision of article and design; Xianchao Jiang: data collection; Simeng Zhang: data analysis; Jinyang Liu: approval of article; Yajuan Zhang: approval of article; Jun Yan: approval of article; Shoujun Li: funding secured by; Qiang Wang: concept and design.
Funding Statement: This study was financially supported by the National Key R&D Program of China 2017YFC1308100.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Kimberly, A. H., Heidi, M. C., Joseph, A. D. (2019). Ebstein’s anomaly. Methodist DeBakey Cardiovascular Journal, 15(2), 138–144.
2. Mann, R. J., Lie, J. T. (1979). The life story of Wilhelm Ebstein (1836-1912) and his almost overlooked description of a congenital heart disease. Mayo Clinic Proceedings, 54(3), 197–204.
3. Christine, H. J., Heidi, M. C., Joseph, A. D., William, D. E., Gordon, K. D. (2007). Ebstein’s anomaly. Circulation, 115(2), 277–285. DOI 10.1161/CIRCULATIONAHA.106.619338.
4. Anderson, H. N., Dearani, J. A., Said, S. M., Norris, M. D., Pundi, K. N. et al. (2014). Cone reconstruction in children with Ebstein anomaly: the Mayo clinic experience. Congenital Heart Disease, 9(3), 266–271. DOI 10.1111/chd.12155.
5. Nagdyman, N., Ewert, P., Komoda, T., Alexi-Meskisvili, V., Weng, Y. et al. (2010). Modified repair in patients with Ebstein’s anomaly. Journal of Heart Valve Disease, 19(3), 364–370.
6. Shiina, A., Seward, J. B., Tajik, A. J., Hagler, D. J., Danielson, G. K. (1983). Two-dimensional echocardiographic surgical correlation in Ebstein’s anomaly: preoperative determination of patients requiring tricuspid valve plication vs replacement. Circulation, 68(3), 534–544. DOI 10.1161/01.CIR.68.3.534.
7. Dearani, J. A., Mora, B. N., Nelson, T. J., Haile, D. T., O’Leary, P. W. (2015). Ebstein anomaly review: what’s now, what’s next?. Expert Review of Cardiovascular Therapy, 13(10), 1101–1109. DOI 10.1586/14779072.2015.1087849.
8. Holst, K. A., Dearani, J. A., Said, S., Pike, R. B., Connolly, H. M. et al. (2018). Improving results of surgery for Ebstein anomaly: where are we after 235 cone repairs?. Annals of Thoracic Surgery, 105(1), 160–168. DOI 10.1016/j.athoracsur.2017.09.058.
9. Dearani, J. A., Said, S. M., O’Leary, P. W., Burkhart, H. M., Barnes, R. D. et al. (2013). Anatomic repair of Ebstein’s malformation: lessons learned with cone reconstruction. Annals of Thoracic Surgery, 95(1), 220–228. DOI 10.1016/j.athoracsur.2012.04.146.
10. Stulak, J. M., Dearani, J. A., Danielson, G. K. (2007). Surgical management of Ebstein’s anomaly. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu, 10, 105–11.
11. Chauvaud, S., Berrebi, A., d’Attellis, N., Mousseaux, E., Hernigou, A. et al. (2003). Ebstein’s anomaly: repair based on functional analysis. European Journal of Cardio-Thoracic Surgery: Official Journal of the European Association for Cardio-Thoracic Surgery, 23(4), 525–531. DOI 10.1016/S1010-7940(02)00836-9.
12. Chen, J. M., Mosca, R. S., Altmann, K., Printz, B. F., Targoff, K. et al. (2004). Early and medium-term results for repair of Ebstein anomaly. Journal of Thoracic and Cardiovascular Surgery, 127(4), 990–999. DOI 10.1016/j.jtcvs.2003.11.037.
13. da Silva, J. P.,Baumgratz, J. F., da Fonseca, L., Franchi, S. M., Lopes, L. M. et al. (2007). The cone reconstruction of the tricuspid valve in Ebstein’s anomaly. The operation: early and midterm results. Journal of Thoracic and Cardiovascular Surgery, 133(1), 215–223. DOI 10.1016/j.jtcvs.2006.09.018.
14. Malhotra, S. P., Petrossian, E., Reddy, V. M., Qiu, M., Maeda, K. et al. (2009). Selective right ventricular unloading and novel technical concepts in Ebstein’s anomaly. Annals of Thoracic Surgery, 88(6), 1975–1981. DOI 10.1016/j.athoracsur.2009.07.019.
15. Geerdink, L. M., du Marchie Sarvaas, G. J., Kuipers, I. M., Helbing, W. A., Delhaas, T. et al. (2017). Surgical outcome in pediatric patients with Ebstein’s anomaly: A multicenter, long-term study. Congenital Heart Disease, 12(1), 32–39. DOI 10.1111/chd.12404.
16. Liu, J., Qiu, L., Zhu, Z., Chen, H., Hong, H. (2011). Cone reconstruction of the tricuspid valve in Ebstein anomaly with or without one and a half ventricle repair. Journal of Thoracic and Cardiovascular Surgery, 141(5), 1178–1183. DOI 10.1016/j.jtcvs.2011.01.015.
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |