DOI:10.32604/CHD.2021.012982
| Congenital Heart Disease DOI:10.32604/CHD.2021.012982 | 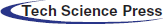 |
| Article |
Pediatric Cardiac Surgical Patterns of Practice and Outcomes in Europe and China: An Analysis of the European Congenital Heart Surgeons Association Congenital Heart Surgery Database
1Department of Surgery, Division of Cardiac Surgery and Pediatric Heart Center, Medical University Vienna, Vienna, Austria
2Department of Pediatric Cardiothoracic Surgery, Shanghai Children’s Medical Center, Shanghai Jiaotong University School of Medicine, Shanghai, China
3Department for Congenital and Pediatric Heart Surgery, German Heart Center Munich, Technische Universität München, Division for Congenital and Pediatric Heart Surgery, University Hospital of Munich, Ludwig-Maximilians-Universität, Munich, Germany
4Pediatric and Cardiac Surgery Unit, Department of Cardio Thoracic Vascular Sciences and Public Health, University of Padua, Padua, Italy
5Department of Cardiothoracic Surgery, University Medical Center Groningen, Groningen, The Netherlands
6Cardiothoracic Surgery, Amsterdam University Medical Center, Amsterdam, The Netherlands
7Pediatric Cardiothoracic Surgery, Children’s Memorial Health Institute, Warsaw, Poland
8St. Petersburg, FL, USA
*Corresponding Author: Claudia Herbst. Email: claudia.herbst@meduniwien.ac.at
Received: 21 July 2020; Accepted: 23 September 2020
Abstract: Background: The European Congenital Heart Surgeons Association (ECHSA) Congenital Heart Surgery Database (CHSD) was founded in 1999 and is open for worldwide participation. The current dataset includes a large amount of surgical data from both Europe and China. The purpose of this analysis is to compare patterns of practice and outcomes among pediatric congenital heart defect surgeries in Europe and China using the ECHSA-CHSD. Methods: We examined all European (125 centers, 58,261 operations) and Chinese (13 centers, 23,920 operations) data in the ECHSA-CHSD from 2006-2018. Operative mortality, postoperative length of stay, median patient age and weight were calculated for the ten benchmark operations for China and Europe, respectively. Results: Benchmark procedure distribution frequencies differed between Europe and China. In China, ventricular septal defect repair comprised approximately 70% of procedures, while Norwood operations comprised less than one percent of all procedures. Neonatal cardiac procedures were rare in China overall. For procedures in STAT mortality category 1, Chinese centers had lower operative mortality rates, while procedures in categories 3 and 5 mortality is lower in European centers. Operative mortality over the time period decreased from 3.89% to 1.64% for the whole cohort, with a sharper decline in China. This drop coincides with an increase of submitted procedures over this 13-year-period. Conclusion: Chinese centers had higher programmatic volume of congenital heart surgeries, while European centers have a more complex case mix. Palliation for patients with functionally univentricular heart was performed less commonly in China. These comparison of patterns of practice and outcomes demonstrate opportunities for continuing bidirectional transcontinental collaboration and quality improvement.
Keywords: Outcomes; congenital heart surgery; China; Europe; database
The European Congenital Heart Surgeons Association Congenital Heart Surgery Database (ECHSA-CHSD) was established in 1999 based on its precursor The European Congenital Heart Defects Database (ECHDD), which was founded in 1994 [1]. Database growth has since been exponential, with more than 300,000 procedures registered in the database by January 2020 [2]. Based in Europe, the ECHSA-CHSD is a worldwide database open for participation by everyone. In 2006 the first Chinese centers started to participate in the ECHSA-CHSD. The current dataset includes a large amount of data from both Europe and China, comprise all economic European regions and east, central and northeastern Chinese regions.
Europe has an area of about 10.2 Mio km² and China has about 9.6 Mio km² [3]. There are about 743 Mio inhabitants [3] living in Europe and about 1.4 Billion inhabitants [3] living in China. The average fertility rate is 1.7 [4] in China. In Europe this number varies in different countries from 2.1 [4] in Turkey to 1.3 [4] in Spain as an example, indicating substantial heterogeneity. Currently, there is a total number of around 5 Mio [5] live births per year in Europe and 15 Mio [6] live births per year in China. That extrapolates the number of children born with congenital heart defects (CHD) to 41.000 per year (8.2/1000) in Europe vs. approximately 139.500 (9.3/1000) per year in China [7]. There is insufficient data on prenatal prevention and screening practices.
Since the first attempts of correcting CHD in 1938 and the development of cardiopulmonary bypass in 1953 further advances took place that today more than 95% of CHD can be surgically cured or treated [8]. Over 25% of the patients with CHD need to undergo palliative or corrective surgery [9].
According to the report from all children’s hospitals in China more than 50 centers could operate over 500 cases per year and two centers perform over 3000 cases annually [10]. There is no reliable data available on the global number of congenital heart surgeries and/or cardiac catheter interventions in Europe or China. The patterns of practice in congenital heart surgery in different countries may vary due to the cultural, religious and legal reasons. The comparison of patterns of practice and outcomes could give opportunities for bidirectional transcontinental collaboration and quality improvement.
The source of data in this article is the ECHSA-CHSD [2]. The nomenclature used in this database is the International Pediatric and Congenital Cardiac Code (IPCCC) derived from the nomenclature of the International Congenital Heart Surgery Nomenclature and Database Project of the European Association for Cardio-Thoracic Surgery (EACTS) and Society of Thoracic Surgeons (STS) [11,12].
This study was approved by the ECHSA-CHSD committee in March 2019. The data in the ECHSA-CHSD is anonymous as to the identity of patients, hospitals or surgeons and all other health care personnel. No personal data is accessible. Strict attention to data confidentiality in compliance with current database rules is applied. Data collection is performed by each center in a local version of the ECHSA-CHSD and subsequently send to the ECHSA-CHSD server for data processing and analysis.
A waiver of informed consent has been given according to the regulations of database studies [13].
The design of the study is a cross-sectional analysis. Inclusion criteria were determined as follows: congenital heart surgery procedures determined as a benchmark procedure (Tab. 1), collected in the ECHSA-CHSD from a Chinese or European Center during the time period between January 01, 2006 and December 31, 2018. STS-EACTS (STAT) mortality scores [14] were used to categorize procedures. Bubble Charts were used to show graphically the case load of each center, correlating to the size of each bubble, in relation to the complexity of the procedures and survival rate.
Table 1: Ten benchmark procedures
The data collected includes age, weight and length, gender, cardiac procedure type with STAT mortality category, cardiopulmonary bypass (CPB) time and aortic cross clamp (AoX) time, postoperative length of stay (PLOS), intermittent positive pressure ventilation (IPPV), 30-days mortality and operative mortality, the latter defined as 30-days mortality combined with hospital mortality.
Descriptive and inference statistical analysis was performed using IBM SPSS® Version 24 (IBM Armonk, NY: IBM Corp.). The significance level was chosen at α = 5%. Therefore, analysis resulting in p ≤ .05 are considered to be significant.
All age groups have been included, divided into subgroups: neonates (up to 28 days), infants (29 days to 1 year), children (1–12 years), adolescents (12–18 years) and adults with congenital heart disease (ACH) (above 18 years).
To describe basic characteristics, median, interquartile range and minimum and maximus were calculated for quantitative and continuous variables: age, weight, length, PLOS, length of stay in ICU, CPB time, AoX time were used. For categorical variables like gender, procedure type, 30-days mortality, percentage and frequency were used. To compare basic characteristics, Student’s T-test or Wilcoxon rank-sum test were used for continuous variables: age, weight, length, PLOS, length of stay in ICU, CPB time, AoX time and Fisher’s exact test for categorical variables: gender, 30-days mortality. Univariable logistic regression analysis was used to find predictors of 30-days mortality. Those variables that were statistically significant at the 10% level were introduced in a multivariable logistic regression model with backward selection. The results are presented as P-value, odds ratios and 95% confidence interval (not all data shown).
We identified all European (125) and Chinese (13) centers with surgical data submitted to the ECHSA-CHSD system from 2006 to 2018.
There were n = 82,181 procedures identified over the 13-year time period, with 23,920 (29.1%) from China and 58,261 (70.9%) from Europe. Subgroup analysis showed 47,680 (58.0%) male and 34,501 (42.0%) female patients. The median age at operation was 202 days (81–711.5). Most procedures occurred among infants, with 39,884 (48.5%) of procedures, followed by children with 24,960 (30.45%), neonates 13,309 (16.2%), adults 2,466 (3.0%) and adolescents 1,562 (1.9%). 94.2% of neonatal patients come from Europe.
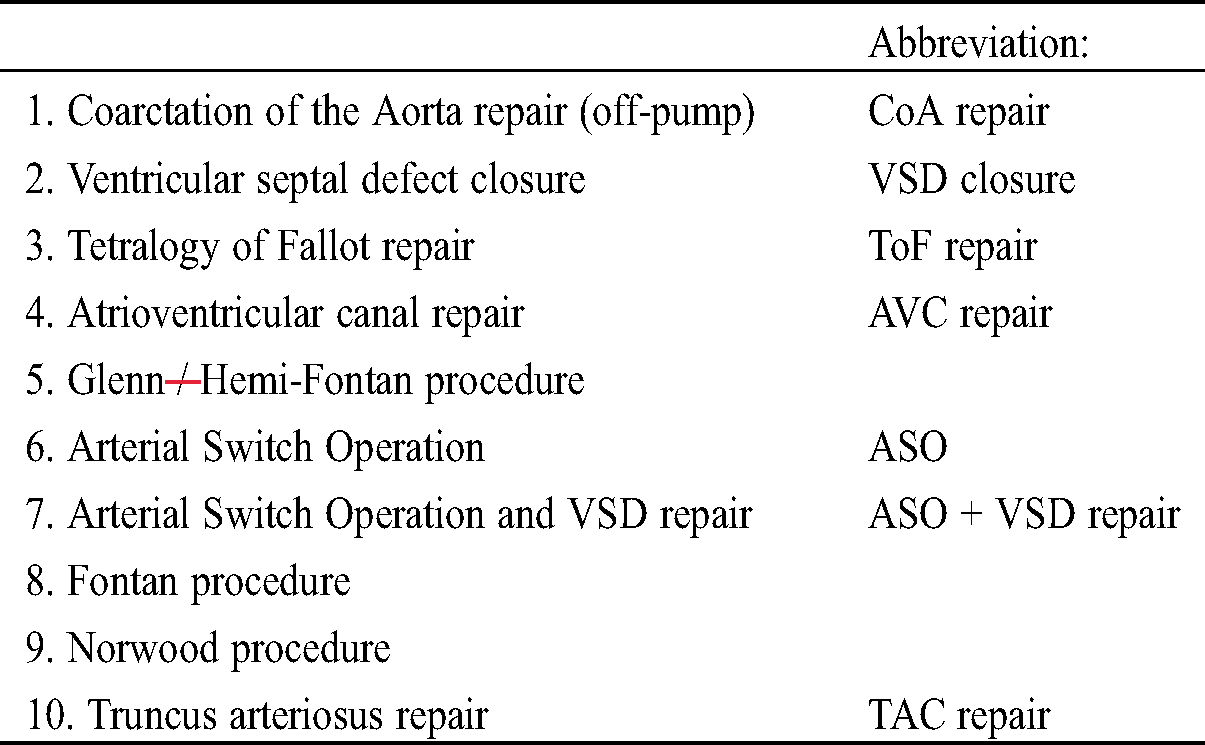
STAT Mortality Score vs. Hospital Survival in Europe and China is shown in Fig. 1. This demonstrates large centers in China with high caseloads and lower mean procedure complexity as well as some smaller centers with a wider spread of complexity. In Europe mean complexity and survival rate are nearly equivalent across centers.
Figure 1: STAT mortality score vs. hospital survival in Europe and China
There were different frequency distributions in benchmark procedures comparing Europe to China. In China, VSD repair represents about 70% of procedures, while Norwood operations comprised less than one percent of all pediatric cardiac surgical procedures (Fig. 2). In general, left heart lesions were rarely seen in China. Tab. 2 documents Operative Mortality, PLOS and Case Mix.
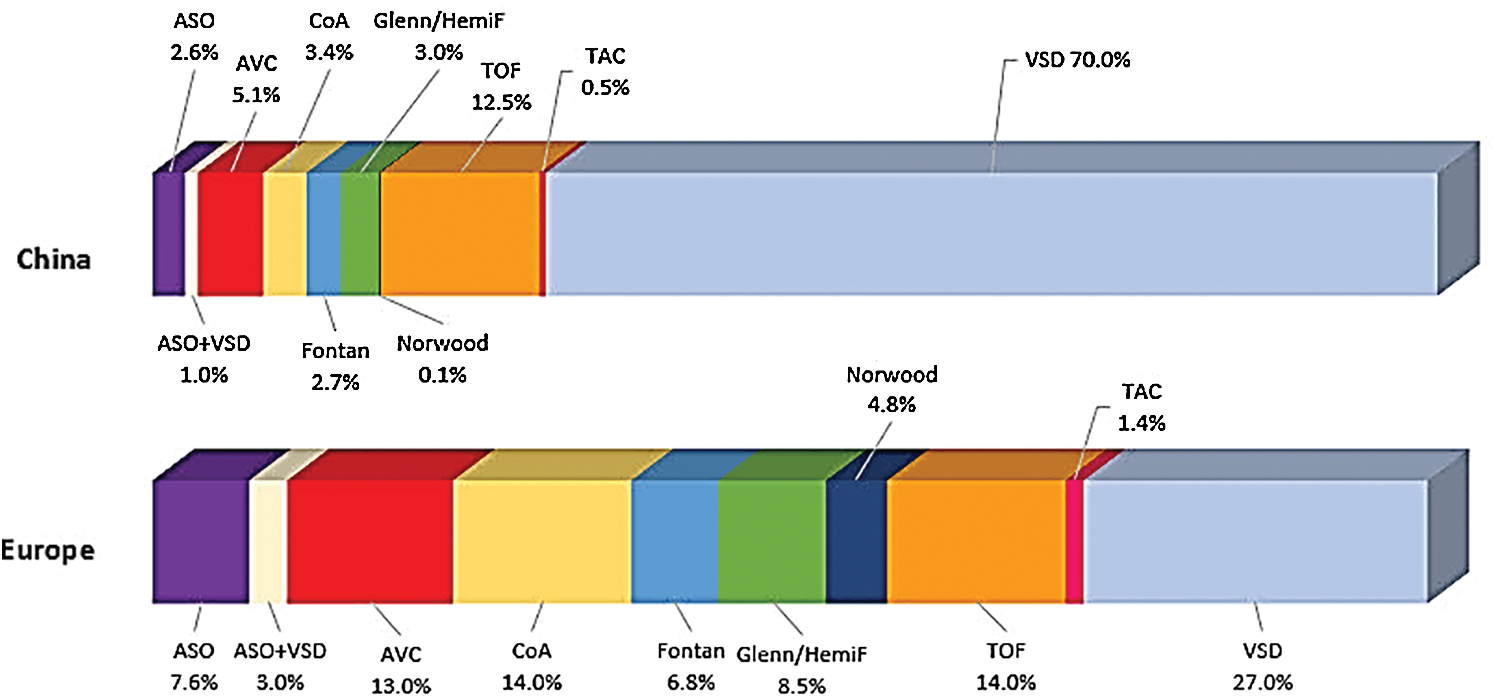
Figure 2: Procedure type percentage in Europe and China
Table 2: Comparison of number of operations, operative mortality and postoperative length of stay, of Europe and China for the ten benchmark operations
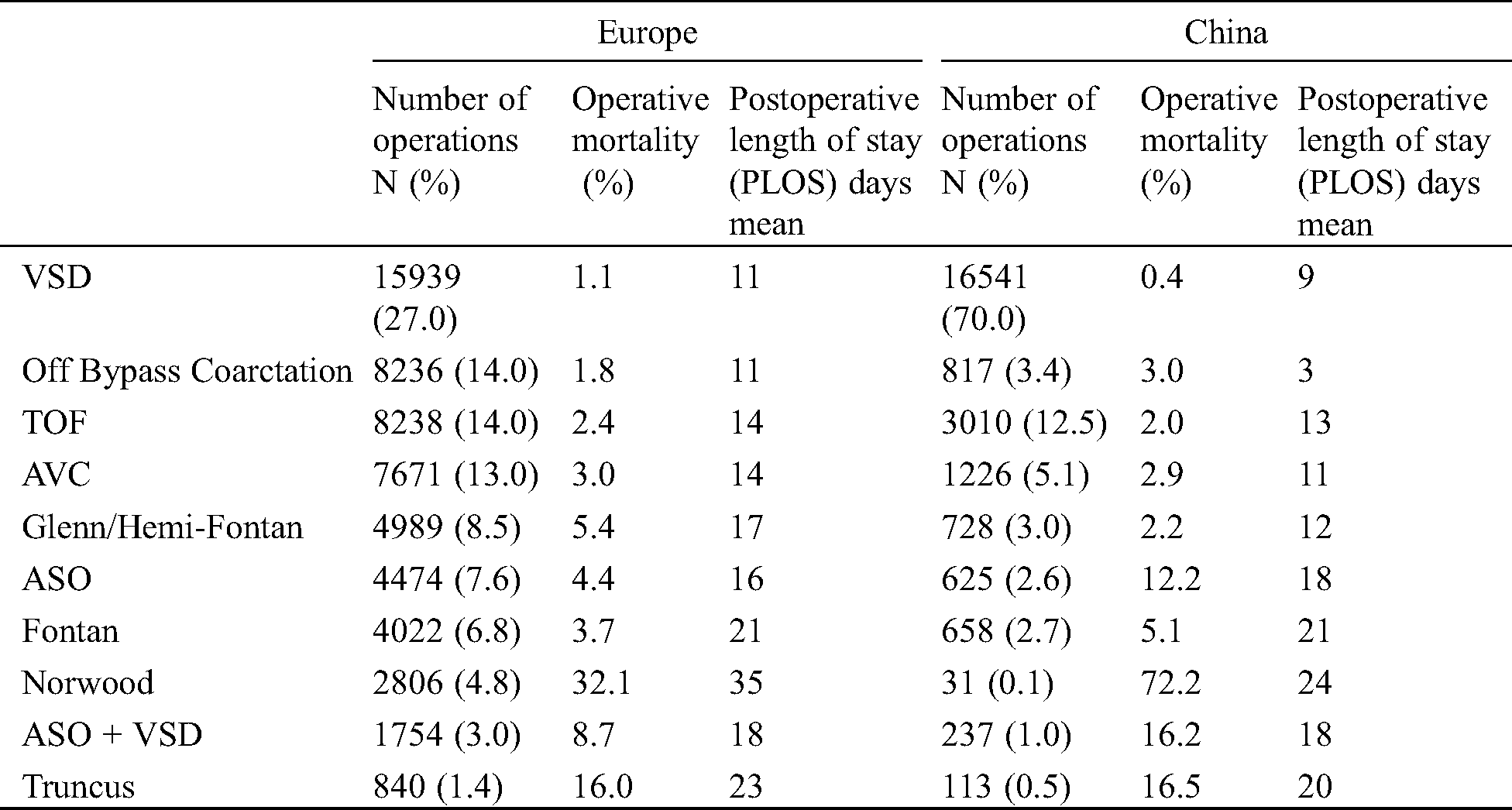
The high incidence of VSD repair as well as Tetralogy of Fallot repair corresponds with a low operative mortality rate with 0.4% in China. Neonatal procedures are rare in China. The Arterial Switch Operation and Arterial Switch Operation with VSD repair accounts for 2.6% and 1.0% of the benchmark operations in China vs. 7.6% and 3.0% in Europe, respectively. Operative mortality is lower in European countries compared to China at 4.4% vs. 12.2% for the Arterial Switch Operation and 8.7% vs. 16.2% for the Arterial Switch Operation with VSD repair, although there were no significant differences in PLOS time. The Norwood procedure in China is performed in 0.1% of all benchmark operations with an operative mortality of 72.2%. In Europe it accounts for 4.8% of all benchmark operations with an operative mortality of 32.1%. Similarly, the proportion of Glenn/Hemi-Fontan procedure was lower in China (8.5% vs. 3.0%) as well as the proportion of Fontan procedures (6.8% vs. 2.7%).
To sum up, operative mortality was significantly lower in Chinese centers for VSD closure, but significantly higher for other procedures. There was no significant difference in mortality following, Glenn and Fontan procedure, Atrioventricular Canal repair, Tetralogy of Fallot repair and Truncus arteriosus repair.
The median duration of CPB, AoX, IPPV and PLOS was significantly longer in China compared to Europe. Median weight, median age and operative mortality were significantly higher in China compared to Europe. Median patient age was 167 days in Europe and 325 days in China with 22% and 3.5% of neonates, respectively. Median patient weight was 5.8 kg in Europe and 8 kg in China.
Operative mortality decreased from 3.9% in 2006 to 1.6% in 2018 overall. This decrease was proportional higher in China, with a fall from 4.4% to 0.9% versus Europe with a drop of 4.0% to 2.5% (Fig. 3).
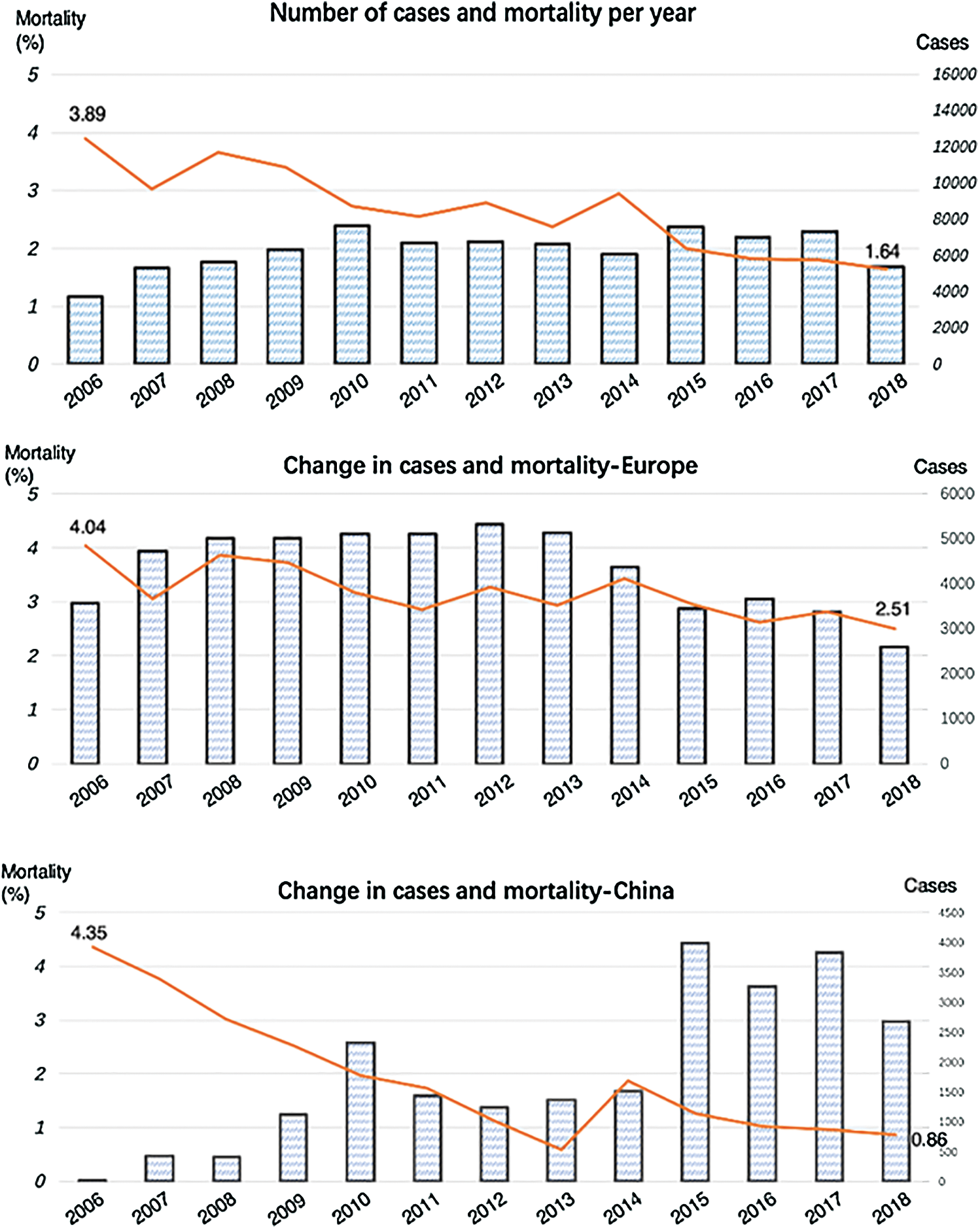
Figure 3: Number of cases and mortality per year for the whole cohort, Europe and China
Case load increased over this 13-year-period in China. After excluding VSD patients in the Chinese group, with an incidence of 70% and a mortality rate of 0.4%, the remaining procedures have a total mortality rate of about 2%. Mortality among neonates decreased from 9.2% in 2006 to 6.7% in 2018 in Europe and to 12.1% in China after a peak in 2014 of 23.5%.
Significant differences in mortality in STAT groups 1, 3 and 5 are seen comparing Europe and China. Chinese centers had lower mortality for procedures categorized as STAT 1, while European centers had lower mortality from procedures in STAT categories 3 and 5 (Fig. 4).
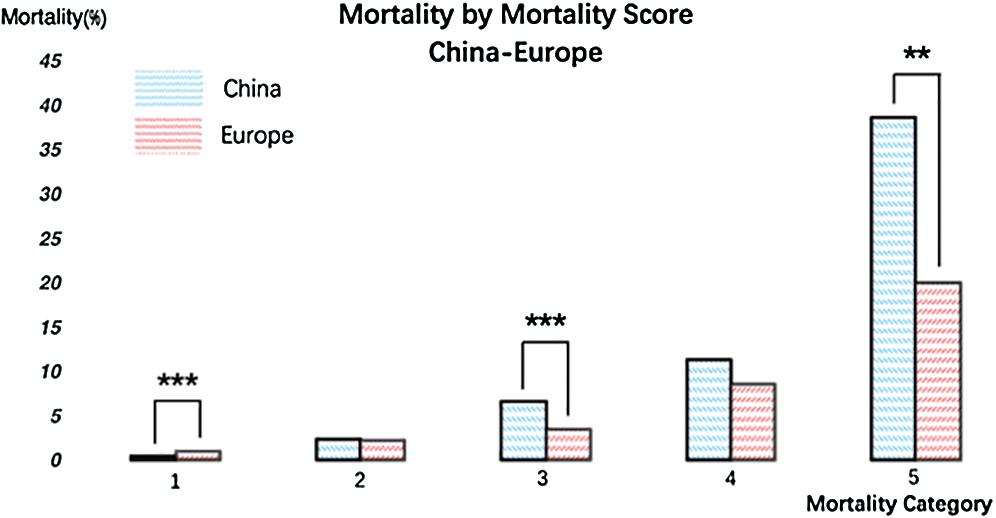
Figure 4: Mortality by STAT Mortality Category in China and Europe. **Weak significance, *** Strong significance
This ECHSA-CHSD study comparing European and Chinese centers over a time period of 13-years gives an overview of surgical patterns of practice for congenital heart disease repair in these countries. By including 125 European and 13 Chinese centers, almost one fourth of all procedures in China and an estimated third of all procedures for congenital heart disease performed in ECHSA-CHSD contributing countries in Europe could be evaluated. Participation in the European database is voluntary and only compulsory in the Netherlands and Poland. Regularly source data verification on a sample basis in participating centers verify completeness and accuracy of these data.
In almost the same area, China has twice the population as compared to Europe. The population distribution also greatly varies, ranging from some of the world’s most densely populated cities to vast rural areas. Most of the CHS centers are located in municipalities, provincial cities, and economic developed coastal cities, as the Chinese centers participating in this study. Differences in economic levels and medical insurance among the regions impact the treatment of patients with CHD [15].
The major finding of this study is that China is a country wherein development of pediatric cardiac surgery in general is in a different phase than in Europe. China is developing both regionally and as to the complexity and younger age of procedures [10]. Termination of pregnancy practices in China are totally different in relation to cardiac anomalies than they are in Europe [16]. At the same time Europe is remarkably heterogeneous per country. Many countries are in different phases of development and subsequent distribution of pediatric cardiac procedures and related results. Many eastern European countries are still catching up after decades of stagnation and poverty behind the Iron Curtain, while others suffer from the ravages of recent wars, such as the Balkan. Religion also plays an important role in the national identity of many countries, which precipitates also in termination of pregnancy practices. All of these historical and socio-economic factors can be sensed when examining the results of this study.
Due to the large number of different congenital cardiac procedures, we restricted this study to the ten benchmark procedures. This restriction made the data more compact and readily comparable. A clear difference in the distribution of frequencies of the ten benchmark procedures was shown. The Chinese data included significantly more VSD closures, while all other procedures were significantly less frequent when compared to European data.
The Norwood procedure accounts for less than 1% of procedures in China. Previous ECHSA-CHSD reports demonstrated that the proportion of children with functionally univentricular hearts among those with congenital heart disease differs in European countries as well—from 6.8% in France to 16.5% in Germany [17]. Norwood procedures, for example, account for 2.7% [17] of all congenital heart operations among neonates in France. On the other extreme the Norwood operation is the most frequent neonatal cardiac procedure in Poland (12.7%) [17]. In Poland every third neonate who had an operation for a congenital heart defect had a functionally single ventricle heart, which may be attributed to their religious identity and subsequent policy in relation to termination of pregnancy. Operative mortality was significantly lower for the Norwood Procedure in Europe than in China, potentially attributed to the frequency with which the procedure is performed in both locations. A previous study describes a higher mortality rate observed at lower volume centers may be related to a higher mortality rate in those with postoperative complications. This association was most prominent in those in the higher surgical categories [18], where the Norwood Procedure belong to.
VSD closure is the most common procedure in China (70%) with an operative mortality rate of less than 0.4%. In contrast, VSD closure counts for 27% in Europe and an operative mortality rate of 1.1%. There is an indication that experience and practice influence mortality rate.
Neonatal cardiac procedures are performed less frequently in China than in Europe, accounting for 3.5% of all benchmark procedures versus 22% in Europe. In contrast to European countries, some societal policies and key factors may affect the occurrence. For example, there are no official legal regulations for abortion in China. Although in European countries abortion regulations do exist, they have a broad variety per country. In recent years, prenatal CHD diagnoses are increasing, with diagnostic methodologies keep improving in all countries [7]. When a pregnant woman is told that her fetus may suffer from congenital heart disease, doctors can only give advice in full consideration of her gestational week and severity of the cardiac anomaly. Whether or not to retain the fetus entirely depends on the national regulations and the parent’s decision. In China pregnant women may choose to abort, even in the third trimester. Due to both, growing prenatal diagnosis [19] and high abortion rate, the spectrum of congenital heart disease is changing in China. The incidence of some congenital heart disease that is easily diagnosed by fetal echocardiography such as Tetralogy of Fallot and Transposition of Great Arteries, decreased by nearly 50% during recent decades in China. Single ventricle is also regarded as “fatal disease” after birth, so termination of pregnancy is recommended in China. As a result, the abortion rate in China is higher than that in most of Europe [19].
Congenital heart surgery outcomes in Europe and China have improved during the last decade. Nevertheless, the results of early life treatment differ between Europe and China as well as between various European countries and different regions in China. The variety of medical and economic levels, as well as health care insurance in different regions may have a major impact on the incidence and the treatment possibilities and practices of congenital heart disease [20].
The intent of this article is to obtain a general overview of patterns of practice between Europe and China as a base for future bilateral collaborations for quality improvement. The dataset used for this article contains aggregated data from various countries in Europe and China. The countries submitting data represents a geographic, economic, developmental and cultural variation. The present analysis is limited to operative mortality, which includes 30-days mortality and in-hospital mortality. Data on long-term follow-up is not available. There is a need to implement follow-up tools into databases.
To conclude, in general, participating Chinese centers have higher programmatic volume and European centers have a more complex case mix. Palliation for patients with functionally univentricular heart is performed less commonly in China. Procedures performed more frequently, including VSD closure and TOF repair have low mortality in China.
The comparison of patterns of practice and outcomes demonstrate opportunities for continuing bidirectional transcontinental collaboration and quality improvement. Further studies could focus on differences based on these results and evaluate in detail variations in surgical techniques, patient care, processes and training.
Funding Statement: The authors received no specific funding for this study.
Conflict of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Maruszewski, B., Tobota, Z. (2002). The European Congenital Heart Defects Surgery Database experience: Pediatric European Cardiothoracic Surgical Registry of the European Association for Cardio-Thoracic Surgery. Seminars in Thoracic and Cardiovascular Surgery: Pediatric Cardiac Surgery Annual, 5(1), 143–147. DOI 10.1053/pcsu.2002.29714. [Google Scholar] [CrossRef]
2. European Congenital Heart Surgeons Association Congenital Database (2020). www.echsacongenitaldb.org. [Google Scholar]
3. Worldometer. 2020). (. www.worldometers.info. [Google Scholar]
4. Worldbank. (2020). Fertility rate (2017). https://data.worldbank.org/indicator. [Google Scholar]
5. Eurostat. (2020). https://ec.europa.eu/eurostat/statistics-explained/index.php/Fertility_statistics. [Google Scholar]
6. Worldbank. (2020). Birth rate (2017). https://data.worldbank.org/indicator. [Google Scholar]
7. van der Linde, D.,Konings, E. E., Slager, M. A., Witsenburg, M., Helbing, W. A. et al. (2011). Birth prevalence of congenital heart disease worldwide: A systematic review and meta-analysis. Journal of the American College of Cardiology, 58(21), 2241–2247. DOI 10.1016/j.jacc.2011.08.025. [Google Scholar] [CrossRef]
8. Cooley, D. A. (1997). Early development of congenital heart surgery: Open heart procedures. Annals of Thoracic Surgery, 64(5), 1544–1548. DOI 10.1016/S0003-4975(97)01025-4. [Google Scholar] [CrossRef]
9. Chong, L., Fitzgerald, D. A., Craig, J. C., Manera, K. E., Hanson, C. S. et al. (2018). Children’s experiences of congenital heart disease: A systematic review of qualitative studies. European Journal of Pediatrics, 177(3), 319–336. DOI 10.1007/s00431-017-3081-y. [Google Scholar] [CrossRef]
10. Zhang, H. B. (2019). Congenital Cardiac Surgery in China: History, Achievements and Challenges, Presented at the Joint Meeting of the European Congenital Heart Surgeons Association (ECHSA) and the World Society for Pediatric and Congenital Heart Surgery (WSPCHS) in Sofia, Bulgaria. [Google Scholar]
11. Mavroudis, C., Jacobs, J. P. (2000). International congenital heart surgery nomenclature and database project. Annals of Thoracic Surgery, 69(3), 1–372. DOI 10.1016/S0003-4975(99)01278-3. [Google Scholar] [CrossRef]
12. Franklin, R. C., Jacobs, J. P., Krogmann, O. N., Béland, M. J., Aiello, V. D. et al. (2008). Nomenclature for congenital and paediatric cardiac disease: Historical perspectives and the International Pediatric and Congenital Cardiac Code. Cardiology in the Young, 18(S2), 70–80. DOI 10.1017/S1047951108002795. [Google Scholar] [CrossRef]
13. Dokholyan, R. S., Muhlbaier, L. H., Falletta, J. M., Jacobs, J. P., Shahian, D. et al. (2009). Regulatory and ethical considerations for linking clinical and administrative databases. American Heart Journal, 157(6), 971–982. DOI 10.1016/j.ahj.2009.03.023. [Google Scholar] [CrossRef]
14. O’Brien, S. M., Clarke, D. R., Jacobs, J. P., Jacobs, M. L., Lacour-Gayet, F. G. et al. (2009). An empirically based tool for analyzing mortality associated with congenital heart surgery. Journal of Thoracic and Cardiovascular Surgery, 138(5), 1139–1153. DOI 10.1016/j.jtcvs.2009.03.071. [Google Scholar] [CrossRef]
15. Mo, X., Yu, D., Shu, Q. (2019). Pediatric heart surgery in China: Progress and challenges. World Journal of Pediatric Surgery, 2(1), e000048. DOI 10.1136/wjps-2019-000048. [Google Scholar] [CrossRef]
16. Bearak, J., Popinchalk, A., Ganatra, B., Moller, A. B., Tunçalp, Ö. et al. (2020). Unintended pregnancy and abortion by income, region, and the legal status of abortion: Estimates from a comprehensive model for 1990-2019. Lancet Global Health, 8(9), e1152–e1161. DOI 10.1016/S2214-109X(20)30315-6. [Google Scholar] [CrossRef]
17. European Congenital Heart Surgeons Association Congenital Database. (2016). Data Presented during the 6th Scientific Meeting of the World Society for Pediatric and Congenital Heart Surgery in Orlando, USA. www.echsacongenitaldb.org. [Google Scholar]
18. Pasquali, S., Li, J. S., Burstein, D., Sheng, S., O’Brien, S. et al. (2012). Association of center volume with mortality and complications in pediatric heart surgery. Pediatrics, 129(2), e370–e376. DOI 10.1542/peds.2011-1188. [Google Scholar] [CrossRef]
19. Chu, C., Yan, Y., Ren, Y., Li, X., Gui, Y. (2017). Prenatal diagnosis of congenital heart diseases by fetal echocardiography in second trimester: A Chinese multicenter study. Acta obstetricia et gynecologica Scandinavica, 96(4), 454–463. DOI 10.1111/aogs.13085. [Google Scholar] [CrossRef]
20. Musa, N., Hjortdal, V., Zheleva, B., Murni, I. K., Sano, S. et al. (2017). The global burden of pediatric heart disease. Cardiology in the Young, 27(S6), S3–S8. DOI 10.1017/S1047951117002530. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |