
 | Congenital Heart Disease | 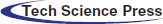 |
DOI: 10.32604/CHD.2021.014628
ARTICLE
Higher Child-Reported Internalizing and Parent-Reported Externalizing Behaviors were Associated with Decreased Quality of Life among Pediatric Cardiac Patients Independent of Diagnosis: A Cross-Sectional Mixed-Methods Assessment
1Children’s Hospital of Eastern Ontario Research Institute, Ottawa, Canada
2Faculty of Health Science, University of Ottawa, Ottawa, Canada
3Faculty of Medicine, University of Ottawa, Ottawa, Canada
4Children’s Hospital of Eastern Ontario, Ottawa, Canada
5The Hospital for Sick Children, Toronto, Canada
*Corresponding Author: Patricia E. Longmuir. Email:plongmuir@cheo.on.ca
Received: 13 October 2020; Accepted: 20 January 2021
Abstract: Background: Pediatric cardiology patients often experience decreased quality of life (QoL) and higher rates of mental illness, particularly with severe disease, but the relationship between them and comparisons across diagnostic groups are limited. This mixed-methods cross-sectional study assessed the association between QoL anxiety and behavior problems among children with structural heart disease, arrhythmia, or other cardiac diagnoses. Methods: Children (6–14 years, n = 76, 50% female) and their parents completed measures of QoL (PedsQL), behavior (BASC-2, subset of 19 children) and anxiety (MASC-2, children 8+ years). Pearson correlations/regression models examined associations between QoL, behavior and anxiety, controlling for age, sex, diagnosis and condition severity. Student t-tests compared results to published normative values. Semi-structured interviews (15 children, 13 parents) examined self- and parent-reported perceptions of the patient’s emotional health. Results: Child reported social QoL (95% CI difference: −11.0, −2.1), emotional well-being (95% CI difference: −12.5, −3.8) and adjustment skills (95% CI difference: −13.9, −3.0) were significantly below published norms (p < 0.05). Neither age, sex, nor diagnosis were significantly related to questionnaire responses. Compared to children with mild conditions, child and parent-reported QoL was significantly lower in children with complex conditions (np2 ≥ 0.14, p < 0.05). Lower QoL was strongly associated with more internalizing problems based on both child (r = −0.78, p < 0.001) and parent (r = −0.67, p < 0.001) reports. Interview responses suggested emotional distress was attributed to “normal” child problems rather than the child’s cardiac problem. Conclusion: Children with complex cardiac conditions, regardless of diagnosis, had diminished QoL. Using the PedsQL in clinical settings may help identify pediatric cardiology patients experiencing emotional distress (i.e., anxiety and depression).
Keywords: Anxiety; emotional well-being; internalizing behaviors; congenital heart defects; arrhythmia; cardiomyopathy
Children living with cardiac diagnoses can experience functional impairments, parental restrictions of activity, extensive medical treatment, and social stress, all of which can have a significant, negative impact on their quality of life (QoL) [1]. As more children are surviving through adulthood with pediatric cardiac diagnoses [2], there is an increasing need to understand and address their psychosocial health. Research indicates children have a greater risk of emotional distress and/or reduced QoL if they live with congenital heart disease [1,3] (i.e., changes to the heart’s structure) or inherited arrhythmia syndromes or cardiomyopathies [4]. However, previous research examined emotional distress and QoL independently, leaving the relationship between them largely anecdotal. One study among adolescents and young adults (12 to 20 years) with cardiac disease (106 moderate to severe congenital heart diagnoses, 8 Kawasaki disease, cardiomyopathy or arrhythmia) did report that lower disease-specific QoL, limited understanding of the cardiac diagnosis and a lack of social support were associated with higher levels of anxiety and depression [5]. However, such measures of health-related QoL are more often reflective of perceived health status (i.e., presence of disease) and may not capture salient changes in overall well-being [6]. Thus, the relationship between overall QoL and emotional distress remains unclear, particularly among younger children, those with non-congenital diagnoses and with simple as well as more complex conditions.
Psychosocial assessments among pediatric populations typically rely on parent-proxy reports because children, depending on age and/or cognitive understanding, are often assumed to be unable to competently answer for themselves [7,8]. While parent reports can be useful for detecting problems in psychological adjustment [3], significant differences between parent and child reports have been recognized; particularly for internalizing problems that cannot be easily observed [9]. Indeed, parent reports tend to identify social and behavior problems, while child self-reports indicate more frequent symptoms of depression compared to healthy peers [10]. It is therefore important to examine both child self- and parent-proxy reports to obtain a comprehensive characterization of the child’s QoL and emotional health.
The purpose of this study was to describe and compare the QoL and emotional health of children across a broad range of cardiac diagnoses, while controlling for age, sex, and severity of disease. Specifically, we sought to examine the association between a brief assessment of overall QoL and more in-depth assessments of emotional health. We hypothesized that QoL would be highly associated with emotional health, making the brief assessment a suitable clinical tool for screening pediatric cardiac patients for emotional distress. Finally, since there is often stigma surrounding mental health, we sought to understand the perceptions of children whose questionnaire responses indicated higher levels of behavior problems or anxiety and the concerns of their families with regards to their emotional health as well as the types of support desired.
An explanatory-sequential, mixed methods design was used to examine QoL and emotional health among children living with a wide variety of cardiac diagnoses. The Research Ethics Boards of both institutions approved this prospective cross-sectional study (The Hospital for Sick Children, Toronto, REB#1000020209; Children’s Hospital of Eastern Ontario, Ottawa, REB #13/63X).
Study participants have been previously described by Patel et al. [9] and were recruited from two large pediatric centers (Toronto and Ottawa, Canada). Pediatric cardiology patients, 6 to 14 years of age, with a Congenital Heart Defect (CHD), arrhythmia disorder, cardiomyopathy (diagnosed or family history), or infectious heart disease (i.e., endocarditis, rheumatic heart disease, Kawasaki’s disease) were eligible. Patients were excluded for acute changes to health status, interventions within the previous 6 months, cognitive disability, or if the child or parent did not speak English or French. The responsible cardiologist provided permission to approach each family. Parents provided written informed consent and children provided verbal assent. Severity classification for patients with CHD used the AHA 2008 Guidelines [11]. Participants with arrhythmia, cardiomyopathy and infectious heart disease were classified by severity based on cardiologist expertise.
Three standardized instruments, measuring quality of life, anxiety and behavior, were completed as child and parent reports (Tab. 1).
Table 1: Description of study assessments
Parents and children completed the study questionnaires independently during their clinic visit, with children assisted by the researcher as required. MASC-2 and BASC-2 scores were reviewed by a clinical psychologist (Dr. G Goldfield (CHEO) and Dr. R. Sananes (SickKids)) to identify children whose scores were in the “elevated” or “clinical” range. None of the participants had clinically significant scores requiring immediate referral to psychiatric support. Children identified as having elevated, but not clinically defined levels of psychosocial stress and their parents were invited to participate in semi-structured interviews. Parents were interviewed without their child present. Children had the choice to complete the interview with the researcher alone, or to have their parent present. Interviews were conducted by three members of the research team (PEL, JJ, BP).
Separate analyses were completed for each outcome (PedsQL, BASC-2, and MASC-2 questionnaires). One sample t-tests compared questionnaire responses to published healthy norms. The impact of age, sex, diagnosis and severity on each measure was assessed through regression analyses with backwards variable selection. Given the small correlation between diagnosis and severity (r = 0.34), both were included in multi-variable models. Parent-reported internalizing problems differed between sites (p = 0.03); as such, site remained a mandatory covariate in all models. Only univariate analyses were done for child BASC-2 scores due to the limited sample size. Finally, Pearson correlations examined the associations between PedsQL total and subdomain (physical, emotional, social, school) scores and the BASC-2 and MASC-2 measures reported separately by parents and children. Sensitivity and specificity analyses were performed for QoL scores that demonstrated strong correlations with BASC-2 and MASC-2 measures. Cut points were calculated using 1 standard deviation below the mean for the PedsQL and 1 standard deviation above the mean for the BASC-2 and MASC-2. Sensitivity and specificity analysis were not performed for child-reported BASC-2 scores since only a small number of children (n = 19) completed the measure.
Audio recordings from the semi-structured interviews were transcribed verbatim by JL, and then verified by PEL. Braun and Clarke’s six steps for thematic analysis [15] were implemented including becoming familiar with the data; generating initial codes; searching for potential themes; reviewing themes; defining and naming themes; and producing the report with examples. The qualitative research component was intended to explain any perceived emotional distress and identify relevant sources of support, thus providing further context to the instrument scores. A deductive analytic approach was used to generate initial codes and identify relationships within the pre-determined framework of perceived emotional health and desired sources of support. Selective coding and situational analyses integrated categories and relationships into overall explanatory themes.
A review of future clinic appointments identified 430 children meeting the study age criteria. The responsible cardiologist provided permission to approach 251 children considered eligible for study participation. During a clinic visit, 186 of the 251 eligible patients were approached with 96 (52%) being enrolled (90 families (48%) declined participation). The final sample included 76 children (50% female) and 76 parents (n = 50 female, n = 16 male, n = 10 not specified) as 20 enrolled families did not return completed questionnaires. Participating children and parents are described in Tab. 2.
Table 2: Description of Participating Children and Parents

3.2 Child Reported Quality of Life and Emotional Health
Children with less severe conditions had significantly QoL compared to children with complex conditions (Tab. 3). Physical and school QoL were better among children with mild and moderate conditions. There was no effect of disease severity on emotional or social QoL. Age, sex, diagnosis, and study site were not significantly associated with PedsQL, behavior (BASC-2), or anxiety (MASC-2) scores.
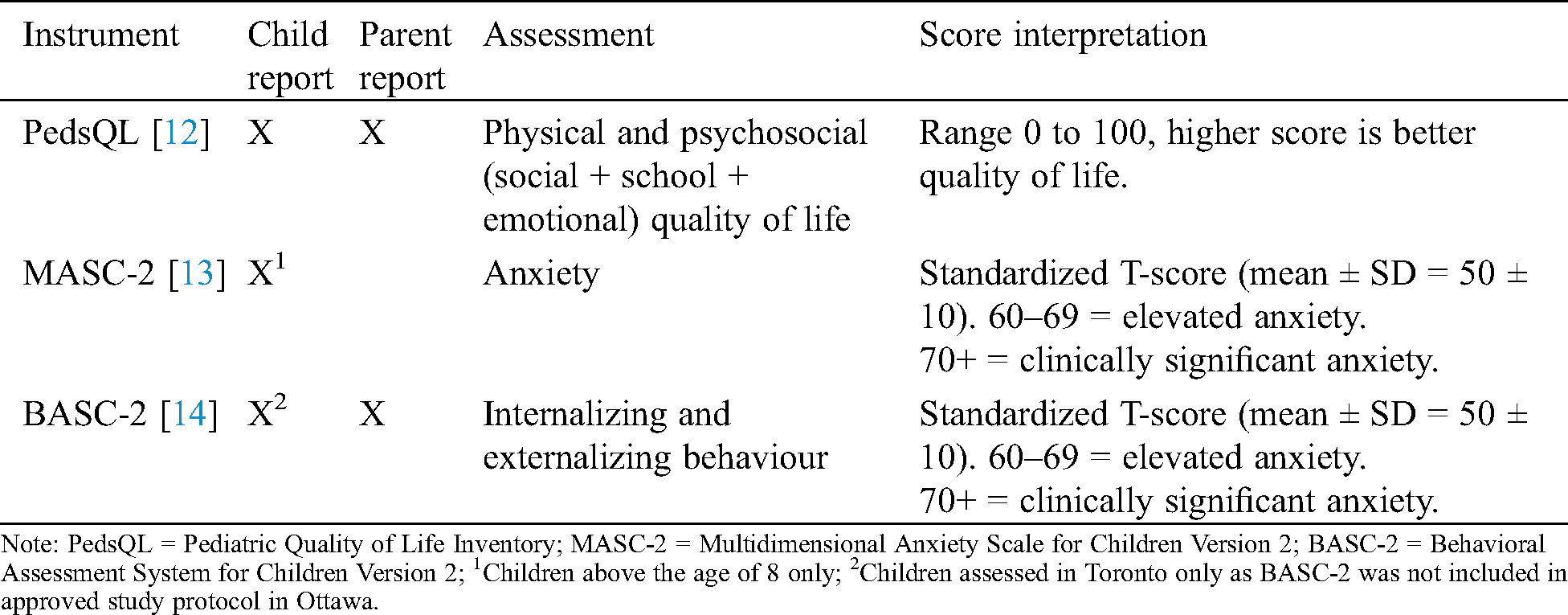
Compared to self-reported norms for healthy children [12], children in this study reported significantly lower psychosocial QoL (Fig. 1), with the largest differences among children with complex conditions (p < 0.004). Children reported that their anxiety (MASC-2) was similar to normative values (mean difference = 0.2 ± 1.20 p = 0.84) while they reported significantly more emotional symptoms (mean difference = 6.6 ± 2.31, p = 0.01) and weaker adjustment skills (mean difference = 8.5 ± 2.60, p = 0.004, Fig. 2). Child-reported QoL explained 30% to 60% of the variance in the standardized assessments of behavior and anxiety.
Table 3: Influence of patient characteristics on measures of emotional health and quality of life

3.3 Parent Reported Quality of Life and Emotional Health
Age, sex, and diagnosis were not significantly related to parent proxy reports of their children’s QoL or behavior (Tab. 3). Parents of children with complex conditions reported significantly lower QoL and weaker adaptive skills compared to parents of children with mild conditions (Tab. 3). Parents of children with mild conditions assessed in Ottawa reported significantly fewer internalizing (p < 0.001) and behavioral symptoms (p < 0.001) than parents of children with more severe disease (Tab. 3). In Toronto, disease severity was not related to parent BASC-2 scores. Sensitivity analyses were then performed because 85% (28/33) of patients assessed in Toronto had congenital heart disease compared to only 19% (8/43) of patients assessed in Ottawa. Differences by site were unchanged when analyzing data from only children with congenital heart disease at each site (p < 0.01).
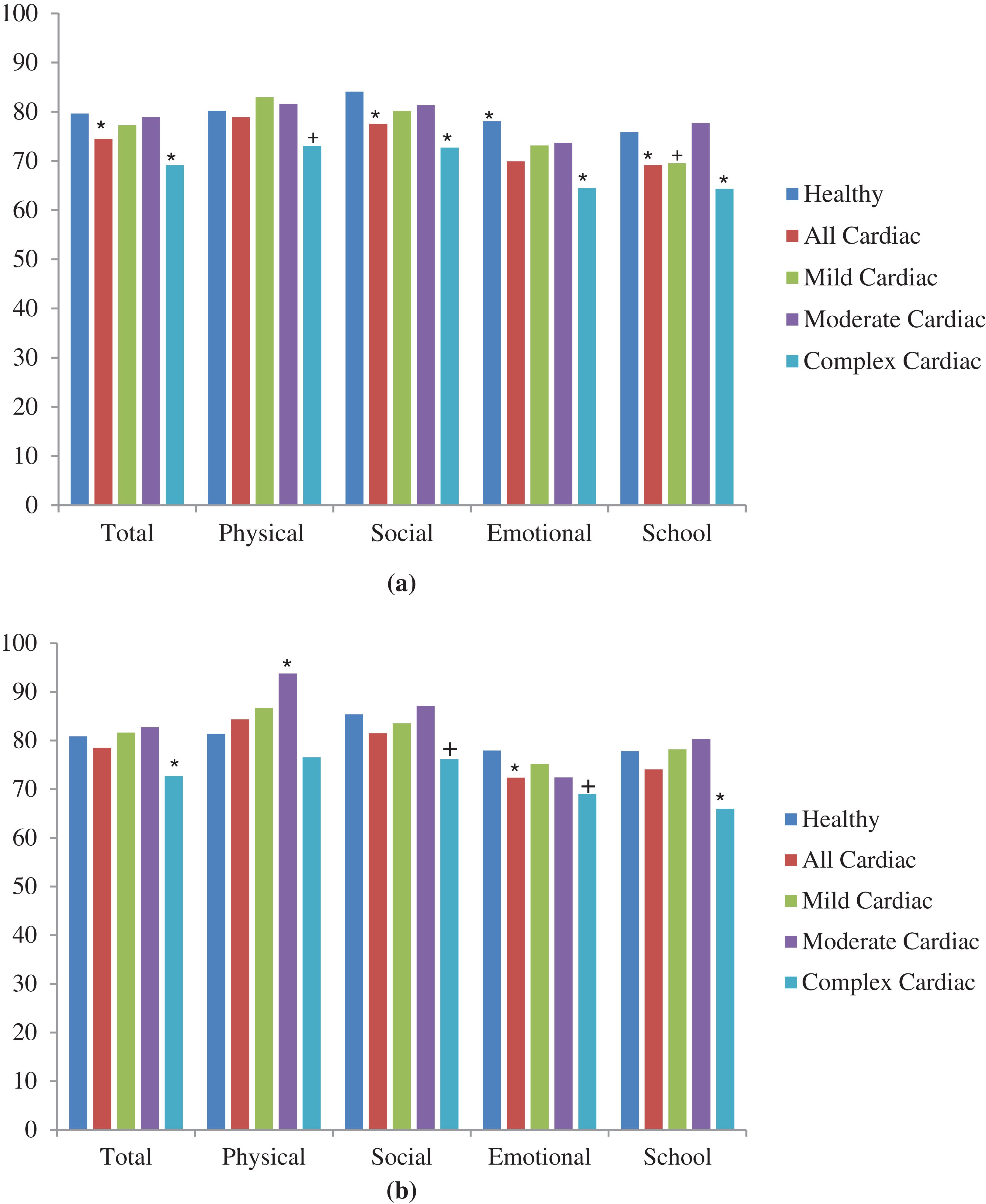
Figure 1: Quality of life among cardiac patients relative to normative data for healthy children. (a) Child-report PedsQL and (b) Parent-proxy PedsQL.
Compared to parent proxy-reported norms for healthy children, parents of children with cardiac diagnoses reported lower emotional QoL (Fig. 1) and more internalizing problems (Fig. 2). Parents of children with complex conditions reported lower total QoL (mean difference = 7.5 ± 2.95, p = 0.01), more internalizing behaviors (mean difference = 8.2 ± 1.86, p < 0.001), more behavioral symptoms (mean difference = 6.5 ± 2.04, p = 0.004) and weaker adaptive skills (mean difference = 4.8 ± 2.26, p = 0.05) than data reported by parents of healthy children. Parent-reported psychosocial QoL explained 14% of the variance in BASC-2 scores and 30% to 42% of the variance in internalizing behavior and adaptive skill scores.
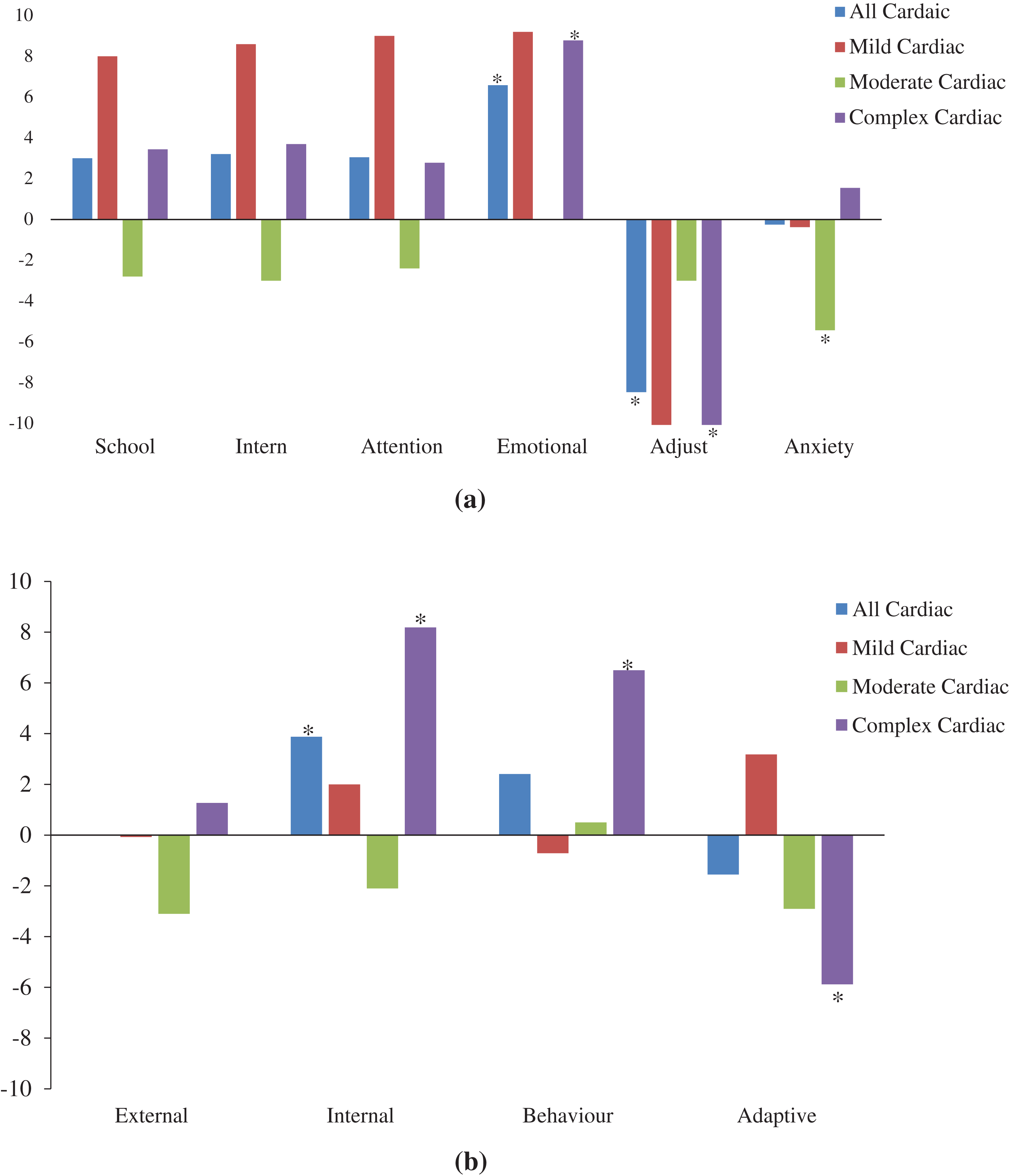
Figure 2: Children with cardiac diagnoses have more emotional distress and fewer adaptive skills than healthy children. a) Child-reported anxiety (MASC-2) and behavior (BASC-2) scores and b) Parent-proxy reported behavior (BASC-2) scores.
3.4 Correlation of Quality of Life with Emotional Health
Correlations between child and parent-reported QoL and the MASC-2 and BASC-2 measures are shown in Tab. 4. Lower PedsQL scores had the strongest correlation with greater child and parent-reported internalizing behaviors on the BASC-2, (r = −0.78, p < 0.001 and r = −0.67, p < 0.001, respectively). Sensitivity and specificity of the PedsQL to identify internalizing behaviors of potential concern, using parent-reported scores of 1 standard deviation below and above the means, were 55% and 88%, respectively.
Table 4: Correlations between quality of life and emotional health measures as reported by children and parents

A subset of 15 children (6 female, mean age = 11.3 ± 2.5) and 13 parents (11 female) participated in brief semi-structured interviews about their emotional health and desired sources of support. Patients included 6 children with congenital heart defects, 6 children with arrhythmia, and 3 children with cardiomyopathy. The severity of their cardiac condition was mild (n = 6), moderate (n = 3), or complex (n = 6). Five parents (42%) and three children (20%) indicated no problems with emotional health during the interview, despite being selected for an interview on the basis of elevated MASC-2 or BASC-2 scores.
Parents reported that children did not enjoy having limitations due to their heart, such as “wanting a new heart to participate like the other kids”, but also that their child’s cardiac treatment did not negatively affect their emotional health. Among parents (62%) and children (80%) who indicated experiences of emotional distress during the interview, the source was primarily identified as “normal” child/teenager problems. For example, “fears that a typical six year old would have but no anxiety related to his heart condition for sure” or “He has had it fixed forever. It’s almost like normal.” Only two children (13%) reported that they worried about their heart. One was worried because “it helps my body live” and the other said “what happens if the muscle gets too big”?
Most children (73%) and all parents acknowledged that when feeling worried or sad the child preferred to be alone. For example, one parent explained: “He detaches himself from people, it is his way of pretty much saying, I do not want to have to deal with people.” Children and parents also identified that distractions, such as watching TV, were common ways of coping. One parent described the treatment course for his/her child’s anxiety, noting learned breathing techniques as a helpful strategy. Parents identified their children’s cardiologists as effective sources of support, citing their ability to address their children’s “fears and apprehensions and put them right at ease.” Parents also indicated that having a combination of individual and family resources as well as support groups would be helpful for their child. From the children’s perspectives, friend/social groups were a helpful source of support. One participant mentioned her desire for “clubs and activities” where children facing similar life challenges could connect, relating her experience with one friend who also had a rare medical condition.
Overall, our sample of children and their parents reported lower QoL and increased behavior or anxiety problems when compared to published norms for healthy children. Children with mild/moderate conditions were more comparable to healthy peers, whereas children with complex conditions reported lower QoL and more internalizing behaviors (e.g., depression, anxiety) regardless of the type of cardiac diagnosis. Age, sex and type of cardiac diagnosis were not related to QoL or internalizing or externalizing behaviors. These findings support the need to examine psychosocial health among all pediatric cardiology patients with moderate to complex diagnoses. Since lower QoL was strongly related to greater child and parent-reported internalizing problems, the PedsQL may have potential as a screening tool among this population for identifying children who may benefit from additional emotional health support.
Despite the small sample size, our QoL results were similar to those reported in larger studies [16] among children with congenital heart defects (PedsQL = 74.5 ± 15.12), suggesting that study participants were representative. Our behavior and anxiety findings are also similar to higher rates of lifetime psychiatric diagnoses among children with congenital heart defects [17], as well as an increased risk of internalizing behaviors, such as anxiety and depression, and externalizing behaviors, such as hyperactivity and aggression [18–20]. Young children with congenital heart defects have emotional health comparable to healthy peers [21], suggesting emotional distress may increase with age and perhaps reflecting children’s developmental understanding of their cardiac condition. The current study extends this knowledge to include children with mild to moderate cardiac conditions [22] and those with a variety of cardiac diagnoses [3] (e.g., congenital health defects, arrhythmia, cardiomyopathy).
Our examination of QoL and emotional health among the same children and at the same point in time enables a greater understanding of the relationship between these variables, and the important association between internalizing behaviors (e.g., anxiety, depression) and QoL. Results suggest that the severity of the cardiac condition, rather than the type of cardiac diagnosis, is the most reliable indicator of an increased risk for emotional distress and decreased QoL. Similar results have previously been identified among young children [21] and adults [23] with congenital heart disease. Lower QoL among children with more severe cardiac diagnoses was primarily attributed to deficits in the physical and school PedsQL sub-domains, reflecting decreased academic and activity competencies reported among children with complex congenital heart disease [24]. Missing school due to illness or medical appointments or neurodevelopmental deficits resulting from cardiopulmonary bypass exposure have been hypothesized as the cause of these deficits [25].
Child and parent interviews attributed emotional distress to “normal” child/teenager problems. These findings reinforce the importance of looking beyond the cardiac diagnosis. Adolescents with congenital heart defects have reported being perceived as “different” [26,27], and the desire for meaningful, social connections could be why peer gatherings to connect children living with heart disease were suggested as potentially helpful sources of support. Interestingly, the stated desire for peer support differed from the preferred coping mechanism (solitude). These findings suggest that more social, or “approach-based” coping mechanisms are desired and should be facilitated, given that more avoidant coping behaviors (i.e., seclusion) have been associated with poor mental health outcomes through adolescence [28].
Unlike previous reports of higher anxiety among those with congenital heart disease [29–31], we found no difference between children’s self-reported anxiety and data reported for healthy children. These differences may reflect differences in participants’ age, as previous studies focused on older adolescents. Research among children with congenital heart defects has also reported that QoL decreases with increasing age [29,30,32]. In this study, condition severity but not age was significant in the multi-variable model. “Age-related” changes in QoL or emotional health may be a proxy measure for condition severity, given that heart function may deteriorate with increasing age in some diagnostic groups. The lack of influence of age on measures of QoL or emotional health may also have been influenced by the relatively homogenous ages of our study participants (70% were 8–12 years of age).
Participants in this study were uniquely representative of the range of diagnoses found within the pediatric cardiac population. Most patients seen in pediatric cardiac clinics in western society have congenital heart disease, which were only 47% of the study participants. The higher proportion of participants with other types of pediatric cardiac disease in this study enabled novel analyses between diagnostic groups assessed with the same methods in the same study. The main limitation of this study was that the BASC-2 was difficult for children to complete, and as such the behavioral assessment among children with cardiac diagnoses occurred in only a small sub-sample (10 girls and 9 boys). Interviews to obtain more context surrounding the emotional health perceptions of children living with heart disease provided unexpected insights in that elevated BASC-2 or MASC-2 scores were not attributed to the children’s cardiac condition.
This study provides novel information about the association between QoL and emotional health among children with mild, moderate and severe congenital heart, arrhythmia, cardiomyopathy, or infectious cardiac diagnoses. Since psychiatric problems in children with cardiac disease often go undiagnosed [19], the effectiveness of the PedsQL to screen for emotional distress during clinical encounters should be assessed prospectively. Children with more severe cardiac conditions reported lower QoL and emotional health, regardless of diagnosis, suggesting that factors other than the cardiac diagnosis or treatment, such as activity limitations, sedentary lifestyles, frequent school absences or “normal” child/teenager problems, warrant further investigation. Interventional studies to evaluate the impact of support from peers with similar conditions, as reported by both children and parents, are recommended.
Acknowledgement: The authors thank the cardiology staff at the Children’s Hospital of Eastern Ontario and The Hospital for Sick Children, as well as the patients and their families who participated in this study.
Ethics Approval and Consent: The Research Ethics Boards of both institutions-The Hospital for Sick Children (Toronto, 2011, REB#1000020209) and Children’s Hospital of Eastern Ontario (Ottawa, 2013 and 2015, IRB/REB #13/63X)-approved this prospective cross-sectional study. Parents provided written informed consent and children provided verbal assent.
Availability of Data and Materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions: RS and PL contributed to the conception of the study. PL, JJ, and BP contributed to the acquisition of the data. PL, LL, and GG contributed to the interpretation of the data. PL, JL, and AB contributed to the data analysis. All authors critically revised the manuscript, gave final approval agree to be accountable for all aspects of work ensuring integrity and accuracy.
Funding Statement: Data collection at SickKids was supported by the Cardiovascular Clinical Research Unit. Data collection by Bhavika Patel was supported by the Mach-Gaensslen Foundation of Canada through a summer research studentship. Data collection by Julia Jackson was supported by a summer studentship from the CHEO Research Institute. The analyses and manuscript preparation by Jacqueline Lee was supported by a Queen Elizabeth II Scholarship.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Drakouli, M., Petsios, K., Giannakopoulou, M., Patiraki, E., Voutoufianaki, I. et al. (2015). Determinants of quality of life in children and adolescents with CHD: A systematic review. Cardiology in the Young, 25(6), 1027–1036. DOI 10.1017/S1047951115000086. [Google Scholar] [CrossRef]
2. Moons, P., Bovijn, L., Budts, W., Belmans, A., Gewillig, M. (2010). Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation, 122(22), 2264–2272. DOI 10.1161/CIRCULATIONAHA.110.946343. [Google Scholar] [CrossRef]
3. Latal, B., Helfricht, S., Fischer, J. E., Bauersfeld, U., Landolt, M. A. (2009). Psychological adjustment and quality of life in children and adolescents following open-heart surgery for congenital heart disease: A systematic review. BMC Pediatrics, 9(1), 6. DOI 10.1186/1471-2431-9-6. [Google Scholar] [CrossRef]
4. Longmuir, P., Sampson, M., Ham, J., Weekes, M., Patel, B. et al. (2018). The mental health of adolescents and pre-adolescents living with inherited arrhythmia syndromes: A systematic review of the literature. Cardiology in the Young, 28(5), 621–631. DOI 10.1017/S104795111700289X. [Google Scholar] [CrossRef]
5. Wang, Q., Hay, M., Clarke, D., Menahem, S. (2014). Associations between knowledge of disease, depression and anxiety, social support, sense of coherence and optimism with health-related quality of life in an ambulatory sample of adolescents with heart disease. Cardiology in the Young, 24(1), 126–133. DOI 10.1017/S1047951113000012. [Google Scholar] [CrossRef]
6. Karimi, M., Brazier, J. (2016). Health, health-related quality of life, and quality of life: What is the difference? Pharmacoeconomics, 34(7), 645–649. DOI 10.1007/s40273-016-0389-9. [Google Scholar] [CrossRef]
7. Varni, J. W., Limbers, C. A., Burwinkle, T. M. (2007). Impaired health-related quality of life in children and adolescents with chronic conditions: A comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the Pediatric Quality of Life Inventory 4.0 Generic Core Scales. Health and Quality of Life Outcomes, 5(1), 43. DOI 10.1186/1477-7525-5-43. [Google Scholar] [CrossRef]
8. Eiser, C., Morse, R. (2001). Can parents rate their child’s health-related quality of life? Results of a systematic review. Quality of Life Research, 10(4), 347–357. DOI 10.1023/A:1012253723272. [Google Scholar] [CrossRef]
9. Patel, B. J., Lai, L., Goldfield, G., Sananes, R., Longmuir, P. E. (2017). Psychosocial health and quality of life among children with cardiac diagnoses: Agreement and discrepancies between parent and child reports. Cardiology in the Young, 27(4), 713–721. DOI 10.1017/S1047951116001141. [Google Scholar] [CrossRef]
10. Miatton, M., De Wolf, D., François, K., Theiry, E., Vingerhoets, G. (2007). Behavior and self-perception in children with a surgically corrected congenital heart disease. Journal of Developmental & Behavioral Pediatrics, 28(4), 294–301. DOI 10.1097/DBP.0b013e3180cabc3c. [Google Scholar] [CrossRef]
11. Warnes, C. A., Williams, R. G., Bashore, T. M., Child, J. S., Connolly, H. M. et al. (2008). ACC/AHA 2008 guidelines for the management of adults with congenital heart disease. Circulation, 118(23), 2395–2451. DOI 10.1161/CIRCULATIONAHA.108.190811. [Google Scholar] [CrossRef]
12. Varni, J. W., Seid, M., Kurtin, P. (2001). PedsQL 4.0: Reliability and validity of the pediatric quality of life inventory version 4.0 generic core scales in healthy and patient populations. Medical Care, 39(8), 800–812. DOI 10.1097/00005650-200108000-00006. [Google Scholar] [CrossRef]
13. March, J. S. (2013). Multidimensional anxiety scale for children. 2nd Edition. North Tonawanda, NY: Multi-Health Systems, Inc. [Google Scholar]
14. Reynolds, C. R., Kamphaus, R. W. (2004). Behavior assessment system for children manual. 2nd Edition. Bloomington, MN: NCS Pearson. [Google Scholar]
15. Braun, V., Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. DOI 10.1191/1478088706qp063oa. [Google Scholar] [CrossRef]
16. Mellion, K., Uzark, K., Cassedy, A., Drotar, D., Wernovsky, G. et al. (2014). Health-related quality of life outcomes in children and adolescents with congenital heart disease. Journal of Pediatrics, 164(4), 781–788.e1. DOI 10.1016/j.jpeds.2013.11.066. [Google Scholar] [CrossRef]
17. DeMaso, D. R., Calderon, J., Taylor, G. A., Holland, J. E., Stopp, C. et al. (2017). Psychiatric disorders in adolescents with single ventricle congenital heart disease. Pediatrics, 139(3), e20162241. DOI 10.1542/peds.2016-2241. [Google Scholar] [CrossRef]
18. Hövels-Gürich, H. H., Konrad, K., Skorzenski, D., Minkenberg, R., Herpertz-Dahlmann, B. et al. (2007). Long-term behavior and quality of life after corrective cardiac surgery in infancy for tetralogy of Fallot or ventricular septal defect. Pediatric Cardiology, 28(5), 346–354. DOI 10.1007/s00246-006-0123-z. [Google Scholar] [CrossRef]
19. Fredriksen, P. M., Mengshoel, A. M., Frydenlund, A., Thaulow, E. (2004). Follow-up in patients with congenital cardiac disease more complex than haemodynamic assessment. Cardiology in the Young, 14(4), 373–379. DOI 10.1017/S1047951104004044. [Google Scholar] [CrossRef]
20. Karsdorp, P. A. (2007). Psychological and cognitive functioning in children and adolescents with congenital heart disease: A meta-analysis. Journal of Pediatric Psychology, 32(5), 527–541. DOI 10.1093/jpepsy/jsl047. [Google Scholar] [CrossRef]
21. Menahem, S., Poulakis, Z., Prior, M. (2008). Children subjected to cardiac surgery for Congenital Heart Disease. Part 1–Emotional and psychological outcomes. Interactive CardioVascular and Thoracic Surgery, 7(4), 600–604. DOI 10.1510/icvts.2007.171058. [Google Scholar] [CrossRef]
22. Berkes, A., Pataki, I., Kiss, M., Kemeny, C., Kardos, L. et al. (2010). Measuring health-related quality of life in Hungarian children with heart disease: Psychometric properties of the Hungarian version of the Pediatric Quality of Life Inventory™ 4.0 Generic Core Scales and the Cardiac Module. Health and Quality of Life Outcomes, 8(1), 14. DOI 10.1186/1477-7525-8-14. [Google Scholar] [CrossRef]
23. Apers, S., Kovacs, A. H., Luyckx, K., Thornet, C., Budts, W. et al. (2016). Quality of life of adults with congenital heart disease in 15 countries: Evaluating country-specific characteristics. Journal of the American College of Cardiology, 67(19), 2237–2245. DOI 10.1016/j.jacc.2016.03.477. [Google Scholar] [CrossRef]
24. Bellinger, D. C., Newburger, J. W., Wypij, D., Kuban, K. C. K., duPlessis, A. J. et al. (2009). Behaviour at eight years in children with corrected transposition of the great arteries: The Boston Circulatory Arrest Trial. Cardiology in the Young, 19(1), 86–97. DOI 10.1017/S1047951108003454. [Google Scholar] [CrossRef]
25. Bellinger, D. C., Newburger, J. W. (2010). Neuropsychological, psychosocial, and quality-of-life outcomes in children and adolescents with Congenital Heart Disease. Progress in Pediatric Cardiology, 29(2), 87–92. DOI 10.1016/j.ppedcard.2010.06.007. [Google Scholar] [CrossRef]
26. McMurray, R., Kendall, L., Parsons, J., Quirk, J., Veldtman, G. et al. (2001). A life less ordinary: Growing up and coping with congenital heart disease. Coronary Health Care, 5(1), 51–57. DOI 10.1054/chec.2001.0112. [Google Scholar] [CrossRef]
27. Moola, F., Fusco, C., Kirsh, J. (2011). “What I wish you knew”: Social barriers toward physical activity in youth with Congenital Heart Disease (CHD). Adapted Physical Activity Quarterly, 28(1), 56–77. DOI 10.1123/apaq.28.1.56. [Google Scholar] [CrossRef]
28. Herman-Stabl, M. A., Stemmler, M., Petersen, A. C. (1995). Approach and avoidant coping: Implications for adolescent mental health. Journal of Youth and Adolescence, 24(6), 649–665. DOI 10.1007/BF01536949. [Google Scholar] [CrossRef]
29. Holland, J. E., Cassidy, A. R., Stopp, C., White, M. T., Bellinger, D. C. et al. (2017). Psychiatric disorders and function in adolescents with tetralogy of fallot. Journal of Pediatrics, 187, 165–173. DOI 10.1016/j.jpeds.2017.04.048. [Google Scholar] [CrossRef]
30. Awaad, M. I., Darahim, K. E. (2015). Depression and anxiety in adolescents with Congenital Heart Disease. Middle East Current Psychiatry, 22(1), 2–8. DOI 10.1097/01.XME.0000457325.90630.4f. [Google Scholar] [CrossRef]
31. McCrindle, B. W., Williams, R. V., Mitchell, P. D., Hsu, D. T., Paridon, S. M. et al. (2006). Relationship of patient and medical characteristics to health status in children and adolescents after the Fontan procedure. Circulation, 113(8), 1123–1129. DOI 10.1161/CIRCULATIONAHA.105.576660. [Google Scholar] [CrossRef]
32. Ruggiero, K. M., Hickey, P. A., Leger, R. R., Vessey, J. A., Hayman, L. L. (2018). Parental perceptions of disease-severity and health-related quality of life in school-age children with congenital heart disease. Journal for Specialists in Pediatric Nursing, 23(1), 1–10. DOI 10.1111/jspn.12204. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |