

 | Congenital Heart Disease |  |
DOI: 10.32604/CHD.2021.014516
ARTICLE
Isolation of the Left Subclavian Artery in D-Transposition of the Great Arteries with Right Aortic Arch
1Department of Neonatology, Toho University Omori Medical Center, Tokyo, 143-8541, Japan
*Corresponding Author: Kotaro Hine. Email: kotaro.hine@med.toho-u.ac.jp
Received: 04 October 2020; Accepted: 17 November 2020
Abstract: Abnormal branching of the aorta associated with the right aortic arch (RAA) has been reported as isolation of left subclavian artery (ILSA), isolation of left common carotid artery, isolation of brachiocephalic artery. ILSA is a rare aortic branch anomaly that originates in the left subclavian artery from the pulmonary artery via ductus arteriosus. Several reports have described ILSA associated with 22q11.2 deletion syndrome and tetralogy of Fallot. Here, we present a very unusual case of RAA with ILSA associated with D-transposition of the great arteries and inferior vena cava interrupted with azygos continuation.
Keywords: Isolated left subclavian artery; transposition of the great arteries; RAA; ILSA
Zero-day-old boy weighing 2,099 g was delivered by emergency caesarean section due to non-reassuring fetal status at 37 weeks and 4 days of gestation, with Apgar scores of 1 and 7 at 1 min and 5 min, respectively. Fetal echocardiography performed at 19 weeks of gestation revealed D-transposition of the great arteries (D-TGA), right aortic arch (RAA), right-sided patent ductus arteriosus (PDA) from the descending aorta and inferior vena cava (IVC) interrupted with azygos continuation. At the time of birth, the baby was cyanotic but showed no respiratory distress. Physical examination revealed grade 2/6 systolic murmur at the right sternal border. The second sound was enhanced. Both radial and both femoral pulses were present. Blood pressure in the right arm was 48/25 mmHg and no significant difference was apparent between extremities. A difference in SpO2 was noted between the left and right upper extremities (oxygen saturation: 75% in the right upper extremity, 94% in the left upper extremity, 76% in both lower extremities). Chest radiography showed cardiomegaly, normal pulmonary vascular markings, and a right aortic arch. Transthoracic echocardiography confirmed type 1 D-TGA, a large patent foramen ovale and an IVC interrupted with azygos continuation. Although RAA and a right-sided PDA from the descending aorta were confirmed, the branching pattern of the aortic arch was unclear, and unusual shunt flow from the left pulmonary artery to the left side was confirmed. Multidetector-row computed tomography (MDCT) angiography showed the following features of the RAA. The first branch of the aortic arch formed the left common carotid artery, the second branch was the right common carotid artery and the third branch was the right subclavian artery, but no left subclavian artery (LSCA) was seen arising from the aortic arch. Instead, the LSCA arose from the junction of the distal main pulmonary artery and proximal left pulmonary artery via left-sided PDA. Until surgery, we did not administer prostaglandin E1, but the left-sided PDA did not close. The patient subsequently underwent Jatene surgery and ligation of the bilateral PDA with good results. LSCA was disconnected from the left pulmonary artery and did not reimplant to other blood vessels. After surgery, the patient presented with no symptoms and signs related to subclavian steal syndrome. Images from MDCT angiography are presented in Fig. 1. G-banding showed a normal karyotype, and submicroscopic deletions in chromosome 22q11.2 were ruled out by fluorescence in situ hybridization (FISH). Written informed consent was obtained from parents.
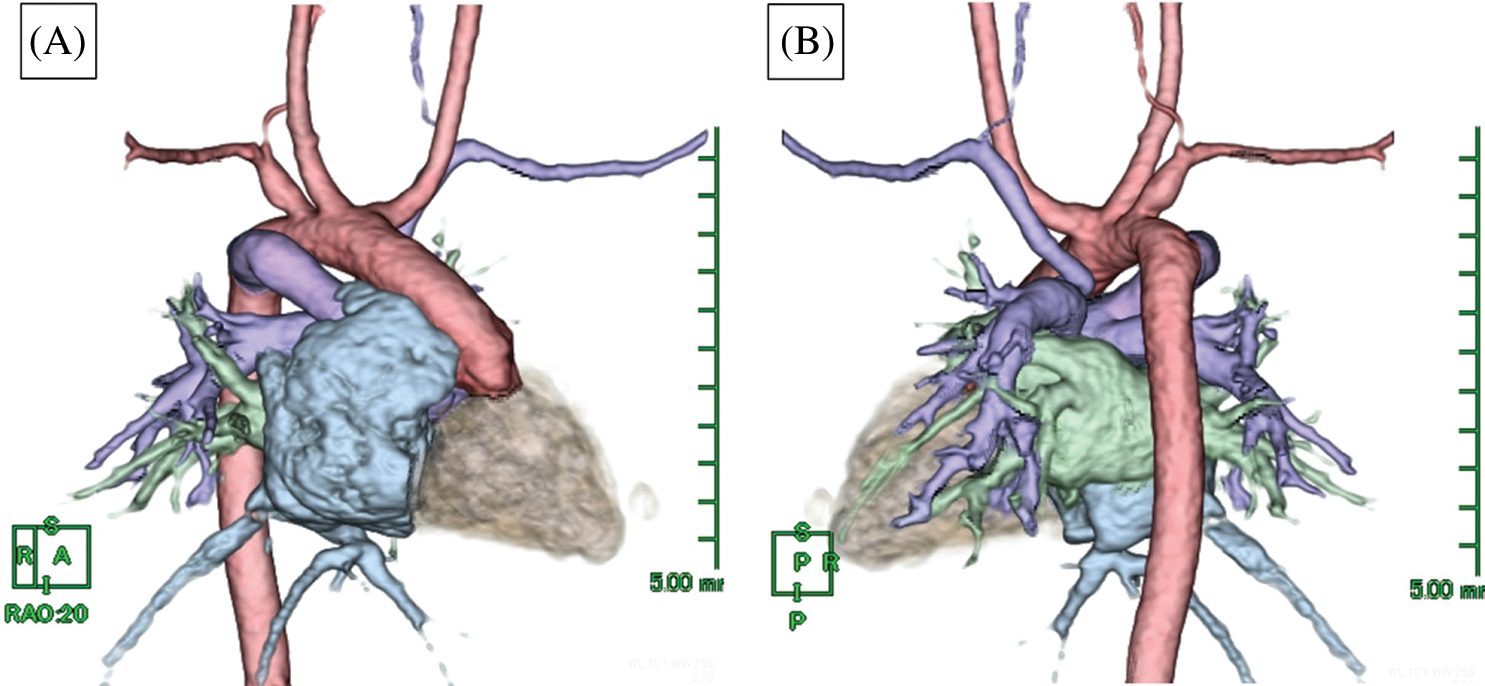
Figure 1: Multidetector-row computed tomography from right anterior oblique position (A) and posterior position (B). The right aortic arch arises from the right ventricle and the left subclavian artery arises from the pulmonary artery via left-sided PDA
Isolation of left subclavian artery (ILSA) is a rare aortic branching abnormality, first described by Stewart et al. [1]. RAA with ILSA is the least common type of RAA, occurring in 0.8% of 298 RAAs [2]. The embryologic development of RAA with ILSA can be explained through the hypothetical functioning double aortic arch model as suggested by Edward et al. [3]. RAA with ILSA regression takes place on two levels in the double aortic arch plan: between the left common carotid artery and LSCA; and at the left dorsal aortic root distal to the left ductus arteriosus. The right ductus arteriosus then persists, and the left ductus arteriosus connects the LSCA to the left pulmonary artery (Fig. 2). However, in this case, the relationship of developmental mechanism between RAA + ILSA and D-TGA was unclear.
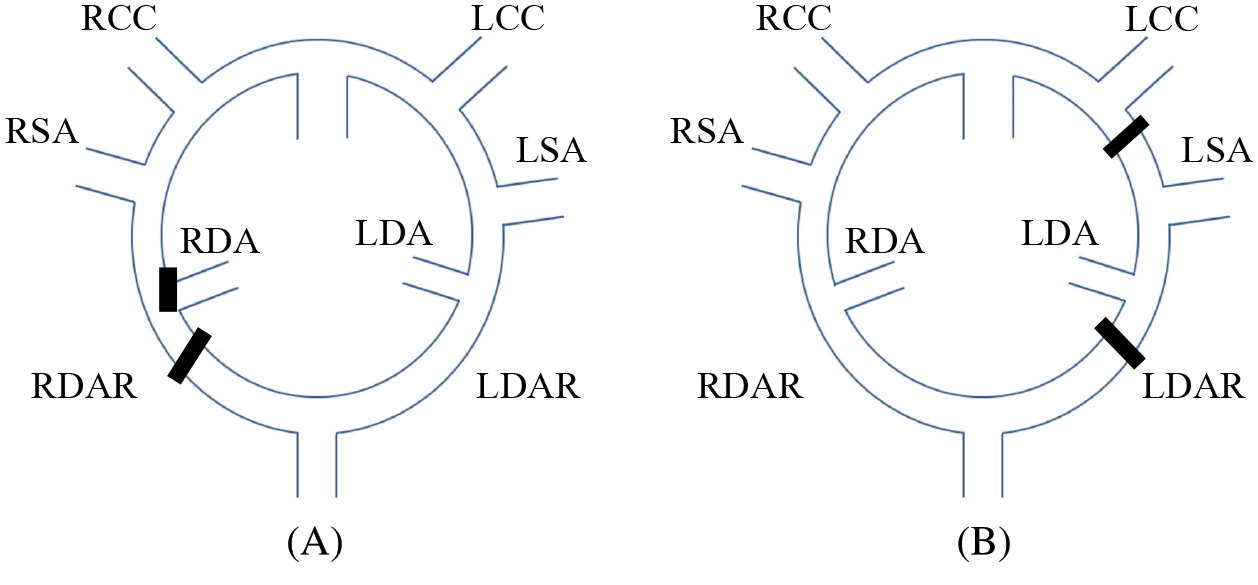
Figure 2: (A) Normal embryological aortic arch pattern. (B) Hypothetical pathological pattern in the present case
ILSA is known to be commonly associated with 22q11.2 deletion syndrome [4]. In the present case, normal karyotype was determined by the G-banding method and 22q11.2 deletion syndrome was ruled out by FISH. Polysplenia was considered, because the interruption of the IVC with azygos continuation was observed, but abdominal ultrasonography and abdominal CT revealed a normal spleen.
RAA with ILSA is commonly associated with congenital heart diseases such as tetralogy of Fallot (TOF) [4,5], but D-TGA with both ILSA and RAA has not been reported previously. The most similar case reported may be transposition with an isolated left brachiocephalic artery, which has been described only twice previously [6,7].
In the present case, oxygenated blood circulated to the LSCA via the pulmonary artery, so SpO2 in the upper left limb was very high from birth, and SpO2 showed a distinct left-right difference in the upper limbs. This clear difference between left and right values from SpO2 monitoring of the upper limbs triggered the diagnosis. The relatively common type of RAA+ILSA (associated with or without TOF), oxygenated blood circulates to right subclavian artery and venous blood circulates to ILSA via the pulmonary artery. So RAA+ILSA usually show higher SpO2 on the right upper limb and lower SpO2 on the left upper limb, while, RAA+ILSA+D-TGA show high SpO2 on the left upper limb and low SpO2 on the right upper limb, respectively, although both situations show the difference between left and right values from SpO2 monitoring of the upper limbs. Knowing these characteristics is very important for the diagnosis.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Stewart, J. A., Kincaid, O. W., Edwards, J. E. (1964). An atlas of vascular rings and related malformations of the aortic arch system. Springfield, IL: Thomas. [Google Scholar]
2. Stewart, J. R., Kincaid, O. W., Titus, J. L. (1966). Right aortic arch: Plain film diagnosis and significance. American Journal of Roentgenology, Radium Therapy, and Nuclear Medicine, 97(2), 377–389. DOI 10.2214/ajr.97.2.377. [Google Scholar] [CrossRef]
3. Edwards, J. E. (1948). Anomalies of the derivatives of the aortic arch system. Medical Clinics of North America, 32, 925–949. DOI 10.1016/S0025-7125(16)35662-0. [Google Scholar] [CrossRef]
4. Lee, J. S., Park, J. Y., Ko, S. M., Seo, D. M. (2015). Isolation of the left subclavian artery with right aortic arch in association with bilateral ductus arteriosus and ventricular septal defect. Korean Journal of Thoracic and Cardiovascular Surgery, 48(6), 415–418. DOI 10.5090/kjtcs.2015.48.6.415. [Google Scholar] [CrossRef]
5. Luetmer, P. H., Miller, G. M. (1990). Right aortic arch with isolation of the left subclavian artery: Case report and review of the literature. Mayo Clinic Proceedings, 65(3), 407–413. DOI 10.1016/S0025-6196(12)62540-3. [Google Scholar] [CrossRef]
6. Bornemeier, R., Ramaciotti, C. (1996). Isolation of the left innominate artery. Echocardiography, 13(4), 435–438. DOI 10.1111/j.1540-8175.1996.tb00917.x. [Google Scholar] [CrossRef]
7. Penslar, J., Menard, C., Lee, S. (2018). Isolated left brachiocephalic artery in transposition of the great arteries. Canadian Journal of Cardiology, 34(10), 1369.e13–1369.e15. DOI 10.1016/j.cjca.2018.07.420. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |