

 | Congenital Heart Disease |  |
DOI: 10.32604/CHD.2021.015257
ARTICLE
An Unusual Cause of Irritability in a Single Ventricle Patient after Bidirectional Glenn Shunt
1The Heart Institute, Cincinnati Children’s Hospital Medical Center, University of Cincinnati College of Medicine, Cincinnati, Ohio, USA
2Division of Neurology, Cincinnati Children’s Hospital Medical Center, Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, Ohio, USA
*Corresponding Author: Sarah Pradhan. Email: sarah.pradhan6@gmail.com
Received: 04 December 2020; Accepted: 01 February 2021
Abstract: The differential diagnosis for irritability in children is broad. In patients with congenital heart disease, one must strongly consider cardiac etiologies such as low cardiac output or elevated central venous pressure (CVP). In patients with single-ventricle physiology, the second stage of palliation includes bidirectional Glenn, which involves anastomosis of the superior vena cava to the pulmonary artery resulting in volume offloading of the single systemic ventricle. Typically, early in the post-operative period, patients may experience a headache due to the acute increase in CVP, and symptoms improve over time. Idiopathic intracranial hypertension (IIH), also known as pseudotumor cerebri, is a rare neurologic disorder in children, characterized by raised intracranial pressure (ICP) in the absence of brain parenchymal lesions or cerebrospinal fluid (CSF) abnormalities. While the pathogenesis of IIH is unknown, early recognition and treatment of IIH are important to prevent permanent vision loss. There are only rare reports of IIH in patients with Fontan circulation. To our knowledge, we report the first case of IIH in a 2-year-old female after bidirectional Glenn.
Keywords: Single ventricle; bidirectional Glenn shunt; idiopathic intracranial hypertension; pseudotumor cerebri
The patient was a 2-year-old female with a history of single ventricle anatomy comprising of a systemic morphologic left ventricle, left atrioventricular (AVV) atresia, L-malposed great arteries with pulmonary atresia, and a subaortic ventricular septal defect (VSD). Her initial palliation on day of life two included an atrial septectomy and a 3.5 mm modified Blalock-Taussig shunt (mBTS). At four months of age, she underwent an uncomplicated bidirectional Glenn shunt (BDG). She presented for routine outpatient cardiology follow-up (six monthly follow-up intervals) with a new complaint of four weeks of progressive irritability, decreased appetite, possible headache, increased appearance of cyanosis, and fatigue. Her parents denied any vomiting or waking from sleep but stated that she occasionally grabbed her head and ears, making them concerned that she was in pain. They also noted that her demeanor had changed, she was speaking less, and that her gait appeared at times to be more unsteady. They denied any recent changes in home environment, abdominal pain, changes in bowel movements, or urinary patterns. Her medications, which included aspirin, propranolol, and furosemide, were unchanged. Her family history was notable only for maternal hypothyroidism.
In the clinic setting, her physical examination was notable for agitation and peri-oral cyanosis with crying. Her oxygen saturation was 79% on room air. Her peripheral examination was normal with warm extremities, brisk capillary refill, and no evidence of pallor, jaundice, or peripheral edema. She had no evident distension of peripheral veins in either upper or lower extremities. Her precordium was quiet with a normal first and single second heart sound, with no murmurs, rubs, or gallops. Her abdomen was soft and un-distended, with no liver or spleen enlargement or any other masses apparent. She had no gross neurologic deficits, and her gait in the clinic was appropriate for age.
Her cardiac testing demonstrated unchanged findings on her echocardiogram, with normal morphologic left ventricular function, trivial right atrio-ventricular valve insufficiency without stenosis, trivial aortic insufficiency, and low-velocity laminar flow through the superior cavo-pulmonary anastomosis. The atrial septum was unrestrictive. She was admitted for an elective cardiac catheterization one week later to exclude elevated Glenn pressure as a possible cause of intermittent headache as the cause of the irritability and behavioral changes since no other obvious etiology was present at the time. Her overall hemodynamics were unremarkable, with the Glenn pressure 14 mmHg, trans-pulmonary gradient 4–5 mmHg, well preserved cardiac index of 5.5 l/min/m2, pulmonary-systemic shunt ratio of 0.63:1, and pulmonary vascular resistance of 1.4 Wood Units × m2. There was no stenosis within her Glenn anastomosis or branch pulmonary arteries. She did have modest aorto-pulmonary collateral vessels originating from her bilateral internal mammary arteries, and they were occluded with micro-embolization particles. There were no veno-venous collateral vessels. Her post catheterization recovery was unremarkable, but she was again admitted one week after discharge with unremitting, and possible deteriorating symptoms of irritability, gait instability and poor appetite. Further initial clinical work-up, which included renal and liver function testing, abdominal ultrasound, and celiac, thyroid, lead, infectious and rheumatologic screening bloodwork were all negative. A neurology consultation was obtained, prompting brain magnetic resonance imaging which was positive for mild diffuse cerebral volume loss; upon later review, there was bilateral posterior flattening of the globes evident (Fig. 1). With no obvious etiology, the patient was treated for possible migraine headache, which resulted in marked but transient symptomatic improvement, with a return of symptoms hours later. At that point, an Ophthalmology examination was obtained, demonstrating bilateral papilledema. This was followed shortly thereafter with a diagnostic lumbar puncture, notable for elevated opening pressure of 28 mmHg. All cerebrospinal fluid studies were negative. Symptoms were greatly improved after the lumbar puncture.
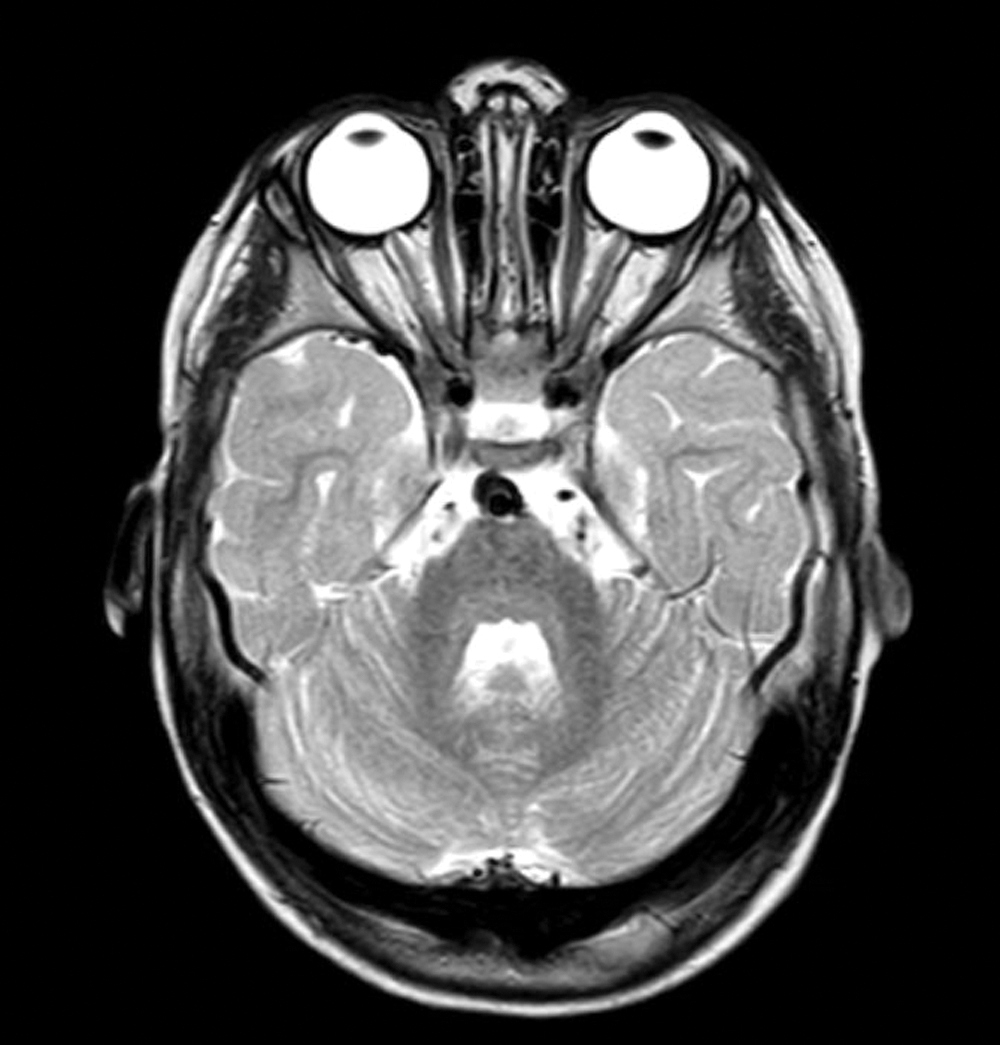
Figure 1: Axial T2 MRI of the brain demonstrating posterior globe flattening. There is normal brain parenchyma, vessels and cerebrospinal fluid flow through the craniocervical junction
The patient was putatively diagnosed with idiopathic intracranial hypertension (IIH), and oral acetazolamide was commenced. With therapy, she had prompt symptomatic improvement, complete resolution of symptoms, and return to behavioral baseline within two weeks. Serial fundoscopic examinations showed improvement in papilledema. Written informed consent was obtained from parents.
IIH, a diagnosis of exclusion, can be challenging to diagnose in children compared to adults, particularly when significant congenital heart disease confounds the clinical presentation. In particular, Glenn physiology, dependent on obligate pulmonary blood flow derived from the superior vena cava, is susceptible to changes in ventricular compliance, atrial septal flow, and pulmonary vascular resistance. Deterioration in any of those components may increase central venous pressure and result in cerebral congestion and headaches. Not surprisingly, this clinical scenario is most common early in the peri-operative period but usually dissipates with venous accommodation or the development of decompressing veno-venous collateral vessels. For the purposes of diagnosis, cardiac catheterization is the only means by which that constellation can be diagnosed or excluded, and should be performed early, as in this case. However, if the hemodynamic measurements are unremarkable, further etiologies need to be aggressively sought.
IIH is most commonly seen in young adults, with an overall annual incidence of 0.9 per 100,000 individuals, with a strong female predominance [1]. It is rare in pediatric patients, particularly in the pre-pubertal child, and the female predilection appears to begin after puberty [1]. The pathophysiology of IIH remains unclear, although many theories have been proposed, including: decreased CSF absorption by arachnoid villi, intracranial venous hypertension, increased CSF production, increased cerebral volume, or obesity causing increased intra-abdominal and intracerebral venous pressure [1]. The increase in central venous pressure caused by Glenn physiology is intuitively a cause for cerebral venous hypertension. However, not all Glenn patients develop IIH, thus indicating a different clinical entity in our patient. Early diagnosis and treatment of IIH are essential to avoid permanent vision loss [1,2]. Vision loss is theorized to be due to the transmission of elevated intracranial pressure to the optic nerve resulting in microvascular compromise [1]. Management is primarily conservative, with medical therapy as needed. Weight loss is advised if appropriate, and acetazolamide (carbonic anhydrase inhibitor that reduces CSF production) is the first-line therapeutic agent [1,2]. Furosemide, a loop diuretic, can be used in conjunction with acetazolamide or as a sole agent [1]. Lumbar puncture (LP) can be therapeutic due to the pressure-lowering effect. However, repeated LP is not advised as long-term management, given the well-known risks and only a temporary effect [1]. Prognosis remains elusive, although IIH is typically a chronic illness requiring long-term follow-up and assessment for vision loss [1].
This report describes the first pediatric diagnosis of IIH in a pediatric patient after a bidirectional Glenn shunt. It highlights the importance of considering and searching for alternative irritability causes in patients with congenital heart disease after obvious hemodynamic abnormalities have been excluded. In cases such as this, missed diagnoses could have irreversible consequences.
Funding Statement: The author(s) received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Mercille, G., Ospina, L. H. (2007). Pediatric idiopathic intracranial hypertension: A review. Pediatrics in Review, 28(11), e77–e86. DOI 10.1542/pir.28-11-e77. [Google Scholar] [CrossRef]
2. Albakr, A., Hamad, M. H., Alwadei, A. H., Bashiri, F. A., Hassan, H. H. (2016). Idiopathic intracranial hypertension in children: Diagnostic and management approach. Sudan J Paediatr, 16(2), 67–76. [Google Scholar]
Video 1: An injection is performed into the superior vena cava. There is normal branch pulmonary artery anatomy, with no stenosis and good distal arborization. There is normal pulmonary venous return to the left atrium in levophase.
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |