
 | Congenital Heart Disease | 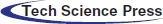 |
DOI: 10.32604/CHD.2022.018728
EDITORIAL
New Insights into Sinus Venosus Defects from Cross-Sectional Imaging
1Department of Diagnostic Imaging, Hospital for Sick Children, University of Toronto, Toronto, Canada
2Division of Cardiology, Department of Paediatrics, Labatt Family Heart Centre, Hospital for Sick Children, University of Toronto, Toronto, Canada
3Department of Diagnostic Imaging, Sejong Heart Center, Bucheon, Korea
4Department of Radiology, Instituto Nacional de Cardiología, Mexico City, Mexico
5Division of Cardiac Surgery, Department of Surgery, Labatt Family Heart Centre, Hospital for Sick Children, University of Toronto, Toronto, Canada
6Pediatric and Congenital Cardiac Surgery Unit, University of Padua Medical School, Padua, Italy
*Corresponding Author: Shi-Joon Yoo. Email: shi-joon.yoo@sickkids.ca
Received: 13 August 2021; Accepted: 23 September 2021
Abstract: Sinus venosus defects include two varieties, superior and inferior sinus venosus defects. The superior sinus venosus defect is characterized by abnormal communication between two closely related venoatrial structures: 1) the normally positioned superior vena cava-right atrium complex and 2) the right pulmonary vein-left atrium complex that is displaced leftward, forward and upward. Inferior sinus venosus defects primarily involve the inferior vena cava-right atrial junction while the right pulmonary vein-left atrial junction can also be affected. Because of the rarity and wide variation of the defects, the morphological characterization of sinus venosus defects is inconsistent among investigators and often inaccurate. Modern imaging technologies with high spatial and temporal resolutions have allowed accurate and detailed assessment of the pathological anatomy in larger numbers of cases. In this pictorial essay, we revisit the established and controversial features of the sinus venous defects using two-dimensional (2D) and three-dimensional (3D) images obtained by magnetic resonance (MR) or computed tomography (CT) with brief discussion on imaging and treatment strategies.
Keywords: Sinus venosus defect; superior sinus venosus defect; inferior sinus venosus defect; anomalous pulmonary venous connection; overriding superior vena cava; overriding inferior vena cava
Sinus venosus defects are commonly described within the group of congenital malformations causing an interatrial shunt and at times inaccurately referred to as one form of atrial septal defects [1–4]. These uncommon defects involve the party wall between the right atrium at the vena caval entrance and the adjacent left atrium at the right pulmonary venous entrance. However, the defects are not limited to the interatrial party wall but extend further beyond the atria. Therefore, they should not be regarded as atrial septal defects [5–9]. These defects are usually found at the superior vena caval entrance to the right atrium or rarely at the inferior vena caval entrance to the right atrium and referred to as superior and inferior sinus venosus defects, respectively. Although they present hemodynamically similar to atrial septal defects, sinus venosus defects are far more complex malformations that show a wide morphological variation.
As in other congenital cardiovascular malformations, understanding of the morphological features of sinus venosus defects has evolved over time with an increasing number of cases encountered. Because of the relatively small numbers of cases in earlier reports, the morphological characterization of these defects is inconsistent among investigators and often inaccurate. Traditionally, congenital cardiovascular malformations were primarily characterized through study of pathologic specimens. Such a largely empirical approach is limited by the small number of available specimens and difficulties in properly exposing the regions of interest. Modern imaging technologies with high spatial and temporal resolutions have allowed accurate and detailed assessment of the normal and pathological anatomy in large numbers of cases. Contemporary experience in living patients with modern imaging technologies has provided us new insights into the complex anatomy of the sinus venosus defect.
In this pictorial essay, we revisit the established and controversial features of sinus venous defects using the interesting cases collection of two-dimensional (2D) and three-dimensional (3D) images obtained by magnetic resonance (MR) or computed tomography (CT) at the authors’ institutions with brief discussion on imaging and treatment strategies. All cases used in this article were reassessed for 3D representation of the complex anatomy using a commercially available software program (Mimics Medical 23.0 and 3-matic medical version 15.0, Materialise NV, Leuven, Belgium). Our discussion will be strictly based on morphological observation without any consideration of the theoretical morphogenesis of the abnormalities.
2 Normal Anatomy of the Interatrial Party Wall and Adjacent Structures
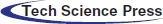
The party wall between the right and left atria consists of the central thin oval area and the peripheral thicker rim that imperceptibly transitions to the atrial free wall and adjoining venous structures (Figs. 1 and 2) [10–12]. As the central thin area is seen as an oval depression from the right atrial side, it is called the fossa ovalis and the surrounding rim is called the limbus of the fossa ovalis. The limbus consists of two thin layers of myocardium and an interposing sliver of fat tissue of variable thickness, all of which appears to be the result of infolding of the atrial wall and epicardial fat (Fig. 2) [10–12]. The intervening fat layer can be particularly prominent in obese individuals, allowing easy understanding of its normal distribution throughout the limbus and the right atrial side of the atrioventricular muscular septum (Figs. 2–4). The limbus is distinctively identifiable superiorly where the free edge of the thin membranous fossa ovalis is fused to the left atrial side of the limbus after birth. The limbus is less prominent or indistinct postero-inferiorly where the fossa ovalis is continuous with the posterior wall of the inferior vena cave (Figs. 1 and 3–A–b) [12–14]. Anteriorly and inferiorly toward the tricuspid valve, the limbus is continuous with the atrioventricular septum (Fig. 2). As most of the limbus is formed by infolding of the atrial wall and epicardial fat, Anderson et al. regard only the floor of the fossa ovalis and the anterior and inferior part of the limbus as the true atrial septum [10–11,13,14]. However, a large part of the interatrial party wall consists of the limbus, while the size of the fossa ovalis varies widely among individuals and can be very small (Fig. 5) [15,16].
Figure 1: Specimen photograph showing normal atrial septum seen from the right atrial side. The party wall between the two atria consists of the floor of the fossa ovalis (FO) surrounded by the limbus (asterisks) that is imperceptibly continuous with the free wall of the atria and the walls of the draining veins. The limbus is poorly formed posterior-inferiorly toward the inferior vena cava (IVC) with the floor of the fossa ovalis appearing to be an interatrial continuation of the inferior vena caval wall. CT, crista terminalis; CS, coronary sinus; SVC, superior vena cava
Figure 2: Cine magnetic resonance images of the normal heart in 4-chamber planes from an obese teenage female showing the two components of the interatrial party wall, the thin membranous fossa ovalis (FO) and the thick surrounding limbus. The limbus consists of the two thin muscle layers (shown as dark strips) and an interposing layer of fatty tissue (bright central zone). Both muscle and fatty tissue layers appear to be the infolding atrial wall and the epicardial fat, respectively. Normally, the central fatty layer is thin and can be hardly identifiable. LA, left atrium; LV, left ventricle; RV, right ventricle
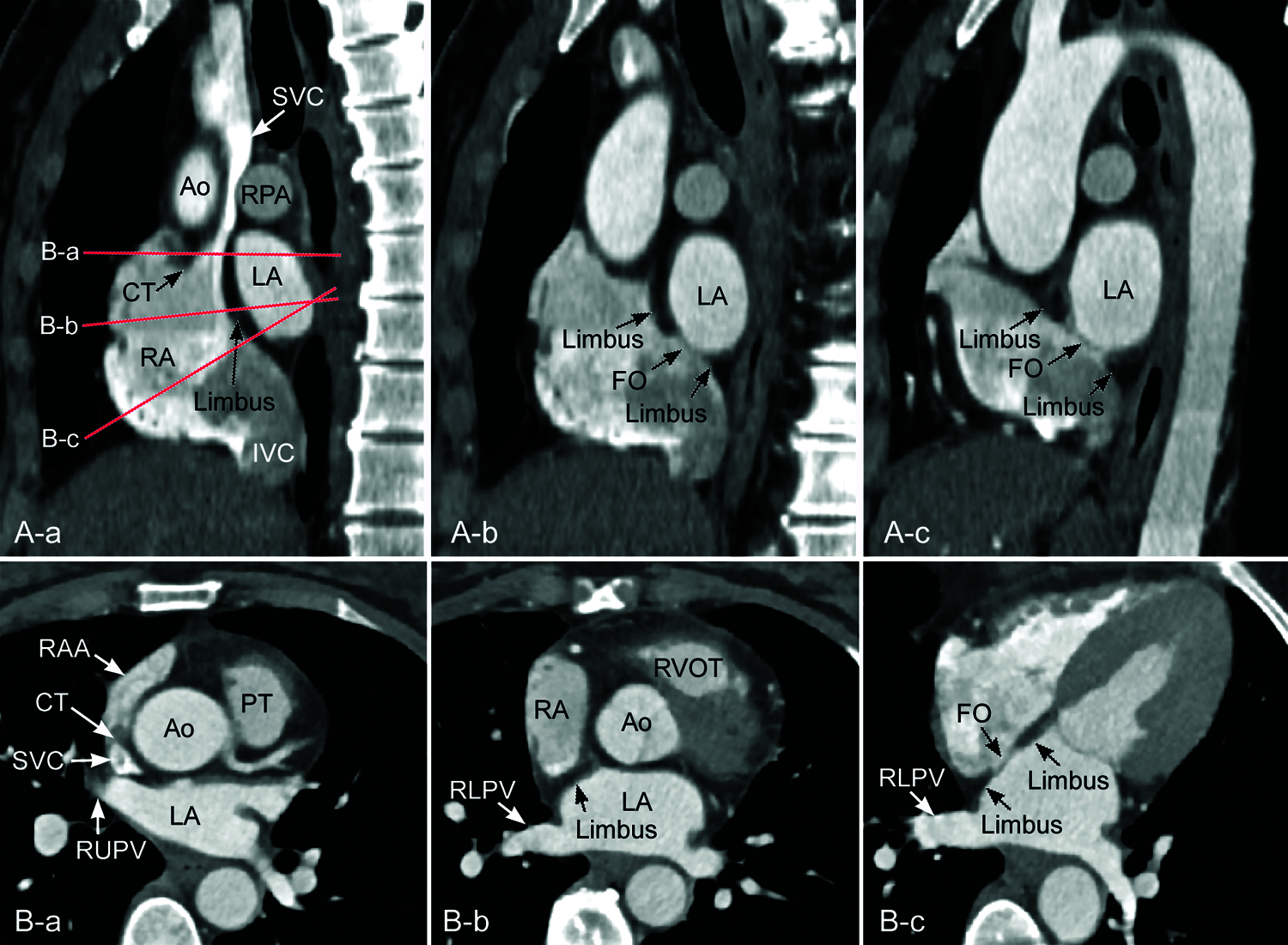
Figure 3: Computed tomographic angiograms from a mildly obese individual. A. Reconstructed images in parasagittal planes along the interatrial party wall. B. Oblique axial images reconstructed along the planes indicated in A-a. The limbus is prominent superiorly and far less prominent inferiorly in A-b and A-c. Note that the interatrial party wall through the central fossa ovalis (FO) in A-c is flat, while the party wall between the sinus venarum and the left atrium in A-a is convex forward and downward. The long axis of the inferior vena cava (IVC) is aligned superiorly to the left atrium (LA). Ao, aorta; IVC, inferior vena cava; CT, crista terminalis; LV, left ventricle; PT, pulmonary arterial trunk; RA, right atrium; RAA, right atrial appendage; RLPV, right lower pulmonary vein; RPA, right pulmonary artery; RV, right ventricle, RVOT, right ventricular outflow tract; RUPV, right upper pulmonary vein; SVC, superior vena cava
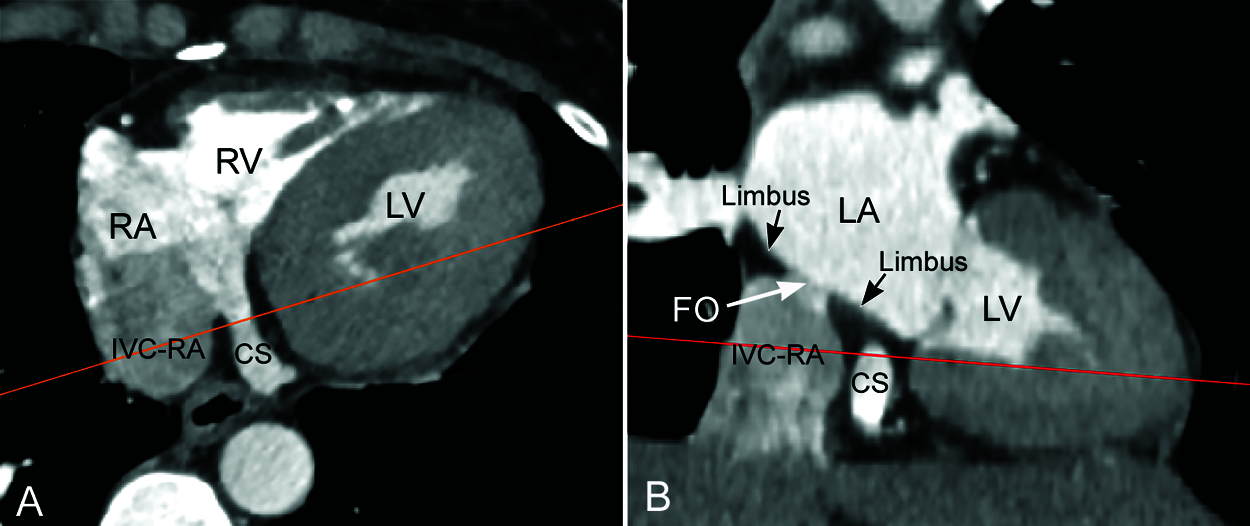
Figure 4: Computed tomographic angiograms along the long (A) and short (B) axes of the coronary sinus (CS) from the same patient shown in Fig. 3. Redlines indicate the imaging planes for the images in the other panel. The coronary sinus is surrounded by low density epicardial fat in this obese individual. Note that the epicardial fat extends into the adjacent limbus. FO, fossa ovalis; IVC-RA, inferior vena cava–right atrial junction; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle
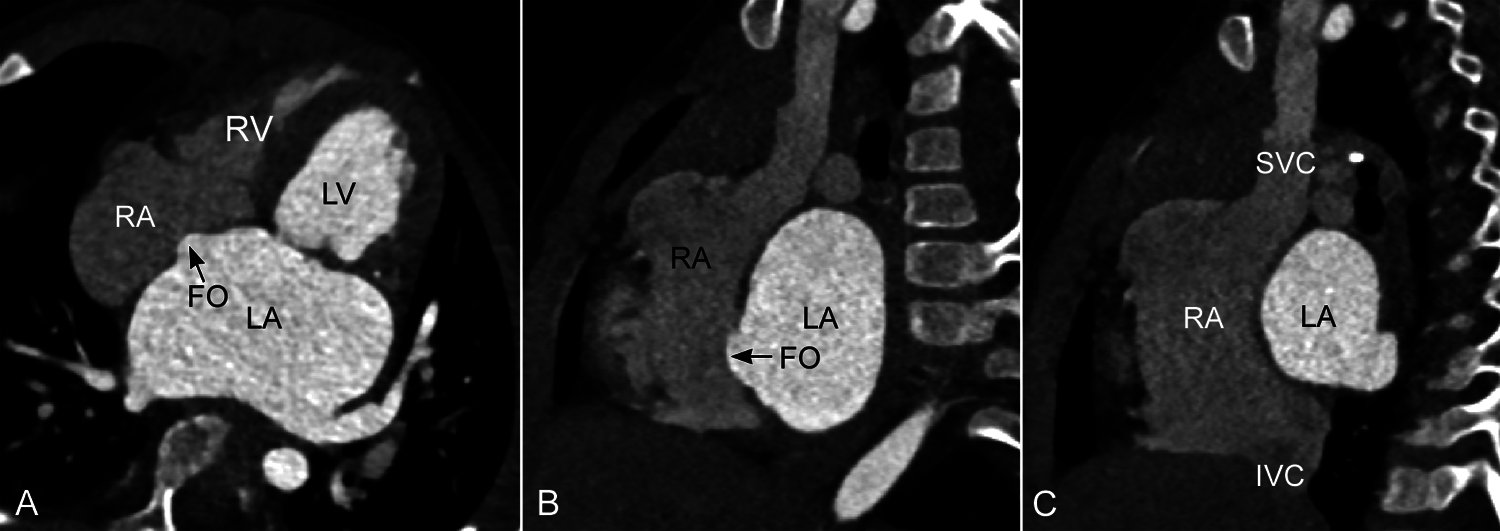
Figure 5: Computed tomographic angiograms in 4-chamber plane (A) and parasagittal intercaval or bicaval planes (B and C) from a patient with severe mitral stenosis. The fossa ovalis (FO) is extraordinarily small and bulges into the right atrium (RA) due to an elevated left atrial pressure. There is exaggerated convexity of the party wall between the sinus venarum and the left atrium (LA) in C. The long axes of both superior (SVC) and inferior (IVC) venae cavae are aligned with the left atrial cavity. LV, left ventricle; RV, right ventricle
The interatrial party wall is mostly flat except for the right lateral posterior aspect where the superior and inferior venae cavae form a confluence called the sinus venarum (Fig. 3). The upper part of the sinus venarum is bounded posteriorly by the far-right side of the left atrium to which the right pulmonary veins connect. As the inferior vena cava is more posteriorly located than the superior vena cava, the party wall between the sinus venarum part of the right atrium and the adjacent left atrium–right pulmonary venous confluence is obliquely oriented with a gentle convex curvature forward and downward. Such oblique orientation of the interatrial party wall along the sinus venarum can be best appreciated in the parasagittal intercaval or bicaval imaging plane (Figs. 3A and 6). In this particular plane, the long axis of the inferior vena cava is oriented vertically toward the left atrium across the most inferior part of the interatrial party wall. The orifice of the inferior vena cava is often guarded anteriorly by a prominent membranous flap called the Eustachian valve (Fig. 6B). When present, the Eustachian valve inserts to the anterior inferior aspect of the limbus, while its superior free edge is aligned with the superior part of the limbus that in fetal medicine is named as the crista dividens [11–12,17]. The Eustachian valve is oriented in such a way to allow the inferior vena caval flow streaming into the left atrium through the patent foramen ovale during fetal life [11,17].
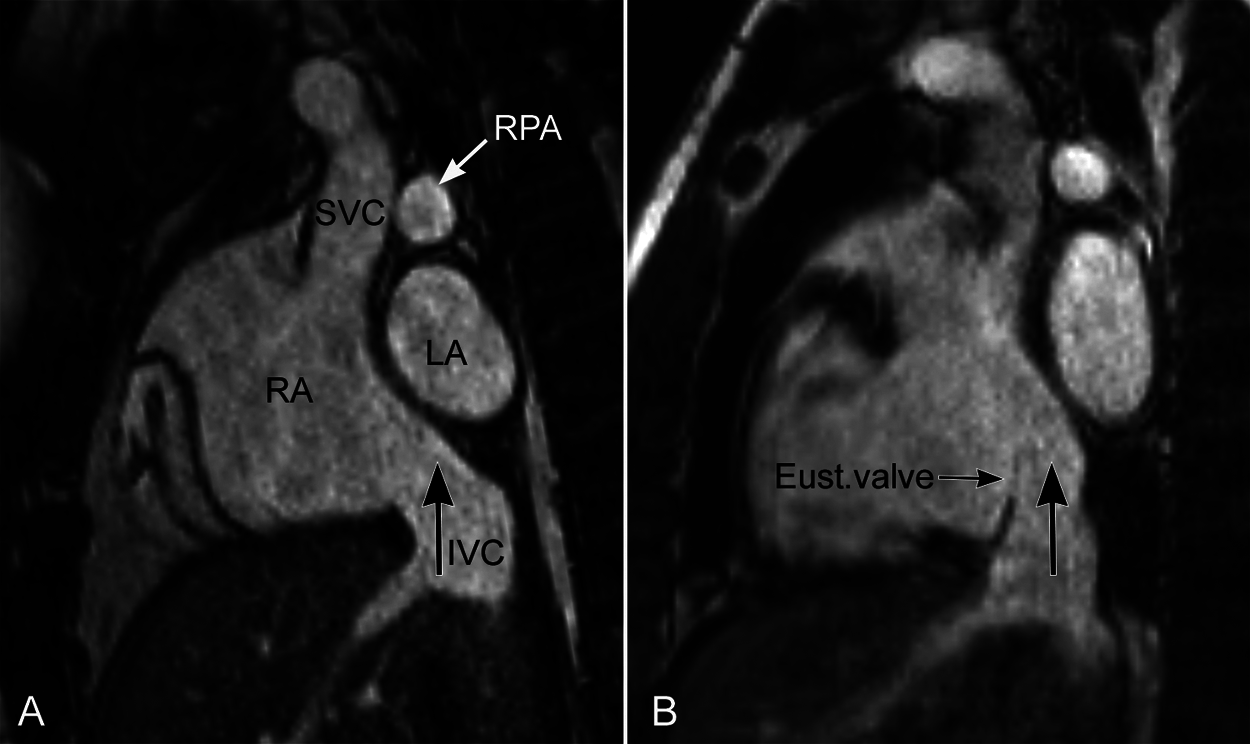
Figure 6: Magnetic resonance images in a parasagittal intercaval or bicaval plane from two individuals. The party wall between the right atrium (RA) and left atrium (LA) is convex forward and downward in this plane with the inferior vena caval axis (IVC, large vertical arrow) directed upward toward the left atrium above. The Eustachian valve (Eust.valve) is prominent in B. Note that the Eustachian valve is aligned with the superior part of the interatrial party wall, i.e., the limbus. RPA, right pulmonary artery; SVC, superior vena cava
3 Morphological Consideration of Sinus Venosus Defects
“Sinus venosus defect” is a widely accepted term for malformations involving vena caval confluence to the right atrium. However, the malformation is not limited to what is called the “sinus venosus”. While superior and inferior varieties share a common generic name of sinus venosus defects, they are distinctly different in regards to the associated pulmonary venous abnormalities and presence or absence of overriding of the vena cava.
3.1 Superior Sinus Venosus Defects
The superior sinus venosus defect is characterized by abnormal communication between two closely related venoatrial structures: 1) the superior vena cava-right atrium complex and 2) the right pulmonary vein-left atrium complex. In most, perhaps all, cases of superior sinus venosus defect, the right pulmonary vein or veins and adjacent part of the left atrium are displaced leftward, forward and upward, while the superior vena cava is normally positioned (Fig. 7). Therefore, the abnormal communication is between the normally positioned superior vena cava–right atrium complex on the one hand and the displaced right pulmonary vein-left atrium complex on the other. Although van Praagh et al. [5] described that the superior sinus venosus defect is a deficiency of the common wall between the superior vena cava and right pulmonary veins, it is important to acknowledge that there is no common wall between the two venous systems [6]. The defect is not a simple hole in the normally existing septal structure or partitioning wall but a far more complex malformation affecting a wider region. Although the defect at the cavoatrial junction may appear most distinct and is constantly described as the hallmark feature of the malformation in the literature, it is only a part of the complex malformation. In fact, variable extent of displacement of the right pulmonary veins and adjacent part of the left atrium is the major underlying reason for wide morphological variation among cases.
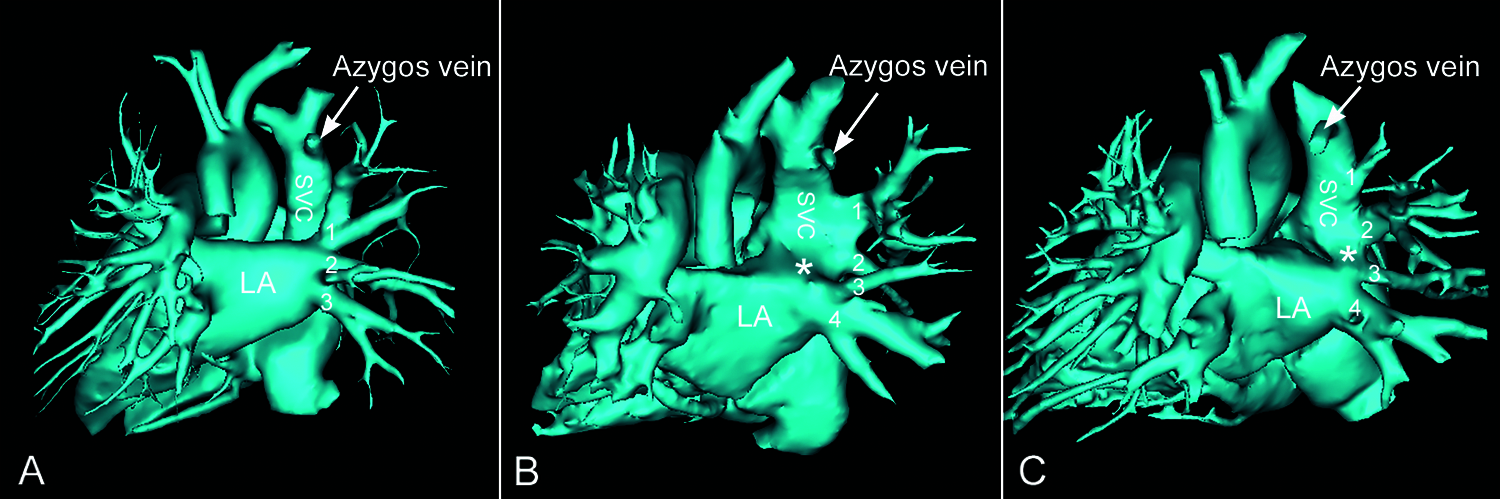
Figure 7: Volume rendered angiograms of a normal heart (A) and two patients with superior sinus venosus defect (B and C) seen from behind. The orientation of the right pulmonary veins in both patients is significantly different from that of the normal heart. Both patients have 4 right pulmonary veins (numbered from top to bottom) with the upper two veins connecting abnormally to the superior vena cava (SVC). The level of abnormal connection of the pulmonary veins to the superior vena cava is higher in C than in B. The defect (asterisk) is between the superior vena cava–right atrium and the upper part of the left atrium (LA) in B, while the defect is between the superior vena cava–right atrium and a pulmonary vein (labeled 3) in C
With a minor degree of leftward, forward and upward displacement, the right upper pulmonary vein–left atrium complex reaches to the cavoatrial junction. With a greater degree of displacement, the uppermost right pulmonary vein reaches the upper part of the superior vena cava below the azygos venous connection and the right middle pulmonary vein–left atrial complex reaches the cavoatrial junction (Fig. 7). The right lower pulmonary vein remains connected to the left atrium in the majority of cases but the connection may appear at a slightly higher level than usual. The displaced right pulmonary veins are connected to the closest part of the superior vena cava or cavoatrial junction. The anomalous pulmonary vein that connects to the cavoatrial junction can be the right upper pulmonary vein but, more frequently, the right middle pulmonary vein. When the right middle pulmonary vein connects to the cavoatrial junction, the right upper pulmonary vein connects separately to the superior vena cava usually through multiple branches (Fig. 7). Therefore, the right pulmonary veins are supernumerary in the majority of cases. Theoretically, it is also possible fort the right lower pulmonary vein–left atrial complex to connect to the cavoatrial junction with the right upper and middle pulmonary veins connecting anomalously to the superior vena cava. Despite the wide variability, abnormalities of the right pulmonary veins are indeed an essential component of the superior sinus venosus defect.
Earlier literature on superior sinus venosus defects invariably described the interatrial communication at the cavoatrial junction as the hallmark feature of the malformation with ample discussion and debate on how to characterize the defects. With new insights into the spectral nature of superior sinus venosus defects, it is quite natural that the communicating channel at the cavoatrial junction does not show a uniform morphological feature. Depending on the spatial relationship between the cavoatrial junction and the displaced right pulmonary vein–left atrium complex, the defect at the cavoatrial junction may appear predominantly interatrial, between the superior vena cava and a right pulmonary vein, between the superior vena cava and the left atrium or between the right atrium and a right pulmonary vein [7]. When the defect is observed from the right atrium, the defect typically involves the superoposterior aspect of the limbus and the adjacent wall of the superior vena cava (Figs. 8A, 9 and 10). The lower margin of the defect is typically at the level of the crista terminalis on the opposite wall but can be higher. The defect may further extend superiorly in front of the right pulmonary artery (Fig. 9). When the defect is seen from the left atrium, the defect appears far more variable. It may open to the left atrium or the anomalous pulmonary vein, or to the venoatrial junction. Such variations depend on the location of the junction between the anomalous pulmonary vein and the left atrium. In cases with the junction formed lateral to the cavoatrial junction, the defect appears to open to the left atrium. In cases with the junction formed medial to the cavoatrial junction, the defect appears to open to the anomalous pulmonary vein. However, the perception can be different among observers as the venoatrial junction is not clearly definable.
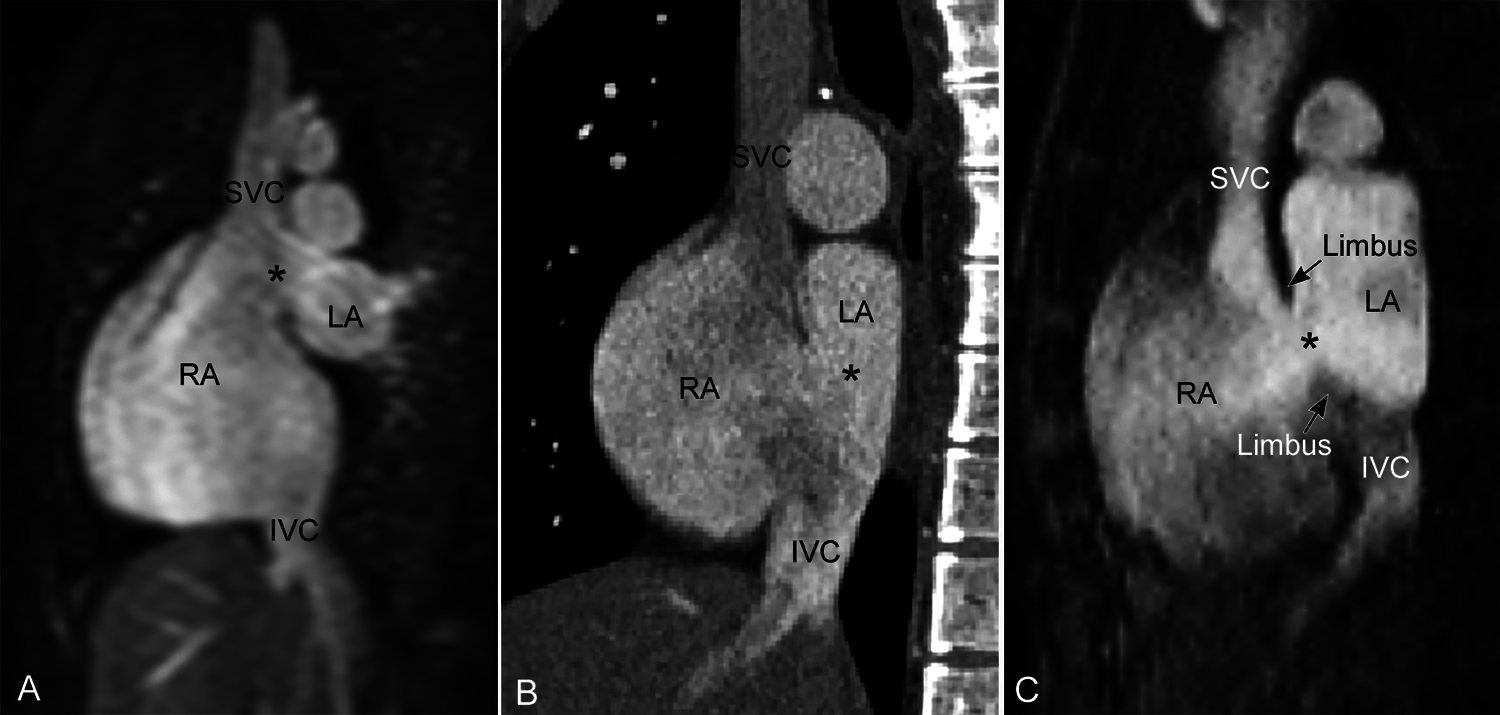
Figure 8: Superior (A) and inferior (B) sinus venosus defects and secundum atrial septal defect (C) shown in parasagittal intercaval or bicaval view. The superior and inferior sinus venosus defects (asterisk) involve the uppermost and lowermost parts of the septum seen in this view. The superior sinus venosus defect in A is not associated with overriding of the superior vena cava across the atrial septum. The inferior sinus venosus defect in B is associated with overt overriding of the inferior vena cava across the atrial septum. This finding is due to the alignment of the affected part of the septum along the trajectory of the inferior vena cava rather than any malalignment of the atrial septum or inferior vena caval orifice. A defect involving the floor of the fossa ovalis (secundum atrial septal defect) may be seen in this view but is bordered by the limbus on both margins as shown in C. IVC, inferior vena cava; LA, left atrium; RA, right atrium; SVC, superior vena cava
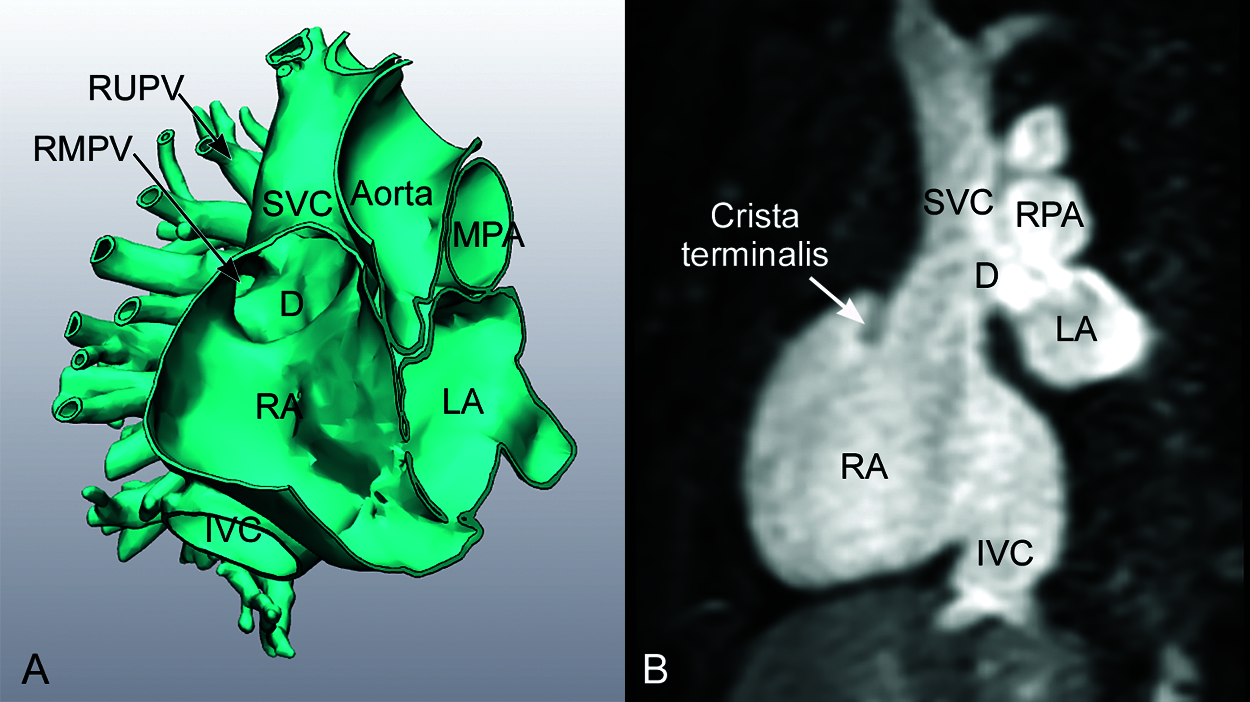
Figure 9: Superior sinus venosus defect with right upper pulmonary vein (RUPV) connecting to the higher level of the superior vena cava and the right middle pulmonary vein (RMPV) connecting to the posterolateral aspect of the cavo-atrial junction. The defect (D) involves the highest part of the party wall and extends further superiorly beyond the interatrial territory. Note that the lower margin of the defect is above the level of the tip of the crista terminalis. In three-dimensional volume rendered image in A, the superior vena cava (SVC) appears to override the atrial septal crest. However, there is no significant overriding of the superior vena cava in two-dimensional section. Neither the superior vena cava nor the atrial septum is malaligned. IVC, inferior vena cava; LA, left atrium; MPA, main pulmonary artery; RA, right atrium; RPA, right pulmonary artery
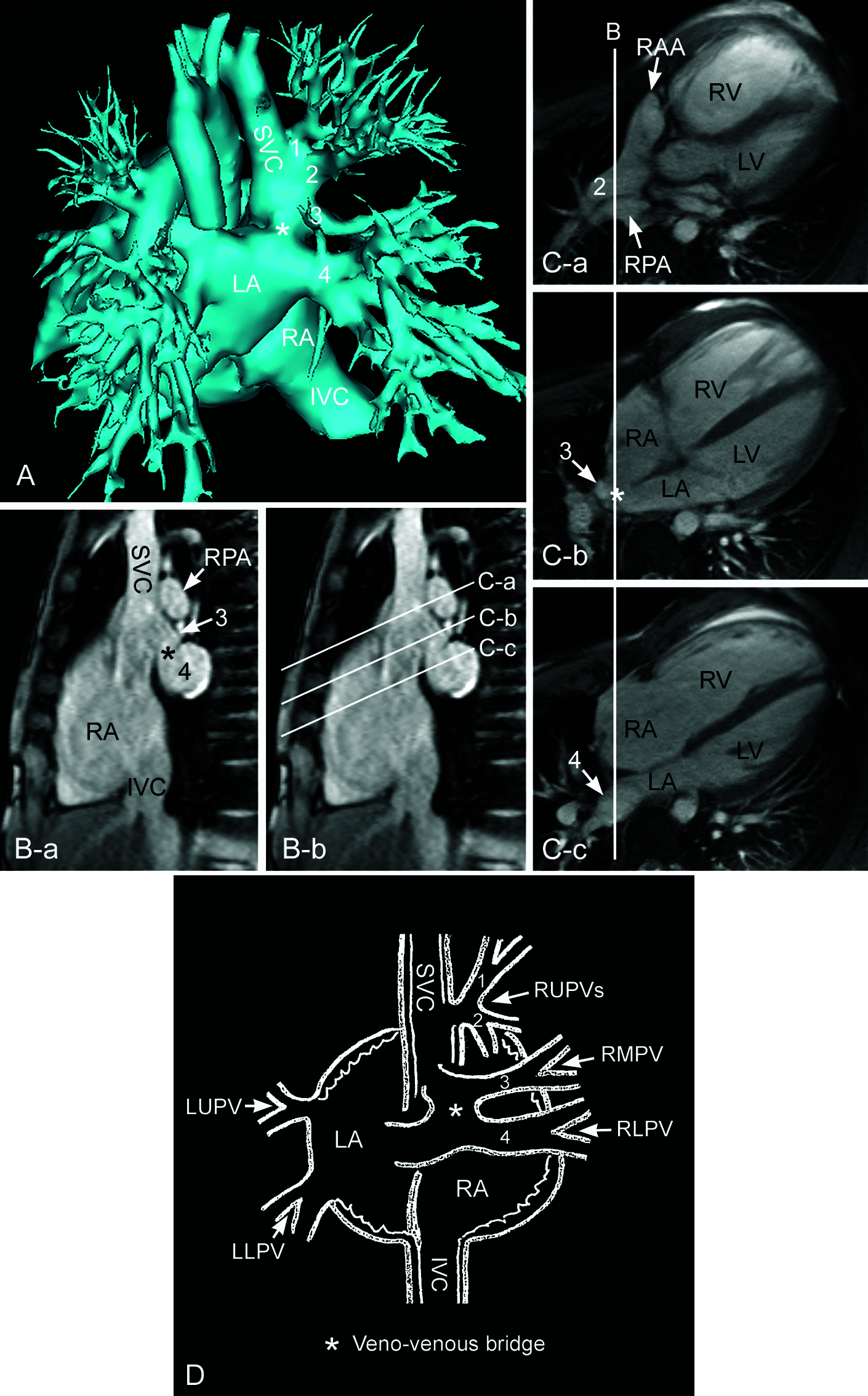
Figure 10: Magnetic resonance images showing superior sinus venosus defect with so-called veno-venous bridge. A. Volume rendered contrast enhanced angiogram. B. Static intercaval or bicaval image. C. Still frames of cine imaging along the planes shown in B. D. Cartoon showing veno-venous bridge. Two pulmonary veins (1 and 2) from the right upper lung connect to the lateral wall of the lower superior vena cava (SVC). Another small pulmonary vein (3) from the right middle lung connects to the posterior lateral wall of the junction between the superior vena cava and the right atrium (RA), forming a small pouch-like space. This small pouch communicates with the large right lower pulmonary vein (4) at its connection to the left atrium (LA) through a defect (asterisk) that can be called a bridge between the right middle and lower pulmonary veins. IVC, inferior vena cava; LLPV, left lower pulmonary vein; LUPV, left upper pulmonary vein; RAA, right atrial appendage; RLPV, right lower pulmonary vein; RMPV, right middle pulmonary vein; RPA, right pulmonary artery; RUPV, right upper pulmonary vein
Infrequently, the interatrial communication is indirectly through the defect between the pulmonary vein that is abnormally connected to the superior vena cava and the right lower pulmonary vein that is connected to the left atrium (Fig. 10). Butts et al. coined the term “veno-venous bridge” for this unique feature [9,18].
The lower part of the superior vena cava usually shows an increased diameter in its transverse dimension at and below the level of the anomalous pulmonary venous connections. Despite the increased diameter, the superior vena cava keeps its normal position and connection to the right atrium in the majority of cases (Figs. 7 and 10). There has been controversy regarding overriding of the superior vena cava across the defective party wall in superior sinus venosus defects. While al Zaghal et al. and others defined overriding of the orifice of the vena cava as the key anatomical criterion for the diagnosis of sinus venosus defects [19], Hsu et al. reported no significant overriding in the majority of their 44 patient surgical series [20]. In our observation from cross-sectional imaging, the alignment of the posterior wall of the superior vena cava and the underlying interatrial party wall is not significantly different from that in normal hearts despite the presence of a hole and the appearance of overriding depends on the observer’s perspective (Figs. 3A and 6 vs. Figs. 8A, 9 and 10). Specifically, the presence or absence and the magnitude of apparent superior vena caval overriding depends on the degree of downward extension of the defect into the atrium. When the defect is small with minimum downward extension, the superior vena cava dose not or barely appears to override the underlying party wall or septum [9,21]. When the defect extends further down to the sloping part of the party wall, the superior vena cava can be perceived as overriding. When the defect extends superiorly, the posterior wall of the left atrium or its confluence with the pulmonary vein may be imperceptibly continuous with the dilated superior vena caval wall, leaving the superior vena cava falsely appearing to override the underlying defective atrial septum (Figs. 9 and 10). Furthermore, overriding of the superior vena cava can be secondary to displacement of the atrial septum toward the right atrium with an elevated left atrial pressure [7]. Apparent overriding of the superior vena cava with preferential streaming of the vena caval flow into the left atrium is only rarely encountered [7,22–24]. From the cross-sectional imaging point of view, overriding of the superior vena cava is a variable feature and should not be used as the diagnostic criterion.
In summary, the superior sinus venosus defect is characterized by abnormal communications between two closely related venoatrial structures: 1) the normally positioned superior vena cava-right atrium complex and 2) the right pulmonary vein-left atrium complex that is displaced leftward, forward and upward. The defect is not a simple hole in the normally existing septal structure or partitioning wall but a far more complex malformation affecting a wider region. Although it is constantly described as the hallmark of the defect in the literature, a hole at the cavoatrial junction is only a part of the complex malformation. Displacement of the right pulmonary veins and adjacent part of the left atrium is universally seen in superior sinus venosus defects and is the major underlying reason for wide morphological variation among cases. Except for the deficiency in its posterior wall, the superior vena cava is positioned and connected normally to the right atrium in the majority of cases. Overriding of the superior vena cava across the party wall or septum is not a consistent finding of the superior sinus venosus defect.
3.2 Inferior Sinus Venosus Defects
The inferior sinus venosus defect affects the lowermost convex part of the interatrial party wall along the sinus venarum. Invariably, the inferior vena cava appears to connect to the left atrium or override the defective atrial septum above. One may speculate malalignment of the atrial septum or malposition of the inferior vena cava as the underlying mechanism for overriding of the inferior vena cava. However, the position of the inferior vena cava and the orientation of the intact part of the atrial septum are not different from those of normal hearts. Overriding of the inferior vena caval orifice is due to the presence of a hole in the interatrial party wall that is normally in the trajectory of the course of the inferior vena cava (Fig. 6). A hole in the sloping posterior inferior part of the interatrial party wall simply lets the vena cava appear to connect to the left atrium especially when the Eustachian valve is prominent (Figs. 11 and 12).
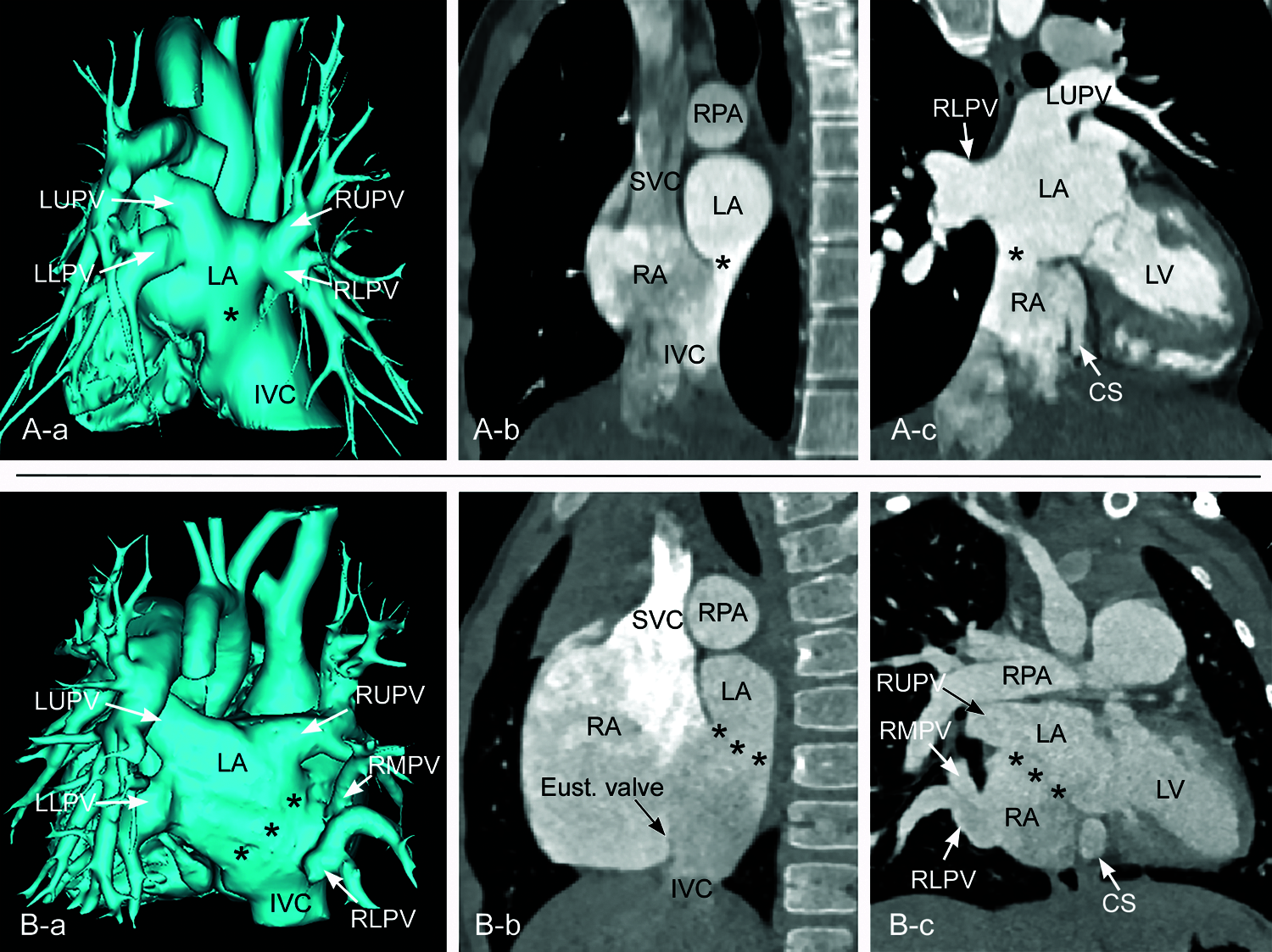
Figure 11: CT angiograms from two different patients showing inferior sinus venosus defects. A. A small defect (asterisk) in the far posterior inferior aspect of the party wall between the right (RA) and left (LA) atria. All pulmonary veins are normally connected to the left atrium. B. A large defect (asterisks) involving the posterior inferior aspect of the party wall between the right and left atria. The right middle and lower pulmonary veins (RMPV and RLPV, respectively) course downward to connect to the lower part of the right atrium. In both cases, the posterior aspect of the inferior vena cava (IVC) is directed toward the left atrium through the defect. In B, the Eustachian valve (Eust.valve) of the inferior vena cava is prominent. CS, coronary sinus; LLPV, left lower pulmonary vein; LUPV, left upper pulmonary vein; LV, left ventricle; RUPV, right upper pulmonary vein; SVC, superior vena cava

Figure 12: Endocardial surface reconstruction of magnetic resonance angiograms from the same patient shown in Fig. 11B, showing the inferior sinus venosus defect. The right anterior wall of the right atrium and ventricle is removed. A is to show the relationship between the fossa ovalis (FO), limbus, coronary sinus ostium (CS) and Eustachian valve (Eust. valve) of the inferior vena cava (IVC). B and C are to show the orifices of the right middle and lower pulmonary veins (RMPV and RLPV, respectively) in relation to the defect and the atrial cavities. A large defect involves the far posterior inferior aspect of the interatrial party wall. The right middle and lower pulmonary veins connect to the lower part of the atrial cavity above the orifice of the inferior vena cava. SVC, superior vena cava
Inferior sinus venosus defects are frequently associated with anomalous connection of the right lower pulmonary vein to the right atrium or inferior vena cavoatrial junction. Some investigators consider the anomalous pulmonary venous connection to be an essential feature of the pathology [25]. However, the inferior sinus venosus defect often occurs with all pulmonary veins normally connected to the left atrium (Fig. 11A) [8,21,26–29]. Therefore, the presence of anomalous pulmonary venous connection to the inferior vena cava or right atrium is not essential for the diagnosis of the inferior sinus venosus defect. Interestingly, inferior sinus venosus defects also may be associated with anomalous connection of the right upper pulmonary vein to the right atrium [30].
In summary, the inferior sinus venosus defect is a congenital malformation that primarily affects the junctional area between the inferior vena cava and the lower part of the sinus venarum. Although frequently associated with an abnormality of the right pulmonary veins, this is not a constant feature required for the diagnosis of an inferior sinus venosus defect. The inferior vena cava appears to override the defective interatrial party wall or septum above or may appear to drain to the left atrium in almost all cases. Importantly, however, this finding is not due to abnormal position or orientation of the inferior vena cava or atrial septum but rather due to the unique alignment of the affected area of the interatrial party wall to the trajectory of the inferior vena cava.
3.3 Other Rare Defects Involving the Limbus of the Fossa Ovalis
An unusual case with the defect involving the limbus of the fossa ovalis midway between the superior and inferior vena caval orifices in the right atrium was also reported [31]. Cases involving the anteroinferior part of the limbus along the atrioventricular septum have also been described by Keith et al. and later called as atrial septal defects of the septum intermedium or vestibular defects [32–35]. One of the authors (SJY) has experienced a case with heterotaxy and left isomerism of the bronchopulmonary and atrial arrangement that had a small defect in the superior part of the limbus away from the orifices of the right and left superior venae cavae (Fig. 13). A similar case was reported as sinus venosus defect by Talwar et al. without description whether the defect involved the cavoatrial junction [36].
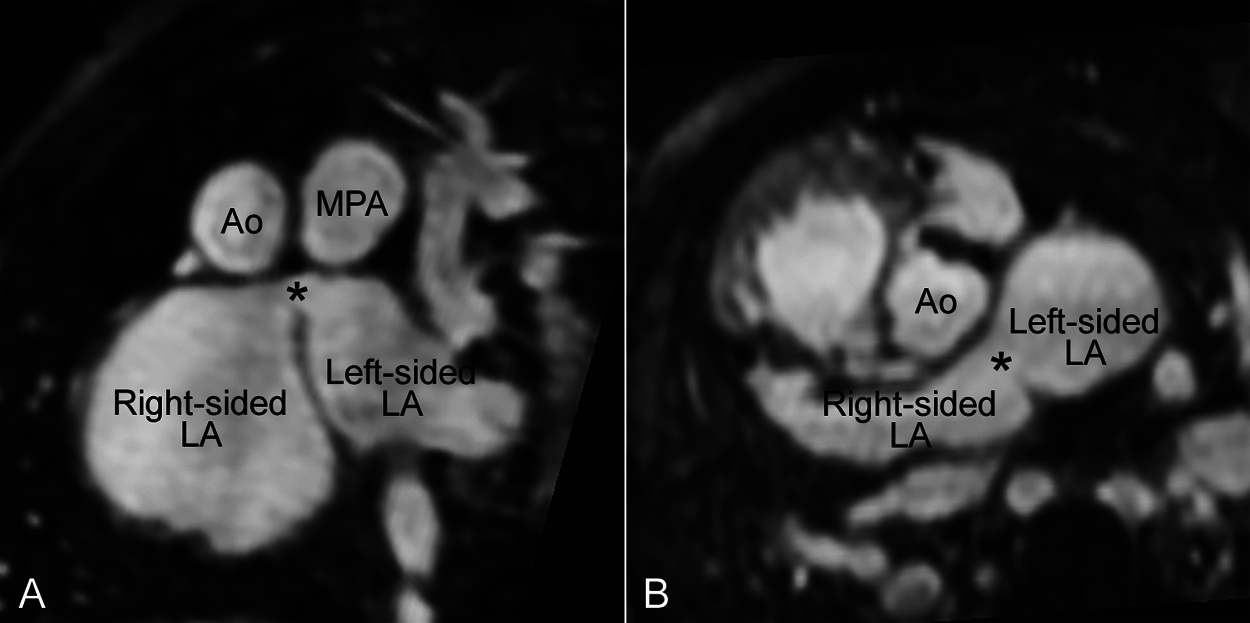
Figure 13: Magnetic resonance angiograms reconstructed in oblique coronal (A) and oblique axial (B) planes showing a defect (asterisk) involving the superior part of the limbus in a patient with heterotaxy and atrial and bronchopulmonary left isomerism. The defect was at distance from the right and left superior vena caval orifices. Ao, aorta; LA, left atrium; MPA, main pulmonary artery
The differentiation of sinus venosus defects from other forms of atrial septal defects is important in planning for surgical versus device closure of the defect [26–27,37,38]. The accuracy of transthoracic echocardiographic diagnosis varies significantly among reported series with adult series invariably showing lower accuracy than pediatric series [39,40]. The diagnosis of inferior sinus venosus defects are particularly challenging with the diagnosis made in less than 50% of cases in earlier reports [25,38]. The major limitation of transthoracic echocardiography is the posterior location of the primary defect that is remote from the transducer on the precordium. The accuracy of echocardiography has improved over time due to observers’ increasing awareness of the morphological characteristics of the defects and by using transesophageal approach, 3D technology and agitated saline contrast [8,27,29,41]. Real-time 3D echocardiography is helpful not only to the imagers for differentiation of the various forms of interatrial communication but also to the surgeons and interventionists for better understanding of spatial orientation of intracardiac anatomy [41].
As sinus venosus defects involve the most posterior aspect of the interatrial party wall, the defects are characterized by the absence of a posterior atrial rim along the free wall of the atrium in axial or short axis planes [8,27–29], which is described as “bald” posterior atrial wall (Figs. 11A–b and 11B–b) [28]. Precise unequivocal localization of the superior sinus venosus defect can be made using a parasagittal imaging plane along the sinus venarum, i.e., the parasternal intercaval or bicaval view [21,29,41–43]. The parasternal intercaval view is also a diagnostic plane for the inferior sinus venosus defect. However, a defect involving the most posterior and inferior part of the fossa ovalis can also be seen in this plane (Figs. 8C, 14 and 15) but without bald posterior atrial wall. Remnant of the attenuated limbus is seen as a small spur-like projection from the posterior atrial wall. As the limbus of the fossa ovalis is normally indistinct inferiorly toward the inferior vena caval orifice, the differentiation of the low lying secundum defect and the true inferior sinus venosus defect can be difficult at surgical inspection as well as at imaging.
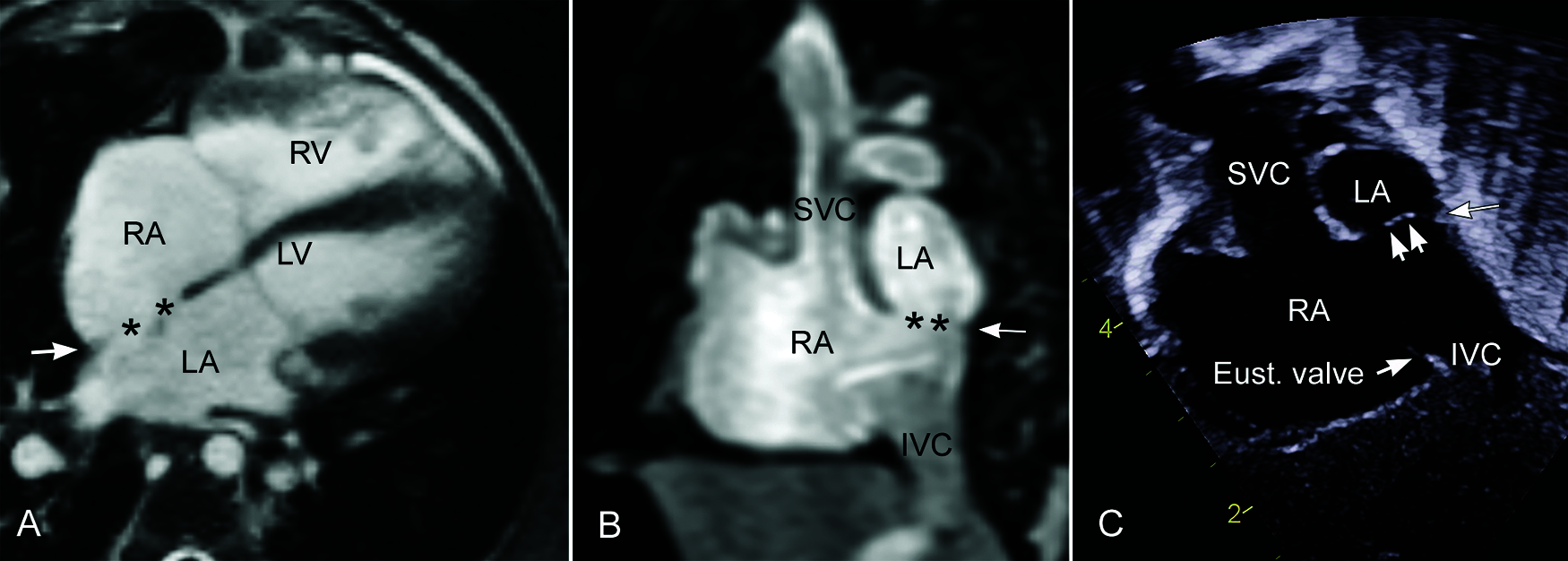
Figure 14: Secundum atrial septal defects located far posteroinferiorly in the fossa ovalis. Magnetic resonance images in axial (A) and parasagittal intercaval (B) planes show the defects (asterisks) involving the fossa ovalis with a small ridge of limbus (arrow) along the posterior and inferior atrial wall. A defect shown in parasagittal plane is similar to an inferior sinus venosus defect. Note the remnant membranous fossa ovalis in echocardiogram in (C). Mildly prominent Eustachian valve (Eust. valve) is aligned with the superior part of the limbus
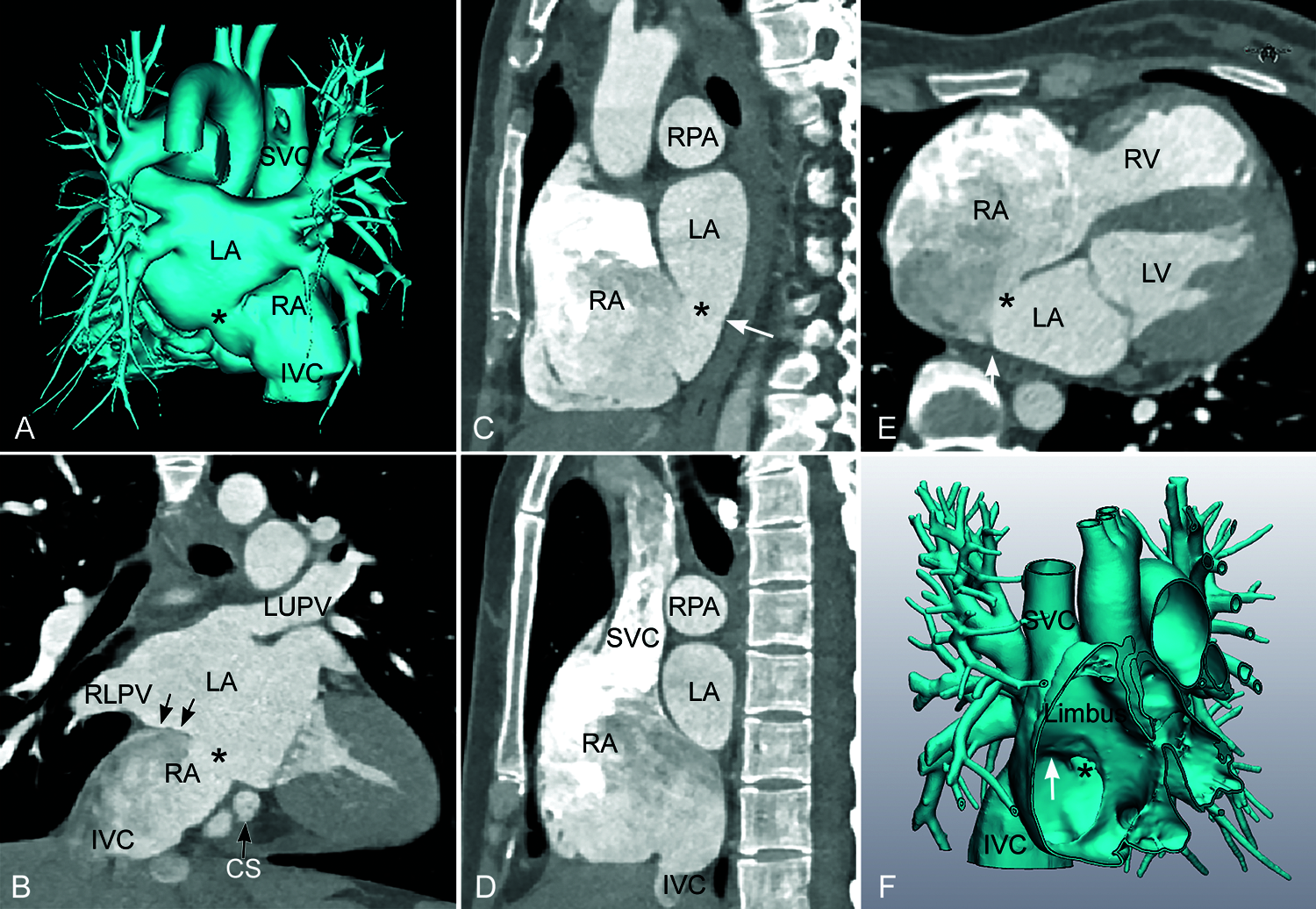
Figure 15: Computed tomographic angiograms obtained from a patient with a low-lying secundum atrial septal defect. Although both imaging and surgical reports described that the defect (asterisk) was an inferior sinus venosus defect, it does not involve the classic location for this type of defect (marked with an arrow in F). Furthermore, the posterior part of the limbus (arrow in C and E) is seen as a small spur-like projection from the posterior wall of the atrium. Volume-rendered image in A shows that the defect is more medially than the true inferior sinus venosus defect shown in Fig. 11. Note that the defect is not aligned with the axis of the superior and inferior venae cavae (SVC and IVC, respectively). LA, left atrium; LUPV, left upper pulmonary vein; RA, right atrium; RLPV, right lower pulmonary vein; RPA, right pulmonary artery
While 3D echocardiography is helpful in assessment of the intracardiac anatomy, both MRI and CT are excellent tools for realistic 3D visualization of the normal and anomalous pulmonary veins [44–48]. MRI is the most comprehensive imaging modality that provides not only precise 3D anatomical information but also accurate hemodynamic data including the amounts of shunt through the defect and anomalous pulmonary vein(s) and the ventricular volumes and function [44–47]. Both MRI and CT angiograms can be used for 3D modeling and printing for feasibility of catheter-based closure of the defect or surgical guidance and simulation (Fig. 16) [49–53].
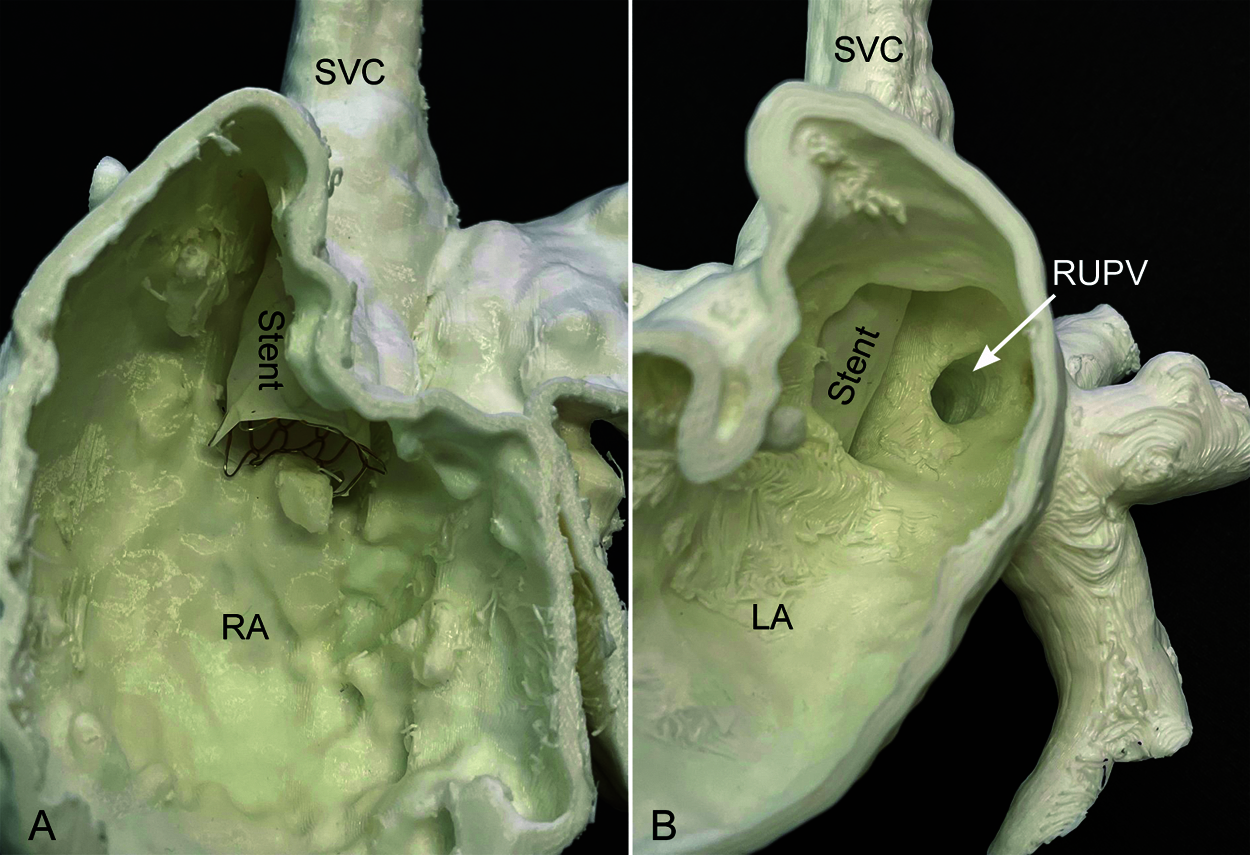
Figure 16: 3D printed model of superior sinus venosus defect. Feasibility of the placement of a covered stent is tested on the model. The inside of the right atrium in A shows that the stent is well positioned from the lower superior vena cava (SVC) to the right atrium (RA) across the defect. The inside of the left atrium in B shows that the orifice of the right upper pulmonary vein (RUPV) is left behind the stent so that it drains to the left atrium (LA)
Surgical treatment has been the standard care until recently. The goal of correction is closure of the interatrial communication with unobstructed drainage of the pulmonary veins to the left atrium and the vena cava to the right atrium. The surgical correction usually consists of rerouting of the anomalous pulmonary vein or veins to the left atrium using a pericardial patch or baffle with or without enlargement of the sinus venosus defect [54–56].
In patients with superior sinus venosus defect, a single autologous pericardial patch/baffle can be sufficient to restore the pulmonary venous return to the left atrium without narrowing of the superior vena caval drainage (single patch technique). When the primary patch/baffle encroaches on the superior vena caval lumen significantly, an additional pericardial patch is applied to the superior vena cava/right atrium to secure unobstructed flow through it (double patch technique) [57]. However, the incision across the cavoatrial junction may result in sinus node dysfunction particularly when a double patch technique is used [56,58]. Direct closure of the defect has been reported in rare instances as well. When the anomalous pulmonary vein is at some distance from the defect, reimplantation of the anomalous vein to the left atrial wall may be required. As reimplantation is associated with a high incidence of postoperative obstruction, the anomalous vein draining a small part of the right lung can better be unaddressed. When a single or double patch technique is deemed to compromise the pulmonary venous and/or superior vena caval patency or result in sinus node damage, Warden procedure is performed [59]. The Warden procedure consists of transection of the superior vena cava above the level of the anomalous pulmonary venous connection, routing of the transected lower part of the superior vena cava to the left atrium using the sinus venosus defect, and connection of the transected upper part of the superior vena cava to the right atrial appendage [59–61].
Reports on surgical correction of the inferior sinus venosus defect are scarce. As the preoperative diagnosis is frequently incorrect, the surgeon’s awareness of the defect is important [38]. The inferior vena caval cannula may obscure visibility of the inferior sinus venosus defect during surgery if the diagnosis is not made preoperatively [62]. When there is a secundum atrial septal defect as well as the inferior sinus venosus defect, the latter may escape detection at both imaging and surgery [62]. Banka et al. showed that rates of misdiagnosis of inferior sinus venosus defect were associated with worse technical outcome scores and greater frequency of reintervention [38]. The intraoperative finding for the inferior sinus venosus defect may be confusing when the prominent Eustachian valve appears to be aligned with the intact atrial septum above the defect [63]. The surgeon may mistakenly apply a patch along the inferior margin of the defective atrial septum and the free edge of the Eustachian valve, leaving the inferior vena cava draining completely into the left atrium [63–69].
Since its introduction in 2013 by Abdullah et al. and in 2014 by Garg et al, transcatheter approach using a covered stent has increasingly been adapted [53,70–72]. A large clinical series showed a suitability of transcatheter correction in >75% of patients with superior sinus venosus defect [53]. Unsuitability of the procedure included the connection of the anomalous pulmonary vein(s) to the superior vena cava well above the right atrial junction or along the anterior wall, potential pulmonary venous compression with stenting and large defects. Catheter treatment of the inferior sinus venosus defects has been regarded unfeasible with only a few cases reported in the literature [73,74].
Superior and inferior sinus venosus defects share a common generic name because of the involvement of the sinus venarum part of the right atrium. However, they are distinctly different pathologies. The superior sinus venosus defect is characterized by abnormal communications between two closely related venoatrial structures: 1) the normally positioned superior vena cava-right atrium complex and 2) the right pulmonary vein-left atrium complex that is displaced leftward, forward, and upward. It is consistently associated with abnormal number, course and connection of the right pulmonary veins. On the other hand, the appearance of superior vena caval overriding is variable and cannot be used as a diagnostic criterion for the diagnosis. The inferior sinus venosus defect is a congenital malformation affecting the junction between the lower part of the sinus venarum in the right atrium and the inferior vena cava. Presence of a defect in this region leaves the inferior vena caval orifice appearing to override the defective party wall or septum. Although it is frequently associated with abnormal connection of the right lower pulmonary vein(s) to the right atrium or cavoatrial junction, it is not a constant feature that is required for the diagnosis.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present article.
1. Ross, D. N. (1956). The sinus venosus type of atrial septal defect. Guy’s Hospital Report, 105, 376–381. [Google Scholar]
2. Jacobs, J. P., Quintessenza, J. A., Burke, R. P., Mavroudis, C. (2000). Congenital heart surgery nomenclature and database project: Atrial septal defect. The Annals of Thoracic Surgery, 69(4 Suppl), S18–24. [Google Scholar]
3. Backer, C. L., Mavroudis, C. (2013). Atrial septal defect, partial anomalous pulmonary venous connection, and scimitar syndrome. In: Mavroudis, C., Backer, L. C. (Eds.Pediatric cardiac surgery. 4th ed., pp. 259–310. USA: Blackwell Publishing Ltd. [Google Scholar]
4. Redington, R. N., Anderson, R. H., Spicer, D. E. (2020). Interatrial communications. In: Wernovsky, G. (Ed.Anderson’s pediatric cardiology. 4th ed., pp. 503–515. USA: Elsevier. [Google Scholar]
5. van Praagh, S., Carrera, M. E., Sanders, S. P., Mayer, J. E., van Praagh, R. (1994). Sinus venosus defects: Unroofing of the right pulmonary veins-anatomic and echocardiographic findings and surgical treatment. American Heart Journal, 128(2), 365–379. DOI 10.1016/0002-8703(94)90491-X. [Google Scholar] [CrossRef]
6. Anderson, R. H., Ettedgui, J. A., Devine, W. A. (1995). Sinus venosus defect. American Heart Journal, 129(6), 1229–1232. DOI 10.1016/0002-8703(95)90423-9. [Google Scholar] [CrossRef]
7. van Praagh, S., Geva, T., Lock, J. E., Nido, P. J., Vance, M. S. et al. (2003). Biatrial or left atrial drainage of the right superior vena cava: Anatomic, morphogenetic, and surgical considerations-report of three new cases and literature review. Pediatric Cardiology, 24(4), 350–363. DOI 10.1007/s00246-002-0329-7. [Google Scholar] [CrossRef]
8. Oliver, J. M., Gallego, P., Gonzalez, A., Dominguez, F. J., Aroca, A. et al. (2002). Sinus venosus syndrome: Atrial septal defect or anomalous venous connection? a multiplane transoesophageal approach. Heart, 88(6), 634–638. DOI 10.1136/heart.88.6.634. [Google Scholar] [CrossRef]
9. Butts, R. J., Crean, A. M., Hlavacek, A. M., Spicer, D. E., Cook, A. C. et al. (2011). Veno-venous bridges: The forerunners of the sinus venosus defect. Cardiology in the Young, 21(6), 623–630. DOI 10.1017/S1047951111000710. [Google Scholar] [CrossRef]
10. Anderson, R. H., Cook, A. C. (2007). The structure and components of the atrial chambers. Europace, 9 (Suppl 6), vi3–9. DOI 10.1093/europace/eum200. [Google Scholar] [CrossRef]
11. Rana, B. S., Shapiro, L. M., McCarthy, K. P., Ho, S. Y. (2010). Three-dimensional imaging of the atrial septum and patent foramen ovale anatomy: Defining the morphological phenotypes of patent foramen ovale. European Journal of Echocardiography, 11(10), i19–25. DOI 10.1093/ejechocard/jeq122. [Google Scholar] [CrossRef]
12. Naqvi, N., McCarthy, K. P., Ho, S. Y. (2018). Anatomy of the atrial septum and interatrial communications. Journal of Thoracic Disease, 10(Suppl 24), S2837–S2847. DOI 10.21037/jtd. [Google Scholar] [CrossRef]
13. Li, J., Al Zaghal, A. M., Anderson, R. H. (1998). The nature of the superior sinus venosus defect. Clinical Anatomy, 11(5), 349–352. DOI 10.1002/(ISSN)1098-2353. [Google Scholar] [CrossRef]
14. Ferreira Martins, J. D., Anderson, R. H. (2000). The anatomy of interatrial communications-what does the interventionist need to know? Cardiology in the Young, 10(5), 464–473. DOI 10.1017/S1047951100008155. [Google Scholar] [CrossRef]
15. Joshi, S. D., Chawre, H. K., Joshi, S. S. (2016). Morphological study of fossa ovalis and its clinical relevance. Indian Heart Journal, 68(2), 147–152. DOI 10.1016/j.ihj.2015.08.001. [Google Scholar] [CrossRef]
16. Klimek-Piotrowska, W., Hołda, M. K., Koziej, M., Piątek, K., Hołda, J. (2016). Anatomy of the true interatrial septum for transseptal access to the left atrium. Annals of Anatomy, 205, 60–64. DOI 10.1016/j.aanat.2016.01.009. [Google Scholar] [CrossRef]
17. Kiserud, T. (1994). Developmental anatomy. In: Kiserud, T. (Ed.The ductus venosus in the human fetus. An ultrasonographic study of its functional anatomy, normal blood flow velocity and its changes during fetal disease, pp. 17–20. Norway: Trondheim, University of Trondheim. [Google Scholar]
18. Aramendi, J. I., Cubero, A., Hamzeh, G., Rey, E. (2014). Cavopulmonary window: An extreme form of sinus venosus defect. Interactive Cardiovascular Thoracic Surgery, 18(2), 253–256. DOI 10.1093/icvts/ivt489. [Google Scholar] [CrossRef]
19. al Zaghal, A. M., Li, J., Anderson, R. H., Lincoln, C., Shore, D. et al. (1997). Anatomical criteria for the diagnosis of sinus venosus defects. Heart, 78(3), 298–304. DOI 10.1136/hrt.78.3.298. [Google Scholar] [CrossRef]
20. Hsu, H. M., Chang, Y. T., Su, W. J., Chu, J. J., Chang, Y. S. et al. (2020). The morphogenesis and associated anomalous pulmonary venous drainage in sinus venosus defect. Pediatric Neonatology, 61(1), 92–99. DOI 10.1016/j.pedneo.2019.06.013. [Google Scholar] [CrossRef]
21. Tretter, J. T., Chikkabyrappa, S., Spicer, D. E., Backer, C. L., Mosca, R. S. et al. (2017). Understanding the spectrum of sinus venosus interatrial communications. Cardiology in the Young, 27(3), 418–426. DOI 10.1017/S1047951116000664. [Google Scholar] [CrossRef]
22. Abadeer, M., Luceri, M., Abraham, B. (2019). Rare case of a superior sinus venosus atrial septal defect presenting with cyanosis. Cardiology in the Young, 29(4), 544–546. DOI 10.1017/S1047951119000234. [Google Scholar] [CrossRef]
23. Abu-Anza, O., Ashwath, R. (2019). Biatrial drainage of right superior caval vein with preferential streaming into the left atrium. Cardiology in the Young, 29(7), 996–998. DOI 10.1017/S1047951119001276. [Google Scholar] [CrossRef]
24. Shariat, M., Grosse-Wortmann, L., Yoo, S. J., Seed, M., Honjo, O. (2012). Normal drainage, abnormal connection: Partial anomalous pulmonary venous connection and sinus venosus atrial septal defect with a Net right-to-left shunt. World Journal for Pediatric and Congenital Heart Surgery, 3(4), 508–510. DOI 10.1177/2150135112454146. [Google Scholar] [CrossRef]
25. Crystal, M. A., Al Najashi, K., Williams, W. G., Redington, A. N., Anderson, R. H. (2009). Inferior sinus venosus defect: Echocardiographic diagnosis and surgical approach. The Journal of Thoracic Cardiovascular Surgery, 137(6), 1349–1355. DOI 10.1016/j.jtcvs.2008.12.010. [Google Scholar] [CrossRef]
26. Chen, C. A., Wang, J. K., Hsu, J. Y., Hsu, H. H., Chen, S. J. et al. (2010). Diagnosis of inferior sinus venosus atrial septal defects using transthoracic three-dimensional echocardiography. Journal of the American Society of Echocardiography, 23(4), e454–e456. DOI 10.1016/j.echo.2009.09.008. [Google Scholar] [CrossRef]
27. Plymale, J., Kolinski, K., Frommelt, P., Bartz, P., Tweddell, J. et al. (2013). Inferior sinus venosus defects: Anatomic features and echocardiographic correlates. Pediatric Cardiology, 34(2), 322–326. DOI 10.1007/s00246-012-0449-7. [Google Scholar] [CrossRef]
28. Snarr, B. S., Liu, M. Y., Zuckerberg, J. C., Falkensammer, C. B., Nadaraj, S. et al. (2017). The parasternal short-axis view improves diagnostic accuracy for inferior sinus venosus type of atrial septal defects by transthoracic echocardiography. Journal of the American Society of Echocardiography, 30(3), 209–215. DOI 10.1016/j.echo.2016.12.007. [Google Scholar] [CrossRef]
29. Tomar, M., Radhakrishnan, S., Kaushal, S. K., Dagar, K. S., Iyer, K. S. et al. (2012). Inferior-type caval vein defect--echocardiographic and surgical description of a large series of patients. Cardiology in the Young, 22(3), 270–278. DOI 10.1017/S104795111100120X. [Google Scholar] [CrossRef]
30. Prasad, D., Snyder, C., Ashwath, R. (2015). Septum primum malposition defect and inferior sinus venosus defect: A rare association. Cardiology in the Young, 25(7), 1389–1392. DOI 10.1017/S1047951114001899. [Google Scholar] [CrossRef]
31. Erickson, L. C., Cocalis, M. W., Lamberti, J. J. (1996). Unusual “midseptal” sinus venosus defect. Pediatric Cardiology, 17(1), 60–62. DOI 10.1007/BF02505816. [Google Scholar] [CrossRef]
32. Goor, D. A., Lillehei, C. W. (1975). Atrial septal defects. In: Goor, D. A., Lillehei, C. W. (Eds.Congenital Malformations of the Heart, pp. 103–111. USA: Grune & Stratton. [Google Scholar]
33. Keith, A. (1903). The anatomy of valvular mechanism around the venous orifices of the right and left auricles with some observations on the morphology of the heart. Journal of Anatomy (Proceedings) 37:2. (Cited from Reference 31.). [Google Scholar]
34. Sharratt, G. P., Webb, S., Anderson, R. H. (2003). The vestibular defect: An interatrial communication due to a deficiency in the atrial septal component derived from the vestibular spine. Cardiology in the Young, 13(2), 184–190. DOI 10.1017/S1047951103000349. [Google Scholar] [CrossRef]
35. Loomba, R. S., Tretter, J. T., Mohun, T. J., Anderson, R. H., Kramer, S. et al. (2020). Identification and morphogenesis of vestibular atrial septal defects. Journal of Cardiovasc Development and Diseases, 7(3), 35. DOI 10.3390/jcdd7030035. [Google Scholar] [CrossRef]
36. Talwar, S., Ramakrishnan, P., Anderson, R. H., Choudhary, S. K., Makhija, N. et al. (2016). Left isomerism of the atrial appendages with sinus venosus defect and anomalous systemic venous drainage. World Journal for Pediatric and Congenital Heart Surgery, 7(5), 661–664. DOI 10.1177/2150135115610283. [Google Scholar] [CrossRef]
37. Mathewson, J. W., Bichell, D., Rothman, A., Ing, F. F. (2004). Absent posteroinferior and anterosuperior atrial septal defect rims: Factors affecting nonsurgical closure of large secundum defects using the amplatzer occluder. Journal of the American Society of Echocardiography, 17(1), 62–69. DOI 10.1016/j.echo.2003.09.018. [Google Scholar] [CrossRef]
38. Banka, P., Bacha, E., Powell, A. J., Benavidez, O. J., Geva, T. (2011). Outcomes of inferior sinus venosus defect repair. The Journal of Thorac and Cardiovscular Surgery, 142(3), 517–522. DOI 10.1016/j.jtcvs.2011.01.031. [Google Scholar] [CrossRef]
39. Mühler, E. G., Engelhardt, W., von Bernuth, G. (1992). Detection of sinus venosus atrial septal defect by two-dimensional echocardiography. European Heart Journal, 13(4), 453–456. DOI 10.1093/oxfordjournals.eurheartj.a060196. [Google Scholar] [CrossRef]
40. Kronzon, I., Tunick, P. A., Freedberg, R. S., Trehan, N., Rosenzweig, B. P. et al. (1991). Transesophageal echocardiography is superior to transthoracic echocardiography in the diagnosis of sinus venosus atrial septal defect. Journal of the American College of Cardiology, 17(2), 537–542. DOI 10.1016/S0735-1097(10)80128-7. [Google Scholar] [CrossRef]
41. Valente, A. M., Sena, L., Powell, A. J., Del Nido, P. J., Geva, T. (2007). Cardiac magnetic resonance imaging evaluation of sinus venosus defects: Comparison to surgical findings. Pediatric Cardiology, 28(1), 51–56. [Google Scholar]
42. Kafka, H., Mohiaddin, R. H. (2009). Cardiac MRI and pulmonary MR angiography of sinus venosus defect and partial anomalous pulmonary venous connection in cause of right undiagnosed ventricular enlargement. American Journal of Roentgenology, 192(1), 259–266. [Google Scholar]
43. Gulati, G. S., Hoey, E. T., Gopalan, D., Agrawal, B. S., Screaton, N. J. (2010). Sinus venosus atrial septal defect in adults: Utility of cardiovascular MRI in resolving this diagnostic dilemma. Heart Lung and Circulation, 19(10), 615–619. [Google Scholar]
44. Prompona, M., Muehling, O., Naebauer, M., Schoenberg, S. O., Reiser, M. et al. (2011). MRI for detection of anomalous pulmonary venous drainage in patients with sinus venosus atrial septal defects. International Journal of Cardiovascular Imaging, 27(3), 403–412. [Google Scholar]
45. Amat, F., Le Bret, E., Sigal-Cinqualbre, A., Coblence, M., Lambert, V. et al. (2011). Diagnostic accuracy of multidetector spiral computed tomography for preoperative assessment of sinus venosus atrial septal defects in children. Interactive Cardiovascular and Thoracic Surgery, 12(2), 179–182. [Google Scholar]
46. McDonald, R. W., Rice, M. J., Reller, M. D., Marcella, C. P., Sahn, D. J. (1996). Echocardiographic imaging techniques with subcostal and right parasternal longitudinal views in detecting sinus venosus atrial septal defects. Journal of the American Society of Echocardiography, 9(2), 195–198. [Google Scholar]
47. Bilska, K. M., Kehrens, C. M., Riley, G., Anderson, R. H., Marek, J. (2012). Subcostal real-time three-dimensional echocardiography of interatrial communications: Reconstruction of an oval fossa defect, a superior sinus venosus defect with partially anomalous pulmonary venous drainage, an infero-posterior oval fossa defect, and a coronary sinus defect. Cardiology in the Young, 22(2), 145–151. [Google Scholar]
48. Reddy, S. C., Ettedgui, J. A. (1994). Images in cardiovascular medicine. profiles of sinus venosus atrial septal defect. Circulation, 89(6), 2919–2920. [Google Scholar]
49. Thakkar, A. N., Chinnadurai, P., Breinholt, J. P., Lin, C. H. (2018). Transcatheter closure of a sinus venosus atrial septal defect using 3D printing and image fusion guidance. Catheterization and Cardiovascular Intervention, 92(2), 353–357. [Google Scholar]
50. Tandon, A., Burkhardt, B. E. U., Batsis, M., Zellers, T. M., Velasco, F. et al. (2019). Sinus venosus defects: Anatomic variants and transcatheter closure feasibility using virtual reality planning. Journal of the American College of Cardiology: Cardiovascular Imaging, 12(5), 921–924. [Google Scholar]
51. Butera, G., Sturla, F., Pluchinotta, F. R., Caimi, A., Carminati, M. (2019). Holographic augmented reality and 3D printing for advanced planning of sinus venosus ASD/partial anomalous pulmonary venous return. percutaneous management. Journal of the American College of Cardiology: Cardiovascular Interventions, 12(14), 1389–1391. [Google Scholar]
52. Sivakumar, K., Qureshi, S., Pavithran, S., Vaidyanathan, S., Rajendran, M. (2020). Simple diagnostic tools may guide transcatheter closure of superior sinus venosus defects without advanced imaging techniques. Circulation Cardiovascular Interventions, 13(12), e009833. DOI 10.1161/CIRCINTERVENTIONS.120.009833. [Google Scholar] [CrossRef]
53. Hansen, J. H., Duong, P., Jivanji, S. G. M., Jones, M., Kabir, S. et al. (2020). Transcatheter correction of superior sinus venosus atrial septal defects as an alternative to surgical treatment. Journal of the American College of Cardiology, 75(11), 1266–1278. DOI 10.1016/j.jacc.2019.12.070. [Google Scholar] [CrossRef]
54. Attenhofer Jost, C. H., Connolly, H. M., Danielson, G. K., Bailey, K. R., Schaff, H. V. et al. (2005). Sinus venosus atrial septal defect: Long-term postoperative outcome for 115 patients. Circulation, 112(13), 1953–1958. DOI 10.1161/CIRCULATIONAHA.104.493775. [Google Scholar] [CrossRef]
55. Okonta, K. E., Tamatey, M. (2012). Is double or single patch for sinus venosus atrial septal defect repair the better option in prevention of postoperative venous obstruction? Interactive Cardiovascular and Thoracic Surgery, 15(5), 900–903. DOI 10.1093/icvts/ivs369. [Google Scholar] [CrossRef]
56. Stewart, R. D., Bailliard, F., Kelle, A. M., Backer, C. L., Young, L. et al. (2007). Evolving surgical strategy for sinus venosus atrial septal defect: Effect on sinus node function and late venous obstruction. The Annals of the Thorac Surgery, 84(5), 1651–1655. DOI 10.1016/j.athoracsur.2007.04.130. [Google Scholar] [CrossRef]
57. Elzein, C., Abdulkarim, M., Abbas, U., Vricella, L., Ilbawi, M. (2020). Repair of superior sinus venosus atrial septal defect using a modified two-patch technique. The Annals of the Thorac Surgery, 109(2), 583–587. DOI 10.1016/j.athoracsur.2019.07.023. [Google Scholar] [CrossRef]
58. Stephens, E. H., Mongé, M. C., Eltayeb, O., Patel, A., Webster, G. et al. (2021). Evolution and current results of a unified strategy for sinus venosus surgery. The Annals of the Thorac Surgery, 111(3), 980–986. DOI 10.1016/j.athoracsur.2020.03.113. [Google Scholar] [CrossRef]
59. Warden, H. E., Gustafson, R. A., Tarnay, T. J., Neal, W. A. (1984). An alternative method for repair of partial anomalous pulmonary venous connection to the superior vena cava. The Annals of the Thorac Surgery, 38(6), 601–605. DOI 10.1016/S0003-4975(10)62317-X. [Google Scholar] [CrossRef]
60. Agrawal, G., Das, A. (2019). Tetralogy of fallot with interatrial communication of the inferior sinus venosus type: A rare association causing post-operative desaturation. World Journal for Pediatric and Congenital Heart Surgery, 10(6), 801–802. DOI 10.1177/2150135119874033. [Google Scholar] [CrossRef]
61. Alkady, H., Elnaggar, A., Eldegwy, M., Nosair, A. (2020). The warden procedure for partial anomalous pulmonary venous connection in children: 10 years experience in 65 cases. Cardiology in the Young, 30(10), 1486–1489. DOI 10.1017/S1047951120002516. [Google Scholar] [CrossRef]
62. Fagan, S., Veinot, J. P., Chan, K. L. (2001). Residual sinus venosus atrial septal defect after surgical closure of atrial septal defect. Journal of the American Society of Echocardiography, 14(7), 738–741. DOI 10.1067/mje.2001.111005. [Google Scholar] [CrossRef]
63. Lin, F., Tang, H., Xiao, X. (2015). Surgical repair of inferior sinus venosus defects: A novel approach with unsnared inferior vena cava. Journal of Cardiothoracic Surgery, 10, 158. DOI 10.1186/s13019-015-0359-x. [Google Scholar] [CrossRef]
64. Desnick, S. J., Neal, W. A., Nicoloff, D. M., Moller, J. H. (1976). Residual right-to-left shunt following repair of atrial septal defect. The Annals of the Thorac Surgery, 21(4), 291–295. DOI 10.1016/S0003-4975(10)64313-5. [Google Scholar] [CrossRef]
65. Sapin, P. M., Salley, R. K. (1997). Arterial desaturation and orthodeoxia after atrial septal defect repair: Demonstration of the mechanism by transesophageal and contrast echocardiography. Journal of the American Society of Echocardiography, 10(5), 588–592. DOI 10.1016/S0894-7317(97)70017-8. [Google Scholar] [CrossRef]
66. Becker, A., Buss, M., Sebening, W., Meisner, H., Döhlemann, C. (1999). Acute inferior cardiac inflow obstruction resulting from inadvertent surgical closure of a prominent eustachian valve mistaken for an atrial septal defect. Pediatric Cardiology, 20(2), 155–157. DOI 10.1007/s002469900427. [Google Scholar] [CrossRef]
67. Tayeh, C., El Khoury, M., Bitar, F., Arabi, M. (2019). Atrial septal defect closure complicated by anomalous inferior vena cava return to the left atrium: A case report of a 5-year-old child. European Heart Journal Case Reports, 3(2). DOI 10.1093/ehjcr/yty169. [Google Scholar] [CrossRef]
68. Jain, S. A., Pinto, R., Dalvi, B. (2012). Iatrogenic diversion of IVC to left atrium after surgical closure of ASD. Annals of Pediatric Cardiology, 5(1), 72–74. DOI 10.4103/0974-2069.93716. [Google Scholar] [CrossRef]
69. Uga, S., Hidaka, T., Takasaki, T., Kihara, Y. (2014). A case of residual inferior sinus venosus defect after ineffective surgical closure. British Medical Journal Case Reports, 2014, bcr2014205377. DOI 10.1136/bcr-2014-205377. [Google Scholar] [CrossRef]
70. Abdullah, H. A. M., Alsalkhi, H. A., Khalid, K. A. (2020). Transcatheter closure of sinus venosus atrial septal defect with anomalous pulmonary venous drainage: Innovative technique with long-term follow-up. Catheterization and Cardiovascular Interventions, 95(4), 743–747. DOI 10.1002/ccd.28364. [Google Scholar] [CrossRef]
71. Garg, G., Tyagi, H., Radha, A. S. (2014). Transcatheter closure of sinus venosus atrial septal defect with anomalous drainage of right upper pulmonary vein into superior vena cava--an innovative technique. Catheterization and Cardiovascular Interventions, 84(3), 473–477. DOI 10.1002/ccd.25502. [Google Scholar] [CrossRef]
72. Rosenthal, E., Qureshi, S. A., Jones, M., Butera, G., Sivakumar, K. et al. (2021). Correction of sinus venosus atrial septal defects with the 10 zig covered cheatham-platinum stent–an international registry. Catheterization and Cardiovascular Interventions, 98(1), 128–136. DOI 10.1002/ccd.29750. [Google Scholar] [CrossRef]
73. Kim, H. D., Kim, M. S., Yun, K. J., Bae, S. M., Her, S. H. et al. (2016). Successful transcatheter closure of an inferior sinus venosus atrial septal defect. Korean Journal of Internal Medicone, 31(1), 176–178. DOI 10.3904/kjim.2016.31.1.176. [Google Scholar] [CrossRef]
74. He, L., Cheng, G. S., Du, Y. J., Zhang, Y. S. (2020). Feasibility of device closure for multiple atrial septal defects with an inferior sinus venosus defect: Procedural planning using three-dimensional printed models. Heart Lung and Circulaton, 29(6), 914–920. DOI 10.1016/j.hlc.2019.07.004. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |