
 | Congenital Heart Disease |  |
DOI: 10.32604/chd.2022.019025
ARTICLE
Predictors and Effects of Persistent Hypertension after Successful Treatment of Coarctation of the Aorta
Ain Shams University, Cairo, Egypt
*Corresponding Author: Mohamed Saber Hafez. Email: dr.mohammadsaber@yahoo.com
Received: 09 September 2021; Accepted: 18 November 2021
Abstract: Background: Coarctation of the aorta is a congenital heart disease that sometimes remains clinically silent until adulthood, usually presenting with arterial hypertension. It is well known that after coarctation treatment, many patients remain hypertensive despite successful repair. In this study we approached the predictors and effects of residual hypertension after successful coarctation therapy. Methods: It was a cross sectional observational study involving 50 patients who underwent Coarctation repair/angioplasty in Ain Shams university hospitals. We divided the patients into two groups (hypertensive and normotensive) and we studied their demographic data (e.g., age, gender, age at first repair, follow up period, etc.) to conclude the possible predictors of persistent hypertension in such cases. We also performed full echocardiographic assessment including 3D speckle tracking echocardiography to detect subtle changes in left ventricular systolic functions. Results: Hypertensive patients had significantly higher BMI (29.1 kg/m2) as compared to normotensives (24 kg/m2), p < 0.0001. Age at first CoA intervention was significantly higher in hypertensive patients. Hypertensive patients had significantly lower 3D left ventricular strain measures (Global area strain, global circumferential strain and global longitudinal strain). The incidence of bicuspid aortic valve was significantly higher in the hypertensive group, yet it was not an independent predictor of persistent hypertension. Conclusions: The predictors for residual hypertension post successful CoA repair were late intervention and higher BMI. Bicuspid aortic valve was more common in the hypertensive group. Regarding the effects of such disease domain, treated CoA patients with persistent hypertension tended to have higher LV mass index and lower values of LV deformation.
Keywords: Coarctation; arterial hypertension; speckle tracking; left ventricular strain
Coarctation of the aorta (CoA) is the most common congenital disease of the thoracic aorta, consisting of an aortic constriction due to prominent ductal ridge usually located just distal to the left subclavian artery. Significant coarctation occurs if the diameter of the tightest aortic segment is smaller than half of the diameter of the abdominal aorta. CoA may present early in life with heart failure symptoms, or may remain clinically silent until adolescence or adulthood, the most common late presentation being hypertension [1].
After successful treatment of CoA, whether surgically or catheter based, not all adult patients regain normal arterial blood pressure (ABP). Depending on the series reviewed and definition used, more than one third of all patients with repaired CoA will have systemic hypertension by 20–30 years after operation, and this subset of patients has more adverse outcome [2].
The pathophysiology of hypertension after coarctation repair is not fully understood. Restenosis or residual stenosis accounts for only a minority of cases of postoperative hypertension. Two hypotheses are postulated to explain this observation: either CoA may be a manifestation of a generalized vascular abnormality (NOTCH1 gene mutation), or CoA may produce an effect on the “upstream” vasculature before repair, that is not completely reversible in some subjects [3].
This was a cross sectional observational study involving 50 patients who underwent Coarctation repair/angioplasty in Ain shams university hospitals. The study group was subdivided into two groups as follows:
Group 1 included 25 patients with Coarctation of the Aorta who previously underwent successful intervention (surgical or catheter based)in the period between January 2018 and March 2020, aged between 15 and 40 years and suffering from arterial hypertension at the time of the study (April and May 2021). Hypertension (HTN) was defined according to the recent 2017 ACC guidelines, and arterial blood pressure was considered high if more than or equal to 130/80 mmHg [4].
Group 2 included 25 patients with Coarctation of the Aorta with the same criteria as in Group 1 but were normotensive at the time of study (April and May 2021).
Exclusion Criteria
1. All patients with complicated interventions, e.g., stent fracture or Aortic aneurysm.
2. Aortic Recoarctation, defined as narrowest diameter at the CoA segment being less than half of the diameter of the Abdominal Aorta below the diaphragm during Echocardiography [3].
3. Associated hemodynamically significant cardiac anomalies (except Bicuspid Aortic Valve and Parachute Mitral Valve without hemodynamically significant effects).
4. Hypertensive patients on antihypertensive medications with controlled blood pressure.
Approval of Ain Shams University ethical committee was achieved (FWA 000017585, Approval No. FMASU MD 23/2021), and informed consent was obtained from each selected patient in privacy.
Detailed history was taken from all patients, with special care to symptoms (e.g., dyspnea, headache, epistaxis), number of previous interventions, type of each intervention, age at first intervention and current medical therapy.
General Examination and local cardiac examination were performed during the study period with special emphasis on measurement of office arterial blood pressure (ABP).
Proper technique for ABP measurement was done; the patient sitting relaxed for five minutes before measurement with an empty bladder and with no caffeine intake nor exercise in the past thirty minutes. Two measurements were taken 5 min apart, and average was used. If there was a significant difference between both readings, a third measurement was obtained.
Proper cuff size was chosen, and the arm positioned at the level of the Right Atrium (midpoint of sternum). Systolic and diastolic blood pressures were recorded as onset of the first Korotkoff sound and disappearance of all Korotkoff sounds, respectively.
Comparison between upper limb and lower limb blood pressure was performed and examination of peripheral pulsations was done. Body mass index (BMI) was calculated from weight and height.
Echocardiography was performed for every patient using a GE E95 Echocardiography machine with an S3 probe with frequency range from 5 to 1 Megahertz according to Body Surface area.
2.3.1 Two-Dimensional (2D) Echocardiography
Each patient lied in supine and left lateral positions; full echocardiographic study was performed by an experienced operator using 2D, M mode and color flow Doppler. To obtain LV dimensions and wall thickness, parasternal long axis view was used. M-mode cursor was positioned perpendicular to the long axis of the ventricle just below the tips of the mitral valve leaflets. LV end systolic and end diastolic diameters were obtained, as well as LV posterior wall thickness and septal thickness.
Left ventricular ejection fraction (LVEF) was measured using a modified Simpson method with tracing the LV endocardial border in the apical 4- and 2-chamber views in both end-diastole and end-systole by which End-diastolic volume (EDV) and end-systolic volume (ESV) were measured and the LVEF was calculated:
LV mass index (LVMI) was calculated as follows:
LV mass = 1.05 ([LVIDD + PWTD + IVSTD]3- [LVIDD]3) g divided by Body surface area in m2.
(LVIDD = Left Ventricular Internal Diameter in Diastole, PWTD = Posterior Wall Thickness in Diastole, IVSTD = Interventricular Septum Thickness in Diastole) [5].
2.3.2 Aortic Coarctation Assessment
Suprasternal window using 2D, color flow mapping and Doppler assessment of:
- Aortic arch sidedness, diameters and anatomy
- Diameter of the Abdominal Aorta below the diaphragm
- Residual stenosis at the site of aortic coarctation by recording Doppler pressure gradient across site of lesion
-Any complications, e.g., Recoarctation, Aneurysm formation, Stent migration
2.3.3 Three-Dimensional (3D) Echocardiographic Strain Quantification
For 3D echocardiography, a fully sampled matrix-array transducer with almost 3,000 active elements was used (4V-D; GE E95 Vingmed Ultrasound AS). The 3D echocardiographic data was acquired in an adjustable volume divided into six equal divisions. The acquisition was triggered to the R wave of the electrocardiogram. To ensure the correct spatial registration of each subvolume, the acquisitions were obtained in an end-expiratory breath-hold lasting 6 to 8 seconds to ensure optimal temporal and spatial resolution.
Offline data analysis was performed using the original raw data from all 3D data sets on an EchoPAC software workstation (version BT11, 4D Auto LVQ; GE Vingmed Ultrasound AS) for semiautomated endocardial surface detection. The 3D echocardiographic strain analysis allows measurement of the 3D global longitudinal strain (GLS) and global circumferential strain (GCS) (Fig. 2). Global Area Strain (GAS) was calculated as the percentage variation in the surface area defined by the longitudinal and circumferential strain vectors [6].
A flow chart summarizing the methodology of the study is shown in Fig. 1.

Figure 1: Consort flow diagram of the study
Data were collected, coded, tabulated and then statistically analyzed using IBM SPSS Statistics version 25 (IBM Corporation, Armonk, NY, USA). Categorical variables were expressed as number and percentage and analyzed using chi-square test. Continuous variables were expressed as mean ± SD and analyzed using student’s t-test for variables that passed normality tests and Mann-Whitney U-test for those that did not pass normality. Correlations were analyzed using Pearson’s correlation coefficient (r) and Spearman correlation for categorical variables. Logistic regression was used to generate independent predictors for persistence of hypertension. A probability value p < 0.05 was considered statistically significant.
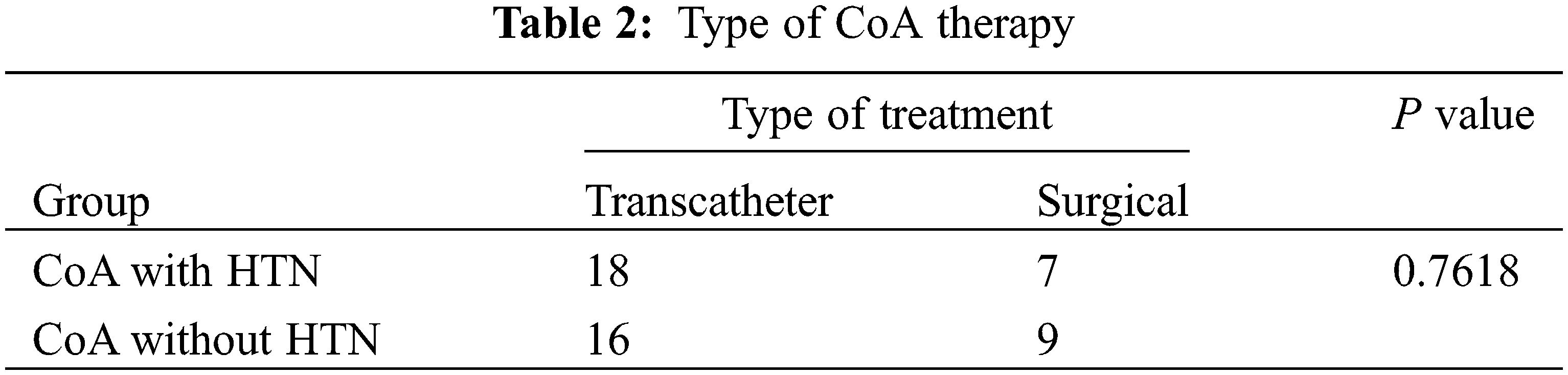
The study population was divided into two groups, Group 1 were hypertensive at the time of examination and Group 2 were normotensive. Nearly a quarter (24%) of the Group 1 were not on any antihypertensive therapy and the rest were on one or more drugs yet were uncontrolled. The mean age of patients at time of study, gender and follow up period (time from last intervention) were similar in both groups (Table 1). Group 1 patients had significantly higher BMI (29.1 kg/m2) as compared to Group 2 (24 kg/m2). Age at first CoA intervention was significantly higher in Group 1. The type of intervention (surgical vs. catheter based) showed no difference between both groups. (Table 2).
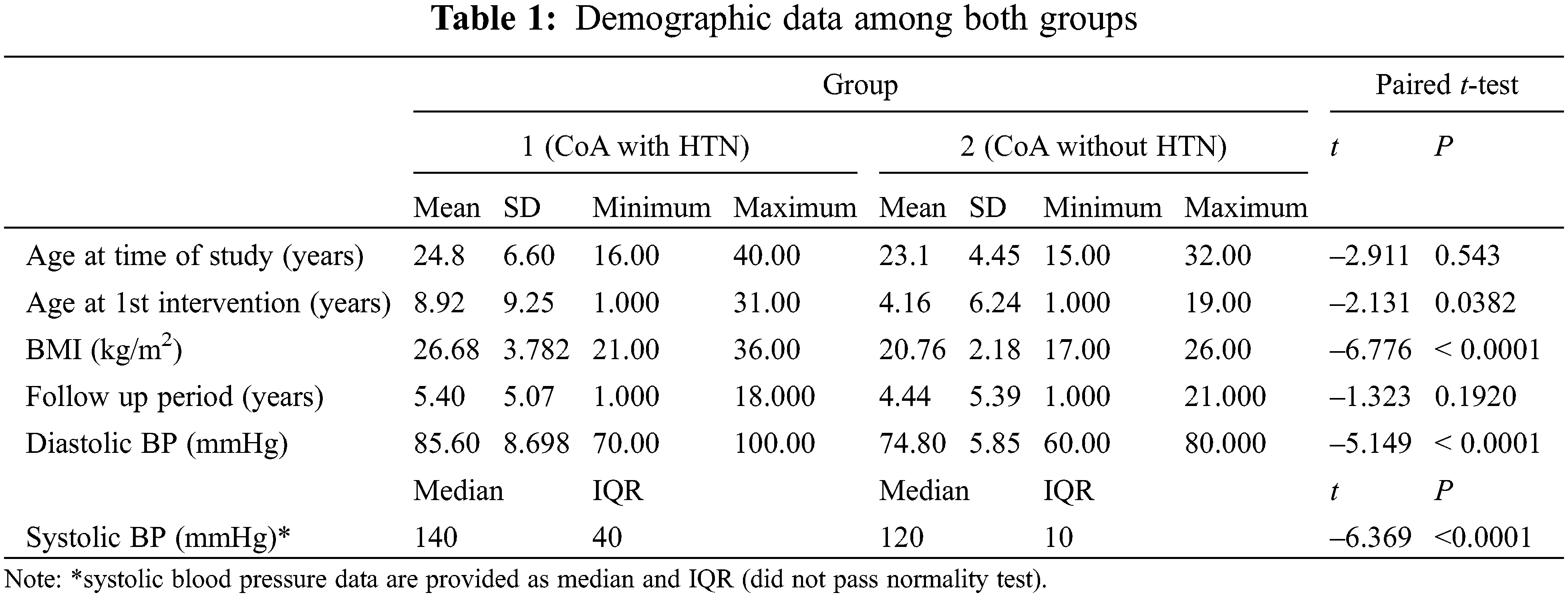
Both groups had normal mean LVEF (65% in Group 1 and 63% in Group 2) and similar CoA site pressure gradient (23 mmHg in Group 1 and 23 mmHg in Group 2). The mean LV mass index was significantly higher in Group 1 (119 g/m2) than in Group 2 (83 g/m2). Group 1 patients had significantly lower 3D LV strain measures (Global area strain, global circumferential strain and global longitudinal strain) as shown in Table 3.
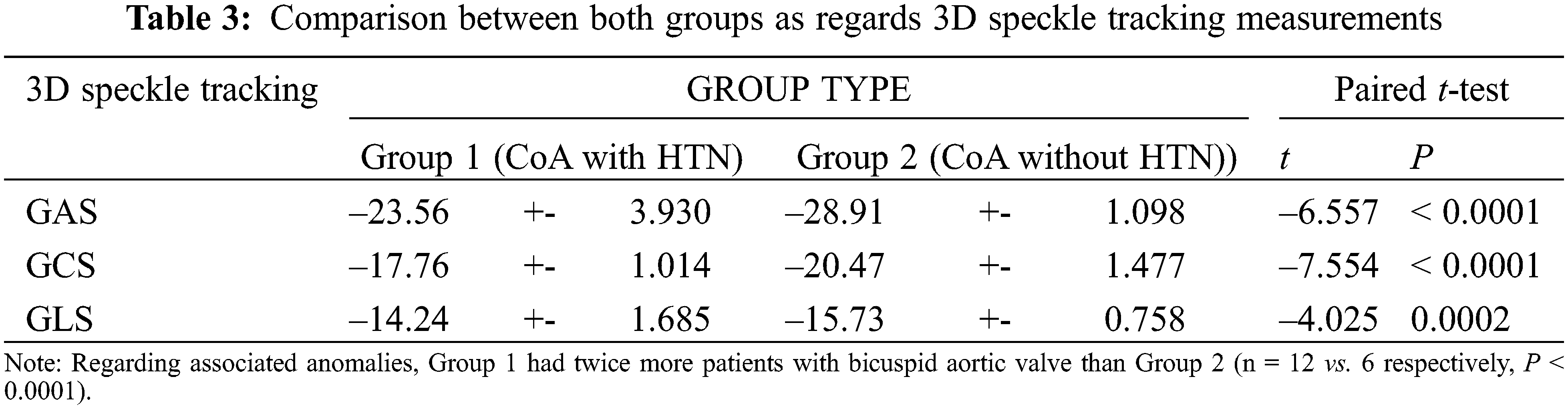
Age at first intervention correlated positively with systolic and diastolic ABP and (r = 0.65, 0.52) and with BMI (r = 0.59). Age at first intervention also showed positive correlation with LV mass index (r = 0.58) and with LV strain levels (GAS, GCS and GLS) with r = 0.46, 0.47 and 0.58, respectively. Arterial blood pressure readings correlated positively with LV mass index (r = 0.38) as well as with GAS, GCS and GLS (r = 0.46, 0.41, 0.55). This means that late age of first intervention and higher blood pressures were associated with higher LV mass and lower LV strain (strain is a negative value) (Figs. 2–5).

Figure 2: Correlation between age at first intervention and LVMI

Figure 3: Correlation between age at first intervention and GLS

Figure 4: Correlation between age at first intervention and GCS

Figure 5: Correlation between age at first intervention and GAS
LVMI correlated positively with GAS, GCS and GLS with r = 0.58, 0.65, 0.55, respectively, indicating that LV hypertrophy was associated with subtle LV systolic dysfunction. BMI correlated positively with ABP (r = 0.55) and LVMI (r = 0.47), but not with LV strain.
Logistic regression analysis was used to determine the most independent predictors of persistence of hypertension among patients post Coarctation repair or percutaneous intervention. All variables which showed significant difference between the 2 subgroups were retained in the logistic regression analysis. The most independent predictors were found to be later age at first intervention (odds ratio 1.1462 (95% CI, 1.0334 to 1.2713)) and higher BMI (odds ratio 1.9379 (95% CI, 1.2384 to 3.0326)). Bicuspid aortic valve did not prove to be an independent predictor.
The significant predictors of hypertension post Coarctation repair in our study were higher age at first intervention, higher BMI. Lower age of first intervention was also associated with better LV strain values.
Many hypotheses were postulated to explain the persistence of hypertension in more than one third of patients despite adequate CoA treatment, like generalized vasculopathy, abnormal NOTCH 1 gene expression, abnormal aortic arch geometry and activation of the renin angiotensin system [7].
A previous study concluded that older age and higher BMI were associated with persistence of hypertension due to loss of aortic elasticity. They also found that longer CoA stent length was associated with higher ABP [8].
A systematic review to study hypertension after CoA repair included many studies from 1987 to 2012 and concluded that older age at first intervention, older age at follow up and repair by patch aortoplasty were all associated with persistent hypertension [9].
Another study concluded that treated CoA patients who have high ABP readings during ambulatory blood pressure monitoring have reduced arterial reactivity to nitrates and increased LV mass, with subsequent adverse effect on late morbidity and mortality [10].
To the best of our knowledge after revision of previous literature, bicuspid aortic valve was not proven to be a predictor of persistent HTN in CoA, though this issue was not extensively studied. In this study bicuspid aortic valve was significantly higher in the hypertensive group yet did not prove to be an independent predictor of persistent HTN. Further studies will be needed with larger number of subjects to prove or disprove this correlation.
Regarding the effects of persistent hypertension after successful CoA repair, we concluded that LV mass increases and subtle LV dysfunction develops (as measured by speckle tracking).
Transient aortic constriction in animal models caused persistent elevation in central systolic pressure and a two-fold increase in LV collagen deposition [11].
In another previous study, global area strain proved to be a sensitive marker of subendocardial damage after CoA repair and was especially impaired in hypertensive patients. This finding was very similar to our results [12].
The predictors for residual hypertension post successful CoA repair were late intervention and higher BMI. Bicuspid aortic valve was more common in the hypertensive group. Treated CoA patients with persistent hypertension tend to have higher LV mass index and lower values of LV deformation as measured by 3D speckle tracking as compared to normotensive patients.
Our study was a single center study with limited number of patients. The follow up period was relatively short. An important subset of patients (hypertensive subjects controlled on medical treatment) was excluded from the study. ABP measurement was not done by ambulatory blood pressure monitoring devices, raising the issue of the possibility of falsely including white coat hypertension amongst the hypertensive group.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Doshi, A. R., Chikkabyrappa, S. (2018). Coarctation of aorta in children. Cureus, 10(12), e3690. DOI 10.7759/curues.3690. [Google Scholar] [CrossRef]
2. Rodrigues, J., Jaring, M., Werndle, M. C., Mitrousi, K., Lyen, S. M. et al. (2019). Repaired coarctation of the aorta, persistent arterial hypertension and the selfish brain. Journal of Cardiovascular Magnetic Resonance, 21(1), 68. DOI 10.1186/s12968-019-0578-8. [Google Scholar] [CrossRef]
3. Dijkema, E. J., Leiner, T., Grotenhuis, H. B. (2017). Diagnosis, imaging and clinical management of aortic coarctation. Heart, 103(15), 1148–1155. DOI 10.1136/heartjnl-2017-311173. [Google Scholar] [CrossRef]
4. Whelton, P. K., Carey, R. M., Aronow, W. S., Casey, D. E., Jr, Collins, K. J. et al. (2017). ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. Journal of the American College of Cardiology, 71(19), e127–e248. DOI 10.1161/HYP.0000000000000065. [Google Scholar] [CrossRef]
5. Lang, R. M., Badano, L. P., Mor-Avi, V., Afilalo, J., Armstrong, A. et al. (2015). Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the american society of echocardiography and the european association of cardiovascular imaging. Journal of the American Society of Echocardiography, 28(1), 1–39.e14. DOI 10.1016/j.echo.2014.10.003. [Google Scholar] [CrossRef]
6. Galderisi, M., Esposito, R., Schiano-Lomoriello, V., Santoro, A., Ippolito, R. et al. (2012). Correlates of global area strain in native hypertensive patients: A three-dimensional speckle-tracking echocardiography study. European Heart Journal–Cardiovascular Imaging, 13(9), 730–738. DOI 10.1093/ehjci/jes026. [Google Scholar] [CrossRef]
7. Kenny, D., Hijazi, Z. M. (2011). Coarctation of the aorta: From fetal life to adulthood. Cardiology Journal, 18(5), 487–495. DOI 10.5603/CJ.2011.0003. [Google Scholar] [CrossRef]
8. Iriart, X., Laïk, J., Cremer, A., Martin, C., Pillois, X. et al. (2019). Predictive factors for residual hypertension following aortic coarctation stenting. Journal of Clinical Hypertension, 21(2), 291–298. DOI 10.1111/jch.13452. [Google Scholar] [CrossRef]
9. Canniffe, C., Ou, P., Walsh, K., Bonnet, D., Celermajer, D. (2013). Hypertension after repair of aortic coarctation--A systematic review. International Journal of Cardiology, 167(6), 2456–2461. DOI 10.1016/j.ijcard.2012.09.084. [Google Scholar] [CrossRef]
10. de Divitiis, M., Pilla, C., Kattenhorn, M., Donald, A., Zadinello, M. et al. (2003). Ambulatory blood pressure, left ventricular mass, and conduit artery function late after successful repair of coarctation of the aorta. Journal of the American College of Cardiology, 41(12), 2259–2265. DOI 10.1016/S0735-1097(03)00480-7. [Google Scholar] [CrossRef]
11. Liu, J., Drak, D., Krishnan, A., Chen, S. Y., Canniffe, C. et al. (2017). Left ventricular fibrosis and systolic hypertension persist in a repaired aortic coarctation model. Annals of Thoracic Surgery, 104(3), 942–949. DOI 10.1016/j.athoracsur.2017.02.027. [Google Scholar] [CrossRef]
12. Kowalik, E., Kowalski, M., Klisiewicz, A., Hoffman, P. (2016). Global area strain is a sensitive marker of subendocardial damage in adults after optimal repair of aortic coarctation: Three-dimensional speckle-tracking echocardiography data. Heart and Vessels, 31(11), 1790–1797. DOI 10.1007/s00380-016-0803-4. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |