
 | Congenital Heart Disease |  |
DOI: 10.32604/chd.2022.021778
ARTICLE
Predictors of Health-Related Quality of Life in Children with Cyanotic Heart Disease Who Underwent Palliative and Total Repair
1Department of Anesthesiology, Faculty of Medicine, Prince of Songkla University, Songkhla, 90110, Thailand
2Department of Surgery, Faculty of Medicine, Prince of Songkla University, Songkhla, 90110, Thailand
3Department of Pediatrics, Faculty of Medicine, Prince of Songkla University, Songkhla, 90110, Thailand
*Corresponding Author: Maliwan Oofuvong. Email: oomaliwa@gmail.com
Received: 04 February 2022; Accepted: 22 March 2022
Abstract: Background: Studies on predictors of health-related quality of life (HRQOL) in pediatric patients with cyanotic heart disease who are waiting for the next stage and those who have undergone total repair are scarce. Therefore, we aimed to identify such predictors in children who received the modified Blalock–Taussig shunt (MBTS) and those who underwent total repair. Methods: In this historical cohort and concurrent follow-up study, data of children who underwent MBTS at the age of 0–3 years between January 2005 and December 2016 at a super-tertiary care hospital in Southern Thailand were obtained. Children who were alive in December 2017 were recruited to evaluate the quality of life at least 1 year after their operation. Between January and December 2018, the “Pediatric Quality of Life Inventory 4.0 Generic Core Scales” with both child self-report and parent proxy-report scores were used to examine the HRQOL. Multivariate linear regression analysis was performed to identify independent predictors of HRQOL. Beta-coefficient (β) and 95% confidence intervals (95% CIs) were calculated and considered statistically significant at p < 0.05. Results: Among the 380 enrolled children, 148 died, 122 survived and waited for total repair, and 110 survived after total repair. In the multivariate analysis, chronic lung disease was a common predictor of lower physical and psychosocial HRQOL reported by the parents (β [95% CI]: −0.42 [−0.81, −0.03] and −0.49 [−0.89, −0.09], respectively). Total repair was a predictor of higher physical HRQOL according to both parents and children (β [95% CI]: 0.33 [0.09, 0.57] and 0.70 [0.36, 1.03], respectively). A predictor of higher psychosocial HRQOL reported by the parents was younger age during MBTS surgery compared with older age (β [95% CI]: 0.012 [0.001, 0.022]). In the total repair subgroup, undergoing the Fontan procedure (vs. Glenn procedure) was a predictor for lower physical HRQOL reported by the parents (β [95% CI]: −0.82 [−1.52, −0.13]). Higher socioeconomic status was a predictor of both physical and psychosocial HRQOL (β [95% CI]: 0.018 [0.001, 0.034] and 0.012 [0.0001, 0.04], respectively). Conclusions: Successful total repair was a predictor of higher physical HRQOL, and younger age during MBTS surgery was a predictor of higher psychological HRQOL in children with cyanotic heart disease. Higher socioeconomic status was a predictor of both physical and psychological HRQOL following total repair [Thai Clinical Trials Registry: TCTR20161221003].
Keywords: Children; modified Blalock–Taussig shunt; predictors; health-related quality of life; total repair
Systemic-to-pulmonary artery shunt is a palliative procedure for children with cyanotic congenital heart disease (CHD) to improve the blood flow to the lung. Currently, the modified Blalock–Taussig shunt (MBTS) is the most commonly used palliative shunt. Since 2000, the discharge mortality rate following MBTS surgery has continued to decline [1]. Children who survive the MBTS procedure further require total correction. The target of the current therapy has shifted its focus from not only improving the survival rate but also enhancing the health-related quality of life (HRQOL). HRQOL is defined as the level of satisfaction and happiness that affects an individual’s life, especially when children have to cope with illnesses or treatment. It is a multi-dimensional concept that is related to the physical, mental, and social functions of an individual [2].
Previous studies have reported that children with non-complex CHD have poorer physical function than their healthy counterparts [3]. Other factors that may worsen HRQOL in children following CHD surgery include lower age at the time of surgery, complex CHD, and low socioeconomic status [4–6]. There are limited data comparing HRQOL in children with complex CHD between palliative shunt and total repair procedures. Therefore, in this study, we aimed to determine whether the total repair procedure improved HRQOL and to compare its outcome with that of a palliative shunt, as well as investigating other factors that affect the HRQOL in children who underwent the MBTS procedure.
This was the second part of a historical cohort and concurrent follow-up study (Thai Clinical Trials Registry: TCTR20161221003). The study was approved by the Institutional Ethics Committee of the Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand (EC 64-067-08-01). Written informed consent for all children and assent for those aged >7 years for the HRQOL assessment were obtained. The inclusion criteria were children aged 1–18 years who had undergone the MBTS procedure at the age of 0–3 years between January 2006 and December 2016 and were awaiting total repair, or had already progressed to the next stage by December 2017 [7]. Children who were lost to follow-up or did not want to participate in the study were excluded. The appointment was made at least 1 year after undergoing the MBTS procedure or total repair/progression to the next stage. Children were interviewed by a pediatric psychologist, and their parents assessed the child’s quality of life by answering a questionnaire.
The outcomes of interest included the HRQOL assessed using the Pediatric Quality of Life Inventory (PedsQL) for children aged at least 2 years and the Pediatric Quality of Life Inventory Infant Scale for children aged < 2 years. The Generic Core Scales Version 4.0 PedsQL includes 23 items. The quality-of-life score was evaluated separately according to each parent and child. The questionnaire for the parent-proxy report was used for children aged between 1 and 18 years whereas the questionnaire for child self-report was used for children aged between 5 and 18 years. Both questionnaires were the same and included questions concerning physical function (8 items), emotional function (5 items), social function (5 items), and school function (5 items). Each question was answered on a scale of 0–4 (0 = never a problem [100 points]; 1 = almost never a problem [75 points]; 2 = sometimes a problem [50 points], 3 = often a problem [25 points], and 4 = almost always a problem [0 point]). These scales were subsequently converted into a total score of 0–100. Physical health referred to physical function (P1/C1). Psychosocial health was the combination of emotional function (P3/C3), social function (P4/C4), and school function (P6/C6). A high score indicated a good quality of life. The PedsQL Infant Scale consisted of a questionnaire for the parent only (assessed in infants aged < 2 years). The questionnaire was evaluated using five topics to evaluate the physical function (P1), physical symptoms (P2), emotional function (P3), social function (P4), and cognitive function (P5). Physical health was the combination of physical function (P1) and physical symptoms (P2). Psychosocial health was the combination of emotional function (P3), social function (P4), and cognitive function (P5). This questionnaire has been validated by Varni et al. [8] in children and passed the reliability test. Its translation and cultural adaptation into Thai were performed by the Mapi Research Institute (https://www.mapi-trust.org) according to the international guidelines.
2.1.1 Details of Quality-of-Life Score
Physical function (P1/C1) consisted of 8 items: walking more than 1 block, running, exercising/playing sports, lifting heavy objects, showering by oneself, doing house chores, pain level, energy level. Emotional function (P3/C3) consisted of 5 items: fearness, sorrow, anger, difficulty sleeping, anxiety. Social function (P4/C4) consisted of 5 items: socializing with friends, playing with friends, being bullied, not being able to do tasks while friend(s) can, getting tired when playing with friend(s). School function (P6/C6) consisted of 5 items: focusing during a class, memorizing problems, finishing a task, missing class due to illness, missing class due to hospitalization. Physical symptoms (P2) was added and cognitive function (P5) was used instead of school function (P6/C6) in infants aged < 2 years. Physical symptoms consisted of the following items: abdominal distension, breathing difficulty, wheezing, swallowing difficulty, constipation, diarrhea, vomiting, rash. Cognitive function problems included: not copying parent’s acting, not copying parent’s facial expression, not copying parent’s voice, not focusing on the environment.
Total repair/progression to the next stage was defined as having undergone the Glenn/Fontan procedure, total correction, Rastelli procedure, or arterial switch procedure depending on the cardiac diagnosis. The palliative shunt group was defined as children who received an MBTS as a definite treatment or who were waiting for the next stage of repair.
2.3 Explanatory Variables/Confounding Factors
The variables collected were categorized into patient-related factors, anesthesia-related factors, and surgery-related factors. Patient-related factors included the age during the MBTS procedure, age at the time of the assessment of the quality of life (QOL), weight during the operation, preterm (gestational age < 37 weeks), cardiac diagnosis (categorized as Tetralogy of Fallot [TOF], univentricular heart [UVH], pulmonary atresia with ventricular septal defect [PA/VSD], and transposition of great arteries [TGA]), non-cardiac abnormalities (categorized as a syndrome, such as dextrocardia, asplenia, delayed development, or chronic lung disease), history of preoperative hypoxic spells, and socioeconomic status. Socioeconomic status was assessed using the Hollingshead two factors index of social position (level of education and parents’ income) [9]. Anesthesia-related factors included the American Society of Anesthesiologists (ASA) classification, intraoperative hypoxemia (arterial oxygen saturation [SpO2] < 75%), and bradycardia (heart rate below the baseline according to the child’s age, which required atropine). Surgery-related factors included differential oxygen saturation, which was defined as the difference in the oxygen saturation between preoperative and postoperative assessments, the ratio of the shunt size to the body weight, duration of postoperative mechanical ventilator use, duration of stay in the intensive care unit (ICU), re-operative thoracotomy at admission, postoperative complications (shunt thrombosis, congestive heart failure, sepsis, pneumonia, and coagulopathy), history of shunt revision at admission, total repair status, number of MBTS procedures and their complications, length of hospital stay, and readmission within 30 days. In the total repair subgroup, age at total repair and surgery-related factors, such as type of surgery, intraoperative complications, and intraoperative blood loss were included in the analyses.
Data record forms were created, and information was extracted from the electronic medical records. They were then double entered into a database using EpiData software version 3.1 (The EpiData Association, Pascal, Denmark). R software version 4.1.1 (R Core Team, Vienna, Austria) was used to analyze the data. Continuous variables are presented as the median and interquartile range while categorical variables were compared using Fisher’s exact test or Chi-square test where appropriate. Continuous variables were compared using the Wilcoxon rank sum test. A univariate analysis was performed to assess the association between the risk factors and outcomes. Any factor with a p-value < 0.2 in the univariate analysis was included in the multivariate linear regression analysis. The subgroup analysis was performed similarly in patients who underwent total repair. Age at the HRQOL assessment was included in the initial multivariate model regardless of its p-value in the univariate analysis.
The sample size was estimated based on the two independent means formula. To estimate a difference of 10 in HRQOL score between the MBTS group and total repair group with a pooled standard deviation of 10, level of significance of 0.05, and 80% power to detect this difference, the estimated sample size was 17 per group. To identify six predictors, including a missing data rate of 10%, 228 children (114 in each group) were required.
A total of 261 children survived following the MBTS procedure that was performed during the study period at age 0–3 years, of which 122 children were waiting for the next stage and 139 had undergone total repair (Fig. 1).
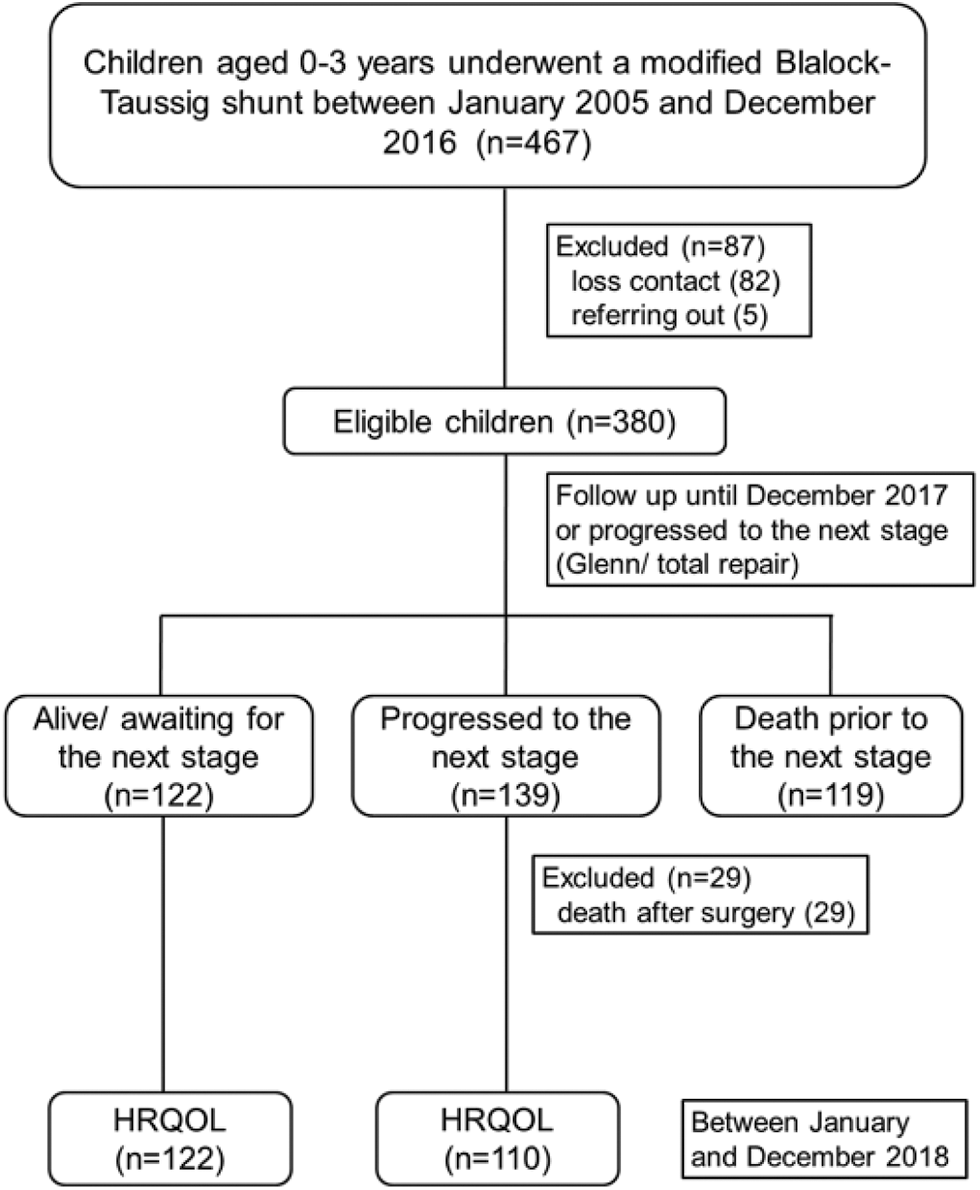
Figure 1: Flowchart depicting the study design. HRQOL, health-related quality of life
Among the 139 who underwent total repair, 29 died. Therefore, 122 children in the MBTS group and 110 children in the total repair group were included in the analyses. Table 1 summarizes the physical and psychosocial HRQOL assessments according to the parents and children between the MBTS and total repair groups.
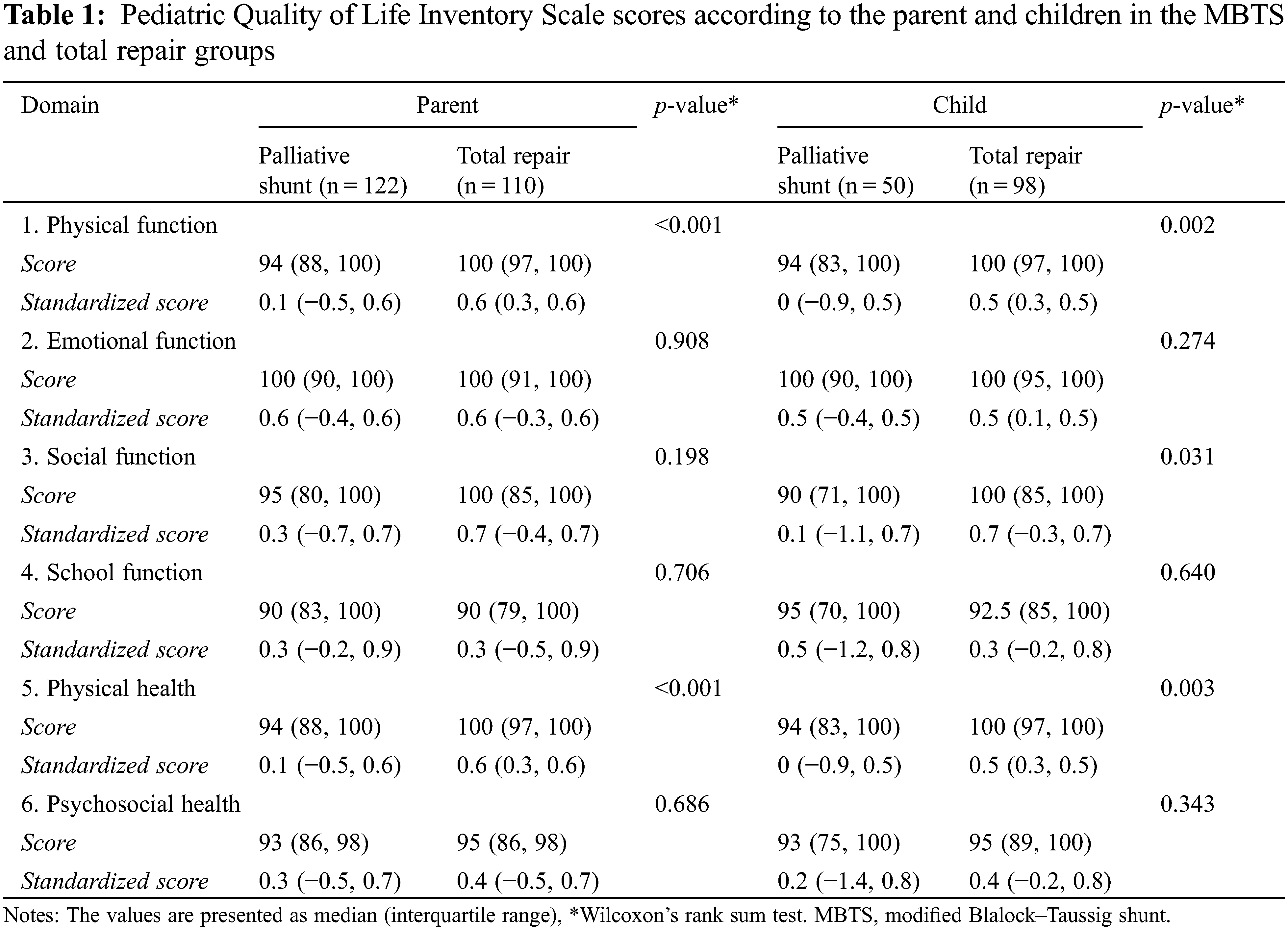
Boxplots demonstrating the scores in each domain in the MBTS and total repair groups according to the parent-proxy report (P1, P3, P4, and P6) and child self-report (C1, C3, C4, and C6) are illustrated in Appendix A and Appendix B, respectively. The physical symptom domain (P2) and cognitive function domain (P5) used for assessments in children aged 1–2 years could not be compared since there were five children in the MBTS group and none in the total repair group.
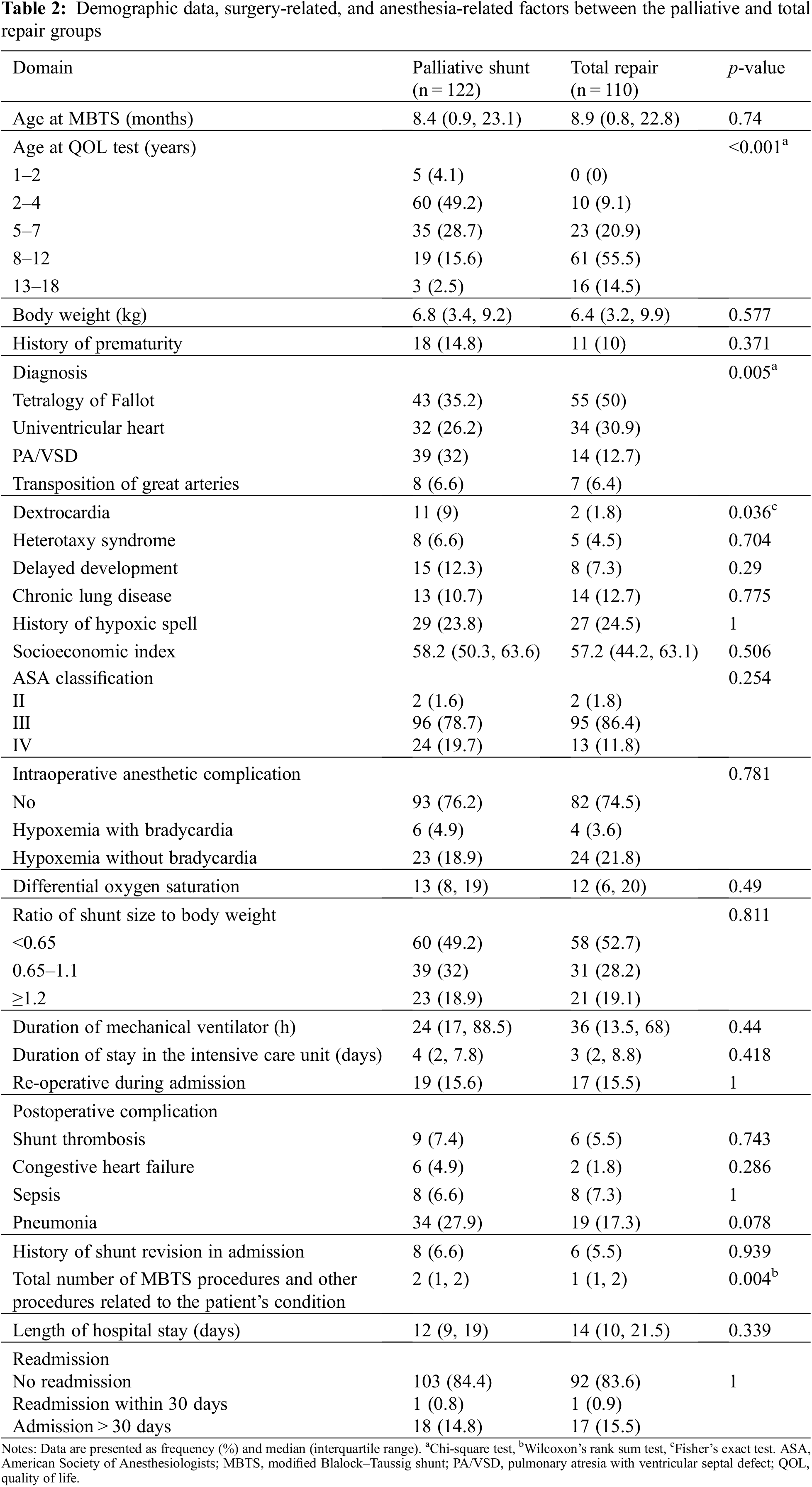
The HRQOL scores assessed by the parents were consistent with the self-assessment scores by the children. The average physical HRQOL score was higher in the total repair group (median, 100) compared with that in the MBTS group (median, 94) both in the parent and child reports. Table 2 summarizes the comparison between MBTS and total repair groups. Children in the total repair group were older at evaluation than those in the MBTS group, and the proportion of TOF in the total repair group (50%) was higher than that in the MBTS group (35%).
3.1 Physical and Psychosocial HRQOL Scores
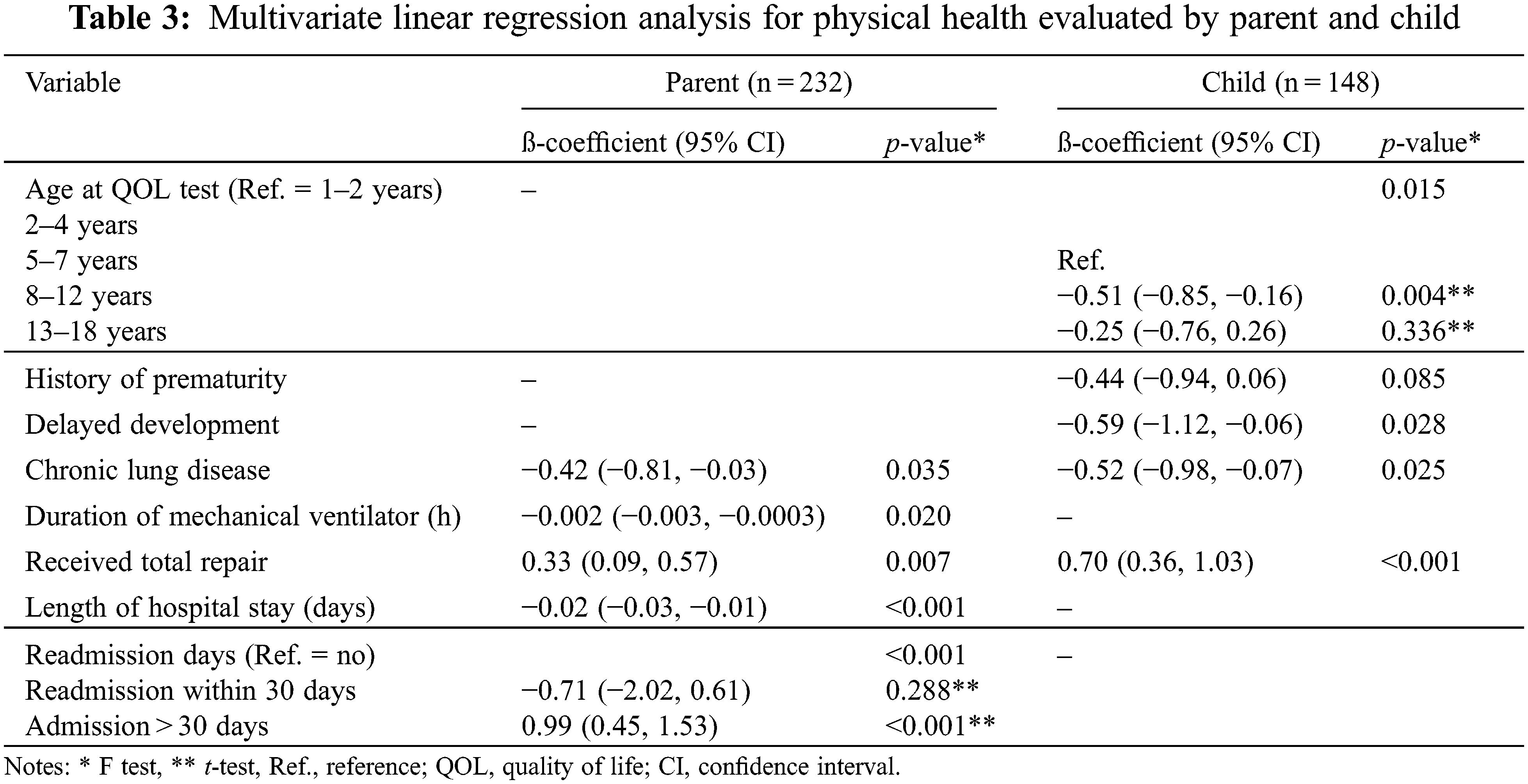
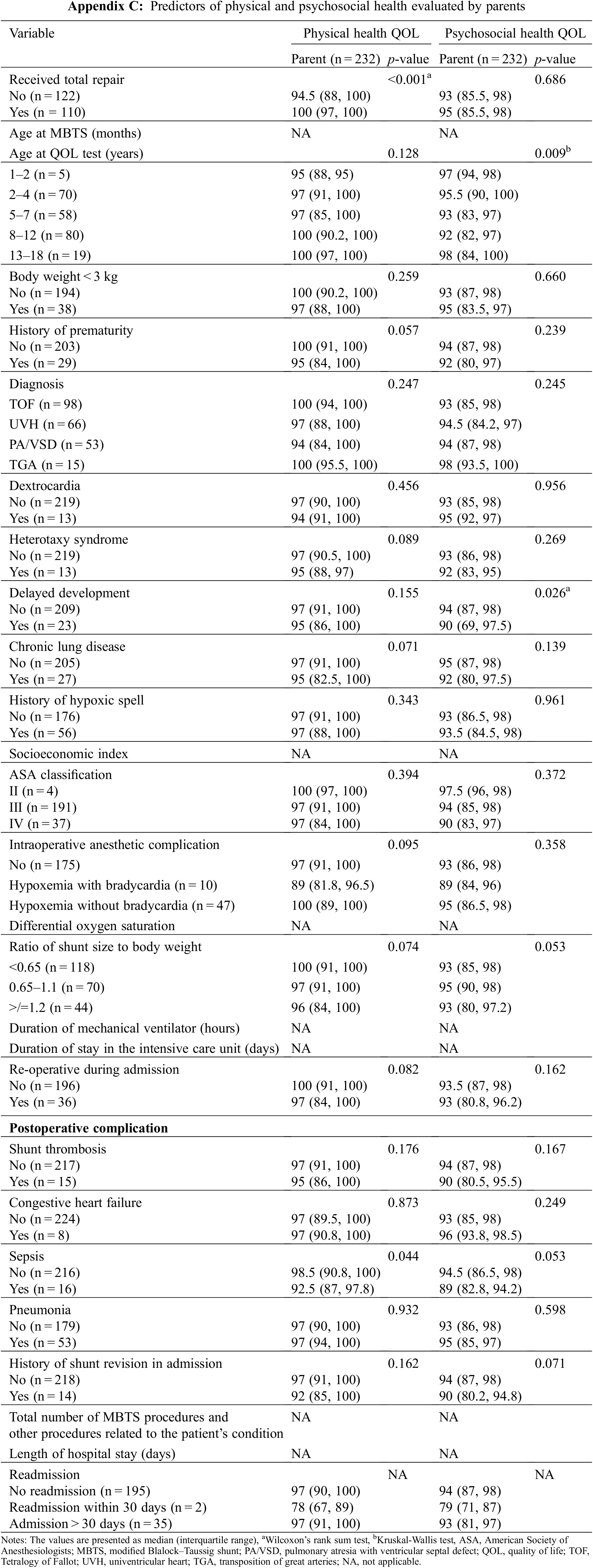
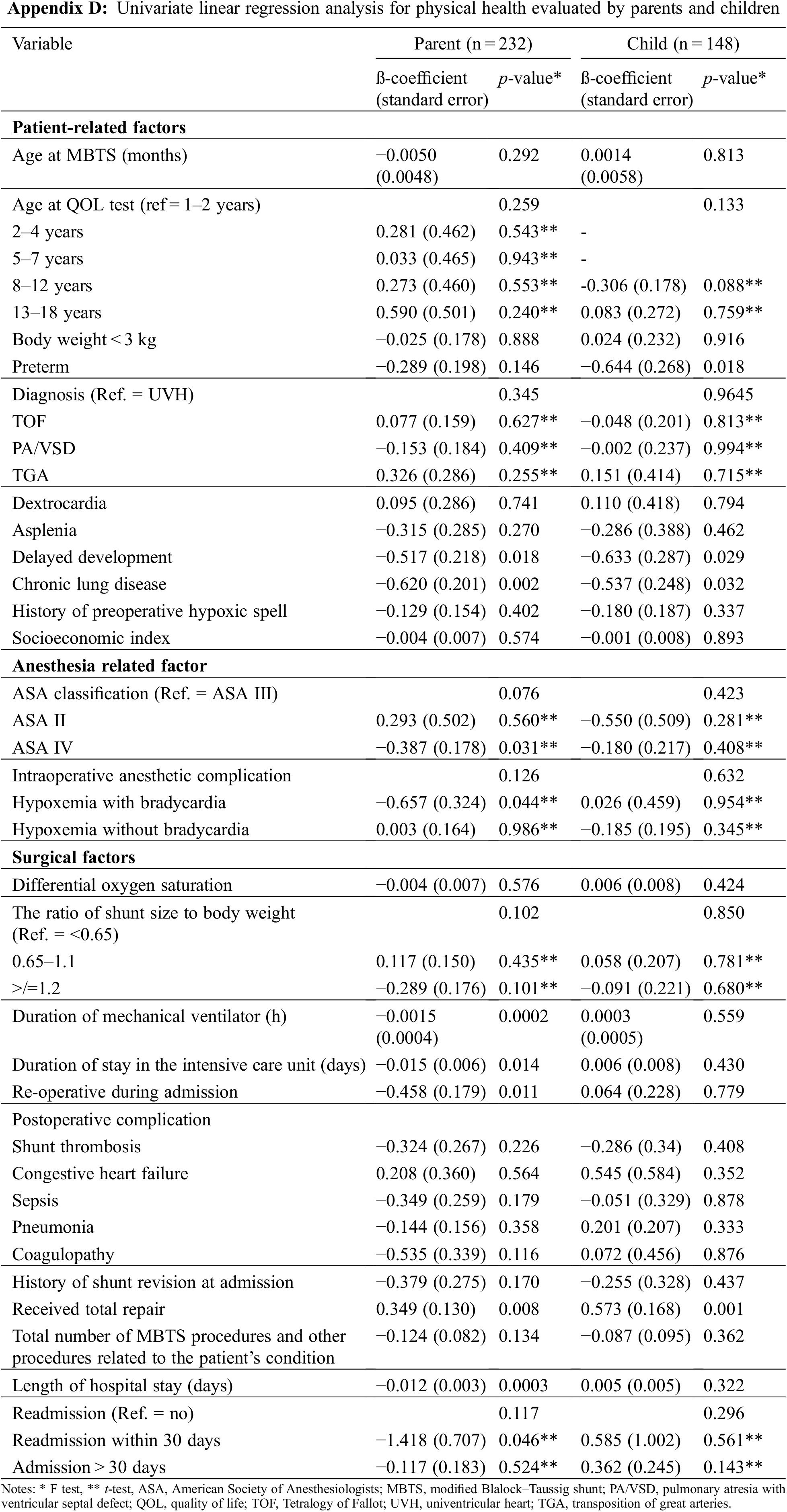
The standardized HRQOL scores were compared using both parent-proxy reports and child self-reports. However, we considered significant predictors based on the parent assessment only since the proportion of missing scores was lower in the parent-proxy reports. Appendix C shows potential predictors of physical and psychosocial health evaluated by parents only. Appendix D summarizes the univariate linear regression results assessing factors associated with physical health evaluated by the parents and children. Sixteen variables in the parent-proxy report (history of prematurity, delayed development, chronic lung disease, ASA classification, intraoperative anesthetic complication, ratio of shunt size to body weight, duration of mechanical ventilator, duration of stay in the intensive care unit, re-operative during admission, postoperative sepsis/coagulopathy, history of shunt revision in admission, total number of MBTS procedures and other procedures related to the patient’s condition, length of hospital stay, readmission and received total repair) and five variables (age at QOL test, history of prematurity, delayed development, chronic lung disease, and received total repair) in the child self-report with p-value < 0.2 were included in the initial multivariate linear regression analysis. After adjusting for covariates, the multivariate model used for both parent-proxy reports and child self-reports is summarized in Table 3. Significant predictors of lower physical standardized HRQOL score included chronic lung disease (p = 0.035), longer duration on a mechanical ventilator (p = 0.02), and longer duration of hospital stay (p < 0.001). Total repair was a predictor of improvements in the physical standardized HRQOL scores in both parent-proxy reports (p = 0.007) and child self-reports (p < 0.001).
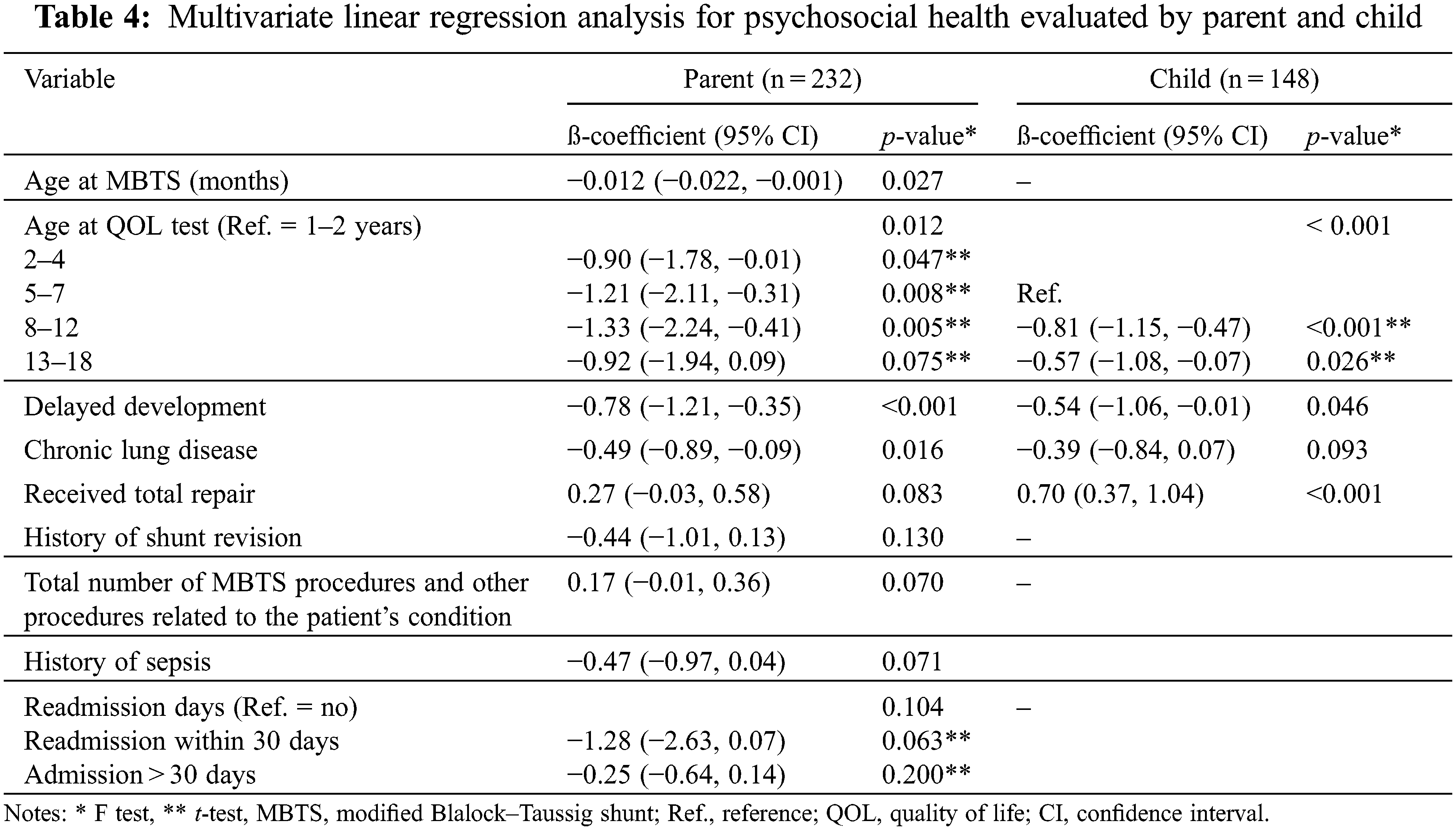
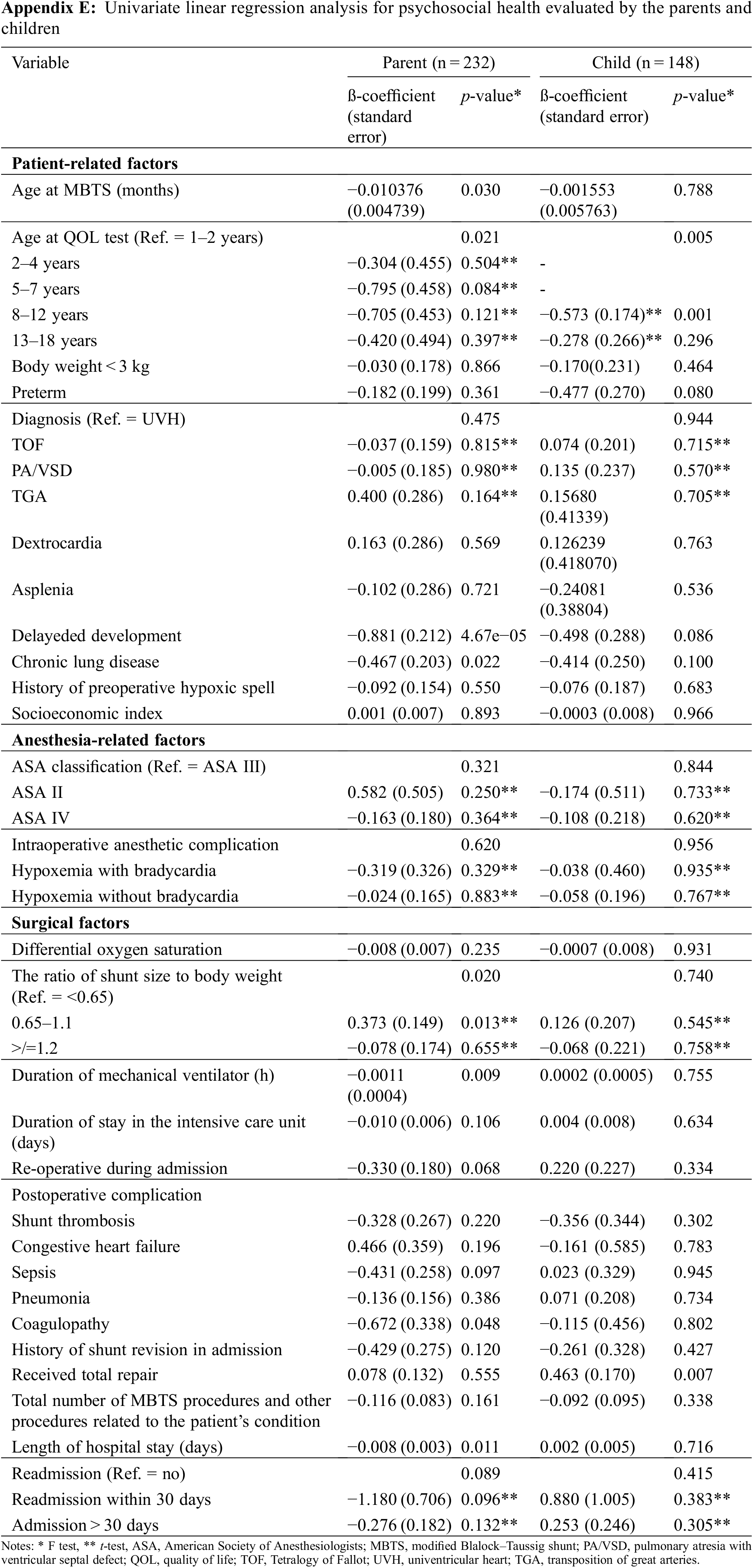
Appendix E summarizes the univariate linear regression analysis for factors associated with the psychosocial health evaluated by the parents and children. Sixteen variables in the parent-proxy report (age at MBTS, age at QOL test, delayed development, chronic lung disease, ratio of shunt size to body weight, duration of mechanical ventilator, duration of stay in the intensive care unit, re-operative during admission, postoperative congestive heart failure sepsis/coagulopathy, history of shunt revision in admission, total number of MBTS procedures and other procedures related to the patient’s condition, length of hospital stay, readmission and received total repair) and five variables in the child self-report (age at QOL test, history of prematurity, delayed development, chronic lung disease, and received total repair) with p < 0.2 were included in the initial multivariate linear regression. The multivariate model used for both parent-proxy reports and child self-reports is summarized in Table 4. Significant predictors of lower psychosocial standardized HRQOL score included older age at QOL assessment (p = 0.012), delayed development (p < 0.001), and chronic lung disease (p = 0.016). Younger age at the time of the MBTS procedure was a predictor of improvements in the psychosocial standardized HRQOL scores (p = 0.027).
3.2 Subgroup Analysis in the Total Repair Group
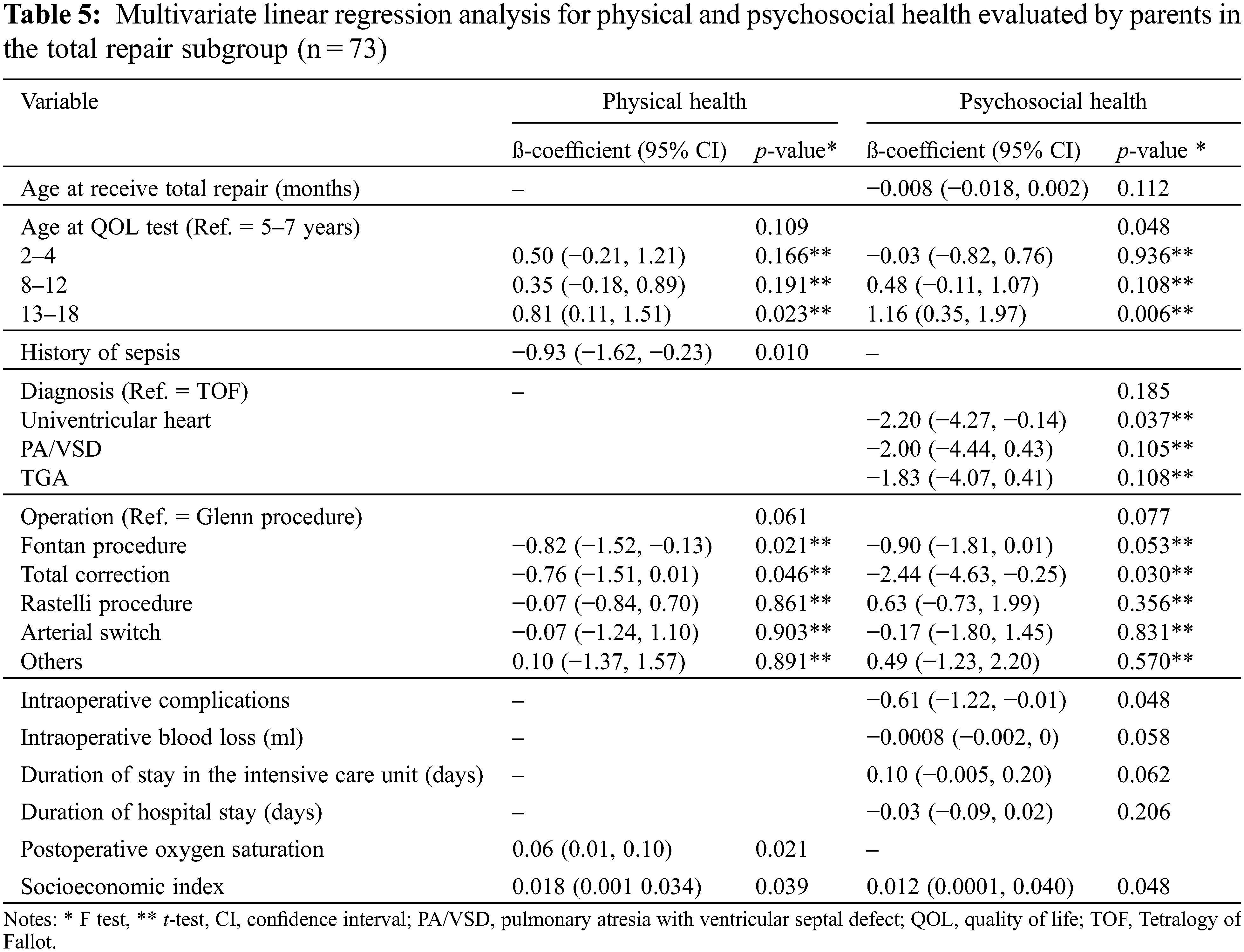
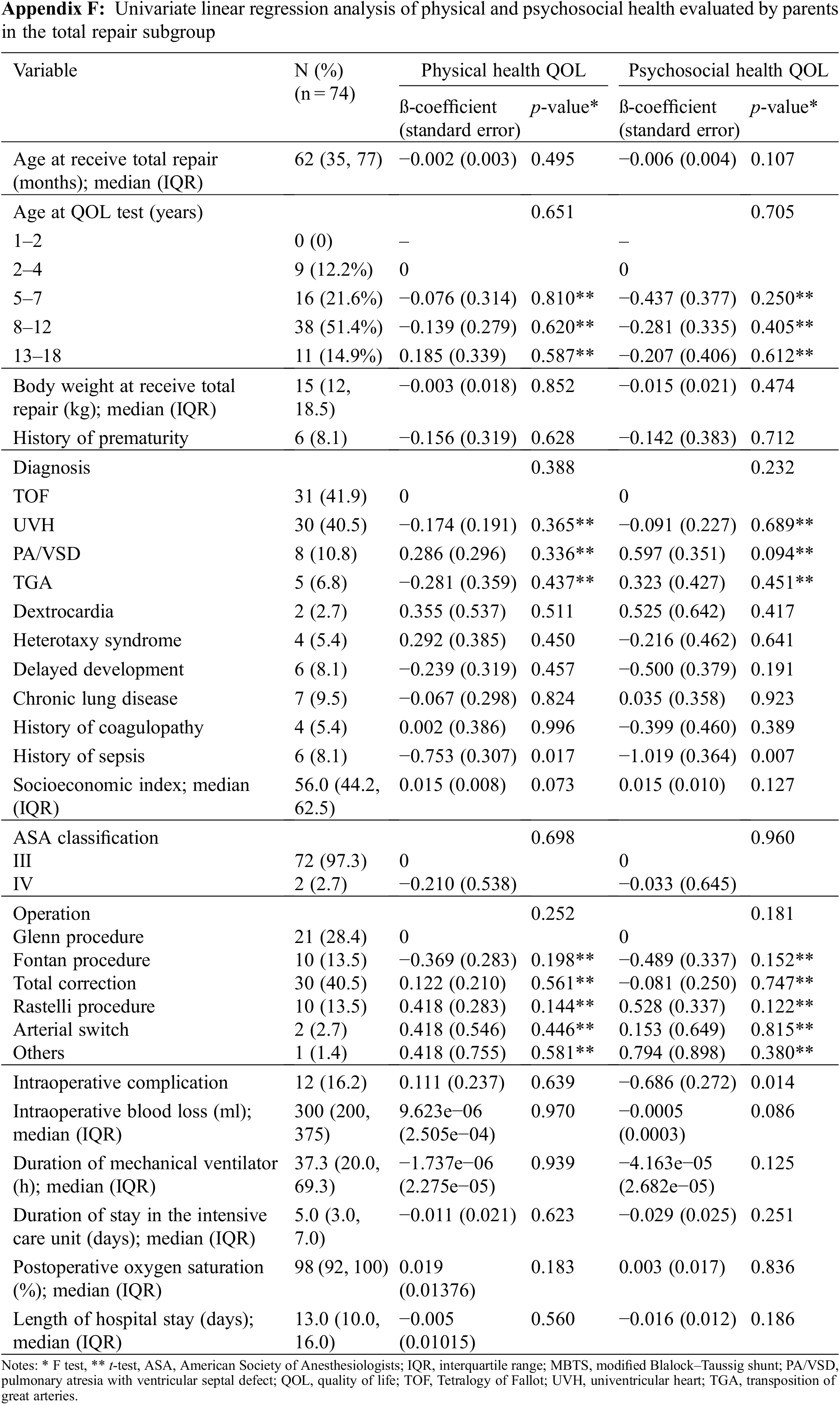
Among the 110 children who underwent total repair, 74 underwent the operation at our hospital and 36 were transferred to other hospitals. We recorded the surgery-related and anesthesia-related variables according to the total repair. Appendix F shows the univariate linear regression analysis for factors associated with the physical health and psychosocial health evaluated by the parents. Table 5 summarizes the multivariate linear regression analysis for factors associated with the physical health and psychosocial evaluated by the parents. Predictors of lower physical standardized HRQOL score included age 5–7 years (vs. 13–18 years) at QOL assessment (p = 0.023 by t-test), history of sepsis (p = 0.010), and children who underwent the Fontan procedure/total correction (vs. Glenn procedure) (p = 0.021/p = 0.046 by t-test). Higher socioeconomic status and higher postoperative oxygen saturation were predictors of improvements in the physical standardized HRQOL score (p = 0.039 and p = 0.021, respectively). Predictors of lower psychosocial standardized HRQOL score included age 5–7 years (vs. 13–18 years) at QOL assessment (p = 0.006 by t-test), UVH (vs. TOF) (p = 0.037 by t-test), total correction (vs. Glenn procedure) (p = 0.030 by t-test); and intraoperative complications (p = 0.048). Predictor of improvement in psychosocial health standardized HRQOL score was higher socioeconomic status (p = 0.048). Higher socioeconomic status was a common predictor of improvements in both physical and psychosocial standardized HRQOL scores.
This historical cohort and follow-up study found that the total/partial correction procedure improved the patients’ physical HRQOL but did not improve the psychosocial HRQOL from the parents’ perspective, which could arise from the fact that parents are subjected to greater burden and suffering across all family dimensions compared with those experienced by their children. A study by Geerdink et al. [10] supports our findings that parents reported significantly more internalizing problems such as anxiety, depression, and attention problems in their children with the Ebstein Anomaly rather than adolescents themselves. According to our results, a variety of predictors related to the patient’s condition and surgical treatment could affect the HRQOL in children with complex heart disease after undergoing the MBTS procedure.
The overall median score in both the physical and psychological HRQOL assessments in children with cyanotic heart disease in our study was high (>92) compared to those reported in France (73.5) [11] and the USA [5] using the same HRQOL tools. The higher HRQOL scores in Thai children with partial correction compared with other populations may be due to parental overprotection/over-support associated with Thai culture, or it could be due to individual resilience [9]; however, further investigations are warranted. Abassi et al. [11] examined the HRQOL in children with CHD aged 5–7 years, while our study and Uzark’s study included children of a wider age range of 2–18 years [5]. Therefore, we generated standardized HRQOL scores for better comparisons and as the outcome variable in the linear regression analysis.
Only children aged at least 5 years can complete the child self-report questionnaire; therefore, the number of child self-reports (n = 148) was fewer than that of parent-proxy reports (n = 232). However, the HRQOL in each domain as well as the overall physical and psychological HRQOL scores between the child self-reports and parent-proxy reports were similar.
4.1 Improvements in Physical and Psychosocial HRQOL
Both univariate and multivariate linear regression analysis revealed that total repair/progression to the next stage (vs. palliative shunt) was one of the important predictors of improvements in physical HRQOL (p = 0.007) but not psychosocial HRQOL scores in the parent-proxy reports (p = 0.083). Nevertheless, approximately 80% of the children survived total repair at our hospital, while the others died from intraoperative and postoperative complications. The children who survived total repair can experience improvements in physical functions, such as walking, running, and doing household chores without developing dyspnea. However, the child self-reports in the total repair group revealed improvements in social function (p = 0.031) as well as the overall psychosocial HRQOL score in the multivariate analysis (p < 0.001). Therefore, physical HRQOL can be improved with total repair; when physical health improves, it may promote better emotional as well as social and school functions [12,13]. Consequently, psychosocial HRQOL may eventually improve following total repair. However, children with a complex cardiac condition might still have poorer psychosocial HRQOL regardless of their diagnosis or type of operation compared to simple conditions [14]. Uzark et al. [5] reported that patients with moderate cardiac disease who underwent curative surgery had higher physical and psychosocial HRQOL scores than those with severe cardiac disease and uncorrectable defects (89 vs. 76 and 82 vs. 74, respectively).
We observed that younger age at the time of the MBTS procedure can help improve the psychosocial HRQOL score. Since all children had cyanotic heart disease in this study, good left-to-right shunt flow could improve the child’s oxygenation and promote fair living in terms of emotional and social functions but not improve complete physical function if total repair is not performed. This may be why younger age at the time of the MBTS procedure could improve the psychosocial but not physical HRQOL score. Moreover, Wang et al. [15] reported that adolescents’ knowledge of their cardiac condition incorporated with an increase in the sense of well-being improved the psychosocial quality of life of the affected individual. In our routine preoperative care, our disciplinary team, especially the pediatric cardiologist, take a reasonable amount of time to explain to the patient their cardiac abnormality condition and discusses the possible morbidities and prognosis with the parent or adolescents themselves at the pediatric outpatient clinic at least 1 month before surgery or at the pediatric ward at least one day before surgery.
4.2 Congenital Heart Defect after Total Repair and HRQOL
In the total repair subgroup, UVH was associated with worse psychosocial HRQOL scores compared with TOF (p = 0.037 using t-test). Previous studies have shown that a diagnosis other than TOF is the principal risk factor for early mortality [16,17], which could be associated with poorer HRQOL if the patients survive. After total repair, the HRQOL score in these children could be similar [11] or lower than those of healthy peers [18]. Higher HRQOL scores following corrective surgery can be due to several factors, such as residual heart defect/chronic disease [19,20], socioeconomic reasons [20,21], and familial relationships [22].
Higher socioeconomic status was not an independent predictor of our primary outcome but was one of the predictors of improvements in both physical and psychosocial HRQOL scores following total repair. Landolt et al. [22] reported that socioeconomic status was not associated with physical and psychosocial HRQOL scores following open-heart surgery, while adverse familial relationships negatively affected the parent-related HRQOL scores. Socioeconomic status includes the family’s income and parents’ education. Families with higher income or higher education would have better capability to take care of sick children than those with poorer socioeconomic status. Since some of the children with UVH (29%) received only the Glenn shunt and not definite Fontan’s procedure, they may still experience cyanotic manifestations. Therefore, parental support in terms of both financial and psychosocial aspects can improve the child’s physical and psychosocial health, which has been previously reported [20,21].
4.3 Risk Factors of Poor Physical and Psychosocial HRQOL Scores
Common risk factors of poor physical and psychosocial HRQOL scores included chronic lung disease and delayed development. Patients with chronic lung disease, such as bronchopulmonary dysplasia, can develop worsening of cyanotic symptoms in conjunction with postoperative shunt problems, which can result in poor physical and psychosocial HRQOL scores. Similarly, children with cyanotic heart defects and intellectual developmental problems can also develop worsening of both physical and psychosocial functions due to shunt malfunction. Both diseases are classified as chronic diseases, which can affect the overall HRQOL in pediatric patients. If children with CHD also have other chronic diseases, they will have a poorer QOL [19]. Such children require a sense of coherence or a sense of appreciation for life and expectations earlier than healthy children, which may affect their HRQOL [23].
Longer duration of mechanical ventilation and longer duration of hospital stay were risk factors for poor physical HRQOL. The duration of mechanical ventilation and the duration of hospital stay may represent the severity of cyanotic heart disease, its treatments, and postoperative MBTS complications, such as shunt thrombosis, coagulopathy, and sepsis. Our previous study has shown that postoperative complications following MBTS procedure, such as shunt thrombosis (5-fold), bleeding (4.5-fold), and renal failure (4.1-fold), were strong predictors of time-to-death <90 days postoperatively [7]. Therefore, children who survive such complications would require prolonged mechanical ventilation, which results in a longer duration of hospital stay. Landolt et al. [22] also reported that prolonged duration of hospital stay was related to impaired HRQOL in children following open-heart surgery based on parent-proxy reports, which was consistent with the findings of our study. The poor physical health might also be related to complications due to shunt problems or partial recovery from infections after prolonged mechanical ventilation and admission. Secondary hypothyroidism in the immediate postoperative period has also been reported in children who underwent cardiac surgery. Furthermore, Bettendorf et al. [24] showed that lower thyroid hormone concentrations were significantly associated with prolonged mechanical ventilation and length of hospital stay. Therefore, the effects of thyroid function on long-term cognitive function during the postoperative period after congenital heart surgery remain to be investigated.
Older age at QOL assessment was also one of the risk factors of poor physical HRQOL in child self-reports and psychological HRQOL in both child and parent reports, irrespective of the status of total repair (Tables 3 and 4). However, older age at QOL assessment in the total repair subgroup was associated with a higher psychological HRQOL score. Therefore, irrespective of total repair status, in children who receive only a palliative shunt (MBTS), increasing waiting time for total repair is associated with worsening physical and psychosocial functions at the time of QOL assessment. In contrast, in children who undergo total repair, the physical and psychosocial functions will improve with time. Longer time after surgery was associated with older age at QOL assessment. We observed that adolescents (aged 13–18 years) had much better QOL scores than children aged 5–7 years (Table 5).
4.4 Summary of Main Finding and Clinical Implications
We found that total repair/progression to the next stage can improve physical HRQOL scores, whereas higher psychological HRQOL scores was associated with younger age during MBTS surgery. In total repair subgroup, higher socioeconomic status and older age at QOL assessment were associated with higher physical and psychological HRQOL scores. Although total repair/progression to the next stage can improve physical HRQOL scores in children with cyanotic heart disease, the overall in-hospital mortality at our hospital following Glenn’s procedure/Fontan procedure/total repair was relatively high (20%) compared with those in other studies, which varied from 2%–12% depending on the severity, co-morbidities and experience of the surgeon [25–30]. Therefore, patient selection for total repair is critical for minimizing postoperative mortality. Competing risk analysis in our previous study revealed that the proportion of children who underwent Glenn’s procedure/total repair increased at approximately 5 months of age; however, only 31.5% had undergone Glenn’s procedure/total repair at 5 years after the MBTS procedure due to various limitations [7]. Therefore, we propose the following two solutions to improve HRQOL. First, Glenn’s procedure/total repair should be considered in young children with chronic conditions that affect HRQOL, such as delayed development and chronic lung disease. Second, the MBTS procedure should be performed as soon as possible after the diagnosis of UVH/biventricular heart or other cyanotic heart conditions to prevent worsening of symptoms and, perhaps, improve HRQOL while awaiting definite repair. Since individual HRQOL courses are unpredictable regardless of the surgery, repeated HRQOL assessments over time might benefit children with congenital heart disease [31].
There are a number of strengths of this study. First, we used a valid Thai translated questionnaire and only one pediatric psychologist for the assessment of HRQOL, which ensured the validity and reliability of the results. Second, we used multivariate linear regression analysis to adjust for potential independent predictors. Third, the results in the total repair subgroup supported the primary findings, which may also reflect the accuracy of the study. Despite these strengths, a few limitations need mentioning. First, the duration between surgery and HRQOL evaluation in each child varied (1–11 years); for example, only five patients were of 1–2 years of age, which might have affected the HRQOL score for that age group. Second, one-third of the patients underwent total repair at other institutions, which resulted in a small sample and, possible oversight related to some predictors of HRQOL.
The total/partial correction procedure was one of the most important predictors of a higher physical HRQOL, although it was not associated with improved psychosocial HRQOL from the parents’ perspective. Young age at the time of the MBTS procedure was a predictor of higher psychological HRQOL scores. Futhermore, higher socioeconomic status and older age at QOL assessment were predictors of higher both physical and psychological HRQOL scores following total repair.
Acknowledgement: We would like to thank Editage and Assistant Professor Edward McNeil for editing the manuscript as well as their valuable suggestions.
Authorship: All those listed as authors contributed to the preparation of the manuscript. Each listed author participated in the work that they can defend its content. JT participated in the study design, collected the data, and wrote the draft manuscript. MO coordinated the study, participated in the study design, undertook the statistical analysis and revised the draft manuscript. WW participated in the study design and coordinated the drafting of the manuscript. VC participated in the study design and coordinated the drafting of the manuscript. PD participated in the study design. JJ participated in the study design. QY collected the data. All authors read and approved the final version.
Availability of Data and Materials: De-identified participant data (including data dictionaries) will be shared in the appendix file.
Funding Statement: This work was funded by the Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand. M.O. received a grant amount of ฿70,320 in January 2017 (Grant No. 59-301-08-01; http://medinfo.psu.ac.th/)
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Alsoufi, B., Gillespie, S., Kogon, B., Schlosser, B., Sachdeva, R. et al. (2015). Results of palliation with an initial modified Blalock-Taussig shunt in neonates with single ventricle anomalies associated with restrictive pulmonary blood flow. The Annals of Thoracic Surgery, 99(5), 1639–1647. DOI 10.1016/j.athoracsur.2014.12.082. [Google Scholar] [CrossRef]
2. Nousi, D., Christou, A. (2010). Factors affecting the quality of life in children with congenital heart disease. Health Science Journal, 4(2), 94–100. [Google Scholar]
3. Atmadja, S., Tobing, T., Evalina, R., Sofyani, S., Ali, M. (2018). Quality of life in children with congenital heart disease after cardiac surgery. Paediatrica Indonesiana, 57(6), 285–290. DOI 10.14238/pi57.6.2017.285-90. [Google Scholar] [CrossRef]
4. Garcia Guerra, G., Robertson, C. M., Alton, G. Y., Joffe, A. R., Dinu, I. A. et al. (2013). Quality of life 4 years after complex heart surgery in infancy. The Journal of Thoracic and Cardiovascular Surgery, 145(2), 482–488.e2. DOI 10.1016/j.jtcvs.2012.03.050. [Google Scholar] [CrossRef]
5. Uzark, K., Jones, K., Slusher, J., Limbers, C. A., Burwinkle, T. M. (2008). Quality of life in children with heart disease as perceived by children and parents. Pediatrics, 121(5), e1060–e1067. DOI 10.1542/peds.2006-3778. [Google Scholar] [CrossRef]
6. Svensson, B., Idvall, E., Nilsson, F., Liuba, P. (2017). Health-related quality of life in children with surgery for CHD: A study from the Swedish national registry for congenital heart disease. Cardiology in the Young, 27(2), 333–343. DOI 10.1017/S1047951116000585. [Google Scholar] [CrossRef]
7. Oofuvong, M., Tanasansuttiporn, J., Wasinwong, W., Chittithavorn, V., Duangpakdee, P. et al. (2021). Predictors of death after receiving a modified Blalock-Taussig shunt in cyanotic heart children: A competing risk analysis. PLoS One, 16(1), e0245754. DOI 10.1371/journal.pone.0245754. [Google Scholar] [CrossRef]
8. Varni, J. W., Seid, M., Kurtin, P. S. (2001). PedsQL 4.0: Reliability and validity of the pediatric quality of life inventory version 4.0 generic core scales in healthy and patient populations. Medical Care, 39(8), 800–812. DOI 10.1097/00005650-200108000-00006. [Google Scholar] [CrossRef]
9. Green, L. W. (1970). Manual for scoring socioeconomic status for research on health behavior. Public Health Reports, 85(9), 815–827. DOI 10.2307/4593972. [Google Scholar] [CrossRef]
10. Geerdink, L. M., van der Mheen, M., Sarvaas, G. J. D. M., Kuipers, I. M., Frerich, S. et al. (2020). Health-related quality of life, emotional and behavioral problems in children and adolescents with Ebstein anomaly. Congenital Heart Disease, 15(6), 457–472. DOI 10.32604/CHD.2020.012994. [Google Scholar] [CrossRef]
11. Abassi, H., Huguet, H., Picot, M. C., Vincenti, M., Guillaumont, S. et al. (2020). Health-related quality of life in children with congenital heart disease aged 5 to 7 years: A multicentre controlled cross-sectional study. Health and Quality of Life Outcomes, 18(1), 366. DOI 10.1186/s12955-020-01615-6. [Google Scholar] [CrossRef]
12. Heusch, A., Calaminus, G., Kahl, J., Schmidt, K. (2014). Health related quality of life after corrective surgery for congenital heart disease. Klinische Padiatrie, 226(5), 281–286. DOI 10.1055/s-0034-1382019. [Google Scholar] [CrossRef]
13. Raj, M., Sudhakar, A., Roy, R., Soman, S., Antony, L. et al. (2018). Health-related quality of life in infants and toddlers with congenital heart disease: A cross-sectional survey from south India. Archives of Disease in Childhood, 103(2), 170–175. DOI 10.1136/archdischild-2017-313165. [Google Scholar] [CrossRef]
14. Lee, J. S., Blais, A., Jackson, J., Patel, B. J., Lai, L. et al. (2021). Higher child-reported internalizing and parent-reported externalizing behaviors were associated with decreased quality of life among pediatric cardiac patients independent of diagnosis: A cross-sectional mixed-methods assessment. Congenital Heart Disease, 16(3), 255–267. DOI 10.32604/CHD.2021.014628. [Google Scholar] [CrossRef]
15. Wang, Q., Hay, M., Clarke, D., Menahem, S. (2014). Associations between knowledge of disease, depression and anxiety, social support, sense of coherence and optimism with health-related quality of life in an ambulatory sample of adolescents with heart disease. Cardiology in the Young, 24(1), 126–133. DOI 10.1017/S1047951113000012. [Google Scholar] [CrossRef]
16. Maghur, H. A., Ben-Musa, A. A., Salim, M. E., Abuzakhar, S. S. (2002). The modified Blalock-Taussig shunt: A 6-year experience from a developing country. Pediatric Cardiology, 23(1), 49–52. DOI 10.1007/s00246-001-0012-4. [Google Scholar] [CrossRef]
17. Hanley, F. L., Sade, R. M., Blackstone, E. H., Kirklin, J. W., Freedom, R. M. et al. (1993). Outcomes in neonatal pulmonary atresia with intact ventricular septum. A multiinstitutional study. The Journal of Thoracic and Cardiovascular Surgery, 105(3), 406–424. DOI 10.1016/S0022-5223(19)34223-0. [Google Scholar] [CrossRef]
18. Holst, L. M., Kronborg, J. B., Idorn, L., Bjerre, J. V., Vejlstrup, N. et al. (2019). Impact of congenital heart surgery on quality of life in children and adolescents with surgically corrected ventricular septal defect, Tetralogy of Fallot, and transposition of the great arteries. Cardiology in the Young, 29(8), 1082–1087. DOI 10.1017/S1047951119001604. [Google Scholar] [CrossRef]
19. Sritipsukho, P., Poomsitong, J. (2012). Health-related quality of life in children with chronic diseases at Thammasat university hospital. Journal of the Medical Association of Thailand, 95(Suppl 1), S8–S12. [Google Scholar]
20. Tahirović, E., Begić, H., Sutović, A., Tahirović, H. (2010). Povezanost socijalnoekonomskog stanja obitelji i kvaliteta zivota djece nakon operacije urodene anomalije srca [Impact of the family socioeconomic status on health related quality of life in children operated on for congenital heart defects]. Acta Medica Croatica, 64(1), 9–16. [Google Scholar]
21. Xiang, L., Su, Z., Liu, Y., Huang, Y., Zhang, X. et al. (2019). Impact of family socioeconomic status on health-related quality of life in children with critical congenital heart disease. Journal of the American Heart Association, 8(1), e010616. DOI 10.1161/JAHA.118.010616. [Google Scholar] [CrossRef]
22. Landolt, M. A., Valsangiacomo Buechel, E. R., Latal, B. (2008). Health-related quality of life in children and adolescents after open-heart surgery. The Journal of Pediatrics, 152(3), 349–355. DOI 10.1016/j.jpeds.2007.07.010. [Google Scholar] [CrossRef]
23. Bertoletti, J., Marx, G. C., Hattge Júnior, S. P., Pellanda, L. C. (2014). Quality of life and congenital heart disease in childhood and adolescence. Arquivos Brasileiros de Cardiologia, 102(2), 192–198. DOI 10.5935/abc.20130244. [Google Scholar] [CrossRef]
24. Bettendorf, M., Schmidt, K. G., Tiefenbacher, U., Grulich-Henn, J., Heinrich, U. E. et al. (1997). Transient secondary hypothyroidism in children after cardiac surgery. Pediatric Research, 41(3), 375–379. DOI 10.1203/00006450-199703000-00012. [Google Scholar] [CrossRef]
25. Silvilairat, S., Pongprot, Y., Sittiwangkul, R., Woragidpoonpol, S., Chuaratanaphong, S. et al. (2008). Factors influencing survival in patients after bidirectional Glenn shunt. Asian Cardiovascular and Thoracic Annals, 16(5), 381–386. DOI 10.1177/021849230801600508. [Google Scholar] [CrossRef]
26. Sarno, L. A., Walters, 3rd, H. L., Bondarenko, I., Thomas, R., Kobayashi, D. (2020). Significant improvements in mortality after the Fontan operation in children with down syndrome. The Annals of Thoracic Surgery, 109(3), 835–841. DOI 10.1016/j.athoracsur.2019.07.085. [Google Scholar] [CrossRef]
27. Ghimire, L. V., Chou, F. S., Pundi, K., Moon-Grady, A. J. (2022). In-hospital outcomes in Fontan completion surgery according to age. The American Journal of Cardiology, 166, 81–87. DOI 10.1016/j.amjcard.2021.11.019. [Google Scholar] [CrossRef]
28. Barron, D. J., Mehsood, D. K., Kutty, R. S., Stickley, J., Botha, P. et al. (2019). Fate of the left ventricular outflow tract after Rastelli with selective infundibular muscle resection. The Annals of Thoracic Surgery, 107(4), 1226–1231. DOI 10.1016/j.athoracsur.2018.10.069. [Google Scholar] [CrossRef]
29. François, K., Vandekerckhove, K., de Groote, K., Panzer, J., de Wolf, D. et al. (2016). Current outcomes of the bi-directional cavopulmonary anastomosis in single ventricle patients: Analysis of risk factors for morbidity and mortality, and suitability for Fontan completion. Cardiology in the Young, 26(2), 288–297. DOI 10.1017/S1047951115000153. [Google Scholar] [CrossRef]
30. Sethasathien, S., Silvilairat, S., Kraikruan, H., Sittiwangkul, R., Makonkawkeyoon, K. et al. (2020). Survival and predictors of mortality in patients after the Fontan operation. Asian Cardiovascular & Thoracic Annals, 28(9), 572–576. DOI 10.1177/0218492320949655. [Google Scholar] [CrossRef]
31. Fuertes-Moure, A., Meyer, M., Häcker, A., Reiner, B., Brudy, L. et al. (2020). Longitudinal health-related quality of life assessment in children with congenital heart disease. Congenital Heart Disease, 15(4), 217–227. DOI 10.32604/CHD.2020.011771. [Google Scholar] [CrossRef]
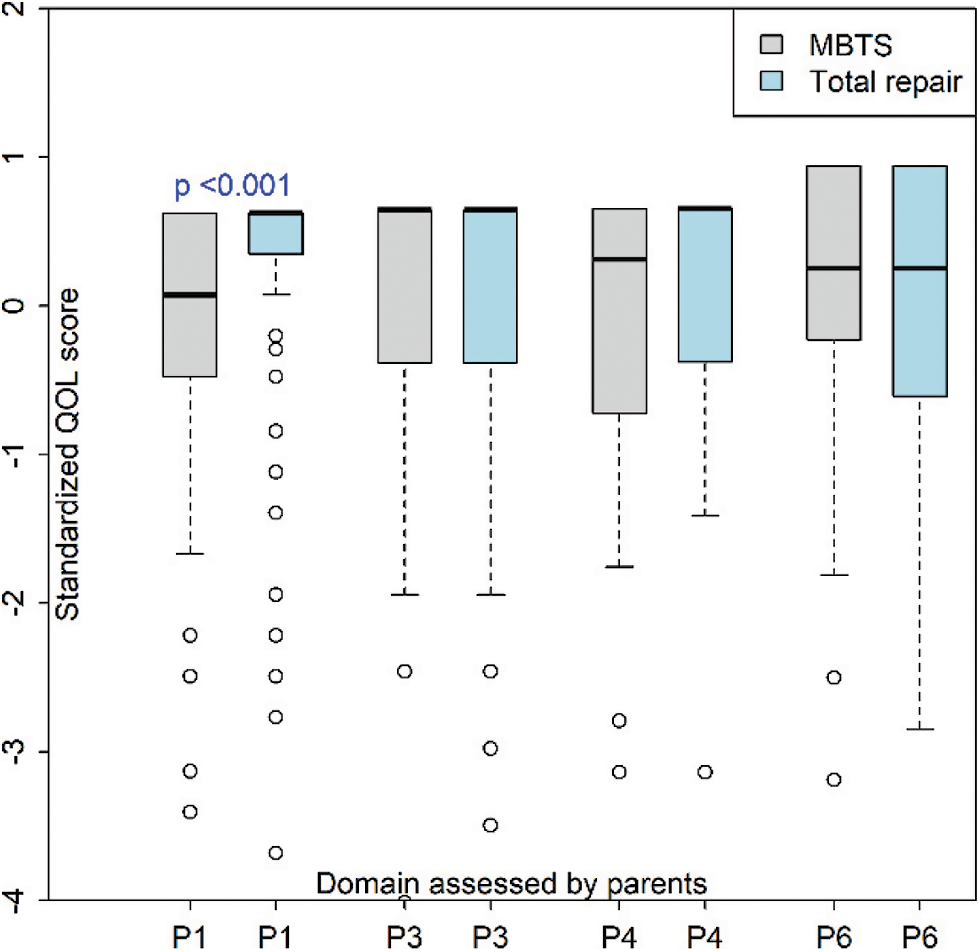
Appendix A: Physical and psychosocial HRQOL assessed using the parent-proxy report. HRQOL, health-related quality of life; MBTS, modified Blalock–Taussig shunt
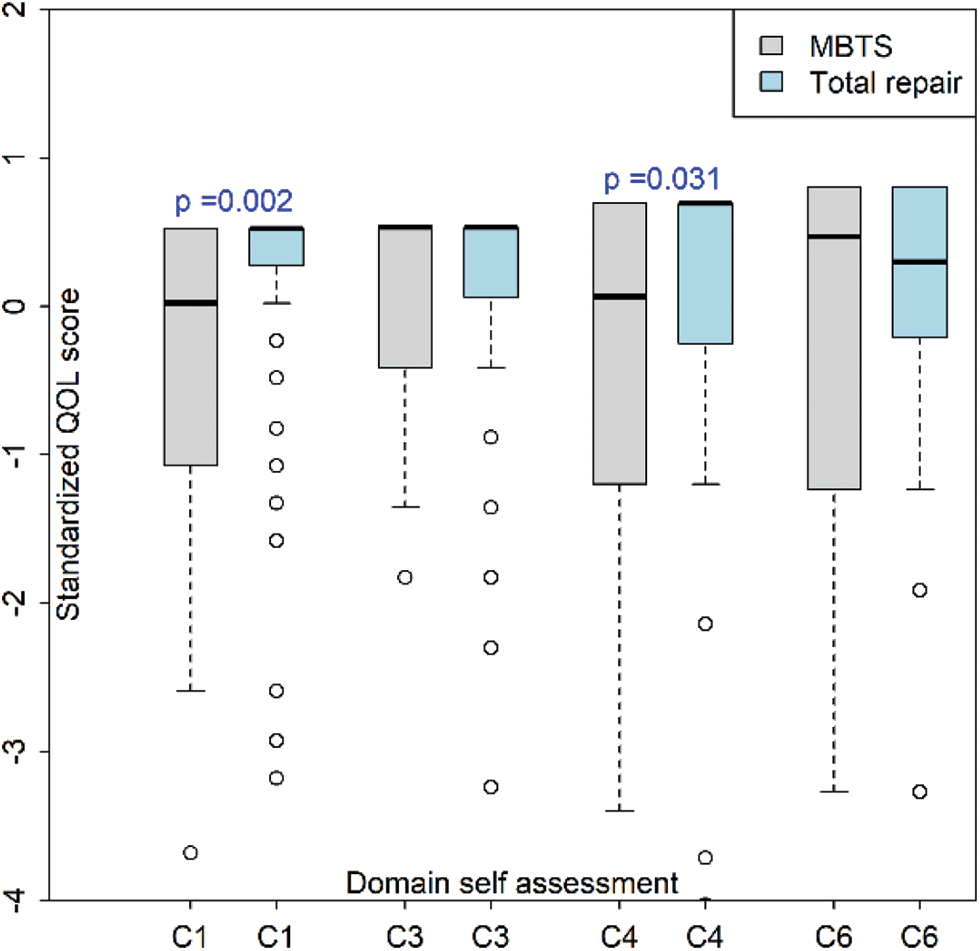
Appendix B: Physical and psychosocial HRQOL assessed using the child self-report. HRQOL, health-related quality of life; MBTS, modified Blalock–Taussig shunt
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |