DOI:10.32604/cmc.2020.013035
| Computers, Materials & Continua DOI:10.32604/cmc.2020.013035 | 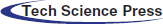 |
| Article |
A Smart Wellness Service Platform and Its Practical Implementation
1Department of Biomedical Engineering, Kyung Hee University, 1732 Deogyeong-daero, Giheung-gu, Yongin-si, Gyeonggi-do 17104, Korea
2Department of Computer Engineering, Kyung Hee University, 1732 Deogyeong-daero, Giheung-gu, Yongin-si, Gyeonggi-do 17104, Korea
*Corresponding Author: Gon Khang. Email: gkhang@khu.ac.kr
Received: 22 July 2020; Accepted: 26 August 2020
Abstract: Advances in the field of medical sciences and medical technology, and present-day challenges, such as an aging population, rising medical expenses, and lifestyle-related diseases, have collectively catalyzed a research ecosystem termed “smart wellness.” This article describes the establishment of a smart wellness service platform designed to empower individuals to create a sense of balance in their lives. Step-by-step details include service model, design, and architectural considerations. As a proof of concept, implementation details of a Health Improvement and Management Systems (HIMS) Hub, a Smart Wellness Service Platform deployed in six cities in South Korea, are presented. An on-site survey conducted in Busan Metropolitan City reveals the percentage of satisfied users to be 91.3%. Furthermore, data gathered from 27,236 physical evaluations of users from a Busan city center over the period of April 2013 to May 2018 reveal that males and females in their 50s and 60s account for the highest number of participants, while males in their 70s have a higher rate of participation than females in the same age group.
Keywords: Wellness; smart wellness; smart wellness service platform; u-Healthcare; sports and exercise medicine
The healthcare discipline is transitioning toward its version 3.0 (wellness). The era prior to the 20th century can be considered HealthCare 1.0, and its focus was on pandemic prevention, with many countries providing services to the general public with the aim of reducing the mortality rate of infectious diseases.
From the 20th century onward, HealthCare 2.0 (the present-day medical service modality) has focused on treatment of diseases. Hospitals provide services to patients designed to increase their life expectancy. An aging population, rising medical costs, and lifestyle-related chronic diseases are the new challenges that are revolutionizing healthcare to focus on maximizing the wellness of individuals. The objective is to make healthcare a proactive discipline in which the focus is on increasing quality of life. This ongoing revolution in healthcare is mainly fueled by two factors: Advances in the field of medicine that let us study the complexity and dynamics of disease, and advances in smart technologies. In fact, smart technologies could be defined as the catalyst for this entire research ecosystem.
Today, cloud and analytics technologies are providing solutions that were never before possible to the world’s health-related problems. Research in the domains of wearable sensors [1,2], in-home monitoring of vital signs [3], AwareCar [4], and cloud architectures [5,6] are but a few examples demonstrating the potential of the integration of two domains: wellness and smart technologies. Until now, wellness has primarily been the prerogative of specialized health centers whose goal is to empower individuals to proactively engage in activities that create a sense of balance in their lives. Gyms, spas, health clubs, and meditation clinics are a few examples of businesses that seek to help individuals achieve their optimum in the dimensions of physical, emotional, mental, and spiritual well-being.
The goal of this article is to describe our efforts to advance the concept of conventional wellness centers to a smart wellness service platform. These efforts start with the introduction of a novel service model, the design of a generalized architecture, and finally the specific details of implementation.
2 State-of-the-Art Model and Architecture
This article presents the ongoing efforts toward the establishment of a smart wellness service platform. However, the objectives of this wellness philosophy are diametrically opposite to those of the field of conventional healthcare, and therefore require a disruption in the service provision methodology. This article identifies the components of a wellness service model, provides an architecture to implement the service model, and finally presents the implementation details of the proof of concept, the Health Improvement and Management Systems (HIMS) Hub, for a physical wellness service platform, followed by the results of the implemented smart wellness service platform, as well as analysis of the results.
Although in its infancy, a large and compelling body of literature has promulgated the fundamental tenets of an ongoing revolution in healthcare [7–10]. Tab. 1 compares the objectives of a wellness service modality with those of conventional medicine. Empowering individuals to manage their well-being requires a disruption in the way present day healthcare services are delivered and incentivized. What is needed is an entirely new approach that centers on individuals and encourages proactive participation throughout the lifespan of an individual. Fig. 1 depicts an analogy of the proposed wellness service model to that of an engine and fuel, consisting of assessment, prescription, and practice services as components of the wellness service engine and the motivational service as the driving force for this ecosystem.
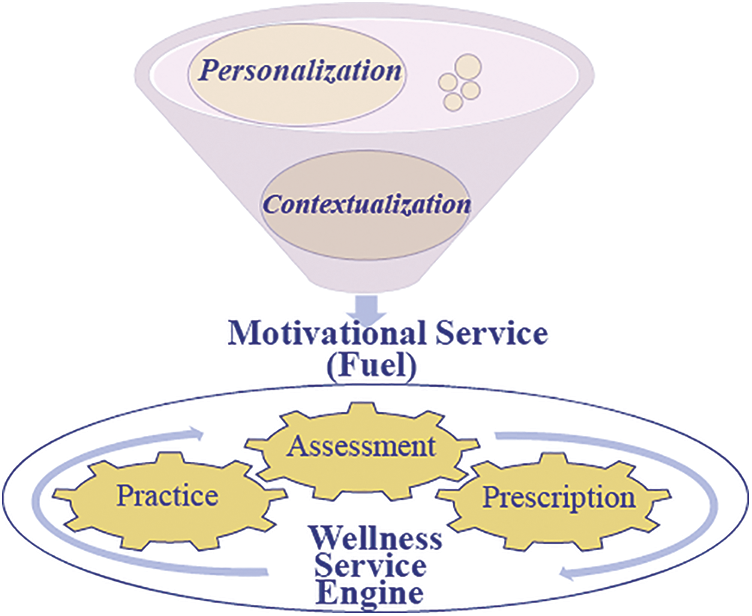
Figure 1: Proposed wellness service model
Table 1: Concept and objectives of wellness service modality
The role of this service is to establish the wellness state of the individual at any given point in time. This is contrary to the diagnosis service in medical service modality, whose role is to locate the presence of disease.
The goal of the prescription, or recommendation, service is to provide guidelines to individuals. Unlike the prescription/treatment service in the medical service modality, the role of the service does not end with the end of disease. Rather, in this case, it proactively engages individuals toward the improvement or maintenance of their well-being.
The role of the practice service is to monitor an individual’s compliance and provide training assistive tools to the individual.
The motivational service, as depicted in Fig. 1, is analogous to the driving force, fueling every component of the wellness service engine. In contrast to the medical service modality, where fear or sickness leads to the onset of service in person’s life, in the wellness paradigm, the motivational service guides individuals toward achieving their optimal wellness state.
The next step is to put the service model into the context of practical realization. The service model assesses the individual’s state of wellness and provides the necessary interventions for achieving a state of optimal wellness makes the case within the optimal control engineering framework. Engineering the pursuit of wellness in this construct helps the individual inherit the intrinsic characteristics of observability and controllability, and breaks down the generalized set of requirements into refined engineering objectives below:
2.2.1 Identification of Input Variables
Depending on the wellness framework, the inputs may represent environmental, physical, intellectual, emotional, spiritual, and vocational parameters [11].
2.2.2 Modeling the Individual’s State of Wellness
The objective here requires identification of the state variables, the rules that help constitute the wellness of the individual, the construction of the wellness state space, and specification of the dynamics of the system, i.e., how an individual’s state of wellness changes over time in response to a combination of their current state and suggestions and recommendations for creating a healthier lifestyle.
2.2.3 Designing the Interventions
A key consideration involves the design and delivery of the intervention that would be the most effective for helping the individual to create a desired wellness state that takes into account that person’s present and previous states of wellness.
Fig. 2 depicts the engineering of the concept of wellness within the control theory framework. The concept illustrates the acquisition of various wellness assessment parameters through devices leading to the integrated construction of an individual’s state of wellness. The current wellness state of the individual is then categorized into a finite set pool consisting of optimal, good, fair, poor, and extremely unhealthy. The categorization serves as a motivation and assistive tool for both users and prescribers. The parameter indices in a broader wellness state category, along with the history of previous wellness states, set the basis for the prescriber to recommend the intervention(s) for individuals to improve or maintain their category.
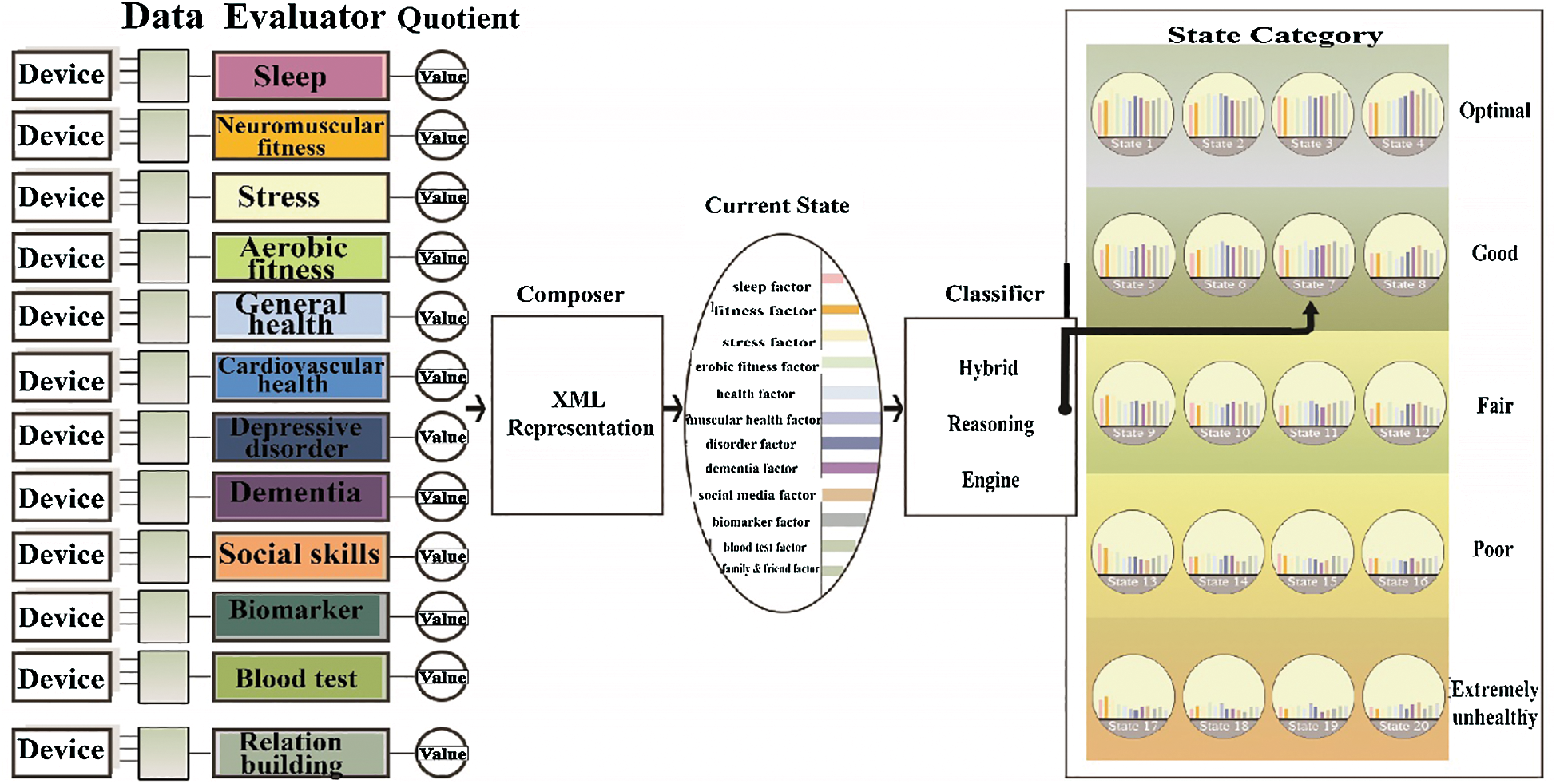
Figure 2: Engineering wellness within the optimal control theory framework
Fig. 3 shows a generalized architecture for a smart wellness service platform. Assessment, prescription, and practice systems provides the abovementioned services in the proposed service model and are connected to a cloud server. The cloud server hosts the core of the management and motivational services, including personalization, contextualization, and analytics.
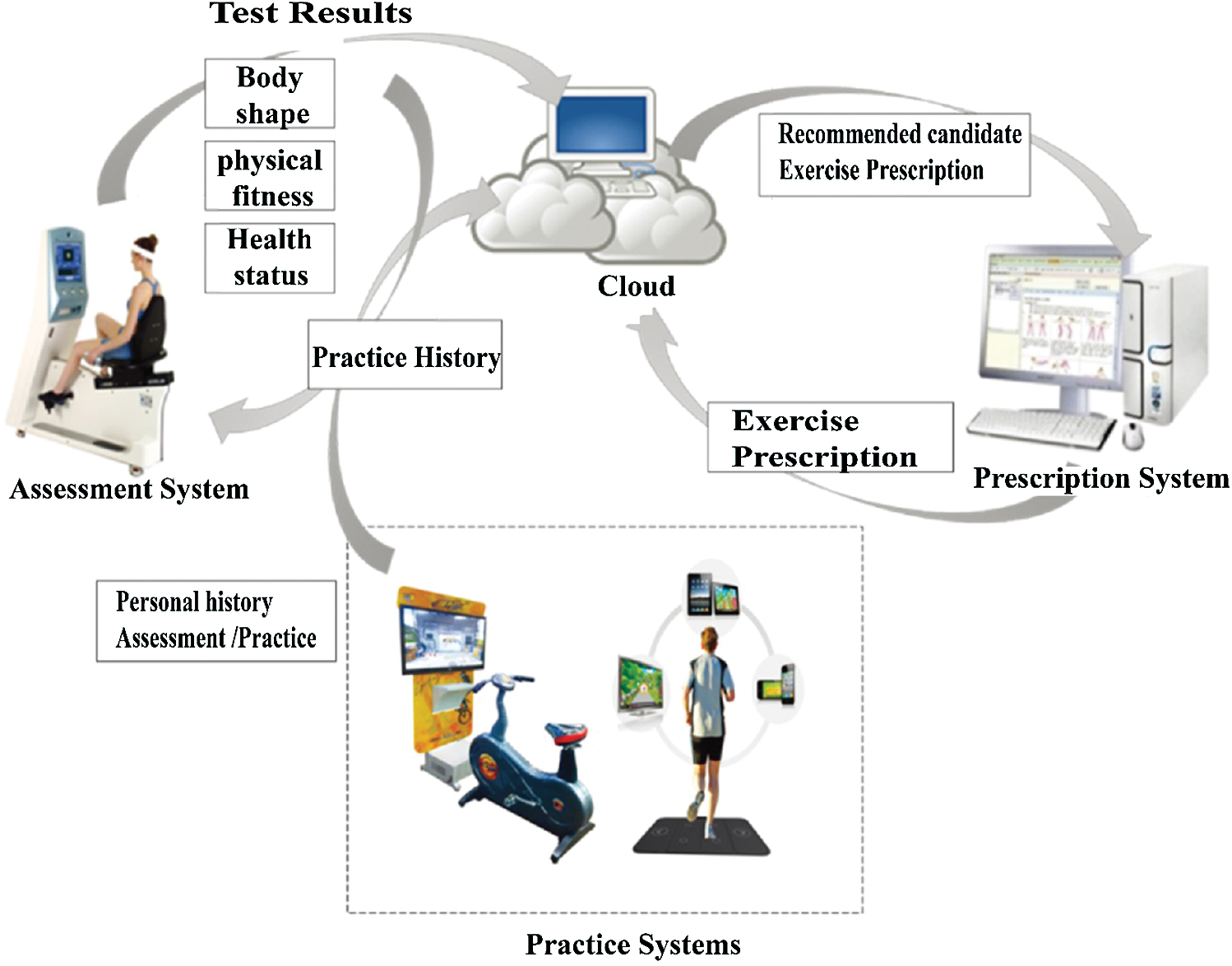
Figure 3: Generalized wellness service platform architecture
3 HIMS Hub: Smart Physical Wellness Service Platform
The HIMS Hub is the practical embodiment of the vision and service model, as discussed in previous sections. Fig. 4 depicts the HIMS Hub, an integrated service provision platform that can exist in wellness service centers, an individual’s home, fitness centers, or outdoor environments. However, at this point in time, we imposed two limitations on our implementation: to limit the service provision platform to the construction of the smart wellness service center and its associated technologies (such as a cloud server, website, or mobile app), and to limit the dimensions of wellness to physical wellness only.
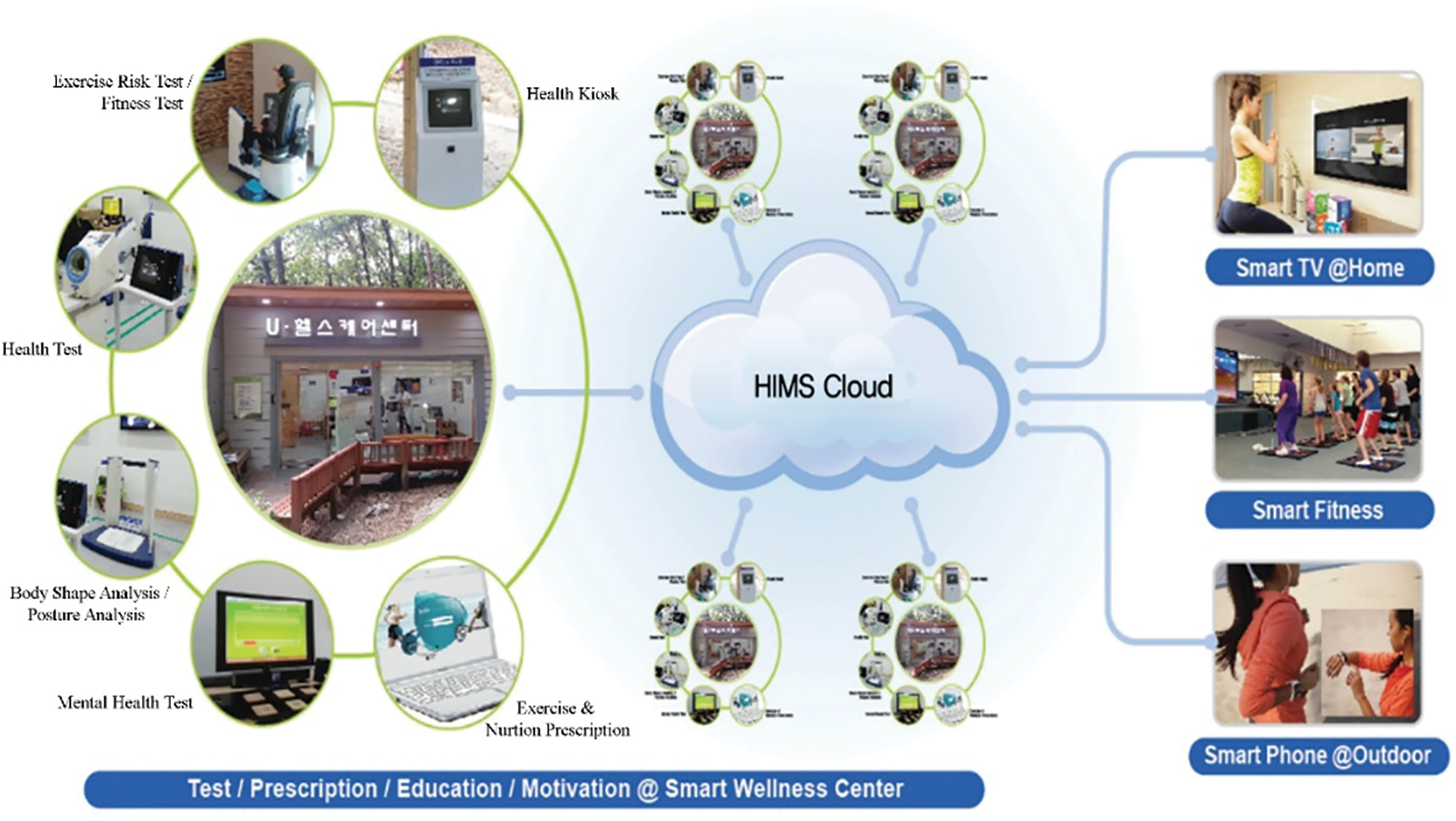
Figure 4: HIMS Hub—The converged technologies of the Smart Wellness platform
Physical wellness may be considered as the most fundamental single dimension in a knowledge and skills pool that can be merged with the technologies needed for embarking the era of smart wellness. The concomitant effects of physical wellness in almost every aspect of human life have been reported in literature, emphasizing benefits such as longevity [10,12], quality of life (management of chronic diseases, physical independence, reducing falls in aging populations) [10,13–16], work productivity [10,17], and reduced absenteeism [10,18].
Despite the many benefits of a wellness discipline, more efforts are needed in this domain to meet the magnitude of the projected burdens (aging population, chronic diseases, and medical expenses). The authors in [10] stated that the fundamental reason for this disparity is the direction of efforts that are largely scaled to fit in the present medical service modality (HealthCare 2.0). It would be an oversight to state that no efforts are being directed toward HealthCare 3.0, as the literature evidence depicted in [4–7,19] shows considerable efforts. However, it is important to highlight that the volume of practical efforts does not represent the readiness and potential of the wellness discipline. In particular, the discipline of sports and exercise medicine within the realm of physical wellness has significantly matured over the last four decades [10]. The discipline’s focus (physical functional capacity over disease diagnosis), holistic and integrated approach, and ongoing efforts of the discipline to transfer knowledge and skills from a performance-oriented population (i.e., athletes) to a general populace is well-positioned to champion the cause of immediate practical realization [10]. The development and testing of the proof of concept will emerge over a period of time, and the design and architectural implementations are described below.
The physical wellness parameters considered for the HIMS Hub are:
Body shape parameters (weight, height, body mass index, and body mass percentage);
Physical fitness parameters (hand muscular strength and endurance, leg muscular strength and endurance, cardio-respiratory endurance, power and agility, body balance, body fat percentage);
Physical health parameters (blood pressure, blood glucose level, and blood cholesterol level).
The two primary design considerations for implementation of the HIMS Hub are scalability and user comfort/ease.
The Information and Communication Technologies (ICT)-enabled center is equipped with four physical devices: Kiosk, HIMS Fitness, HIMS Health, and HIMS Expert.
The Kiosk provides user management functions, including user registration through a radio frequency identification (RFID) card, the monitoring of a user’s progress over a period of time, and letting users know their status, not only in comparison to a generalized standard but also in comparison to other users of the same age and gender. HIMS Health and HIMS Fitness are devices for assessing the user’s wellness state. HIMS Health assesses a user’s body shape and physical health parameters. HIMS Fitness assesses physical fitness parameters in addition to HIMS Health parameters. The HIMS Health device provides user comfort, monitoring the parameters most frequently assessed by users, while HIMS Fitness performs a comprehensive assessment of physical wellness. For further design consideration of user comfort, which is particularly important for the elderly, each assessment device is equipped with an RFID-based login facility, a touchscreen interface, a focus on text size and color for better readability, and a simple and easy-to-use graphic user interface (GUI) that offers five commands (Start Test, Stop Test, Skip Test, Next Test, and Finish Test). Fig. 5 shows HIMS Health, HIMS Fitness, and a three-layered architecture consisting of device, library, and application layers. The device layer includes sensors and actuators, including the abstractions for the user interface. The library layer provides a range of libraries including but not limited to the domain of signal processing, sports and exercise medicine, database, and web services. The application layer includes the apps for assessing the physical wellness parameters. HIMS Expert is software for managing a user’s exercise prescriptions. The software offers two options: One for prescription expert authors and one for health center managers. Implementation of a smart physical wellness center entails not only technology but also human expertise, in the form of the Healthcare Manager (HCM). HCM guides the users in the use of the equipment, provides education about and interpretation of their test results, recommends appropriate prescriptions, and motivates the users to improve their state of wellness and to continually assess it. The prerogative for the selection of physical wellness parameters, design of prescriptive interventions, and categorization within the wellness state space has been given to experts in the field of exercise and sports medicine.
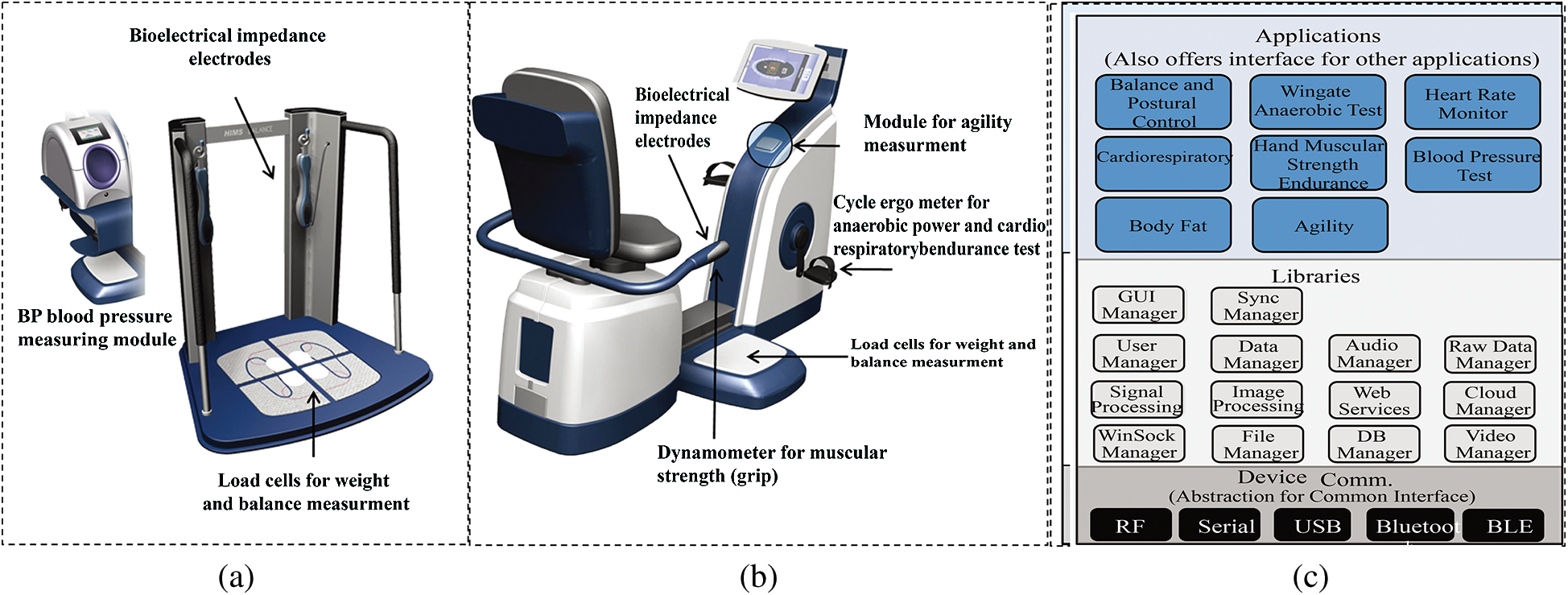
Figure 5: (a) HIMS Health, (b) HIMS Fitness, and (c) Three-layer assessment systems architecture
Fig. 6 shows that the prescription service consists of three modules: Feature Extraction, Inference Engine, and System Optimization. Details pertinent to the design, considerations, and architecture are given in [20].
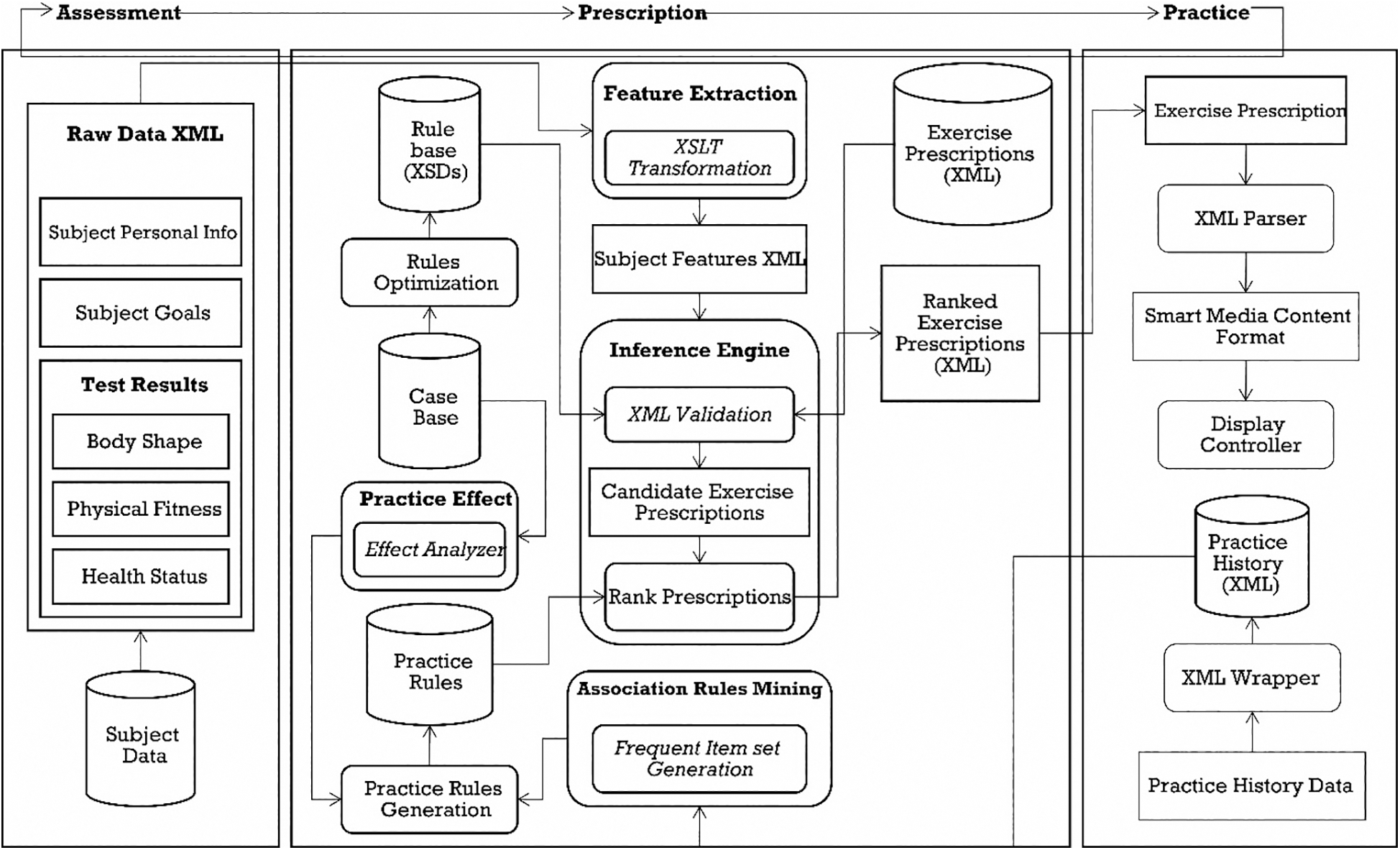
Figure 6: HIMS Expert—Prescription service architecture
Peripheral to the smart physical wellness center are a mobile phone app and a website, which provide users with an assessment history and prescription. Fig. 7 shows the screenshots of the mobile app, and the links in [21,22] show the implemented websites in the various centers.

Figure 7: Mobile app for HIMS Hub shows historical results and prescriptions
4 HIMS HUB: Analysis and Results of the Implementation of the Smart Wellness Service Platform
HIMS HUB has been deployed successfully in six major cities in South Korea, as shown in Fig. 8. Data gathered from these deployments are currently being used for the improvement of the design and architecture of the overall service platform, as well as for epidemiological and demographic studies. Research articles published in [23–25] are representative of the ongoing research based on the wellness service platform.
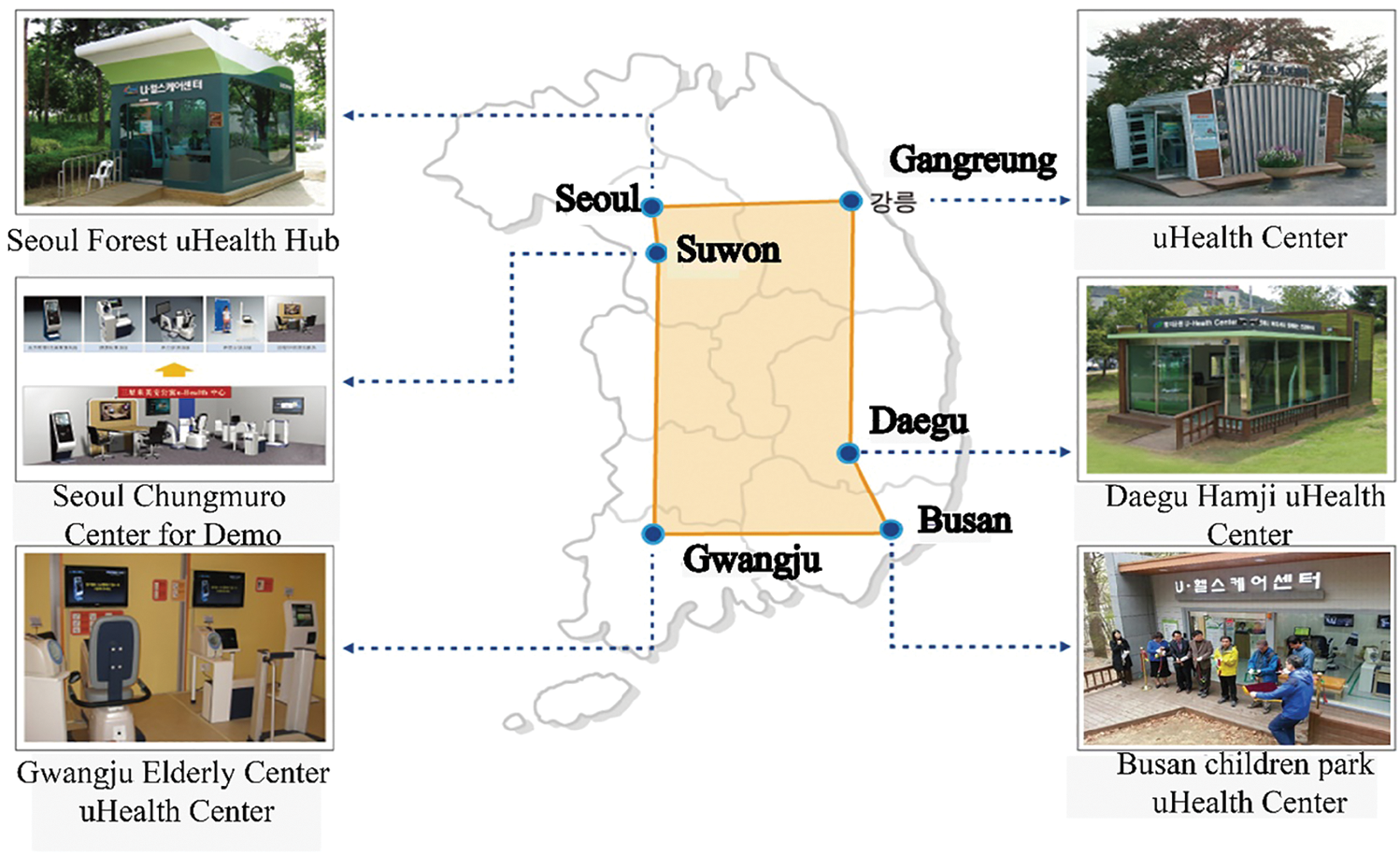
Figure 8: HIMS Hub deployed in six major cities in South Korea
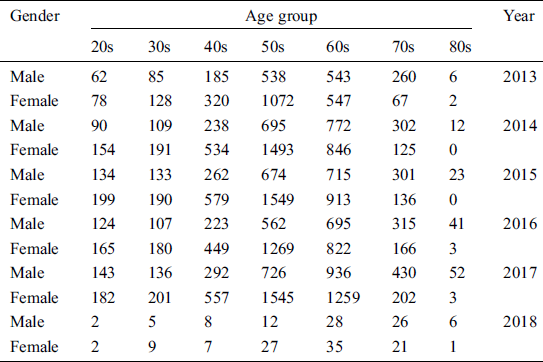
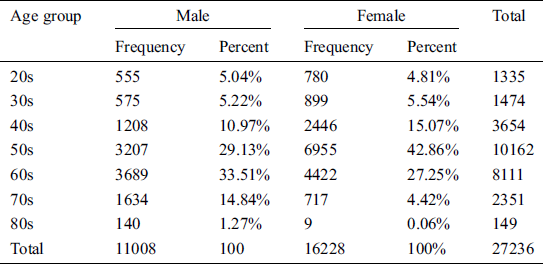
The HIMS Hub smart physical wellness service platform is approved by the Korea Food and Drug Administration (KFDA). Analysis and results of the implementation of the smart wellness service platform are presented. Data gathered from 27,236 users’ physical evaluations at a wellness center in Busan City from April 2013 to May 2018 were used for analysis. We used StataCorp’s Stata version 12.0 for the statistical analysis. Fig. 9 shows the data pertaining to usage of health and fitness tests. Fig. 10 shows the demographics for the user of the service platform, by gender. The actual statistics are shown in Tabs. 2, 3 and 4. The percentage of female participants was 59.58%, vs. 40.42% for males. The same higher participation by females is observed in nearly all years. These results show the demographics for the participants by age group and gender. The seven age categories were 20s, 30s, 40s, 50s, 60s, 70s, and 80s or older. The highest percentage of participants was females and males in their 50s and 60s, while males in their 70s have a higher rate of participation than females in the same age group.
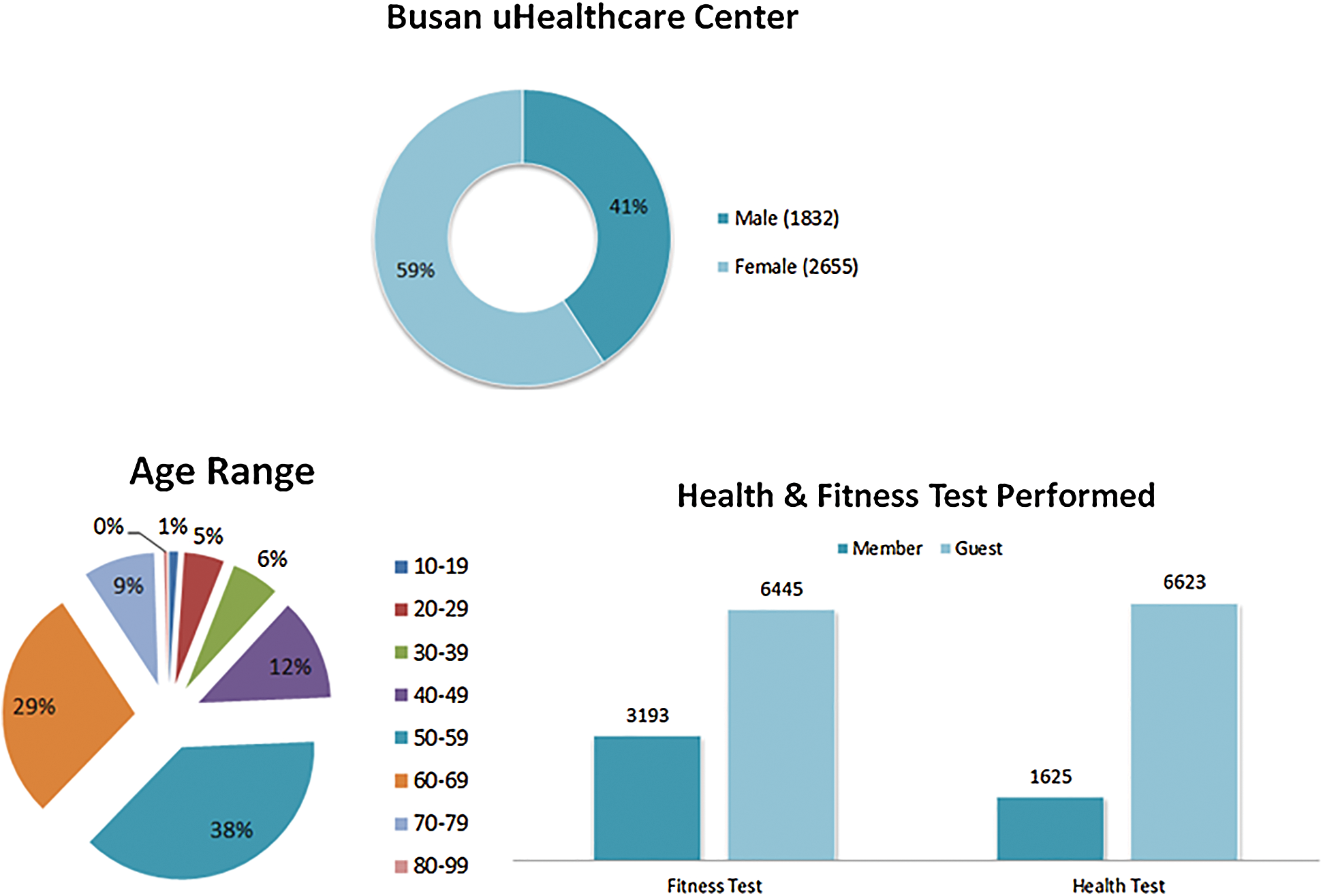
Figure 9: Data pertaining to the health and fitness test
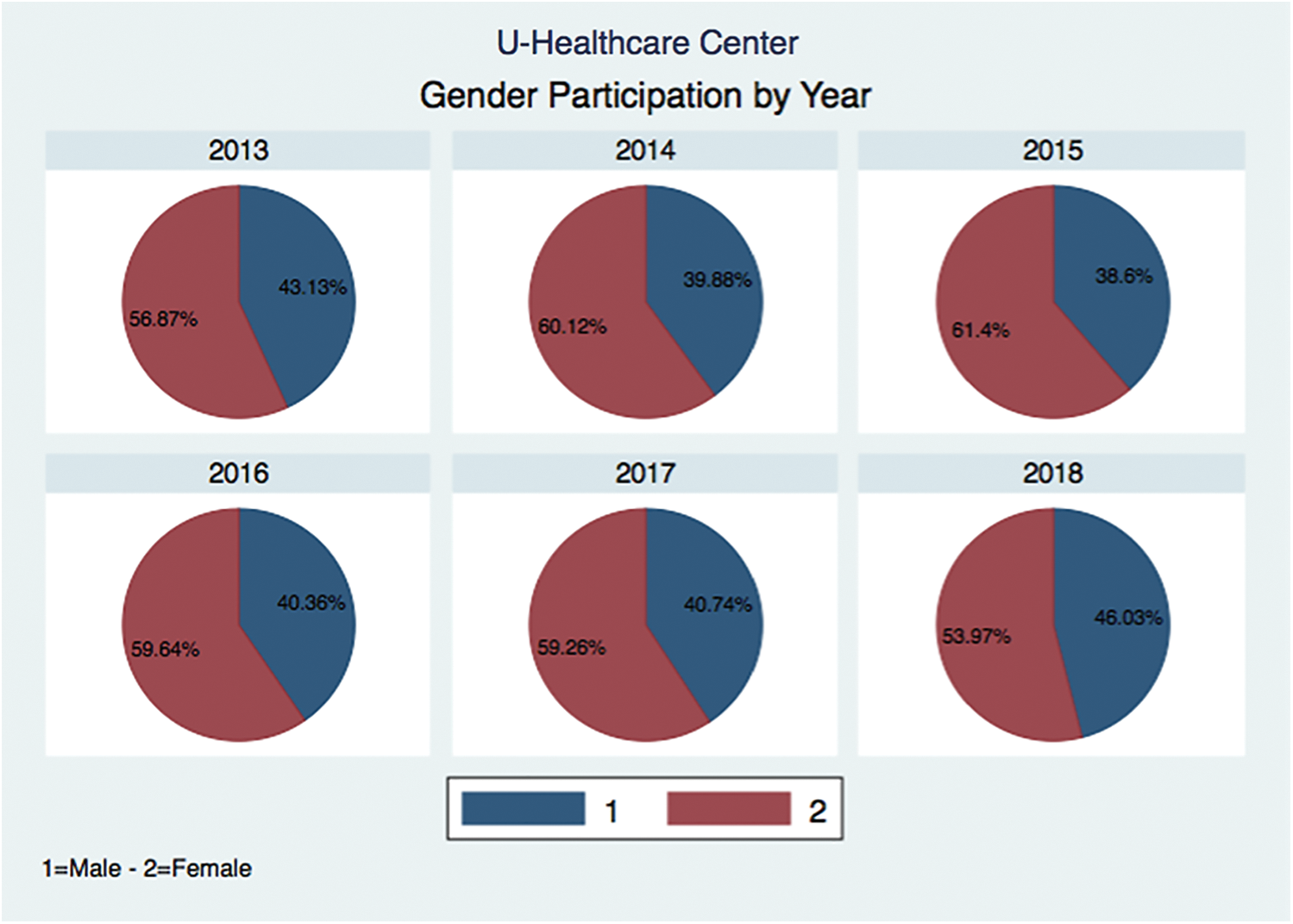
Figure 10: HIMS Hub and gender participation by year
Table 2: Total gender participation
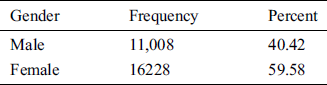
Table 3: Yearly participation by gender
This article reports on the design and deployment of a smart wellness service platform, as well as the development of a software architecture to support the building of wellness applications. HIMS Hub includes the following physical wellness parameters:
Body shape parameters (weight, height, body mass index, and body mass percentage);
Physical fitness parameters (hand muscular strength and endurance, leg muscular strength and endurance, cardio-respiratory endurance, power and agility, body balance, body fat percentage);
Physical health parameters (blood pressure, blood glucose level, and blood cholesterol level).
Next, four physical devices were installed: Kiosk, HIMS Health, HIMS Fitness, and HIMS Expert. Through Kiosk, the user’s progress was monitored using an RFID card. The user’s wellness was monitored through HIMS Health and HIMS Fitness. HIMS Expert is software for managing a user’s exercise prescriptions. The software offers two options: one for prescription expert authors and one for health center managers.
Furthermore, Developers of previous wellness applications have only been able to use a limited variety of sensors that provide only basic information related to physiological data (i.e., an ECG) or physical activity, but this article provides a comprehensive assessment of wellness. The data from 27,236 users in Busan Metropolitan City, during the period of April 2013 to May 2018, were used for analysis. The seven age categories were the 20s, 30s, 40s, 50s, 60s, 70s, and 80s or older. It was found that females and males in their 50s and 60s constituted the highest percentage of participants, while males in their 70s had a higher rate of participation than females in the same age group.
Future work includes increasing the number of sites in South Korea as well as in other countries, increasing the dimensions of wellness to beyond physical wellness, construction of biofeedback base monitoring systems for practice service, and improving the overall service platform based on user feedback.
Acknowledgement: We are thankful to Dr. Dae-Geun Jang and Dr. Ramiro Bravo Santisteban for their valuable efforts overall.
Funding Statement: This research work was supported by Korea Electric Power Corporation (Grant Number: R18XA02).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. A. Sano and R. W. Picard. (2014). “Understanding ambulatory and wearable data for health and wellness,” in Proc. AAAI, 2014 Spring Sym., Stanford, CA, USA, pp. 59–60.
2. S. Hiremath, G. Yang and K. Mankodiya. (2014). “Wearable Internet of Things: Concept, architectural components and promises for person-centered healthcare,” in Proc. 4th Int. Conf. on Wireless Mobile Communication and Healthcare, Athens, Greece, pp. 304–307.
3. S. S. Intille. (2002). “Designing a home of the future,” IEEE Pervasive Computing, vol. 1, no. 2, pp. 76–82.
4. J. F. Coughlin, B. Reimer and B. Mehler. (2011). “Monitoring, managing, and motivating driver safety and well-being,” IEEE Pervasive Computing, vol. 10, no. 3, pp. 14–21.
5. P. Y. S. Hsueh, R. J. R. Lin, M. J. H. Hsiao, L. Zeng, S. Ramakrishnan et al.. (2010). , “Cloud-based platform for personalization in a wellness management ecosystem: why, what, and how,” in Proc. 6th Int. ICST Conf. on Collaborative Computing: Networking, Applications, Worksharing, Chicago, IL, USA, pp. 1–8.
6. L. Zeng, P. Y. Hsueh, H. Chang, C. Chung and R. Huang. (2010). “Greenolive: an open platform for wellness management ecosystem,” in Proc. 2010 IEEE Int. Conf. on Service Operations and Logistics, and Informatics, Qingdao, China, pp. 88–93.
7. E. Dishman. (2004). “Inventing wellness systems for aging in place,” Computer, vol. 37, no. 5, pp. 34–41.
8. L. Hood and S. H. Friend. (2011). “Predictive, personalized, preventive, participatory (P4) cancer medicine,” Nature Reviews Clinical Oncology, vol. 8, no. 3, pp. 184–187.
9. J. F. Coughlin. (2007). “Disruptive demographics, design, and the future of everyday environments,” Design Management Review, vol. 18, no. 2, pp. 53–59.
10. G. O. Matheson, M. Klügl, J. Dvorak, L. Engebretsen, W. H. Meeuwisse et al.. (2011). , “Responsibility of sport and exercise medicine in preventing and managing chronic disease: Applying our knowledge and skill is overdue,” British Journal of Sports Medicine, vol. 45, no. 16, pp. 1272–1282.
11. J. E. Myers, T. J. Sweeney and J. M. Witmer. (2000). “The wheel of wellness counseling for wellness: A holistic model for treatment planning,” Journal of Counseling & Development, vol. 78, no. 3, pp. 251–266.
12. C. E. Matthews, A. L. Jurj, X. O. Shu, H. L. Li, G. Yang et al.. (2007). , “Influence of exercise, walking, cycling, and overall nonexercise physical activity on mortality in Chinese women,” American Journal of Epidemiology, vol. 165, no. 12, pp. 1343–1350.
13. I. J. Hickman, J. R. Jonsson, J. B. Prins, S. Ash, D. M. Purdie et al.. (2004). , “Modest weight loss and physical activity in overweight patients with chronic liver disease results in sustained improvements in alanine aminotransferase, fasting insulin, and quality of life,” Gut, vol. 53, no. 3, pp. 413–419.
14. K. S. Courneya and C. M. Friedenreich. (1999). “Physical exercise and quality of life following cancer diagnosis: A literature review,” Annals of Behavioral Medicine, vol. 21, no. 2, pp. 171–179.
15. R. C. Cassilhas, V. A. R. Viana, V. Grassmann, R. T. Santos, R. F. Santos et al.. (2007). , “The impact of resistance exercise on the cognitive function of the elderly,” Medicine & Science in Sports & Exercise, vol. 39, no. 8, pp. 1401–1407.
16. C. D. Lee, S. N. Blair and A. S. Jackson. (1999). “Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men,” American Journal of Clinical Nutrition, vol. 69, no. 3, pp. 373–380.
17. D. M. Gates, P. Succop, B. J. Brehm, G. L. Gillespie and B. D. Sommers. (2008). “Obesity and presenteeism: The impact of body mass index on workplace productivity,” Journal of Occupational and Environmental Medicine, vol. 50, no. 1, pp. 39–45.
18. G. Brunello, P. C. Michaud and A. Sanz-de-Galdeano. (2009). “The rise of obesity in Europe: an economic perspective,” Economic Policy, vol. 24, no. 59, pp. 551–596.
19. K. C. Tseng, A. M. K. Wong, C. L. Hsu, T. H. Tsai, C. M. Han et al.. (2013). , “The iFit: an integrated physical fitness testing system to evaluate the degree of physical fitness of the elderly,” IEEE Transactions on Biomedical Engineering, vol. 60, no. 1, pp. 184–188.
20. F. Anwar, J. Jang, R. Bravo and S. H. Park. (2012). “XML based personalized exercise prescription system using hybrid reasoning technique,” in Proc. 2012 Cairo Int. Biomedical Engineering Conf., Giza, Egypt, pp. 14–17.
21. Daegu City, Daegu u-Healthcare Center. [Online]. accessed on 20 May 2015. Available: http://u-health.buk.daegu.kr.
22. Busan City, Busan u-Healthcare Center. [Online]. accessed on 20 May 2015. Available: http://u-healthcare.busan.go.kr.
23. S. Youm and S. H. Park. (2015). “How the awareness of u-healthcare service and health conditions affect healthy lifestyle: An empirical analysis based on a u-healthcare service experience,” Telemedicine and e-Health, vol. 21, no. 4, pp. 286–295.
24. R. D. Bravo Santisteban, S. Youm and S. H. Park. (2015). “U-healthcare center service in Busan City, South Korea: An empirical analysis and the results of 1 year of service,” Telemedicine and e-Health, vol. 21, no. 10, pp. 774–781.
25. R. D. Bravo Santisteban, Y. L. Kim, U. Farooq, T. S. Kim, S. Youm et al.. (2016). , “Environment and its influence on health and demographics in South Korea,” International Journal of Environmental Research and Public Health, vol. 13, no. 2, pp. 183.
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |