DOI:10.32604/cmc.2022.019097
| Computers, Materials & Continua DOI:10.32604/cmc.2022.019097 |  |
| Article |
RFID Adaption in Healthcare Organizations: An Integrative Framework
1College of Technical Innovation, Zayed University, Abu Dhabi, UAE
2Nathan Campus, Griffith University, Australia
3Department of Computer Science, King Saud University, Riyadh, Saudi Arabia
4Golden Gate University, San Francisco, California, USA
*Corresponding Author: Ahed Abugabah. Email: ahed.abugabah@zu.ac.ae
Received: 02 April 2021; Accepted: 13 May 2021
Abstract: Radio frequency identification (RFID), also known as electronic label technology, is a non-contact automated identification technology that recognizes the target object and extracts relevant data and critical characteristics using radio frequency signals. Medical equipment information management is an important part of the construction of a modern hospital, as it is linked to the degree of diagnosis and care, as well as the hospital’s benefits and growth. The aim of this study is to create an integrated view of a theoretical framework to identify factors that influence RFID adoption in healthcare, as well as to conduct an empirical review of the impact of organizational, environmental, and individual factors on RFID adoption in the healthcare industry. In contrast to previous research, the current study focuses on individual factors as well as organizational and technological factors in order to better understand the phenomenon of RFID adoption in healthcare, which is characterized as a dynamic and challenging work environment. This research fills a gap in the current literature by describing how user factors can influence RFID adoption in healthcare and how such factors can lead to a deeper understanding of the advantages, uses, and impacts of RFID in healthcare. The proposed study has superior performance and effective results.
Keywords: RFID; healthcare; information technology; user factors
RFID is one of the 16 core innovations for the next decade, according to MIT [1], which also ranks it as the tenth most groundbreaking technology in the last 25 years. RFID is a smart technology for data capture and real-time information visibility, according to its proponents. Many sectors, including logistics and supply chains, engineering, automotive and food safety management, and healthcare, have high potential for it [2]. Despite the fact that RFID was established in the early 1970s, it has recently piqued the interest of academics and practitioners.
Innovative technology, such as RFID, smart information systems, and networks, have been implemented into the healthcare sector to eliminate medical errors, minimize costs, improve decision-making, and assist in the discovery of medical solutions [3–5]. Insufficient and unreliable pharmaceutical inventory monitoring and operations, lack of patient identification, inability to accurately monitor patient locations, administration of incorrect medication to patients, and inability to track equipment are just a few of the problems facing healthcare organizations, according to recent studies [6–7]. This led many healthcare organizations to invest on IT and its applications with the hope of overcoming such challenges.
RFID tags are hailed as one of the most promising technologies for addressing these issues [8] and enhancing performance efficiency and service quality [9–14]. RFID may, for example, aid in the safety of medical personnel by identifying and tracing potentially infected individuals [15], improving patient monitoring and safety, improving pharmaceutical operations and medication use, and improving in-hospital location tracking, as well as patient identification [16–19], tracking hospital assets and supplies, error prevention, medicine tracking, and securing patient information.
Despite the potential benefits of RFID applications, healthcare organizations are still in the early stages of adopting RFID in various functional areas [20–22]. The scarcity of RFID adoption in healthcare, as well as the lack of publications and empirical studies that compare RFID adoption in healthcare to other settings, such as manufacturing and logistics and supply, are cited as reasons.
As a result, researchers argue that decisions about the implementation of information technology (IT) in healthcare are dynamic and include multiple stakeholders, rather than being strictly based on technological characteristics and environmental factors [23,24]. Many IT technologies in businesses have a two-part and/or multi-level adoption decision mechanism that involves formal decision-making as well as local adoption. Key decision makers normally make a structured decision to implement and purchase the innovation and make it available to the company. The following is a typical local adoption decision: Individuals such as doctors and medical practitioners, who are intended consumers, determine when and how to use the innovation [25]. The second portion, which concerns the advantages obtained from such decisions for both parties, appears to be just as relevant as the first. Most previous IT studies that investigated adoption decisions focused on organizational and environmental variables to help organizations explain their significant financial investments and measure performance outcomes, according to the literature review discussed below. Person and consumer considerations, unfortunately, have been identified as crucial aspects that have received insufficient attention in previous research. There has been an absence and/or overlooking of consumer considerations in many studies.
As a result, the aim of this study is to create an integrated view of a theoretical framework to identify factors that influence RFID adoption in healthcare and to conduct an empirical review of the impact of several factors on RFID adoption in the healthcare industry, including technology, organizational, environmental, and individual factors. Unlike other studies, the current one will focus more on person and human factors in order to better understand the phenomenon of RFID adoption in the healthcare industry, which has been identified as a complex and challenging work environment in previous research [26]. This study fills a gap in the current literature by demonstrating how user factors can influence RFID adoption in healthcare and how such factors can lead to a deeper understanding of the advantages, applications, and effects of RFID in the healthcare sector. The aim of this study is to develop a structure for RFID technology adoption in healthcare organizations by taking into account a variety of factors and dimensions, such as RFID adoption and implementation, as well as the benefits and challenges that may prevent healthcare organizations from reaping the benefits of such technology.
Adoption of technology is a research subject that has piqued the interest of IT researchers for a long time. Various theories and models have been built in IT to recognize and forecast the acceptance of innovations by both individuals and organizations, as well as to define adoption drivers of innovations. Diffusion of technologies (DOI), technology-organization-environment system (TOE), technology adoption model (TAM), theory of reasoned action (TRA), and united theory of acceptance and use of technology are some of these models.
RFID technology adoption, like other technologies, occurs over time and in phases, including initiation, experimentation, and deployment [27–29]. As a result, researchers have used innovation frameworks and hypotheses to investigate the essential factors of RFID technology adoption as well as the reasons for the slow adoption rate. Since they have been found to assist researchers in predicting the factors that contribute to RFID adoption and usage, the DOI and TOE theories have been the primary theories used by researchers for grounding RFID adoption research. Thus, existing studies on RFID have been dominated by organizational, behavioral, and information system perspectives, with only limited conceptual and empirical studies.
Aside from the well-developed theory of DOI and TEO, much of the literature on adoption and diffusion for various IT cases comes from various perspectives, including country [30], industry [31], and organization [32]. Organizational viewpoints, on the other hand, have gotten the most coverage in the literature [33–35]. Different research goals and topics characterize studies of IT adoption at the country level, with a strong emphasis on key IT infrastructure aspects and IT expenditure, resulting in various evaluations and research outcomes [36]. Similarly, industry-level studies have had a limited emphasis and have addressed RFID adoption without presenting specific results of the factors that led to the adoption decision. This may be because the structure was adapted from a business perspective to justify investment decisions and clarify the connection between IT and business success [37].
Despite the fact that RFID has the ability to play a critical role in providing safe and reliable healthcare, adoption of RFID and IT advances in general in the healthcare industry has lagged behind other industries [38,39]. Many professionals are aware of the potential benefits of RFID, but they are unable to justify a significant investment in the technology. As a result, the DOI and TOE tenets may not hold true in the case of RFID adoption. The refusal of certain Wal-Mart vendors to accept RFID amid the retailing giant’s RFID mandate is the best anecdotal proof of a reluctance to embrace RFID. This means that, despite the technology’s potential advantages, many organizations are hesitant to implement RFID, and that there are other factors that influence an organization’s decision to adopt RFID. This emphasizes the importance of including other factors in previous studies’ frameworks, rather than focusing solely on organizational factors and benefits perceived at the organizational level [40].
In addition to the DOI and TOE models, researchers have used the human-organization-technology fit model (HOT-fit model) to conduct detailed evaluation research on IT application adoption in healthcare settings [41]. Reference [42] provided a comprehensive, specific assessment of factors, measurements, and measures (HOT-fit model) that could be used in IT acceptance and evaluation studies. Human factors are crucial to the assessment of IT technology acceptance and growth in healthcare, according to the HOT-fit model. The role of human behavior in hospital settings in affecting IT adoption has been ignored in the literature on healthcare IT [43]. According to researchers, certain human factors must be taken into account when introducing and implementing any technological breakthrough in the healthcare industry [44–48]. In other words, researchers in IT adoption in general, and healthcare in particular, hold a firm belief in the role of human factors in the adoption and evaluation of IT applications. Researchers also discovered a significant overlap between the HOT-fit model and the TOE system in this regard. They also mentioned that the HOT-fit model does not take into account the environmental context. Human factors, on the other hand, are not specifically stated in the TOE system. As a result, each one is telling a different part of the story. Incorporating these two models, as well as DOI measurements, seems reasonable and will result in a more comprehensive structure. In this regard, the authors of [49] argue that the better the match between technical, human, and organizational influences, the more healthcare IT’s potential can be realized. As a result, these considerations can be used to create a more systematic and precise assessment process for assessing RFID adoption in healthcare.
The current research incorporates an integrated model of DOI and TOE, as well as the HOT-fit model and the inclusion of user variables that are crucial to RFID adoption decisions, based on the literature on IT and RFID adoption and the theoretical perspectives discussed in the previous section. This will aid in the development of a solid theoretical basis for a deeper understanding of the factors that influence RFID adoption in the healthcare industry. The current model appears to be more inclusive, taking into account more aspects that are thought to be essential when implementing new technologies. We believe that integrating human “user” factors into these models would provide a thorough understanding of how individual and organizational factors interact to influence RFID adoption decisions, both collectively and individually. This will also help us understand how RFID usage will affect individual perceptions of success and healthcare facilities, which can help organizations and management justify substantial investments in such technology. The current model has a lot of potential for refocusing researchers’ attention on other variables when assessing RFID benefits.
3 Research Model and Hypotheses
The research framework was created after a thorough analysis of the literature and comparison of previous models and frameworks. As shown in Fig. 1, the research structure integrates various IT models such as TOE, DOI, and HOT-fit. These models have been extensively studied in the IT literature and have been cited as suitable for testing RFID adoption in healthcare.
Many prior IT innovation studies have cited technological factors such as complexity, compatibility, relative advantage, and privacy and protection as determinants influencing the decision to implement new technology [50]. In this regard, Davenport and Brooks (2004) identified uncertainty regarding RFID’s compatibility with other systems, such as enterprise resource planning systems, as a possible stumbling block. RFID is a diverse collection of resources that includes a variety of operating systems, middleware, hardware, programming languages, and architectural frameworks. The fact that RFID networks require globally coordinated numbering, frequency, and power standards adds to the complexity of these factors. Among a list of 12 problems affecting the future of RFID, researchers rated standards as the most difficult task [51]. RFID also necessitates a number of essential network and infrastructure requirements in order to function properly [52]. The following hypothesis was suggested based on the above discussion:
H1: Technological factors are associated with RFID adoption in healthcare organizations.
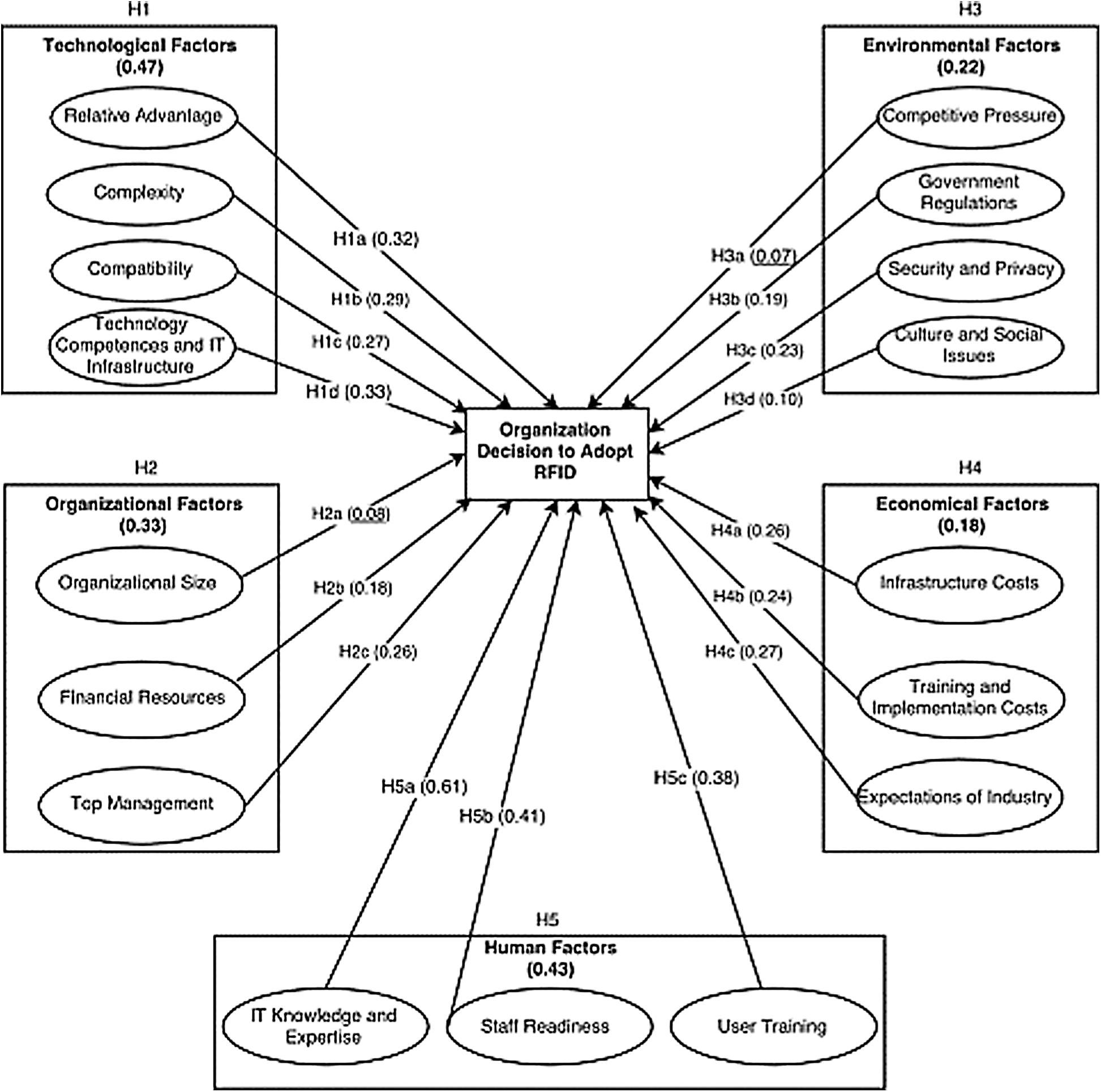
Figure 1: Research model
The degree to which an invention is viewed as having greater organizational benefits than the concept it supersedes is known as relative advantage. It is investigated whether RFID technology is regarded as superior to the technology it replaces, such as barcodes and/or conventional “manual” methods of holding records and performing tasks in hospitals [53–65]. As a result, RFID is supposed to provide hospitals with a competitive advantage. In other words, hospitals that see greater relative benefits from RFID applications are more likely to use it. As a result, the following hypothesis is put forth:
H1a: Relative advantage is associated with RFID adoption in healthcare organizations.
Based on the study model, the following hypotheses were drawn and tested in this study.
1. Technological factors
H1: Technological factors are associated with RFID adoption in healthcare organizations.
Technological factors that were tested in this study included relative advantage, complexity, compatibility and: technology competences and IT infrastructure.
2. Organizational factors
H2: Organizational factors are associated with the adoption of RFID in healthcare organizations.
Organizational factors that were tested in this study included organizational size, financial resources and top management support.
3. Environmental factors
H3: Environmental factors are associated with RFID adoption in health care organizations.
Environmental factors that were tested in this study included competitive pressure, government regulations, security and privacy concerns and culture.
4. Economic factors.
H4: Economic factors are associated with RFID adoption in healthcare organizations.
Economic factors that were tested in this stud included the costs, infrastructure costs, training and implementation costs and expectations of industry and market trends.
5. Human Factors
H5: Human factors are associated with RFID adoption in healthcare organizations.
Human factors that were tested in this study included IT knowledge and expertise
staff readiness and user training.
The research was conducted in the UAE’s healthcare system. Data was gathered from major hospitals in various cities throughout the UAE. The hospitals have restricted RFID application use in some functional areas and are preparing to expand RFID deployment to other operating areas. The research instrument (survey) was sent to the hospitals via email [66–73]. The study team received a total of 191 questionnaires. To ensure that the returned surveys were complete and eligible for review, data filtering and cleaning were performed. Because of their incompleteness and ineligibility, nine of the questionnaires were eliminated from further study.
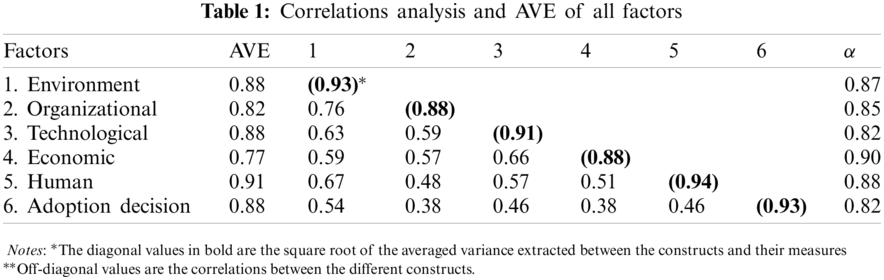
The research used a two-step structural equation modeling (SEM) method for model estimation and testing. The measurement model was first examined for validity using this methodology. The study instrument and measurements were subjected to a SEM test for hypothesis testing reliability and validity analysis in the second phase. Reliability was examined using Cronbach’s alpha (®). As shown in Tab. 1 all factors exceeded (0.70) alpha score indicating a satisfactory construct reliability (Tabachnick and Fidell, 2007). Discriminant and convergent validity analysis is used to assess validity. Calculating the square root of the average variance derived (AVE) for each factor was used to test discriminant validity. The AVE values for all variables are greater than the shared variance [74,75], as shown in Tab. 1.
According to Tabachnick and Fidell (2007), convergent validity is achieved when all variables load significantly, the composite reliability reaches 0.70, and the AVE values for all products surpass the threshold value (0.50). As shown in Tab. 1, all loadings scores are greater than 0.70, while AVE scores are greater than (0.50) demonstrating thus convergent validity [76,77].
6.1 Test of the Measurement Model
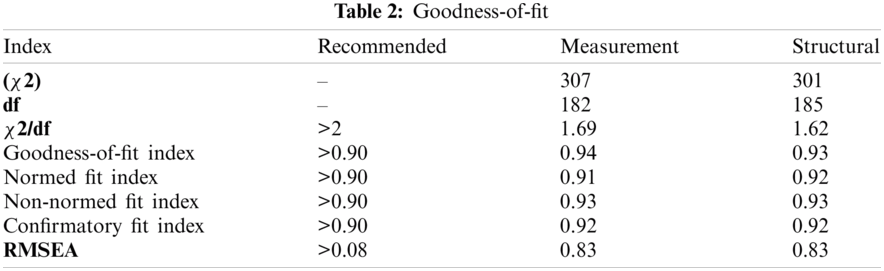
To evaluate the research hypotheses and analyze the research model, we used the structural equation method. The research model was tested using the chi-square goodness-of-fit index model (GFI) prior to hypotheses testing. Researchers often recommend a GFI index exceeding 0.80, and the cut-off criterion should be ≥0.90 for both indices of normed fit index (NFI) and incremental fit index (IFI) for acceptable model fitness. Researchers also recommend that fit values for the GFI should be greater than 0.90, whereas the adjusted GFI (AGFI) should be greater than 0.80. In general, if the value of χ2/df is smaller than 5, it is considered a good fit. Conversely, it is generally reported in conjunction with the root mean square error of approximation (RMSEA), and in a well-fitting model, the lower limit is close to 0, whereas the upper limit should be less than 0.08 t. As shown in Tab. 2 goodness-of-fit (GOF) statistics indicate an acceptable model fitness demonstrating thus that the proposed model has a good fit with the data.
6.2 Tests of the Structural Model
The relationships between the research contracts were evaluated using path coefficients and t-test tests, and the structural model was tested using structural equation modeling. To make it easier to compare the validity findings, the structural model results for fitness measures are shown in Tab. 3. The GOF indices for the structural model were X2/df = 1.62, CFI = 0.92, GFI = 0.93, NFI = 0.92, and RMSEA = 0.83. Thus, the proposed model revealed a good fit with RFID data. Overall, most study hypotheses were supported, and only two hypotheses were rejected (H2a, β = 0.08 and H3a, β = 0.09). The paths between most of the factors were found to have significant and positive relationships. The hypotheses, path coefficients (β), and t-values for all factors are summarized in Tab. 3, P < 0.05.
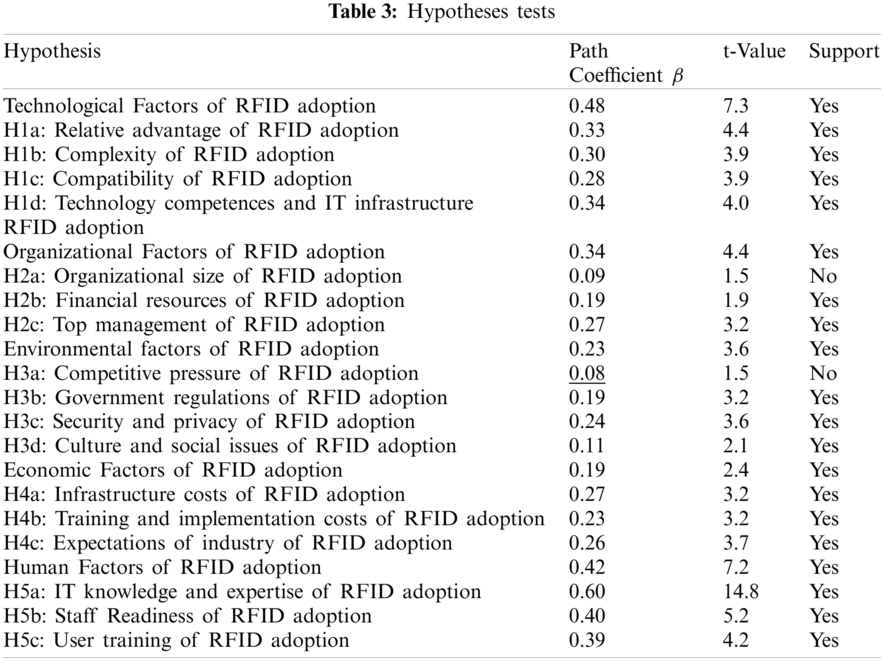
The study analysis showed that environmental factors, organizational factors, economic factors, technological factors, and human factors significantly affect the adopt RFID in with (β = 0.47, t = 809). The analysis also indicated that technological factors were the most influential factors on RFID adoption among all the study factors as (β = 0.47, t = 7.35, p < 0.05). Hence, H1 is supported. Whereas small impact but significant was found for the environment factors on RFID adoption as (β = 0.18, t = 2.46). As expected, the findings revealed a significant impact of human factors on RFID adoption indicating that these factors are crucial when adopting RFID in as (β = 0.43, t = 7.20).
Surprisingly, neither organizational size nor competitive pressure had a major impact on RFID adoption decisions in healthcare organizations, according to the research. This may be because all hospitals, regardless of scale, use the same resources, treatments, and operations, and/or because these hospitals are government-funded. As a result, they have no incentive to compete because they all receive the same amount of support from the government. This finding is intriguing, and further research is needed to determine if private entities have different adoption determinants than government organizations, and/or whether IT adoption models function differently in different environments.
Our integrated platform serves as a useful guide for hospital stakeholders interested in promoting RFID adoption and reaping the benefits of the technology. The findings empirically support the suitability of combining HOT-fit with DOI and TOE, indicating that the combined model is effective and a good place to start understanding RFID adoption. In order to better understand professionals’ adoption of RFID technology, the study stressed the importance of considering variables at the consumer and person level, such as user characteristics and discrepancies. For example, doctors, nurses, and physicians’ perceptions of RFID benefits can influence their willingness to adopt and/or use RFID applications in their daily work. In other words, physicians can consider RFID as a tool that can provide them with a variety of operational and functional solutions based on their task needs and job requirements. As a result, such individual variations must be evaluated and taken into account prior to adopting and implementing RFID applications, rather than as a post-implementation problem. This finding is intriguing because it implies that when it comes to IT acceptance and implementation, different healthcare contexts will tell different stories. As a result, by using the same hypotheses and models, researchers might not obtain comparable findings to those obtained in other industries.
Organizational aspects such as top management views and financial capital are major determinants of RFID adoption, according to the findings. However, neither competitive intensity nor organizational size were found to have a major effect in the report (e.g., Lin et al., 2012; [5]). This may be explained by the fact that similar stresses exist in the private sector, where rivalry forces businesses to offer quality services in order to thrive and achieve competitive advantages. Given that government hospitals are non-profit entities, this study was performed in public hospitals, where such pressure does not exist.
In terms of technological factors, some dimensions, such as compatibility and technological competence, have received a lot of empirical support in the classic innovation and IT diffusion literature, whereas the importance of other dimensions has been emphasized in various RFID studies, such as IT infrastructure and complexity studies. This study also discovered that public hospitals place a higher value on IT department experience and knowledge than on other dimensions. These are significant variables that are often ignored in other research. Technological factors were found to be the most important determinants of RFID adoption in the healthcare industry, in line with previous conceptualizations of DOI and TOE models. IT infrastructure and technology competence were found to be the most important factors influencing a hospital’s RFID adoption decisions among these determinants. Furthermore, although IT vendors have addressed infrastructure and technology standards concerns [46], some technical issues remain with RFID adoption. Many variables, such as RFID reader range and the position of metal components and antennae, can affect read rates and data accuracy, so the installation of hardware and the positioning of RFID components, such as readers and tags, must be precisely handled. The resolution of these problems would encourage hospitals to implement RFID more easily and make top management decisions easier [9].
Whether an organization fully adopts RFID applications depends on the organization’s existing IT hardware and software and the possibility of integrating new IT implementations with existing systems. The findings reveal that available organization resources, such as current IT infrastructure and IT department staff skills, determine whether the organization (® = 0.33) will move to RFID. These factors also have an impact on RFID adoption and implementation within a business. As a result, the higher the level of IT skills and infrastructure, the greater the acceptance and use of RFID in healthcare organizations. This result backs up Brown and Russell’s (2007) findings, which claim that the lack of RFID adoption in many organizations is due to RFID’s incompatibility with current infrastructure, making organizations hesitant to commit to a full-scale implementation.
Human factors are central to the evaluation of healthcare IT adoption and development [75]. Person and human factors drive RFID adoption, according to the empirical findings. Individual variations and human factors were often overlooked in previous IT adoption studies. By integrating user and person variables, the predictive capacity of other IT adoption models (e.g., TOE and DOI) can be enhanced [14]. The key factors used in this study provide a valuable context for researching relevant domains of human factors, and this study demonstrates that they are important factors to consider when assessing RFID adoption in healthcare organizations. When hospitals consider RFID as an IT solution for their work process and operations, consumer IT awareness and experience, staff readiness, and training are all found to be significant and relevant.
Acknowledgement: The authors would like to thank the editors and reviewers for their review and recommendations.
Funding Statement: This work was supported by the Institute for Social and Economic Research (ISER), Zayed University, Under Policy Research Incentive Plan, 2017
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. N. Adhiana, Y. M. Hwang, M. J. Park and J. J. Rho, “An integrated framework for RFID adoption and diffusion with a stage-scale-scope cubicle model: A case of Indonesia,” International Journal of Information Management, vol. 3, no. 2, pp. 378–389, 2013. [Google Scholar]
2. N. Adhiana, Y. Hwang and J. J. Rho, “A two-dimensional framework for RFID adoption and diffusion: Strategic implications for developing,” Journal of Technology Management and Innovation, vol. 6, no. 2, pp. 176–188, 2011. [Google Scholar]
3. V. Aggelidis and P. Chatzoglou, “Using a modified technology acceptance model in hospitals,” International Journal of Medical Informatics, vol. 78, no. 2, pp. 115–126, 2009. [Google Scholar]
4. H. Ahmadi, M. Nilashi and O. Ibrahim, “Organizational decision to adopt hospital information system: An empirical investigation in the case of Malaysian public hospitals,” International Journal of Medical Informatics, vol. 84, no. 3, pp. 166–188, 2015. [Google Scholar]
5. H. Ahmadi, M. Nilashi, L. Shahmoradi and O. Ibrahim, “Hospital information systems adoption: Expert perspectives on an adoption framework for malaysian public hospitals,” Computes in Human Behavior, vol. 67, no. 2, pp. 161–189, 2017. [Google Scholar]
6. A. Anand and S. Kulshreshtha, “The B2C adoption in retail firms in india,” in Second Int. Conf. on Systems, Martinique, France, pp. 46–52, 2007. [Google Scholar]
7. M. Attaran, “RFID: An enabler for supply chain operations,” Supply Chain Management, vol. 12, no. 4, pp. 249–257, 2007. [Google Scholar]
8. J. Backhouse, “Assessing certification authorities: Guarding the guardians of secure e-commerce?,” Journal of Financial Crime, vol. 9, no. 3, pp. 217–226, 2002. [Google Scholar]
9. M. Bhattacharya, “A conceptual framework of RFID adoption in retail using rogers stage model,” Business Processes Management Journal, vol. 21, no. 3, pp. 517–540, 2015. [Google Scholar]
10. R. Bunduchi, C. Weisshaar and A. U. Smart, “Mapping the benefits and costs associated with process innovation: The case of RFID adoption,” Technovation, vol. 31, no. 9, pp. 505–521, 2011. [Google Scholar]
11. Q. Cao, D. R. Jones and H. Sheng, “Contained nomadic information environments: Technology, organization, and environment influences on adoption of hospital RFID patient tracking,” Information and Management, vol. 51, no. 2, pp. 225–239, 2014. [Google Scholar]
12. A. S. Carr, M. Zhang, I. Klopping and H. Min, “RFID technology: Implications for healthcare organizations,” American Journal of Business, vol. 25, no. 2, pp. 25–40, 2010. [Google Scholar]
13. A. Chong and F. Chan, “Structural equation modeling for multi-stage analysis on radio frequency identification (RFID) diffusion in the health care industry,” Expert Systems with Applications, vol. 39, no. 10, pp. 8645–8654, 2012. [Google Scholar]
14. A. Chong, M. Liu, J. Lou and O. Boon, “Predicting RFID adoption in healthcare supply chain from the perspective of users,” International of Production Economics, vol. 159, no. 1, pp. 66–75, 2015. [Google Scholar]
15. W. L. Currie, “Institutional isomorphism and change: The national programme for IT–10 years on,” Journal of Information Technology, vol. 27, no. 3, pp. 236–248, 2012. [Google Scholar]
16. S. Devarai, T. T. Ow and R. Kohli, “Examining the impact of information technology on healthcare performance: A theory of swift and even flow (TSEF) perspective,” Journal of Operations Management, vol. 31, no. 4, pp. 181–192, 2013. [Google Scholar]
17. S. Faber, M. Geenhuizen and M. D. Reuver, “Ehealth adoption factors in medical hospitals: A focus on the natherlands,” International Journal of Medical Informatics, vol. 100, no. 5, pp. 77–89, 2017. [Google Scholar]
18. M. Glabman, “Room for tracking: RFID technology finds the way,” Materials Management in Health Care, vol. 13, no. 5, pp. 26–36, 2004. [Google Scholar]
19. M. P. Liborio, O. S. Matinuci, S. Laudars, R. M. Lyrio, A. M. C. Machado et al., “Measuring intra-urban inequality with structural equation modeling: A theory-grounded indicator,” Sustainability, vol. 12, no. 20, pp. 1–18, 2020. [Google Scholar]
20. H. Hakim, R. Renouf and J. Enderle, “Passive RFID asset monitoring system in hospital environments,” in Proc. of the IEEE 32nd Annual Northeast Bioengineering Conf., USA, pp. 1–6, 2006. [Google Scholar]
21. W. Hong and K. Zhu, “Migrating to internet-based e-commerce: Factors affecting e-commerce adoption and migration at the firm level,” Information & Management, vol. 43, no. 2, pp. 204–221, 2006. [Google Scholar]
22. Z. Huang, B. D. Janz and M. N. Frolick, “A comprehensive examination of internet-EDI adoption,” Information Systems Management, vol. 25, no. 3, pp. 273–286, 2008. [Google Scholar]
23. S. Hung, W. Hung, C. Tsai and S. Jiang, “Critical factors of hospital adoption on CRM system: Organizational and information system perspectives,” Decision Support Systems, vol. 48, no. 4, pp. 592–603, 2010. [Google Scholar]
24. S. Kim and G. Garrison, “Understanding user’s behaviors regarding supply chain technology: Determinants impacting the adoption and implementation of RFID technology in south korea,” International Journal of Information Management, vol. 30, no. 5, pp. 388–398, 2010. [Google Scholar]
25. L. Lapointe, M. Mignerat and I. Vedelc, “The IT productivity paradox in health: A stakeholder’s perspective,” International Journal of Medical Informatics, vol. 80, no. 2, pp. 102–115, 2011. [Google Scholar]
26. C. Lee and J. Shim, “An exploratory study of radio frequency identification (RFID) adoption in the healthcare industry,” European Journal of Information Systems, vol. 16, no. 6, pp. 712–724, 2007. [Google Scholar]
27. J. Li, Y. F. Wang, Z. M. Zhang and C. H. Chu, “Investigating acceptance of RFID in chinese firms: The technology-organization-environment framework,” in IEEE Int. Conf. on RFID-Technology and Applications, Guangzhou, China, pp. 263–268, 2010. [Google Scholar]
28. J. W. Lian, D. C. Yen and Y. T. Wang, “An exploratory study to understand the critical factors affecting the decision to adopt cloud computing in Taiwan hospital,” International Journal of Information Management, vol. 34, no. 1, pp. 1–21, 2014. [Google Scholar]
29. C. Y. Lin and Y. H. Ho, “RFID technology adoption and supply chain performance: An empirical study in china’s logistics industry,” Supply Chain Management: An International Journal, vol. 14, no. 5, pp. 369–378, 2009. [Google Scholar]
30. C. Lim, I. Lin, J. Roan and J. Yeh, “Critical factors influencing hospitals adoption of h17 version 2 standards: An empirical investigation,” Journal of Medical Systems, vol. 36, no. 3, pp. 1183–1192, 2010. [Google Scholar]
31. C. Liu, “Key factors influencing the intention of telecare adoption: An institutional perspective,” Telemedicine and E-Health, vol. 17, no. 4, pp. 288–293, 2011. [Google Scholar]
32. M. Lu, S. Lin and G. Tzeng, “Improving RFID adoption in taiwan’s healthcare industry based on a DEMATEL technique with a hybrid MCDM model,” Decision Support Systems, vol. 56, no. 24, pp. 259–269, 2013. [Google Scholar]
33. D. K. Maduku, M. Mpinganiira and H. Duh, “Understanding mobile marketing adoption intention by south africans: A multi-perspective framework,” International Journal of Information Management, vol. 36, no. 5, pp. 711–723, 2016. [Google Scholar]
34. A. Marques, T. Oliveira, S. Dias and M. Martins, “Medical records system adoption in european hospitals,” The Electronic Journal Information Systems Evaluation, vol. 14, no. 1, pp. 89–99, 2011. [Google Scholar]
35. V. Matta, D. Koonce and A. Jeyaraj, “Initiation, experimentation, implementation of innovations: The case for radio frequency identification systems,” International Journal of Information Management, vol. 32, no. 2, pp. 164–174, 2012. [Google Scholar]
36. V. Maugis, N. Choucri, S. E. Madnick, M. D. Siegel, S. E. Gillett et al., “Global e-readiness–for what? Readiness for e-banking,” Information Technology for Development, vol. 11, no. 4, pp. 313–342, 2005. [Google Scholar]
37. Y. Z. Mehrjerdi, “RFID-enabled healthcare systems: Risk-benefit analysis,” International Journal of Pharmaceutical and Healthcare Marketing, vol. 4, no. 3, pp. 282–300, 2010. [Google Scholar]
38. D. Choi, C. Y. Chung, T. Seyha and J. Young, “Factors affecting organizations resistance to the adoption of blockchain technology in supply networks,” Sustainability, vol. 12, no. 21, pp. 1–37, 2020. [Google Scholar]
39. E. W. Ngai, J. K. Poon, F. F. Suk and C. C. Ng, “Design of an RFID-based healthcare management system using an information system design theory,” Information Systems Frontiers, vol. 11, no. 4, pp. 405–417, 2009. [Google Scholar]
40. M. Nilashi, H. Ahmadi, A. Ahani, R. Rawangard and O. B. Ibrahim, “Determining the importance of hospital information system adoption factors using fuzzy analytic network process (ANP),” Technological Forecasting and Social Change, vol. 111, no. 3, pp. 244–264, 2016. [Google Scholar]
41. S. Paydar and I. Endut, “Key drivers of RFID adoption in Malaysian retail industry: A theoretical model,” in IEEE Int. Conf. on RFID Technologies and Applications, Bahru, Malaysia, pp. 1–6, 2013. [Google Scholar]
42. A. A. AlZubi, “An optimal sensor placement algorithm (O-SPA) for improving tracking precision of human activity in real-world healthcare systems,” Computer Communications, vol. 148, no. 6, pp. 98–105, 2019. [Google Scholar]
43. S. Rahman, L. Yang and S. Waters, “Factors affecting RFID adoption in Chinese manufacturing firms: An investigation using AHP,” in Proc. of the IFAC Conf. on Manufacturing Modelling, Management, and Control, Russia, pp. 1–8, 2013. [Google Scholar]
44. S. Kamble, A. Gunasekaran and H. Arha, “Understanding the blockchain technology adoption in supply chains-indian context,” International Journal of Production Research, vol. 57, no. 7, pp. 2009–2033, 2019. [Google Scholar]
45. P. M. Reyes and P. Jaska, “Is RFID right for your organizations or application,” Management Research News, vol. 30, no. 8, pp. 570–580, 2007. [Google Scholar]
46. P. M. Reyes, S. Li and J. K. Visich, “Accessing antecedents and outcomes of RFID implementation in health care,” International Journal of Production Economics, vol. 136, no. 1, pp. 137–150, 2012. [Google Scholar]
47. P. M. Reyes, S. Li and J. K. Visich, “Determinants of RFID adoption stage and perceived benefits,” European Journal of Operational Research, vol. 254, no. 3, pp. 801–812, 2016. [Google Scholar]
48. E. M. Rogers, “Intention to receive the COVID-19 vaccination in china: Application of the diffusion of innovations theory and the moderating role of openness to experience,” Vaccines 95-Molecular Approaches to the Control of Infectious Diseases, vol. 9, no. 2, pp. 1–15, 2021. [Google Scholar]
49. Y. Bendavid and L. Cassivi, “Bridging the gap between RFID/EPC concepts, technological requirements and supply chain e-business processes,” Journal of Theoretical and Applied Electronic Commerce Research, vol. 5, no. 3, pp. 1–16, 2010. [Google Scholar]
50. A. A. AlZubi, A. Sharma and A. Citurs, “Strategic and institutional perspective in the adoption and early integration of radio frequency identification (RFID),” in Proc. of the 40th Hawaii Int. Conf. on System Sciences, Hawaii, pp. 112–119, 2007. [Google Scholar]
51. J. Zhang, G. Y. Tian, A. J. Marindra, A. I. Sunny and A. B. Zhao, “A review of passive RFID tag antenna-based sensors and systems for structural monitoring applications,” Sensors, vol. 17, no. 2, pp. 1–21, 2017. [Google Scholar]
52. S. A. Sherer, C. D. Meyerhoefer and L. Peng, “Applying institutional theory to the adoption of electronic health records in the US,” Information & Management, vol. 53, no. 5, pp. 23–38, 2016. [Google Scholar]
53. H. Shipton, K. Sanders, C. Atkinson and S. Frenkel, “Sense-giving in health care: The relationship between the HR roles of line managers and employee commitment,” Human Resource Management Journal, vol. 26, no. 1, pp. 29–45, 2016. [Google Scholar]
54. M. Srite and E. Karahanna, “The influence of national culture on the acceptance of information technologies: An empirical study,” MIS Quarterly, vol. 30, no. 3, pp. 679–704, 2006. [Google Scholar]
55. S. R. Velu, A. A. Mamun, T. Kanesan, N. Hayat and S. Gopinathan, “Effect of information system artifacts on organizational resilience: A study among Malaysian SMEs,” Sustainability, vol. 11, no. 11, pp. 1–21, 2019. [Google Scholar]
56. Q. Zhang, L. Wang, H. Wang, X. Zhu and W. Lijun, “Spatio-temporal variation of groundwater quality and source apportionment using multivariate statistical techniques for the hutuo river alluvial-pluvial fan, China,” International Journal of Environmental Research and Public Health, vol. 17, no. 3, pp. 1–17, 2020. [Google Scholar]
57. S. L. Ting, S. K. Kwok, A. H. Tsang and W. B. Lee, “Critical elements and lessons learnt from the implementation of an RFID-enabled healthcare management systems in a medical organization,” Journal of Medical Systems, vol. 35, no. 3, pp. 657–669, 2011. [Google Scholar]
58. Y. Zhang, U. Khan, S. Lee and M. Salik, “The influence of management innovation and technological innovation on organization performance. A mediating role of sustainability,” Sustainability, vol. 11, no. 2, pp. 1–21, 2019. [Google Scholar]
59. M. Tsai, W. Lee and H. Wu, “Determinants of RFID adoption intention: Evidence from Taiwanese retail chains,” Information & Management, vol. 47, no. 5, pp. 255–261, 2010. [Google Scholar]
60. V. R. Togt, P. J. Bakker and M. W. Jaspers, “A framework for performance and data quality assessment of radio frequency identification (RFID) systems in healthcare settings,” Journal of Biomedical Informatics, vol. 44, no. 2, pp. 372–383, 2011. [Google Scholar]
61. S. Ajami and A. Rajabzabeh, “Radio frequency identification (RFID) technology and patient safety,” Journal of Research Medical Sciences, vol. 18, no. 9, pp. 809–813, 2013. [Google Scholar]
62. V. Venkatesh, M. Morris, G. Davis and F. Davis, “User acceptance of information technology: Toward a unified view,” MIS Quarterly, vol. 27, no. 3, pp. 425–478, 2003. [Google Scholar]
63. V. Venkatesh, T. A. Sykes and X. Zhang, “Just what the doctor ordered: A revised UTAUT for EMR system adoption and use by doctors,” in IEEE 44th Hawaii Int. Conf. on System Sciences, Kauai, USA, pp. 1–7, 2011. [Google Scholar]
64. N. Wrzosek, A. Zimmermann and L. Balwicki, “Doctors’ perceptions of e-prescribing upon its mandatory adoption in Poland, using the unified theory of acceptance and use of technology method,” Healthcare, vol. 8, no. 4, pp. 1–16, 2020. [Google Scholar]
65. D. Viehland and A. Wong, “The future of radio frequency identification,” Journal of Theoretical and Applied Electronic Commerce Research, vol. 2, no. 2, pp. 74–82, 2007. [Google Scholar]
66. G. Khalil, R. Doss and M. Chowdhury, “A comparison survey on RFID based anti-counterfeiting systems,” Journal of Sensor and Actuator Networks, vol. 8, no. 3, pp. 1–16, 2019. [Google Scholar]
67. S. Wamba, A. Anand and L. Carter, “A literature review of RFID-enabled healthcare applications and issues,” International Journal of Information Management, vol. 33, no. 5, pp. 875–891, 2013. [Google Scholar]
68. Y. M. Wang, Y. S. Wang and Y. F. Yang, “Understanding the determinants of RFID adoption in the manufacturing industry,” Technological Forecasting and Social Change, vol. 77, no. 5, pp. 803–815, 2010. [Google Scholar]
69. I. V. Weerd, I. S. Mangula and S. Brinkkemper, “Adoption of software as a service in indonesia: Examining the influence of organizational factors,” Information & Management, vol. 53, no. 7, pp. 915–928, 2016. [Google Scholar]
70. T. T. Wei, G. Mathandan, A. Y. Chong, K. Ooj and S. Arumugam, “What drives Malaysian m-commerce adoption? An empirical analysis,” Industrial Management & Data Systems, vol. 109, no. 3, pp. 370–388, 2009. [Google Scholar]
71. X. Wu and C. Subramanian, “New understanding of RFID adoption and infusion in retail supply chain,” in Proc. of the Int. Conf. on System Sciences, Hawaii, pp. 1–10, 2009. [Google Scholar]
72. W. Yao, C. H. Chu and Z. Li, “The adoption and implementation of RFID technologies in healthcare: A literature review,” Journal of Medical Systems, vol. 36, no. 6, pp. 3507–3525, 2012. [Google Scholar]
73. H. J. Yazici, “An exploratory analysis of hospital perspectives on real time information requirements and perceived benefits of RFID technology for future adoption,” International Journal of Information Management, vol. 34, no. 5, pp. 603–621, 2014. [Google Scholar]
74. W. D. Yu, P. Ray and T. Motoc, “WISH: A wireless mobile multimedia information system in healthcare using RFID,” Telemedicine and E-Health, vol. 14, no. 4, pp. 362–370, 2008. [Google Scholar]
75. M. M. Yusof, J. Kuljis, A. Papazafeiropoulou and L. K. Stergioulas, “An evaluation framework for health information systems: Human, organization and technology-fit factors (HOT-fit),” International Journal of Medical Informatics, vol. 77, no. 6, pp. 386–398, 2008. [Google Scholar]
76. W. Zhou and S. Piramuthu, “Framework, strategy and evaluation of health care processes with RFID,” Decision Support Systems, vol. 50, no. 1, pp. 222–233, 2010. [Google Scholar]
77. H. Zhu, T. Hummel, J. C. Clemens, D. Berdnik, S. L. Zipursky et al., “Dendritic patterning by dscam and synaptic partner matching in the dropsophila antenna lobe,” Nature Neuroscience, vol. 9, no. 3, pp. 349–355, 2006. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |