DOI:10.32604/cmc.2022.026660
| Computers, Materials & Continua DOI:10.32604/cmc.2022.026660 | 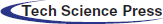 |
| Article |
Early Rehabilitation After Craniosynostosis Surgery
1Department of Neurosurgery, Children's Hospital of Nanjing Medical University, Nanjing, 210008, China
2Department of Surgery, Children's Hospital of Nanjing Medical University, Nanjing, 210008, China
3Quality Management Office, Children's Hospital of Nanjing Medical University, Nanjing, 210008, China
4International Business Machines Corporation (IBM), NY, 10504, USA
5Department of Rehabilitation Medicine, Children's Hospital of Nanjing Medical University, Nanjing, 210008, China
*Corresponding Author: Yiming Liu. Email: liuyimingetyy@163.com
Received: 31 December 2021; Accepted: 22 February 2022
Abstract: Craniosynostosis is a common congenital craniofacial deformity caused by premature ossification and closure of one or more cranial sutures. Craniosynostosis will not only affect the normal development of the skull, but also may cause a variety of complications, damage the nervous system, and cause long-term effects on the development of physical and mental health. Therefore, it is particularly important to provide new ideas for clinical treatment by studying the rehabilitation methods of craniosynostosis, and to improve the cure rate. To this end, this paper studies the early rehabilitation methods after craniosynostosis surgery and designs a comprehensive early rehabilitation process and corresponding comprehensive early rehabilitation measures after surgery. The comparative data also shows that after comprehensive early rehabilitation nursing measures, the duration of the postoperative swelling of sick children was reduced and the degree was significantly reduced, which alleviated the discomfort of sick children; and the time of sick children spent in ICU treatment and monitoring was reduced, and the separation time between sick children and their parents was shorten, is of great significance to the postoperative rehabilitation of craniosynostosis. In addition, the total cost of hospitalization was reduced accordingly, which greatly increased the satisfaction of patients.
Keywords: Craniosynostosis; early rehabilitation; desirability function
Craniosynostosis, also known as cranial stenosis, refers to the premature ossification and closure of one or more cranial sutures in pregnancy or infancy, followed by abnormal diseases such as craniofacial deformities. The total incidence of craniosynostosis is 1/2500-4000, and there will be one sick child in every 4000 sick children [1].
According to the different closure of cranial sutures, craniosynostosis can be divided into sagittal craniosynostosis (60%), coronal craniosynostosis (23%), frontal craniosynostosis (15%), herringbone craniosynostosis (2%) and complex craniosynostosis with multiple closure of cranial sutures [2]. In addition, according to clinical manifestations, craniosynostosis can be divided into syndromic craniosyndromes, such as Apert, Crouzon, or Saethre-Chotzen syndrome, and more common non-syndromic craniosyndromes, such as scaphocephaly (sagittal craniosynostosis), anterior plagiocephaly (coronal craniosynostosis), posterior plagiocephaly (unilateral herringbone craniosynostosis), trigonocephaly (frontal craniosynostosis), brachycephaly (bilateral coronal craniosynostosis) [3]. In addition to skull deformities, the syndromic craniosynostosis also has deformities in other parts of the body, such as complex syndactyly of Apert syndrome, and special facial deformities of Crouzon and Saethre-Chotzen syndrome [4].
Craniosynostosis not only causes deformity of skull growth, but also causes complications such as intracranial hypertension, hydrocephalus, and Chiari deformity, but also affects the development of the nervous system of such sick children and causes neuropathological damage such as cognitive dysfunction [5]. It should be treated as soon as possible, and early rehabilitation training methods should be adopted to maximize the recovery or improvement of patient's function and prevent complications.
Craniosynostosis is manifested as cranial deformity. Multiple cranial sutures often have complications, including hydrocephalus, limited brain development, syndactyly, limbs or spine joint ankylosis, respiratory tract obstruction, vision and/or hearing impairment, etc. In order to effectively guide the clinical treatment scheme, craniosynostosis is divided into non-syndromic craniosyndrosis and syndromic craniosynostosis according to the severity of the skull deformity and the disease manifestations of other organs. Non-syndromic craniosynostosis is a skull deformity caused by the premature fusion or absence of 1 to 2 cranial sutures and its treatment is mainly based on morphological improvement. Syndromic craniosynostosis is due to changes in intracranial pressure and obvious limitation of brain development, the expansion of cranial cavity through frontal orbital anterior displacement should be considered first to improve the prognosis [6–8]. The classification and manifestation of common non-syndromic craniosynostosis are shown in Tab. 1, and the classification and manifestation of common syndromic craniosynostosis are shown in Tab. 2.


Postoperative complications
The surgery of craniosynostosis is more complicated, with long surgery time and great trauma [9]. The surgical complications are quite serious. At present, the main complications are: (1) Postoperative cerebrospinal fluid leakage caused by dura mater injury (usually rhinorrhea). The mild ones can heal by themselves, while the severe ones need to be repaired by craniotomy. (2) Epidural hematoma. (3) Infection. (4) Vision and eye movement dysfunction: blindness is optic nerve injury, and oculomotor nerve injury can cause strabismus. (5) Death: The case fatality rate is about 1% to 2.5%, mainly caused by epidural hematoma, acute brain edema, secondary brain edema and meningitis.
Neurophysiological theory believes that after the central nervous system is injured, the central nervous system has the ability to reorganize or be plastic in structure and function, and some neurons can be regenerated when conditions are suitable [10]. Therefore, rehabilitation therapy can influence output by inputting normal movement mode, promote the formation of normal functional mode, and achieve the purpose of maximizing the recovery of motor function.
Early rehabilitation intervention therapy can carry out corresponding rehabilitation training as long as sick children's condition permits. Early rehabilitation can not only lead to the completion of the pattern integration of functional areas of cerebral cortex, but coordination is also trained during exercise. The movement of muscles and joints, in turn, provides a large amount of shallow and deep impulse input to the central nervous system, which plays a role in activation [11–13]. Moreover, it can effectively prevent complications and make sick children's limb movement as coordinated and natural as possible.
In the past, rehabilitation was considered to be suitable for rehabilitation training only 48 h after the patient was conscious, the vital signs were stable and the nervous system symptoms no longer progress [14]. However, foreign rehabilitation experts advocated early rehabilitation in 2006, they believed that rehabilitation nursing can promote the reorganization and compensation of patients’ brain function, and the earlier the rehabilitation, the more beneficial to the rehabilitation of patients [15]. At present, the nursing staff in the intensive care unit of our hospital have a high-level technical basis for rescuing and nursing, but they generally have no knowledge of rehabilitation nursing. In addition to completing basic nursing for sick children with cerebral palsy, our nurses in the rehabilitation department can also do a good job in rehabilitation nursing in spinal cord injury, orthopedics and ICU convalescent patients, and effectively implement the characteristics of high-quality nursing services. The benefits of early rehabilitation of some diseases in sick children are analyzed as follows:
(1) Impact on early rehabilitation of sick neonates
The study found that the age of “0–2” is the period with the fastest brain development and the strongest compensatory ability. Therefore, early intervention and early treatment of high-risk newborns is the only way to ensure that sick children's potential abilities can be maximized, and it has twice the result with half the effort [16–20].
(2) Impact on early rehabilitation of patients with spinal cord injury
The meaning of “early” in early rehabilitation of spinal cord injury refers to: under the premise of stable condition, starting from the day of injury, starting from admission to the hospital, starting immediately after surgery, starting from ICU. As long as the condition is stable and there is no other combined injury, rehabilitation intervention should be involved. For patients with incomplete SCI, early rehabilitation is conducive to the recovery of nerves and ADL ability. Patients with complete SCI can also recover their neurological function to varying degrees through early rehabilitation and can effectively prevent the occurrence of complications [21].
(3) Impact on early rehabilitation after heart disease surgery
Early postoperative rehabilitation can better improve the quality of life of patients, and all kinds of pain, sleep, appetite, self-care ability and exercise condition of patients have been significantly improved [22].
(4) Impact on early rehabilitation of sick children with brain surgery and orthopedics
Early postoperative rehabilitation can better improve the Barthel index. The correct placement of good posture can prevent or reduce the occurrence of spasms and deformities, maintain the functional state of the trunk and limbs, and reduce the occurrence of complications and secondary damage [23].
Rehabilitation major is not a major that only the rehabilitation department can engage in. Rehabilitation can be applied to many clinical departments. While doing a good job in specialized basic nursing for sick children, our nursing staff can provide sick children with professional nursing technology for early rehabilitation and shape the unique brand charm of our nursing staff to achieve the satisfaction of parents, hospitals and society [24,25].
3 Early Rehabilitation After Craniosynostosis Surgery
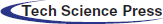
In recent years, people have paid more and more attention to craniosynostosis. The number of patients admitted to our department has increased year by year. Take 698 cases of craniosynostosis admitted to our department from 2018 to 2020 as an example, of which 463 were boys and 235 were girls, as shown in Fig. 1.
Figure 1: Number of sick children with craniosynostosis in recent three years
184 people were admitted in 2018, 251 people were admitted in 2019, and 263 people were admitted in 2020. The number of boys was significantly higher than that of girls. Among them, the incidence of sagittal craniosynostosis in sick boys was about four times that in sick girls.
After admission, doctors, nurses and rehabilitation therapists evaluated sick children with craniosynostosis, formulated rehabilitation plans, and formed early rehabilitation nursing and guidance in all aspects from admission to post-surgery.
3.1 Early Rehabilitation Before Surgery
Early rehabilitation measures that can be taken before surgery are as follows.
(1) Sick children are young and have poor cough and sputum reflex. They do not cough up sputum, and anesthesia intubation causes hoarseness. Guide parents to pat the back and expel phlegm for their children to help discharge respiratory secretions and prevent postoperative pneumonia occurred during bed rest.
(2) Guide parents to perform limb massage and passive exercises for sick children.
(3) Teach methods, importance and matters of lying position management after surgery.
(4) Guide sick children to eat in bed.
3.2 Early Rehabilitation After Surgery
Early rehabilitation measures that can be taken after surgery are as follows.
3.2.1 Maintain a Good Limb Posture
① Supine position: Turn over at least once every 2 h, place a clean low soft pillow under the head, and prepare a towel to make a pillow ring.
Premature closure of sagittal suture: Keep the supine position for more than 20 h/day, use the head ring when lying on the back, remove the head ring when turning over and lying on the side, keep the tip of the nose at 12 o'clock when lying on the back, and less than 2 o'clock and 10 o'clock when lying on the side, use foam dressing to prevent pressure ulcers where the head is under pressure [26].
Unilateral coronal suture: The contralateral supine position alternates with the horizontal position, no more than 2 h to turn over. Awake after general anesthesia can raise the head of the bed 30 degrees to reduce brain edema, observe the degree of swelling of the head and face, and increase the frequency of turning over if necessary.
② Micro-turn-over: Under the concept of micro-turn-over, actively prevent stress injury in sick children who are absolutely bedridden in neurosurgery.
Change limb posture at a low angle: Intermittently help sick children to lie on the side at 15° or 30°. Sick children are comfortable and easy to tolerate. The body posture slightly changed by moving the limbs [27]. The nurse helps sick children to passively move once every 30 min, so as to move the buttocks and coccyx by changing the position of the lower limbs, and to replace the stress points alternately to reduce the possibility of stress injury. Within the range of acceptance of sick children, sick children can cooperate [28].
Shorten the interval between turning over: Change the concept of turning over every two hours, and appropriately increase the number of body posture changes in sick children. After the condition is stable, sick children can be lifted off the bed for 30 s to 2 min every 1–2 h [29].
③ Put in a good posture as early as possible to prevent or reduce spasms, and prevent complications that will seriously affect the rehabilitation process in the future, such as swelling, muscle shortening, and limited joint mobility, so as to improve functions as soon as possible and prevent complications, including the use of quilt frame support to prevent the quilt from being too heavy and pressing the hemiplegic foot to cause foot drop [30].
① After sick children's postoperative condition is stable, sick children can be massaged on the limbs. Muscles can be lifted up to relax with soothing massage, which can promote the blood circulation of the limbs, increase their comfort and sense of security, promote the relationship between parents and sick children, and improve the awakening ability of sick children.
② Observe whether the eyelids can be closed or not, children with eye swelling to eyelid ectropion can be covered with Vaseline gauze, and the latter complies with the doctor's instructions to use eye ointment, eye drops and so on.
After sick children's postoperative condition is stable, passive movement of the limb joint can be carried out, which can also promote the blood circulation of the limbs, promote nerve reflex, maintain normal joint mobility, relieve muscle spasm, stretch shortened muscles and tendons, and promote rehabilitation of sick children after surgery [31]. Rehabilitation training for functional exercises of limbs and prevention of disuse syndrome can be carried out after sick children's postoperative condition is stable, from easy to difficult, from small to large, time from short to long, intensity from low to high, from passive exercise to autonomous exercise, step by step [32].
① It mainly refers to the extension, flexion, adduction, internal rotation, external rotation and extension of the finger (toe) joints of the limb joints.
② Move the joints of sick children, from small joints to large joints, from the proximal end to the distal end.
③ The amplitude should be gradual, avoid excessive force, so as not to cause damage to patient's muscles and surrounding soft tissues. Exercise at the same time to communicate with patients to avoid pain to patients, the movements are gentle, 10–15 times per movement, and the time should not be too long.
④ Induce active movement of upper and lower limbs. Sick children's condition is in the recovery period, and the muscle strength is gradually restored, so the correct body position and limb function position should be maintained.
⑤ Balance and coordination ability training. When sick children's postoperative condition is stable, from lying to sitting, the head of the bed is raised and the angle is gradually increased, and at the same time, the time is prolonged, and the number of times is increased. After sitting up, train the patient to droop his legs and practice standing by the bed. The upper limb can do finger climbing wall movement to exercise fine movements.
⑥ Daily living ability training. As educators and managers, nurses can make plans for children who are older and cooperative to resume self-care activities. They can eat, wash, wear and undress, pick up soybeans, and practice grip strength with a gripper.
⑦ During the activity, pay attention to observe sick children's complexion, breathing, etc., once there is a sharp fluctuation, stop immediately and report to the doctor.
① Maintaining a semi-recumbent position above 30° under a stable state is a simple and effective measure to prevent lung infections.
② Scientific and standardized airway management. Patients with cough and hoarse voice should be given atomization inhalation, pat the back of sick children, turn over frequently, and instruct parents to give small amounts of water for sick children several times. For those with excessive cough and sputum, suck sputum as needed, when necessary, shallow sputum suction is better than deep sputum suction.
③ Postural drainage : Sick children with stable disease can turn over and change their posture regularly, turning over slightly along the axis.
④ Help cough when necessary: Place the palm under patient's xiphoid process and use an inward and upward movement to pressurize patient's abdomen to help cough when the patient coughs.
⑤ Increase chest wall movement: Older sick children who can cooperate can maintain or improve the range of chest wall movement through deep breathing exercises, cough assistance, passive manual traction and joint exercises.
⑥ Breathing training: Older sick children who can cooperate can be given breathing exercises, starting with slow, relaxed abdominal breathing and gradually transitioning to resistance training for the diaphragm.
⑦ Chest physiotherapy: Vibrate and tap patient's chest and back with a certain technique and move the secretions from the small bronchus to the large bronchus through vibration and tapping, and then be coughed out of the body.
① Play gentle music, favorite cartoons, and storytelling for sick children to distract their attention, relieve their discomfort and pain, increase their sense of security and promote their psychological recovery.
② Older and cooperative sick children carry out daily smile, frown, bulging gills, tongue extension training and bilateral facial massage, and carry out cold stimulation of pharynx, empty swallowing, breath-holding, and vocal exercises twice a day, 15 min each time.
③ Evaluation of swallowing function and classification of swallowing dysfunction: Japanese drinking water test (30 ml warm water in a glass, instruct patients to swallow, observe time and cough), promote the recovery of dietary function, make a normal diet as soon as possible, and increase dietary nutrition , and help postoperative rehabilitation.
④ Young children gradually increase the ability to grasp toys and play games; older children can gradually increase their ability to wash hands, brush teeth and wash faces according to their bearing capacity to restore their living ability.
3.3 Evaluation of Early Rehabilitation Effect Based on Desirability Function Method
Desirability Function (DF) can be defined as: the mathematical relationship between patients and medical services. The desirability function method transforms each response value
Among then,
Hope small individual desirability function:
Hope large individual desirability function:
Considering the relative importance between the responses, construct the overall desirability function D as follows.
Choose the hope large individual desirability function in the desirability function method to calculate the overall desirability of each group of people with the treatment plan under the preference difference [33]. The family members of sick children and medical staff have different preference coefficients for the attributes of different treatment plans, and the utility function for each treatment plan is as follows.
Among them,
In order to unify the units of each attribute, the level values of different attributes are transformed into dimensionless data on [−1, 1]. Use the following formula to convert the preference coefficient into a relative preference coefficient under the same measurement range.
4 Effect of Early Rehabilitation
Through the implementation and guidance of early rehabilitation and nursing measures, parents’ recognition of ward doctors and nursing staff was significantly improved, the satisfaction return visits rate has increased from 81% in 2018 to 99% in 2020, and the average monthly third-party satisfaction score has increased from 96.03 points to 98.16 points.
Data of craniosynostosis from 2018 to 2020 is shown in Tab. 3.
The duration of the 2-degree peak of skin swelling after craniosynostosis surgery is shown in Fig. 2. The median duration of postoperative skin swelling (disappearance of streaks) in sick children with craniosynostosis was 92 h in 2018, 85 h in 2019, and 55.5 h in 2020. After comprehensive rehabilitation nursing, the duration of skin swelling has been reduced from 80–100 h in 2018 to 48–60 h in 2020.

The number of cases of skin swelling after craniosynostosis surgery and the appearance of tension blisters and swelling that affect the delayed suture removal of the incision is shown in Fig. 3. The number of cases of postoperative tension blisters in sick children with craniosynostosis was 13 cases in 2018, 6 cases in 2019 and 2 cases in 2020. The number of cases of delayed suture removal due to skin swelling to incision was 9 cases in 2018, 5 cases in 2019 and 1 case in 2020. Through comprehensive rehabilitation and nursing measures, the number of sick children with tension blisters after surgery has dropped significantly, from 13 to 2 cases. The number of sick children with delayed suture removal due to skin swelling after surgery has decreased from 9 to 1 case.
Figure 2: The peak of skin swelling after craniosynostosis was 2 degrees
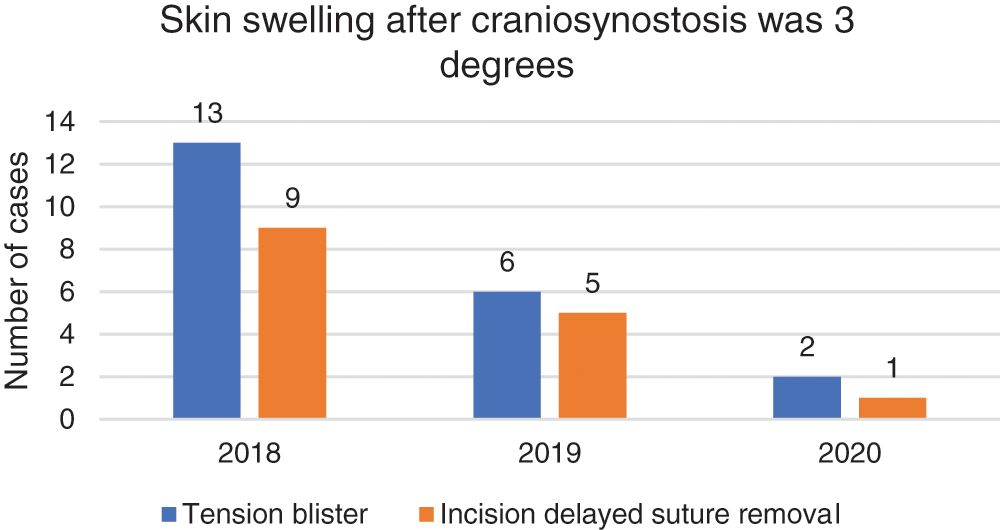
Figure 3: Skin swelling after craniosynostosis was 3 degrees
The time for sick children with craniosynostosis to be admitted to the intensive care unit after surgery is shown in Fig. 4. The median time of postoperative treatment in ICU for sick children with craniosynostosis was 60.3, 49.2, and 19.3 h, respectively. In which, 48–72 h in 2018, 40–60 h in 2019 and 16–24 h in 2020. The time for sick children to be treated and monitored in intensive care unit after surgery was significantly reduced, and the separation time between sick children and parents was reduced.
The hospitalization cost of sick children with craniosynostosis is shown in Fig. 5. The median hospitalization cost of sick children with craniosynthesis was 105000 yuan in 2018, 97000 yuan in 2019, and 69000 yuan in 2020. The average total cost was 83600 yuan in 2018, 80900 yuan in 2019, and 73500 yuan in 2020. On the basis of ensuring the safety of sick children, through comprehensive rehabilitation and nursing measures, the total cost of hospitalization for sick children has reduced.
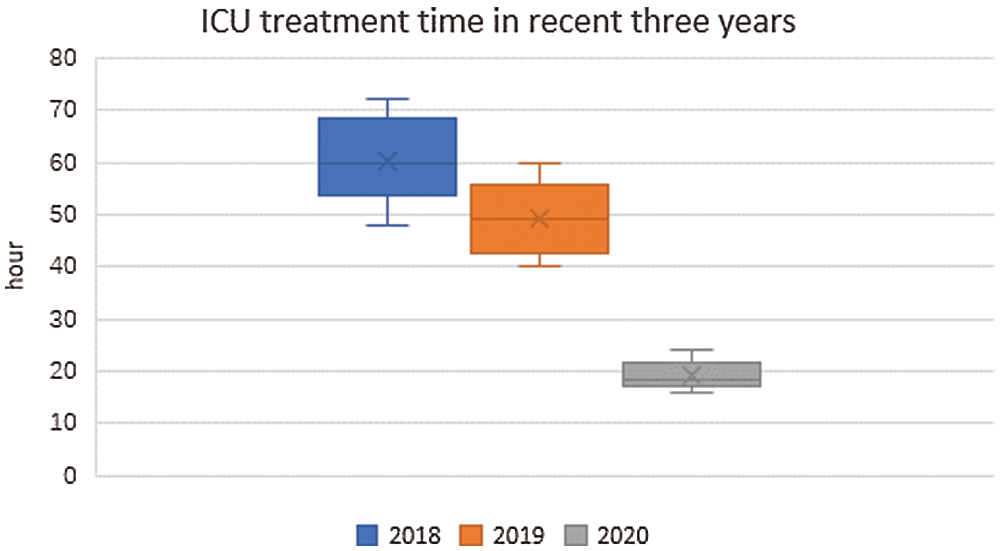
Figure 4: ICU treatment time in recent three years
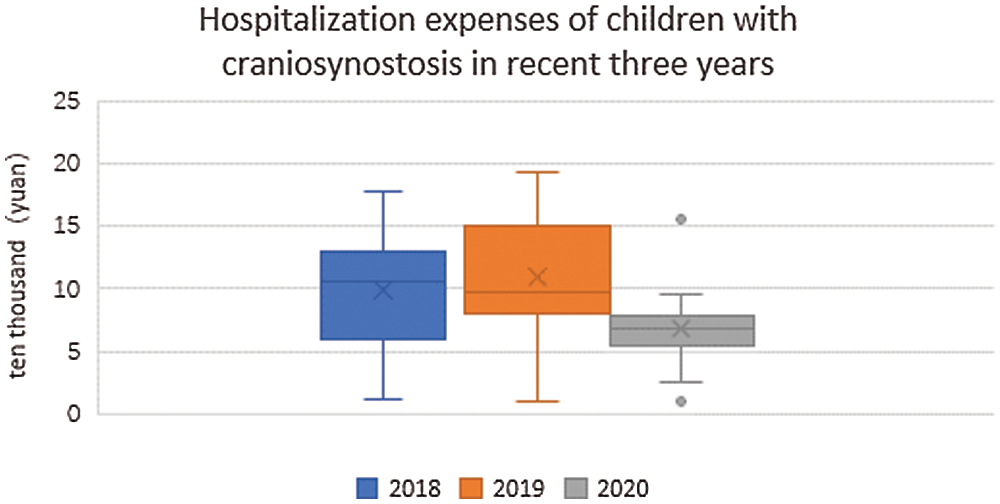
Figure 5: Cost in hospitalization
In summary, today, with the continuous progress of medical technology, sick children and their parents have an increasing demand for humanistic care. Providing sick children with safe and efficient rehabilitation nursing and guidance plays a good role in promoting their rehabilitation. After rehabilitation and nursing operations, the comfort of sick children was improved, and the time of each phase of skin swelling after surgery was reduced. The separation time between sick children and their parents has been shortened, which has relieved the separation anxiety between them. The medical expenses of sick children during hospitalization have been reduced, and the satisfaction of parents to the department has also been improved.
Craniosynostosis leads to complications and neuropathological damage. In severe cases, there may be intelligence, language and psychological abnormalities in adults. This paper focuses on comprehensive early rehabilitation measures after craniosynostosis surgery. Various early rehabilitation measures such as maintaining good limb posture, limb massage and lung rehabilitation have reduced the duration and degree of postoperative swelling in sick children and relieved the discomfort of sick children. In addition, the time spent in ICU treatment and monitoring of sick children was reduced, which shortened the separation time between sick children and their parents. Moreover, the total cost of hospitalization was reduced accordingly, which greatly increased the satisfaction of patients.
Funding Statement: This work is supported by science and technology development fund of Nanjing Medical University (Grand No. NMUB2018095). Yiming Liu received the grant and the URLs to sponsors’ websites is https://www.njmu.edu.cn.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. C. Caron, B. Pluijmers, K. Joosten, I. Mathijssen, M. Van Der Schroeff et al., “Obstructive sleep apnoea in craniofacial microsomia: A systematic review,” International Journal of Oral and Maxillofacial Surgery, vol. 44, no. 5, pp. 592–598, 2015. [Google Scholar]
2. P. D. Ketwaroo, C. D. Robson and J. A. Estroff, “Prenatal imaging of craniosynostosis syndromes,” In Seminars in Ultrasound, CT and MRI, vol. 36, no. 6, pp. 453–464, 2015. [Google Scholar]
3. W. Xu, J. Li, P. A. Gerety, J. A. Taylor and S. P. Bartlett, “Impact of front-orbital advancement on frontal sinus volume, morphology, and disease in nonsyndromic craniosynostosis,” Plastic and Reconstructive Surgery, vol. 138, no. 5, pp. 1051–1059, 2016. [Google Scholar]
4. R. H. Han, D. C. Nguyen, B. S. Bruck, G. B. Skolnick, C. K. Yarbrough et al., “Characterization of complications associated with open and endoscopic craniosynostosis surgery at a single institution,” Journal of Neurosurgery: Pediatrics, vol. 17, no. 3, pp. 361–370, 2016. [Google Scholar]
5. Y. J. Ren, Y. Leng, J. Qi, K. S. Pradip, J. Wang et al., “Multiple cloud storage mechanism based on blockchain in smart homes,” Future Generation Computer Systems, vol. 115, pp. 304–313, 2021. [Google Scholar]
6. C. P. Ge, W. Susilo, Z. Liu, J. Y. Xia, L. M. Fang et al., “Secure keyword search and data sharing mechanism for cloud computing,” IEEE Transactions on Dependable and Secure Computing, vol. 18, no. 6, pp. 2787–2800, 2021. [Google Scholar]
7. J. Wang, H. Han, H. Li, S. He, P. K. Sharma et al., “Multiple strategies differential privacy on sparse tensor factorization for network traffic analysis in 5G,” IEEE Transactions on Industrial Informatics, vol. 18, no. 3, pp. 1939–1948, 2022. [Google Scholar]
8. T. Li, Q. Qian, Y. J. Ren, Y. Z. Ren and J. Y. Xia, “Privacy-preserving recommendation based on kernel method in cloud computing,” Computers, Materials & Continua, vol. 66, no. 1, pp. 779–791, 2021. [Google Scholar]
9. R. Festa, F. Tosi, A. Pusateri, S. Mensi, R. Garra et al., “The scalp block for postoperative pain control in craniosynostosis surgery: A case control study,” Child's Nervous System, vol. 36, pp. 3063–3070, 2020. [Google Scholar]
10. J. Chen, K. Li, K. Bilal, K. Li, S. Y. Philip et al., “A bi-layered parallel training architecture for large-scale convolutional neural networks,” IEEE Transactions on Parallel and Distributed Systems, vol. 30, no. 5, pp. 965–976, 2018. [Google Scholar]
11. Y. J. Ren, F. J. Zhu, S. P. Kumar, T. Wang, J. Wang et al., “Data query mechanism based on hash computing power of blockchain in internet of things,” Sensors, vol. 20, no. 1, pp. 1–22, 2020. [Google Scholar]
12. C. Chen, K. Li, S. G. Teo, X. Zou, K. Li et al., “Citywide traffic flow prediction based on multiple gated spatio-temporal convolutional neural networks,” ACM Transactions on Knowledge Discovery from Data (TKDD), vol. 14, no. 4, pp. 1–23, 2020. [Google Scholar]
13. M. Duan, K. Li, X. Liao and K. Li, “A parallel multiclassification algorithm for big data using an extreme learning machine,” IEEE Transactions on Neural Networks and Learning Systems, vol. 29, no. 6, pp. 2337–2351, 2017. [Google Scholar]
14. C. P. Ge, Z. Liu, J. Y. Xia and L. M. Fang, “Revocable identity-based broadcast proxy re-encryption for data sharing in clouds,” IEEE Transactions on Dependable and Secure Computing, vol. 18, no. 3, pp. 1214–1226, 2021. [Google Scholar]
15. Y. J. Ren, Y. Leng, Y. P. Cheng and J. Wang, “Secure data storage based on blockchain and coding in edge computing,” Mathematical Biosciences and Engineering, vol. 16, no. 4, pp. 1874–1892, 2019. [Google Scholar]
16. L. M. Fang, M. H. Li, Z. Liu, C. T. Lin, S. L. Ji et al., “A secure and authenticated mobile payment protocol against off-site attack strategy,” IEEE Transactions on Dependable and Secure Computing, vol. 21, no. 2, pp. 1–12, 2021. [Google Scholar]
17. X. R. Zhang, W. F. Zhang, W. Sun, X. M. Sun and S. K. Jha, “A robust 3-D medical watermarking based on wavelet transform for data protection,” Computer Systems Science & Engineering, vol. 41, no. 3, pp. 1043–1056, 2022. [Google Scholar]
18. Y. J. Ren, J. Qi, Y. P. Liu, J. Wang and G. Kim, “Integrity verification mechanism of sensor data based on bilinear map accumulator,” ACM Transactions on Internet Technology, vol. 21, no. 1, pp. 1–20, 2021. [Google Scholar]
19. Y. J. Ren, F. Zhu, J. Wang, P. Sharma and U. Ghosh, “Novel vote scheme for decision-making feedback based on blockchain in internet of vehicles,” IEEE Transactions on Intelligent Transportation Systems, vol. 21, no. 8, pp. 1–10, 2021. [Google Scholar]
20. J. Tong, J. K. Emelin, R. Wong, H. S. Meltzer and S. R. Cohen, “Subgaleal drain placement improves surgical outcomes after primary cranioplasty in craniosynostosis patients,” Journal of Craniofacial Surgery, vol. 26, no. 6, pp. 1963–1966, 2015. [Google Scholar]
21. C. Vaughan, B. Attlmayr, L. Dalton, N. Upile, C. Xie et al., “Assessment of smell function in syndromic craniosynostosis patients,” Journal of Craniofacial Surgery, vol. 27, no. 6, pp. 1598–1599, 2016. [Google Scholar]
22. N. K. Addo, S. Javadpour, J. Kandasamy, P. Sillifant, P. May et al., “Central sleep apnea and associated chiari malformation in children with syndromic craniosynostosis: Treatment and outcome data from a supraregional national craniofacial center,” Journal of Neurosurgery: Pediatrics, vol. 11, no. 3, pp. 296–301, 2013. [Google Scholar]
23. C. P. Ge, W. Susilo, J. Baek, Z. Liu, J. Y. Xia et al., “Revocable attribute-based encryption with data integrity in clouds,” IEEE Transactions on Dependable and Secure Computing, vol. 99, pp. 1, 2021. [Google Scholar]
24. J. Wang, C. Y. Jin, Q. Tang, N. X. Xiong and G. Srivastava, “Intelligent ubiquitous network accessibility for wireless-powered MEC in UAV-assisted B5G,” IEEE Transactions on Network Science and Engineering, vol. 8, no. 4, pp. 2801–2813, 2021. [Google Scholar]
25. Y. J. Ren, J. Qi, Y. P. Cheng, J. Wang and O. Alfarraj, “Digital continuity guarantee approach of electronic record based on data quality theory,” Computers, Materials & Continua, vol. 63, no. 3, pp. 1471–1483, 2020. [Google Scholar]
26. T. Li, W. D. Xu, L. N. Wang, N. P. Li, Y. J. Ren et al., “An integrated artificial neural network-based precipitation revision model,” KSII Transactions on Internet and Information Systems, vol. 15, no. 5, pp. 1690–1707, 2021. [Google Scholar]
27. X. R. Zhang, X. Sun, X. M. Sun, W. Sun and S. K. Jha, “Robust reversible audio watermarking scheme for telemedicine and privacy protection,” Computers, Materials & Continua, vol. 71, no. 2, pp. 3035–3050, 2022. [Google Scholar]
28. D. Apostolopoulou, O. S. Kaxira, A. Hatzaki, K. P. Panagopoulos, K. Alexandrou et al., “Genetic analysis of syndromic and nonsyndromic patients with craniosynostosis identifies novel mutations in the twist1 and efnb1 genes,” The Cleft Palate-Craniofacial Journal, vol. 55, no. 8, pp. 1092–1102, 2018. [Google Scholar]
29. Y. J. Ren, K. Zhu, Y. Q. Gao, J. Y. Xia, S. Zhou et al., “Long-term preservation of electronic record based on digital continuity in smart cities,” Computers, Materials & Continua, vol. 66, no. 3, pp. 3271–3287, 2021. [Google Scholar]
30. X. R. Zhang, X. Sun, W. Sun, T. Xu and P. P. Wang, “Deformation expression of soft tissue based on BP neural network,” Intelligent Automation & Soft Computing, vol. 32, no. 2, pp. 1041–1053, 2022. [Google Scholar]
31. C. P. Ge, W. Susilo, J. Baek, Z. Liu, J. Y. Xia et al., “A verifiable and fair attribute-based proxy re-encryption scheme for data sharing in clouds,” IEEE Transactions on Dependable and Secure Computing, vol. 21, no. 7, pp. 1–12, 2021. [Google Scholar]
32. N. Mitsukawa, T. Morishita, A. Saiga, N. Omori, Y. Kubota et al., “A case of crouzon syndrome treated by simultaneous bimaxillary distraction,” Journal of Plastic, Reconstructive & Aesthetic Surgery, vol. 67, no. 1, pp. 124–125, 2014. [Google Scholar]
33. L. M. Morris, “Nonsyndromic craniosynostosis and deformational head shape disorders,” Facial Plastic Surgery Clinics, vol. 24, no. 4, pp. 517–530, 2016. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |