
 | Oncologie |  |
DOI: 10.32604/Oncologie.2021.016002
ARTICLE
Awareness of Human Papilloma Virus and Its Association with Cervical Cancer among Female University Students: A Study from United Arab Emirates
1School of Life Sciences, Manipal Academy of Higher Education, Dubai, 345050, United Arab Emirates
2Department of Medical Biotechnology, College of Applied Medical Sciences, Qassim University, Buraydah, Saudi Arabia
3Research and Scientific Studies Unit, College of Nursing and Allied Health Sciences, Jazan University, Jazan, Saudi Arabia
*Corresponding Author: Arif Hussain. Email: dr.arifhussain@yahoo.co.in
Received: 30 January 2021; Accepted: 07 April 2021
Abstract: Cervical cancer is the neoplasm of the uterine cervix in women, which is highly preventable. With the advent of vaccination against HPV infection, a gradual decline in the incidence of cervical cancer cases has been observed in developing countries. The developing nations bear the brunt of cervical cancer incidence due to low acceptance of vaccination. This survey-based study was designed to assess the awareness and opinions of female university students regarding human papilloma virus, vaccination and cervical cancer. A survey questionnaire was distributed among female expatriate students (18 to 26 years of age) of a private university. The survey sought information on socio-demographic characteristics, family and personal health history, knowledge of cervical cancer, its association with HPV, preventive care and their opinions on vaccination. GraphPad was used for statistical calculations. Of the 269 respondents, only 6% had attended awareness programs and 11% reported having read any information leaflet. 78% of the respondents did not know how HPV infection occurs and less than 40% of the participants believed that cervical cancer is preventable. 75% of the respondents had not heard about the PAP smear test. 20% of the participants stated that they were uninterested in taking the vaccination and only 5% of the survey respondents had received vaccination. Majority of the respondents (78%) demonstrated positive attitude towards practices related to influence of nutrition in having a disease-free life. The present study indicates low levels of awareness regarding HPV and its role in cervical cancer among female university-going students. It was found that the awareness of HPV, their role in cervical cancer development and the availability of information regarding vaccination was very low. The authors recommend that educational institutions and government health authorities must offer a well-designed comprehensive awareness cum vaccination camp in order to educate young women about HPV infection and risk of developing cervical cancer. This will help ensure future economic and health benefits for all.
Keywords: Cervical cancer; human papilloma virus; awareness; vaccination; knowledge; health
With 19.3 million new cases and 10 million cancer-related deaths globally in 2020 alone, cancer presents itself as one of the foremost causes of death [1]. Cervical cancer, a malignant neoplasm of the uterine cervix is the fourth most common cancer affecting women across the world and accounts for 6.5% of cancer incidence globally; with 604000 new cases and 342000 deaths in 2020 [1,2]. Despite cervical cancer being one of the most preventable forms of cancer, the developing and less developed regions of the world bear 85% of the total burden [1,3]. Even in the UAE, cervical cancer is the second most common cancer prevalent in women living in UAE with 50% of the reported cases in women aged between 35 and 55 years [4,5]. However, in the higher income, developed countries, cervical cancer cases have steadily declined by 4% annually [3]. A staggering nine out of ten deaths happen in the developing countries with the risk of death three folds higher, when compared with the more developed regions [1]. The disparity in the statistics is stark. The lower incidence and better outcomes in the developed world can be attributed to better screening programs and higher adoption of vaccination schedules. The Health Authority of Abu Dhabi (HAAD) aims to reduce the incidence and mortality by 60% by the year 2025.
Persistent infection with Human Papilloma Virus (HPV), a common sexually transmitted virus is one of the primary causes of cervical cancers; and the type of virus indicates the risk of cancer onset [6]. Nearly, 65% to 80% of all cervical cancers are caused by HPV 16 and HPV 18 two high-risk genotypes [6,7]. During the long incubation period prior to onset of cancer after HPV infection, it has been noted that several risk factors such as multiple sexual partners, number of pregnancies, smoking, exposure to mutagens, co-infections, immune-deficiency/suppression, genetic predisposition and epigenetic alterations may also contribute to cancer development [8–13].
Cervical cancer is preventable by adopting vaccination against HPV in adolescent girls from the age of 11 to 26 years [14]. Three vaccines are currently available namely, Cervarix (GlaxoSmithKline), Gardasil (Merck), and Gardasil 9 (Merck). All three protect against infection by the two high-risk types, HPV 16 and HPV 18. Additionally, Gardasil protects against HPV 6 and HPV 11 infections. Gardasil 9 was licensed in 2014, and it is capable of preventing 90% of cervical cancer by guarding against 9 types of HPV [14]. The World Health Organization through the Global Advisory Committee on Vaccine Safety (GACVS) update, has emphasized that 200 million doses of these vaccines have been given since 2006 and they were found to be safe and free of any adverse effects [15]. The development of these vaccines is indeed a significant step and can be credited with the decline in the incidence of cervical cancer cases over the past decade [2]. Papanicolaou (PAP) smear test is used as an effective screening test for early detection of cancer.
The major problem facing the vaccination drive amongst young women are the various cultural taboos as well as a lack of acceptance of the vaccine. This survey-based study was designed to assess the understanding of young, female expatriate university students regarding cervical cancer, its association with HPV infection and their attitudes towards vaccination. Further, an attempt was made to understand their thoughts and practices related to health and nutrition. Through this survey-based study, we have made an attempt to understand the prevalence of vaccination among expatriate women as well as gauge their reasons for vaccine avoidance. By eliciting information regarding vaccination hesitancy, we may be able to employ better strategies for the National Vaccination Plan and meet public health goals.
A survey questionnaire was prepared and piloted on a small group of students and their opinions on clarity and ease of understanding of the questionnaire was sought. After approval of the Institutional Review Board of the Ethics Committee the survey questionnaire was distributed among female students at a private university, irrespective of their educational specialization. Convenience sampling was followed. Participation in the survey was voluntary and informed consent was obtained. All respondents were found to be expatriates, reflecting the population of the university. All the respondents included were between 18 to 26 years age. Faculty and staff members were excluded. The survey questionnaire consisted of two sections. The first section sought information on subject’s socio-demographic characteristics, family history as well as health and nutrition status. The second part of the questionnaire had 13 closed-ended questions designed to assess their understanding and thoughts on cervical cancer, HPV and vaccination. Respondents who correctly identified that cervical cancer and HPV were linked were grouped as respondents with knowledge (n = 86). The responses and attitudes of these high knowledge respondents were then compared with the other respondents and associations were evaluated. For statistical analysis, chi square test and comparison of expected and observed frequencies as well as calculation of p-value was performed using online tool QuickCalcs available at Graph Pad (https://www.graphpad.com/quickcalcs/).
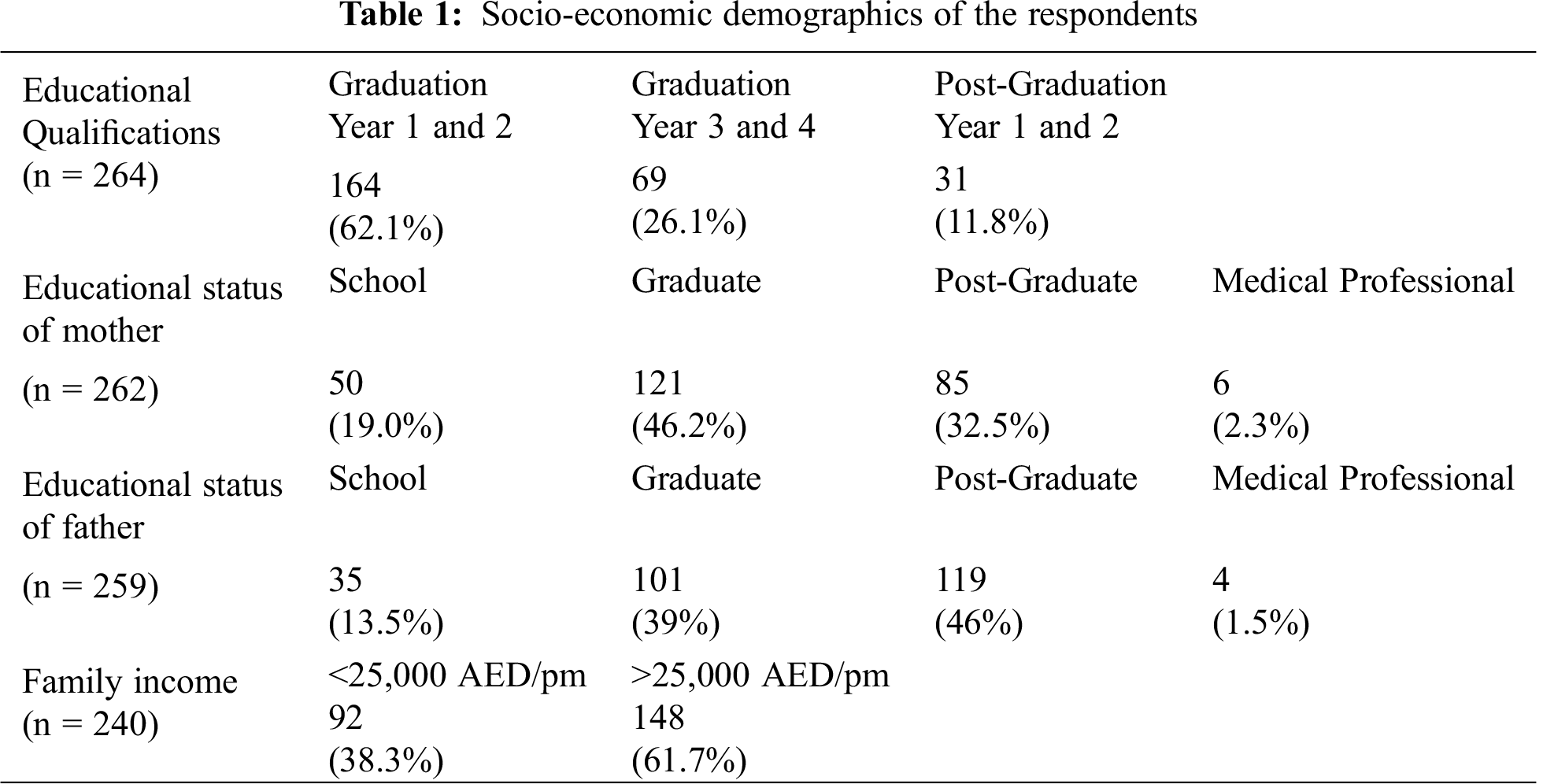
3.1 Socio-Demographic Characteristics
A total of 269 university attending female expatriate students belonging to the age group of 18 to 26 responded to the survey. This sample size was calculated to be statistically sufficient to provide significant results with a precision of ±5%. Majority of the students were expatriates associated with Asian sub-continent ancestry predominantly from India, Pakistan, Bangladesh, and others were either from the African continent or neighboring Arab nationals. The recruited subjects were mostly (88%) undergraduates and remaining (12%) were postgraduates. Almost all the respondents were unmarried. The socio-demographic findings of the recruited subjects are presented in Tab. 1.
3.2 Nutrition and other Health Related Practices
A majority (71%) of the respondents informed that they consume dairy products daily; also 47.5% of the respondents informed that they eat at least three servings of fruits and vegetables daily. Nearly 75% of the recruited subjects were not taking any health supplements. Most of the respondents believed that a healthy diet (79%) and a diet rich in fruits and vegetables (71%) decrease the risk of any kind of disease (Tab. 2).
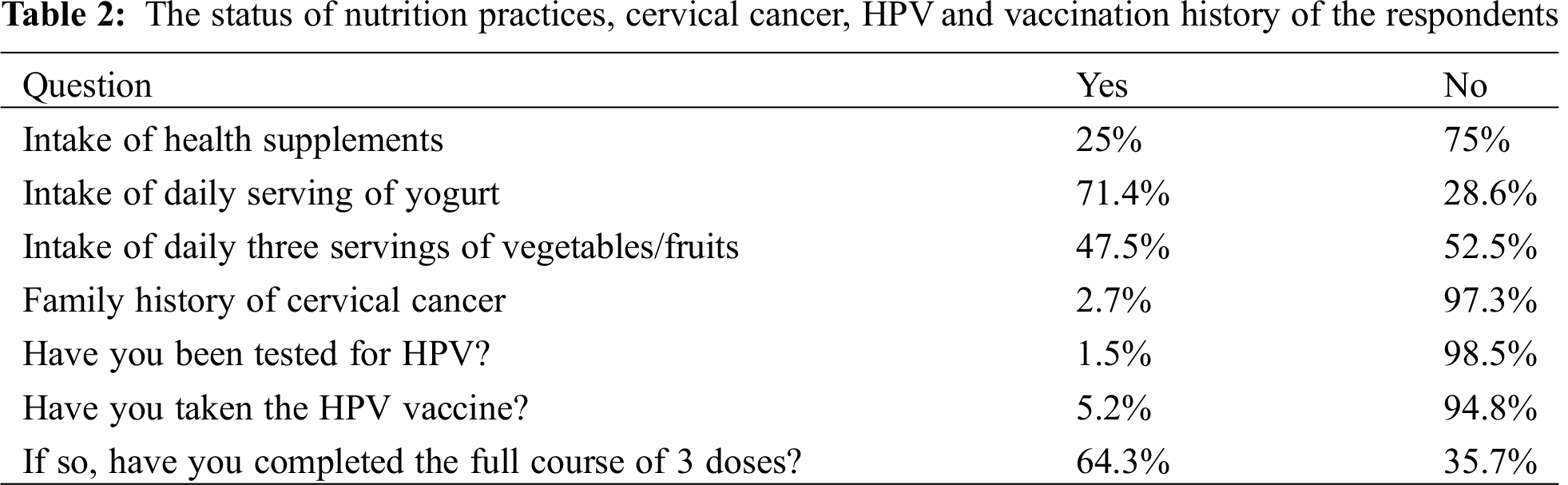
3.3 Cervical Cancer History and Vaccination
A very small percentage of the students (2.6%) reported a history of cervical cancer in their families. Nearly 5% of the participants reported that they had taken the vaccination, however, ~35% of them had not completed the full dosage schedule. Only 1.4% of the respondents were tested for HPV (Tab. 2).
3.4 Knowledge and Thoughts on Cervical Cancer and HPV
Only 1/4th of the participants (25%) responded that they are aware of HPV infection, but ~85% were aware of cervical cancer. A majority of the students (68%) were not aware of the association between HPV infection and cervical cancer development. Likewise, ~61% of the students were unaware of the availability of vaccines. Nearly 31% of the students reported having been recommended to take HPV vaccination by their physicians. The level of awareness was quite less with only 6% having attended any awareness program and only 11% reported having read any pertinent information leaflet. A fairly high number of the respondents (75%) had no knowledge of the PAP smear screening test. Amongst the 25% who had heard about PAP smear test, a good amount of them stated that they did not know its utility or application. Less than 40% of the participants believed that cervical cancer is preventable and ~85% believed that there was no-risk of the disease after vaccination.
Nearly 78% respondents were not familiar with the occurrence pattern of HPV infection and only 1% of the respondents correctly identified it as a sexually transmitted infection. Surprisingly, 1.5% of the respondents blamed bad luck as a cause of the infection. When asked about the prevention strategy for cervical cancer, a majority (68%) of them were not aware of it, and only 21% and 9% of the students identified vaccination and PAP smear test, respectively as prevention strategies. Lack of awareness of the availability of vaccination against HPV (55% of respondents) was reported as the major obstacle in taking the vaccine, while ~20% of the participants indicated a carefree attitude towards taking vaccination, others listed location, pain or cost as the major deterring factors (Tab. 3; Fig. 1). Respondents who knew that cervical cancer and HPV are linked (n = 86) were considered as having knowledge of cervical cancer. To check if these respondents had better knowledge and attitudes to nutrition, vaccination and other parameters, comparison was made for each question between responders with knowledge (n = 86) and lack of knowledge (n = 183). The significance of these associations was also drawn (Tab. 4). No association was found between levels of awareness and respondent’s course of study, year of study, age, family income and parent education level (all p values > 0.05).
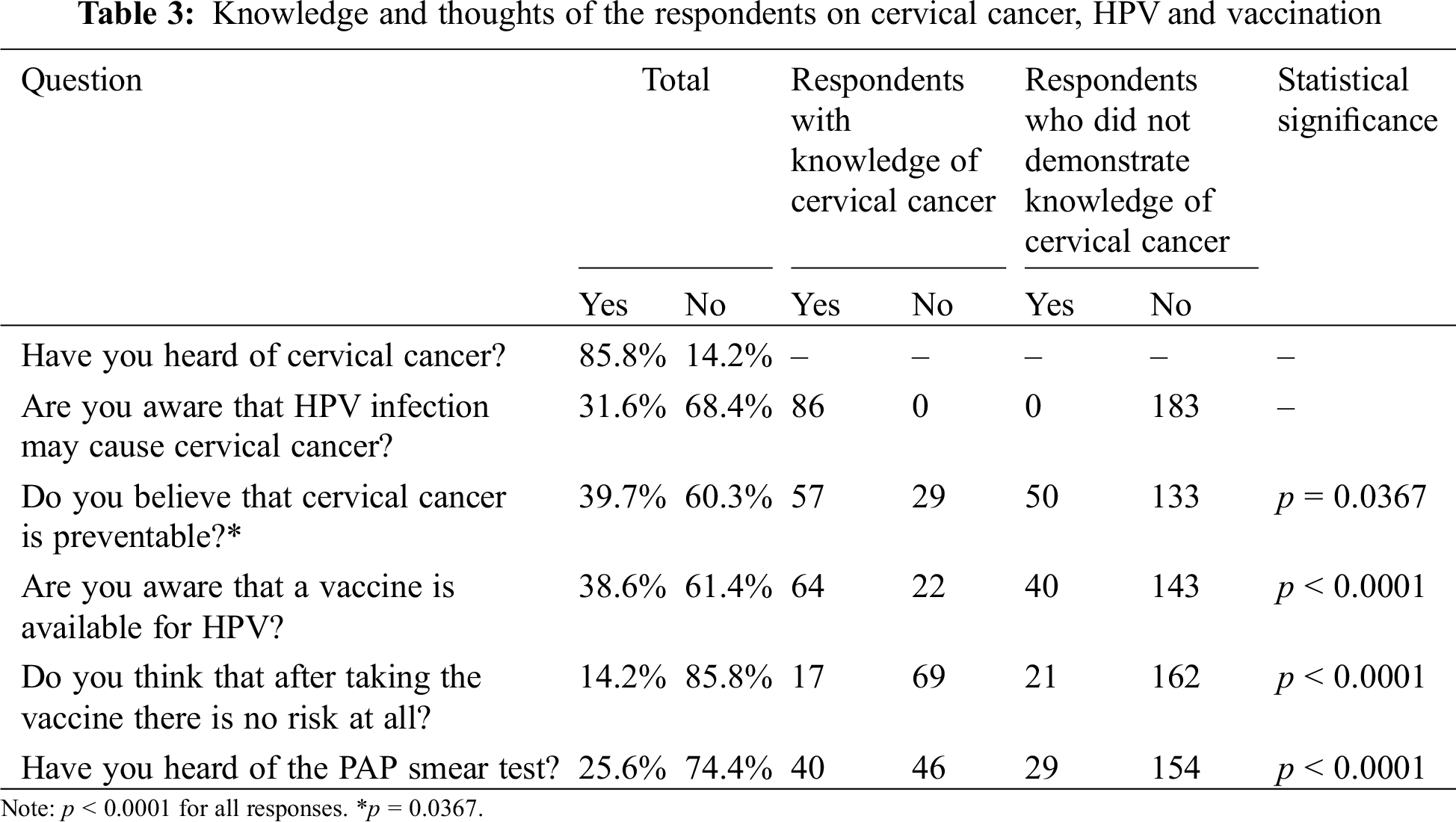
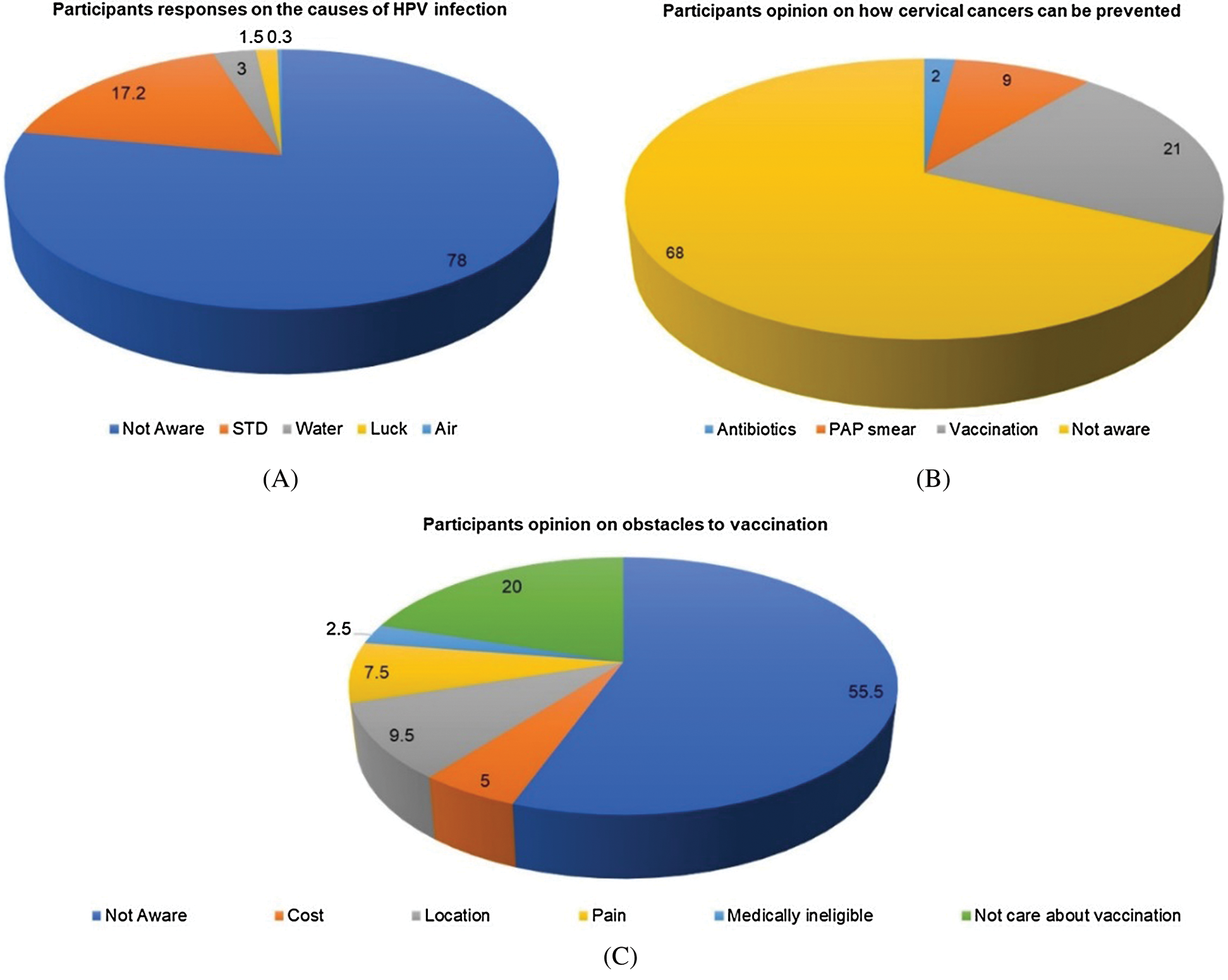
Figure 1: A: Participants responses on the causes of HPV infection. B: Participants opinion on how cervical cancers can be prevented. C: Participants opinion on obstacles to vaccination. All values are in percentage
Our study suggests that awareness about cervical cancer HPV and available vaccination is very low amongst young, university-going female students in the UAE. There is a pressing need to educate them regarding HPV infection, its modalities, vaccinations and screening programs in order to equip them towards taking well informed decisions. Cervical cancer being a preventable form of cancer, it is imperative that every effort be taken to educate the young females; this will protect them and in turn prompt them to counsel their older female relatives to undergo PAP smear testing. Earlier, Ortashi et al. [16] reported that amongst women aged 18 to 50 years in Al Ain, the knowledge of HPV infection and vaccine was very low. Likewise, a small descriptive survey study on 53 women in Umm al Quwain, also reported low awareness of cervical cancer, Pap smear testing and vaccination [17].
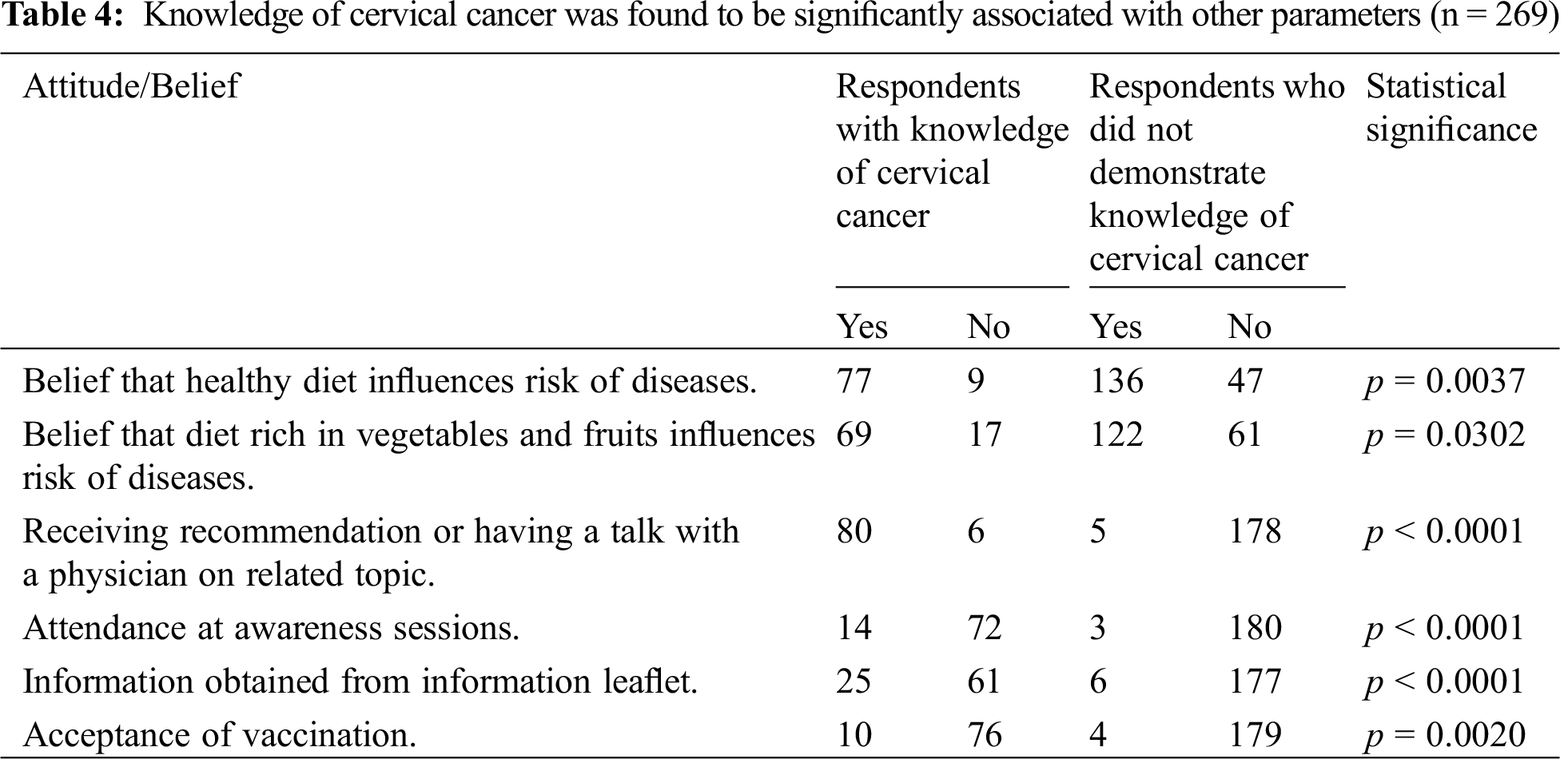
Respondents who knew that cervical cancer and HPV are linked (n = 86) were considered as having sufficient knowledge of cervical cancer. To check if these respondents had better knowledge and attitudes to nutrition and vaccination, comparison was made for each question between high responders (n = 86) and the remainder. A significant association (p < 0.0001) was found between those who had better awareness about cervical cancer with vaccination recommendation from their physician. This age group of the students is in general gifted with a strong immune system and therefore not likely to visit medical professionals that frequently, neither are they are young enough for periodic visits to pediatricians nor are they are old enough to warrant visits to the gynecologists. Thus, it appears that this age group does not enjoy much access to counseling or recommendations by medical professionals. The low levels of vaccination amongst the students and the fact that it has only been a little over a decade since the approval of the vaccines, suggests that parental knowledge of the disease and its prevention could be low. Subject to the validation of this thought through further parental age groups surveys, vaccination awareness drives targeting parents of young women is recommended. This study could also find no significant correlation between the education level of both parents with the information given by the respondent. Further, a strong association was found between knowledge of HPV and cervical cancer amongst those who had attended an awareness session or had read an information leaflet. This suggests the assumption that, if young women are armed with more knowledge, there will be greater acceptability of vaccination. This is also supported by the significant association we found between the level of the knowledge and vaccination status (p < 0.002). Interestingly, no association was found for age, difference in year and course of education and monthly family income with the knowledge level of the respondent.
However, it was heartening to note that a high percentage of the respondents had positive attitude towards nutritional diet and its impact in avoiding diseases. The respondents who believed that a healthy diet decreases the risk of the disease (p = 0.0037), and intake of fruits and vegetables decreases the risk of the disease (p = 0.0302) were found to be more aware about cervical cancer. It is clear that they believe that healthy eating is a key to a healthy life. This is particularly true in the case of diseases such as cervical cancer, where there is a long incubation period during which environmental factors influence initiation and progression of the disease. Several studies have already documented that a healthy diet rich in fruits and vegetables contributes to a reduced risk of cancer [18–20]. Consistent drives to influence good eating habits, positive food goals and availability of nutritious and balanced meals at cafeterias is key to ensure compliance.
More than 78% of the respondents did not know that HPV is sexually transmitted, only 17% of them were able to correctly identify it (Fig. 1). When asked how cervical cancer can be prevented, 68% of them reported that they were not aware (Fig. 1). Respondents reported several obstacles to vaccination, 55 % felt that lack of awareness was a primary obstacle, 7.5% reported that the associated pain was an obstacle, 5% reported cost and 20% reported being unconcerned about vaccination. Lack of concern could potentially stem from being unaware of the risk of disease and benefits of vaccination which can be addressed through awareness drives.
The statistics presented by GLOBOCAN and other germane agencies clearly identified the declining incidences in cervical cancer cases in countries that have adopted national level immunization and screening programs [1–3,21]. One of the primary approaches given by WHO-South East Asia for controlling cervical cancer in the region is mandatory vaccination for girls aged 9 to 13 years [22]. The development of cheap vaccines and/or substantial government subsidy could lift a significant economic barrier. Further, reduction in the number of dosages might also help in adherence to the vaccination schedules, as few previously published studies have supported the recommendation of a two-dose vaccine schedule [23].
Government supported vaccination programmes can help reach an entire generation of girls with the advantage of future cancer control, avoidance of medical costs and strain on national resources at a later date. We recommend that the national program launched by HAAD, UAE to reach out to public school girls in the capital city of Abu Dhabi, be extended to other private schools/universities in the country. Vaccination of school students before their last year of schooling has an added advantage of not missing out on those students who decide not to pursue higher education at universities. However, catch-up vaccination programs implemented at university level will ensure that dosages are completed, and no one is missed out. We believe that at university level, conducting annual awareness programs is essential and will benefit the students. An earlier study published from Kenya, reports that empowering teachers with knowledge facilitates the acceptability of vaccines [24]. Bakheit et al. [25] showed that while female teachers in Sharjah knew about PAP smear tests, they did not regularly undertake the screening test. This shows that awareness without add on facility and convenience of implementation, might not be sufficient in meeting the objectives. Therefore, the possibility of converting these awareness programs into awareness cum vaccination camps/programs in the university premises can be explored with a view to ensure complete coverage of females who are eligible for vaccination.
Cervical cancer is highly prevalent in UAE and the Middle East and North Africa region in general. Low level of awareness about a largely preventable form of cancer is detrimental to the health of young women. Serious effort must be taken by educational organizations in conjunction with governmental health authorities to educate them and provide them with the ease of access to vaccination. Medical awareness camps, counseling by family physicians will help remove vaccine hesitancy and advocate vaccination for young women and regular screening for eligible older women. Further, effort should be directed at improving nutritional practices and bring about a general awareness of other risk factors with an aim to improving general health and lower cancer risk.
Acknowledgement: The authors thank the authorities of MAHE, Dubai for permitting the conduct of this survey. We thank the participants for sharing their views voluntarily. The authors are thankful to the volunteers, Ms. Munazzah, Ms. Aishwarya Kolai and Ms. Keerthi Krishnakumar for their assistance in administering the survey. The author, Dr. Shafiul Haque is grateful to the Deanship of Scientific Research, Jazan University for providing access to the Saudi Digital Library.
Data Sharing: Data will be shared on request.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I. et al. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 12, e7386. DOI 10.3322/caac.21660. [Google Scholar] [CrossRef]
2. Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A. et al. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 68(6), 394–424. DOI 10.3322/caac.21492. [Google Scholar] [CrossRef]
3. Torre, L. A., Siegel, R. L., Ward, E. M., Jemal, A. (2016). Global cancer incidence and mortality rates and trends—An update. Cancer Epidemiology and Prevention Biomarkers, 25(1), 16–27. DOI 10.1158/1055-9965.EPI-15-0578. [Google Scholar] [CrossRef]
4. HAAD AD, Health Statistics 2012. https://www.scad.gov.ae/Release%20Documents/Health%202012%20English.pdf. [Google Scholar]
5. HAAD AD, HAAD Report on Cervical Cancer 2013. https://www.scad.gov.abudhabi/Release%20Documents/health%202013.pdf. [Google Scholar]
6. Burd, E. (2003). Human papillomavirus and cervical cancer. Clinical Microbiology Reviews, 16(1), 1–17. DOI 10.1128/CMR.16.1.1-17.2003. [Google Scholar] [CrossRef]
7. De Sanjose, S., Quint, W. G., Alemany, L., Geraets, D. T., Klaustermeier, J. E. et al. (2010). Human papillomavirus genotype attribution in invasive cervical cancer: A retrospective cross-sectional worldwide study. Lancet Oncology, 11(11), 1048–1056. DOI 10.1016/S1470-2045(10)70230-8. [Google Scholar] [CrossRef]
8. Alizon, S., Murall, C. L., Bravo, I. G. (2017). Why human papillomavirus acute infections matter. Viruses, 9(10), 293. DOI 10.3390/v9100293. [Google Scholar] [CrossRef]
9. Schiffman, M., Doorbar, J., Wentzensen, N., De Sanjosé, S., Fakhry, C. et al. (2016). Carcinogenic human papillomavirus infection. Nature Reviews Disease Primers, 2(1), 1–20. DOI 10.1038/nrdp.2016.86. [Google Scholar] [CrossRef]
10. Roura, E., Castellsagué, X., Pawlita, M., Travier, N., Waterboer, T. et al. (2014). Smoking as a major risk factor for cervical cancer and pre-cancer: Results from the EPIC cohort. International Journal of Cancer, 135(2), 453–466. DOI 10.1002/ijc.28666. [Google Scholar] [CrossRef]
11. Makuza, J. D., Nsanzimana, S., Muhimpundu, M. A., Pace, L. E., Ntaganira, J. et al. (2015). Prevalence and risk factors for cervical cancer and pre-cancerous lesions in Rwanda. Pan African Medical Journal, 22(1), 26. DOI 10.11604/pamj.2015.22.26.7116. [Google Scholar] [CrossRef]
12. Roura, E., Travier, N., Waterboer, T., de Sanjosé, S.,Bosch, F. X. et al. (2016). The influence of hormonal factors on the risk of developing cervical cancer and pre-cancer: Results from the EPIC cohort. PLoS One, 11(1), e0147029. DOI 10.1371/journal.pone.0147029. [Google Scholar] [CrossRef]
13. Wu, S., Powers, S., Zhu, W., Hannun, Y. A. (2016). Substantial contribution of extrinsic risk factors to cancer development. Nature, 529(7584), 43–47. DOI 10.1038/nature16166. [Google Scholar] [CrossRef]
14. Petrosky, E., Bocchini, J. A.,Jr, Hariri, S., Chesson, H., Curtis, C. R. (2015). Use of 9-valent human papillomavirus (HPV) vaccine: Updated HPV vaccination recommendations of the advisory committee on immunization practices. Morbidity and Mortality Weekly Report, 64(11), 300. [Google Scholar]
15. Bonanni, P., Zanella, B., Santomauro, F., Lorini, C., Bechini, A. et al. (2018). Safety and perception: What are the greatest enemies of HPV vaccination programmes? Vaccine, 36(36), 5424–5429. DOI 10.1016/j.vaccine.2017.05.071. [Google Scholar] [CrossRef]
16. Ortashi, O., Raheel, H., Shalal, M., Osman, N. (2013). Awareness and knowledge about human papillomavirus infection and vaccination among women in UAE. Asian Pacific Journal of Cancer Prevention, 14(10), 6077–6080. DOI 10.7314/APJCP.2013.14.10.6077. [Google Scholar] [CrossRef]
17. Al Sabbah, H., Haran, A., Saeed, A. (2015). Knowledge and beliefs related to cervical cancer, Pap smear screening and HPV vaccination among women in Umm Al Qawain UAE. International Journal of Excellence in Healthcare Management, 183(2831), 1–11. DOI 10.12816/0021392. [Google Scholar] [CrossRef]
18. van Berleere, M.,Dauchet, L. (2017). Fruits, vegetables, and health: Evidence from meta-analyses of prospective epidemiological studies. Vegetarian and plant-based diets in health and disease prevention, pp. 215–248. Cambridge, Massachusetts, USA: Academic Press. [Google Scholar]
19. Farvid, M. S., Chen, W. Y., Michels, K. B., Cho, E., Willett, W. C. et al. (2016). Fruit and vegetable consumption in adolescence and early adulthood and risk of breast cancer: Population-based cohort study. BMJ, 353, i2343. DOI 10.1136/bmj.i2343. [Google Scholar] [CrossRef]
20. Wang, X., Ouyang, Y., Liu, J., Zhu, M., Zhao, G. et al. (2014). Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: Systematic review and dose-response meta-analysis of prospective cohort studies. BMJ, 349, g4490. DOI 10.1136/bmj.g4490. [Google Scholar] [CrossRef]
21. Siegel, R. L., Miller, K. D., Jemal, A. (2016). Cancer statistics, 2016. CA: A Cancer Journal for Clinicians, 66(1), 7–30. DOI 10.3322/caac.21332. [Google Scholar] [CrossRef]
22. World Health Organization. Regional Office for South-East Asia (2015). Strategic framework for the comprehensive control of cancer cervix in South-East Asia Region. WHO Regional Office for South-East Asia. New Delhi, India. https://apps.who.int/iris/handle/10665/205921. [Google Scholar]
23. Kreimer, A. R., Struyf, F., Del Rosario-Raymundo, M. R., Hildesheim, A., Skinner, S. R. et al. (2015). Efficacy of fewer than three doses of an HPV-16/18 AS04-adjuvanted vaccine: Combined analysis of data from the Costa Rica Vaccine and PATRICIA trials. Lancet Oncology, 16(7), 775–786. DOI 10.1016/S1470-2045(15)00047-9. [Google Scholar] [CrossRef]
24. Masika, M. M., Ogembo, J. G., Chabeda, S. V., Wamai, R. G., Mugo, N. (2015). Knowledge on HPV vaccine and cervical cancer facilitates vaccine acceptability among school teachers in Kitui County, Kenya. PLoS One, 10(8), e0135563. DOI 10.1371/journal.pone.0135563. [Google Scholar] [CrossRef]
25. Bakheit, N. M., Haroon, A. I. B. (2004). The knowledge, attitude and practice of pap smear among local school teachers in Sharjah district. Middle East Journal of Family Medicine, 4(4), 10–18. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |