 Open Access
Open Access
CASE REPORT
Implementation of a High-Risk Outpatient Clinic for Children with Complex Congenital Heart Disease in a Reference Service in Brazil
1 Department of Pediatric Cardiology and Adult Congenital Heart Diseases, Heart Institute of the University of São Paulo, São Paulo, Brazil
2 Foronda Clinic, São Paulo, Brazil
3 Institute of Orthopedics and Traumatology, University of São Paulo, São Paulo, Brazil
4 Department of Echocardiography, Heart Institute of the University of São Paulo, São Paulo, Brazil
* Corresponding Author: Vanessa Ferreira Amorim de Melo. Email:
Congenital Heart Disease 2023, 18(6), 649-656. https://doi.org/10.32604/chd.2023.027987
Received 25 November 2022; Accepted 23 October 2023; Issue published 19 January 2024
Abstract
Background: Children with congenital heart disease (CHD), even after surgical approaches, and especially those who undergo staged procedures in the first months of life, remain vulnerable to readmissions and complications, requiring very close monitoring and differentiated intervention strategies. Methods: Descriptive and exploratory study, of the experience report type, which presents the process of building the high-risk outpatient clinic for complex congenital heart diseases (AAR) at the Instituto do Coração (InCor). Results: Report of the path taken to structure the AAR, demonstrating the organization, interface with the multidisciplinary team, admission and discharge criteria, training, and patient profile. In these five years of care, 275 patients were treated, 59.65% with biventricular interstage physiology, followed by univentricular interstage physiology (34.55%), residual defects after surgical procedures (3.63%), tumors with risk of mechanical obstruction (1.45%) and patients with an intrauterine approach (0.72%). The significant number of critical patients who were successfully discharged from hospital (44.72%), the low mortality rate due to sudden deaths at home and the high adherence to follow-up corroborate the impact of this specialized assistance. Conclusions: Despite the limitations of the study, this experience report showed that with few resources, there is the possibility of organizing an AAR with differentiated care, with the objective of early detection and treatment of residual injuries, identification of early interventions, education of parents for follow-up of their children, resulting in individualized treatment, promoting a better quality of life for this population.Keywords
Technological advances in recent decades have significantly improved intensive care and surgical approaches for congenital heart disease (CHD) in pediatric patients. These advancements have led to increased positive outcomes and subsequently, a rising number of children requiring specialized post-hospital discharge follow-up [1,2].
Children with CHD, particularly those who undergo staged procedures in the early months of life, remain vulnerable to readmissions and complications even after surgical interventions [1]. Published guidelines on outpatient treatment for complex congenital heart disease emphasize the importance of specialized monitoring to identify both expected and unexpected complications and physiological changes in these children’s development [2].
Therefore, frequent cardiovascular evaluations by specialists are essential to identify potential interventions before emergency care becomes necessary [3]. Several risk factors contribute significantly to adverse events outside the hospital setting and need close monitoring by pediatric cardiologists. These factors include comorbidities, complexity of surgical procedures, postoperative nutritional changes, medical complications, residual defects, and socioeconomic status, among others [1,4]. Moreover, outpatient follow-up also contributes to better family education, increasing their understanding of their child’s health, care, and adherence to treatment [2].
The structuring of this outpatient clinic in the largest congenital heart disease treatment center in Latin America was extremely important for the differentiated monitoring of high-risk patients. This type of strategy is scarce in the literature, with few published studies that guide the practice of organizing an outpatient clinic for complex congenital heart diseases (AAR), the different strategies, the challenges presented, and, mainly, how to start it with few resources available, given the economic disparities between countries. Therefore, our objective in this study is to show the path taken to structure this service, how it is organized and the profile of the patients served.
The objective of the study was to describe how the high-risk outpatient clinic for complex congenital heart disease patients at the Heart Institute (InCor) of the Clinics Hospital of the School of Medicine of the University of São Paulo (HCFMUSP) was conceived and structured to offer differentiated follow-up for this specific patient profile and contextualize the clinical and epidemiological data of the patients treated in the last five years.
This descriptive and exploratory study, an experience report type, presents the process of construction of the high-risk outpatient clinic for complex congenital heart diseases at the InCor, a public university hospital of high complexity, specialized in cardiology, pulmonology, cardiac and thoracic surgery and part of the HCFMUSP. It has 6 neonatal ICU beds, 21 pediatric ICU beds, 28 postoperative ICU beds and 33 ward beds.
For the description of the experience, the following aspects were considered: idealization of the outpatient clinic and the importance of its structure for the care of children with CHD who are at high risk of complications, developing the consultation and home monitoring model, interfacing with the multidisciplinary team and characterizing patients treated from January 2015 to July 2020.
The criteria for inclusion in the AAR are: patients from the Unified Health System (SUS), need for an early surgical approach, patients in the interstage period, residual defects that require strict monitoring and patients who require frequent medication adjustments.
The data presented were collected from January 2015 to July 2020, resulting from demands generated by medical care performed every Monday, and all information was recorded in an electronic medical record.
After collection, the data were organized into Excel spreadsheets, in which descriptive analysis of absolute and relative frequencies were carried out, represented by tables and graphs. This study was approved by the ethics committee, which waived the need for informed consent.
InCor’s AAR was designed to offer care with a multidisciplinary, individualized approach and advance care, providing an evaluation with the pediatric cardiologist and multidisciplinary team at shorter intervals than the common outpatient clinic, promoting early detection of residual injuries and clinical instabilities, and education in health.
However, establishing this specific care model faced numerous challenges, primarily due to limited financial resources as a public service. It initially began with consultations conducted by pediatric cardiologists and the nursing team. Still, it lacked a multidisciplinary team and dedicated testing facilities for echocardiograms, radiography, electrocardiograms, etc.
Over time, with the recognition of the importance of this differentiated outpatient clinic and collaboration with senior hospital leadership, the AAR expanded. The care evolved from a physician-centered approach to a multidisciplinary approach encompassing medical, social, nutritional, and developmental needs.
The AAR maintained the same permanent pediatric cardiologist, fostering trust among patients and family members. This trust significantly influenced treatment adherence and home care. Additionally, as a teaching hospital, resident physicians in pediatric cardiology had the opportunity to work under direct supervision, enhancing specialized training.
After a year and a half since its inception, a nutritionist appointment was added before every consultation with the pediatric cardiologist. Furthermore, the AAR offered social service assistance on-demand. Nursing played a crucial role in the clinic’s structure, organizing care logistics and conducting preoperative nursing consultations. When the need for evaluation by other specialties arose, it was managed within the HCFMUSP complex.
A significant improvement was the availability of regular slots for transthoracic echocardiograms, in addition to emergency slots specific to pediatric cardiology. The frequency of echocardiograms is individualized based on variables such as functional status, cardiac function, presence of valvular disease, arrhythmias, etc. When necessary, magnetic resonance imaging and angiotomography can be scheduled, along with radiographs and electrocardiograms.
On average, the AAR conducts 15 to 20 consultations per week, with return intervals determined by the pediatric cardiologist based on the patient’s specific needs, varying from weekly to every 15 days.
The clinic also prioritizes surgical interventions. While most surgical reinterventions are planned, some patients may require unplanned interventions, and the AAR is prepared to expedite these cases to reduce waiting list complications.
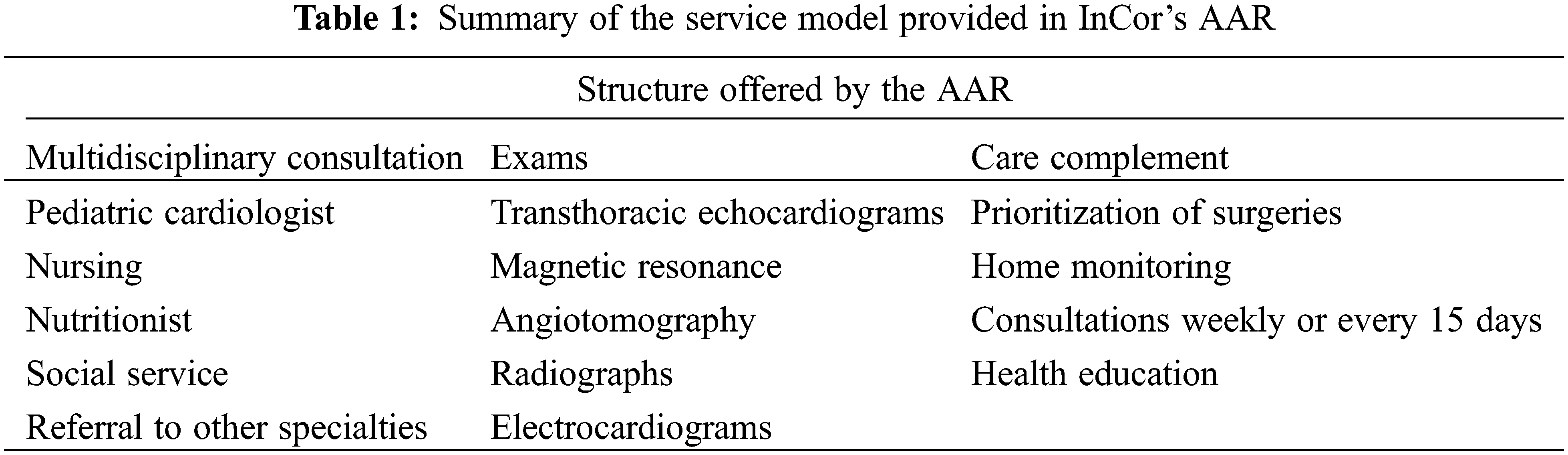
Another unique aspect of the AAR is the family’s training in monitoring stressors that can affect the clinical stability of the patients. The pediatric cardiologist provides guidance on using an oximeter at home, identifying alarm signals, and taking appropriate action. Table 1 summarizes the service model provided by InCor’s AAR.
To be eligible for the high-risk outpatient clinic, neonates, infants, children, and adolescents monitored at InCor must meet specific criteria. These include the need for early surgical intervention, being in the interstage period, having residual defects requiring close monitoring, and requiring frequent medication adjustments.
Regarding discharge criteria, clinical stability guides the decision. Patients who have undergone surgical stages, corrected residual defects, and are clinically stable are discharged from the AAR and referred for follow-up at the InCor congenital heart disease outpatient clinic. However, patients at risk of rapid decompensation remain under this strategy.
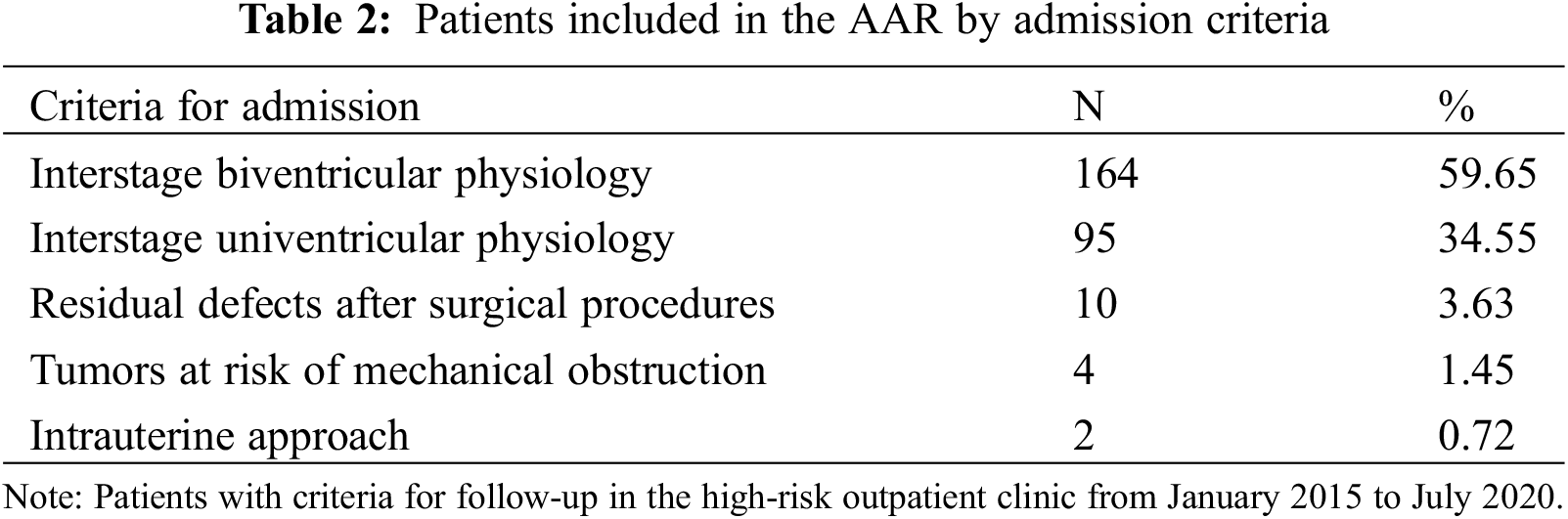
Table 2 shows the percentage of patients admitted to the outpatient clinic based on inclusion criteria. Most patients have interstage biventricular physiology (59.65%), followed by interstage univentricular physiology (34.55%), residual defects after surgical procedures (3.63%), tumors at risk of mechanical obstruction (1.45%), and patients with an intrauterine approach (0.72%).
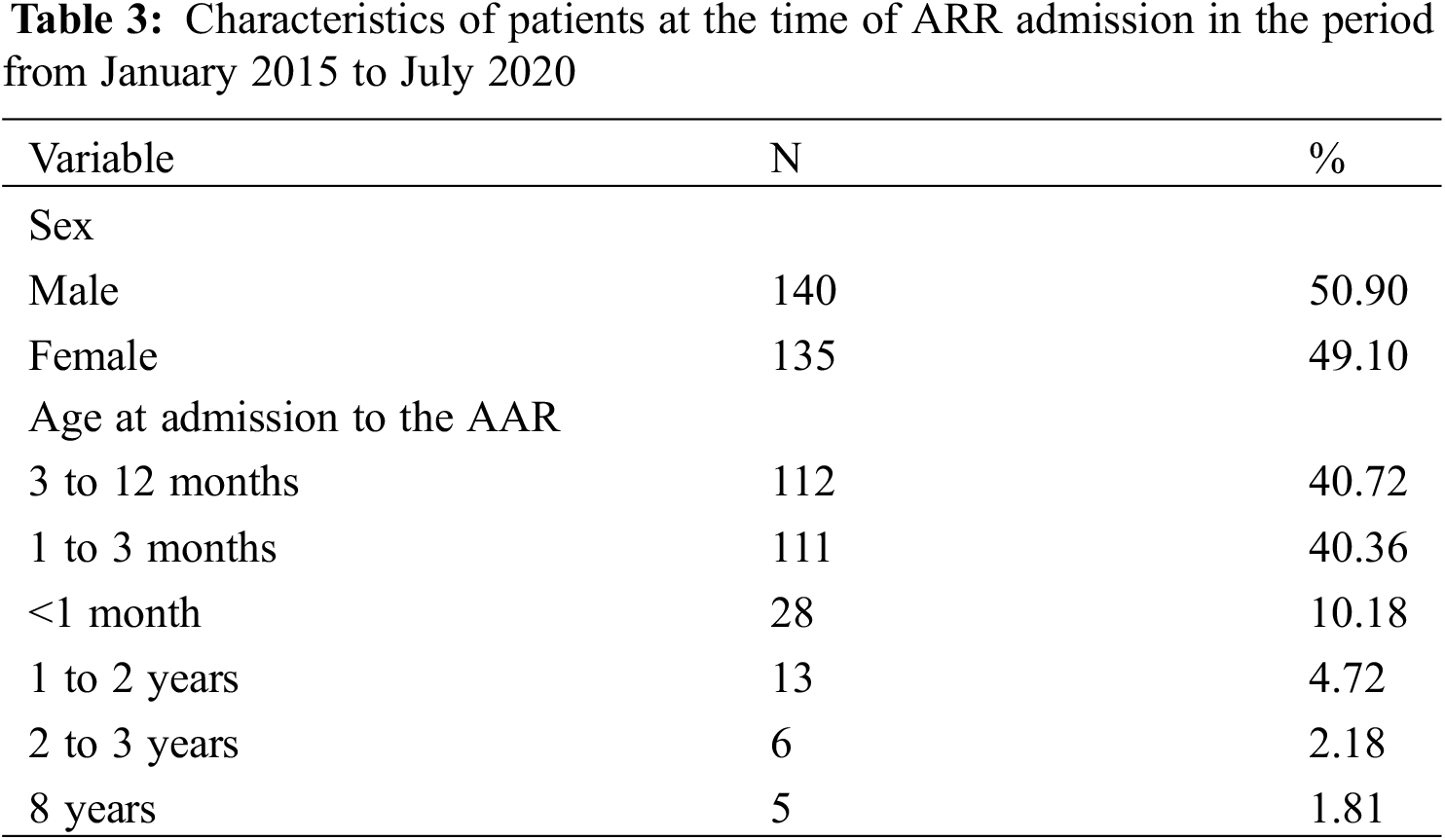
There was no significant difference in the distribution of patients according to gender, with 49.10% being female and 50.90% being male. In terms of the age of the patients at the time of admission to the AAR, 81.09% were between 1 month and 1 year old, followed by patients aged up to 31 days (10.18%), as shown in Table 3.
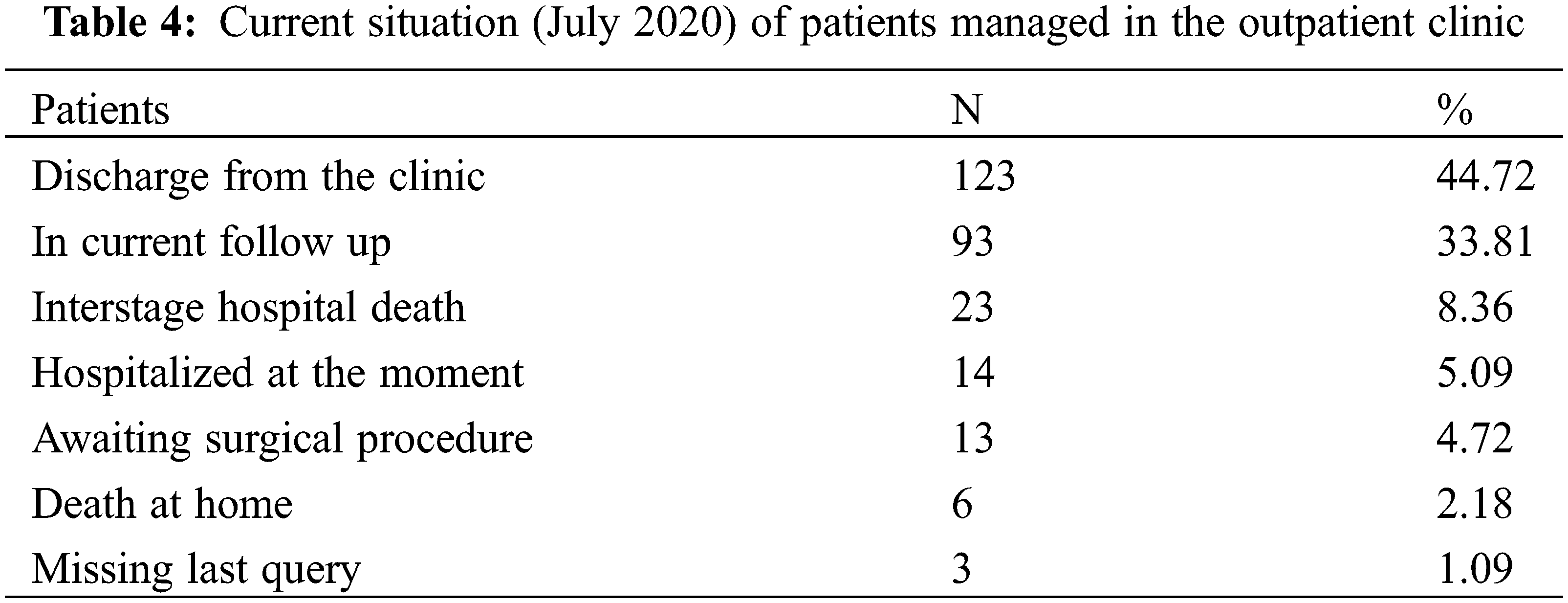
The current situation of patients over these 5 years of care is summarized in Table 4, which illustrates the significant number of critically ill patients who were successfully discharged, the low occurrence of sudden deaths at home, and the high adherence to this specialized follow-up.
In the context of CHDs, in Brazil, there is a shortage of highly complex cardiovascular hospitals. Of the 277 hospitals with just over 3,000 beds, only 9.6% perform pediatric cardiac surgery [5,6]. InCor, a public hospital, teaching, and research facility affiliated with the Medicine School of the University of Sao Paulo, is recognized as the largest reference center for congenital heart diseases in the country.
Initially, InCor had set up an outpatient clinic to monitor patients with congenital heart diseases in the pre- and postoperative periods. However, the concept of AAR is based on serving a particularly vulnerable population, with significant mortality in the first year of life, where approximately one-fifth of postoperative deaths due to congenital heart defects occur after hospital discharge [5].
Therefore, the referral criteria for this outpatient clinic were established to include patients at high risk of serious complications due to various expected and unexpected physiological challenges that require individualized planning [2,6].
In the literature, experiences with this type of service are scarce. To ensure the quality of care and minimize variation in the care provided to patients with severe congenital heart defects, members of the Cardiac Center of the Children’s Hospital of Philadelphia published guidelines for the treatment of complex congenital heart diseases, providing a structural model for an outpatient clinic [2].
This care model is aligned with these recommendations, which are based on complete cardiovascular assessment, health education, and communication with primary doctors [2]. Initially, care focused exclusively on doctors evolved into multidisciplinary care focused on medical and social needs, nutrition, and development, in accordance with international recommendations [2,7].
The inclusion of nutritional care was based on the need to recover and/or maintain nutritional balance, aiming to reduce the risk of surgical complications and provide adequate nutrients to prevent nutritional deficiencies [8]. Malnutrition and poor growth are problems found in children with CHD, especially univentricular, which can have negative impacts on the postoperative period and neurodevelopment [8].
The multidisciplinary team establishes contact with social service support upon demand. These professionals work to address social issues, to expand opportunities for choices and access to resources [2]. The availability of social support is essential for the family to adapt to home care for a high-risk child, as these patients may require different needs [9].
Another important component of the care model provided is the use of transthoracic echocardiograms to assist in the decision-making process and therapy guidance. Transthoracic echocardiograms are essential for monitoring patients, as they can evaluate the systemic function of the right ventricle, the degree of systemic tricuspid regurgitation, the presence or absence of subpulmonary obstruction of the left ventricular outflow tract, etc. [10].
Training for home monitoring carried out by family members is one of the pillars of the outpatient clinic, especially during the period of interest, as patients are at great risk of instability, and any factor that creates an imbalance in the relationship between demand and supply of oxygen can lead to cyanosis and decompensation important [7]. This justifies the recommendation of using a home oximeter for patients with high-risk heart disease, a simple and reliable strategy to detect worsening blood oxygenation.
The practice of home monitoring by parents, supported by the literature, significantly contributes to better adherence to treatment and caregiver empowerment. Combining home monitoring by a health team, even through telephone contact, enhances patient care, which is an important gain for the future of InCor’s AAR [3,11].
Table 1 summarizes the structure of care provided by InCor’s AAR, in which assistance does not present different approaches in relation to developed countries, however, for developing countries with a lack of resources for basic care for patients with CHD, this outpatient clinic’s experience demonstrates the feasibility of replicating this approach with limited resources in developing countries.
Another area of improvement involves providing psychological support for both the families and the children, including cognitive and learning assessments. Studies suggest that severe CHD can have adverse effects on cognitive and psychological functioning. Possible risk factors include reduced cerebral perfusion, treatment characteristics, overprotective parenting, or hospitalizations [12].
Until now, 275 children have benefited from this differentiated strategy, containing a significant number of critically ill patients who were successfully discharged and a low mortality rate from sudden deaths, which reflects the need to expand this external assistance to more complex needs when compared to lower risk congenital heart diseases. However, there is room for improvement within the AAR, primarily focusing on enhancing support and care strategies.
To implement these future perspectives, there is a need to either relocate or hire more professionals, which would require public funding, as this outpatient clinic is funded by the SUS.
Our study encountered the limitation of accessing retrospective data, which would have contributed to a better characterization of the patients treated at the AAR. Additionally, we were unable to quantify differences in clinical outcomes after the establishment of the outpatient clinic due to the absence of a retrospective database. Such an analysis would have been essential to strengthen our results. To enhance our evidence-based care, creating a comprehensive database is both essential and urgent for our service.
Technological advances in recent decades have greatly improved intensive care and the success rates of surgical approaches to CHD. This increase in favorable outcomes is evident in the growing number of children in need of specialized follow-up after their hospital discharge [2,6].
Tailored care for congenital heart diseases at high risk of home death is imperative. It enables the early detection and treatment of residual injuries, identifies opportunities for early interventions, and educates parents in monitoring their children at home. This approach results in individualized treatment and ultimately enhances the quality of life for this population.
The goal of this work was to share our experience in implementing an outpatient clinic focused on high-risk congenital heart diseases, elucidate the strategies employed and the structural organization, document our progress, and primarily demonstrate that this model of care can be implemented with limited resources and replicated in numerous healthcare settings.
Acknowledgement: None.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: Gustavo Foronda, Vanessa Ferreira Amorim de Melo; data collection: Ingrid Magatti Piva, Ana Cristina Sayuri Tanaka; analysis and interpretation of results: Claudia Regina Pinheiro de Castro Grau, Glaucia Maria Penha Tavares, Nana Miura, Gustavo Foronda; draft manuscript preparation: Vanessa Ferreira Amorim de Melo. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Data availability is not applicable to this article as no new data were created or analysed in this study.
Ethics Approval: This study was approved by the Ethics Committee, which waived the need for informed consent. Certificate of Presentation of Ethical Review: 46190821.7.0000.0068.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Brown, K. L., Wray, J., Knowles, R. L., Crowe, S., Tregay, J. et al. (2016). Infant deaths in the UK community following successful cardiac surgery: Building the evidence base for optimal surveillance, a mixed-methods study. Health Services and Delivery Research, 4(19), 29–49. [Google Scholar]
2. Wernovsky, G., Rome, J. J., Tabbutt, S., Rychik, J., Cohen, M. S. et al. (2006). Guidelines for the outpatient management of complex congenital heart disease. Congenital Heart Disease, 1(10), 10–26 [Google Scholar] [PubMed]
3. Dobrolet, N. C., Nieves, J. A., Welch, E. M., Khan, D., Rossi, A. F. et al. (2011). New approach to interstage care for palliated high-risk patients with congenital heart disease. The Journal of Thoracic and Cardiovascular Surgery, 142(4), 55–860. [Google Scholar]
4. Lantin-Hermoso, M. R., Berger, S., Bhatt, A. B., Richerson, J. E., Morrow, R. et al. (2017). The care of children with congenital heart disease in their primary medical home. Pediatrics, 140(5), 2017–2607. [Google Scholar]
5. Selig, A. F. (2020). Outlook and perspectives in diagnosis and treatment of congenital heart diseases in Brazil. Arquivos Brasileiros de Cardiologia, 115(6), 1176–1177 [Google Scholar] [PubMed]
6. American Academy of Pediatrics. Committee on Fetus and Newborn (1998). Hospital discharge of the high-risk neonate—Proposed guidelines. Pediatrics, 102(2), 411–417. [Google Scholar]
7. Ghanayem, N. S., Hoffman, G. M., Mussatto, K. A., Cava, J. R., Frommelt, P. C. et al. (2003). Home surveillance program prevents interstage mortality after the Norwood procedure. The Journal of Thoracic and Cardiovascular Surgery, 126(5), 1367–1377 [Google Scholar] [PubMed]
8. Medoff-Cooper, B., Ravishankar, C. (2013). Nutrition and growth in congenital heart disease: A challenge in children. Current Opinion in Cardiology, 28(2), 122–129 [Google Scholar] [PubMed]
9. Sarreta, F. O. (2008). The work of the social worker in health. Ciência et Praxis, 1(2), 39–46. [Google Scholar]
10. Buber, J., Schwaegler, R. G., Mazor Dray, E. (2019). Echocardiographic evaluation of univentricular physiology and cavopulmonary shunts. Echocardiography, 36(7), 1381–1390 [Google Scholar] [PubMed]
11. Hansen, J. H., Furck, A. K., Petko, C., Buchholz-Berdau, R., Voges, I. et al. (2012). Use of surveillance criteria reduces interstage mortality after the Norwood operation for hypoplastic left heart syndrome. European Journal of Cardio-Thoracic Surgery, 41(5), 1013–1018 [Google Scholar] [PubMed]
12. Karsdorp, P. A., Everaerd, W., Kindt, M., Mulder, B. J. (2007). Psychological and cognitive functioning in children and adolescents with congenital heart disease: A meta-analysis. Journal of Pediatric Psychology, 32(5), 527–541 [Google Scholar] [PubMed]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools