 Open Access
Open Access
ARTICLE
Long-Term Outcome of Adult Congenital Heart Disease Patients with Implantable Cardioverter-Defibrillators
1 Department of Cardiovascular Medicine, National Cerebral and Cardiovascular Center, 6-1 Kishibe-Shimmachi, Suita, 564-8565, Japan
2 Department of Cardiovascular Medicine, Graduate School of Medicine, The University of Tokyo, 7-3-1 Hongo, Bunkyo-ku, Tokyo, 113-8655, Japan
3 Department of Pediatric Cardiology, National Cerebral and Cardiovascular Center, 6-1 Kishibe-Shimmachi, Suita, 564-8565, Japan
* Corresponding Author: Kohei Ishibashi. Email:
Congenital Heart Disease 2025, 20(3), 273-286. https://doi.org/10.32604/chd.2025.067716
Received 10 May 2025; Accepted 02 July 2025; Issue published 11 July 2025
Abstract
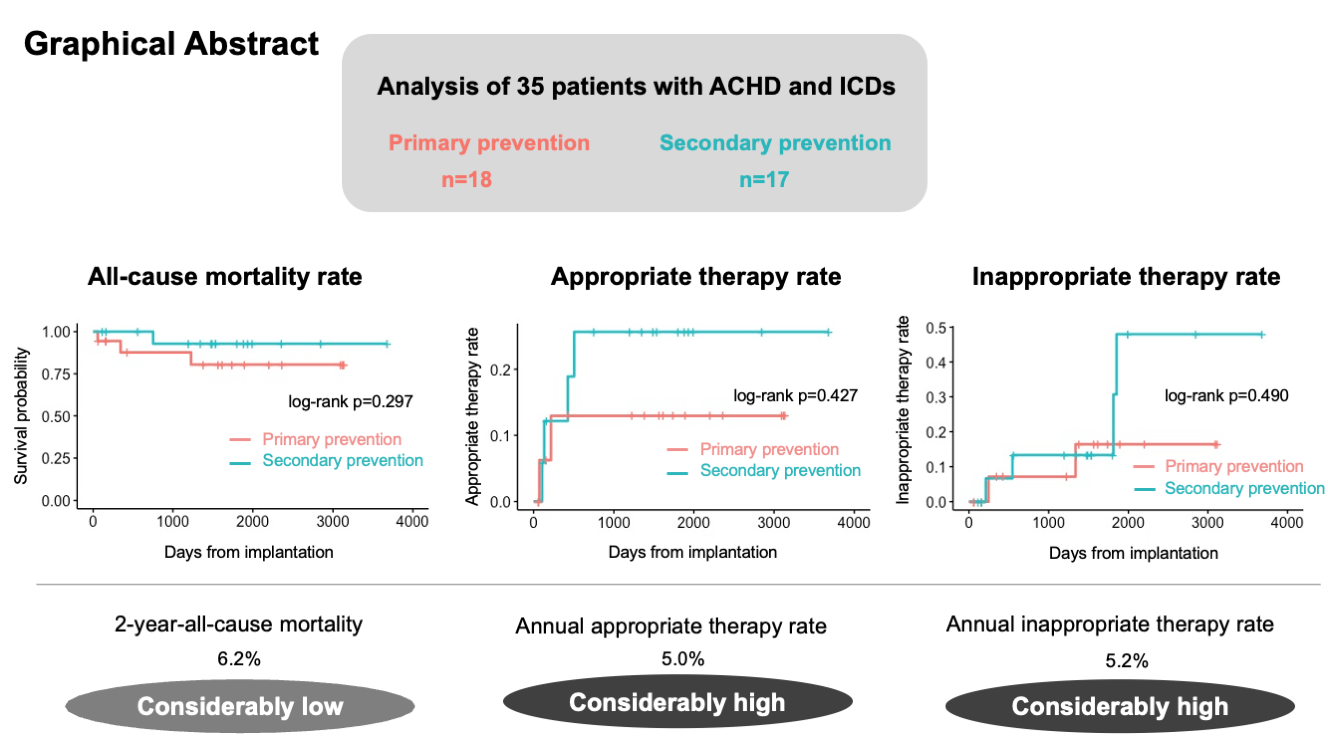
Background: Ventricular arrhythmia is a common cause of mortality in adult congenital heart disease (ACHD). The beneficial effects of implantable cardioverter-defibrillators (ICD) in patients with ACHD have been demonstrated; however, evidence on this topic remains insufficient. This study aimed to assess the long-term outcomes after ICD implantation in the ACHD population. Methods: We retrospectively reviewed 35 consecutive patients with ACHD who underwent ICD implantation between December 2012 and August 2022. ICD implantation was classified as primary or secondary prevention. The long-term outcomes, including all-cause mortality, appropriate and inappropriate ICD therapy, and complications related to ICD implantation, were evaluated. Results: Among the 35 patients, 18 patients underwent ICD implantation for primary prevention. During a median follow-up period of 1484 days, 3 patients in the primary prevention group and 1 patient in the secondary prevention group died. The 2- and 5-year all-cause mortality rates were 6.2% and 13.6%, respectively. Two (11.1%) and 4 (23.5%) patients in the primary and secondary prevention groups, respectively, received appropriate therapy. Six patients (17%) were administered inappropriate therapy, and 2 patients (5.7%) experienced device-related complications. Kaplan-Meier analysis revealed no significant differences in the all-cause mortality or the rates of appropriate and inappropriate therapy between the primary and secondary prevention groups (p = 0.297, p = 0.427, and p = 0.490, respectively). Conclusions: The incidence of appropriate ICD therapy in patients with ACHD was considerably high and comparable to that observed in patients with acquired heart disease, both in primary and secondary prevention. ICD implantation for primary prevention as well as for secondary prevention may be important in patients with ACHD.Graphic Abstract
Keywords
Supplementary Material
Supplementary Material FileCite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools