 Open Access
Open Access
ARTICLE
Efficacy of Singing Bowls in Childhood Asthma—A Pilot and Feasibility Study
Shahid Clinic, Mumbai, 400077, India
* Corresponding Author: Sukhbir Shahid. Email:
Sound & Vibration 2022, 56(3), 245-253. https://doi.org/10.32604/sv.2022.016139
Received 10 February 2021; Accepted 10 July 2021; Issue published 10 August 2022
Abstract
The potential use of sound and vibration for diagnostic and therapeutic purposes remains largely under-explored and under-estimated. Sound and vibrational energy has great positive impact on the mind and body. It could be particularly useful for psychosomatic diseases as a complementary therapy. Singing bowls, the spiritual ancient therapy has been claimed to aid in mind relaxation and painful and inflammatory conditions. Childhood asthma is an inflammatory airway disease and a psychosomatic disorder. The psychological management in it is often neglected leading to under-treatment or a relapse. Hence, we hypothesized that sound therapy with singing bowls might be useful as complementary therapy in management of childhood asthma. We aimed to study the effect of singing bowl session on child’s asthma severity and control and on the psychological well-being. Children <18 years of age and suffering from childhood asthma were recruited after informed written consent of parents. At the baseline, demographic and clinical details were noted. Anthropometric parameters, PEFR readings, asthma severity, parental and child’s subjective feeling of well-being, asthma control score, and pediatric symptom checklist score (based on age) were determined. The child was given 15 min of singing bowl session as per the set protocol. The subjective and objective evaluation of asthma control and psychological assessment was repeated at 1 month and 3 months follow-up and compared with the baseline results for clinical significance. Eighteen children formed the study group with a mean age of 9.13 ± 2.15 years (range 2–15.25 years). 4 children had psychological issues on initial screening. There was a significant improvement in asthma severity, subjective feeling of well-being and asthma control score at 3 months (p < 0.05). Singing bowl therapy could be a useful, low-cost complementary therapy in childhood asthmatics.Keywords
Sound and vibration have great practical and clinical usefulness but these remain largely under-evaluated and underestimated. Pleasant sound soothes and heals and this sound healing has been found to be effective for mental relaxation, sleep-induction, and as a cure for mental health diseases [1,2]. It can relieve mental tension and cause mood elevation [3]. Hence, it is postulated that it may be useful in therapy of psychosomatic diseases such as psoriasis, bronchial asthma, and the like.
Childhood asthma is a chronic inflammatory disease of the airways in children characterized by hyper-responsiveness of the airways to a variety of stimuli that is reversible either spontaneously or with treatment [4]. Since long, it is known that asthma is a psychosomatic disorder and mental stress and emotions play a role in the onset and progress of the disease through neuro-endocrine, autonomous, or immune mechanisms [5]. This exacerbates the disease and the disease can itself cause an enhancement of the negative emotions in the affected person. Recommended anti-asthma drugs target the inflammation but the psychosocial part of the ailment remains unattended. Hence, the disease is either not completely controlled or makes a comeback sooner or later once the anti-inflammatory medicines are stopped [6–8]. Therefore, the assessment and management of childhood asthma requires a comprehensive approach. Psychotherapy in form of relaxation techniques, systemic desensitization, and biofeedback has been found to be useful in therapy in childhood asthma [9,10]. But well-conducted studies in this field are limited [10].
Himalayan singing bowls deliver both a harmonious sound and vibration to the mind and body. It is made of 7 metals namely lead, tin, iron, copper, mercury, silver, and gold and is either hand-made or machine made. It is a form of ancient medicine and is used in many centers for spiritual purposes. The 7 metals signify the different astrological planets of our solar system. Lead is for Saturn, tin for Jupiter, iron for Mars, copper of venus, mercury for mercury, silver for moon, and gold for the sun [11]. The singing bowls of modern times is usually a bronze alloy of copper and tin only [1]. Some studies have revealed that singing bowls and sound therapy can decrease inflammation and pain and also lead to a state of mental well-being through its sound and vibrational energy [1,12,13]. Other studies have claimed that it boosts the immune function and helps repair the damaged cells and tissues of the body [14–17].
The use of this sound modality in children is not well-studied [18]. There is no study to date conducted on the role of singing bowls as complementary therapy in childhood asthma. Therefore, we started this pilot study based on the hypothesis that singing bowls could help in childhood asthma which is both a psychosomatic disease and an inflammatory disorder.
This pilot study was specifically meant to evaluate the efficacy, feasibility, difficulties if any, and any other unimagined side-effects of singing bowls on children with asthma. For this study, we recruited children ≤ 18 years of age who had repeated episodes of wheezing in the past one year. These children were on anti-asthma medications for their respiratory ailment and they were asked to continue them. A detailed history was taken and a thorough examination was carried out on them. After the demographic data, we enquired about family history of asthma or other atopy, and self-symptoms of other associated allergies such as allergic rhinitis, allergic conjunctivitis, and atopic dermatitis in the past or present. The anthropometric data such as weight and height was noted. Any current signs or remnants of atopy on the body were looked into. PEFR reading was taken in each child on this visit. PEFR values were compared with ERS and Polgar Spirometry normal values and graded as normal green zone >80%, yellow zone−50%–80%, and red zone =<50% normal values for height [19,20]. Based on the history and PEFR, each child’s asthma severity was gauged and noted. Thus they were mild, moderate, or severe asthmatics [21]. Details of the medications they are currently taking were interrogated into for each child. The parent’s subjective feeling about their child’s health condition was enquired into. The child was also queried about how he or she felt about his or her health. This was also assessed objectively by the asthma control score. Thus, they were classified as well-controlled, not well-controlled, or very poorly controlled [22,23]. Psychosocial analysis was done on each child by means of Pediatric Symptom Checklist (PSC) based on their age [24]. For children 6–18 years, PSC proforma was used. A cutoff score value of 28 was taken and if the score was above 28, it implied that the child had psychosocial issue. If the child was above 10 years of age and able to reliably answer the questionnaire, then for them Y-PSC form was used and a total score of 30 was considered abnormal. For children > 18 months < 6 years, preschool PSC was used. In this, a total score of above 9 was considered pathological.
The children were then subjected to the singing bowl session. The singing bowl therapy is a sound therapy and totally non-invasive in nature. There are no drugs administered. Hence a formal Ethical approval was not taken consistent with previous studies. Nonetheless, patients were informed in advance about the session and their written and informed consent was taken prior to the experimental therapy [25,26].
Singing bowl session-This 15-min duration session was served by means of a hand-made singing bowl of diameter 5 inches and of about 400 Hz frequency as per a set protocol to induce both an effect on the mind as well as the body and especially the lungs. This was so done so that both the sound and the vibrations of the singing bowl can induce the desired effect on the child’s body.
The child was called for review at 1 month and later at 3 months. On each of these follow-up visits, a detailed history, clinical examination, and severity of asthma were gauged. Any change in medications was questioned. The frequency of use of salbutamol inhaler puffs in the past 1 or 3 months respectively was enquired into. The parental and child’s subjective feelings about the health condition were noted. The control of asthma was assessed at each session. The psychoanalysis was repeated and changes if any noted. The study endpoints were asthma severity estimation, changes in asthma control score, the child’s and parent’s subjective feelings about child’s asthma, and changes in psychoanalytic assessment of the child after the singing bowl treatment.
Data analysis: The numerical data is expressed in the results section as Mean ± SEM. We used the chi-square test for analysis of categorical data and student’s t test for the numerical data. A p value of < 0.05 was considered as significant for this study [27].
20 children ≤ 18 years of age formed our study group. 2 children aged 1.08 years and 1.5 years could not cooperate enough for the singing bowl session. These two were excluded and hence we had a sample size of 18 children for this pilot study. The mean age of the children was 9.13 ± 2.15 years (range 2–15.25 years). There were 9 females and 9 males in this group. Family history of allergy was elicited in 7 (38.9%) children. The children had duration of wheezing of at least 1 year. The mean duration of symptoms in these children was 3.22 ± 0.76 years [range 1 to 5 years]. 5 children had mild asthma, 10 had moderate asthma, and 3 were severe asthmatics (Table 1).
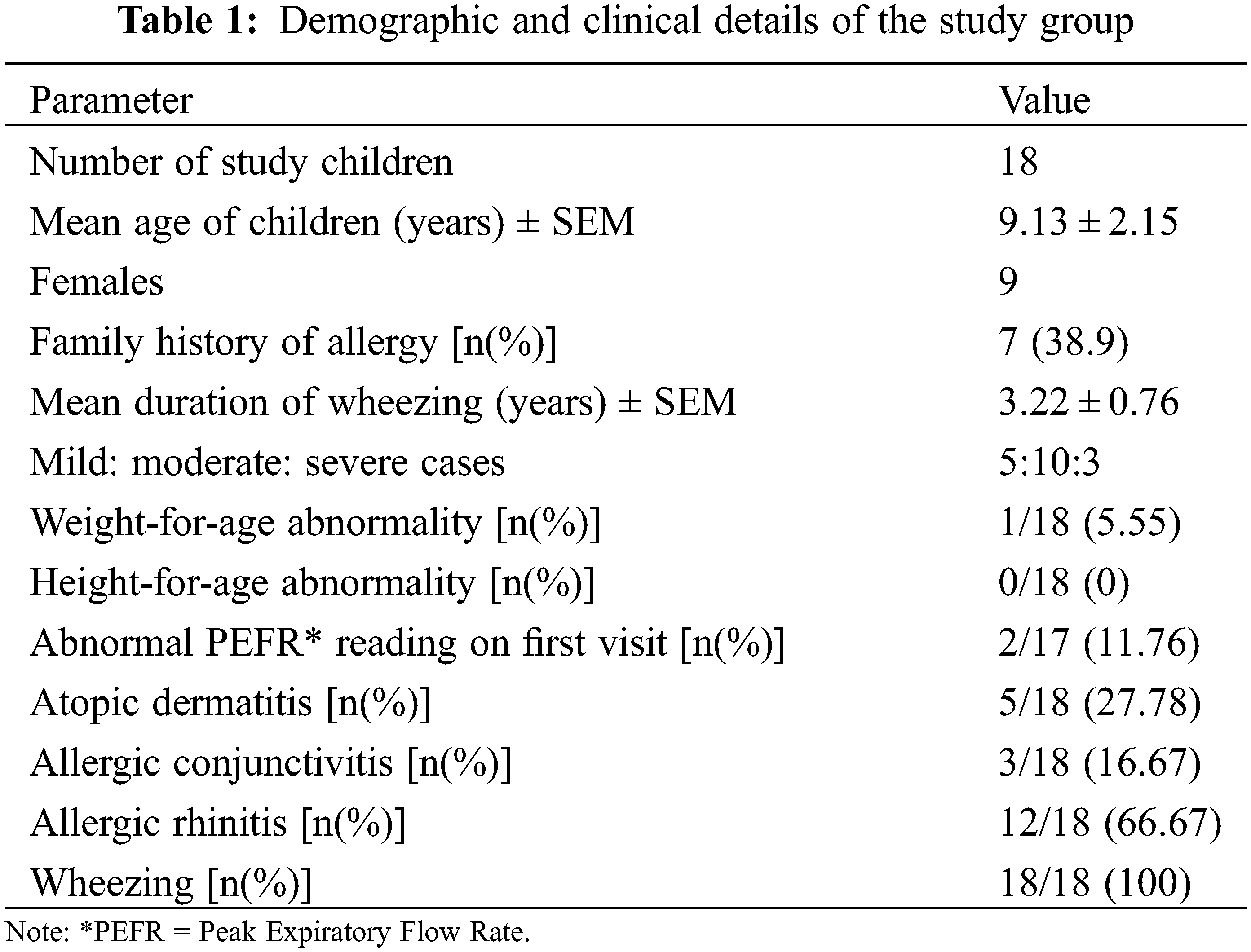
None of the children had any faltering of growth present except one 10-year-old male child who had less weight for age but normal height for age. Their heights and weights were compared with CDC charts and only one child has mild malnutrition. Besides, none of these kids were either tall or short for age.
At the time of the first test, the PEFR of 15 patients was above 80% of normal. But in two cases, it was in between 70–80 cases and both the children had severe type of asthma. One child who was 2 years of age was unable to give a reliable PEFR reading.
5 children had associated atopic dermatitis. One child had a past history of atopic dermatitis and was now cleared of it. History of allergic conjunctivitis was present in 3 children and 12 had symptoms suggestive of allergic rhinitis (Table 1). At the start, parents of 14 children felt that their children do not have good health condition and only 4 felt that despite the asthma, their child is okay. Also, when asked directly 15 children had a subjective feeling of ill-health due to asthma, while only 3 felt that they are okay despite the respiratory problem. The asthma control scoring revealed that 4 children had good control of asthma, 13 were not well controlled and 1 had poor control of asthma.
3 children were administered preschool PSC, 3 were given Y-PSC and the rest had PSC tests on them. A total of 4 children (2 in PSC, 1 in preschool PSC, and 1 in Y-PSC group) had higher than the cutoff scores on psychoanalysis testing. Hence, 22.22% children had associated psychosocial problems, on first screening.
At one month after singing bowl session, no children had ceased the prescribed medications or changed the doses. The parents of 15 children reported that they felt some improvement in their child after the intervention. 1 parent felt that there is minimal improvement while 2 did not see any appreciable difference post therapy. The same figures emerged when the child was asked directly about any improvement after therapy. This difference in subjective feelings of parents and child towards the child’s wellbeing revealed statistical significance (Fig. 1).
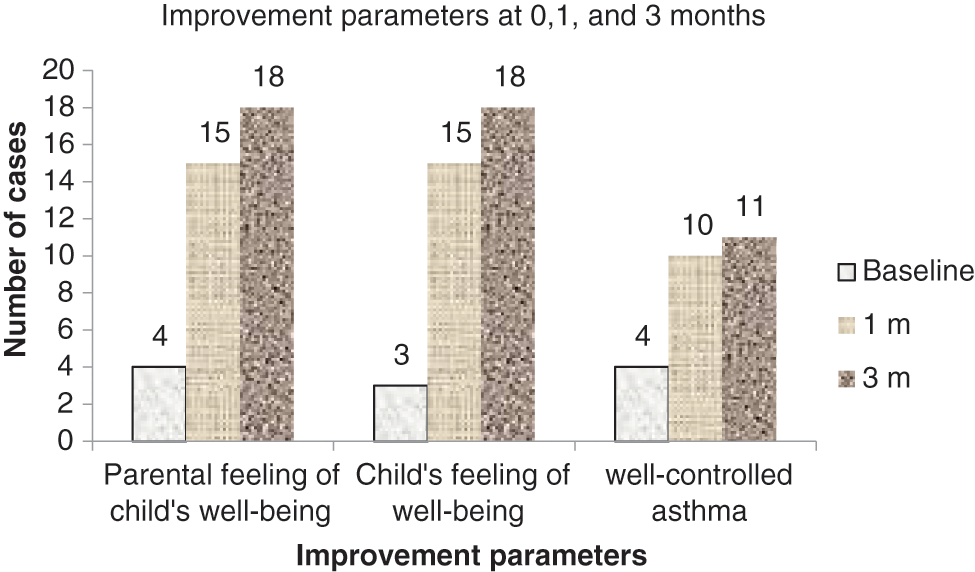
Figure 1: Improvement parameters at 0, 1, and 3 months
Objective assessment with asthma control score revealed that children with good control of asthma had risen from 4 to 10. The one child who earlier had as asthma score implying poor control now had a score of well-controlled asthma. The number of children with not well-controlled asthma fell from 13 to 8. But the fall was not statistically significant. Reassessment of the asthma severity also showed that now 12 children fell in the mild category and only 6 were moderate, while there was no severe case now in the group (p < 0.05) (Fig. 2).
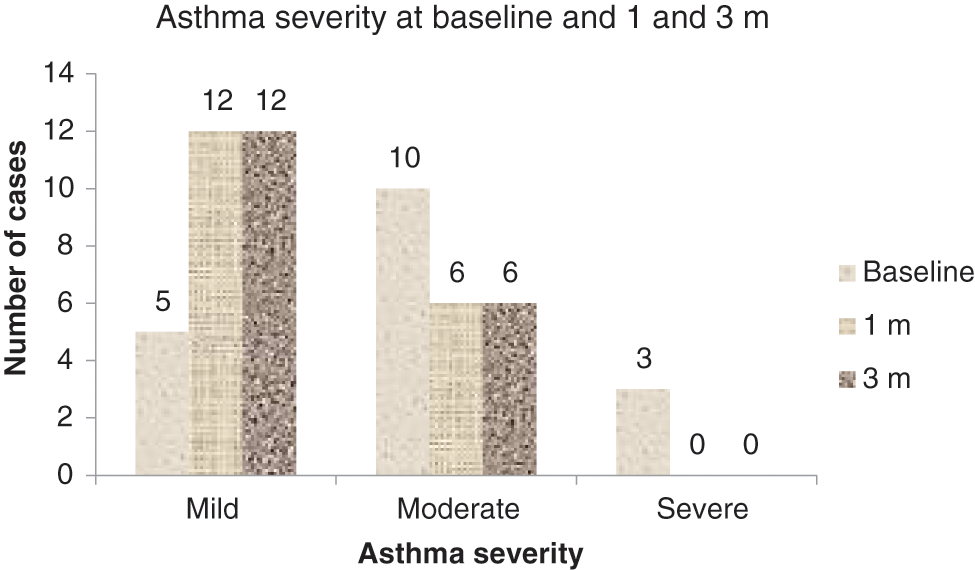
Figure 2: Asthma severity at 0, 1, and 3 months
The PEFR readings of all children was >80% normal (p > 0.05). Out of the 4 children with disturbed psychoanalysis on first visit, 3 had better scores on subsequent 1 month visit. And only one female child who was 3.5 years of age had a score above the cutoff value of 9 (p > 0.05) (Fig. 3).
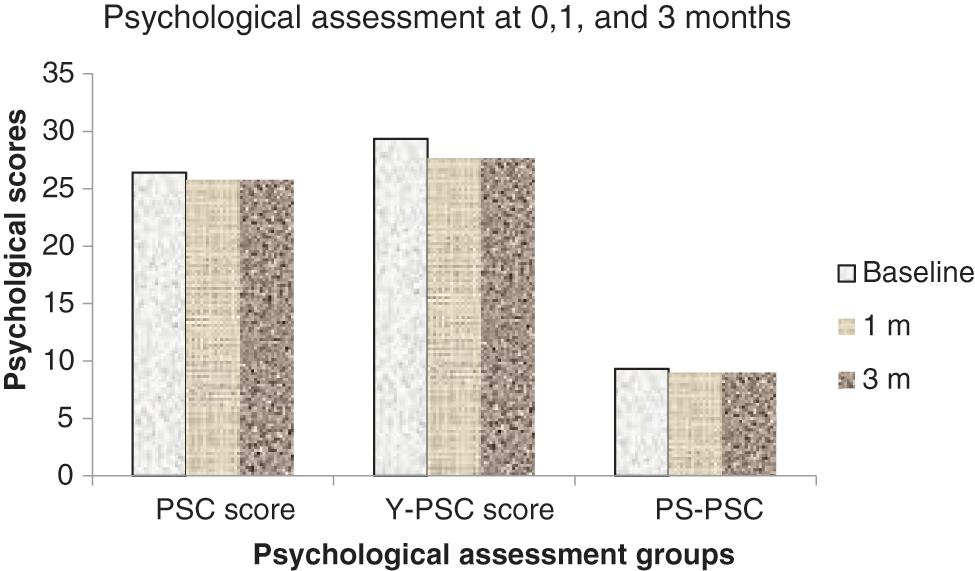
Figure 3: Psychological assessment at 0, 1, and 3 months
Thus, the percentage of children with abnormal PSC fell from 4 to 1, that is, 22.2% to 5.55% (Table 2).
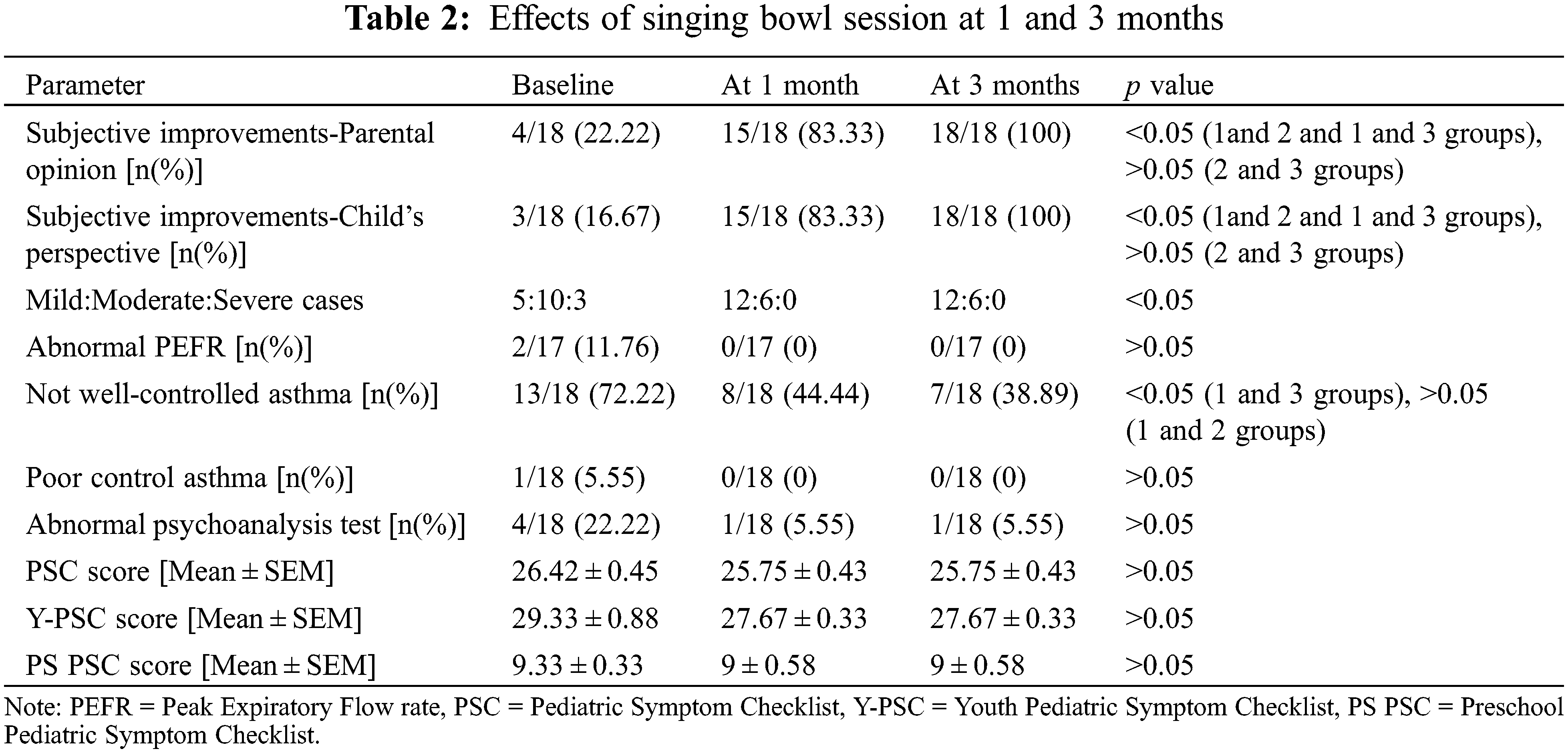
The psychoanalytic scores showed improvement but not in the statistical significance range (Table 2).
At 3 months, we noticed that the proportion of studied children with mild, moderate, and severe grade of asthma were similar to that at 1 months follow-up. PEFR readings were good in all the children. No changes in medications were recorded by the study children. All the children gave a subjective feeling of well-being and their parents also echoed similar feelings (p < 0.05). After 3 months of therapy, asthma score was well-controlled in 11 children and 7 had not well-controlled asthma. This was found to be significantly better compared to the baseline level. 17 children had good PSC scores while only 1 child continued to falter on it. Therefore, at 3 months, abnormal PSC remained at 5.55% (Table 2).
Sound healing with singing bowls has a great place in the therapeutics especially for mental relaxation in adults. There are very limited studies in children and none carried out in childhood asthma. This pilot study is the first of its kind in the world about the role of singing bowls in management of children with childhood asthma [18].
Our study showed that singing bowls could be used as a complementary therapy in childhood asthma. Out of the 18 children that participated in our study, all of them reported satisfaction with the treatment. The subjective improved feeling of well-being was reported both by the parents/caretaker as well as the children themselves. No ill-effects of the therapy were reported. Besides, on objective assessment of the asthma severity revealed that the therapy had benefited the patients in the control of their disease. The severity was lessened and their PEFR showed an improvement but the difference was not significant statistically.
The asthma control score and mean PSC scores also showed an improvement. A good control of wheezing was noted in significantly more children at 3 months interval post-therapy (Table 2). The mean PSC scores showed improvement though the difference was not significant. 89 children with severe asthma in Switzerland and Netherlands underwent intensive multidisciplinary inpatient treatment including psychotherapy and were followed up for 3–6 months. The control improved significantly though the researchers did not find any change in the children’s coping and parenting stress in parents [8]. We have done only one session on these children for this study. But we feel that a repeat singing bowl session after an interval of 3 or 6 months might be beneficial and might reveal a significant improvement in the mean PSC scores. Besides, this study was only a pilot study with a small sample size. We wish to continue the study with more participants.
It would be worthwhile to compare the findings in the asthmatic children who had singing bowl session with those asthmatic children who were on regular therapy but had no singing bowl sessions. The study was unable to differentiate whether the noted positive impact of the singing bowl session was due to its sound or vibrational component or both. Besides, we are also not certain whether the improvement in the asthma severity was solely due to the direct effect on the lungs of the vibrations or via the effect of it on the mental/emotional function of the individual [3]. There are some claims that sound therapy has helped even people who are deaf [28]. This implies that it is more of the vibrations emitted from the singing bowls that have a positive impact on these children. A singing bowl study on hearing impaired children with wheezing might help in this differentiation. A more detailed psychological testing of each child by a psychologist before and after the session would also be useful for the study.
Landry JM had studied the impact of 12 min of singing bowl session on heart rate, blood pressure, and PANAS (Positive and negative Affect schedule). They found that compared with silence, singing bowl session decreased heart rate and systolic blood pressure significantly. Diastolic blood pressure readings documented a non-significant fall. PANAS score fall was similar with singing bowl as well as silence session [29]. The singing bowl also causes an increase in alpha, theta, and delta brain waves, decreases the stress hormones such as cortisol and adrenaline, and increases the happy or feel-good hormones such as dopamine, serotonin, endorphins, and oxytocin [29–32]. We will also attempt to incorporate these in the further study.
When we compared the parental and child’s subjective feeling of well-being, asthma control score, and PSC scores in children with a family history of asthma/allergy and those who did not have such a history, there was no difference in these parameters in the two groups. The wheeze severity and systems affected also did not differ in the two groups.
The singing bowls could be used to provide a feeling of well-being in children with asthma. This in turn might affect their emotional well-being and lessen the psychological problems that trigger and exacerbate this psychosomatic disease. More elaborate studies would provide a deeper insight into the mechanism of benefit of the singing bowls in these children. But nonetheless, singing bowls could be tried as a low-cost, non-invasive, and feasible complementary therapy in the control of childhood asthma. This pilot study could serve as the foundation for a more randomized and controlled study of its effects on childhood asthma control.
Sound therapy in the form of singing bowls can be a useful supplementary tool in the management of childhood asthma. It does give the patient and its caretaker a subjective feeling of well-being and also lessens the wheeze severity. It also does improve the child on the psychological front though in our study this change was not significant. But large-scale detailed studies would help us to know the impact of this form of sound therapy on the psychology of the child.
Funding Statement: The author received no specific funding for this study.
Conflicts of Interest: The author declares that she has no conflicts of interest to report regarding the present study.
References
1. Emoto, M. (2005). The hidden messages in water. Illustrated Edition. New York: Atria Books. [Google Scholar]
2. Bergmann, M., Riedinger, S., Stefani, A., Mitterling, T., Holzknecht, E. et al. (2020). Effects of singing bowl exposure on karolinska sleepiness scale and pupillographic sleepiness test: A randomized crossover study. Public Library of Science One, 15(6), e0233982. DOI 10.1371/journal.pone.0233982. [Google Scholar] [CrossRef]
3. Goldsby, T. L., Goldsby, M. E., McWalters, M., Mills, P. J. (2017). Effects of singing bowl sound meditation on mood, tension, and well-being: An observational study. Journal of Evidence Based Complementary and Alternative Medicine, 22(3), 401–406. DOI 10.1177/2156587216668109. [Google Scholar] [CrossRef]
4. Quirt, J., Hildebrand, K. J., Mazza, J., Noya, F., Kim, H. (2018). Asthma. Allergy Asthma and Clinical Immunology, 14(Suppl 2), 50. [Google Scholar]
5. Graham, P. J., Rutter, M. L., Yule, W., Pless, I. B. (1967). Childhood asthma: A psychosomatic disorder? Some epidemiological considerations. British Journal of Preventive and Social Medicine, 21, 78–85. DOI 10.1136/jech.21.2.78. [Google Scholar] [CrossRef]
6. Barnthouse, M., Jones, B. L. (2019). The impact of environmental chronic and toxic stress on asthma. Clinical Reviews in Allergy and Immunology, 57(3), 427–438. DOI 10.1007/s12016-019-08736-x. [Google Scholar] [CrossRef]
7. Oland, A. A., Booster, G. D., Bender, B. G. (2017). Psychological and lifestyle risk factors for asthma exacerbations and morbidity in children. World Allergy Organization Journal, 10(1), 35. DOI 10.1186/s40413-017-0169-9. [Google Scholar] [CrossRef]
8. Verkleij, M., Beelen, A., van Ewijk, B. E., Geenen, R. (2017). Multidisciplinary treatment in children with problematic severe asthma: A prospective evaluation. Pediatric Pulmonology, 52(5), 588–597. DOI 10.1002/ppul.23623. [Google Scholar] [CrossRef]
9. Lask, B. (1992). Psychological treatments for childhood asthma. Archives of Disease in Childhood, 67, 891. DOI 10.1136/adc.67.7.891. [Google Scholar] [CrossRef]
10. Schuers, M., Chapron, A., Guihard, H., Bouchez, T., Darmonc, D. (2019). Impact of non-drug therapies on asthma control: A systematic review of the literature. European Journal of General Practice, 25(2), 65–76. DOI 10.1080/13814788.2019.1574742. [Google Scholar] [CrossRef]
11. Anonymous (2020). About antique singing and healing bowls. A unique collection of rare and beautiful sacred and ceremonial himalayan singing bowls for sale. https://www.antiquesingingbowls.com/about/7-metal-bowls.html. [Google Scholar]
12. Aravena, P. C., Almonacid, C., Mancilla, M. I. (2020). Effect of music at 432 Hz and 440 Hz on dental anxiety and salivary cortisol levels in patients undergoing tooth extraction: A randomized clinical trial. Journal of Applied Oral Science, 28, e20190601. DOI 10.1590/1678-7757-2019-0601. [Google Scholar] [CrossRef]
13. Bartel, L., Mosabbir, A. (2021). Possible mechanisms for the effects of sound vibration on human health. Healthcare, 9(5), 597. DOI 10.3390/healthcare9050597. [Google Scholar] [CrossRef]
14. Chanda, M. L., Levitin, D. J. (2013). The neurochemistry of music. Trends in Cognitive Science, 17(4), 179–193. DOI 10.1016/j.tics.2013.02.007. [Google Scholar] [CrossRef]
15. Pauwels, E. K., Volterrani, D., Mariani, G., Kostkiewics, M. (2014). Mozart, music and medicine. Medical Principles and Practice, 23(5), 403–412. DOI 10.1159/000364873. [Google Scholar] [CrossRef]
16. Babayi, T., Riazi, G. H. (2017). The effects of 528 Hz sound wave to reduce cell death in human astrocyte primary cell culture treated with ethanol. Journal of Addiction and Research Therapy, 8(4), 329–335. DOI 10.4172/2155-6105. [Google Scholar] [CrossRef]
17. Innes, K. E., Selfe, T. K., Brundage, K., Montgomery, C., Wen, S. et al. (2018). Effects of meditation and music-listening on blood biomarkers of cellular aging and Alzheimer’s disease in adults with subjective cognitive decline: An exploratory randomized clinical trial. Journal of Alzheimer’s Disease, 66(3), 947–970. DOI 10.3233/JAD-180164. [Google Scholar] [CrossRef]
18. Stanhope, J., Weinstein, P. (2020). The human health effects of singing bowls: A systematic review. Complementary Therapies in Medicine, 51, 102412. DOI 10.1016/j.ctim.2020.102412. [Google Scholar] [CrossRef]
19. European Respiratory Society (2021). Normal values of pulmonary functions. https://vitalograph.com/resources/ers-normal-values. [Google Scholar]
20. American Lung Association (2022). Measuring your peak flow rate. https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/living-with-asthma/managing-asthma/measuring-your-peak-flow-rate. [Google Scholar]
21. Global Initiative for Asthma (2019). Global strategy for asthma management and prevention. http://ginasthma.org/wp-content/uploads/2019/06/GINA-2019-main-report-June-2019-wms.pdf. [Google Scholar]
22. Pollart, S. M., Elward, K. S. (2009). Overview of changes to asthma guidelines: Diagnosis and severity. American Family Physician, 79(9), 761–767. [Google Scholar]
23. GlaxoSmithKline (2020). Understanding asthma. https://www.asthma.com/understanding-asthma/severe-asthma/asthma-control-test/. [Google Scholar]
24. Jellinek, M. S., Murphy, J. M., Robinson, J., Feins, A., Lamb, S. et al. (1988). Pediatric symptom checklist: Screening school-age children for psychosocial dysfunction. Journal of Pediatrics, 112(2), 201–209. DOI 10.1016/S0022-3476(88)80056-8. [Google Scholar] [CrossRef]
25. Bidin, L., Pigaiani, L., Casini, M., Seghini, P., Cavanna, L. (2016). Feasibility of a trial with Tibetan singing bowls, and suggested benefits in metastatic cancer patients. A pilot study in an Italian oncology unit. European Journal of Integrative Medicine, 8, 747–755. DOI 10.1016/j.eujim.2016.06.003. [Google Scholar] [CrossRef]
26. Trivedi, G. Y., Saboo, B. (2019). A comparative study of the impact of himalayan singing bowls and supine silence on stress index and heart rate variability. Journal of Behavior Therapy and Mental Health, 2(1), 40–50. DOI 10.14302/issn.2474-9273. [Google Scholar] [CrossRef]
27. Tyagi, V. N., Tyagi, N. K. (2019). Statistics in health and disease research. Chennai, India: Notion Press Private Limited. [Google Scholar]
28. Worseg, J. (2016). Sound for deaf-blind people and people with hearing disability. http://peter-hess-academy.com.au/sound-for-deaf-blind/. [Google Scholar]
29. Landry, J. M. (2014). Physiological and psychological effects of a himalayan singing bowl in meditation practice: A quantitative analysis. American Journal of Health Promotion, 28(5), 306–309. DOI 10.4278/ajhp.121031-ARB-528. [Google Scholar] [CrossRef]
30. Dukiu, H. (2018). Music, brain plasticity, and the resilience: The pillars of new receptive therapy. PsychiatriaDanubina, 30(Suppl 3), S141–147. [Google Scholar]
31. Moraes, M. M., Rabelo, P. C. R., Pinto, V. A., Pires, W., Wanner, S. P. et al. (2018). Auditory stimulation by exposure to melodic music increases dopamine and serotonin activities in rat forebrain areas linked to reward and motor control. Neuroscience Letters, 673, 73–78. DOI 10.1016/j.neulet.2018.02.058. [Google Scholar] [CrossRef]
32. Mallik, A., Chanda, M. L., Levitin, D. J. (2017). Anhedonia to music and mu-opioids: Evidence from the administration of naltrexone. Scientific Reports, 7, 41952. DOI 10.1038/srep41952. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2022 The Author(s). Published by Tech Science Press.
Copyright © 2022 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools