 Open Access
Open Access
ARTICLE
Comparison of clinical effectiveness and safety of 272 µm and 365 µm holmium lasers in retrograde intrarenal surgery
1 Department of Urology Clinic, Ankara Bilkent City Hospital, Ankara, 06800, Turkey
2 Department of Urology Clinic, Karabük University, Karabük, 78200, Turkey
* Corresponding Author: Demirhan Örsan Demir. Email:
Canadian Journal of Urology 2025, 32(2), 111-118. https://doi.org/10.32604/cju.2025.063970
Received 30 January 2025; Accepted 18 April 2025; Issue published 30 April 2025
Abstract
Introduction: Surgeons typically prefer 270 µm and 272 µm laser probes in retrograde intrarenal surgery (RIRS) due to the reduced deflection capacity of flexible ureterorenoscopes when using larger probe diameters. This study aims to investigate the effects of 272 and 365 µm holmium laser probes on operative time, clinical efficacy, and complication rates in RIRS. Materials and Methods: A total of 285 patients with proximal ureteral or kidney stones who met the inclusion criteria were enrolled in the study. Patients were divided into two groups based on laser probe thickness: 272 µm and 365 µm. Stone-free rates, operative time, and complication rates were compared between the groups. Factors affecting stone-free rates were analyzed using multivariate logistic regression analysis. Results: Patient and stone characteristics were similar between the two groups. No significant differences were found in stone-free or complication rates. However, operative time was significantly shorter in the 365 µm probe group. In univariate analysis, risk factors for postoperative residual stones included multi-calyceal stones, lower pole stones, high Hounsfield unit (HU) values on non-contrast computed tomography, and larger stone size. In multivariate analysis, independent prognostic factors for residual stones were identified as multi-calycal stones, lower pole stones, and high HU values. Conclusion: Compared to 272 µm laser probes, operative time was shorter in surgeries performed with 365 µm laser probes. The 365 µm holmium laser can be effectively and safely used in the treatment of proximal ureteral and renal stones, demonstrating high clinical efficacy and safety.Keywords
Retrograde intrarenal surgery (RIRS) is one of the methods commonly used in the treatment of renal stones, along with percutaneous nephrolithotomy (PCNL) and extracorporeal shockwave lithotripsy (ESWL).1 RIRS is recommended as the first treatment option, especially for stones between 1–2 cm.2 With advancements in flexible ureterorenoscopy (FU) and holmium laser technology, RIRS is now increasingly used for the management of stones larger than 2 cm.3
As the role of RIRS has expanded in the treatment of renal stones, some disadvantages of this method have also emerged. The main disadvantages are the difficulty in accessing lower pole stones, especially those with a narrow infundibulopelvic angle, low stone-free rates (SFR) in lower pole stones, and prolonged operative time for large stones.4,5
The deflection capacity of FU is of great importance in the treatment of lower pole stones with RIRS. As the diameter of the laser fiber used increases, the deflection capacity of FU decreases; therefore, using a small diameter laser, especially in lower pole stones, facilitates deflection.6 For this reason, conventionally small-diameter laser fibers such as 200 μm are preferred at FU.7 However, using small-diameter laser fibers also has some operational disadvantages. Although easier deflection may seem like an advantage, excessive deflection increases the risk of laser fiber breakage, thus increasing the cost of surgery.7 Furthermore, reducing the laser diameter may extend the duration required to fragment the stone, thereby prolonging the overall operative time.7,8
In this study, we investigated the efficacy and safety of 272 and 365 μm diameter holmium lasers used in the treatment of proximal ureteral and renal stones at different locations with RIRS.
The patients with proximal ureteral or kidney stones who underwent RIRS in our hospital’s urology clinic between December 2022 and December 2023 were retrospectively analyzed after obtaining local ethics committee approval. (Karabük University Medical Ethics Committee, IRB no: 2022/988). This study was planned following the Declaration of Helsinki. Informed consent was obtained from all patients before the operation day. Unilateral stones larger than 5 mm on non-contrast computed tomography (NCCT) and patients aged older than 18 years were inclusion criteria. Exclusion criteria were the urinary tract anomalies such as horseshoe kidney, ureteropelvic junction stenosis, preoperative urinary tract infection, presence of mid-ureteral and distal ureteral stones together with kidney and proximal ureteral stones, and bilateral stones. Upon applying the established inclusion criteria, a total of 285 patients were included in the study. Patients who underwent surgery with a 272 μm Holmium: YAG laser were classified as Group 1, and patients who underwent surgery with a 365 μm Holmium: YAG laser were classified as Group 2.
Preoperative age, gender, body mass index (BMI), Charlson Comorbidity Index (CCI) score, presence of preoperative JJ stent, previous stone surgeries, and whether ESWL was performed were recorded for all patients. All patients were evaluated with NCCT preoperatively. The number of stones, Hounsfield unit of the stone, location (proximal ureter, renal pelvis, upper/middle/lower calyces, multiple calyces), the kidney in which the stone was located (right, left), and the hydronephrosis presence and degree were recorded. Stone size was recorded by measuring the maximum length of the stone (for multiple stones, the sum of the maximum lengths of the stones). Intraoperative and postoperative data such as operative time (the time between the start and end of laser stone fragmentation was measured), number of pulses, complications, pain visual analog score (PVAS), duration of hospital stay, postoperative 1st day, and postoperative 1st month SFR were recorded.
All surgeries were performed under spinal anesthesia by 2 surgeons with experience of more than 250 cases. First, diagnostic ureterorenoscopy was performed by reaching the proximal ureter with a semi-rigid ureterorenoscope via a 0.035-inch guide wire. Then, after placing a ureteral access sheath (Flexor 9.5/11.5 Fr, Cook Medical Bloomington, IL, USA) over the guide wire, access to the proximal ureter and kidney was achieved with a non-digital flexible ureterorenoscope (Flex X2TM, Karl Storz, Tutlingen, Germany). In cases of lower pole stones, which presented difficulties in accessing the stone, a 1.9 Fr Zero Tip nitinol basket catheter (Boston Scientific, Marlborough, USA) was used to transport the stone to the appropriate calyx. The irrigation rate was kept below 25 mL/min, and irrigation pressure was increased when image quality deteriorated. Upon accessing the stone, fragmentation was performed using either a 365 µm or 272 µm holmium laser fiber, aiming to ensure that no fragments larger than 2 mm were left.
During the procedures, various stone-breaking techniques, such as fragmentation, dusting, and popcorn, were employed. Since the ultimate goal was to avoid leaving clinically significant stones larger than 2 mm, the stone fragmentation techniques, laser frequency, and power were adjusted and applied according to the characteristics of the stone.
Laser probe selection was made in order, independent of the patient and the characteristics of the stone. If a 272 µm laser probe was used in a case, a 365 µm laser probe was used in the next surgery. The power and frequency of the laser were changed according to the hardness and size of the stone. At the end of the operation, a 4.7 Fr JJ stent was placed in all cases, and the stent was removed after 2–3 weeks.
The stone-free rate (SFR) of the patients was assessed on postoperative day 1 and one month following surgery. Direct urinary system radiography was performed on the first postoperative day, and NCCT was performed on the first month. Patients with no residual stones larger than 2 mm were considered stone-free.9 Complications were classified using the Modified Clavien Classification System (MCCS).10 The pain level of the patients was measured with PVAS (range 1–10) on the first postoperative day.
The data analysis was performed using SPSS for Windows, version 23 (SPSS Inc., Chicago, IL, USA). The Shapiro-Wilk test, Kolmogorov-Smirnov test, histogram, and Q-Q plots were used to evaluate whether the variables showed normal distribution. Descriptive data were presented as the number and percentage for categorical data and as the median and interquartile range (IQR) for continuous variables. In the comparison of continuous independent variables between the two groups, the Student’s t-test and Mann-Whitney U-test were used; and in the comparison of categorical variables, the Chi-square test was used for categorical variables, Values determined as statistically significant in the univariate analysis were evaluated with multivariate logistic regression analysis to determine whether they were independent prognostic risk factors, increasing the residual stone. A value of p < 0.05 was accepted as statistically significant.
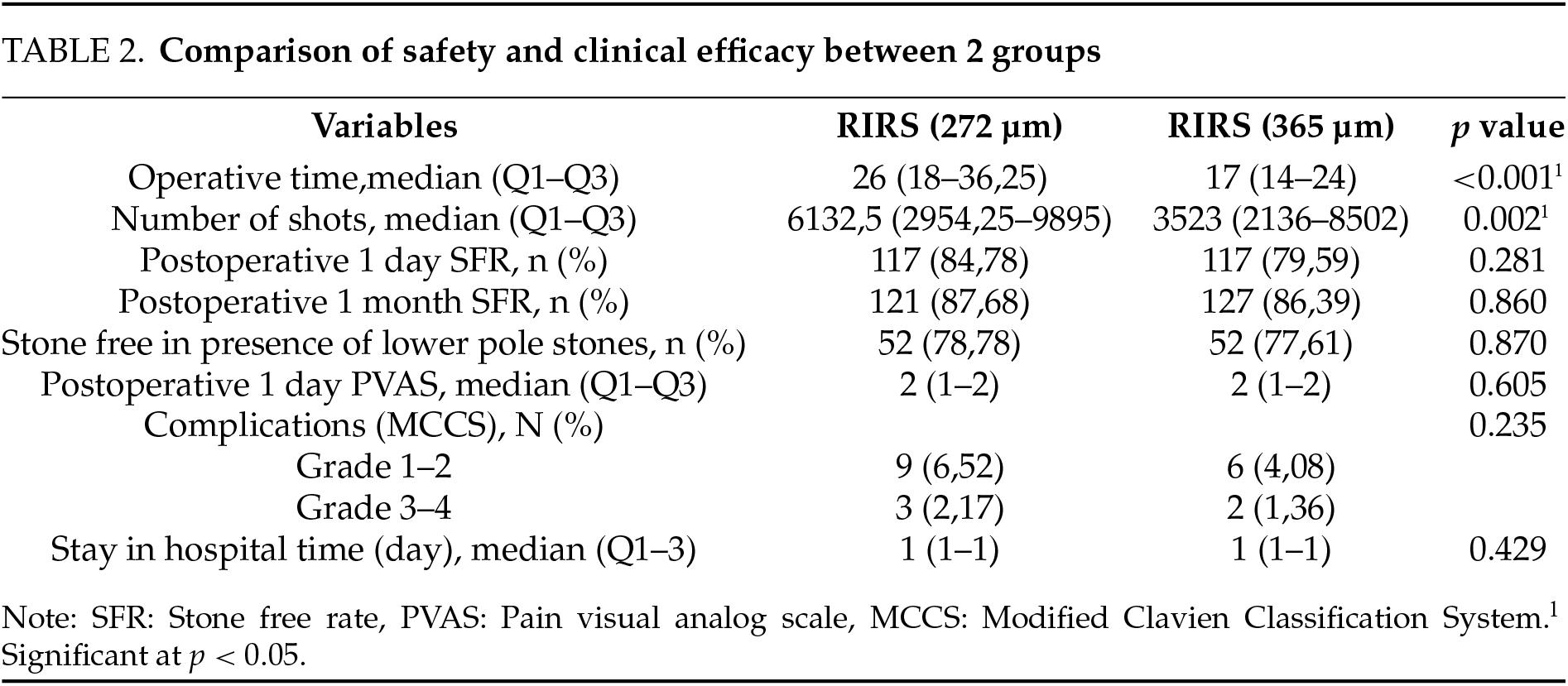
In this study, the medical records of a total of 317 patients who underwent RIRS were reviewed, and 32 patients who did not meet the inclusion criteria were excluded. 272 µm laser was used in 138 patients (Group 1), and 365 µm laser was used in 147 patients (Group 2). Demographic data and stone characteristics for both groups are summarized in Table 1. The demographic data and stone characteristics of the 2 groups were compared, and no statistically significant difference was found. When operation times were compared, it was seen that the operation time was statistically significantly shorter in Group 2, where a 365 µm laser was used (p < 0.001). In addition, the total number of laser pulses was found to be lower in Group 2 than in Group 1 (p = 0.002). No significant difference was observed between the groups in terms of PVAS score, total stone-free rates, stone-free rates in lower pole stones, complications, and hospitalization times. Data regarding the operation results and operation safety between the groups are given in Table 2.

When patients were categorized into two groups—stone-free and those with residual stones—it was found that stone-free rates were statistically significantly lower in patients with multiple stones or lower pole stones (p < 0.001 for both). Additionally, in patients with residual stones, preoperative NCCT revealed significantly higher Hounsfield unit values and larger stone sizes (p = 0.001 and p = 0.002, respectively). No significant differences were observed between the groups regarding preoperative JJ stent placement rates or the presence of hydronephrosis. Furthermore, when the number of cases treated with 272 µm and 365 µm lasers was compared, no statistically significant difference was found between the groups. Data for stone-free patients and those with residual stones are summarized in Table 3.

Finally, multivariate logistic regression analysis was performed to find prognostic risk factors affecting stone-free rates at 1 month postoperatively. The presence of multiple stones, the high HU value of the stone, and the lower pole stones were found to be independent predictive risk factors for postoperative residual stones. (p < 0.001, p = 0.001 and p = 0.029, respectively). Stone size was not found to be an independent risk factor for postoperative residual stones (p = 0.093). Multivariate analysis results are summarized in Table 4.

With the advancements in FU technology, RIRS is increasingly utilized in the treatment of renal stones. As the use of RIRS has become widespread, even in the treatment of renal stones larger than 2 cm, research to increase the effectiveness and safety of the operation has also increased.11 In addition to patient and stone-related factors, factors related to FU and laser devices may also affect postoperative stone-free and complication rates.12 Due to the reduced deflection capacity of FU, the use of conventional 200–272 µm holmium lasers is preferred during the RIRS procedure.7 Previous studies have indicated that the deflection capacity of FU improves as the laser diameter decreases; however, there has been limited attention given to the potential disadvantages of reducing the laser diameter.7,13 The subject of this study is to investigate the effects of changing the diameter of the laser probe, other than the deflection capacity of the device. The primary objective of an ideal RIRS is to achieve high stone-free rates while minimizing complications. Previous studies have reported stone-free rates ranging from 60% to 85% following RIRS.14,15 In our study, stone-free rates using both 272 and 365 µm lasers were found to be similar to the literature. Total complication rates according to the MCCS classification have been reported as 4.8%–20.1% in the literature, and these rates are similar in both groups in our study.7,16 In this study, although the use of 272 and 365 µm lasers was found to have no effect on stone-free and complication rates, there was a significant difference between the operation times of the 2 groups.
One of the most common complications of RIRS is postoperative infection. Previous studies have shown that prolonged operation time increases the risk of postoperative urinary tract infection.17,18 Increased intrapelvic pressure resulting from prolonged surgery may contribute to the elevated risk of infection, potentially due to myelogenous backflow.18 In addition to increasing the risk of postoperative infection, prolonged operation time may also lead to other complications. Studies are reporting that prolonged use of ureteral access sheath (UAS) may impair ureteral blood flow and cause ischemia.19,20 While there is no definitive evidence in the literature linking the use of UAS to ureteral stricture, there is also a lack of sufficient research on long-term outcomes. Özsoy et al. reported in their study that edema and inflammation resulting from 30 min of UAS use resolved within one week, whereas this duration extended to two weeks following 60 min of UAS use.21
The presence of a laser fiber in the working channel of the FU reduces the deflection capacity of the device. The biggest advantage of the small laser fiber diameter is that it reduces the deflection capacity of the device less than larger diameter lasers.22 Especially the easier access to lower pole stones has made thin laser fibers such as 200–272 µm more attractive to surgeons for a long time.7 Moreover, the presence of a thinner laser in the working channel facilitates the flow of irrigation fluid. In cases where the irrigation rate is insufficient to maintain image quality with the 365 µm laser probe, increasing the flow rate by increasing the height of the irrigation fluid or by using an inflatable cuff on the irrigation fluid can resolve this issue.23 A stone basket can also be used to overcome the limitation of the 365 µm laser fiber in accessing the lower pole of the kidney. Huang et al. reported in their study that the relocation of lower pole stones to an appropriate calyx using a stone basket improved the stone-free rate.24 In this study, the effectiveness of 272 and 365 µm lasers in lower pole stones was found to be similar.
This study also showed that fewer laser pulses are required in surgeries conducted with the 365 µm laser compared to those performed with the 272 µm laser. Fewer pulses and shorter surgery times may increase the lifespan of the laser probe. In addition, there are publications in the literature reporting that as the laser gets thinner, the possibility of the laser fiber breaking during deflection increases.7 In this context, the diameter of the laser may also influence the overall cost of the surgery. There are many studies in the literature investigating the factors affecting stone-free rates in RIRS. Resorlu et al. reported in their study that the stone being larger than 2 cm, being in the lower pole, and being multi-calyceal increases the possibility of residual stone.25 In addition to these factors, some studies have reported that an increase in stone density correlates with a higher rate of residual stones.26 In our study, univariate analysis showed that stone size, lower pole location, density, and multi-calyceal nature were factors influencing stone-free rates. As a result of multivariate analysis, it was observed that stone density, lower pole location, and multi-calyceal nature are independent prognostic risk factors for residual stones. Contrary to findings in the literature, multivariate analysis concluded that stone size alone is not an independent risk factor for residual stones. This result is unexpected, as numerous scoring systems designed to predict stone-free rates following RIRS have indicated that larger stone size is associated with a higher rate of residual stones.25,26 However, surgeons increasingly prefer RIRS in the treatment of renal stones larger than 2 cm.27 Therefore, although stone size is an important criterion for the surgeon, it is not the only criterion for treatment modality selection. For example, while RIRS may be preferred for a renal pelvis stone of 25 mm in size, it may be more difficult to make this decision for a lower pole stone of the same size. Sen et al. reported that the presence of multi-calyceal stones was an independent predictive factor for residual stones in pediatric patients undergoing RIRS, but they concluded that there was no statistically significant difference in stone size.28
Our study also had several limitations. First of all, this study was conducted retrospectively. Secondly, the patients’ stone analysis results could not be obtained. The strength of our study lies in being one of the few investigations in the literature examining the effects of holmium laser diameters used in RIRS.
The use of a 365 µm laser in the RIRS procedure significantly reduces the operation time compared to the conventional laser. Even in lower pole stones, the 365 µm laser has similar efficacy to the conventional laser, and the complication rates are also similar. As a result, 365 µm lasers can be used with high efficiency and safety instead of conventional lasers in RIRS.
Acknowledgement
Not applicable.
Funding Statement
The authors did not receive support from any organization for the submitted work.
Author Contributions
Demirhan Demir: Conceptualization, data curation, investigation, methodology, project administration, visualization, writing—original draft, writing—review & editing. Yusuf Gökkurt: Conceptualization, data curation, investigation, formal analysis, visualization. Salih Bürlükkara: investigation, methodology, project administration, visualization, writing—original draft. Turgay Kaçan: Conceptualization, data curation, resources investigation, formal analysis, visualization. Ali Yıldız: investigation, methodology, project administration, visualization, software, supervision. Ufuk Bozkurt: Data curation, methodology, formal analysis, visualization, validation. Tolga Karakan: Conceptualization, methodology, resources, supervision, validation, writing, review & editing. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
Data is not available due to ethical and legal restrictions. Due to the nature of this research, participants of this study did not agree to their data being shared publicly, so supporting data is not available.
Ethics Approval
Ethics committee approval has been granted from Karabük University’s Non-Interventional Clinical Research Ethics Board (Approval No: 2022/988, Date: 30.06.2022) This study was planned following the Declaration of Helsinki. Informed consent was obtained from all patients before the operation day.
Conflicts of Interest
The authors declare no conflicts of interest to report regarding the present study.
References
1. Srisubat A, PotisatS, Lojanapiwat B, Setthawong V, Laopaiboon M. Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst Rev 2014;166(6):CD007044. doi:10.1002/14651858.CD007044.pub3. [Google Scholar] [PubMed] [CrossRef]
2. Türk C, Neisius A, Petrík A et al. EAU guidelines on urolithiasis 2020. In: European Association of Urology Guidelines. 2020 Edition. Arnhem, The Netherlands: European Association of Urology Guidelines; 2020. [Google Scholar]
3. Kim DS, Yoo KH, Jeon SH, Lee SH. Risk factors of febrile urinary tract infections following retrograde intrarenal surgery for renal stones. Medicine 2021;100(13):e25182. doi:10.1097/MD.0000000000025182. [Google Scholar] [PubMed] [CrossRef]
4. Resorlu B, Oguz U, Resorlu EB, Oztuna D, Unsal A. The impact of pelvicaliceal anatomy on the success of retrograde intrarenal surgery in patients with lower pole renal stones. Urology 2012;79(1):61–66. doi:10.1016/j.urology.2011.06.031. [Google Scholar] [PubMed] [CrossRef]
5. Luk A, Geraghty R, Somani B. Endourological options for small (<2 cm) lower pole stones—does the lower pole angle matter? Curr Urol Rep 2023;24(8):365–370. doi:10.1007/s11934-023-01161-w. [Google Scholar] [PubMed] [CrossRef]
6. Mues AC, Teichman JM, Knudsen BE. Evaluation of 24 holmium: YAG laser optical fibers for flexible ureteroscopy. J Urol 2009;182(1):348–354. doi:10.1016/j.juro.2009.02.112. [Google Scholar] [PubMed] [CrossRef]
7. Lu P, Chen K, Wang Z et al. Clinical efficacy and safety of flexible ureteroscopic lithotripsy using 365 μm holmium laser for nephrolithiasis: a prospective, randomized, controlled trial. World J Urol 2020;38(2):481–487. doi:10.1007/s00345-019-02776-w. [Google Scholar] [PubMed] [CrossRef]
8. Sfoungaristos S, Gofrit ON, Katafigiotis I et al. Comparing the efficacy and safety of 365- and 550-μm laser fibers in semirigid ureteroscopic Ho: YAG lithotripsy. Int Urol Nephrol 2015;47(12):1947–1952. doi:10.1007/s11255-015-1130-x. [Google Scholar] [PubMed] [CrossRef]
9. Wang C, Wang S, Wang X, Lu J. External validation of the R.I.R.S. scoring system to predict stone-free rate after retrograde intrarenal surgery. BMC Urol 2021;21(1):33. doi:10.1186/s12894-021-00801-y. [Google Scholar] [PubMed] [CrossRef]
10. Xu Y, Min Z, Wan SP, Nie H, Duan G. Complications of retrograde intrarenal surgery classified by the modified Clavien grading system. Urolithiasis 2018;46(2):197–202. doi:10.1007/s00240-017-0961-6. [Google Scholar] [PubMed] [CrossRef]
11. Pan J, Chen Q, Xue W et al. RIRS versus mPCNL for single renal stone of 2-3 cm: clinical outcome and cost-effective analysis in Chinese medical setting. Urolithiasis 2013;41(1):73–78. doi:10.1007/s00240-012-0533-8. [Google Scholar] [PubMed] [CrossRef]
12. Ozbek R, Senocak C, Haberal HB, Damar E, Sadioglu FE, Bozkurt OF. Comparison of scoring systems for predicting stone-free status and complications after retrograde ıntrarenal surgery. World J Urol 2021;39(7):2741–2746. doi:10.1007/s00345-020-03478-4. [Google Scholar] [PubMed] [CrossRef]
13. Lusch A, Heidari E, Okhunov Z, Osann K, Landman J. Evaluation of contemporary holmium laser fibers for performance characteristics. J Endourol 2016;30(5):567–573. doi:10.1089/end.2015.0600. [Google Scholar] [PubMed] [CrossRef]
14. Chen P, Wei TT, Huang EY et al. Comparison of stone-free rate between percutaneous nephrolithotomy and retrograde intrarenal surgery. J Chin Med Assoc 2023;86(5):485–488. doi:10.1097/JCMA.0000000000000913. [Google Scholar] [PubMed] [CrossRef]
15. Awedew AF, Alemu CT, Yalew DZ. Efficacy and safety of various endosurgical procedures for management of large renal stone: a systemic review and network meta-analysis of randomised control trials. Urolithiasis 2023;51(1):87. doi:10.1007/s00240-023-01459-x. [Google Scholar] [PubMed] [CrossRef]
16. Grosso AA, Sessa F, Campi R et al. Intraoperative and postoperative surgical complications after ureteroscopy, retrograde intrarenal surgery, and percutaneous nephrolithotomy: a systematic review. Minerva Urol Nephrol 2021;73(3):309–332. doi:10.23736/S2724-6051.21.04294-4. [Google Scholar] [PubMed] [CrossRef]
17. Corrales M, Sierra A, Doizi S, Traxer O. Risk of sepsis in retrograde intrarenal surgery: a systematic review of the literature. Eur Urol Open Sci 2022;44:84–91. doi:10.1016/j.euros.2022.08.008. [Google Scholar] [PubMed] [CrossRef]
18. Li T, Sun XZ, Lai DH, Li X, He YZ. Fever and systemic inflammatory response syndrome after retrograde intrarenal surgery: risk factors and predictive model. Kaohsiung J Med Sci 2018;34(7):400–408. doi:10.1016/j.kjms.2018.01.002. [Google Scholar] [PubMed] [CrossRef]
19. Lallas CD, Auge BK, Raj GV, Santa-Cruz R, Madden JF, Preminger GM. Laser Doppler flowmetric determination of ureteral blood flow after ureteral access sheath placement. J Endourol 2002;16(8):583–590. doi:10.1089/089277902320913288. [Google Scholar] [PubMed] [CrossRef]
20. Breda A, Territo A, López-Martínez JM. Benefits and risks of ureteral access sheaths for retrograde renal access. Curr Opin Urol 2016;26(1):70–75. doi:10.1097/MOU.0000000000000233. [Google Scholar] [PubMed] [CrossRef]
21. Özsoy M, Kyriazis I, Vrettos T et al. Histological changes caused by the prolonged placement of ureteral access sheaths: an experimental study in porcine model. Urolithiasis 2018;46(4):397–404. doi:10.1007/s00240-017-1007-9. [Google Scholar] [PubMed] [CrossRef]
22. Baghdadi M, Emiliani E, Talso M et al. Comparison of laser fiber passage in ureteroscopic maximum deflection and their influence on deflection and irrigation: do we really need the ball tip concept? World J Urol2017;35(2):313–318. doi:10.1007/s00345-016-1873-8. [Google Scholar] [PubMed] [CrossRef]
23. Salka B, Bahaee J, Plott J, Ghani KR. Under pressure: irrigation practice patterns during flexible ureteroscopy. Ther Adv Urol 2023;15:17562872231179009. doi:10.1177/17562872231179009. [Google Scholar] [PubMed] [CrossRef]
24. Huang R, Chen JC, Zhou YQ et al. Relocation of lower pole renal stones helps improve the stone-free rate during flexible ureteroscopy with a low complication rate. World J Urol 2024;42(1):30. doi:10.1007/s00345-023-04703-6. [Google Scholar] [PubMed] [CrossRef]
25. Resorlu B, Unsal A, Gulec H, Oztuna D. A new scoring system for predicting stone-free rate after retrograde intrarenal surgery: the resorlu-unsal stone score. Urology 2012;80(3):512–518. doi:10.1016/j.urology.2012.02.072. [Google Scholar] [PubMed] [CrossRef]
26. Xiao Y, Li D, Chen L et al. The R.I.R.S. scoring system: an innovative scoring system for predicting stone-free rate following retrograde intrarenal surgery. BMC Urol 2017;17(1):105. doi:10.1186/s12894-017-0297-0. [Google Scholar] [PubMed] [CrossRef]
27. Ucer O, Erbatu O, Albaz AC, Temeltas G, Gumus B, Muezzinoglu T. Comparison stone-free rate and effects on quality of life of percutaneous nephrolithotomy and retrograde intrarenal surgery for treatment of renal pelvis stone (2–4 cma prospective controlled study. Curr Urol 2022;16(1):5–8. doi:10.1097/CU9.0000000000000071. [Google Scholar] [PubMed] [CrossRef]
28. Sen H, Baydilli N, Ozturk M, Golbasi A, Seckiner İ., Demirci D. Factors effecting the success of retrograde intrarenal surgery in pediatric patients with renal stones: the experience of two tertiary centres with 368 renal units. J Pediatr Urol 2024;20(3):403.e1–403.e9. doi:10.1016/j.jpurol.2024.01.004. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools