 Open Access
Open Access
ARTICLE
Group Psychological Intervention for Children with Hyperactivity Disorder
School of Education and Science, Henan Finance University, Zhengzhou, 450046, China
* Corresponding Author: Ying Xu. Email:
International Journal of Mental Health Promotion 2023, 25(1), 81-97. https://doi.org/10.32604/ijmhp.2022.023720
Received 11 May 2022; Accepted 26 July 2022; Issue published 29 November 2022
Abstract
ADHD is a broad psychiatric disorder that affects children of normal or near-normal intelligence. It is characterized by inattention, hyperactivity, and age-inappropriate impulsivity, and it is often accompanied by learning difficulties, behavioral, emotional, and interpersonal problems. On the other hand, hyperactive tendencies in children with ADHD exhibit ADHD-like behaviors such as lack of self-control, inattention, hyperactivity, and emotional impulsivity. However, because their symptoms are less severe, they do not meet the diagnostic criteria for ADHD but are ADHD or at risk of developing ADHD. The purpose of this study is to alleviate and reduce children’s hyperactivity symptoms by investigating the current situation of the children studied, and systematically intervening and educating children with ADHD through psychological group intervention. Research data shows that ADHD is most commonly diagnosed in school-age children, and in 70%–80% of children with ADHD, symptoms persist into adolescence and 30% into adulthood. Through the use of group psychological intervention in the experiment, the prevalence rate of children with hyperactivity disorder tendency has been effectively reduced. This shows that group psychological intervention training has a significant effect on improving hyperactivity symptoms in children with ADHD tendency.Keywords
ADHD is one of the most common behavioral disorders in children and adolescents. The cause and pathogenesis of ADHD is unclear, and most researchers believe it is a combination of biological, psychological and social factors. The incidence of ADHD varies by culture and geographic location. Epidemiological data from Europe and the United States suggest that the prevalence of ADHD in school-aged children is approximately 3%–7%. In China, the prevalence of ADHD in school-aged children is about 6% and is increasing every year. However, in fact, the occurrence rate of students with attention problems is easy to fall due to the accuracy of diagnostic criteria or diagnostic tools. In 2012, Taiwanese scholars conducted statistics on ADHD children among school-age children and found that the incidence of ADHD accounted for about 1%–9% of school-age children. But it did not include students with learning disabilities with attention problems. Therefore, the actual occurrence rate may be even higher. ADHD is still the case, the proportion of ADHD-prone children in school-age children is only a lot more.
In real life, children with ADHD often exhibit similar behaviors such as poor self-control, bad temper, inattention, hyperactivity, impulsiveness, and inability to empathize with others. However, the degree of the problem is relatively mild, and it does not meet the ADHD screening standards and cannot be diagnosed with ADHD. It is called ADHD-prone children. These children, like children with ADHD, have a variety of problem behaviors in addition to poor attention quality. The specific manifestations are different degrees of school maladaptation. They often have problems such as inattentiveness in lectures, interference in class, many problem behaviors, procrastination in completing homework, falling behind in grades, lacking of patience and persistence in learning tasks, frequent loss of stationery and textbooks, affecting other students, and poor interpersonal relationships. The main place for school-age children to study and live is the school. Maladaptation in school will have a profound impact on the future development of children. If there is no timely intervention and correction, it will develop into a learning disability in senior grades, and academic failure will occur after middle school, high school, and college. In the end, the socioeconomic status and education level of adulthood will be affected, and the work ability and social skills are generally not high. The risk of poor academic and professional performance is also high, placing a huge burden on families and society. Therefore, there is an urgent need to reduce the developmental risk of children with ADHD and to find practical and effective interventions.
This paper studies some techniques of children’s psychological intervention, which can be fully applied to the research in this field. Ana believed that low adherence to cardiac rehabilitation programs is influenced by psychosocial factors, such as the patient’s cognitive and emotional state. Fernandes et al. [1] assessed the impact of short-term inpatient psychological interventions on cognitive and emotional adaptation in patients with ACS. Perricone et al. [2] studied the “Lègami/Legèmi service” initiated by the Italian Society of Pediatric Psychology and carried out a descriptive analysis. Shi et al. [3] compared and evaluates the regulatory effect of comprehensive psychological intervention on the adverse mood and immune status of cancer patients during the perioperative period. Firth et al. [4] aimed to review the evidence on the association between deprivation and dropout in contemporary adult common mental disorder (CMD) psychological interventions. Wu discussed the nursing and psychological intervention methods of deep brain stimulation (DBS) implantation in patients with Parkinson’s disease (PD). Wu et al. [5] aimed to scientifically explore the clinical effect of nursing psychological intervention and improve the quality of life of patients with Parkinson’s disease. These methods provide some references for our research, but due to the short time and small sample size of the relevant research, they have not been recognized by the public.
We optimized psychological intervention studies based on the following relevant information on children with ADHD tendencies. The Assari’s clinical study documented gender differences in affective, behavioral, and cognitive functioning in children with attention deficit and hyperactivity disorder (ADHD) [6]. Arya et al. [7] believed that ADHD is one of the most common disorders in children, and parents complain of being unable to control their children. ADHD is highly comorbid with various psychiatric disorders, further increasing the difficulty of diagnosis and management. The George study learned that one in five (21%) children in the United States has a diagnosable mental, emotional, or behavioral disorder, with attention-deficit/hyperactivity (ADHD) being the most prevalent [8]. Dilek et al. [9] studied neonatal exposure to oxygen in excess of physiological needs that may lead to behavioral problems such as learning disabilities, anxiety, and hyperactivity. The Alice C study demonstrated that a significant proportion of boys with ADHD at an average age of 18 still displayed core symptoms of inattention, impulsivity and hyperactivity, as well as poorer educational, social and psychiatric outcomes than control boys. It includes non-alcoholic substance use disorders [10]. The Sutarmi et al.’s study [11] aimed to determine the effectiveness of Smart Brain Exercise (SBE) and Love Touch Therapy (LTT), and a combination of the two (LTT and SBE), on behavioral changes in children with ADHD. These methods provided sufficient literature support for our study of group psychological interventions for children with ADHD tendencies.
This article is to carry out systematic intervention and training for ADHD-prone children through the study of group psychological intervention for ADHD-prone children. An analysis of data from an experimental study of children with ADHD found that ADHD is most commonly diagnosed in school-aged children. Symptoms persist into adolescence in 70%–80% of children with ADHD and into adulthood in 30%. The main effects of behavioral characteristics were found to be significant regardless of whether the children were members of the group or bystanders. In the experiment, the prevalence of hyperactivity disorder-prone children was effectively reduced through the use of group psychological intervention. This shows that group psychological intervention training has a significant effect on improving hyperactivity symptoms in children with ADHD tendencies.
2 Methods of Group Psychological Intervention for Children with ADHD Tendencies
ADHD is a clinical psychiatric disorder, if not timely treatment and intervention, ADHD children may have a profound negative impact on their school, work and social life. Through the research on children with hyperactivity tendency, this paper adopts the method of group psychological intervention, and systematically conducts intervention and training to relieve and reduce children’s hyperactivity symptoms.
Attention deficit hyperactivity disorder (ADHD) is a group of behavioral and emotional syndromes. It is characterized by inattention, hyperactivity, impulsiveness, irritability and uncontrolled behavior. ADHD can be divided into three subtypes according to the diagnostic criteria of the fourth edition of the American Diagnostic and Statistical Manual of Psychiatry. ADHD type I is dominated by inattention; ADHD type H is dominated by hyperactivity and impulsivity; ADHD type C is a combination of these symptoms [12].
ADHD is more harmful and has more negative effects. It not only affects the healthy development of children, but also causes many troubles to teachers and parents. Attention deficit hyperactivity disorder in children has become a major public health problem in China, but the understanding of it by teachers and parents is still quite backward. Therefore, through epidemiological investigation and interview process, it is not only helpful for early detection of ADHD children, but also helps teachers and parents to understand ADHD-related knowledge and implement effective prevention and intervention measures.
Many ADHD researchers have found that the factors that cause ADHD are not caused by a single factor. It is the result of a combination of factors. Although neurophysiological factors are the decisive factors affecting the prevalence of ADHD. However, in real life, physiological factors and environmental factors interact and influence each other, and it forms the symptoms of ADHD from various paths. By sorting out relevant literature, the following introduces the pathogenic factors of ADHD from biological, psychosocial and other aspects. Biological factors: A large number of studies have confirmed that genetic factors are important pathogenic factors leading to ADHD. Neurochemical studies have found that disorders in the metabolic pathways of monoamine neurotransmitters may be the pathological basis of ADHD. Psychosocial factors: There are many psychosocial factors that induce ADHD patients, including personality factors, family environment, school environment, social environment, etc. [13].
In recent years, research on ADHD has been extremely extensive. In the fields of behavior, cognition and neuroscience, the research on ADHD is extremely rich, and many valuable and meaningful theoretical results have been obtained. On this basis, many researchers continue to summarize and innovate, and establish some highly influential theoretical models. The response inhibition model is shown in Fig. 1 below.

Figure 1: Barkley’s model of response inhibition
Barkley, based on a theoretical synthesis of different models of executive function and functional models of the prefrontal cortex, proposed a model of response inhibition and integrated the results of a large number of empirical studies on response inhibition. This model suggests a link between ADHD and behavioral inhibition, executive function, and motor control [14]. Behavioral inhibition allows the brain to have sufficient room to process information after receiving external stimuli, so that working memory and behavioral execution can be realized. The cognitive energy model is shown in Fig. 2 below.

Figure 2: The cognitive energy model of sergeant
The model suggests that children with ADHD may have varying degrees of impairment at three fundamental levels: cognition, energy mechanisms, and executive control. The main deficit in ADHD lies in the energy system, the control and management system. Also known as a control or judgment mechanism, it involves planning, monitoring, detecting and correcting errors.
Sleep problems/disorders are common in children with ADHD. Sleep is a basic physiological process of the human body. This is a state of reorganization of brain function that is related to the body’s energy reserves and plays an important role in promoting brain development and growth and restoring the body’s strength and energy. Adequate sleep is essential for normal growth and development in children, and adequate sleep patterns play a very important role in the development and maturation of the central nervous system. Sleep is affected by many different factors, including environmental factors, genetic factors, disturbances arising from the interaction of physical growth and development with the environment, and respiratory and neurological diseases. Sleep problems/disorders refer to a variety of abnormal conditions that affect sleep. There are three types of sleep disorders in children: sleep disorders, heterogeneous sleep, and pathological sleep. Sleep disturbances are disturbances in the quantity, quality, and consistency of sleep for a variety of reasons. It is characterized by disturbed sleep and excessive sleep, the former such as difficulty falling asleep, frequent night awakenings, etc. The latter include, for example, OSAHS (obstructive sleep apnea syndrome), narcolepsy, and primary daytime sleepiness. Parasomnias are abnormal events in sleep, such as sleepwalking, nightmares, and night terrors. Morbid sleep refers to sleep disturbances caused by physical or mental illness [15].
Sleep problems/disorders and ADHD are bidirectional. It may manifest in several ways: Sleep problems/disorders may be associated with ADHD-like symptoms. Sleep problems/disorders may exacerbate ADHD symptoms. The body itself has sleep problems/disorders or sleep problems are exacerbated by ADHD. Psychotropic medications used to treat ADHD may contribute to the development of sleep problems/disorders. According to subjective studies, children with ADHD have an extremely high incidence of insomnia, increased problems falling asleep, night and morning awakenings, sleep-disordered breathing, and daytime sleepiness. This objective study using somatosensory devices and polysomnography found that children with ADHD had higher sleep latency, number of sleep transitions, and sleep apnea. And sleep efficiency, sleep duration, and average sleep duration were also lower. So monitoring of sleep can be a good predictor of ADHD.
At present, the diagnosis of ADHD is mainly based on scales and questionnaires, which are not objective enough. In ADHD, this paper uses electroencephalography (EEG) and magnetic resonance imaging (MRI), combining signal processing, bispectral analysis, image processing, and deep learning to study the brain. It also delves into the neural mechanisms of ADHD. The flow chart of the bispectral algorithm is shown in Fig. 3 below.

Figure 3: Flow chart of bispectral algorithm
The bispectrum research algorithm first preprocesses the collected EEG signal, then estimates the bispectrum of the processed signal, draws a two-dimensional EEG bispectrum graph, and records the frequency position of the main peak of the bispectrum. Then, the bispectral image is segmented in this paper, and the area with larger bispectral response is segmented, and the area contained in it is calculated to represent the size of bispectral effective energy. It finally performs a statistical test on the frequency position and the effective energy size to see if there is a significant difference [16].
Assuming that the computer signal sequence m(t) is a zero-mean stationary random process, its third-order autocorrelation function or third-order cumulant can be defined as:
τ1, τ2 represent delay, and E represents mathematical expectation. The bispectral Bm(
There are three general methods for estimating bispectrum: the first is the direct method. It first segments the sampled data, and then uses Fourier transform to obtain spectral estimates of each order. Usually, in order to reduce the estimation error, each segment of data needs to be windowed and smoothed, the second is the indirect method, which firstly estimates the third-order cumulant for the finite-length data, and then obtains its two-dimensional Fourier transform through windowing. The third is the parametric model estimation method. It parametrizes the model by modeling the observed data in an appropriate way, resulting in a bispectrum. The first two methods are called nonparametric estimation methods. In this study, this paper uses the direct method because it is less computationally intensive. The estimation method of the direct method is as follows:
1. It divides the given sample data into K segments, each segment contains X observed sample values, and allows the overlap of two adjacent segments. By subtracting the mean of each segment, a series with zero mean can be constructed [17].
2. It calculates the discrete Fourier transform (DFT) coefficients of each data segment, the formula is as follows:
λ = 0, 1,…, X/2; k = 1, 2,…, K.
3. It uses the DFT coefficients to determine the bispectral estimate for each data segment:
In the formula, L1 represents the number of smooth points, and the selection of Y0 and L1 should satisfy X = (2L1 + 1)Y0.
4. Averaging the bispectral estimation results of each segment to obtain the bispectral estimation average value:
Among them
After bispectrum estimation, the frequency position of the main peak of the bispectrum is recorded, and the bispectrum color image is segmented at the same time to segment the area with larger bispectrum response. It adopts a threshold-based image segmentation method, and the basic steps are as follows:
1. Read in image: It reads the original bispectral color image and converts it into a grayscale image;
2. High-hat transformation and low-hat transformation: High-hat transformation can detect peaks of grayscale images through morphological high-hat filtering, and low-hat transformation can detect valleys of grayscale images through morphological low-hat filtering [18]. Among them, the definition of the top hat transformation operator is:
And the algorithm of low-hat transformation is defined as:
s is the bispectral image, g is the structural element; ° is the opening operation; ⋅ is the closing operation.
3. Enhanced image: It uses the difference between the high-hat image and the low-hat image and inverts it. The formula is as follows:
4. Searching the valley value of the enhanced image.
A neural network (NN) is a very traditional machine learning model that simulates the learning process of the human brain. It builds models based on historical data, automatically combines scattered data, and makes the right decisions for new data. A neural network consists of an input layer, a hidden layer and an output layer. Input and output layers have only one layer, while hidden layers can have multiple layers [19]. The calculation formula of the neuron model is as follows:
In order to realize the nonlinear modeling of the neural network, a nonlinear function needs to be added on the basis of the neural network model. This nonlinear function is called the activation function, and the final result is the result of the nonlinear input.
Commonly used activation functions include step function, sigmoid function, modified linear unit (ReLU), hyperbolic tangent (tanh), etc. The specific expressions of these functions are:
The expression of the step function is:
The sigmoid function expression is:
The expression of the modified linear unit (ReLU) is as follows:
The expression for the hyperbolic tangent function (tanh) is:
Currently, the most commonly used activation functions are the sigmoid function and the ReLU function [20].
When training a neural network, E(w) is determined to measure the variance of training the neural network with the current weight vector w, and obtain the best weights. In the actual neural network training model, the squared error is often used as the error function, and its formula is as follows:
ny is the actual output of the network for the training sample y; ty is the target output (i.e., the label) of the training sample y; D is the sample collection. ty is fixed and ny is determined by the weight vector w, so the error function E is a function of w. The global minimum of E corresponding to w is the target value of w.
In order to reach the minimum value of the error function, it is necessary to descend down the steepest slope to reach the lowest point quickly. This means finding the partial derivative of the error function E(w) with respect to the weight vector w. The gradient descent algorithm works as follows:
1. It first determines the gradient of the error function of the current position, using the following gradient expression:
2. Initializing the weights;
3. The product of the specified step size and the slope of the error function is the distance that must be covered at the current position;
4. Determining whether the gradient descent distance of all weights w is less than the final distance of the algorithm;
5. Updating the parameters, and the update expression is as follows:
The commonly used gradient methods include the traditional decreasing gradient method and the stochastic decreasing gradient method. At present, most neural network models are built with stochastic gradient method, because if the error function E(w) has multiple local minima, the traditional gradient descent method can often solve the local minima problem. The stochastic decreasing gradient method can avoid the local minimum problem more effectively.
Group coaching is a group approach. A facilitator facilitates interaction among group members by building a group where people learn about themselves, explore and accept themselves through observation, learning and experience. It adapts and improves the skills of getting along with others, learns new attitudes and behaviors to get along with others, and improves the ability to adapt.
Group counseling has unique advantages over individual counseling: A group is a microcosm of society. People can model and share common experiences, gain support, develop a sense of belonging and identity, experience good relationships, and develop adaptive behaviors. Central to the therapeutic change that occurs in group counseling is the experience of the nature of the interpersonal process.
Outward Bound training is a form of learning. It empowers individuals and groups to make change by purposefully placing learners in an environment of “challenges,” “adventures,” and “new growth experiences.” It works by presenting learners with seemingly difficult or even impossible tasks. Individuals and groups learn to overcome preconceived notions of their abilities, break through habitual thinking patterns, and enable learning and change.
Outward Bound training can use the outdoor natural environment to carry out activities, and can also use artificial environment to carry out field activities. Wherever the activity takes place, it is about driving the individual or team to complete the task in the process of exploration. Tasks are mainly divided into “problem solving” and “challenge” parts. The purpose is to allow participants to connect and associate with real life or work through the specific shared experience of group activities, and then inspire learning and change.
Group activities are guided by the concept of “challenges” in information learning. In practice, the dissemination and effects of information learning are complemented by “breakthrough” experiences. It provides a practical basis for group activities.
Different from group counseling and counseling, experiential group activities place more emphasis on “experience” and “knowing later”, less emphasis on “reflection” and “sharing”, and its effects are mostly manifested in real life. The groups created in group counseling are not a true microcosm of society, and people are rarely able to live in an environment of complete acceptance and self-disclosure. It is in the environment of interpersonal competition, group pressure, and mutual judgment that we can experience practical problems such as interpersonal communication, competition, and adaptation. Group activities take place in a natural, interactive way. It stimulates deep experience and interaction between people through specially designed activities. It leads to the acquisition of prior knowledge through limited group activities. Once experienced, it invites people to make a real connection, leading to real-life psychological changes.
2.3 Psychological Intervention
Currently, there are pharmacological and non-pharmacological treatments for ADHD. Among drug treatments, central nervous system stimulants are most often recommended. Nonpharmacological treatments include behavioral interventions, parent education, and school-based measures, as well as various treatments such as sensory integration therapy, EEG feedback therapy, and dietary changes. Evidence-based research suggests that central stimulants and behavioral therapy are first-line treatments.
The American Academy of Pediatrics recommends behavioral therapy as the primary treatment for preschool children (ages 4–5) in its 2011 Clinical Practice Guidelines for the Diagnosis, Evaluation, and Treatment of Illness in Children and Adolescents (Diagnosis, Evaluation, and Treatment of Illness in Adolescents). If behavioral methods are ineffective, it is advisable to combine medication with behavioral methods. For school-aged children (ages 6–11), it recommends a combination of medication and behavioral approaches. It recommends that adolescents (ages 12–18) receive medication. For adolescents aged 12 to 18, it recommends medication as the first treatment, supplemented by psychotherapy.
The 2016 edition of Recommendations for the Prevention and Treatment of Attention Deficit Hyperactivity Disorder (ADHD) in China is based entirely on the latest developments in different countries, confirming the importance of comprehensive care, prevention and treatment. To achieve therapeutic goals, it treats children with ADHD in schools and promotes their healthy development. China’s recommendations for the prevention and treatment of attention deficit hyperactivity disorder (ADHD) call for comprehensive pharmacological interventions for children with ADHD, as well as individual, group and family counselling and school-based interventions.
At the 3rd International Conference on Mental Health held in 1946, mental health was defined as “a person’s state of mind attaining the highest level, without conflict with the physical, mental and emotional mental health of others”. A mentally healthy person is defined as: 1. A person who is well-adjusted physically, intellectually, and emotionally; 2. A person who is well-adjusted to the environment and inconspicuous in interpersonal relationships; and 3. A person who has a good sense of well-being. 4. People who can give full play to their abilities to live an effective life in work and occupation. Some researchers believe that mentally healthy people are characterized by: 1. A general sense of security. 2. A comprehensive understanding of oneself and the ability to properly evaluate oneself; 3. Realistic life ideals and goals; 4. The ability to maintain a good connection with the environment; 5. The ability to maintain personality integrity and harmony. 6. Ability to learn from experience; 7. Maintaining good physical fitness and health. 8. The ability to express and control feelings appropriately; 9. The ability to develop individuality within the limits of society; 10. The ability to appropriately meet basic needs within the framework of social norms.
The strong link between forgiveness and mental health is supported by several studies in the fields of counseling and clinical psychology. People who tend to forgive others are more tolerant and have better mental health. The degree of forgiveness affects a person’s subjective well-being. Forgiveness was positively associated with self-esteem and negatively associated with anxiety and depression. The study found that people who did not forgive others and those who did not forgive themselves were associated with indicators of mental illness on the personality scale. It shows that people who are unable to forgive themselves and others are more vulnerable to factors that compromise their mental health.
Another current research topic is examining the relationship between coping styles and mental health. The study found that students’ coping styles of negative stress were significantly positively correlated with their learning difficulties, impulsivity, loneliness and self-harm tendencies. Positive coping styles were significantly negatively correlated with their loneliness and impulsive tendencies. The relationship between forgiveness tendency, coping style and mental health is shown in Fig. 4 below.

Figure 4: The relationship between forgiveness tendency, coping style and mental health
Studies have shown that coping styles as a mediator of stress responses are closely related to mental health, and different coping styles are significantly associated with anxiety and depression. And coping styles can predict the occurrence of negative emotions. Among them, emotional coping can lead to the occurrence and degree of anxiety and depression, while problem coping can reduce the occurrence and degree of anxiety and depression.
Psychobehavioral therapy includes cognitive behavioral therapy, relaxation therapy, self-awareness, functional or situation-based management approaches, and systemic desensitization therapy. Cognitive behavioral therapy: It is a combination of cognitive therapy and behavioral therapy. It emphasizes the important role of cognitive activities in the occurrence and outcome of psychological or behavioral problems. It uses both cognitive and behavioral modification techniques in the treatment process. Relaxation training: Relaxation training has two purposes: one is to relax the muscles, and the other is to relieve the anxiety disorder associated with the child. Self-awareness: It refers to allowing patients to deliberately pay attention to their symptoms by increasing self-awareness, thereby reducing the frequency of hyperactivity. Functional or Context-Based Management Approach: This refers to managing problems in a context-dependent manner, and this intervention is not intended to treat hyperactivity symptoms. Rather, it is to establish a systematic management approach to minimize the occurrence of hyperactivity symptoms. Systemic desensitization therapy: Its main purpose is to slowly expose the child to situations that trigger anxiety or anxiety neurosis and counter this anxiety through relaxation training to eliminate anxiety or fear.
3 Experiment on Group Psychological Intervention for Children with ADHD Tendencies
3.1 Experiments on Children with ADHD
Attention Deficit Hyperactivity Disorder (ADHD) is a common psychological and behavioral problem in children. A 2013 meta-analysis in China found that the overall prevalence of ADHD among Chinese children was 5.7%, including 7.5% in boys and 3.4% in girls, with the highest prevalence in school-aged children.
This study was based on the data of patients with hyperactive or focused symptoms who were first examined in the Department of Psychiatry, Children’s Hospital of Chongqing Medical University from August to October 2015. Doctors surveyed children with suspected multiple diseases and asked their parents and teachers to fill out a questionnaire to assess symptoms.
A total of 292 children with suspected ADHD were included during the study period, and after excluding 73 cases with inaccurate or incomplete data sources, 219 cases were included in the analysis. The distribution of the research subjects is shown in Fig. 5 below.

Figure 5: Case distribution of research objects
It can be seen from Fig. 5 that the median age of ADHD children is 8 years old, of which 7–8 years old are the largest, accounting for 19.7%, and 14–15 and 15–16 years old are the least, accounting for 1.2%. The distribution of male and female subjects by age is shown in Fig. 6 below.

Figure 6: Distribution of male and female subjects by age
From Fig. 6, the gender distribution of ADHD children was 192 males and 27 females. Among them, the largest number of boys is 7 years old and 39 people, and the least is 14 years old and 15 years old, both are 2 people. Among them, the largest number of girls are 6 and 7 years old, both are 5 people, and the least are 12 and 13 years old, both are 1 person.
All 219 cases were recorded by parents and teachers on a separate symptom scale. The parent and teacher symptom scale fills out as shown in Table 1 below.
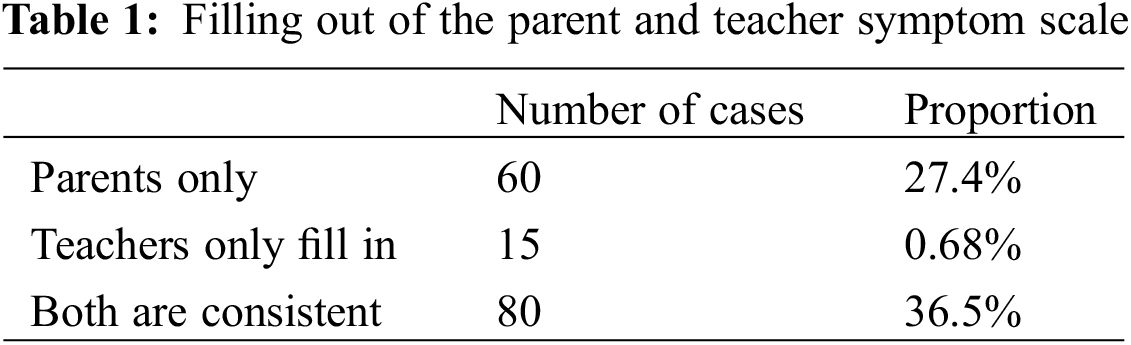
As can be seen from Table 1, when only the parents’ questionnaires met the diagnostic criteria, 60 (27.4%) of the 219 cases met the symptom diagnostic criteria. When only the teacher’s questionnaire met the diagnostic criteria, 15 of 219 cases (0.68%) met the symptom diagnostic criteria. 36.5% of all cases met both criteria.
ADHD is the most common neurobehavioral disorder in children and adolescents and is primarily diagnosed in school-aged children. Symptoms persist into adolescence in 70%–80% of children with ADHD and into adulthood in 30%, and ADHD is thought to be potentially a lifelong disorder. Based on the above experiments, this study found that 87.2% (191/219) of suspected cases were aged 6–12 years. The peak age of consultation was 6–8 years old, accounting for 42.9% (94/219) of all suspected cases.
3.2 Experiments in Children’s Groups
This experiment selected 349 children from a kindergarten (the youngest was 4 years old, the oldest was 6 years old, M = 5.82, SD = 0.38), including 112 in the senior class, 116 in the middle class, 121 in the small class, 177 boys and 172 girls. The sample conditions under the four experimental treatments are shown in Table 2 below:
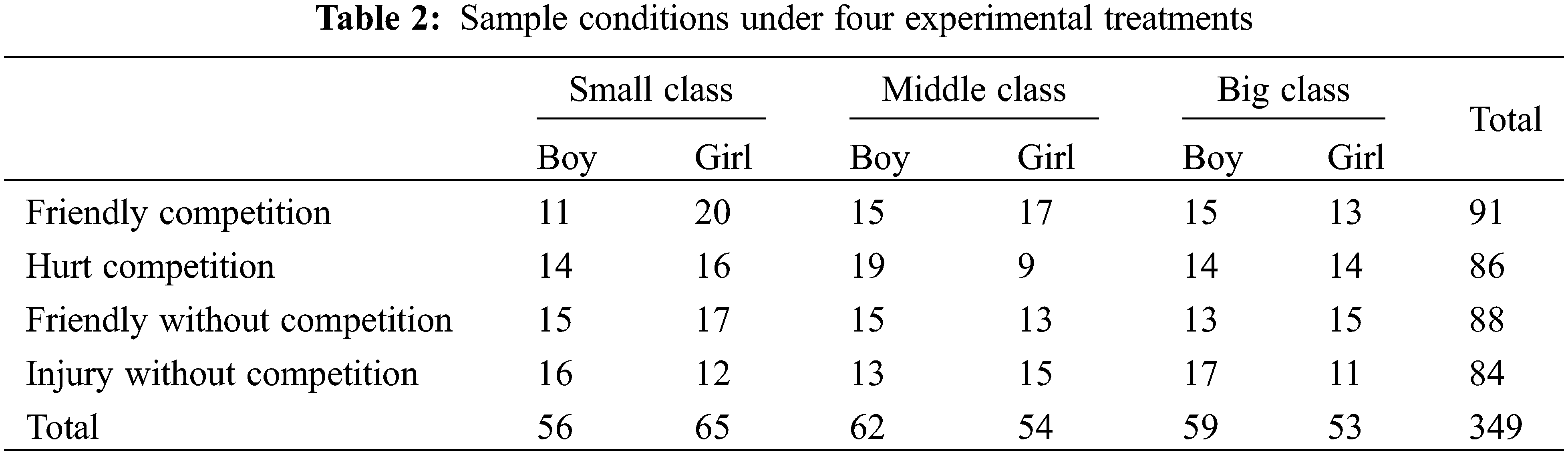
This article selects a quiet place in the kindergarten to conduct one-on-one structured interviews with the above children. In order to understand what kind of predictive judgments 4–6-year-old children will make when facing different social behaviors under different group characteristics, this paper uses group characteristics and behavioral characteristics as operating variables. Age and gender were tested variables, and the selection rate of out-group attribution was performed by multivariate analysis of variance as the dependent variable. The significant results of the analysis of variance among the variables among the subjects are shown in Table 3 below.
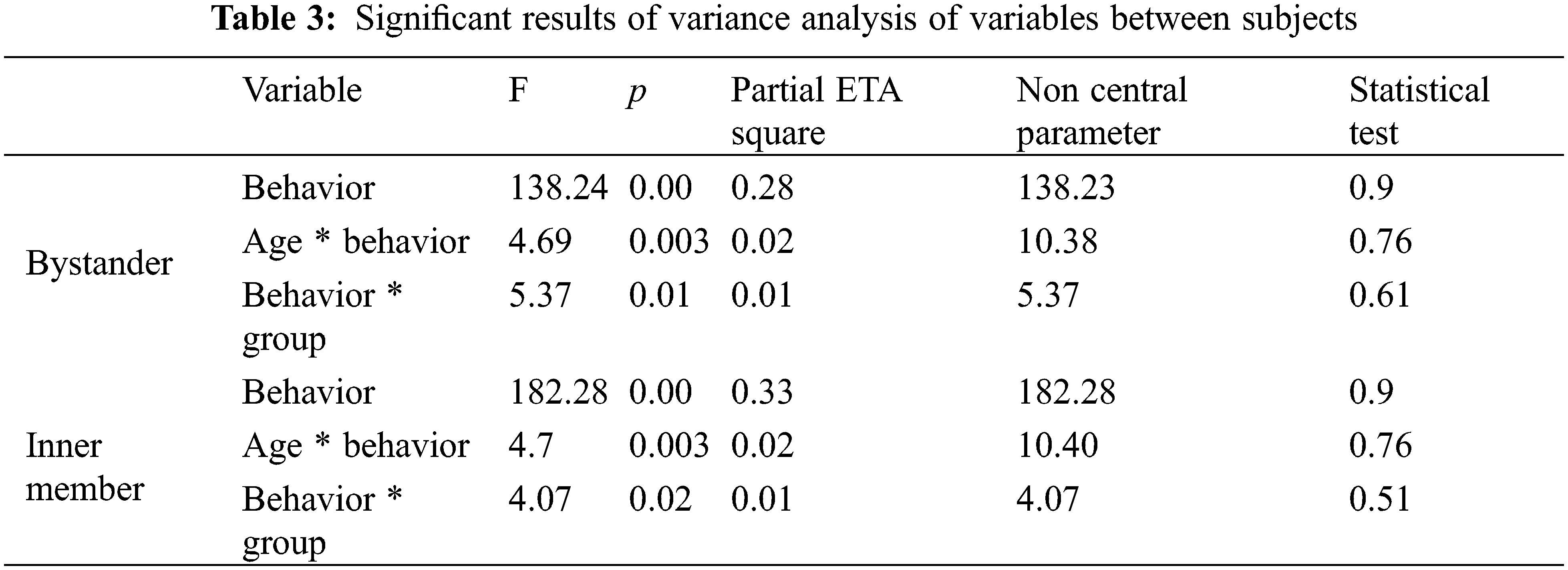
The results of variance analysis in Table 3 show that no matter whether the children are members of the group or bystanders, the main effects of behavioral characteristics are found to be significant (p(side) = 0.00 < 0.001; p(inside) = 0.00 < 0.001). The interaction effect of age and behavioral characteristics was significant (p(side) = 0.003 < 0.01. p(inside) = 0.003 < 0.01), and the interaction effect of behavioral characteristics and group characteristics was also significant (p(side) = 0.01 < 0.05; p(inside) = 0.02 < 0.05). No main effect or interaction effect for gender was found (p(next/in) > 0.05). Specifically, regardless of the child’s status, selection rates for outgroup attribution were higher for children under the condition of hurtful behavior compared with friendly behavior.
3.3 Experiments on Children’s Psychological Intervention
Using “ADHD” as the key word to search in the Chinese Journal Full-text Database, this paper found 1600 related studies from 2010 to 2015, and from 2000 to 2009, there were 1200 related studies on ADHD. Using “ADHD” as the keyword to search its academic trends in the Chinese Journal Full-text Database. After 2000, the academic attention on ADHD showed an upward trend, and after 2005, the academic attention on ADHD became flat, with an average of 201 related studies per year. The academic attention of ADHD in the Chinese Journal Full-text Database is shown in Fig. 7 below.

Figure 7: Academic attention of ADHD in Chinese journal full-text database
In recent years, the related researches on ADHD mainly focus on the etiology, diagnosis, symptoms and intervention of ADHD. The following is a review of interventions based on national literature.
Research on ADHD intervention is a hot spot in ADHD research in recent years. It uses “ADHD intervention” as the key word to search in the Chinese Journal Full-text Database, and the total number of documents from 2005 to 2015 is 392. It can also be seen from the academic trends of the full-text database of Chinese periodicals that after 2005, the research on ADHD intervention has increased year by year, and after 2010, it has shown a steady trend. The academic attention of ADHD intervention in Chinese Journal Full-text Database is shown in Fig. 8 below.
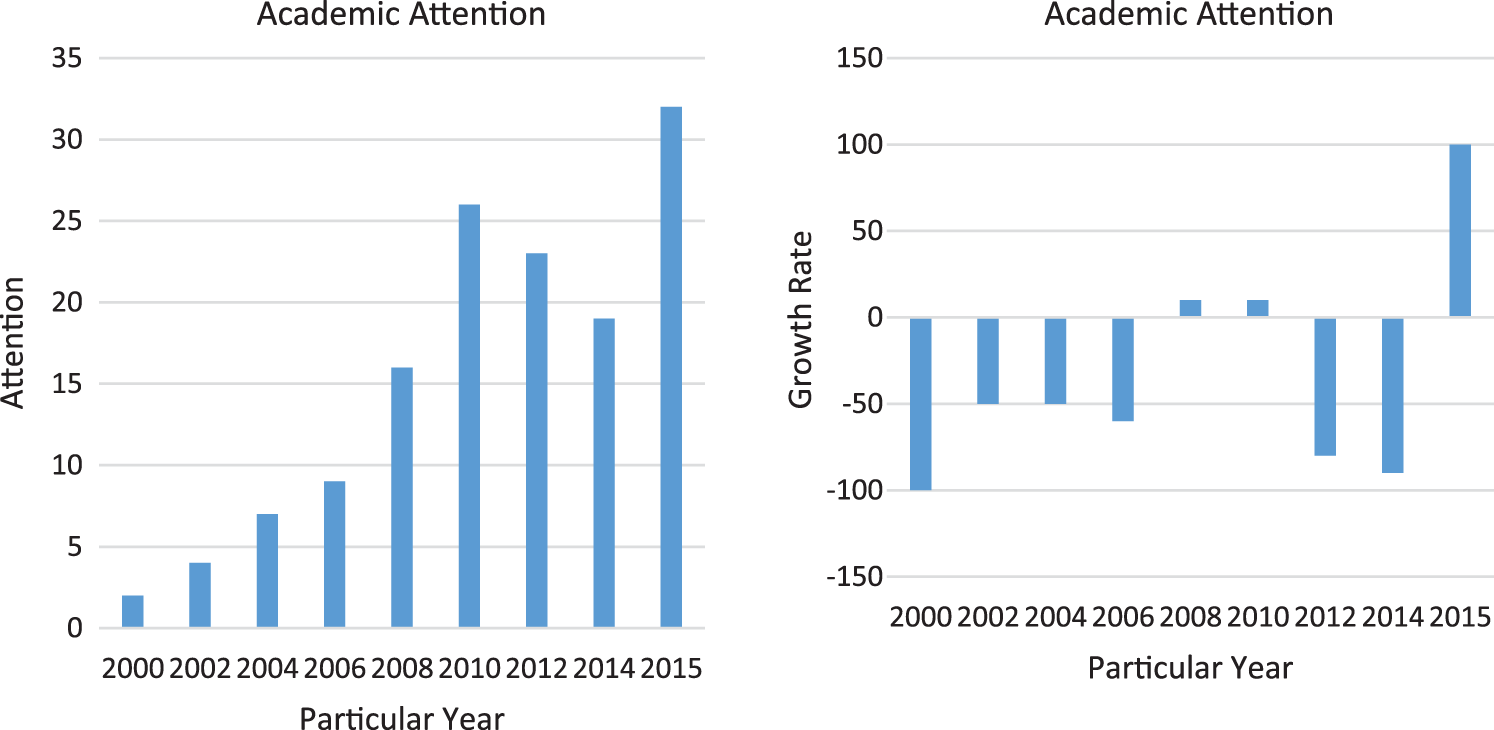
Figure 8: Academic attention of ADHD intervention in Chinese Journal Full-text Database
The types of ADHD intervention research also involve medicine, psychology, education and many other fields. A review of the existing literature shows that the research on ADHD intervention can be divided into drug intervention, biofeedback training, diet and nutrition intervention, psychological-behavioral intervention, and multi-dimensional combined therapy.
By studying the symptoms and causes, family factors, intervention training process and effects of the two cases, this paper discusses which methods in the intervention training of the two cases’ similarities and differences in their symptoms and causes can more arouse the children’s enthusiasm. It includes the influence of changes in family environment and parenting attitudes on the effect of intervention training, the effect of drug treatment plus psycho-behavioral intervention and simple psycho-behavioral intervention on the effect of individual intervention, etc.
The researchers analyzed and summarized the main symptoms of little Y and little Z by observing and recording little Y and little Z, interviewing their parents and teachers, and measuring related scales:
The children’s behavior scale (Parent Questionnaire) and SNAP-IV rating scale were used to evaluate the parents of little Y and little Z. By evaluating the teacher-student rating scales for the head teachers of Xiao Y and Xiao Z, this paper analyzes the results. This article understands the evaluation results of Little Y and Little Z on the Children’s Behavior Scale (Parent Questionnaire), SNAP-IV Rating Scale and their performance in school. The comparison of hyperactivity symptoms in the two cases is shown in Table 4 below.
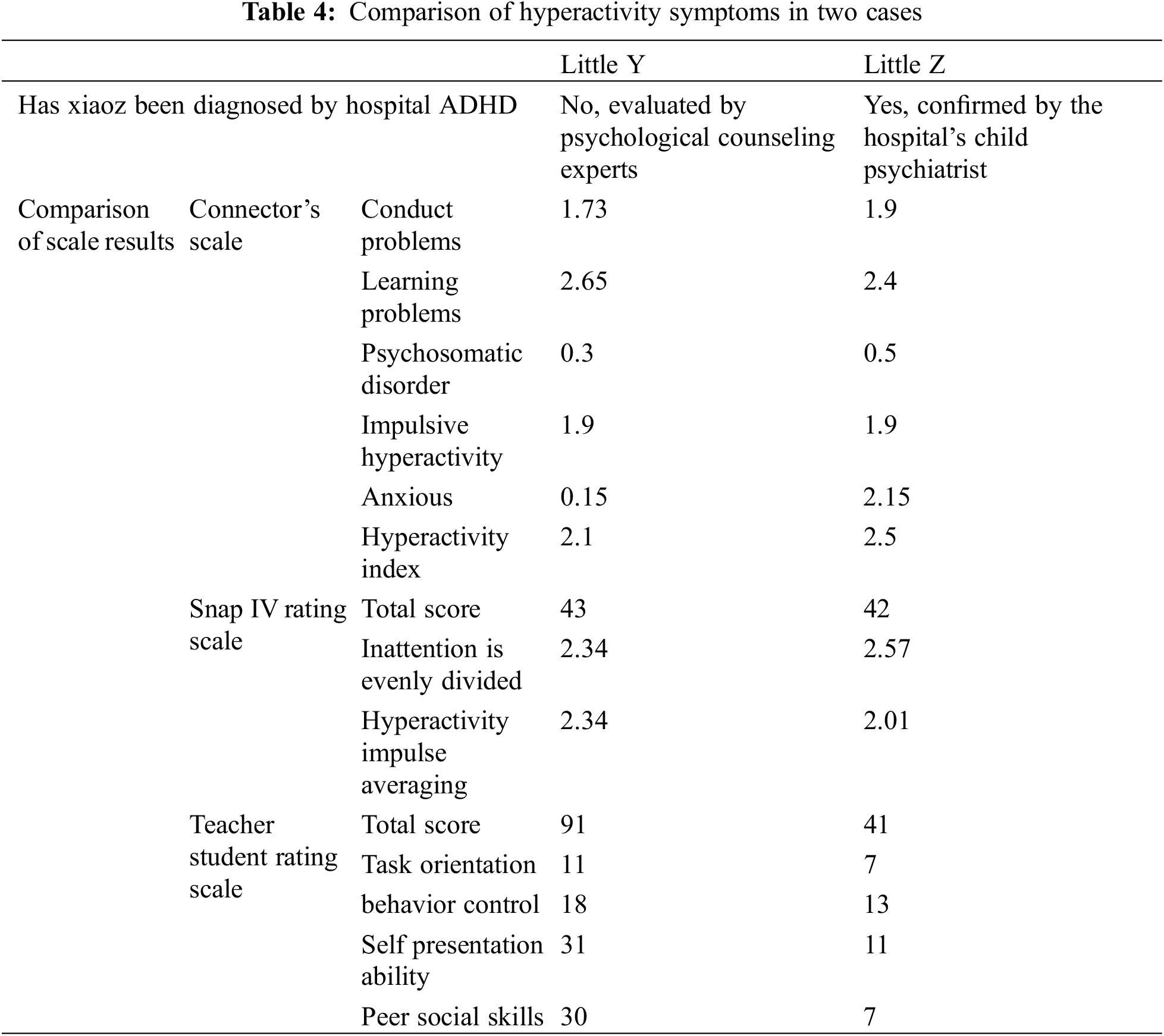
Through the comparison in Table 4, in terms of hyperactivity symptoms, both cases have core symptoms of inattention, hyperactivity, and impulsivity, as well as school problems, criminal behavior, emotional instability, and interpersonal problems. But overall, little Y’s symptoms were milder, while little Z’s symptoms were more severe and complex. Therefore, in the design of intervention, a common intervention program should be designed for common symptoms, and individual intervention programs should be designed for specific symptoms.
After psychological intervention, the hyperactivity symptoms of little Y and little Z improved significantly, and their scores on all four factors (behavioral problems, learning problems, impulsivity-hyperactivity and hyperactivity index) were significantly improved. Attention levels improved, and bad behavior, learning problems, impulsivity-hyperactivity, and anxiety were all reduced. It shows that psychological intervention training has obvious effect on improving the hyperactivity symptoms.
Hyperactivity disorder is a neurodevelopmental disorder common in childhood. There are children in life who behave like children with ADHD but do not meet the diagnostic criteria for ADHD. Because of their minor problems, these children are known as ADHD-prone children. Hyperactivity-prone children also have different degrees of academic problems, inattention, and poor interpersonal relationships. If the behavioral problems of hyperactive-prone children are not effectively paid attention to and intervened, they may develop into ADHD. The family plays a very important role in the growth of children, and the play of family functions also affects the growth of children. This paper uses group psychological intervention to improve the prevalence of hyperactive children. The results of the study show that group psychological intervention training has a significant effect on improving hyperactivity symptoms in children prone to hyperactivity disorder. The research on group psychological intervention for children with ADHD tendency is also of great significance for promoting the development of current psychological intervention.
Funding Statement: The author received no specific funding for this study
Conflicts of Interest: The author declares that they have no conflicts of interest to report regarding the present study
References
1. Fernandes, A. C., McIntyre, T., Coelho, R., Prata, J., Maciel, M. J. (2017). Brief psychological intervention in phase I of cardiac rehabilitation after acute coronary syndrome. Revista Portuguesa de Cardiologia, 36(9), 641–649. DOI 10.1016/j.repc.2017.01.005. [Google Scholar] [CrossRef]
2. Perricone, G., Rotolo, I., Beninati, V. (2021). The lègami/legàmi service—An experience of psychological intervention in maternal and child care during COVID-19. Pediatric Reports, 13(1), 142–162. DOI 10.3390/pediatric13010021. [Google Scholar] [CrossRef]
3. Shi, X., Ma, L., Hao, J. (2021). Regulatory effects of comprehensive psychological intervention on adverse emotions and immune status of cervical cancer patients during the perioperative period. American Journal of Translational Research, 13(6), 6362–6371. [Google Scholar]
4. Firth, N., Barkham, M., Delgadillo, J. (2021). Socioeconomic deprivation and dropout from contemporary psychological intervention for common mental disorders: A systematic review. Administration and Policy in Mental Health and Mental Health Services Research, 49(3), 490–505. DOI 10.1007/s10488-021-01178-8. [Google Scholar] [CrossRef]
5. Wu, L., Ke, Y., Chen, Y. (2020). Nursing, psychological intervention and self-management after deep brain stimulation in Parkinson’s disease. Journal of Behavioral and Brain Science, 10(12), 517–530. DOI 10.4236/jbbs.2020.1012031. [Google Scholar] [CrossRef]
6. Assari, S. (2021). Emotional, behavioral, and cognitive correlates of attention deficit and hyperactive disorder (ADHD) screening and diagnosis history: Sex/Gender differences. Journal of Neurology and Neuromedicine, 6(1), 1–12. DOI 10.29245/2572.942X. [Google Scholar] [CrossRef]
7. Arya, S., Jangid, P., Verma, P. (2019). Psychiatric co-morbidities in attention deficit hyperactive disorder (ADHDA retrospective clinical chart review from a tertiary hospital in North India. Journal of Indian Association for Child and Adolescent Mental Health, 15(1), 39–48. DOI 10.1177/0973134220190104. [Google Scholar] [CrossRef]
8. George, M. (2017). Attention deficit hyperactive disorder (ADHD) impact upon community health from a pediatric endocrine perspective. Primary Healthcare: Open Access, 8(3), 1–5. [Google Scholar]
9. Dilek, M., Orallar, H., Cetinkaya, A. (2019). Can excessive oxygen cause hyperactive behavior disorder in preterm children? Cognitive effects of hyperoxia in the preterm brain of rats. Neurophysiology, 51(5), 1–7. DOI 10.1007/s11062-019-09819-3. [Google Scholar] [CrossRef]
10. Alice, C. (2018). Hyperactive boys grown up. Journal of the American Academy of Child & Adolescent Psychiatry, 57(8), 540–541. DOI 10.1016/j.jaac.2018.05.013. [Google Scholar] [CrossRef]
11. Sutarmi, Kistimbar, S., Nuryanti, E. (2020). Effectiveness of smart brain exercise and loving touch therapy on behavior among children with attention deficit hyperactive disorder (ADHD). Systematic Reviews in Pharmacy, 11(7), 618–625. [Google Scholar]
12. Ahmadi, N., Chaudhry, S., Salam, T. (2017). Trial of positive psychiatry in comorbid attention-deficit hyperactive/disorder (ADHD) with posttraumatic stress disorder (PTSD). Journal of the American Academy of Child & Adolescent Psychiatry, 56(10), S176–S177. DOI 10.1016/j.jaac.2017.09.082. [Google Scholar] [CrossRef]
13. Myers, B., Westhuizen, C. V. D., Pool, M. (2021). Responding to COVID-19 threats to trial conduct: Lessons learned from a feasibility trial of a psychological intervention for South African adolescents. Trials, 22(1), 1–9. DOI 10.1186/s13063-021-05400-8. [Google Scholar] [CrossRef]
14. Yang, Y., Li, Z. (2017). Association between hypertension and emotional disorders: Effect of psychological intervention. Zhonghua Xin Xue Guan Bing Za Zhi [Chinese Journal of Cardiovascular Diseases], 45(12), 1093–1096. [Google Scholar]
15. Rodin, G., Lo, C., Rydall, A. (2018). Managing cancer and living meaningfully (CALMA randomized controlled trial of a psychological intervention for patients with advanced cancer. Journal of Clinical Oncology, 36(23), 2422–2432. DOI 10.1200/JCO.2017.77.1097. [Google Scholar] [CrossRef]
16. Cheng, S., Han, B., Ding, M. (2020). Identifying psychiatric disorder-associated gut microbiota using microbiota-related gene set enrichment analysis. Briefings in Bioinformatics, 21(3), 1016–1022. DOI 10.1093/bib/bbz034. [Google Scholar] [CrossRef]
17. Petker, T., Ferro, M., Ameringen, M. V. (2021). Daily, but not occasional, cannabis use is selectively associated with more impulsive delay discounting and hyperactive ADHD symptoms in binge-drinking young adults. Psychopharmacology, 238(4), 1–11. DOI 10.1007/s00213-021-05781-3. [Google Scholar] [CrossRef]
18. Swetha, P., Ramya, R. (2020). Prevalence of attention deficit hyperactivity disorder among school children at selected schools, Eluru, Andhra Pradesh. International Journal of Research in Pharmaceutical Sciences, 11, 1961–1966. DOI 10.26452/ijrps.v11iSPL4.4404. [Google Scholar] [CrossRef]
19. Mor, D. E., Sohrabi, S., Kaletsky, R. (2020). Metformin rescues Parkinson’s disease phenotypes caused by hyperactive mitochondria. Proceedings of the National Academy of Sciences, 117(42), 26438–26447. DOI 10.1073/pnas.2009838117. [Google Scholar] [CrossRef]
20. Pisula, A., Bryńska, A., Wójtowicz, S. (2020). The change in the intensity of symptoms in children and adolescents with attention deficit hyperactivity disorder after workshops for parents of hyperactive children. Psychiatria Polska, 54(2), 317–332. DOI 10.12740/PP/103618. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools