 Open Access
Open Access
ARTICLE
Effectiveness of Post-Traumatic Growth Intervention to Promote Positive PostTraumatic Traits in Chinese Breast Cancer Patients: A Randomized Controlled Trial
1
Department of Nursing, Zhongda Hospital Southeast University, Nanjing, 210009, China
2
School of Medicine, Southeast University, Nanjing, 210009, China
3
School of Medicine and Dentistry, Gold Coast Campus, Griffith University, Queensland, Q4215, Australia
4
Institute for Integrated Intelligence and Systems, Gold Coast Campus, Griffith University, Queensland, Q4215, Australia
5
Department of Critical Care Medicine, Zhongda Hospital Southeast University, Nanjing, 210009, China
6
Breast Diagnosis and Treatment Center, Zhongda Hospital Southeast University, Nanjing, 210009, China
7
Department of Oncology, Zhongda Hospital Southeast University, Nanjing, 210009, China
* Corresponding Authors: Jing Sun. Email: ; Cuirong Xu. Email:
International Journal of Mental Health Promotion 2023, 25(10), 1089-1102. https://doi.org/10.32604/ijmhp.2023.030526
Received 08 April 2023; Accepted 20 June 2023; Issue published 03 November 2023
Abstract
Objective: The purpose of this study was to evaluate the effectiveness of post-traumatic growth (PTG) model-based intervention to improve positive psychological traits in Chinese breast cancer patients. Design: A randomized control trial of a psychological group intervention based on PTG model. Methods: The Clinical Trial was registered on 17 August 2019 at Chinese Clinical Trials.gov with Registration number ChiCTR1900025264. A total of 92 patients with breast cancer were recruited. The participants were randomly assigned to the experimental group (n = 46) and the control group (n = 46). A six-session psychological group intervention based on PTG model was implemented in the experimental group, and a six-session health education was implemented in the control group. The outcomes were measured at baseline (pre-intervention), 3 weeks, 6 weeks after the intervention. The primary outcome was posttraumatic growth assessed by the Chinese version of the Post-Traumatic Growth Inventory (PTGI); Secondary outcomes included psychological resilience, family resilience, rumination, and self-disclosure. Results: A total of 87 patients with breast cancer completed this study, including 44 patients in the experimental group and 43 patients in the control group. There was no significant difference in baseline data of breast cancer patients between the two groups except for the treatment regimen (p > 0.05). The two groups were compared after the intervention; the interaction effects between the total scores of posttraumatic growth, family resilience, and self-disclosure and the time term were statistically significant (p < 0.05), indicating that the trend of change in total scores of post-traumatic growth, family resilience, and self-disclosure differed between the experimental and control groups over time, and the scores improved in the experimental group were significantly higher than those in the control group. The comparison of psychological resilience and total score of rumination at each time point was statistically significant (p < 0.05), indicating that group intervention based on the PTG model could improve the psychological recovery ability and rumination level of the experimental group. Conclusion: The psychological group intervention based on the PTG model significantly improved post-traumatic growth, family resilience, and self-disclosure in patients with breast cancer. However, the impact on psychological resilience and rumination was relatively small. Long-term intervention is needed to further test the effect of the PTG model on psychological resilience and rumination.Keywords
In women, breast cancer is the most commonly diagnosed cancer (11.7% of total cases). According to the data from International Agency for Research on Cancer, there were about 19.29 million new cases of cancer worldwide in 2020, of which there were about 2.3 million new cases of breast cancer, which has surpassed the incidence of lung cancer and is also the fifth leading cause of cancer death worldwide. From the perspective of development trends, the incidence of breast cancer is still on the rise in most countries or regions worldwide [1]. An earlier median age of onset suggests that more women have breast cancer at younger ages in China. Consequently, patients require longer follow-up and treatment periods and have fewer healthy life years, thus increasing the disease burden for both individuals and society. In China, breast cancer is the cancer type with the highest incidence in women, with 416,371 new cases and 117,174 deaths in 2020, accounting for 18% of new cases and 17% of deaths worldwide, respectively [2].
Cancer diagnosis and treatment can give rise to considerable mental health issues for individuals, such as anxiety and depression. Compared with healthy populations, cancer patients are at a higher risk of mental health problems. According to previous systematic estimation of cancer prevalence in China, 15.8% of cancer patients had clinical symptoms of mental disorders, with depression, anxiety, psychotic symptoms, and stress-related disorders accounting for 13.3%, 10.2%, 2.8%, and 1.4%, respectively. Left untreated mental health problems in cancer patients can lead to destructive consequences, including decreased treatment adherence, decreased survival rate, increased healthcare cost, and poor quality of life [3]. However, in the face of this major traumatic event, a higher proportion of breast cancer patients still report positive changes in their disease background, mainly reflected in Post Traumatic Growth (PTG) [4]. Breast cancer is a disease that includes not only physical parts but also mental parts. So far, the psychological desire has been ignored by paying attention to the patient’s physical crisis. PTG is the forward growth psychology of humans after trauma. This changes the direction of research focused on negative psychology after trauma to positive trauma after trauma. PTG is a positive change resulting from fighting an extremely challenging life crisis [5]. PTG not only brings more hope for breast cancer patients to overcome the disease but also changes the patients’ perception of cancer, reduces their negative emotions, and enables them to better receive relevant treatments. Recently, research [6] related to post-traumatic growth and group intervention also shows that this intervention model is suitable for breast cancer patients and can help breast cancer patients reduce anxiety and depression, but does not take into account the patient’s psychological resilience, family hardiness, and event-related ruminant meditation.
PTG model was first proposed by Tedeschi and Calhoun in 1996 [4]. The positive post-traumatic trait is defined as an individual’s struggle with traumatic or challenging life events that produce positive psychological changes beyond previous functions [4]. PTG includes the following five aspects: appreciation for life, relating to others, personal strength, new possibilities, and spiritual growth. PTG is different from resilience, and the PTG is looking beyond the previous state and is not prepared to return to the normal state after trauma. Evidence from the cancer diagnosis and medical experience increases that individuals can express PTG. Given the evidence suggesting that PTG reflects positive psychological change and resilience among cancer survivors, opportunities exist for developing, testing, and implementing evidence-based interventions to promote PTG as an important part of survivorship care [7]. Previous studies have shown that resilience is a positive factor for PTG in breast cancer patients [8]. The resilience model believes that individuals with high levels of resilience have four intellectual resources: control, openness to experience, reflective attitude, and emotional regulation [9]. Patients with high-level resilience are more inclined to challenge adversity and demonstrate cognitive flexibility. The higher level of resilience, the more interest patients have in learning new ideas and experiences. Broadly speaking, resilience is a trait that enables a person to function optimally despite failures. It is an ability to stay away from negative experiences; it is a type of positive adaptation associated with trauma. Experts underscore the significance of developing resilience during a lifetime. This competence is essential in overcoming difficulties in life, stress, or traumas [8].
Rumination is a cognitive processing style after an individual experience a traumatic event and includes two types: intrusive and purposive rumination [10]. The study shows that there is a positive correlation between purposive rumination contemplation level and PTG level in breast cancer patients [11]. The higher the rumination level, the more likely the patients tend to actively think about the significance of cancer to themselves, and achieve self-regulation to correctly face the condition, adapt to changes in the condition, help them maintain a relatively positive emotional experience in traumatic events, and produce positive cognitive changes. It is suggested that clinical medical staff should carry out psychological interventions to help breast cancer patients change from invasive rumination to purposive rumination and improve their PTG levels.
Self-disclosure is another important factor affecting PTG levels in breast cancer patients [12]. Self-disclosure can help breast cancer patients vent their emotions, eliminate annoyance, maintain psychological balance, and improve their PTG level. Self-disclosure can enhance self-awareness ability, enhance individual self-knowledge, help focus attention on positive emotional gain and promote changes in interpersonal relationships. At the same time, positive feedback from the listener can also help the venting person enhance personal strength and re-appreciate life [13]. It is suggested that a safe self-disclosure environment should be created for breast cancer patients in clinical nursing practice to improve their self-disclosure willingness to promote their positive psychological adjustment and obtain more growth. A large number of studies have shown that PTG model-based interventions are beneficial for improving the mental health and quality of life in breast cancer patients. The forms of PTG model intervention include individual intervention and group intervention. Calzone and colleagues compared the effects of group intervention and individual intervention on breast cancer patients in education counseling and stress management and concluded that both PTG modes of intervention methods had the same final effect, with a higher efficiency in group intervention [14,15]. Due to its high efficiency, good follow-up effect, and wide range of adaptation, PTG model-based group interventions become an emerging intervention model to improve PTG in breast cancer patients. However, some research interventions have not been exhaustive or lacked a theoretical framework in the literature. Even within the group intervention technique, the content and activities of intervention from individual studies are not the same, which may affect the effectiveness of the intervention program. Thus, the quality of the interveners is inconsistent across studies. Furthermore, previous studies did not consider different traumatic events which may influence individual traits of resilience in breast cancer patients [7]. Individuals with different levels of resilience show different adaptive abilities when confronting the same major stress event.
This study aimed to address these research gaps by assessing the effects of PTG model-based intervention on the improvement of PTG in Chinese breast cancer patients. The group-based PTG intervention was conducted to promote five domains of positive after-traumatic traits. First, the PTG model [16] and positive psychology theory [17] were adopted to provide a general framework for the formation and development of intervention. The multidisciplinary team’s intervention strategies for PTG of breast cancer patients are divided into four themes: promoting emotional expression, transforming negative emotions, reducing disease uncertainty, and developing new values. Finally, we modified the initial intervention program through expert meetings to ensure that all information was included in the evidence-based intervention. It is hypothesized that PTG and PTG-related protective factors are significantly improved in breast cancer patients in the intervention group compared to the control group, and the proposed post-intervention protective factors in this study include resilience, rumination, and self-disclosure.
The study is a two-armed cluster randomized controlled trial in the breast diagnosis and treatment center of Zhongda Hospital Southeast University and Jiangsu Cancer Hospital. Before the trial, the possible risks and benefits of the trial were explained to patients in detail, and patients were asked to sign the informed consent form. To avoid contamination of the intervention between the experimental and control groups, subjects attending the same hospital will be uniformly assigned to either the experimental or control group. Due to the particularity of psychological intervention, it is impossible to achieve measurer blindness, so this study is single-blind, that is, subject blindness. A psychological group intervention based on PTG model was used in the intervention group, and health education activity was conducted in the control group. The PTG-based intervention was conducted over six weeks. The outcomes were measured at 3-time points: baseline (pre-intervention), 3 weeks, 6 weeks. The intervention was designed and reported as RCTs following the SPIRIT 2013 Statement guidelines. The study protocol was approved by IEC for clinical research at Zhongda Hospital, affiliated with Southeast University (Ref no. 20190117). The trial was registered on 17 August 2019 at Chinese Clinical Trials.gov (ChiCTR1900025264).
Patients who met the following criteria were included in the study: (1) Female patients diagnosed with breast cancer by pathological diagnosis; (2) Aged 18–65 years; (3) Had normal comprehension and expression skills; (4) Had access to a telephone or mobile phone; (5) Informed consent and voluntary participation in this study. Patients who had other severe diseases had mental illness or cognitive and communication impairments, or had received other psychological interventions were excluded from the study. The calculation formula for the comparison of two sample mean values is based on a completely random design.
Measures experimental and control conditions
Participants in the experimental group received intervention based on the PTG model delivered by a multidisciplinary team plus health education. A breast cancer group psychological intervention research team has been formed, mainly comprising 13 members of the multidisciplinary medical and nursing team (2 oncology nurses, 1 psychological counselor, 2 breast surgeons, 1 medical oncology radiotherapy team doctor, 1 medical oncology chemotherapy team doctor, 1 chronic disease management specialist, 1 breast surgery nurse manager, 3 medical oncology nurse managers, 1 psychology nurse manager) and 2 postgraduate students (with a national level 3 psychological counselor qualification, 3 months’ rotation in the psycho-psychiatry department as a specialist and several times in the department’s psychotherapy workshops). The director of the nursing department was responsible for coordinating the allocation of team members and quality control of intervention programs; the nurse from the breast diagnosis and treatment center was responsible for recruiting breast cancer patients. Other team members were responsible for the implementation of different intervention-theme meetings and group psychological games. The postgraduate student was responsible for preparing the audio, video, course materials, and group game tools required for intervention. The research team leader and researchers trained the team members in the form of lectures, workshop interaction, etc. At the same time, the PPT, audio, video, and other relevant information on the intervention content were sent to the person in charge of the corresponding subject in the form of an e-mail one week before the intervention, and the person in charge of the corresponding subject was communicated offline three days before the intervention to make the final modification and improvement.
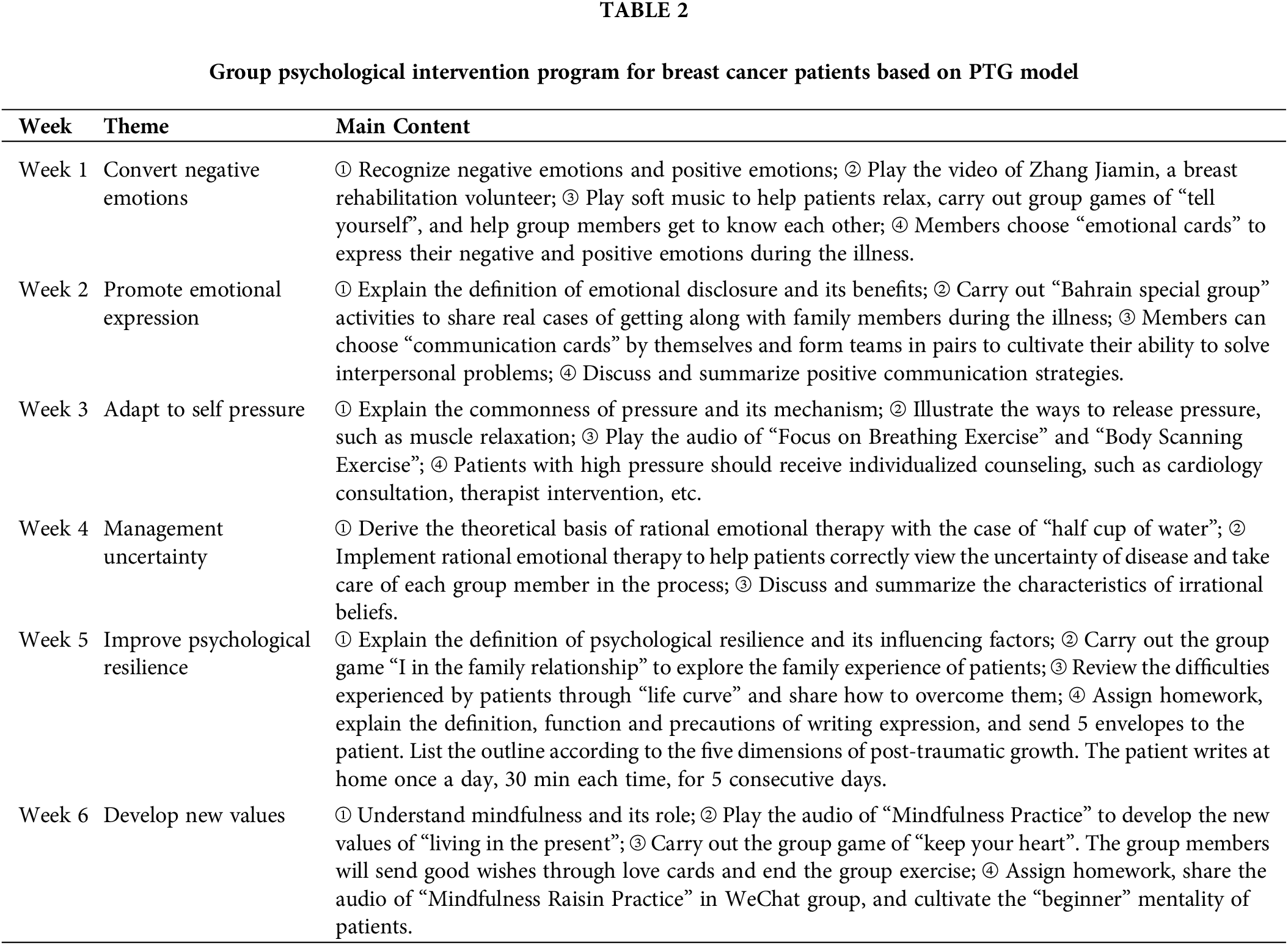
The experimental intervention was based on the Socioecological PTG model that focused on the promotion of PTG, resilience, rumination, and self-disclosure. The intervention was divided into 2 parts, health education and group psychological intervention based on the PTG model. In the health education part, the breast cancer group psychological intervention research team established by this study gave lectures, and the health education courses for breast cancer patients are 15 min each time, once a week. The intervention section was carried out after the health education section. The specific intervention activities are described in Table 1 below. In the group psychological intervention based on the PTG model part, The breast cancer patients in the experimental group were divided into 6 group psychological support groups based on the factors such as an address, tumor stage, and treatment plan, and 7–8 people in each group. The contents of the group psychological intervention included: (1) Theoretical exposition of positive psychology-related topics in breast cancer; (2) Cognitive-behavioral psychological strategies to achieve the goals related to psychosocial adjustment of breast cancer patients; (3) Encouraging patients to participate in group discussions on meeting topics. The intervention frame and the intervention activities are described in Fig. 1 and Table 2 below. The head of the research team timely spot-checked the familiarity of the team members with the intervention content to ensure the quality of the group’s psychological intervention.
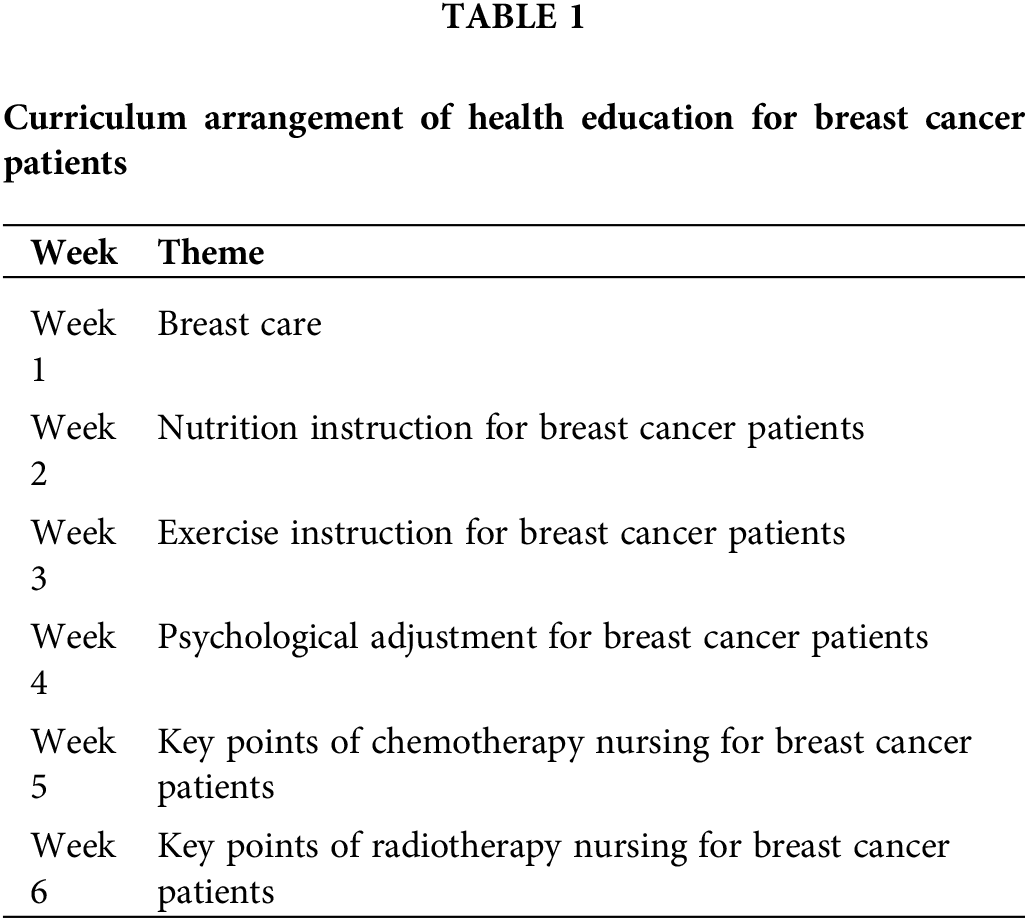
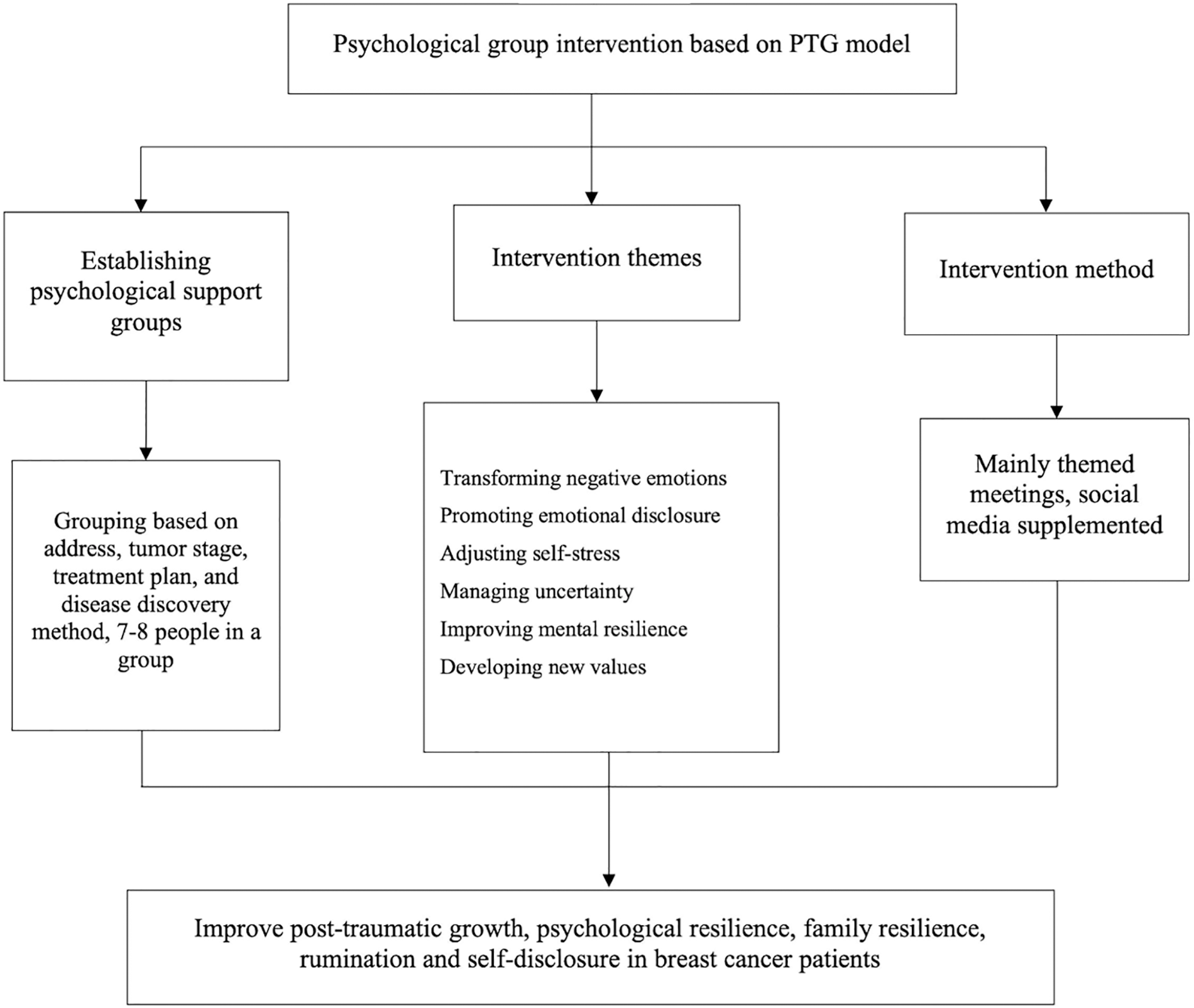
Figure 1: Group psychological intervention frame for breast cancer patients based on PTG model.
To ensure patients’ participation in the study, researchers went to the bedside to remind hospitalized patients and notified home patients in the social media group or contacted the patients by phone when patients failed to respond. The research team gave the research object certain material rewards and expert consultation opportunities and encouraged the patient to participate in the whole process; At the same time, a WeChat group was established to timely push the audio of breast cancer-positive psychology-related exercises, to improve the enthusiasm of patients to participate in the intervention program.
Participants in the control group received the same health education provided by the multidisciplinary team as those in the experimental group. They received group-based health education once a week for 6 weeks, including information on breast self-tests, diet, medications, functional exercises, chemotherapy self-care instruction, and radiation therapy self-care instruction. The specific intervention activities are described in Table 1 below.
Demographic and clinical variables
The general condition questionnaire was designed by the members of the study group which included two parts: demographic data and clinical characteristics. The self-reported demographic characteristics obtained included age, body mass index (BMI), education level, religion, marital status, current work status, annual family income, and payment methods. The clinical characteristics included cancer stages, type of treatment (surgery, chemotherapy, radiotherapy, and endocrine therapy), the time course of the disease, surgical site, the existence of recurrence, and metastasis.
Posttraumatic growth inventory, PTGI
Individual positive posttraumatic changes were evaluated by the Chinese version of the Post-Traumatic Growth Inventory (PTGI) [19]. There were 21 items in total, including the five dimensions of personal strength, new possibilities, relating to others, appreciation of life, and spiritual change. It was arranged on a five-point scale ranging from 0 (I did not experience this change as a result of my crisis) to 5 (I experienced this change to the highest degree as a result of my crisis). The total scores were 0 to 105 points. Higher scores indicated a higher level of PTG. The overall Cronbach’s α coefficient of PTGI was 0.930, the Cronbach’s α coefficient of each dimension was 0.817–0.864, and the structural validity was 0.90.
Connor-davidson resilience scale, CD-RISC
The resilience level was measured with the Chinese version of the Connor-Davidson Resilience Scale (CD-RISC), which had 25 items that assessed individual psychological resilience. It included 3 domains of resilience: hardiness, self-reliance, and optimism. It was arranged on a four-point Likert scale ranging from 0 (not at all) to 4 (extremely) [20]. The total scores were 0~100 points. Higher scores indicated a higher level of individual resilience. The Cronbach’s α coefficient was 0.90, and the content validity was 0.90.
The Chinese version of the Family Hardness Index (FHI) was used to measure the level of family hardiness, which includes three domains of family resilience: coherence, coping, and control, with a total of 20 items. Items 1, 2, 3, 8, 10, 14, 16, 19, 20 are reverse scoring questions. Each item assesses family resilience on a 4-point Likert scale ranging from 1 (strongly agree) to 4 (strongly disagree) [21]. The total score ranged from 20 to 80. Higher scores indicate higher levels of family resilience. Cronbach’s alpha coefficient for FHI was 0.803.
Event related rumination inventory, ERRI
Levels of rumination were assessed using the Chinese version of the Event-Related Rumination Inventory (ERRI) [22]. Individuals’ cognitive processing ability to stressful events was evaluated according to their meditation frequency for a certain period (last 2 weeks), and the questionnaire consists of 20 items, including two dimensions: intrusive rumination and purposive rumination. Using the Likert 4-level scoring method, 0 = never had this idea, 3 = often had this idea, with a total score of 0 to 60 points, and the higher the score, the higher the frequency of rumination contemplation. Cronbach’s α coefficients were 0.92 for the total scale and 0.93 and 0.85 for each dimension.
Distress disclosure index, DDI
The Chinese Distress Disclosure Index was used to assess the patients’ level of self-disclosure [23]. The scale consists of 12 items arranged on a 5-point scale ranging from 1 (not at all) to 5 (extremely), with a total score of 12 to 60. The higher score indicated a higher degree of self-disclosure. The Cronbach’s α coefficient of the scale was 0.866, the split-half correlation coefficient was 0.847, and the test-retest reliability was 0.780.
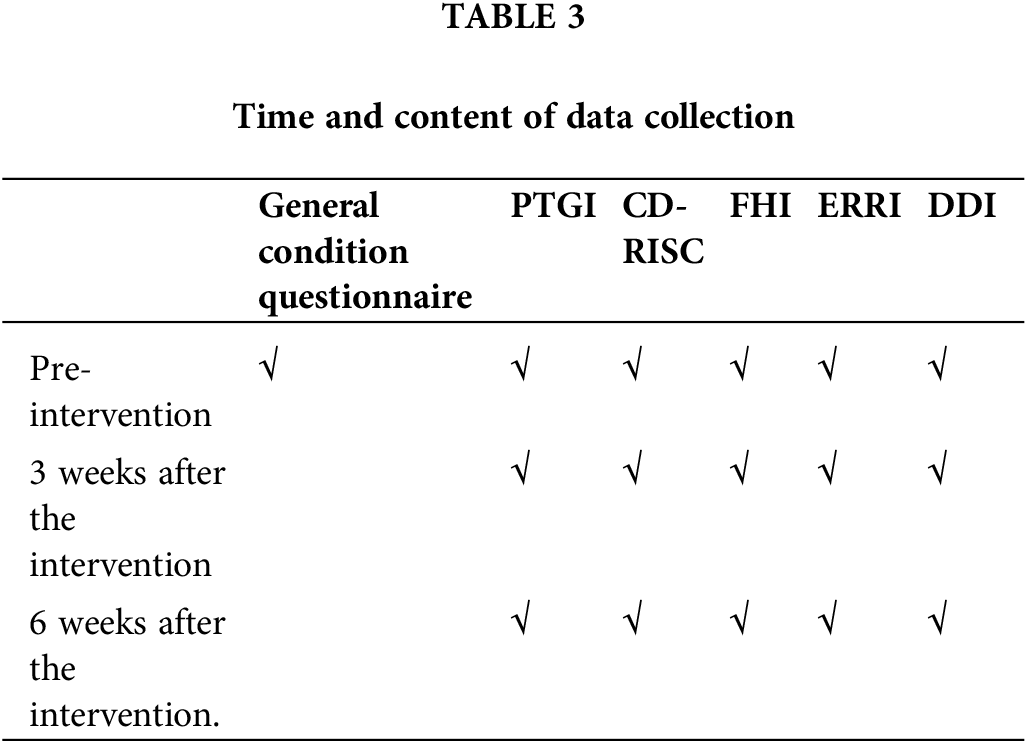
This study considers not only the impact of the intervention on the level of PGI in breast cancer patients but also secondary outcome measures, including psychological resilience, family resilience, rumination, and self-disclosure. The general condition questionnaire, including demographic and clinical variables, was collected at baseline; mental health-related scales were repeated at baseline (before intervention), 3 weeks, and 6 weeks after intervention in the experimental and control groups. Data were collected through questionnaires and interviews. The researcher uniformly trained data collection personnel to ensure the homogeneity of data collection standards. Before the collection, the researcher himself explained the filling requirements using unified guidance; For the research objects that cannot be filled in independently, the researcher used interviews to understand their real ideas. After collection, the researcher reviewed the completeness and logic of the completed questionnaire. If there was any missing or obvious logical error, the researcher would return to the research object to fill in or modify it. After checking, the questionnaire would be withdrawn again. The specific time and content of data collection are shown in Table 3.
Epidata 3.0 was used for double entry of data, and SPSS 20.0 was used for statistical description and statistical analysis of data, with α = 0.05 as the test level. Normally distributed measurement data were expressed as 'x ± s, skewed distribution measurement data were expressed as M (P25, P75), and enumeration data were expressed as frequency and constituent ratio. Chi-square test, independent sample t-test, or Mann-Whitney U-test were used to compare the general data of the experimental group and the control group, and single-factor analysis of variance and repeated measurement analysis of variance were used to compare the measurement data of the experimental group and the control group.
During the 6-week trial period, 2 cases in the experimental group were unable to participate in the follow-up study due to exacerbation of the disease; 3 cases in the control group refused to participate in the follow-up study. Therefore, 87 cases were finally included in this study, including 44 cases in the experimental group and 43 cases in the control group, which met the sample size requirements of this study.
Comparative analysis of baseline data
The study finally included 87 patients with breast cancer, with an average age of (54.00 ± 9.90) years in the experimental group and (49.53 ± 11.08) years in the control group. Education level: in the experimental group, 52.27% were junior high school and below, 22.73% were senior high school/technical secondary school, and 25% were junior college and above; In the control group, 51.16% were junior high school and below, 18.61% were senior high school/technical secondary school, and 30.23% were junior college and above. Marital status: 95.45% of the experimental group were married; The control group was 100% married. Current working status: 31.82% of the experimental group are in service, and 68.18% are retired or never employed; In the control group, 37.21% were employed, and 62.79% were retired or never employed. The course of disease: in the experimental group, 84.09% were less than 1 year, 6.82% were 1 year to 3 years, 2.27% were 3 years to 5 years, and 6.82% were more than 5 years; The control group accounted for 86.05% for less than 1 year, 11.63% for 1–3 years, and 2.33% for more than 5 years. Breast preservation: 47.73% in the experimental group; The control group accounted for 55.82%. Operation site: 95.43% of the patients in the experimental group were unilateral, and 4.55% were bilateral; In the control group, 93.02% were unilateral, and 6.98% were bilateral. Recurrence or metastasis: 9.09% in the experimental group and 4.65% in the control group. Other chronic diseases: 27.27% in the experimental group and 18.60% in the control group. The baseline data of breast cancer patients in the two groups were not significantly different (p > 0.05) except for the treatment plan as shown in Table 4.
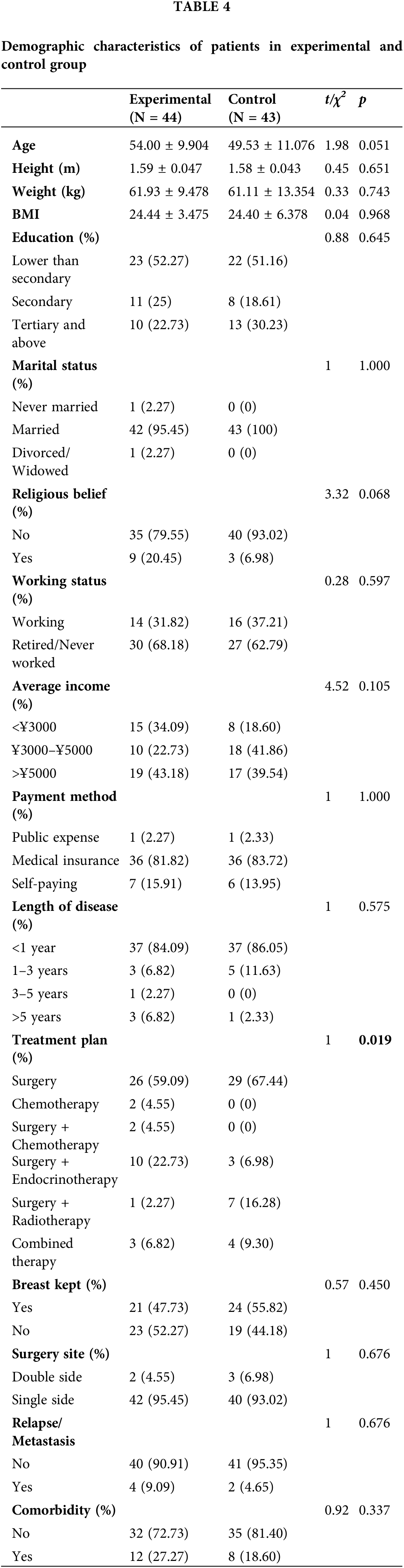
Comparison of intervention effects
The effect of group intervention based on the PTG model on post-traumatic growth, resilience, family hardness, rumination, and distress disclosure in breast cancer patients were presented in Table 5.
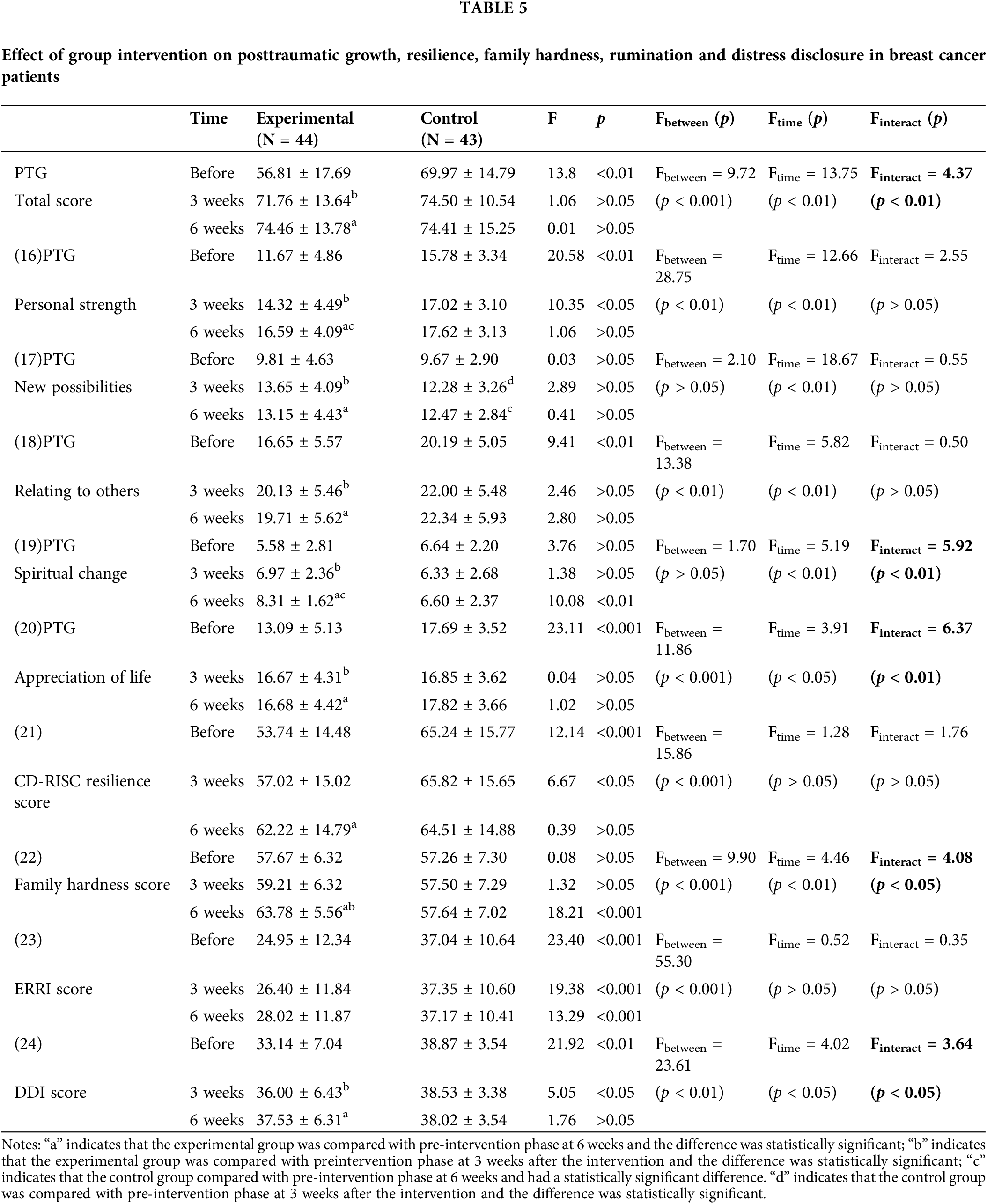
PTG score: The results of repeated measurement analysis of variance showed that a significant difference of total PTG score was found between the intervention group and the control group (Fbetween = 9.72, p < 0.001) at different time points (Ftime = 13.75, p < 0.01). There was a significant interaction between the intervention and time (Finteract = 4.37, p < 0.01). The difference of total PTG score between the intervention group and control group was statistically significant at pre-intervention (F = 13.80, p < 0.01), but the difference was not significant after 3 weeks (F = 1.06, p > 0.05) and 6 weeks (F = 0.01, p > 0.05) of intervention. The total PTG score in the intervention group was significantly different between 3 weeks compared with pre-intervention and 6 weeks compared with pre-intervention.
Personal strength of PTG score: The results of repeated measurement analysis of variance showed that the score of personal strength dimension in PTG inventory was significantly different between groups (Fbetween = 28.75, p < 0.01) and different time points (Ftime = 12.66, p < 0.01). No significant interaction between intervention and time was identified (Finteract = 2.55, p > 0.05). PTG personal strength score in the intervention group and control group was significantly different in pre-intervention (F = 20.58, p < 0.01) and after 3 weeks of intervention (F = 10.35, p < 0.05). In contrast, the difference between groups was not significant at 6 weeks (F = 1.06, p > 0.05). PTG personal strength score in the intervention group was significantly different between 3 weeks and 6 weeks compared with pre-intervention. In the control group, PTG personal strength score was significantly different between 6 weeks compared with pre-intervention.
New possibilities of PTG score: The results of repeated measurement analysis of variance showed that the new possibilities dimension score in PTG inventory had no significant difference between groups (Fbetween = 2.10, p > 0.05). The significant difference was found at different time points (Ftime = 18.67, p < 0.01), with a weak interaction (Finteract = 0.55, p > 0.05) between intervention and time. PTG new possibilities scores between groups were not significantly different at pre-intervention (F = 0.03, p > 0.05), at 3 weeks (F = 2.89, p > 0.05), and 6 weeks (F = 0.41, p > 0.05). In addition, PTG new possibilities scores were significantly increased in both the intervention group and control group at 3 weeks and 6 weeks compared with pre-intervention.
Relationship with others of PTG score: The results of repeated measurement analysis of variance showed that the score of relationship with others dimension in PTG inventory was significantly different between groups (Fbetween = 13.38, p < 0.01) and different time points (Ftime = 5.82, p < 0.01). No significant interaction between intervention and time was found (Finteract = 0.50, p > 0.05). PTG relationship with others score between groups was significantly different at pre-intervention (F = 9.41, p < 0.01), but the difference was no longer significant at 3 weeks (F = 2.46, p > 0.05) and 6 weeks (F = 2.80, p > 0.05). A significant difference in PTG relationship with others’ scores was found in the intervention group at both 3 weeks and 6 weeks compared with pre-intervention.
Spiritual change dimension score of PTG: The results of repeated measurement analysis of variance showed that there was no significant difference in spiritual change dimension score in PTG inventory between groups (Fbetween = 1.70, p > 0.05). The significant difference was found at different time points (Ftime = 5.19, p < 0.01), with strong interaction (Finteract = 5.92, p > 0.05) between intervention and time. PTG spiritual change scores between groups were not significantly different at pre-intervention (F = 3.76, p > 0.05) and at 3 weeks (F = 1.38, p > 0.05), while a significant difference between groups was found at 6 weeks (F = 10.08, p < 0.01). The significant difference in PTG spiritual change scores was revealed when data at 3 weeks and 6 weeks was compared with pre-intervention in the experimental group and 6 weeks with pre-intervention in the control group.
Appreciation of life dimension in PTG: The results of repeated measurement analysis of variance showed that the score of appreciation of life dimension in PTG inventory was significantly different between groups (Fbetween = 11.86, p < 0.001) and different time points (Ftime = 3.91, p < 0.05), with a strong interaction between intervention and time (Finteract = 6.37, p < 0.01). PTG appreciation of life score between groups was significantly different preintervention (F = 23.11, p < 0.001), but the difference was not significant at 3 weeks (F = 0.04, p > 0.05) and 6 weeks (F = 1.02, p > 0.05). A significant difference in PTG appreciation of life scores was found when data at 3 weeks and 6 weeks was compared with pre-intervention in the experimental group.
Resilience: The results of repeated measurement analysis of variance showed that the level of resilience measured by CD-RISC score was statistically different between groups (Fbetween = 15.86, p < 0.001), but the difference was not significant at different time points (Ftime = 1.28, p > 0.05), with a weak interaction between intervention and time (Finteract = 1.76, p > 0.05). CD-RISC scores between groups were significantly different at pre-intervention (F = 12.14, p < 0.001) and after 3 weeks (F = 6.67, p < 0.05), while not significantly different after 6 weeks (F = 0.39, p > 0.05). A significant difference in CD-RISC score was only found in the experimental group when comparing 6 weeks with pre-intervention.
Family hardiness: The results of repeated measurement analysis of variance showed that family hardiness measured by FHI score was significantly different between groups (Fbetween = 9.90, p < 0.001) and different time points (Ftime = 4.46, p < 0.01), with a strong interaction between intervention and time (Finteract = 4.08, p < 0.05). There was a significant difference in FHI scores between groups at 6 weeks (F = 18.21, p < 0.001), while the difference was not significant at pre-intervention (F = 0.08, p > 0.05) and at 3 weeks (F = 1.32, p > 0.05). A significant difference in FHI score was only found in the experimental group when data at 3 weeks and 6 weeks was compared with pre-intervention.
Rumination: The results of repeated measurement analysis of variance showed that there was a significant difference in rumination volume measured by the ERRI score between groups (Fbetween = 55.30, p < 0.001), and no statistically significant difference was found in the total score of ruminant contemplation between different time points (Ftime = 0.52, p = 0.60). It showed that there was no interaction between intervention methods and time (Finteraction = 0.35, p = 0.71). There was a statistically significant difference in the total score of ruminant contemplation between the experimental group and the control group (F = 55.30, p < 0.05), while the difference was significant in the total score of ruminant contemplation between the two groups before the intervention, 3 weeks after intervention, and 6 weeks after intervention (p < 0.05). There was no statistically significant difference in the total score of rumination contemplation among the three-time points in the experimental group (F = 0.67, p = 0.52); There was no statistically significant difference in the total score of ruminant contemplation between the three time points in the control group (F = 0.01, p = 0.93).
The results of repeated measurement analysis of variance showed that the results also showed that rumination measured by ERRI score was significantly different between groups (Fbetween = 55.30, p < 0.001). No significant difference was found at different time points (Ftime = 0.52, p > 0.05), and the interaction between intervention and time was weak (Finteract = 0.35, p > 0.05). There was a significant difference in ERRI score between the experimental and control group at pre-intervention (F = 23.40, p < 0.001), at 3 weeks (F = 19.38, p < 0.001), and at 6 weeks (F = 13.29, p < 0.001). No difference within the groups was found for the ERRI score.
Distress disclosure: Repeated measurement analysis of variance results show distress disclosure measured by DDI score was significantly different between groups (Fbetween = 23.61, p < 0.01) and at different time points (Ftime = 4.02, p < 0.05), with a strong interaction between intervention and time (Finteract = 3.64, p < 0.05). The difference between groups was significant at pre-intervention (F = 21.92, p < 0.01) and at 3 weeks (F = 5.05, p < 0.05) but not significant at 6 weeks (F = 1.76, p > 0.05). A significant difference in DDI score within the group was found in the experimental group when data at 3 weeks and 6 weeks was compared with pre-intervention.
Intervention effect of PTG model intervention on post-traumatic growth of breast cancer patients
The results of this study showed that the total PTG score of breast cancer patients in the two groups at pre-intervention was at an upper-middle level, which is consistent with the research results from previous studies [24,25]. The results showed that the intervention effect between the two groups of PTG total scores and time was statistically significant (p < 0.05), which means that with the change of time, the change of the two groups of PTG total scores was different, and the PTG score of the experimental group was significantly higher than that of the control group. It shows that group-based psychological intervention with the PTG model can promote PTG in breast cancer patients more than conventional health education, which is consistent with the findings from previous studies [26,27]. It is likely that the intervention scheme constructed in this study has been specifically tailored to the characteristics of breast cancer patients. Firstly, the intervention theme is relevant to patients. Previous studies and literature reviews found that psychological toughness, rumination, and self-disclosure were protective factors of PTG in breast cancer patients. The intervention strategies designed for this study were based on the mechanism of promoting PTG levels, and intervention themes were designed around the protective factors of PTG, including transforming negative emotions, promoting emotional expression, adjusting self-stress, managing uncertainty, improving mental toughness, and developing new values. Secondly, the intervention content progressed from easy to difficult levels to guide patients’ positive changes. For example, in the first week of this study, the group intervention focused on the recognition of negative emotions and positive emotions. A series of group games were carried out to give patients opportunities to express their perceptions about the disease and express their negative and positive emotions during a role play. This gradually progressed to week 2 to 6 when they learned to communicate with family members, actively expressed their inner feelings to therapists and family members, accepted the intervention content and team members of the intervention group, proactively formed an objective and positive self-evaluation action, and established their social support system. Thirdly, various intervention techniques have been integrated. The intervention plan of this study draws on and integrates a variety of psychological support techniques in which participants can learn from each other’s strengths to supplement one’s weaknesses. At the same time, it has strong openness and adaptability and helps breast cancer patients to master methods and skills to reduce psychological pain and promote emotional expression. Therefore, the increase in PTG levels in the intervention group of breast cancer patients was more significant than in the control group [28].
The group PTG model-based intervention has significantly improved breast cancer patients in their mental change of PTG and appreciation of life dimension more than conventional health education. With the change of time, the changing trend of PTG mental change and life appreciation dimension scores between the two groups was different, and the scores of the experimental group were significantly higher than those of the control group, which is in line with the research results of Li and colleagues [29]. There can be several aspects to account for this. Firstly, the improvement may be explained by the fact that 85% of the breast cancer patients included in this study had a disease duration of less than one year. Before the intervention, the patients were in a state of fear of experiencing major stressful events. The intervention plan of this study was developed to help patients to view cancer from a positive perspective, so patients had clearer mental changes after intervention than before they joined the study. Secondly, the intervention plan of this study divided the patients into several psychological support groups. Through learning and modeling the positive qualities of their peers, they changed their attitudes toward life and learned how to appreciate life around them. Therefore, the dimension of appreciation of life has changed significantly. However, the differences in the remaining dimensions of PTG before and after the intervention were not significant. The reason may be that breast cancer patients were still in a relatively closed hospital environment before and after the intervention, and their interpersonal relationships remained the same without obvious changes. PTG-based group intervention encourages and supports members to express themselves. When breast cancer patients have psychological problems, group intervention can give patients opportunities to share the general spirit of “group members face similar challenges”. Because breast cancer patients cannot change their diseases, but what can be changed is the improper interpretation and ineffective coping style of breast cancer patients, which helps breast cancer patients to reduce depression, anxiety, and other negative emotions, And develop problem-solving, promoting their ‘self transformation’ and gaining ‘new possibilities’. This intervention can develop the potential resources of breast cancer patients, share their experiences and praise others, and explore “personal strength”. Through the experience of group activities and observation of other members of the group, the positive cognition of breast cancer patients was promoted, and the growth of the “philosophy of life” was achieved. It is suggested that future research can help patients further strengthen their positive psychological experience by assigning homework, such as a positive psychological diary.
Analysis of the effects of group psychological intervention based on PTG model on family resilience of breast cancer patients
In a previous study, the research team used the Social Support Rating Scale (SSRS) to assess the degree of social support in breast cancer patients. However, multiple linear regression analysis showed that the protective factor of social support was not included in the regression equation, which was inconsistent with the results of previous studies [30,31]. A plausible explanation is that SSRS does not have specificity for evaluating breast cancer patients despite its wide use in measuring social support. Therefore, the replacement of the SSRS with the Family Hardiness Index (FHI) in the follow-up empirical application research is also consistent with the positive psychology theory employed in this study. Family resilience has changed the pessimism of families in the face of cancer stress and encouraged the family as a whole unit to actively cope with the major stress event of cancer and to continuously complete their social support functions [32,33].
Our results showed that the total score of family resilience in the two groups of breast cancer patients at pre-intervention was at the upper middle level, which was calculated with a maximal score of 80 points on the FHI scale. This is consistent with the research results from previous studies [34,35]. The results also showed that the interaction between the total score of family resilience and time in the two groups was statistically significant (p < 0.05), and the score was improved significantly in the experimental group than that of the control group. It indicates that group psychological intervention based on the PTG model can improve the family resilience of breast cancer patients better than with conventional health education. The analysis points out that group psychological intervention based on the PTG model can guide breast cancer patients to view the changes brought about by cancer from a positive perspective, encourage patients to actively communicate with their families, enhance family cohesion and family resilience, and form a meaningful source of social support [36]. For example, the research team designed a “Communication card” activity in week 2 for patients to reproduce a communication situation between family members through scenario simulation. This exercise promoted the direct expression of emotions to improve the patient’s family resilience level. Furthermore, patients observed the communication techniques of other group members to understand the harm caused by miscommunication to family members. Through this process, patients adopted positive communication strategies so that the patient’s family members felt that they understood each other and enhanced the family support to patients.
Analysis of the effect of group psychological intervention based on PTG model on psychological resilience of breast cancer patients
The results of this study showed that the total psychological resilience score of the two groups of breast cancer patients before the intervention was at an upper-middle level with the CD-RISC scale maximal score of 100, which is in agreement with previous findings [37,38]. There was no significant difference in the level of mental toughness between the experimental group and the control group after the intervention. However, the level of psychological resilience of the patients in the experimental group showed a gradually increasing trend, while the level of psychological resilience of the patients in the control group showed a gradually decreasing trend. This suggests that group psychological intervention based on the PTG model may have implications for improving psychological resilience levels in breast cancer patients if the intervention duration is prolonged.
Since this study only measured the data from 3 weeks of intervention and 6 weeks of intervention, it could not demonstrate the long-term effect of group psychological intervention based on the PTG model on the psychological resilience of breast cancer patients. Richardson’s Mental Resilience Model points out that self-efficacy, perceived social support, optimism, and mastery are the four protective factors for mental resilience, with self-efficacy playing the most significant role among them [39]. Self-efficacy encourages patients to perceive personal abilities and gain acceptance of self and life, a process that takes time [40]. Therefore, it is recommended that future studies extend the follow-up period to observe the long-term effect of group psychological intervention based on the PTG model on psychological resilience. The ultimate aim is to gradually help breast cancer patients to complete the whole process of dysfunctional reintegration-loss of integration ability-restoration of homeostasis-elastic reintegration. In addition, the health education in this study was conducted by a multidisciplinary team based on the most concerned issues of patients, including breast care, nutrition guidance, exercise guidance, psychological adjustment, chemotherapy nursing points, and radiotherapy nursing points, all of which alleviated the suffering of breast cancer patients to a certain extent. The patient’s fear of cancer, a major stress event, cultivates positive psychological qualities such as strength, optimism, and tenacity, leading to an improvement in the level of psychological resilience.
Analysis of the effect of group psychological intervention based on PTG model on rumination in breast cancer patients
The results of this study showed that the total score of rumination in the experimental group before intervention was at the lower middle level out of the maximal score of the ERRI scale of 60 points, and the total score of rumination in the control group was at the upper middle level, which was similar to the reports of Soo et al. [11]. The results of this study showed that there was no significant interaction effect between the total score of rumination and musing and time in the two groups of subjects (p > 0.05), which means that no significant difference in the level of rumination was found between the experimental group and the control group after the intervention. It demonstrates that the group psychological intervention based on the PTG model cannot significantly improve the rumination of breast cancer patients. We speculate that more than 50% of the breast cancer patients included in this study had an education level of junior high school and below, and their thinking about the meaning of life was limited. In addition, more than 85% of patients with the course disease less than 1 year were still focusing on the disease and the treatment itself rather than rumination. We suggest that future studies should include more breast cancer patients with different educational levels and disease durations to observe the effect of group psychological intervention based on the PTG model on the level of rumination in breast cancer patients.
Analysis of the effect of group psychological intervention based on PTG model on self-disclosure of breast cancer patients
The results of this study showed that the total score of mental toughness in the two groups of breast cancer patients at pre-intervention was at an upper-middle level out of the maximal score of the DDI scale of 60, which was consistent with the results of Chen and colleagues [41]. The findings showed a significant difference in the changing trend of the total score of self-disclosure between the two groups, with the score improving significantly in the experimental group than that of the control group. This indicates that the group psychological intervention based on the PTG model can improve the self-disclosure of breast cancer patients better than conventional health education. Therefore, this intervention paradigm may encourage breast cancer patients to reconstruct traumatic memories into new schemas and reduce automatic intrusive rumination thoughts, thereby helping patients to see things in a new and positive way by assessing the traumatic event itself [27]. Self-regulation theory also points out that in the process of expressing emotion-related experiences, patients use certain emotion regulation strategies, such as directing attention, promoting habituation, and cognitive restructuring, to achieve emotional balance. Ultimately, the regulation of negative emotions and improvement in the level of self-disclosure is also closely related to the use of various psychological adjustment techniques in the process of this study.
This study comprehensively examined the impact of post-traumatic growth and psychological group intervention on the post-traumatic growth of breast cancer patients. It also discusses the impact of this intervention on the family resilience, self-disclosure, and psychological resilience of breast cancer patients. The strength of the PTG group intervention can be found in the following aspects. Firstly, a multidisciplinary team was established, which gave general guidance and actively participated in the implementation of the intervention. Secondly, individual traits related to PTG were considered. Finally, the content of the theme conference focused on the protective factors related to PTG, and multiple psychological intervention techniques were integrated into the intervention that actively guided patients to think about the positive experiences of traumatic events. A variety of relevant themes in each session was used to give patients role-play opportunities to reinforce the cognitive thinking that they developed during the sessions. At present, there are few reports on intervention research focusing on the post-traumatic growth of breast cancer patients in China. The group psychological intervention based on the PTG model constructed in this study focuses on the protective factors of post-traumatic growth, integrates multiple psychological intervention technologies, focuses on interaction and communication with patients, and actively guides patients to think, providing valuable empirical evidence for improving the quality of tumor care.
There are also some limitations in this study. Firstly, considering that the psychological intervention measures of the experimental group may pollute the control group, we used simple randomization, and patients from a hospital were divided into the same group. Due to the different cultural atmosphere, the comparability of the two groups of baseline-related indicators may be affected to some extent. Secondly, due to the particularity of psychological intervention and the limitations of its research conditions, it is impossible to achieve measurer blindness and only achieve single blindness, namely, subject blindness. Thirdly, this study was a 6-week intervention with good compliance, so we could not access the lost follow-up rates in a longer study. Fourthly, this study was only conducted in a comprehensive tertiary hospital, and the results may not be generalized to primary and community healthcare settings. Last, Although the WeChat group has also been set up for the group psychological support group, and the members of the research team can be contacted by telephone at any time to obtain support, the participation of the research subjects in the information platform is not high.
Compared with health education, group psychological intervention based on the PTG model significantly improved the PTG level, family resilience level, and self-disclosure level of breast cancer patients. However, PTG model intervention did not bring a significant improvement in psychological resilience level and rumination level, both of which may require further investigation with longer-term PTG model intervention and in-depth verification. It is recommended the patient care cancer patients may consider incorporating PTG model intervention in clinical and hospital settings.
Acknowledgement: Thanks to Director Zhang Yanan and Head Nurse Li Kunpeng of the Breast Diagnosis and Treatment Center of Zhongda Hospital Southeast University. Thanks to the Head Nurses Kang Guojuan, Rui Yehao, and Lin Juan from the Department of Oncology. Thanks to Tan Liangliang and Yang Li from the Department of Psychiatry.
Funding Statement: Funding from the 2018 Postgraduate Research & Practice Innovation Program of Jiangsu Province is gratefully acknowledged (SJCX18_0082).
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design, data collection, analysis and interpretation of results: Xu CR, Sun J, Yan H; draft manuscript preparation: Sun J, Xu DW, Xu CR, Yan H, Xu Q, Chen GJ; review and edit manuscrip: Li KP, Rui YH, Sun J; the results section and critical editing of the manuscript: Sun J, Xu DW, Song ZM, Gill N. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: All the data and the materials could be accessed upon the request to the corresponding author with reasonable protocols.
Ethics Approval: The study protocol was approved by IEC for clinical research of Zhongda Hospital, affiliated to Southeast University (Ref no. 20190117). The trial was registered on 17 August 2019 at the Chinese Clinical Trials.gov (ChiCTR1900025264).
Conflicts of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin [Internet]. 2021;71(3):209–49. doi:https://doi.org/10.3322/caac.21660. [Google Scholar] [PubMed] [CrossRef]
2. Ding R, Xiao Y, Mo M, Zheng Y, Jiang YZ, Shao ZM. Breast cancer screening and early diagnosis in Chinese women. Cancer Biol Med [Internet]. 2022;19(4):450–67. doi:https://doi.org/10.20892/j.issn.2095-3941.2021.0676. [Google Scholar] [PubMed] [CrossRef]
3. Wang YY, Duan ZZ, Ma ZK, Mao YZ, Li XY, Wilson A, et al. Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Transl Psychiat [Internet]. 2020;10(1):607. doi:https://doi.org/10.1038/s41398-020-00950-y. [Google Scholar] [PubMed] [CrossRef]
4. Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress [Internet]. 1996;9(3):455–71. [Google Scholar] [PubMed]
5. Fu X, Sun J, Wang XX, Cui MK, Zhang Q. Research progress on influencing factors and intervention measures of post-traumatic growth in breast cancer patients. Front Public Health [Internet]. 2022;10:927370. doi:https://doi.org/10.3389/fpubh.2022.927370. [Google Scholar] [PubMed] [CrossRef]
6. McDonough MH, Sabiston CM, Wrosch C. Predicting changes in posttraumatic growth and subjective well-being among breast cancer survivors: the role of social support and stress. Psycho-Oncol [Internet]. 2014;23:114–20. doi:https://doi.org/10.1002/pon.3380. [Google Scholar] [PubMed] [CrossRef]
7. Capaldi JM, Shabanian J, Finster LB, Asher A, Wertheimer JC, Zebrack BJ, et al. Post-traumatic stress symptoms, post-traumatic stress disorder, and post-traumatic growth among cancer survivors: a systematic scoping review of interventions. Health Psychol Rev [Internet]. 2023;12:1–34. doi:https://doi.org/10.1080/17437199.2022.2162947. [Google Scholar] [PubMed] [CrossRef]
8. Michalczyk J, Dmochowska J, Aftyka A, Milanowska J. Post-traumatic growth in women with breast cancer: intensity and predictors. Int J Env Res Pub Health [Internet]. 2022;19(11):6509. doi:https://doi.org/10.3390/ijerph19116509. [Google Scholar] [PubMed] [CrossRef]
9. Jiang XX, Yang YJ, Li HP, Li SW, Su D, Zhang T, et al. An intervention based on protective factors to improve resilience for breast cancer patients: Study protocol for a randomized controlled trial. J Adv Nurs [Internet]. 2019;75(11):3088–96. doi:https://doi.org/10.1111/jan.14108. [Google Scholar] [PubMed] [CrossRef]
10. Allen N, Hevey D, Cogley C, O’Keeffe F. A meta-analysis of the association between event-related rumination and posttraumatic growth: the event-related rumination inventory and the posttraumatic growth inventory. J Trauma Stress [Internet]. 2022;35(6):1575–85. doi:https://doi.org/10.1002/jts.22875. [Google Scholar] [PubMed] [CrossRef]
11. Soo H, Sherman KA. Rumination, psychological distress and post-traumatic growth in women diagnosed with breast cancer. Psycho-Oncol [Internet]. 2015;24(1):70–9. doi:https://doi.org/10.1002/pon.3596. [Google Scholar] [PubMed] [CrossRef]
12. Pluta M. Online self-disclosure and social sharing of emotions of women with breast cancer using instagram-qualitative conventional content analysis. Chronic Illn [Internet]. 2022;18(4):834–48. doi:https://doi.org/10.1177/17423953211039778. [Google Scholar] [PubMed] [CrossRef]
13. Ryu JH, Suh KH. Self-disclosure and post-traumatic growth in Korean adults: a multiple mediating model of deliberate rumination, positive social responses, and meaning of life. Front Psychol [Internet]. 2022;13:149. doi:https://doi.org/10.3389/fpsyg.2022.878531. [Google Scholar] [PubMed] [CrossRef]
14. Calzone KA, Prindiville SA, Jourkiv O, Jenkins J, DeCarvalho M, Wallerstedt DB, et al. Randomized comparison of group versus individual genetic education and counseling for familial breast and/or ovarian cancer. J Clin Oncol [Internet]. 2005;23(15):3455–64. doi:https://doi.org/10.1200/JCO.2005.04.050. [Google Scholar] [PubMed] [CrossRef]
15. Rissanen R, Arving C, Ahlgren J, Nordin K. Group versus individual stress management intervention in breast cancer patients for fatigue and emotional reactivity: a randomised intervention study. Acta Oncol [Internet]. 2014;53(9):1221–9. doi:https://doi.org/10.3109/0284186X.2014.923935. [Google Scholar] [PubMed] [CrossRef]
16. Seiler A, Jenewein J. Resilience in cancer patients. Front Psychiatry [Internet]. 2019;10:598. doi:https://doi.org/10.3389/fpsyt.2019.00208. [Google Scholar] [PubMed] [CrossRef]
17. Macintyre PD, Gregersen T, Mercer S. Setting an agenda for positive psychology in SLA: theory, practice, and research. Mod Lang J [Internet]. 2019;103(1):262–74. doi:https://doi.org/10.1111/modl.12544. [Google Scholar] [CrossRef]
18. Liu JE, Wang HY, Wang ML, Su YL, Wang PL. Posttraumatic growth and psychological distress in Chinese early-stage breast cancer survivors: a longitudinal study. Psycho-Oncology [Internet]. 2014;23(4):437–43. doi:https://doi.org/10.1002/pon.3436. [Google Scholar] [PubMed] [CrossRef]
19. Dong L, Hu Y, Xu G, Huang J. Reliability and validity of the Chinese version of post-traumatic growth inventory scale in breast cancer survivors. J Nurs Sci [Internet]. 2013;28(22):21–3. [Google Scholar]
20. Yu X, Zhang J. A comparison between the Chinese version of ego-resiliency scale and connor-davidson resilience scale. Psychol Sci [Internet]. 2007;30(5):1169–71. [Google Scholar]
21. Fan YW, Xie PH, Liu QL. Reliability and validity of the Chinese version of the family hardiness index among patients with cancer. Psychooncology [Internet]. 2018;27:117–8. [Google Scholar]
22. Dong C, Gong S, Liu X. Reliability and validity of the simplified Chinese version of event related rumination inventory among accidentally injured patients. Chin J Nurs [Internet]. 2013;48(9):831–4. [Google Scholar]
23. Kahn JH, Hessling RM. Measuring the tendency to conceal versus disclose psychological distress. J Soc Clin Psychol [Internet]. 2001;20(1):41–65. doi:https://doi.org/10.1521/jscp.20.1.41.22254. [Google Scholar] [CrossRef]
24. Parikh D, de Ieso P, Garvey G, Thachil T, Ramamoorthi R, Penniment M, et al. Post-traumatic stress disorder and post-traumatic growth in breast cancer patients—a systematic review. Asian Pac J Cancer Prev [Internet]. 2015;16(2):641–6. doi:https://doi.org/10.7314/APJCP.2015.16.2.641. [Google Scholar] [PubMed] [CrossRef]
25. Shi J, Sznajder KK, Liu S, Xie XY, Yang XS, Zheng Z. Resilience and posttraumatic growth of patients with breast cancer during the COVID-19 pandemic in China: the mediating effect of recovery. Front Psychol [Internet]. 2022;12:e936. doi:https://doi.org/10.3389/fpsyg.2021.811078. [Google Scholar] [PubMed] [CrossRef]
26. Sarenmalm EK, Martensson LB, Andersson BA, Karlsson P, Bergh I. Mindfulness and its efficacy for psychological and biological responses in women with breast cancer. Cancer Med [Internet]. 2017;6(5):1108–22. doi:https://doi.org/10.1002/cam4.1052. [Google Scholar] [PubMed] [CrossRef]
27. Ramos C, Costa PA, Rudnicki T, Maroco AL, Leal I, Guimaraes R, et al. The effectiveness of a group intervention to facilitate posttraumatic growth among women with breast cancer. Psychooncology [Internet]. 2018;27(1):258–64. doi:https://doi.org/10.1002/pon.4501. [Google Scholar] [PubMed] [CrossRef]
28. Wang GR, Li ZY, Luo X, Wei R, Liu H, Yang J, et al. Effects of nurse-led supportive-expressive group intervention for post-traumatic growth among breast cancer survivors: a randomized clinical trial. J Nurs Scholarsh [Internet]. 2022;54(4):434–44. doi:https://doi.org/10.1111/jnu.12752. [Google Scholar] [PubMed] [CrossRef]
29. Li JJ, Peng XC, Su YL, He Y, Zhang SF, Hu XL. Effectiveness of psychosocial interventions for posttraumatic growth in patients with cancer: a meta-analysis of randomized controlled trials. Eur J Oncol Nurs [Internet]. 2020;48(21):101798. doi:https://doi.org/10.1016/j.ejon.2020.101798. [Google Scholar] [PubMed] [CrossRef]
30. Kolokotroni P, Anagnostopoulos F, Tsikkinis A. Psychosocial factors related to posttraumatic growth in breast cancer survivors: a review. Women Health [Internet]. 2014;54(6):569–92. doi:https://doi.org/10.1080/03630242.2014.899543. [Google Scholar] [PubMed] [CrossRef]
31. Yeung NCY, Lu Q. Perceived stress as a mediator between social support and posttraumatic growth among Chinese American breast cancer survivors. Cancer Nurs [Internet]. 2018;41(1):53–61. doi:https://doi.org/10.1097/NCC.0000000000000422. [Google Scholar] [PubMed] [CrossRef]
32. Li YL, Qiao YJ, Luan XR, Li SJ, Wang KF. Family resilience and psychological well-being among Chinese breast cancer survivors and their caregivers. Eur J Cancer Care [Internet]. 2019;28(2):e12984. doi:https://doi.org/10.1111/ecc.12984. [Google Scholar] [PubMed] [CrossRef]
33. Liu Y, Li YL, Chen LJ, Li YR, Qi WY, Yu L. Relationships between family resilience and posttraumatic growth in breast cancer survivors and caregiver burden. Psycho-Oncology [Internet]. 2018;27(4):1284–90. doi:https://doi.org/10.1002/pon.4668. [Google Scholar] [PubMed] [CrossRef]
34. Wang WH. Correlation between family adaptability and family resilience factors in families of cancer patients (Master’s Thesis). Liaoning: Dalian Medical University; 2015. [Google Scholar]
35. Shi J, Sznajder KK, Liu S, Xie X, Yang X, Zheng Z. Resilience and posttraumatic growth of patients with breast cancer during the COVID-19 pandemic in China: The mediating effect of recovery. Front Psychol [Internet]. 2022;12:811078. doi:https://doi.org/10.3389/fpsyg.2021.811078. [Google Scholar] [PubMed] [CrossRef]
36. Wu D, Li H, Yang Y, Zhang T, Zhang M, Jiang X, et al. Development and prospect of family resilience and related assessment tools of cancer patients. Chin Nurs Manag [Internet]. 2018;18(11):1566–70. [Google Scholar]
37. Li LB, Hou YC, Li LB, Hou YC, Kang FY, Wei XL. The mediating and moderating roles of resilience in the relationship between anxiety, depression, and post-traumatic growth among breast cancer patients based on structural equation modeling an observational study. Med [Internet]. 2020;99(50):e23273. doi:https://doi.org/10.1097/MD.0000000000023273. [Google Scholar] [PubMed] [CrossRef]
38. Tu PC, Yeh DC, Hsieh HC. Positive psychological changes after breast cancer diagnosis and treatment: the role of trait resilience and coping styles. J Psychosoc Oncol [Internet]. 2020;38(2):156–70. doi:https://doi.org/10.1080/07347332.2019.1649337. [Google Scholar] [PubMed] [CrossRef]
39. Richardson GE. The metatheory of resilience and resiliency. J Clin Psychol [Internet]. 2002;58(3):307–21. [Google Scholar] [PubMed]
40. Sheeran P, Maki A, Montanaro E, Avishai-Yitshak A, Bryan A, Klein WMP, et al. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: a meta-analysis. Health Psychol [Internet]. 2016;35(11):1178–88. doi:https://doi.org/10.1037/hea0000387. [Google Scholar] [PubMed] [CrossRef]
41. Chen JJ, Li HP, Yang YJ, Zhang T, Wang QL, Wu DY, et al. The impact of self-disclosure on benefit findings in breast cancer patients: chain mediating effects of intimacy and self-efficacy. Chin J Clin Psychol [Internet]. 2019;27(6):1205–9. [Google Scholar]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools