 Open Access
Open Access
ARTICLE
Socio-Psychological Factors of Rising Trend of Suicidal Ideation among Indigenous Workforce: Evidence from Himalayan Range
1 Faculty of Business Administration, Lahore Leads University, Lahore, 54000, Pakistan
2 Department of Management, Marketing and Information Systems, College of Business & Finance, Ahlia University Manama, Manama, 10878, Bahrain
3 Department of Food Service and Management, Faculty of Food Science and Technology, Universiti Putra Malaysia, Serdang, Selangor, 43400, Malaysia
4 College of Hospitality and Tourism Management, Sejong University, Seoul, 143-747, Korea
* Corresponding Author: Heesup Han. Email:
International Journal of Mental Health Promotion 2023, 25(12), 1245-1256. https://doi.org/10.32604/ijmhp.2023.030577
Received 13 April 2023; Accepted 19 September 2023; Issue published 29 December 2023
Abstract
Apart from socio-economic disparities, indigenous people of the Himalayan range in Asia face an increasing trend of suicides. The tragic suicidal events usually go unaddressed, and no strategies are presently in place to mitigate suicides in the future. This study aims to explain the prevailing causes of suicidal ideation to come up with some policy recommendations. Through a preliminary survey, we identified social stigma, social isolation, lack of healthcare facilities, and domestic violence as the potential reasons for suicidal ideation. We identified individuals with suicide ideation for further data collection to test the relationships between the identified variables and suicidal ideation. A quantitative, explanatory and cross-sectional design was used to test the hypotheses. Inferential statistics were applied to the data containing 314 responses, and the results revealed that all the predictive variables influence the formation of suicidal ideation. The study uncovered some new dimensions of social stigma and social isolation that are common among the indigenous people. The results also indicate that some domestic violence is socially acceptable and considered a normal familial matter. The findings have theoretical and practical implications. We have identified new dimensions of social stigma, social isolation, and domestic violence that are new additions to the existing bank of literature. It provides insights to encourage public authorities, healthcare providers, and NGO managers to play their role in the right direction to mitigate the problem. This study opens further venues for researchers to investigate the complex issue of suicide more deeply.Keywords
Self-annihilation is a mounting public health issue, [1] and due to a lack of direct knowledge of the causes of the problem, solutions cannot be devised to mitigate it [2]. Since the causes of suicide may vary from society to society, culture to culture, and place to place [3], it is quite difficult to standardize suicidal causes to discover a generalizable remedy for it. The issue requires context-specific contextual studies and case studies to uncover the factual reasons for suicide. Suicide is one of the growing social and illegal issues in the northern belt of Pakistan. An increasing trend of suicide is prevailing, particularly in the youth of the region, and no intervention to mitigate the issue is in place as such [2]. The region is relatively peaceful, and the only major rising concern is self-annihilation [4]. This act is usually buried as soon as it is committed without proper investigation and trial [2].
The problem of understanding the phenomenon of suicide and its causes is grave because of the scarcity of data, scant literature, and lack of relevant and context-specific studies [5]. Additionally, weak investigation and trial processes and the noncooperation of family members of the victim are the major hurdles to arriving at the root causes of suicide [2]. The causes of the same suicide case are reported differently by different stakeholders. For example, police and family members declare the victim to have a mental disorder, friends of the victim report domestic violence as the cause, and other evidence depict it to be due to marital disharmony [5].
The indigenous population of the Himalayan Range, particularly in northern Pakistan is more prone to suicide, and the rate of suicide is on the increase. The problem of suicide is preventable; however, it is prevalent due to the absence of national suicide prevention strategies and policies, lack of multi-sectoral interventions, unawareness, weak culture and social system, and scarcity of research work [6]. Unfortunately, suicide cases are under-reported [7] since it is supposed to be a stigma, and as a result, correct data cannot be originated and extracted for policymaking. Mental health issues worsen due to the lack of access to healthcare services. It is alarming that not even a single measure to prevent suicide is in place from either stakeholder, but many factors are evident that provoke suicidal behaviours. People who instigate suicidal attitudes persist while counselling is yet to be established. The sense of stigma is there, whereas violence is not considered disgusting. The few reported cases are not properly investigated and litigated. Given the prevailing circumstances and the intricate nature of the suicide phenomenon, the present study sets out to elucidate the primary causes of suicidal ideation within the specific community under investigation. Social stigma, social isolation, inadequate healthcare facilities, and domestic violence emerge as seemingly dominant factors contributing to suicide attempts (see Fig. 1). Therefore, the central aim of the study is to comprehensively examine the ways in which these variables intensify suicidal ideation and subsequently propose policy recommendations to guide relevant institutions in effectively addressing this pressing issue.
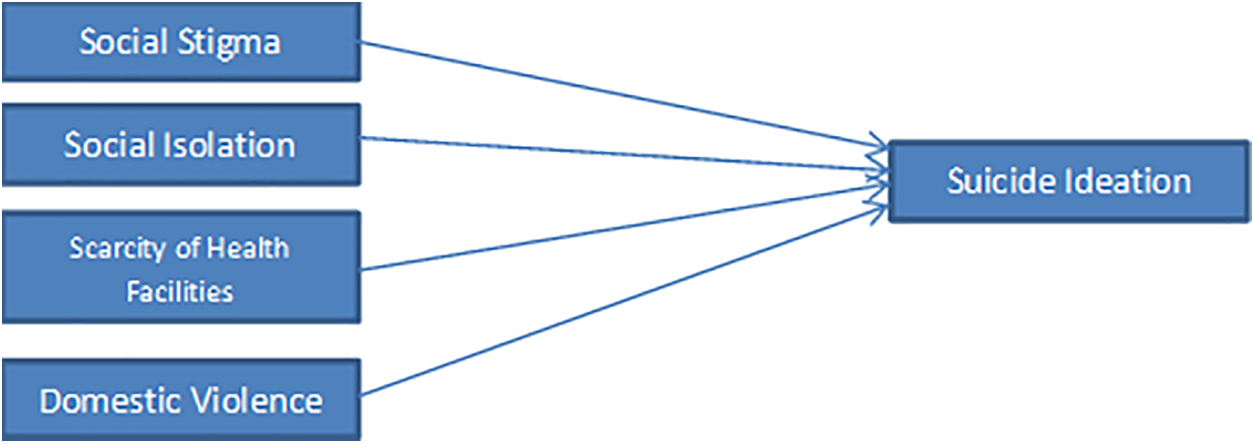
Figure 1: Conceptual model.
Exploring the causes of suicidal ideation and suicide in the given region is crucial for several reasons. Different regions have unique compositions that influence suicidal ideation and suicidal behaviour differently. By uncovering the specific causes in the given area, interventions can be tailored to the root causes that contribute to the issue. The awareness can reduce stigma associated with mental health issues and suicide, encouraging individuals to seek support and help. Equipped with correct data on the causes of suicide, public health officials, policymakers, and other concerned bodies can engage in long-term and sustainable interventions to tackle underlying issues. The findings can serve as inputs to further research to advance the understanding the causes and remedies in more deep ways. Moreover, these findings can be integrated into educational programs to create more awareness about mental issues and suicide. Understanding the causes can lead to early intervention before the situation goes worst. In short, by addressing the root causes, communities can create a safer and more supportive environment for individuals struggling with mental health challenges, potentially saving lives and improving the well-being of their residents.
Suicide accounts for about one million deaths per year, and is also one of the major causes of death among younger age groups [8]. Over recent decades, suicide has decreased by an average of 26% in most World Health Organization (WHO) regions, including in Western countries [9,10]. We do not, however, know whether all socioeconomic groups have benefited from this decrease. Suicide is indeed more frequent in vulnerable groups such as the less educated, the poor, and those in lower social classes [11]. So far, studies have been conducted in one country only or have had low statistical power [7]. Given the wide variability of suicide mortality between countries, international comparative data are needed to create a better picture of the general evolution of socioeconomic inequalities in suicide [12]. Although suicide is a preventable social and health-related problem, it continues to be a serious problem even in high-income countries. However, 79% of all suicides occur in low- and middle-income countries, which bear the larger part of the global suicide burden [13]. Although in high-income countries three times as many men die by suicide as women, the male-to-female ratio for suicide is more even in low- and middle-income countries, at 1.6 men to each woman. Suicide rates for both men and women are lowest in persons under 15 years of age and highest in persons aged 70 years or older in almost all regions of the world [8,14]. In some regions, suicide rates increase steadily with age, while in others there is a peak in suicide rates in young people [15]. In low- and middle-income countries, young adults and elderly women have much higher suicide rates than their counterparts in high-income countries, while middle-aged men in high-income countries have much higher suicide rates than those in low- and middle-income countries [16].
When the family members, friends, colleagues, and communities of those who attempt suicide or die by suicide are taken into consideration, many millions of people worldwide are affected by suicide every year [17,18]. Because suicide remains a sensitive issue, it is likely underreported due to stigma, criminalization, and weak surveillance systems. Social, psychological, cultural, and many other factors can interact to increase the risk of suicidal behavior, but the stigma attached to suicide means that many people who need help feel unable to seek it [19]. Risk factors for suicide include previous suicide attempts, mental health problems, harmful use of alcohol or drugs, job or financial loss, relationship breakdown, trauma or abuse, violence, conflict or disaster, and chronic pain or illness [20,21].
Unfortunately, suicide prevention is too often a low priority for governments and policy-makers. Suicide prevention needs to be prioritized on global public health and public policy agendas, and awareness of suicide as a public health concern must be raised by using a multidimensional approach that recognizes social, psychological, and cultural impacts [16].
A national suicide prevention strategy is important because it indicates a government’s clear commitment to prioritizing and tackling suicide while providing leadership and guidance on the key evidence-based suicide prevention interventions [22]. Stigma, particularly surrounding mental disorders and suicide, means many people thinking of taking their own life or who have attempted suicide are not seeking help, and are therefore not getting the help they need [19,23]. The prevention of suicide has not been adequately addressed due to a lack of awareness of suicide as a major public health problem [24] and the taboo in many societies to openly discuss it [25]. To date, only a few countries have included suicide prevention among their health priorities, and only 38 countries report having a national suicide prevention strategy [26,27].
Many theories explain the phenomenon of suicide. For example, Shneidman [28,29] explained suicide as a response to overwhelming pain (i.e., psychache), Durkheim [30] emphasized the role of social isolation, Baumeister [31] described suicide as an escape from an aversive state of mind, and Beck and Abramson et al. [32,33] highlighted the role of hopelessness. These theories have been tremendously useful in guiding suicide research and prevention efforts. However, we use The Three Steps Theory of Suicide (3ST) [34] to provide a theoretical basis for this study. This theory emphasizes that in the first step suicide ideation comes into play as a result of pain and hopelessness. The interaction of pain and hopelessness creates suicidal thoughts, but pain or hopelessness alone does not cause suicidal ideation. A person with pain and the hope that things will get better in the future will engage with life, and a hopeless person without pain will also continue with life. The second step of the theory explains the degree of intensity of suicide ideation. Connectedness in social circle, job, projects, role, and interest is the investment in one’s life and the connectedness will moderate the intensity of suicide ideation. The third step of this theory explains the progression from suicide ideation to a suicide attempt. This is the capacity of a person to demonstrate suicide behavior. The Three Step Theory of Suicide seemingly incorporates the variables considered in our study. Initially, domestic violence and social stigma inflict pain upon the victims, which often becomes unbearable. Subsequently, the absence of adequate healthcare facilities prolongs this pain and fosters a sense of hopelessness regarding its alleviation. Moreover, social isolation deprives the victims of connectedness, that intensify suicidal thoughts and eventually leading to the act of suicide.
Stigma: it is the mark of disgrace associated with an individual due to a suicide attempt or other social reasons [35]. Stigma causes social disapproval or society places shame on a person for living with a particular social characteristic [36]. Thus, the stigmatized person faces negative attitudes and discrimination based on any socially constructed phenomenon.
Isolation: it is a lack of connectedness to the people or group or society. Isolation also takes place, as a result, of a lack of social acceptance [37]. It is the absence of meaningful relationships and absence of social interactions, contacts, and relationships with family and friends [38].
Scarcity of Healthcare Services: it means failing to have the timely use of personal health services to achieve the best health outcomes. It is characterized by the lack of affordability, availability, accessibility, accommodation, and acceptability [39].
Domestic Violence: it is the physical, mental, psychological, or sexual abuse or violence within the domestic circle of the victim [40]. The victim feels insecure at home, and in most cases, the family violence occurs repeatedly [41].
Suicide Ideation: it occurs when someone wishes to die. This includes thoughts and ideas about the possibility of ending one’s life [42]. This idea usually comes when one experiences pain and hopelessness and life appears to be a troublesome burden [34]. We use suicide ideation as the criterion variable in the research model.
Suicide ideation is the causation of suicide attempts and self-killing, and the intensity of suicide ideation determines the commitment towards suicide. Social stigma causes acute psychological pain and has a long-lasting impact [43]. A stigma causes disgrace, and members of the community keep a scornful attitude due to the stigma. A person becomes stigmatized due to suicide attempts or demonstrating some kind of suicidal behavior or self-harming [19]. We believe that stigma may inflict due to certain reasons other than suicidal ones [44], for example, the stigma associated with physical appearance or the stigma attached to association with a particular race, ethnicity, religion, and ideology. The quickest way to eliminate such social stigma is to end one’s life. Thus, we formulate the following hypothesis:
Hypothesis 1: We assume a direct relationship between social stigma and suicide ideation
A socially isolated person becomes vulnerable to the risk of mental health issues such as depression, anxiety, and substance abuse, as well as chronic conditions like high blood pressure, heart disease, and diabetes [45]. People with mental health issues and chronic diseases have a considerable rate of attempted or completed suicides. On the other hand, people connected to social and family circles, jobs, roles, etc., have little tendency towards suicide because this embeddedness is an investment in life [46]. When there is no investment in life, any pain and hopelessness may drive a person towards ending life. So we develop the following hypothesis:
Hypothesis 2: We assume a direct relationship between social isolation and suicide ideation
Mental health crises devastate lives, and persistent mental health issues or chronic diseases are dominant sources of suicidal behaviours [47]. People with suicidal ideation can be rehabilitated through neurological, psychological, and psychiatric therapy [48]. Mental or chronic diseases are mostly curable, and negligence in this regard may cause suicide. Several signs and symptoms people demonstrate prior to suicide ideation or suicide attempts include depression, anxiety, insomnia, and restlessness [49]. When these curable mental conditions are left unattended, suicide can result. The population under study has limited access to healthcare because of poverty and the unavailability of government-managed healthcare services. Keeping in view these conditions we frame the following hypothesis:
Hypothesis 3: We assume a direct relationship between scarcity of healthcare facilities and suicide ideation
Domestic violence exists more prevalent in the extended family system [2]. Domestic violence is repetitive in nature and domestic violence or intimate partner violence is a type of violence that is defined as a pattern of coercive control against a former or current intimate partner and includes physical, sexual, and or psychological assaults. Women are more vulnerable to suicide due to domestic and family violence [50]. Women spend the majority of their time at home where their main concern is to run domestic affairs. When the domestic environment is violent, life can become intolerable. Thus, we formulate the following hypothesis:
Hypothesis 4: We assume a direct relationship between domestic violence and suicide ideation
Population, sampling and data collection
The belt houses a population of 170,000 indigenous people, residing in an underdeveloped area lacking essential life amenities [51]. Due to geographical isolation and limited government attention, economic opportunities are scarce, and the corporate sector is virtually non-existent. Some individuals manage to secure government jobs, others seek work outside the region, while some remain unemployed. However, the provision of public goods and services is inadequate, and access to healthcare facilities is limited. The prevalence of mental illness is on the rise, leading to an increase in the suicide rate among this population. Despite the rising trend of suicide, no one has previously compiled data on this grave problem [52]. For the purpose of our study, we focused on this specific population experiencing mental illness to the extent that it triggers suicidal ideation. Our criterion variable revolves around suicide ideation, so it is crucial that our respondents have experienced such thoughts in order to make the study more targeted and relevant. Agha Khan Health Services Pakistan, field office Chitral, Booni, led by a psychologist and her team, was engaged to identify people with mental diseases, particularly patients with depression, and provide counseling or guidance for medical therapy. The office maintains records of mentally ill patients and makes frequent follow-up contacts with them. The project employees were a great help in collecting data. Regarding the sample’s inclusion and exclusion criteria, we included individuals who were actively involved in economic activities for earning, had a mental disorder, and experienced suicidal ideation. Conversely, we excluded those who were unemployed or not earning, had been deemed mentally sound by a qualified psychologist, and scored below 21 on the Suicide Ideation Attribute Scale. Our focus was on working individuals who were experiencing mental distress and contemplating suicidal thoughts. We used Suicidal Ideation Attributes Scale (SIDAS) [53] to identify the patients with suicidal ideation. Since those who score 21 or above on SIDAS are considered to have suicidal thoughts, we included those who scored 21 or higher on the scale (SIDAS). The author, along with the assistance of two trained research assistants, personally collected the data. This team randomly selected the patients for the SIDAS test, and administered questionnaires to those who qualified on the SIDAS scale. The author conducted regular follow-up visits over a period of a couple of months to gather the questionnaires and complete the data collection process.
1200 patients were randomly selected from a list of 4238 registered mental health patients were tested for suicidal ideation and 359 patients scored 21 or higher. So, we administered questionnaires to all 359 patients and received 326 back with 91% response rate. We excluded questionnaires with 5% or more missing values, resulting in the removal of 12 questionnaires. After this step, we included 314 questionnaires that were filled out with an acceptable level of accuracy.
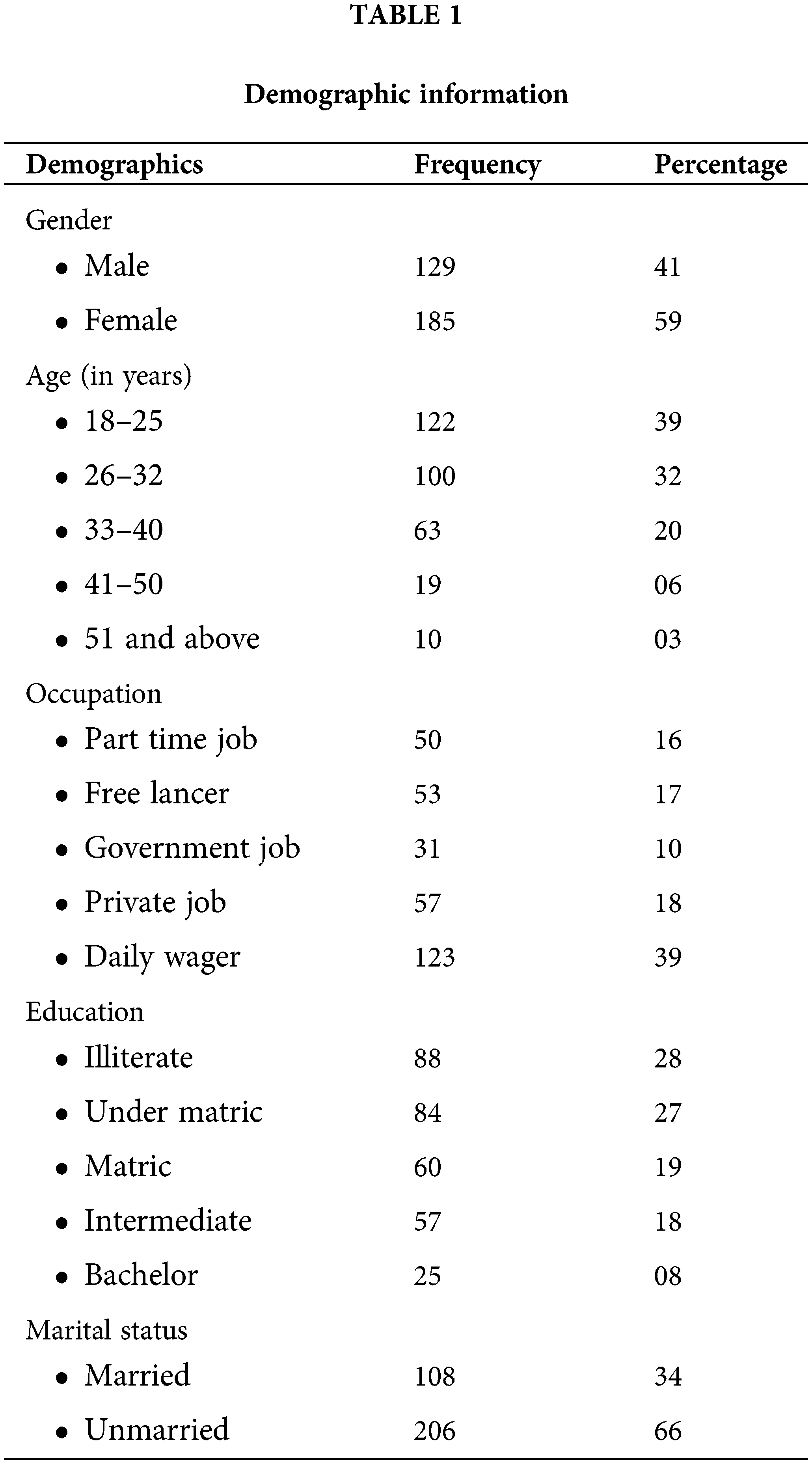
Demographic information of the respondents is shown in Table 1.
We adopted previously used scales to measure our variables. Stigma was measured using the Scale of Suicide Stigma (SOSS) developed by Batterham et al. [54], which has 16 items. The scale developed by Cornwell et al. [55], which carries nine items, was used to measure social isolation. The healthcare services availability and access difficulty was measured using the scale of Haggerty et al. [56,57] with six items. Though the adopted scales were validated, we further tested for reliability and validity as these scales were being used in a different context. Besides reliability and convergent and discriminant validity, we tested for multicollinearity, autocorrelation, and common method bias. We found our data to be free from such kind of discrepancies.
The data analysis process involved two main steps. Firstly, quality control tests were performed to ensure the validity and reliability of the data while also checking for the possibility of multicollinearity and Common Method Bias. Secondly, inferential statistics were employed to test the hypotheses by using Structural Equation Modelling (SEM) [58–60]. For SEM, the researchers utilized a Partial Least Square (PLS) approach, which is an advanced level data analysis tool [61] This method allows for the investigation of both the structural components (path model) and the measurement model (factor model) simultaneously within a single model. By employing structural equation modelling (SEM) in this manner, the researchers were able to gain a comprehensive understanding of reliability, validity, and causality all at once.
The author had multiple meetings with the administrator of the healthcare centre to obtain formal approval for data collection. Additionally, they signed an agreement with the ethical committee of the healthcare centre to ensure confidentiality and anonymity. To address any potential ethical concerns, the authors adhered to the ethical norms outlined in the Helsinki Declaration [62–64]. As part of this commitment to ethics, every participant was guaranteed by the authors that any information shared by an employee would remain confidential and would only be used for the purposes of the current research [65,66]. Informed consent was obtained from each participant, and they were also given the right to withdraw from the information-giving process at any time if they felt uncomfortable, without the need to provide a specific reason to the authors [67,68].
Although the scales were tested for reliability and validity, we further tested the scales to avoid any discrepancy arising due to changes in context and respondents. Reliability was measured using Cronbach and composite reliability tests (Table 2). Cronbach’s alpha values for all the variables were above the cut-off value of 0.70, ensuring inter-rater reliability, and similarly composite reliability values for all five variables were higher than the threshold value, which is also 0.70 [69,70]. These two tests guarantee the reliability of a scale [71].
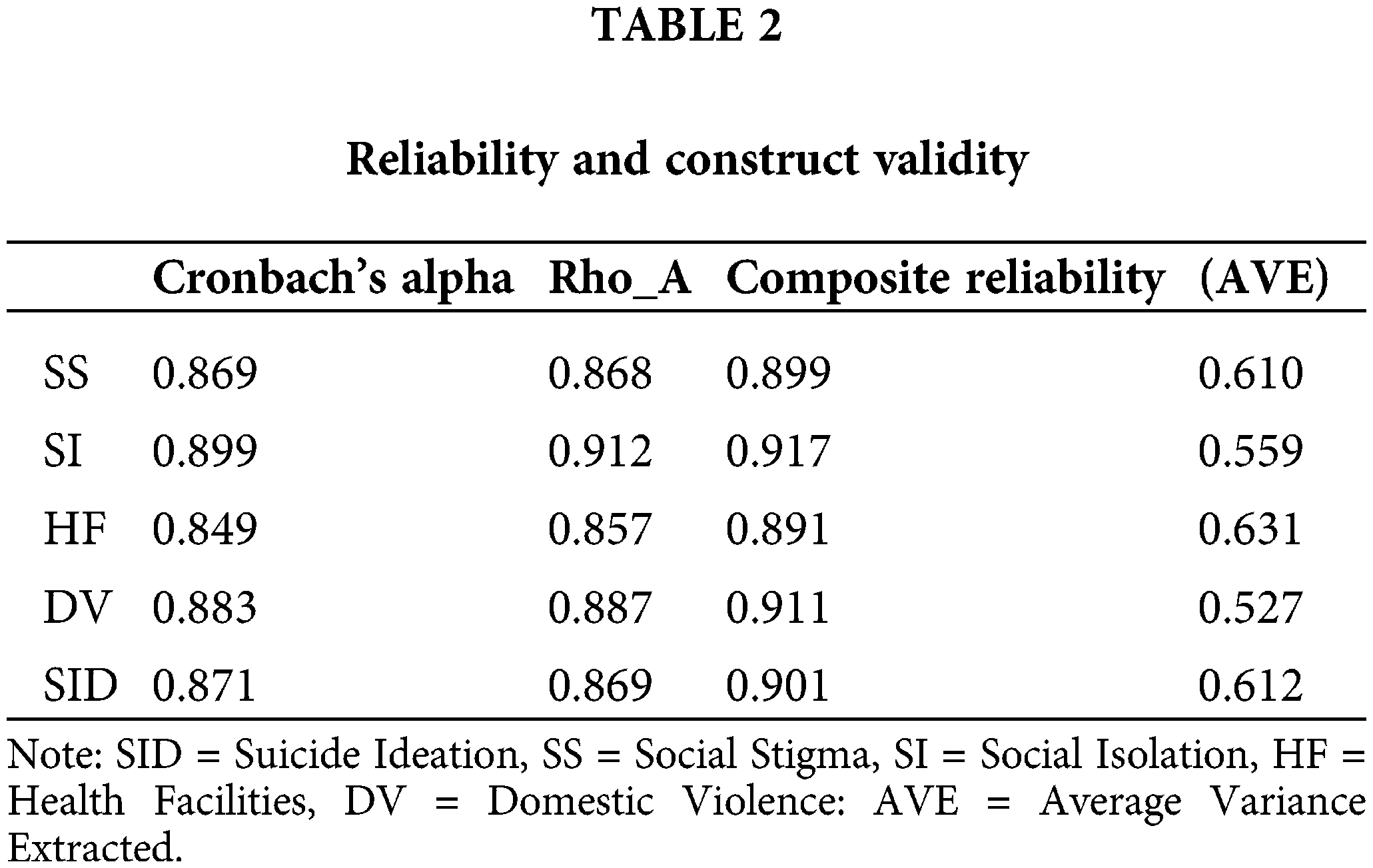
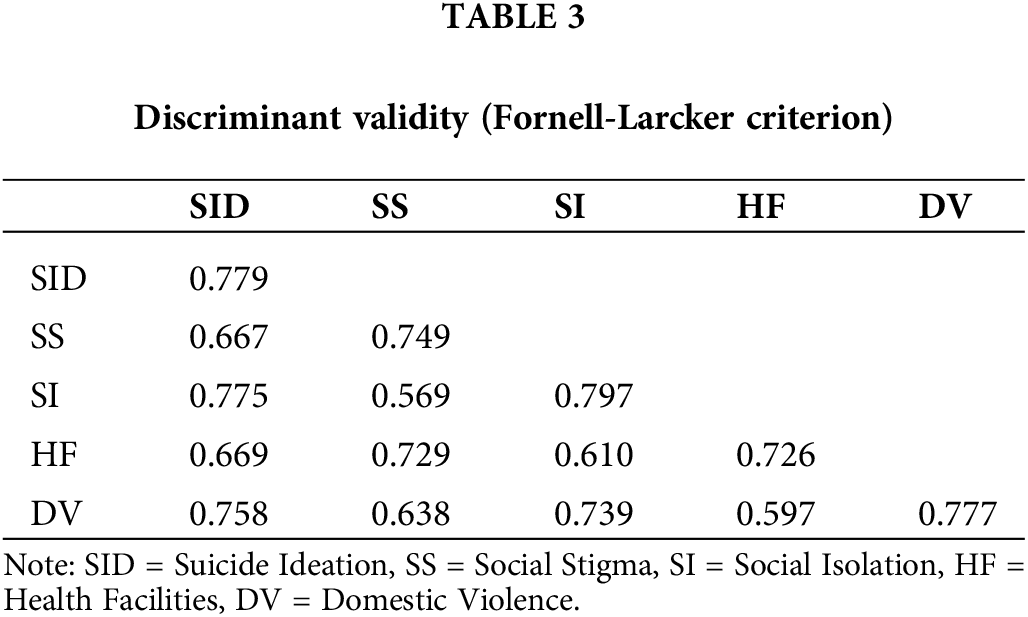
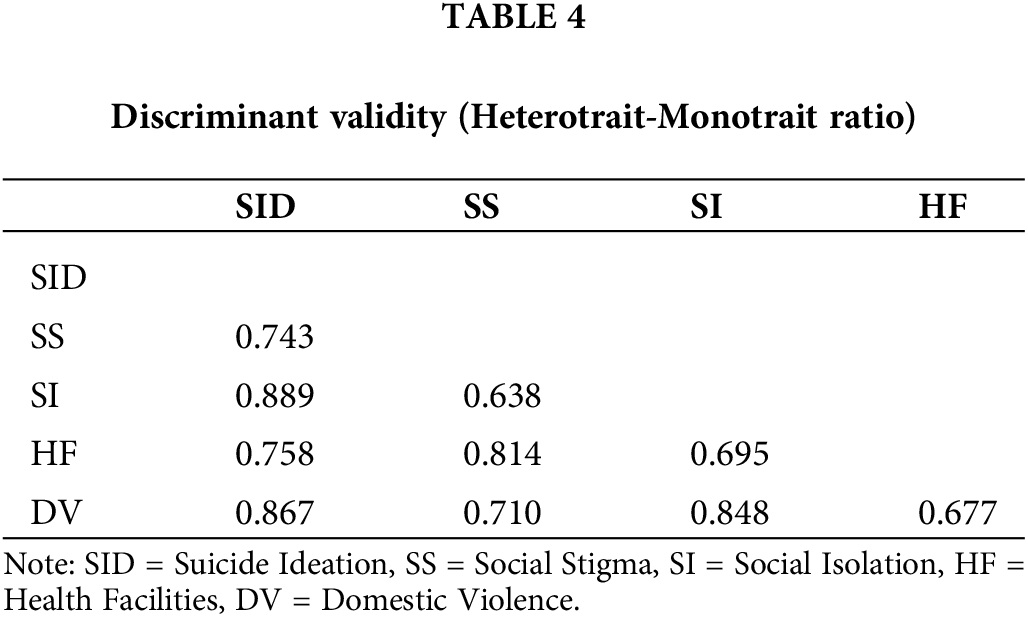
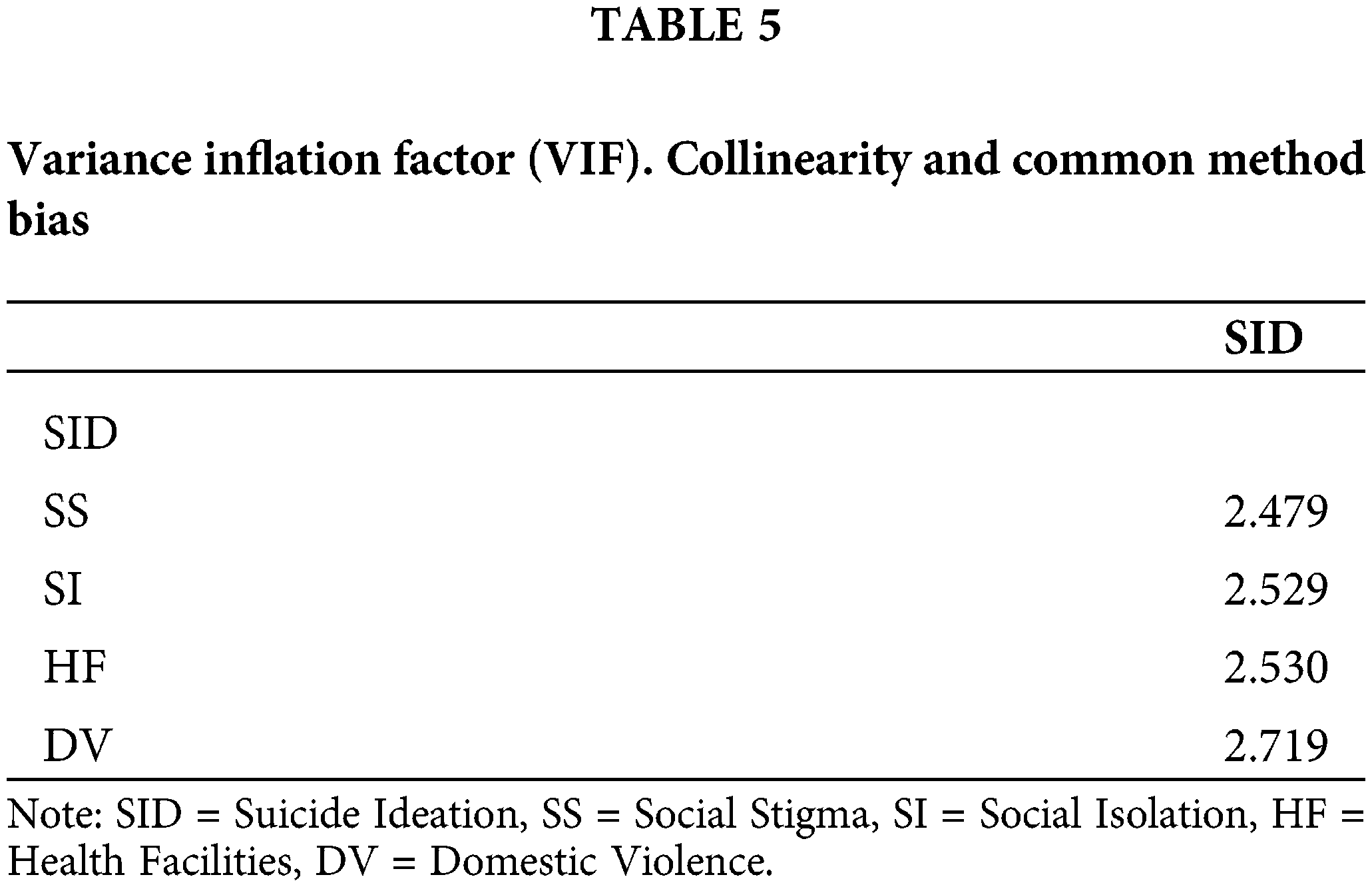
The values of Average Variance Extracted (AVE) were used to check convergent validity [72,73] (Table 2). AVE values for all the variables were higher than the cutoff value (0.50), ensuring that convergent validity was in place for all the variables. We applied Fornell et al. [74] criterion and Heterotrait-Monotrait (HTMT) to verify discriminant validity as suggested by Henseler et al. [75]. According to the Fornell-Larcker approach, a variable should better explain the loadings of its own indicator rather than the loadings of another latent variable [76]. Thus, the value of each construct is greater than the correlations of other constructs endorsing high Discriminant Validity (Table 3). According to the Heterotrait-Monotrait ratio the values above 0.9 show a lack of Discriminant validity [77], while in the given case all the values are less than 0.90, which reinforces discriminant validity (see Table 4). Additionally, variance inflation factor (VIF) statistics (Table 5) provided strong evidence against multicollinearity as the values are less than 5.0 as proposed by Belsley et al. [78]. In the same way, the possibility of common method bias is ruled out as the VIF values are less than 3.30 as proposed by Kock et al. [79].
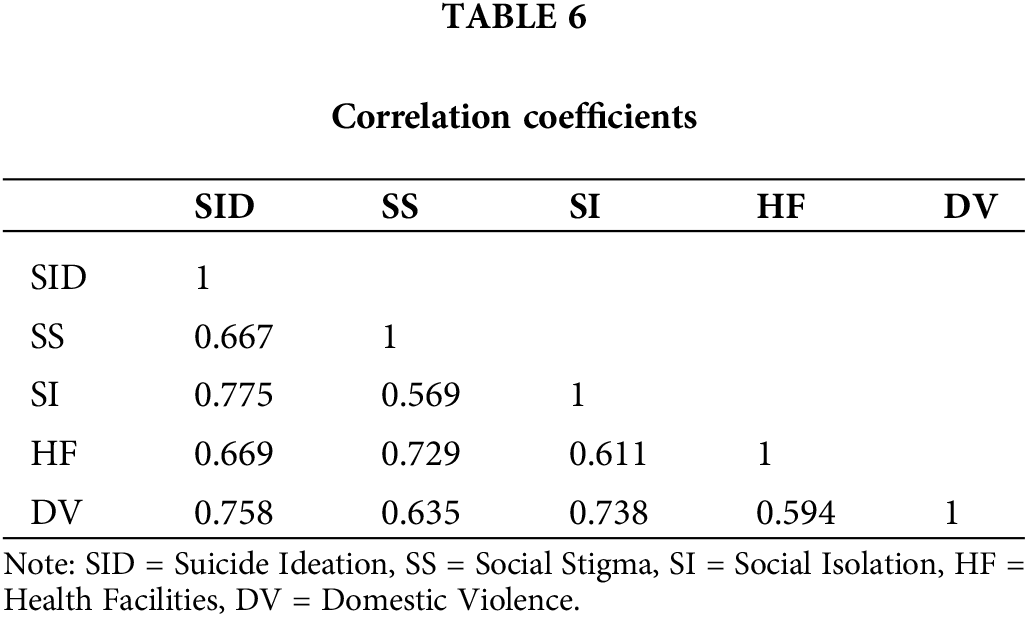
The correlation coefficients indicated positive relationships among variables (Table 6). SID and the remaining variables are significantly correlated. Domestic Violence (DV) and Social Isolation (SI) are strongly correlated with Suicide Ideation, while Social Stigma (SS) is moderately correlated with SID. Since no coefficient of correlation is greater than 0.8, the possibility of auto-correlation is ruled out.
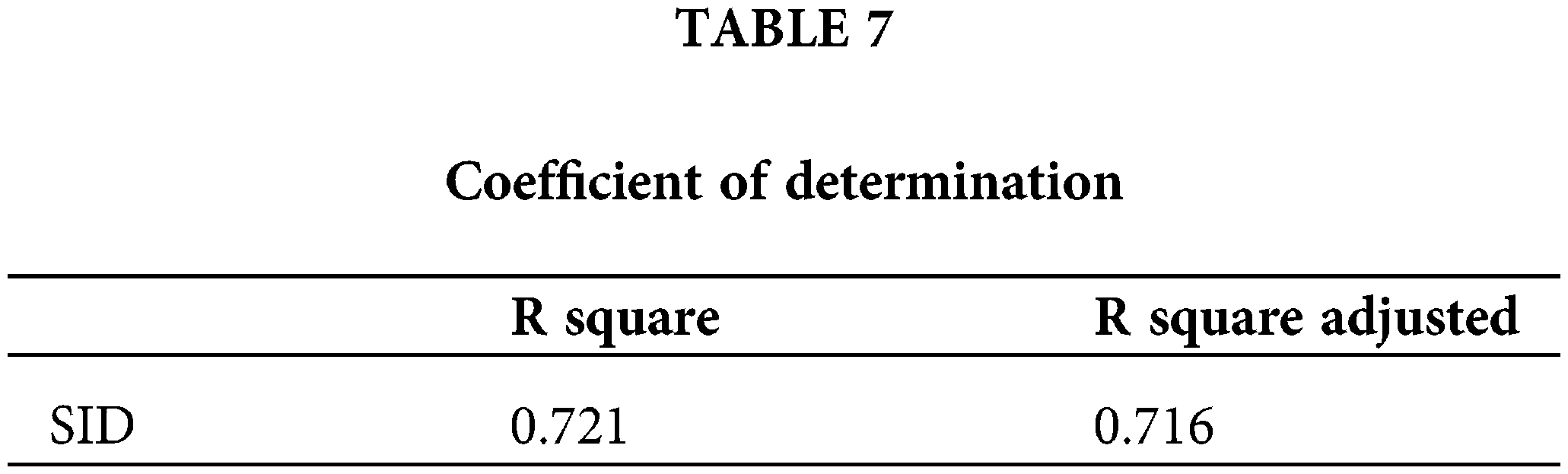
The extent to which causal relationship is concerned, R Square (coefficient of determination) establishes that 72 percent variation in criterion variable (Suicide Ideation) is explained with the variation in predictive variables (SS, SI, HF and DV) (Table 7).
The coefficients of inferential statistics substantiate all the hypotheses of the study (Table 8). Our first hypothesis (social stigma generates suicidal ideation) is proven and significant at p = 0.05. T statistics for this relationship (2.665) provide sufficient evidence against the null hypothesis and confirm the significance of outer model loading. The path coefficient (0.251) exhibits a positive impact of SS on SID; however, the impact is not that strong.
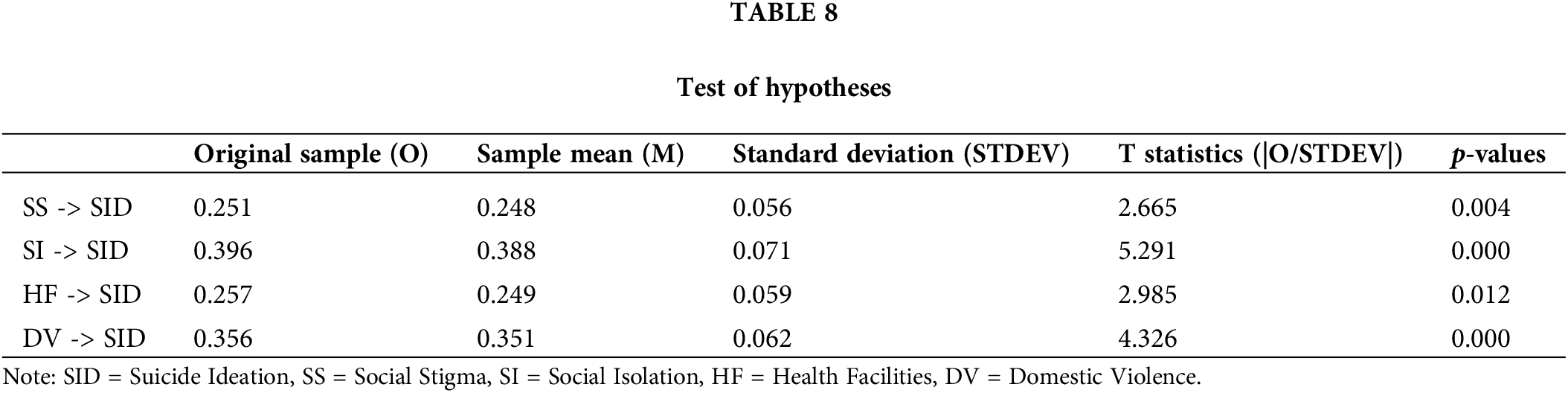
The second hypothesis (H2) assuming that social isolation is one of the causes of suicidal ideation is accepted. Path coefficient for this hypothesis (0.396) shows that social isolation (SI) is the highest contributor to suicidal ideation (SID) among all the variables of the study. It is significant as per the p-value, as T statistics (5.291) show the significance of outer model loading and reject the null hypothesis.
The third hypothesis (H3) assuming that lack of health facilities add to suicidal ideation has been substantiated. The scarcity of healthcare services impacts suicidal ideation, but not profoundly. Path coefficient (0.257) indicates a positive impact of HF on SID; however, the degree of intensity of the relationship is moderate. Other indicators like p-value and t value establish a causal relationship between these variables.
The fourth hypothesis (H4) assuming that domestic violence causes suicidal ideation became true. Domestic violence (DV) significantly enhances or generates suicidal ideation (SID). Path coefficient (0.356) indicates the existence of the considerable relationship, p-value at 0.000 indicates that the relationship is significant, and T statistics substantiate that outer model loading is significant and provides sufficient evidence against the null hypothesis.
The indigenous people living in the Himalayan range constitute a tiny part of the overall world population of indigenous people. These indigenous people inherit distinct values, norms, and overall lifestyles [80]. The culture and indigeneity of these people are on the brink of extinction. The unavailability and scarcity of even basic needs including food, health, and education have compelled the indigenous community to move to urban sites in search of living a prosperous life [81]. Consequently, urban cultures penetrate and indigenous culture is being overridden [82]. In addition to this, the rate of suicide is on the increasing trend among the indigenous community. Unfortunately, no intervention is in place to protect the culture and lives of these indigenous people. Suicide is a growing and tragic social problem faced by the indigenous community, and negligible attention has been given in terms of understanding, policy-making, and institutional interventions. Rigorous literature and valid data on suicide are almost nonexistent [5], so an effective solution has not been devised. The seminal work by Ullah et al. [2] and the present study have identified causes of suicide that can be managed, and the suicide rate can be brought down to the lowest levels.
Social stigma is found to be one of the triggering factors of suicide ideation. Generally, the literature identifies stigma with reference to suicide as social disapproval or shame as a result of attempted or unsuccessful suicides [23,44]. This kind of stigma drives a person again towards suicide, but this time to escape this stigma. The study finds diverse types of stigmas that lead to suicide ideation. We found many cases of suicide ideation due to social stigmas, but we did not find even a single case of stigma due to failed suicide attempts. We found that other social stigmas such as divorce, caught in a crime like theft, the stigma of addiction, the stigma of belonging to the lowest (least respectable) cast, the stigma of having illegitimate or extramarital sexual relations, or the stigma of bearing an illegitimate child also lead to suicidal ideation and eventually completed suicides. Our results indicate that stigma of any nature can lead to suicidal behaviors. social stigmas do affect suicidal ideation positively; however, the intensity of effect remained the lowest among all the variables of our research model. The findings of our study are consistent with the literature [23,83–84], however, the contexts of these studies differ significantly in terms of socio-cultural and economic dynamics.
Social Isolation was found to be a strong reason for suicide in the given context. Social isolation is an unnoticed evil that causes many psychological ailments. Previous studies indicate a causal relationship between social isolation and suicidal ideation or suicide [38,85]. Our study finds that not only does society isolate its members but also, in many cases, individuals suffer from self-created social isolation. We found most of the respondents suffered from either self-created or imposed social isolation. As a result, they can neither share their feelings nor receive counseling on how to manage their problems. Individuals think more and more of their problems in isolation, and the psychological impacts of these problems become more severe. The findings of the study are partially consistent with the findings of previous researches as imposed isolation leads to suicide ideation or suicide behaviour [86–90], however, existing literature does not address the correlation between self-created isolation and suicidal thoughts or outcomes. Typically, social isolation is observed as a consequence of depression, anxiety, or other mental disorders. As such, it appears that social isolation may act as a mediator between mental health issues and the occurrence of suicidal outcomes.
The availability of adequate and timely healthcare facilities plays a key role in managing suicidal thoughts. Any problem, irrespective of its nature, creates psychological disorder and acute psychological disorder may lead to suicidal behaviors [91]. The availability of mental healthcare facilities including neurological, psychological and psychiatric therapies will help neutralize the adverse impact of the causes of suicide [2]. Previous studies have yielded comparable results. The healthcare facilities are generally accessible in most parts of the world, enabling patients with mental disorders to receive appropriate treatment and recover from their ailments [92–94]. However, the situation is markedly different in the given region, where mental healthcare facilities are scarce or practically non-existent [95–97]. Consequently, treatable mental disorders tragically progress into fatal conditions, and the presence of social stigma surrounding mental illness further amplifies the likelihood of suicidal outcomes. Recognizing the pivotal role of mental healthcare facilities in reducing suicide rates and addressing the repercussions of mental disorders is crucial [98]. Nevertheless, it remains disheartening that this vital aspect is still largely overlooked or neglected. Domestic violence is another powerful cause of suicide that is usually found in extended families [2,99]. Domestic violence is prevalent in the area, and certain violence is socially acceptable, even desirable. For instance, it is believed that parents, husbands, and mother/fathers-in-law have the right to be violent, and children and wives should obediently accept the violence. There are no proper platforms where a complaint against violence can be registered. Most female suicide cases in the area were caused by domestic violence. Our findings were consistent with the related literature as a leading factor of suicide.
In the population under consideration, it is essential to consider alternative explanations for suicide. Researchers worldwide have identified various potential causes of suicidal behaviors, including academic setbacks, economic conditions, social status, marital disharmony, social injustices, inheritance issues, sudden shocks, drug addiction and the collapse of love affairs [100–104]. These factors might also be present and influential within the given indigenous community. Therefore, it becomes imperative to conduct comprehensive studies to gain a deeper understanding of the phenomenon of suicide in the region. By exploring these factors and their impact, we can better address the complexities surrounding suicide and develop targeted interventions to prevent and support those at risk within the indigenous population.
Indigenous people of the Himalayan range in northern Pakistan face tremendous problems [105,106], and the rising trend of suicide is one of them. The present study aims at identifying some of the causes of suicide ideation. To begin with, individuals with suicidal ideation were contacted for data collection. Based on discussion with respondents and literature review we identified social stigma, social isolation, lack of healthcare facilities, and domestic violence as potential causes of suicide ideation. Our data verified that all these variables were the causes of suicide ideation with social isolation and domestic violence being prominent. The study produced some interesting and novel results. Firstly, social stigma is not solely responsible for suicide attempts; other social stigmas can also lead to suicide. Illegal sexual relationships, conceiving an illegitimate child, theft, addiction, divorce, and slavery were found as prevalent social stigmas that often lead to suicide ideation. The majority of the respondents were found to be mentally out of the social circle. They neither can share their sufferings with others nor get counseling to manage their problems. Under such conditions the adverse effects of the problems multiply. Furthermore, healthcare facilities to treat mental disorders are almost nonexistent. Curable mental disorders including depression usually remain untreated and cause suicidal behaviors. In addition, domestic violence is common in the region and the major cause of suicide. Domestic violence is usually found in extended families. Finally, economic issues, improper division of work, and tug of war for resources in joint families cause domestic violence. In many cases, domestic violence is socialized and treated as a normal part of family affairs.
Due to its highly intricate nature, suicide and suicide ideation cannot be fully elucidated by a mere few variables. The underlying causes may exhibit variations across different time periods, geographical locations, and societies. Consequently, the findings of the study may have limitations in terms of generalizability, necessitating the inclusion of additional factors and a context-sensitive approach in future research endeavors. Despite these limitations, the study’s findings offer valuable insights for policymakers and interventionists, contributing valuable inputs to address this complex issue.
Although the suicide rate in the given region is increasing year by year, this tragic problem remains unattended. The causes of suicide identified in this research are quite manageable, and effective intervention will surely mitigate the problem of suicide. Keeping in view our findings, we present the following recommendations:
• Domestic violence is identified as the leading cause of suicide and it is more prevalent in extended families. The culture of the joint family system needs to be restructured into small units to avoid domestic violence and other familial complications. Domestic violence should be declared an unlawful and punishable crime. Laws and public policies are to be formulated and implemented to curb domestic violence through law-enforcement agencies. Complaint centers should be established where complaints against such violence can be registered.
• Social isolation is one of the prime reasons for suicide. Individuals with suicidal ideation were found to be mentally isolated. This isolation multiplies the incidences of suicides. Hospitals should provide services of psychologists to counsel and provide psychological therapies. Government and NGOs should establish counseling and rehabilitation centers where individuals with psychological ailments will share their problems and get advice to cope with them.
• Existing healthcare facilities do not contain neurological, psychological, and psychiatric therapies, and such patients must move to other cities for treatment. Therefore, this treatment becomes too expensive to be afforded by common people. The provision of specialized neurological and psychiatric treatments will significantly reduce the occurrences of suicide. Placement of neurologists, psychologists, and psychiatrists in the existing public sector hospitals of the locality may yield positive results.
• Social stigma also leads to suicidal ideation. Social stigma is a complex societal phenomenon and it is relatively difficult to reduce it. However, it is not impossible to manage it. Belittlement on the basis of stigma should be held unlawful and punishable behavior. Teachers and religious clerics should include this topic in their teachings and sermons to educate people regarding the negative impacts of placing a stigma on someone.
The findings of the study have implications for public policymakers, healthcare providers, researchers and NGO managers who are directly or indirectly connected to public health. The study has uncovered some of the facts that previous literature did not explain. For instance, some new dimensions of social stigma were added to related literature. Self-created isolation has also been identified as a dimension of social isolation. The model we tested was somewhat novel in terms of combining these variables into one model to explain suicide ideation. Regarding the practical implications, the study offers significant recommendations for various stakeholders. Firstly, government organizations and health-focused NGOs should prioritize the provision of healthcare facilities, including mental health services. By offering proper and timely treatment for mental disorders, the overall mental well-being of individuals can be improved, subsequently reducing suicidal behaviors. Secondly, rehabilitation centers have a role to play in extending their counseling services to individuals experiencing mental depression. Assisting these individuals in maximizing their social connectedness can prove beneficial in their journey towards recovery.
Thirdly, educational institutions can leverage the study’s findings to develop strategies that foster awareness and understanding of mental health issues. Moreover, educational institutions have the opportunity to conduct extensive awareness campaigns about the causes, consequences, and remedies for suicide. Raising awareness about this critical issue can contribute to reducing stigma and encouraging open discussions about mental health.
Lastly, considering the region’s religious inclination, religious centers and clergy can play a pivotal role in creating awareness through their sermons. Utilizing their influence, they can promote understanding and compassion towards mental health challenges, ultimately helping to reduce the prevalence of suicide.
In summary, the study’s practical implications offer valuable guidance to various stakeholders. By heeding these recommendations, government organizations, NGOs, rehabilitation centers, educational institutions, religious centers, and clergy can all contribute to a more supportive and compassionate society that addresses mental health challenges and reduces the occurrence of suicide.
Limitations and future research
Like all other research studies, this investigation has its limitations. However, these limitations present opportunities for future research. Firstly, the sample used may not be fully representative, which hinders the generalizability of the findings. The study focused on mentally ill patients who scored 21 or more on SIDAS, but this subgroup may not accurately represent the entire population of mentally ill patients. Future research could aim to include a more diverse population facing various health-related challenges.
Secondly, due to the complexity of suicide and suicide ideation, this study could not encompass all potential alternative explanations. Factors such as academic setbacks, marital disharmony, financial issues, unequal distribution of inherited properties, and the impact of incurable diseases on mental health leading to suicide ideation were not fully considered. Incorporating these factors in future studies would provide a more comprehensive understanding of the issue, benefiting policymakers and institutions seeking to address this problem effectively.
Thirdly, the study relied on cross-sectional data and is thus limited to a particular time of measurement. So, it does not help determine cause and effect relationship in a true sense. Employing a longitudinal approach in future research would allow a more thorough analysis of temporal effects, letting for a better understanding of cause and effect dynamics.
Acknowledgement: The authors thank research participants for their participation in this study.
Funding Statement: This work was supported by Institute of Information & Communications Technology Planning & Evaluation (IITP) under the Metaverse Support Program to Nurture the Best Talents (IITP-2023-RS-2023-00254529) grant funded by the Korea government (MSIT).
Author Contributions: Study conception by ZU and EA; Design by FA and HH; analysis and interpretation of results by ZU, BLC and FA; complete the final version of the manuscript by ZU, EA, and HH.
Availability of Data and Materials: The data will be provided upon request to the corresponding author.
Ethics Approval: The authors adhered to the ethical norms outlined in the Helsinki Declaration.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Värnik P. Suicide in the world. Int J Environ Res Public Health. 2012;9(3):760–71. [Google Scholar]
2. Ullah Z, Shah NA, Khan SS, Ahmad N, Scholz M. Mapping institutional interventions to mitigate suicides: a study of causes and prevention. Int J Environ Res Public Health. 2021;18(20):10880. [Google Scholar] [PubMed]
3. Lester D. Suicide and culture. Understanding suicide: a global issue. CA, USA: ABC-CLIO; 2013. p. 209–32. [Google Scholar]
4. Ghazal L, Arthur D, Hussain S, Khudadad U, Malik G, Ali ZZ. Cry for help: perceptions of young adults on suicide from northern Pakistan. Khyber Med Univ J. 2021;13(2):54–9. [Google Scholar]
5. Khan MM. Suicide prevention in Pakistan: an impossible challenge? JPMA J Pak Med Assoc. 2007;57(10):478–80. [Google Scholar] [PubMed]
6. Shah A, Bhat R. The relationship between elderly suicide rates and mental health funding, service provision and national policy: a cross-national study. Int Psychogeriatr. 2008;20(3):605–15. [Google Scholar] [PubMed]
7. Snowdon J, Choi NG. Undercounting of suicides: where suicide data lie hidden. Glob Public Health. 2020;15(12):1894–901. [Google Scholar] [PubMed]
8. Arensman E, Scott V, de Leo D, Pirkis J. Suicide and suicide prevention from a global perspective. Crisis. 2020;1:9–14. [Google Scholar]
9. Vuong QH, Nguyen MH, Le TT. A mindsponge-based investigation into the psycho-religious mechanism behind suicide attacks. Berlin, Germany: Walter de Gruyter GmbH; 2021. [Google Scholar]
10. Duncan S, Luce A. Using the responsible suicide reporting model to increase adherence to global media reporting guidelines. Journalism. 2020;23(5):1132–48. [Google Scholar]
11. Kim HHS, Chun J. Bullying victimization, school environment, and suicide ideation and plan: focusing on youth in low-and middle-income countries. J Adolesc Health. 2020;66(1):115–22. [Google Scholar] [PubMed]
12. Vaz E, Shaker RR, Cusimano MD. A geographical exploration of environmental and land use characteristics of suicide in the greater Toronto area. Psychiatry Res. 2020;287(1):112790. [Google Scholar] [PubMed]
13. Schosser PP-DDA. Brain derived neurotrophic factor-genetic and epigenetic mechanisms with relevance to the major depressive disorder and suicide phenotypes (Doctoral Thesis). Vienna: Medical University of Vienna. 2020. [Google Scholar]
14. Katz C, Bolton J, Sareen J. The prevalence rates of suicide are likely underestimated worldwide: why it matters. Soc Psychiatry Psychiatr Epidemiol. 2016;51(1):125–7. [Google Scholar] [PubMed]
15. Glenn CR, Kleiman EM, Kellerman J, Pollak O, Cha CB, Esposito EC, et al. Annual research review: a meta-analytic review of worldwide suicide rates in adolescents. J Child Psychol Psychiatry. 2020;61(3):294–308. [Google Scholar] [PubMed]
16. World Health Organization. Suicide worldwide in 2019: global health estimates. 2021. [Google Scholar]
17. Pitman A, Osborn D, King M, Erlangsen A. Effects of suicide bereavement on mental health and suicide risk. Lancet Psychiatry. 2014;1(1):86–94. [Google Scholar] [PubMed]
18. Cerel J, Sanford RL. It’s not who you know, it’s how you think you know them: suicide exposure and suicide bereavement. Psychoanal Study Child. 2018;71(1):76–96. [Google Scholar]
19. Kučukalić S, Kučukalić A. Stigma and suicide. Psychiatria Danubina. 2017;29(suppl 5):895–9. [Google Scholar] [PubMed]
20. Beautrais AL. Risk factors for suicide and attempted suicide among young people. Austr N Zeal J Psychiatry. 2000;34(3):420–36. [Google Scholar]
21. Vijayakumar L, Rajkumar S. Are risk factors for suicide universal? A case-control study in India. Acta Psychiatr Scand. 1999;99(6):407–11. [Google Scholar] [PubMed]
22. Fleischmann A, de Leo D. The World Health Organization’s report on suicide: a fundamental step in worldwide suicide prevention. Crisis. 2014;35(5):289–91. [Google Scholar] [PubMed]
23. Cvinar JG. Do suicide survivors suffer social stigma: a review of the literature. Perspect Psychiatr Care. 2005;41(1):14–21. [Google Scholar] [PubMed]
24. Souza MLPd, Orellana JDY. Suicide among the indigenous people in Brazil: a hidden public health issue. Brazil J Psychiatry. 2012;34(4):489–90. [Google Scholar]
25. Chapple A, Ziebland S, Hawton K. Taboo and the different death? Perceptions of those bereaved by suicide or other traumatic death. Sociol Health Illness. 2015;37(4):610–25. [Google Scholar]
26. Platt S, Arensman E, Rezaeian M. National suicide prevention strategies-progress and challenges. Hogrefe Publishing; 2019. [Google Scholar]
27. Iskander JK, Crosby AE. Implementing the national suicide prevention strategy: time for action to flatten the curve. Prev Med. 2021;152:106734. [Google Scholar] [PubMed]
28. Shneidman E. Definition of suicide. Brooklyn, NY, USA: Jason Aronson, Incorporated; 1977. [Google Scholar]
29. Shneidman ES. Commentary: suicide as psychache. J Nerv Ment Dis. 1993;181(3):145–47. [Google Scholar] [PubMed]
30. Durkheim E. Suicide: a study in sociology, 1897. New York: The Free Press; 1951. [Google Scholar]
31. Baumeister RF. Suicide as escape from self. Psychol Rev. 1990;97(1):90. [Google Scholar] [PubMed]
32. Beck A. Depression. New York: Harper and Row; 1967. [Google Scholar]
33. Abramson LY, Alloy LB, Hogan ME, Whitehouse WG, Gibb BE, Hankin BL, et al. The hopelessness theory of suicidality. In Suicide Science. NY, USA: Springer; 2002. pp. 17–32. [Google Scholar]
34. Klonsky ED, May AM. The three-step theory (3STa new theory of suicide rooted in the ideation-to-action framework. Int J Cogn Ther. 2015;8(2):114–29. [Google Scholar]
35. Room R. Stigma, social inequality and alcohol and drug use. Drug Alcohol Rev. 2005;24(2):143–55. [Google Scholar] [PubMed]
36. Dardas L, Simmons LA. The stigma of mental illness in Arab families: a concept analysis. J Psychiatr Ment Health Nurs. 2015;22(9):668–79. [Google Scholar] [PubMed]
37. Cacioppo JT, Hawkley LC, Norman GJ, Berntson GG. Social isolation. Ann N Y Acad Sci. 2011;1231(1):17–22. [Google Scholar] [PubMed]
38. Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends Cogn Sci. 2009;13(10):447–54. [Google Scholar] [PubMed]
39. Ullah Z, Khan MZ, Khan MA. Towards service quality measurement mechanism of teaching hospitals. Int J Healthc Manag. 2021;14(4):1435–40. [Google Scholar]
40. Walby S. The cost of domestic violence. 2004. Available from: https://openaccess.city.ac.uk/id/eprint/21695/ [Accessed 2022]. [Google Scholar]
41. Smith LJ. Domestic violence: an overview of the literature. London, UK: HM Stationery Office; 1989. [Google Scholar]
42. Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the scale for suicide ideation. J Consult Clin Psychol. 1979;47(2):343–52. [Google Scholar] [PubMed]
43. Rimkeviciene J, Hawgood J, O’Gorman J, de Leo D. Personal stigma in suicide attempters. Death Stud. 2015;39(10):592–9. [Google Scholar] [PubMed]
44. Hanschmidt F, Lehnig F, Riedel-Heller SG, Kersting A. The stigma of suicide survivorship and related consequences—A systematic review. PLoS One. 2016;11(9):e0162688. [Google Scholar] [PubMed]
45. Wang J, Lloyd-Evans B, Giacco D, Forsyth R, Nebo C, Mann F, et al. Social isolation in mental health: a conceptual and methodological review. Social Psychiatry Psychiatr Epidemiol. 2017;52(12):1451–61. [Google Scholar]
46. Kim U, Bhullar N. Life in the pandemic: social isolation and mental health. J Clin Nurs. 2020;29(15–16):2756–7. doi:10.1111/jocn.15290. [Google Scholar] [PubMed] [CrossRef]
47. Mennicke A, Kaniuka AR, Pruneda P, Cramer RJ. Substance use-related suicide after release from correctional, behavioral health, and healthcare facilities using national violent death reporting system data. Suicide Life-Threat Behav. 2021;52:132–46. [Google Scholar] [PubMed]
48. Dagliana G, Albolino S, Belloni L, Bellandi T. Reducing the risk of patient suicide in Tuscany. BJPsych Int. 2020;17(4):82–5. [Google Scholar] [PubMed]
49. Anjum A, Ali TS, Pradhan NA, Khan M, Karmaliani R. Perceptions of stakeholders about the role of health system in suicide prevention in Ghizer, Gilgit-Baltistan, Pakistan. BMC Public Health. 2020;20(1):1–14. [Google Scholar]
50. Kavak F, Aktürk Ü., Özdemir A, Gültekin A. The relationship between domestic violence against women and suicide risk. Arch Psychiatr Nurs. 2018;32(4):574–9. [Google Scholar] [PubMed]
51. Butz D. Sustaining indigenous communities: symbolic and instrumental dimensions of pastoral resource use in Shimshal, Northern Pakistan. Can Geographer/Le Géographe Can. 1996;40(1):36–53. [Google Scholar]
52. Kiran M, Rana MH, Azhar M. Posttraumatic growth amongst survivors of a suicide bombing attack in Northern Pakistan. J Pak Psychiatr Soc. 2010;7(1):29. [Google Scholar]
53. van Spijker BA, Batterham PJ, Calear AL, Farrer L, Christensen H, Reynolds J, et al. The suicidal ideation attributes scale (SIDAScommunity-based validation study of a new scale for the measurement of suicidal ideation. Suicide Life-Threat Behav. 2014;44(4):408–19. [Google Scholar] [PubMed]
54. Batterham PJ, Calear AL, Christensen H. The stigma of suicide scale. Crisis. 2013;34:13–21. [Google Scholar] [PubMed]
55. Cornwell EY, Waite LJ. Measuring social isolation among older adults using multiple indicators from the NSHAP study. J Gerontol Series B: Psychol Sci Soc Sci. 2009;64(suppl_1):i38–46. [Google Scholar]
56. Haggerty JL, Levesque JF. Validation of a new measure of availability and accommodation of health care that is valid for rural and urban contexts. Health Expect. 2017;20(2):321–34. [Google Scholar] [PubMed]
57. AlDhaen E. Awareness of occupational health hazards and occupational stress among dental care professionals: evidence from the GCC region. Front Public Health. 2022;10:922748. [Google Scholar] [PubMed]
58. Guan X, Ahmad N, Sial MS, Cherian J, Han H. CSR and organizational performance: the role of pro-environmental behavior and personal values. Corp Soc Responsib Environ Manag. 2023;30(2):677–94. [Google Scholar]
59. Ahmad N, Ullah Z, AlDhaen E, Han H, Scholz M. A CSR perspective to foster employee creativity in the banking sector: the role of work engagement and psychological safety. J Retail Consum Serv. 2022;67:102968. [Google Scholar]
60. Ahmad N, Ullah Z, AlDhaen E, Han H, Araya-Castillo L, Ariza-Montes A. Fostering hotel-employee creativity through micro-level corporate social responsibility: a social identity theory perspective. Front Psychol. 2022;13:853125. [Google Scholar] [PubMed]
61. Ahmad N, Ahmad A, Siddique I. Responsible tourism and hospitality: the intersection of altruistic values, human emotions, and corporate social responsibility. Admin Sci. 2023;13(4):105. [Google Scholar]
62. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. [Google Scholar]
63. Fu Q, Cherian J, Ahmad N, Scholz M, Samad S, Comite U. An inclusive leadership framework to foster employee creativity in the healthcare sector: the role of psychological safety and polychronicity. Int J Environ Res Public Health. 2022;19(8):4519. [Google Scholar] [PubMed]
64. Ahmad N, Ullah Z, Ryu HB, Ariza-Montes A, Han H. From corporate social responsibility to employee well-being: navigating the pathway to sustainable healthcare. Psychol Res Behav Manag. 2023;16:1079–95. [Google Scholar] [PubMed]
65. Zhou X, Ahmad N, Lho LH, Han H. Social ripple: unraveling the impact of customer relationship management via social media on consumer emotions and behavior. Soc Behav Pers. 2023;51(10):1–12. [Google Scholar]
66. Liu Y, Cherian J, Ahmad N, Han H, de Vicente-Lama M, Ariza-Montes A. Internal corporate social responsibility and employee burnout: an employee management perspective from the healthcare sector. Psychol Res Behav Manag. 2023;16:283–302. [Google Scholar] [PubMed]
67. Ahmad N, Ullah Z, AlDhaen E, Han H, Ariza-Montes A, Vega-Muñoz A. Fostering advocacy behavior of employees: a corporate social responsibility perspective from the hospitality sector. Front Psychol. 2022;13:865021. [Google Scholar] [PubMed]
68. Deng Y, Cherian J, Ahmad N, Scholz M, Samad S. Conceptualizing the role of target-specific environmental transformational leadership between corporate social responsibility and pro-environmental behaviors of hospital employees. Int J Environ Res Public Health. 2022;19(6):3565. [Google Scholar] [PubMed]
69. Peng J, Samad S, Comite U, Ahmad N, Han H, Ariza-Montes A, et al. Environmentally specific servant leadership and employees’ energy-specific pro-environmental behavior: evidence from healthcare sector of a developing economy. Int J Environ Res Public Health. 2022;19(13):7641. [Google Scholar] [PubMed]
70. Chen J, Ghardallou W, Comite U, Ahmad N, Ryu HB, Ariza-Montes A, et al. Managing hospital employees’ burnout through transformational leadership: the role of resilience, role clarity, and intrinsic motivation. Int J Environ Res Public Health. 2022;19(17):10941. [Google Scholar] [PubMed]
71. Wong KK-K. Partial least squares structural equation modeling (PLS-SEM) techniques using SmartPLS. Market Bull. 2013;24(1):1–32. [Google Scholar]
72. Xu L, Mohammad SJ, Nawaz N, Samad S, Ahmad N, Comite U. The role of CSR for de-carbonization of hospitality sector through employees: a leadership perspective. Sustainability. 2022;14(9):5365. [Google Scholar]
73. Ahmad N, Scholz M, AlDhaen E, Ullah Z, Scholz P. Improving firm’s economic and environmental performance through the sustainable and innovative environment: evidence from an emerging economy. Front Psychol. 2021;12:651394. [Google Scholar] [PubMed]
74. Fornell C, Larcker DF. Structural equation models with unobservable variables and measurement error: algebra and statistics. Los Angeles, CA: Sage Publications Sage CA; 1981. [Google Scholar]
75. Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acade Mark Sci. 2015;43(1):115–35. [Google Scholar]
76. HairJr JF, Sarstedt M, Hopkins L, Kuppelwieser VG. Partial least squares structural equation modeling (PLS-SEM). Eur Bus Rev. 2014;26:106–21. [Google Scholar]
77. Gold S, Heesen C, Schulz H, Guder U, Mönch A, Gbadamosi J, et al. Disease specific quality of life instruments in multiple sclerosis: validation of the Hamburg quality of life questionnaire in multiple sclerosis (HAQUAMS). Mult Scler J. 2001;7(2):119–30. [Google Scholar]
78. Belsley DA, Kuh E, Welsch RE. Regression diagnostics: identifying influential data and sources of collinearity. NJ, USA: John Wiley & Sons; 2005. [Google Scholar]
79. Kock N, Lynn G. Lateral collinearity and misleading results in variance-based SEM: an illustration and recommendations. J Assoc Inf Syst. 2012;13(7):546–80. [Google Scholar]
80. Sargent S. Transnational networks and United Nations human rights structural change: the future of indigenous and minority rights. Int J Hum Rights. 2012;16(1):123–51. [Google Scholar]
81. Skinner K, Pratley E, Burnett K. Eating in the city: a review of the literature on food insecurity and Indigenous people living in urban spaces. Societies. 2016;6(2):7. [Google Scholar]
82. Ali SS, Rehman J. Indigenous peoples and ethnic minorities of Pakistan: constitutional and legal perspectives. Oxfordshire, UK: Routledge; 2013. [Google Scholar]
83. Islam MR, Hossain MJ. Social stigma and suicide in Bangladesh: the COVID-19 has worsened the situation. Chronic Stress. 2021;5:24705470211035602. [Google Scholar] [PubMed]
84. Feigelman W, Gorman BS, Jordan JR. Stigmatization and suicide bereavement. Death Stud. 2009;33(7):591–608. [Google Scholar] [PubMed]
85. House JS. Social isolation kills, but how and why? Psychosom Med. 2001;63(2):273–4. [Google Scholar] [PubMed]
86. Trout DL. The role of social isolation in suicide. Suicide Life-Threat Behav. 1980;10(1):10–23. [Google Scholar] [PubMed]
87. Calati R, Ferrari C, Brittner M, Oasi O, Olié E, Carvalho AF, et al. Suicidal thoughts and behaviors and social isolation: a narrative review of the literature. J Affect Disord. 2019;245:653–67. [Google Scholar] [PubMed]
88. Motillon-Toudic C, Walter M, Séguin M, Carrier J-D, Berrouiguet S, Lemey C. Social isolation and suicide risk: literature review and perspectives. Eur Psychiatry. 2022;65(1):1–42. [Google Scholar]
89. Heuser C, Howe J. The relation between social isolation and increasing suicide rates in the elderly. Qual Ageing Older Adults. 2019;20(1):2–9. [Google Scholar]
90. Lay-Yee R, Matthews T, Moffitt T, Poulton R, Caspi A, Milne B. Are trajectories of social isolation from childhood to mid-adulthood associated with adult depression or suicide outcomes. Soc Psychiatry Psychiatr Epidemiol. 2023;58(3):373–82. [Google Scholar] [PubMed]
91. Grover KE, Green KL, Pettit JW, Monteith LL, Garza MJ, Venta A. Problem solving moderates the effects of life event stress and chronic stress on suicidal behaviors in adolescence. J Clin Psychol. 2009;65(12):1281–90. [Google Scholar] [PubMed]
92. Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clin Psychol Sci. 2013;1(2):170–91. [Google Scholar]
93. Jacob K, Sharan P, Mirza I, Garrido-Cumbrera M, Seedat S, Mari JJ, et al. Mental health systems in countries: where are we now? Lancet. 2007;370(9592):1061–77. [Google Scholar] [PubMed]
94. Rathod S, Pinninti N, Irfan M, Gorczynski P, Rathod P, Gega L, et al. Mental health service provision in low-and middle-income countries. Health Serv Insights. 2017;10:1178632917694350. [Google Scholar] [PubMed]
95. Javed A, Khan MNS, Nasar A, Rasheed A. Mental healthcare in Pakistan. Taiwan J Psychiatry. 2020;34(1):6–14. [Google Scholar]
96. Saraceno B, van Ommeren M, Batniji R, Cohen A, Gureje O, Mahoney J, et al. Barriers to improvement of mental health services in low-income and middle-income countries. Lancet. 2007;370(9593):1164–74. [Google Scholar] [PubMed]
97. Dixon A, McDaid D, Knapp M, Curran C. Financing mental health services in low-and middle-income countries. Health Policy Plan. 2006;21(3):171–82. [Google Scholar] [PubMed]
98. Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370(9590):859–77. [Google Scholar] [PubMed]
99. Haqqi S. Suicide and domestic violence: could there be a correlation? Medsc J Med. 2008;10(12):287. [Google Scholar]
100. Memari A, Ramim T, Amirmoradi F, Khosravi K, Godarzi Z. Causes of suicide in married women. Hayat. 2006;12(1):47–53. [Google Scholar]
101. Lester D, Bean J. Attribution of causes to suicide. J Soc Psychol. 1992;132(5):679–80. [Google Scholar] [PubMed]
102. Hicks MHR, Bhugra D. Perceived causes of suicide attempts by UK South Asian women. Am J Orthopsychiatry. 2003;73(4):455–62. [Google Scholar] [PubMed]
103. Millner AJ, Robinaugh DJ, Nock MK. Advancing the understanding of suicide: the need for formal theory and rigorous descriptive research. Trends Cogn Sci. 2020;24(9):704–16. [Google Scholar] [PubMed]
104. Emamgholipour S, Arab M, Shirani R. Socioeconomic determinants of suicide in Iran: panel data study. Iran J Public Health. 2021;50(11):2309. [Google Scholar] [PubMed]
105. Yeats R, Lawrence R editors. Tectonics of the Himalayan thrust belt in Northern Pakistan. US-Pakistan Workshop on Marine Sciences in Pakistan. USA: NASA/ADS; 1982. [Google Scholar]
106. Majeed R, Khan MA, Fatima SU, Mahmood N, Sulman N, Shaukat SS. Public health status and socioeconomic conditions in climate change-affected northern areas of Pakistan. Int J Biol Biotechnol. 2020;17:307–17. [Google Scholar]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools