 Open Access
Open Access
ARTICLE
Short-Term Mindfulness Intervention on Adolescents’ Negative Emotion under Global Pandemic
1 Northwest Normal University, Lanzhou, 730070, China
2 Hongkong Baptist University, Hong Kong, 999077, China
3 Faculty of Education, University of Malaya, Kuala Lumpur, 50605, Malaysia
* Corresponding Authors: Yue Yuan. Email: ; Aibao Zhou. Email:
International Journal of Mental Health Promotion 2023, 25(4), 563-577. https://doi.org/10.32604/ijmhp.2023.022161
Received 25 May 2022; Accepted 15 September 2022; Issue published 01 March 2023
Abstract
Objective: In this research, we tried to explore how short-term mindfulness (STM) intervention affects adolescents’ anxiety, depression, and negative and positive emotion during the COVID-19 pandemic. Design: 10 classes were divided into experiment groups (5 classes; n = 238) and control (5 classes; n = 244) randomly. Hospital Anxiety and Depression Scale (HADS) and Positive and Negative Affect Schedule (PANAS) were used to measure participants’ dependent variables. In the experiment group, we conducted STM practice interventions every morning in their first class from March to November 2020. No interventions were conducted in the control group. Methods: Paired-sample t-tests were used to identify if a significant difference exists between every time point of the experimental and control groups. Repeated ANOVA and Growth Mixture Model (GMM) were used to analyze the tendency of positive and negative emotions, anxiety, and depression in the experimental group. Results and Conclusions: (1) With the intervention of STM, there was a significant decrease in negative emotions and an increase in positive emotions in the experimental group, whereas there were non-significant differences in the control group. (2) To explore the heterogeneity trajectories of dependent variables, we built a GMM and found there were two latent growth classes in the trajectories. (3) The results of the models showed their trajectories were downward, which meant that the levels of anxiety, depression, and negative emotions of participants decreased during the STM training period. Nonetheless, the score of positive affect showed upward in three loops of intervention, which indicated that the level of the participants’ positive affect increased through the STM intervention. (4) This research indicated that STM should be given increasing consideration to enhance mental health during the worldwide outbreak of COVID-19.Keywords
The COVID-19 pandemic expanded from Wuhan and spread to more than 200 countries, with millions of people becoming infected and even losing their lives to the disease, thus causing large mental health problems (e.g., depression, anxiety, and posttraumatic stress disorder (PTSD) symptoms) [1–6]. Most research has indicated that individuals’ mental health has been negatively affected by the COVID-19 pandemic [7–9] through a cross-sectional study. Thus, it is vital for psychological research to explore effective and beneficial means to improve individuals’ mental health long-term. This research aimed to explore whether the intervention of short-term mindfulness training is a constructive method for reducing negative emotions (e.g., anxiety and depression) and increasing positive emotions.
1.1 Negative Emotions Influenced by the COVID-19 Pandemic
Anxiety and depressive disorders are two of the largest negative emotional issues evident during the COVID-19 pandemic [1,2,4–6]. One research by Li et al. [10] showed that the rates of anxiety (from 11.4% to 14.7%) and depression (from 21.6% to 26.3%) significantly increased from the outbreak to the remission stage of the COVID-19 in Guangdong Province of China. Besides, research among Chinese college students and the general population during the initial stage of the COVID-19 to widely outbreak indicated the rates of depression significantly increased from 6.9% to 48.3% [2,9,11], while anxiety significantly increased from 7.5% to 36.4% [2,5].
First, the emotion of anxiety is defined as an uncertain threat that triggers emotional, cognitive, and behavioral reactions, which provoke an individual’s attention and prompt them to prepare responses to uncertain threats [12]. The core of anxiety is the experience of uncertain threats. During the period of widespread increases in COVID-19 cases during the pandemic, many people lost their lives to the disease. The disease is highly contagious, and everyone seemed afraid of being infected and uncertain about if they come in contact with the disease. Thus, a large number of people felt anxiety [1]. Individuals with high anxiety are prone to experience uncertain issues with worse consequences. For instance, Dugas et al. [13] showed that participants with high anxiety interpret a headache as a sign of a brain tumor or cancer. Studies on anxiety have found that individuals with high anxiety rarely obtain positive emotions [14] and more easily experience depression [15].
Second, the emotion of depression combined with the internalization of a negative cognitive model affects the enhanced acquisition of negative information over time [16]. This negative cognitive model incurs passive self-referential cognition internalization, leading to worse depressive feelings. In addition, a negative cognitive model can affect appraisals and interpretations of information in a passive way, therefore making a person vulnerable to greater depressive symptoms [17]. Alongside the processing of passive-biased cognition, individuals with depressive feelings encounter a decreased capability to obtain positive emotions [18]. For instance, Pizzagalli et al. [19] selected patients with depression and gave them positive stimuli. They found that compared to non-depressed participants, depressed patients not only showed a blunted response toward positive stimuli and rewards but also lacked positive thinking. Badly, the decreased ability to recognize positive emotions can be persistent in these patients’ minds [20], which results in negative cognition being harder to change. In addition, the lack of positive emotion contributes to negative downward spirals of mood and thinking [21].
1.2 Mindfulness Training Regulates Emotions
Mindfulness can be defined as embodied nonjudgmental attention and lucid awareness of oneself, others, and the environment [22], which originated from Eastern Buddhism. Emotions and cognition tend to be more open and accepted when someone is in the condition of mindfulness [23,24]. Studies have theoretically combined the concept of mindfulness with emotion regulation and have led to the development of the mindfulness emotion regulation model [25,26] to explain why mindfulness is beneficial for decreasing negative and increasing positive emotions. Mindfulness practice advocates a nonjudgmental approach toward all emotions and thoughts. By encouraging an open and nonjudgmental perspective toward negative information, passive information processing biases can be decreased. Simultaneously, mindfulness encourages individuals to recognize and accept all feelings, be they positive, negative, or neutral. By this means, mindfulness may reduce an individual’s negative patterns of cognition as well as increase positive cognition and emotional patterns [27–32].
Not only does the mindfulness emotion regulation model confirm the internal mechanism relationship between mindfulness and emotion, but neurophysiological research on mindfulness and emotion has provided a more objective scientific basis to explain this effect. Mindfulness regulates emotions by changing the balance of the cerebral hemispheres [33], brain activity [34,35], and brain structure [32,36].
In summary, overall statements seem to explain the vital role that mindfulness plays in increasing positive and decreasing negative emotions. Nonetheless, knowledge and empirical research on the dynamic process by which mindfulness decreases negative emotion and enhances positive emotion is still scant, especially during the global COVID-19 pandemic. Thus, this study aimed to explore the dynamic emotional changes associated with mindfulness interventions during the COVID-19 pandemic.
After obtaining approval from the Ethical Committee of Northwest Normal University (Grant Number: 202003016), we contacted the headmaster of middle school X to discuss our research project. Permission for our intervention program was granted, and informed consent was obtained from the selected students and their guardians. G*Power was used to estimate the sample size for a repeated-measures analysis of variance (ANOVA) with experimental and control groups, and four time-points indicated that a total of 73 participants were needed to detect a medium-to-large effect size (f = 0.40) data changes with a type I error rate (alpha) of 0.05, a power of 0.80, and a 0.50 correlation between repeated measures (Heinrich Heine University Düsseldorf). We selected all students in Grade 8 from a total of 10 classes. All selected students and their guardians agreed to participate in this intervention program. We administered the Chinese versions of the Hospital Anxiety and Depression Scale (HADS) and Positive and Negative Affect Schedule (PANAS) to all students using paper in class on March 16th (T1). Then, we randomly divided the 10 classes in each grade into two groups; the experimental group comprised five classes (n = 252; males = 124, females = 128; age: M (SD) = 13.25(0.45)), and the control group comprised five classes (n = 254; males = 129, females = 125; age: M (SD) = 13.35 (0.25)). There was no significant difference in the HADS or PANAS scores between the experimental and control groups at T1 (p > 0.05). In the experimental group, six participants were absent in the first assessment (T2), five participants were absent in the second assessment (T3), three participants were absent in the second assessment (T4), and ten participants were absent in the control group when we performed the assessment in November (T4). Ultimately, there were 238 (males = 118, females = 120; age: M (SD) = 13.50 (0.25)) participants in the experimental group and 244 (males = 127, females = 117; age: M (SD) = 13.35 (0.45)) participants in the control group. Fig. 1 illustrated more details about procedure.
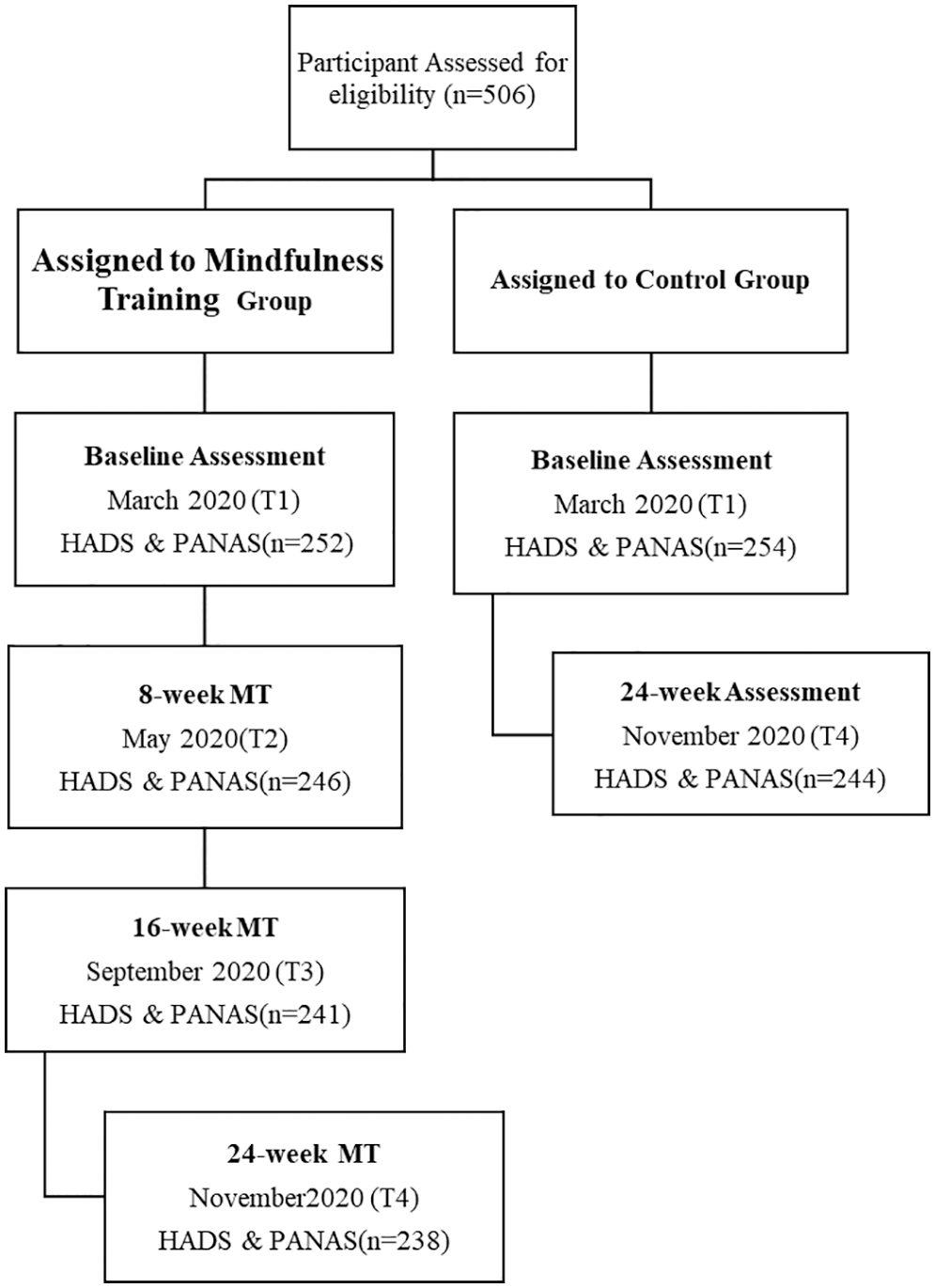
Figure 1: Flow diagram of controlled trial
This intervention study was conducted during the COVID-19 pandemic in China. This study started on March 15, when all students started school after a long period of confinement and a winter holiday. Before March 15th, the area where the sample school was located did not have a case for two weeks. Confinement restrictions were lifted from the area in early March. In addition, this study was conducted on November 27. During the research period, all students studied at school every day. During school, they still faced strict pandemic prevention and control requirements, such as taking body temperature measurements before entering school, not being allowed to gather, wearing masks in class, and so on.
Most research on mindfulness training programs usually lasts 45 min per course [37] or even longer, such as mindfulness-based cognitive therapy (MBCT). This long-period course is a barrier for adolescents, since they live with a full school schedule and multitasking outside of school. Therefore, we abandoned the usual format of a mindfulness training program (for example. Mindfulness-based stress reduction, MBSR and Mindfulness-based Cognitive Therapy, and MBCT). To adapt to our target participants’ local context, we chose the engaged time of mindfulness course to be approximately 10 min. To explore how short-term mindfulness influences adolescents’ emotions in the COVID-19 epidemic context in a long-period training intervention, we played a short-term mindfulness course for three loops in the experimental group. After each round of the course cycle, the participants’ positive and negative emotions, anxiety, and depression were measured.
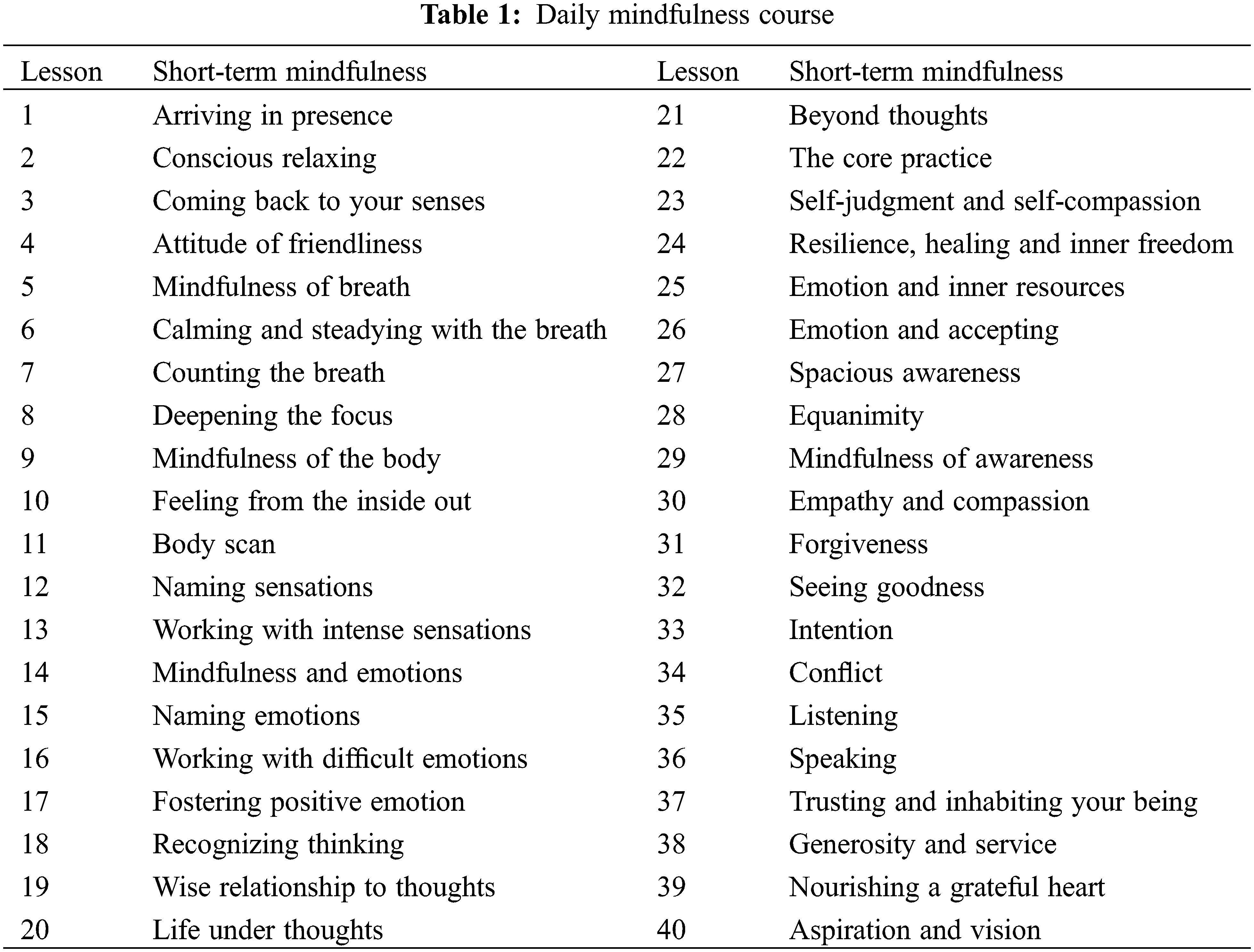
The mindfulness voice media used in this research was from the Daily Mindfulness Course in the Himalayan APP. The daily mindfulness course was developed by respected mindfulness instructors Jack Kornfield and Tara Brach. Two senior Chinese mindfulness instructors, HuiQi Tong and HaiFeng Guo, completed the course’s Chinese version (https://www.ximalaya.com/album/48145271). The Daily Mindfulness Course contains four parts: (1) basic mindfulness (lessons 1 to 13); (2) emotional intelligence (lessons 14 to 21); (3) resilience, healing, and inner freedom (lessons 22 to 29); and (4) mindful living (lessons 30 to 40). Every lesson in this course lasted for approximately 10 min. More details are provided in Table 1.
We conducted short-term mindfulness practice interventions in the experimental group every morning in the first class. Specifically, the researcher sent a daily audio file of short-term mindfulness to head teachers. We trained the head teachers and class monitors in the experimental classes to play the audio. In addition, we put a mindfulness course voice on the DingTalk App so that participants in the experiment could practice mindfulness at home independently. However, no intervention was performed in the control group. In the experimental group, three assessments were performed: after (1) the first loop of the course (8 weeks in May (T2)); (2) the second loop of course (16 weeks in September (T3)); and (3) the third loop of course (24 weeks in November (T4)). No intervention was conducted during the summer holiday between late June and July. In the control group, the assessments were performed only in November (T4).
We conducted short-term mindfulness practice interventions in the class of experiment group every morning in their first class. Specifically, researcher send the daily audio file of short-term mindfulness to the head teachers. And we trained the head teachers and class monitors in experiment classes to play the audio. Also, we put mindfulness course voice on DingTalk App, so participants in experiment can practice mindfulness at home by themselves. Nonetheless, no intervention were conducted in control group. In group of experiment, 3 assessments were performed: (1), after the first loop of course (8 weeks, in May (T2)); (2), the second loop of course (16 weeks, September (T3)); (3), the third loop of course (24 weeks in November (T4)). No intervention were conducted in the summer holiday, which between late June and July. In the control group, we only performed assessments in November (T4).
Depression and Anxiety: The Chinese version of Hospital Anxiety and Depression Scale (HADS) measures depression and anxiety of participants which combine with 7-item anxiety and 7-item depression subscales [38,39]. HADS was used the assess the emotions in the past one month. Total 14 items are scored on a four-point Likert-type scale (0 to 3) and total score is 42, the score of each subscale is 21. Higher scores indicate higher levels of depression or anxiety [39]. In the current study, the Cronbach alpha for anxiety subscale was 0.78 at T1, 0.83 at T2, 0.79 at T3, and 0.85 at T4 while for depression subscale was 0.82 at T1, 0.76 at T2, 0.84 at T3, and 0.79 at T4.
Positive and Negative Affect Schedule: Positive affect and negative affect were assessed with the Positive and Negative Affect Schedule (PANAS), which consists of 20 items of which 10 assess positive affective mood states (PA) and 10 assess negative affective mood states (NA) involving to the last week, including the day itself. The items are scored using a 5-point Likert scale anchored from “never” to “extremely”. Higher score indicate higher levels of positive/negative affective states. PANAS was used the assess the emotions in the past two weeks. The cross-sample stability, internal reliability, temporal stability, and convergent and criterion-related validities of the scale were validated in Chinese population including teenagers and young adults [40]. The average score of the questionnaire was used in this research. The internal consistency in this research was superb for positive affect (α = .93) and good for negative affect (α = .89). The average score of the questionnaire was used in this research. The internal consistency in this research was fine for positive affect (α = .91 at T1; α = .90 at T2; α = .92 at T3; α = .89 at T4) and good for negative affect (α = .89 at T1; α = .92 at T2; α = .93 at T3; α = .91 at T4).
First, we used IBM SPSS 26.0 for data management, descriptive analysis, paired-sample t-tests, and repeated ANOVA. Paired-sample t-tests were used to compare whether there was a significant difference between each time point of the experiment (T1, T2, T3, T4) and control (T1, T4) groups. Repeated ANOVA was used to analyze the tendencies of positive and negative emotions, anxiety, and depression in the experimental group. Then, we use Mplus 8.3 (Muthén & Muthén, 1998–2019) to build a growth mixture model (GMM) in the experimental group.
3.1 Comparison of Experimental Group and Control Group
Firstly, we conducted paired sample t-test to make comparison of how dependent variable change by the intervention of short-term mindfulness in every assessment. In Experiment group, anxiety depression, positive and negative emotion have significant difference at 0.01 levels, while there were no significant difference in control group.
Specifically, short-term mindfulness training increased positive emotion from T1 to T2 (t = −43.14, p < 0.01, M ± SD: −8.00 ± 2.86), from T2 to T3 (t = −48.88, p < 0.01, M ± SD: 5.90 ± 1.86), and from T3 to T4 (t = −30.39, p < 0.01, M ± SD: −7.20 ± 3.65) in experiment group, while there was no significant difference from T1 to T4 on positive emotion (t = 1.08, M ± SD: 0.18 ± 2.67) in the control group. In experiment group, negative emotion decreased from T1 to T2 (t = 25.01, p < .01, M ± SD: 6.04 ± 3.73), from T2 to T3 (t = 21.01, p < 0.01, M ± SD: 3.44 ± 2.53), and from T3 to T4 (t = 32.04, p < 0.01, M ± SD: 5.78 ± 2.78); anxiety decreased from T1 to T2 (t = 27.67, p < .01, M ± SD: 2.71 ± 1.51), from T2 to T3 (t = 22.58, p < 0.01, M ± SD: 1.76 ± 1.20), and from T3 to T4 (t = 29.73, p < 0.01, M ± SD: 3.12 ± 1.62); depression decreased from T1 to T2 (t = 25.08, p < 0.01, M ± SD: 3.27 ± 2.01), from T2 to T3 (t = 15.79, p < 0.01, M ± SD: 1.82 ± 1.78), and from T3 to T4 (t = 16.55, p < 0.01, M ± SD: 2.21 ± 2.06). However, there’s no significant difference between time point of T1 to T4 on the score of anxiety (t = −1.46, M ± SD: −0.08 ± 0.90) depression (t = −0.92, M ± SD: −0.11 ± 1.85) and negative emotion (t = −1.84, M ± SD: −0.27 ± 2.31) in control group, indicating the score of anxiety depression, positive and negative emotion did not have significant change overtime. The results illustrated in Table 2.
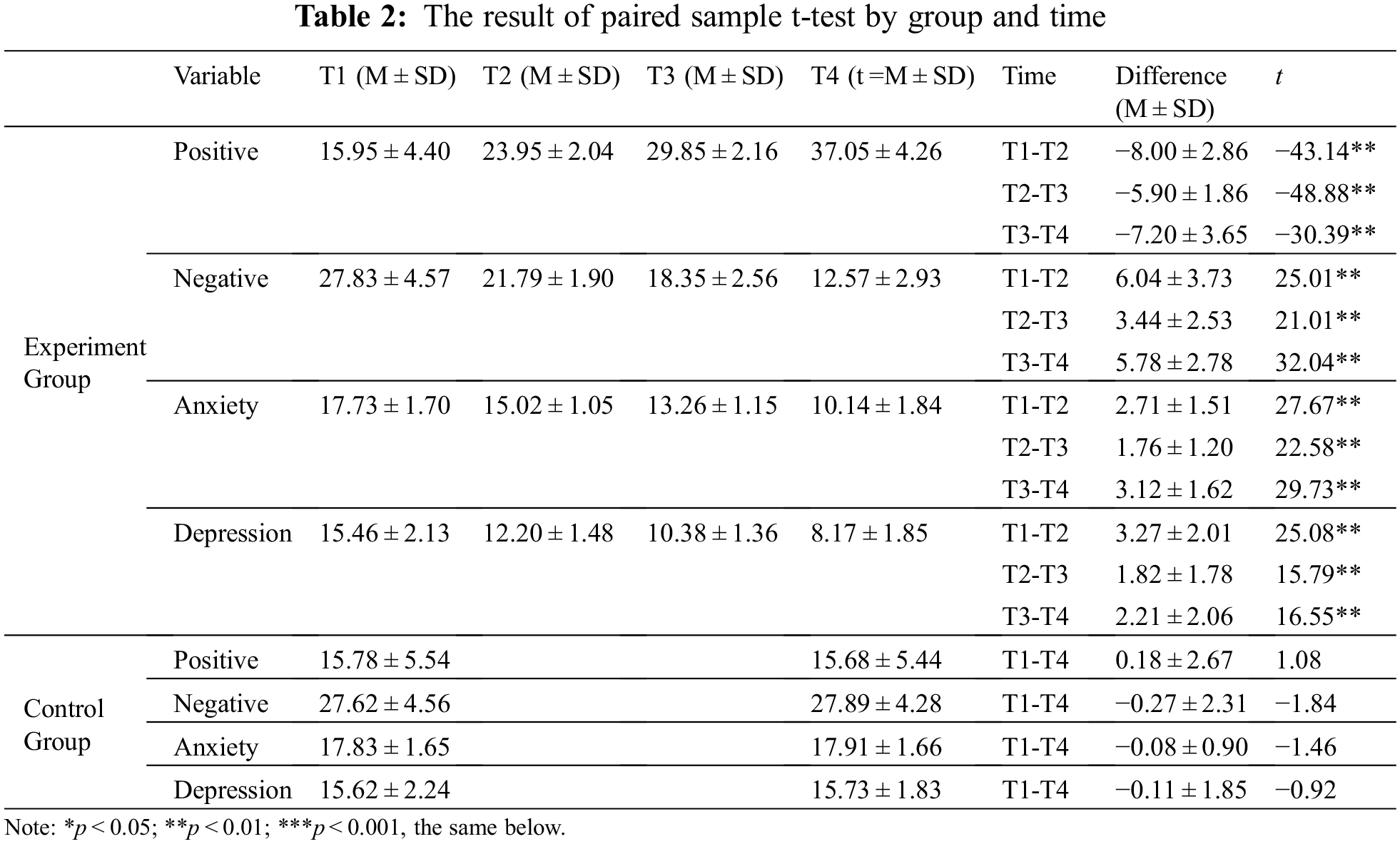
We conducted 2 (Time: T1, T4) × 2 (Group: Experiment, Control) ANOVA on the process dependent shifts. For positive emotion, the main effect of time is significant (F (1, 237) = 1364.71, p < 0.01, ɳ2p = 0.85) and there was main effect of group (F (1, 237) = 578.37, p < 0.01, ɳ2p = 0.95); there was a significant interaction between time and group (F (1, 237) = 839.77, p < 0.01, ɳ2p = 0.95). For negative emotion, the main effect of time is significant (F (1, 237) = 4725.25, p < 0.01, ɳ2p = 0.95) and there was main effect of group (F (1, 237) = 3423.18, p < 0.01, ɳ2p = 0.94); there was a significant interaction between time and group (F (1, 237) = 4422.29, p < 0.01, ɳ2p = 0.92). For anxiety, the main effect of time is significant (F (1, 237) = 3483.12, p < 0.01, ɳ2p = 0.94) and there was main effect of group (F (1, 237) = 3209.75, p < 0.01, ɳ2p = 0.93); there was a significant interaction between time and group (F (1, 237) = 3769.60, p < 0.01, ɳ2p = 0.94). For depression, the main effect of time is significant (F (1, 237) = 1620.01, p < 0.01, ɳ2p = 0.87) and there was main effect of group (F (1, 237) = 1275.13, p < 0.01, ɳ2p = 0.84); there was a significant interaction between time and group (F (1, 237) = 1791.48, p < 0.01, ɳ2p = 0.88). The result of ANOVA indicated the score of anxiety, depression and negative emotion decreased by the intervention of short-term mindfulness training, while positive emotion trended upward, as can be seen in Fig. 2. This means short-term mindfulness training has important impact on emotion under epidemic of COVID-19.
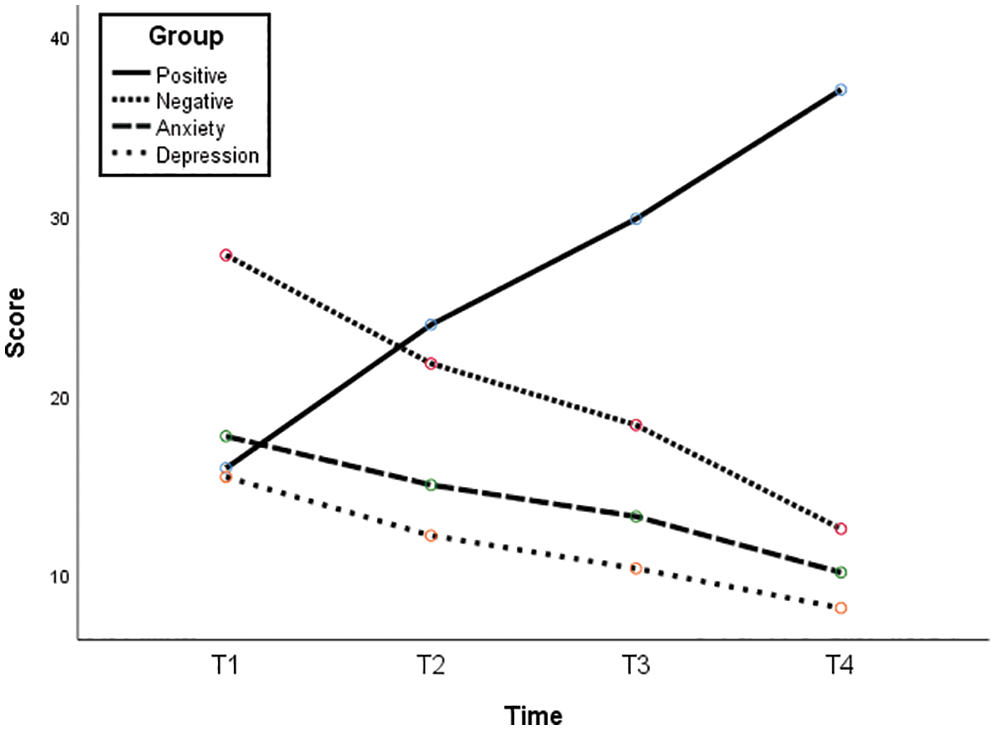
Figure 2: Growth tendency of dependent variables
3.2 Intervention Effect of the Experimental Group
For the experimental group, it is essential to choose the most appropriate analytic strategies needed to identify adolescent subgroups following qualitatively distinct joint trajectories. We conducted growth mixture modeling (GMM) of anxiety, depression, and positive and negative emotions to explore the potential categories to examine the heterogeneity of the trajectory under the intervention among adolescents [41–43].
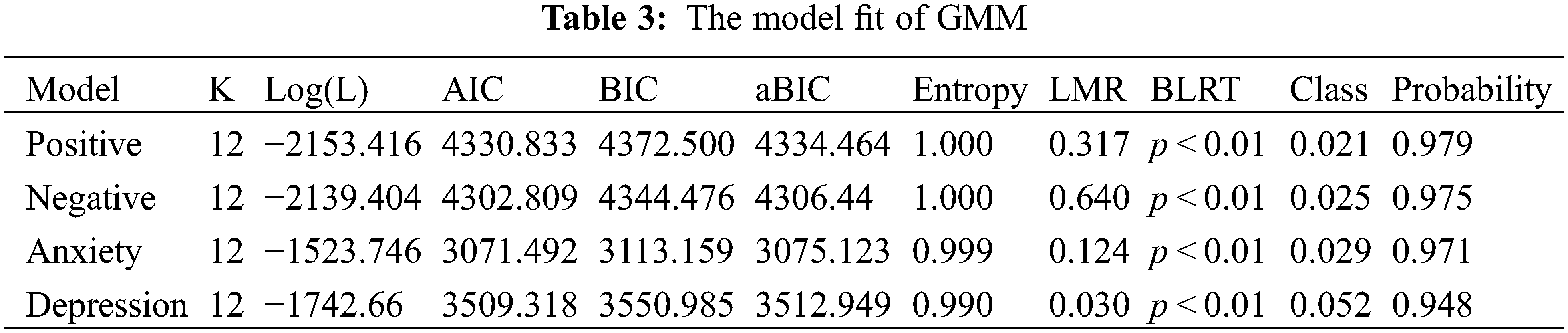
Entropy is a standardized index of model-based classification accuracy, with higher values indicating a more precise assignment of individuals to latent profiles [41]. Entropy is 0.6, indicating that approximately 20% of individuals have classification errors, while entropy is 0.8, indicating that the classification accuracy rate exceeds 90%; an entropy score closer to 1 indicates a more accurate classification [44]. In our research, the entropy scores of positive and negative emotions were 1.000; the entropy scores of anxiety and depression were 0.999 and 0.990, respectively, which demonstrated that a 2-class model was accurate in this study (Table 3).
Growth Mixture Modeling of Positive Trajectories: Two latent-class GMM trajectories of positive emotion are demonstrated in Fig. 3A. The participants in the two classes shared ascending trajectories with different increasing patterns. There were five participants in Class 1 (the red line in the figure), accounting for 2.10% of the total, with mean values of intercept and slope of 25.3321 (p < 0.01) and 1.118 (p = 0.080), respectively. There were 233 participants in the Class 2 group (the blue line in the figure), accounting for 97.90% of the total. The mean intercept and slope values were 17.564 (p < 0.01) and 6.643 (p < 0.01), respectively. The distribution is the mean value of the intercept and slope of each of the two class groups illustrated in Fig. 4A, which shows obvious differences between the two class groups.
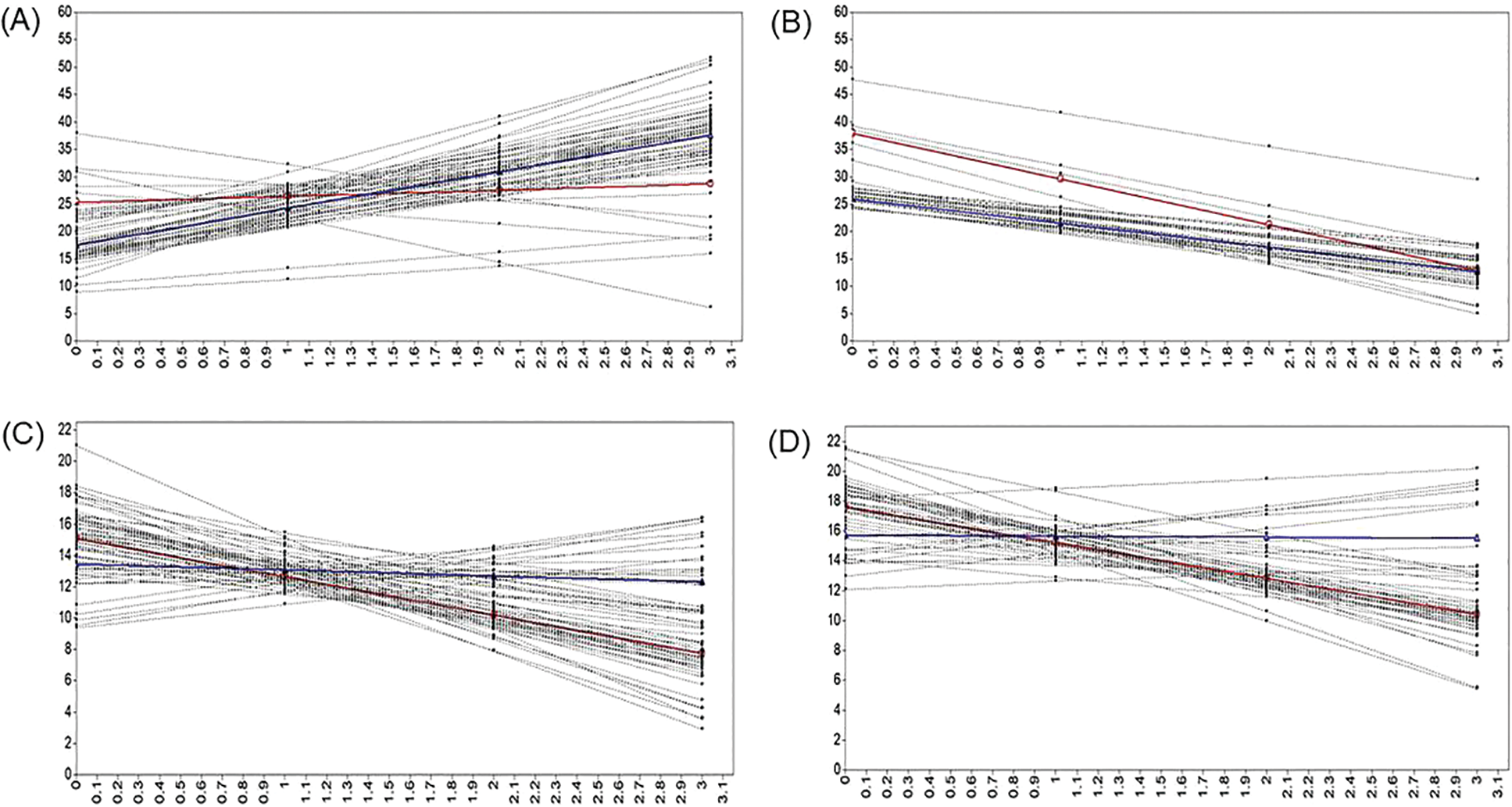
Figure 3: GMM growth trend chart of Positive (A) Negative (B) Anxiety (C) and Depression (D) Emotion
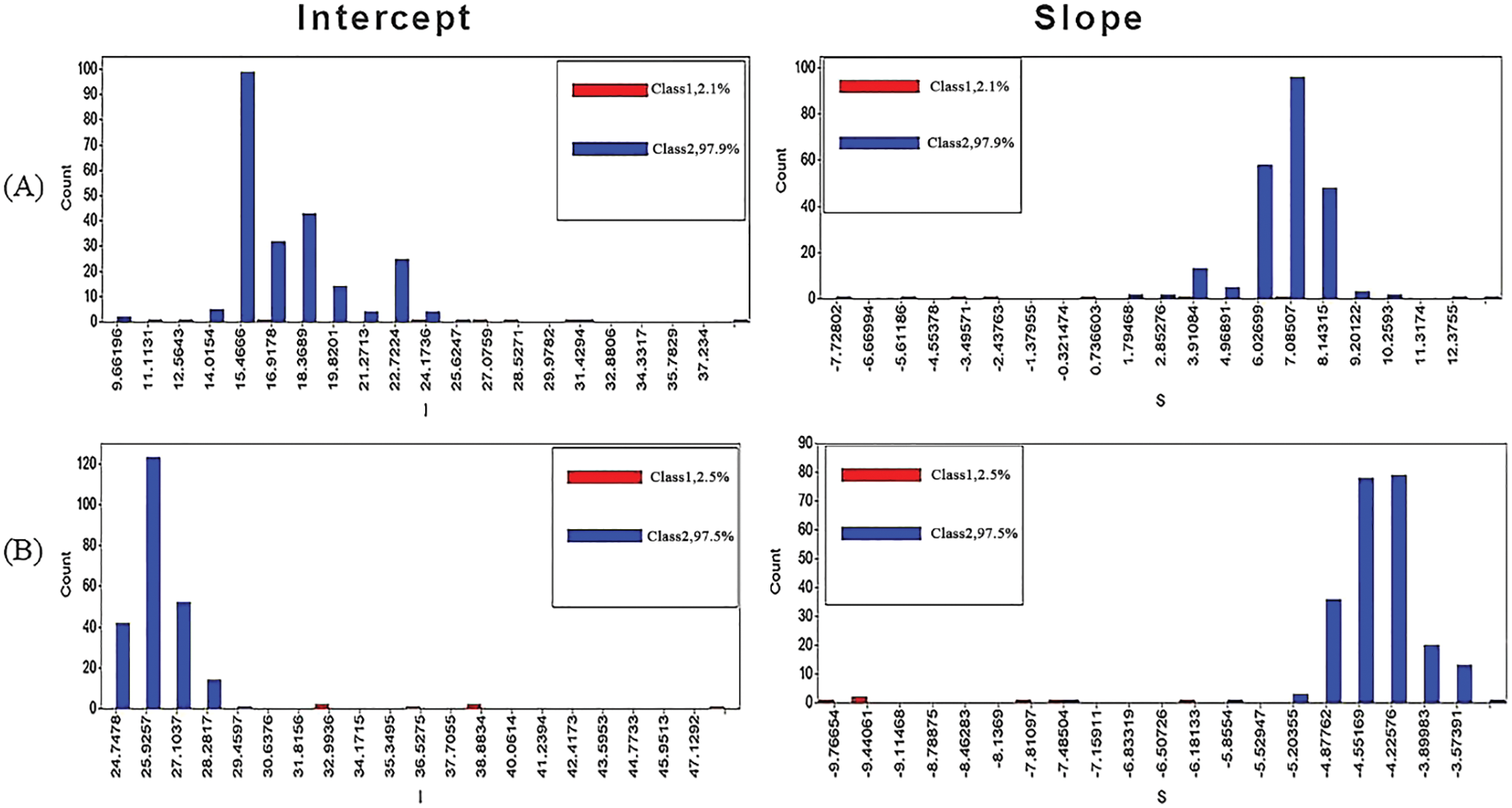
Figure 4: GMM latent variable mean distribution chart of Positive (A) & Negative (B) Emotion
Growth Mixture Modeling of Negative Trajectories: Two latent-class GMM trajectories of negative emotion are demonstrated in Fig. 3B. The participants in the two classes shared exactly the same ascending trajectory but showed different declining patterns. There were six participants in Class 1 (the red line in the figure), accounting for 2.52% of the total, with mean values of intercept and slope of 37.891 (p < 0.01) and −8.326 (p < 0.01), respectively. There were 232 participants in Class 2 (the blue line in the figure), accounting for 97.48% of the total, with mean intercept and slope values of 25.973 (p < 0.01) and −4.426 (p < 0.01), respectively. The distribution is the mean value of the intercept and slope of each of the two class groups illustrated in Fig. 4B, which showed obvious differences between the two class groups.
Growth Mixture Modeling of Anxiety Trajectories: Two latent-class GMM trajectories of anxiety are demonstrated in Fig. 3C. The participants in the two classes shared exactly the same ascending trajectory and showed different declining patterns. There were 231 participants in class 1 (the red line in the figure), accounting for 97.05% of the total, with mean intercept and slope values of 17.604 (p < 0.01) and −2.399 (p < 0.01), respectively. There were seven participants in the Class 2 group (the blue line in the figure), accounting for 2.95% of the total. The mean intercept and slope values were 15.712 (p < 0.01) and −0.069 (p = 0.809), respectively. The distribution is the mean value of the intercept and slope of each of the two class groups illustrated in Fig. 5A, which shows obvious differences between the two class groups.
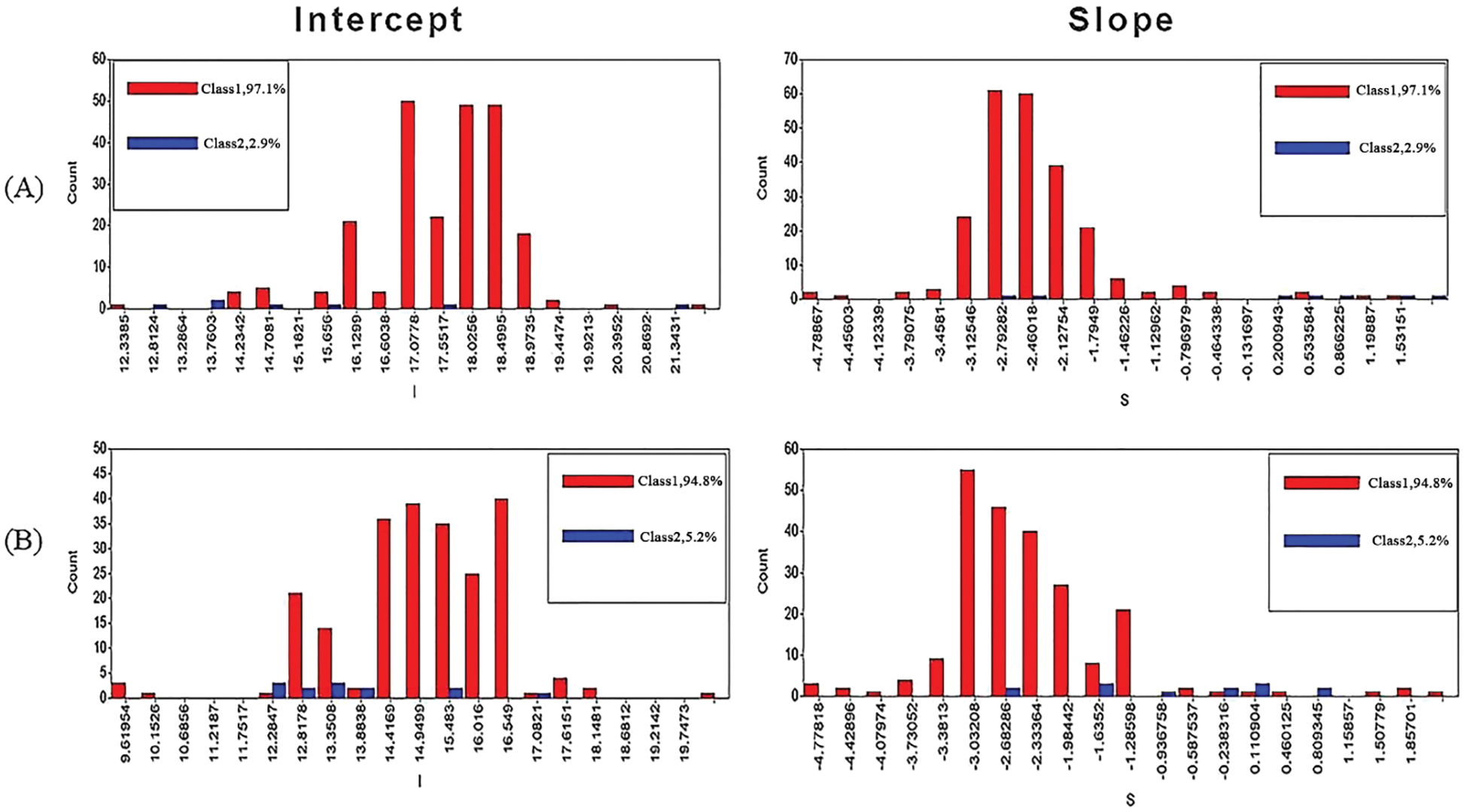
Figure 5: GMM latent variable mean distribution chart of Anxiety (A) & Depression (B)
Growth Mixture Modeling of Depression Trajectories: Two latent-class GMM trajectories of depression are demonstrated in Fig. 3D. The participants in the two classes shared exactly the same ascending trajectory and showed different declining patterns. There were 225 participants in Class 1 (red line in the figure), accounting for 94.77% of the total. The mean intercept and slope values were 15.054 (p < 0.01) and −2.439 (p < 0.01), respectively. There were 13 participants in the Class 2 group (the blue line in the figure), accounting for 5.23% of the total. The mean intercept and slope values were 13.453 (p < 0.01) and −0.294 (p = 0.200), respectively. The distribution is the mean value of the intercept and slope of each of the two class groups illustrated in Fig. 5B, which shows obvious differences between the two class groups.
The purpose of the present research was to explore whether the intervention of mindfulness training is a constructive method that can reduce negative emotions (e.g., anxiety and depression) and increasing positive emotions long-term. Thus, we first performed a randomized controlled trial to evaluate the changes in anxiety, depression, negative and positive emotions in the experimental group and control group. As expected, after mindfulness training, there was a significant decrease in negative emotions and an increase in positive emotions in the experimental group, whereas there was no significant difference in the control group. This result is in line with previous research [29,33,45] and in accordance with existing theories [29,30,32]. Additionally, this result proved that mindfulness training is beneficial for emotional regulation during the COVID-19 pandemic. Then we built two latent class GMM of the development of anxiety, depression, negative emotions and positive emotions. The entropy score of anxiety, depression, negative emotions and positive emotions all fit the two latent class GMM well. For anxiety, depression and negative emotions, the results of the models showed two downward trajectories. One trajectory of most adolescents’ negative emotion (including anxiety and depression) decreased quickly and another trajectory of other adolescents’ decreased quickly. Nonetheless, in the score of positive affect showed upward in 3 loop of intervention, the result of GMM indicated most adolescents’ (97.10%) positive emotion enhanced quickly and other adolescents’ (2.90%) positive emotion enhanced slowly.
As expected, this study indicated that after short term mindfulness training, the anxiety, depression and negative affect scores decreased, whereas there were no changes in the control group. With the continuous intervention of short term mindfulness training in the experimental group, the trajectory of anxiety, depression and negative affect was reduced, and the trajectory of positive affect was enhanced. This result is consistent with the results of several studies showing that mindfulness training is beneficial for regulating positive and negative emotions [27–29]. The following reasons may explain this phenomenon.
In addition, neurophysiological research on mindfulness and emotion has indicated that by mindfulness, the activation of an individual’s left prefrontal brain area is enhanced; pertinently, the left prefrontal brain area can provoke positive emotion [46,47]. Davidson et al. randomly divided 41 healthy participants into mindfulness intervention and control groups. In the mindfulness intervention group, participants participated in 8 weeks of mindfulness training, including 2.5 to 3 h of group training once a week and 1 h of home practice every day. Using EEG technology to test participants’ brain electrical activity before and after intervention in each group while the participants watched an emotional video and wrote down the best and the worst experience in their lives. The results indicated that the mindfulness intervention increased the activation of the left prefrontal brain area and positive emotion in the experimental group. Moreover, the increased activity of the left prefrontal brain area could predict the increase in the value of antibody concentration and promote an individual’s immune response [33]. From this, we can see that mindfulness training can improve neurobiological-related indicators to help individuals recover as soon as possible from complex environmental challenges.
The results of this study are also consistent with some brain imaging studies on depression and anxiety patients [34,35,45]. Studies of brain images have indicated that brain regions, mainly those involved with the dorsolateral prefrontal cortex and the dorsal medial prefrontal cortex, that are connected with negative emotions are changed when participants experience mindfulness [48]. Frab et al. investigated the self-referential processing mechanism while participants engaged in mindfulness to regulate negative emotions [48]. The study indicated that the brain area associated with sadness recovery and self-reference processing is located in the midline of the cerebral cortex. The mindfulness group showed significantly different neural responses, including increased repair of the viscera associated with somatosensory and somatosensory areas of the right brain area. At the same time, the enhancement of somatosensory repair in sadness-related stress was associated with a decrease in depression. Another study used fMRI to investigate the relationship between mindfulness and depression while participants watched negative facial pictures [35]. The results showed a negative relationship between mindfulness and self-referential processing of resting-state nerve activity in brain regions; this outcome was the opposite in patients with depression. Mindfulness is negatively related to resting activity of the bilateral amygdala, whereas depression is positively related to the right side of the amygdala. This means that mindfulness is associated with implicit nerve activity. Specifically, changes in the activity of the bilateral amygdala in the resting state are a potential mechanism of mindfulness intervention in the treatment of depression.
In the condition of mindfulness, the thickness of an individual’s right insula, right hippocampus and left inferior temporal gyrus cortex increased; all of these regions are related to inner and physical perception. Notably, the hippocampus regulates the activity of the amygdala, which is involved in the process of attention and emotion [49]. A subsequent study by Hölzel et al. used 8 weeks of mindfulness stress reduction therapy as a means of intervention to test the effects of perceived stress associated with structural changes in the amygdala. After 26 participants underwent the intervention, the self-reported perceived pressure was significantly reduced, and this reduction was positively correlated with the decrease in gray matter density of the right basolateral amygdala [50]. Later, in a longitudinal controlled study, Hölzel et al. chose 17 participants who took part in mindfulness training and used fMRI to check the thickness of the ectocinerea before and after mindfulness training intervention [36]. The results indicated that compared to the control group, participants’ brain structures changed in the intervention group, with increased thickness of the left hippocampal gray matter, posterior cingulate gyrus, temporal lobe-parietal junction, and cerebellar gray matter.
Currently, the magnitude and rapid spread of the COVID-19 viral disease during the pandemic has led to the proliferation of anxiety, depression, and other negative emotions in a range of different factions of society, in addition to the contagion. In this circumstance, learning to face negative emotions without repression and to enhance positive emotions is particularly vital. In view of this situation and considering the results of this study, the intervention of short-term mindfulness practice offers an efficient strategy to help reduce negative emotions.
In addition, there are a few limitations that may guide future research. All subjects in this research had undergone other positive incidents, such as transitioning from being quarantined to being free, and transitioning from taking classes online to attending school. These incidents may have also improved positive emotions and decreased negative emotions in adolescents. Further research can extend tracking time and comprehensively consider life changes, personality characteristics, and other factors.
As predicted, our results showed that short-term mindfulness is a practical intervention to increase positive emotions and decrease anxiety, depression, and negative emotions. To thoroughly check the trajectory and heterogeneity in the experimental group, we conducted GMM analyses. The GMM analyses distinguished two classes of participants that differed in the change trajectory of anxiety, depression, negative emotions, and positive emotions in the three loops of intervention.
Funding Statement: This research was funded by Regional Science Fund Project of Northwest Normal University, Grant No. 31660281.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: Yue Yuan, Aibao Zhou; data collection: Yue Yuan, Tinghao Tang; analysis and interpretation of results: Yue Yuan, Manying Kang, Tinghao Tang; draft manuscript preparation: Aibao Zhou, Yue Yuan, Tinghao Tang, Zhi Wang. All authors reviewed the results and approved the final version of the manuscript.
Conflicts of Interest: We declare that they have no conflicts of interest to report regarding the present study.
References
1. World Health Organization (2020). Rolling updates on coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-theyhappen. [Google Scholar]
2. Cao, W., Fang, Z., Hou, G., Han, M., Xu, X. et al. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research, 287, 112934. DOI 10.1016/j.psychres.2020.112934. [Google Scholar] [CrossRef]
3. Yuan, Y. (2020). Mindfulness training on the resilience of adolescents under the COVID-19 epidemic: A latent growth curve analysis. Personality and Individual Differences, 172, 1–9. DOI 10.1016/j.paid.2020.110560. [Google Scholar] [CrossRef]
4. Rogers, J. P., Chesney, E., Oliver, D., Pollak, T. A., McGuire, P. et al. (2020). Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. The Lancet, 7(7), 611–627. DOI 10.1016/S2215-0366(20)30203-0. [Google Scholar] [CrossRef]
5. Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L. et al. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. DOI 10.3390/ijerph17051729. [Google Scholar] [CrossRef]
6. Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B. et al. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 33(2), e100213. DOI 10.1136/gpsych-2020-100213. [Google Scholar] [CrossRef]
7. Liu, C. H., Zhang, E., Wong, G., Hyun, S., Hahm, H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research, 290, 113172. DOI 10.1016/j.psychres.2020.113172. [Google Scholar] [CrossRef]
8. McGinty, E. E., Presskreischer, R., Han, H., Barry, C. L. (2020). Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA, 324(1), 93–94. DOI 10.1001/jama.2020.9740. [Google Scholar] [CrossRef]
9. Tang, W., Hu, T., Hu, B., Jin, C., Wang, G. et al. (2020). Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. Journal of Affective Disorders, 274, 1–7. DOI 10.1016/j.jad.2020.05.009. [Google Scholar] [CrossRef]
10. Li, Y., Zhao, J., Ma, Z., McReynolds, L. S., Lin, D. et al. (2020). Mental health among college students during the COVID-19 pandemic in China: A 2-wave longitudinal survey. Journal of Affective Disorders, 281(1), 597–604. DOI 10.1016/j.jad.2020.11.109. [Google Scholar] [CrossRef]
11. Huang, Y., Wang, Y., Wang, H., Liu, Z., Yu, X. et al. (2019). Prevalence of mental disorders in China: A cross-sectional epidemiological study. The Lancet, 6(3), 211–224. DOI 10.1016/S2215-0366(18)30511-X. [Google Scholar] [CrossRef]
12. Grupe, D. W., Nitschke, J. B. (2013). Uncertainty and anticipation in anxiety: An integrated neurobiological and psychological perspective. Nature Reviews Neuroscience, 14(7), 488–501. DOI 10.1038/nrn3524. [Google Scholar] [CrossRef]
13. Dugas, M. J., Hedayati, M., Karavidas, A., Buhr, K., Francis, K. et al. (2005). Intolerance of uncertainty and information processing: Evidence of biased recall and interpretations. Cognitive Therapy and Research, 29(1), 57–70. DOI 10.1007/s10608-005-1648-9. [Google Scholar] [CrossRef]
14. Allen, M. T., Myers, C. E., Servatius, R. J. (2016). Uncertainty of trial timing enhances acquisition of conditioned eyeblinks in anxiety vulnerable individuals. Behavioural Brain Research, 304, 86–91. DOI 10.1016/j.bbr.2016.02.007. [Google Scholar] [CrossRef]
15. Chin, B., Nelson, B. D., Jackson, F., Hajcak, G. (2016). Intolerance of uncertainty and startle potentiation in relation to different threat reinforcement rates. International Journal of Psychophysiology, 99, 79–84. DOI 10.1016/j.ijpsycho.2015.11.006. [Google Scholar] [CrossRef]
16. Beck, A. T. (2008). The evolution of the cognitive model of depression and its neurobiological correlates. American Journal of Psychiatry, 165(8), 969–977. DOI 10.1176/appi.ajp.2008.08050721. [Google Scholar] [CrossRef]
17. Disner, S. G., Beevers, C. G., Haigh, E. A. P., Beck, A. T. (2011). Neural mechanisms of the cognitive model of depression. Nature Reviews Neuroscience, 12, 467–477. DOI 10.1038/nrn3027. [Google Scholar] [CrossRef]
18. Pizzagalli, D. A., Iosifescu, D., Hallett, L. A., Ratner, K. G., Fava, M. (2008). Reduced hedonic capacity in major depressive disorder: Evidence from a probabilistic reward task. Journal of Psychiatric Research, 43(1), 76–87. DOI 10.1016/j.jpsychires.2008.03.001. [Google Scholar] [CrossRef]
19. Pizzagalli, D. A., Jahn, A. L., O’Shea, J. P. (2005). Toward an objective characterization of an anhedonic phenotype: A signal-detection approach. Biological Psychiatry, 57(4), 319–327. DOI 10.1016/J.BIOPSYCH.2004.11.026. [Google Scholar] [CrossRef]
20. Pechtel, P., Dutra, S. J., Goetz, E. L., Pizzagalli, D. A. (2013). Blunted reward responsiveness in remitted depression. Journal of Psychiatric Research, 47(12), 1864–1869. DOI 10.1016/J.JPSYCHIRES.2013.08.011. [Google Scholar] [CrossRef]
21. Garland, E. L., Hanley, A. W., Goldin, P. R., Gross, J. J. (2017). Testing the mindfulness-to-meaning theory: Evidence for mindful positive emotion regulation from a reanalysis of longitudinal data. PLoS One, 12(12), e0187727. DOI 10.1371/journal.pone.0187727. [Google Scholar] [CrossRef]
22. Khoury, B. (2018). Mindfulness: Embodied and embedded. Mindfulness, 9(4), 1037–1042. DOI 10.1007/s12671-017-0858-z. [Google Scholar] [CrossRef]
23. Kabatzinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. Behaviour Research and Therapy, 33(8), 996. DOI 10.1016/0005-7967(95)90133-7. [Google Scholar] [CrossRef]
24. Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D. et al. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11, 230–241. DOI 10.1093/clipsy.bph077. [Google Scholar] [CrossRef]
25. Chambers, R., Gullone, E., Allen, N. B. (2009). Mindful emotion regulation: An integrative review. Clinical Psychology Review, 29(6), 560–572. DOI 10.1016/j.cpr.2009.06.005. [Google Scholar] [CrossRef]
26. Jimenez, S. S., Niles, B. L., Park, C. L. (2010). A mindfulness model of affect regulation and depressive symptoms: Positive emotions, mood regulation expectancies, and self-acceptance as regulatory mechanisms. Personality and Individual Differences, 49(6), 645–650. DOI 10.1016/j.paid.2010.05.041. [Google Scholar] [CrossRef]
27. Hargus, E., Crane, C., Barnhofer, T., Williams, J. M. G. (2010). Effects of mindfulness on meta-awareness and specificity of describing prodromal symptoms in suicidal depression. Emotion, 10(1), 34–42. DOI 10.1037/a0016825. [Google Scholar] [CrossRef]
28. Michalak, J., Hölz, A., Teismann, T. (2011). Rumination as a predictor of relapse in mindfulness-based cognitive therapy for depression. Psychology and Psychotherapy: Theory, Research and Practice, 84(2), 230–236. DOI 10.1348/147608310X520166. [Google Scholar] [CrossRef]
29. Shahar, B., Britton, W. B., Sbarra, D. A., Figueredo, A. J., Bootzin, R. R. (2010). Mechanisms of change in mindfulness-based cognitive therapy for depression: Preliminary evidence from a randomized controlled trial. International Journal of Cognitive Therapy, 3(4), 402–418. DOI 10.1521/ijct.2010.3.4.402. [Google Scholar] [CrossRef]
30. Garland, E. L., Farb, N. A., Goldin, P. R., Fredrickson, B. L. (2015). The mindfulness-to-meaning theory: Extensions, applications, and challenges at the attention–appraisal–emotion interface. Psychological Inquiry, 26(4), 377–387. DOI 10.1080/1047840X.2015.1092493. [Google Scholar] [CrossRef]
31. Geschwind, N., Peeters, F., Drukker, M., van Os, J., Wichers, M. (2011). Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 79(5), 618–628. DOI 10.1037/a0024595. [Google Scholar] [CrossRef]
32. Segal, Z. V., Williams, J. M. G., Teasdale, J. D. (2013). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford Press. [Google Scholar]
33. Davidson, R. J., Kabat-Zinn, J., Schumacher, J., Rosenkranz, M., Muller, D. et al. (2003). Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine, 65, 564–570. DOI 10.1097/01.PSY.0000077505.67574.E3. [Google Scholar] [CrossRef]
34. Modinos, G., Ormel, J., Aleman, A. (2010). Individual differences in dispositional mindfulness and brain activity involved in reappraisal of emotion. Social Cognitive and Affective Neuroscience, 5(4), 369–377. DOI 10.1093/scan/nsq006. [Google Scholar] [CrossRef]
35. Way, B. M., Creswell, J. D., Eisenberger, N. I., Lieberman, M. D. (2010). Dispositional mindfulness and depressive symptomatology correlations with limbic and self-referential neural activity during rest. Emotion, 10(1), 12–24. DOI 10.1037/a0018312. [Google Scholar] [CrossRef]
36. Hölzel, B. K., Carmody, J., Vangel, M., Congleton, C., Yerramsetti, S. M. et al. (2011). Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research: Neuroimaging, 191(1), 36–43. DOI 10.1016/j.pscychresns.2010.08.006. [Google Scholar] [CrossRef]
37. Mak, W. W., Tong, A. C., Yip, S. Y., Lui, W. W., Chio, F. H. et al. (2018). Efficacy and moderation of mobile app-based programs for mindfulness-based training, self-compassion training, and cognitive behavioral psychoeducation on mental health: Randomized controlled noninferiority trial. JMIR Mental Health, 5(4), e60. DOI 10.2196/mental.8597. [Google Scholar] [CrossRef]
38. Leung, C. M., Ho, S., Kan, C. S., Hung, C. H., Chen, C. N. (1993). Evaluation of the Chinese version of the hospital anxiety and depression scale: A cross-cultural perspective. International Journal of Psychosomatics, 40(1), 29–34 [Google Scholar]
39. Spinhoven, P., Ormel, J., Sloekers, P. P. A., Kempen, G. I. J. M., Speckens, A. E. M. et al. (1997). A validation study of the hospital anxiety and depression scale (HADS) in different groups of Dutch participants. Psychological Medicine, 27(2), 363–370. DOI 10.1017/S0033291796004382. [Google Scholar] [CrossRef]
40. Weidong, Z., Jing, D., Schick, C. J. (2004). The cross-cultural measurement of positive and negative affect examining the dimensionality of PANAS. Psychological Science (China), 27(1), 77–79. [Google Scholar]
41. Wang, M. C., Deng, Q., Bi, X., Ye, H., Yang, W. (2017). Performance of the entropy as an index of classification accuracy in latent profile analysis: A monte carlo simulation study. Acta Psychologica Sinica, 49(11), 1473–1482. DOI 10.3724/SP.J.1041.2017.01473. [Google Scholar] [CrossRef]
42. Kim, S. Y. (2012). Sample size requirements in single-and multiphase growth mixture models: A monte carlo simulation study. Structural Equation Modeling, 19, 457–476. DOI 10.1080/10705511.2012.687672. [Google Scholar] [CrossRef]
43. Wang, M. C., Bi, X., Ye, H. (2014). Growth hybrid model-analysis of the development trend of different types of individuals. Sociological Research, 4, 220–241. [Google Scholar]
44. Li, Z. X. W., Yin, X., Liu, W., Zhou, X. (2018). Developmental trajectory of depressive symptoms in college students: A latent growth mixture model. Chinese Journal of Clinical Psychology, 26(4), 711–715. DOI 10.16128/j.cnki.1005-3611.2018.04.018. [Google Scholar] [CrossRef]
45. Goldin, P., Gross, J. (2010). Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion, 10(1), 83–91. DOI 10.1037/a0018441. [Google Scholar] [CrossRef]
46. Barnhofer, T., Duggan, D., Crane, C., Hepburn, S., Fennell, M. J. V. (2007). Effects of meditation on frontal alpha-asymmetry in previously suicidal individuals. Neuroreport, 18(7), 709–812. DOI 10.1097/WNR.0b013e3280d943cd. [Google Scholar] [CrossRef]
47. Chan, A. S., Han, Y. M. Y., Cheung, M. C. (2008). Electroencephalographic (EEG) measurements of mindfulness-based triarchic body-pathway relaxation technique: A pilot study. Applied Psychophysiology and Biofeedback, 33(1), 39–47. DOI 10.1007/s10484-008-9050-5. [Google Scholar] [CrossRef]
48. Farb, N. A. S., Anderson, A. K., Mayberg, H., Bean, J., McKeon, D. (2010). Minding one’s emotions: Mindfulness training alters the neural expression of sadness. Emotion, 10(1), 25–33. DOI 10.1037/a0017151. [Google Scholar] [CrossRef]
49. Hölzel, B. K., Ott, U., Gard, T., Hempel, H., Weygandt, M. (2008). Investigation of mindfulness meditation practitioners with voxel-based morphometry. Social Cognitive & Affective Neuroscience, 3(1), 55–61. DOI 10.1093/scan/nsm038. [Google Scholar] [CrossRef]
50. Hölzel, B. K., Carmody, J., Evans, K. C., Hoge, E. A., Dusek, J. A. et al. (2010). Stress reduction correlates with structural changes in the amygdala. Social Cognitive and Affective Neuroscience, 5(1), 11–17. DOI 10.1093/scan/nsp034. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools