 Open Access
Open Access
ARTICLE
The COVID-19 Pandemic: A Double Threat to Chinese Americans’ Mental Health
1
School of Nursing, Dali University, Dali, 671000, China
2
Department of Nursing, Chuxiong Higher Institute of Medicine, Chuxiong, 675005, China
3
Department of Nursing, Kunming Third People’s Hospital, Kunming, 650041, China
4
Department of Quality Management, Dali People’s Hospital, Dali, 671000, China
5
Department of Nursing, College of Natural Science, California State University, San Bernardino, CA 92407, USA
* Corresponding Authors: Qilian He. Email: ;
# The first two authors (Aoli Li and Yan You) contributed equally to this paper and should be considered co-first authors
International Journal of Mental Health Promotion 2023, 25(6), 783-797. https://doi.org/10.32604/ijmhp.2023.026956
Received 06 October 2022; Accepted 16 January 2023; Issue published 06 May 2023
Abstract
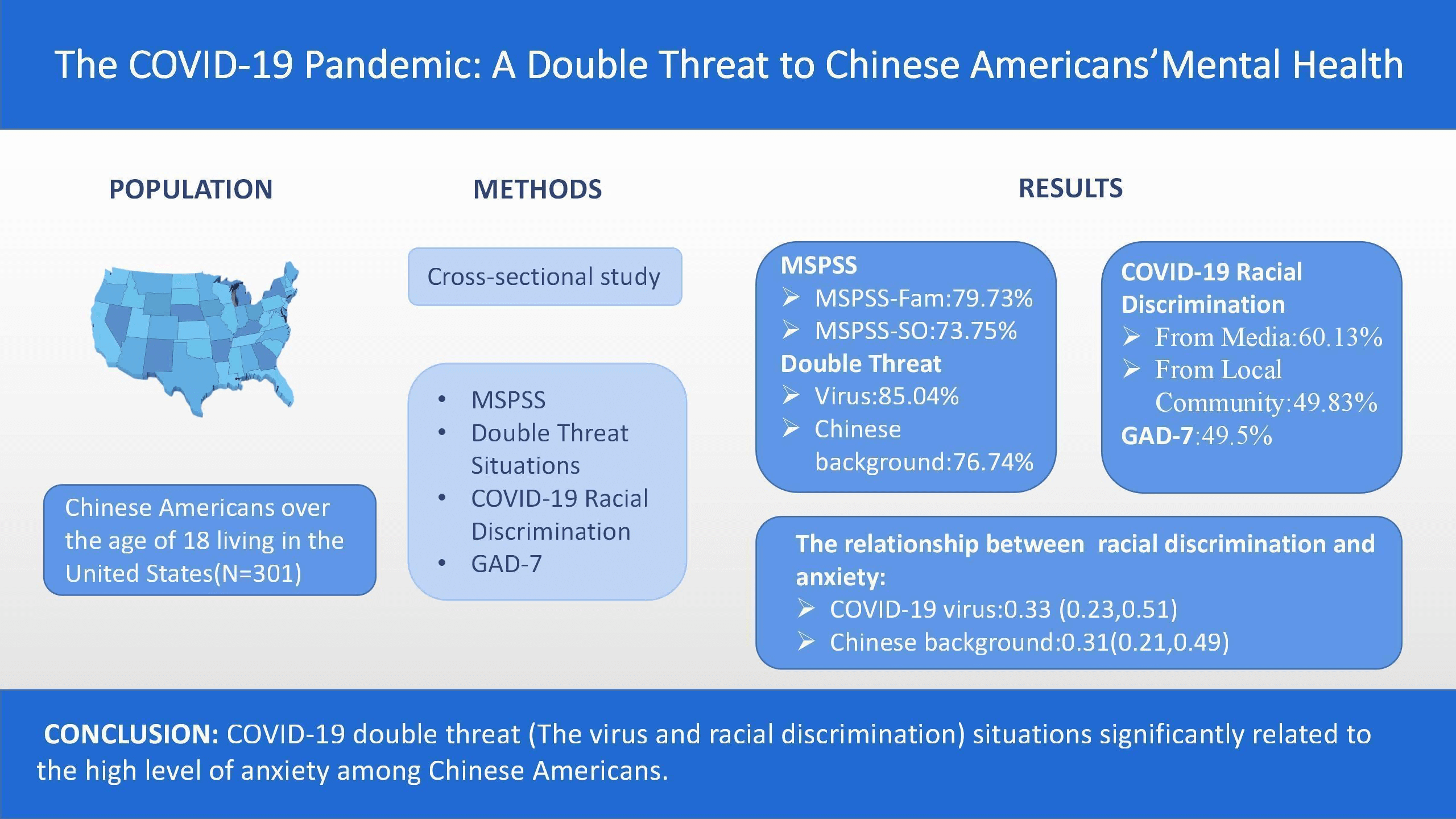
Objective: To explore the double psychosocial threats of the COVID-19 pandemic, targeted behavior toward Chinese Americans, and the correlates to their mental health. Methods: A quantitative, cross-sectional, and descriptive design was utilized by using a purposive convenience sample of 301 Chinese Americans over the age of 18 residing in the United States. Online data collection was conducted through the social media platform WeChat from April 8–21, 2021. Descriptive statistical analysis was used for the participants’ demographic characteristics, Multidimensional Scale of Perceived Social Support (MSPSS), Double Threat Situations, COVID-19 Racial Discrimination, and General Anxiety Disorder-7 (GAD-7). Stepwise logistic regression was conducted to verify predictors for anxiety levels by GAD-7. Results: In this sample (N = 301), 127 (42.19%) were male and 174 (57.81%) were female. The average age was 41.67 (SD = 5.89). Among MSPSS subscales, social support from family (MSPSS-Fam, 79.73%, n = 240) and social support from significant others (MSPSS-SO, 73.75%, n = 222) were high. 231 (76.74%) reported threats due to their Chinese ethnic background during the COVID-19 outbreak. Predictors for the high anxiety level by GAD-7 were COVID-19 racial discrimination from the local community (OR = 0.47, 95% CI = 0.39–0.71, p < 0.001), media/online (OR = 0.36, 95% CI = 0.26–0.53, p < 0.001), the perceived threat from the COVID-19 virus (OR = 0.33, 95% CI = 0.23–0.51, p < 0.001) and Perceived racism threat from Chinese background related to COVID-19 (OR = 0.31, 95% CI = 0.21–0.49, p < 0.001). Conclusions: COVID-19 double-threats (The virus and racial discrimination) situations are significantly related to the high level of anxiety among Chinese Americans. The sense of belonging and social perceptions of Chinese immigrants is closely related to public health problems in Western societies and needs to be addressed at all levels. Our findings call for the attention of healthcare workers to specific racism double-threatened situations and high mental health risks, as well as direct and indirect ethnic discrimination that Chinese Americans are experiencing during this pandemic, the long-term influences and effective coping ways related to this issue should be explored in further research.Graphic Abstract
Keywords
As of September 18, 2022, the World Health Organization (WHO) reported 609 million confirmed global cases of COVID-19, including 6.5 million deaths in 216 countries [1]. The COVID-19 pandemic has upended individual victim lives and continues to influence the world’s economy and challenge global healthcare workers to meet the health promotion needs of populations everywhere [2,3]. To control the spread of the virus, individual governments in many countries declared a national state of public health emergency. Although necessary, these unexpected changes created problems for government programs as well as the populations they served [4,5].
During the Chinese Spring Festival vacation period at the end of January 2020, China reported the Coronavirus outbreak and the quick spread of infections. Despite the multiple crowds that gathered during that time, the territory of China was able to contain the outbreak within a few months. This required citizens to wear masks, preparing hospitals to receive people with the most severe cases of COVID-19 and health professionals to provide critical care for those hospitalized with severe disease. Starting from mid-April 2020, the epidemic in China appeared to be under control, with significant decreases in the number of confirmed cases [6].
The WHO [6] also published numbers of COVID-19 cases and related deaths from other countries. On January 03, 2020, the United States (U.S.) started reporting confirmed COVID-19 cases, and the number of cases began to escalate beginning in March 2020. Since then, the virus has begun to spread around the world. Authorities in many countries have since ordered people to recognize the pandemic and take the necessary precautions to prevent being infected through face masks, hand washing, social distancing, and quarantining.
Several recent investigations have explored the psychological influences of the COVID-19 outbreak on health professionals caring for those who were ill and the public as well. Surveys of healthcare worker populations found negative effects of the COVID-19 outbreak [7–9]. Studies have reported a high level of physical and psychological pressure experienced by Chinese healthcare professionals as they responded to this huge public health emergency [10–15].
Several reports have identified depression issues related to COVID-19 experienced by all age groups and populations in other countries as well [16–19]. Liu et al. [20] found that 43.3% of United States young adult (18–30 years) respondents reported high clinical levels of anxiety, depression, and post-traumatic stress disorder (PTSD) symptoms related to the COVID-19 pandemic. College students experienced COVID-19-related fear and anxiety [21–23]. Adolescents and children also have reported anxiety and emotional disorders caused by pandemic-related quarantine [24].
When the United States became the epicenter of the COVID-19 pandemic, the level of fear and anxiety about individual safety increased in many states. No national COVID-19 prevention plan was instituted, so the closure of businesses and schools, and “stay-at-home” orders were inconsistent. With minimal knowledge about the virus and how it spread to the United States, some groups began to search for a target to blame. From March to December 2020, [25] identified over 2000 reports of ethnic discrimination against Asian Americans. Shoichet [26] was the first investigator to identify the double threat faced by Chinese Americans; they are not only faced with the threat of the COVID-19 virus but also the ethnic discrimination specifically targeting them. Surveys of Chinese students studying abroad found they suffered from a high level of anxiety caused by racial discrimination and conflicting messages they received related to the COVID-19 outbreak [27,28].
These accusations filtered to Chinese American residents of the United States, with little regard for their positive contributions to stem the tide of the pandemic. U.S. Chinese Americans had donated money and medical materials to China and the United States and volunteered in many settings for COVID-19 testing and personal protective equipment (PPE) such as face masks, protective suits, and goggles [29–31].
Within the last 10 years, Chinese Americans have become the largest group of Asian American immigrants, surpassing the number of Hispanic immigrants [32,33]. Despite the number of reports of targeted Chinese Americans’ blame for the pandemic and the psychological effects of the pandemic on other population groups, no evidence has been collected from Chinese Americans to link the racially biased attacks with the psychological effects on this population group. Therefore, our study aimed to explore the double psychosocial threats of the COVID-19 pandemic and targeted behavior toward Chinese Americans and the correlation to their mental health.
A quantitative descriptive approach was used in this study. The focus of this study was to explore the double psychosocial threats of the COVID-19 pandemic and targeted behavior toward Chinese Americans and the correlation to their mental health.
The target population for our study was Chinese Americans over the age of 18 residing in the United States. Based on a power analysis by G* Power 3.1.9.7, with an alpha of 0.05, power of 0.80, and odds ratio of 1.5, the required sample size was at least 242 participants. The convenience sample was recruited through the social media platform WeChat. According to [34], Chinese Americans frequently used the WeChat application for messaging, payments, and mini programs. Previous research revealed WeChat to be a significant and useful tool for education and research studies during global disease outbreaks such as COVID-19 [35].
The study invitation was posted on the WeChat platform through chat groups in different regions in the United States. Persons who identified as Chinese Americans were invited to view the study on the linked study website. The website included study descriptions and exclusion criteria for persons who had already been diagnosed with depression, thyroid dysfunction, sleep apnea, and substance dependence. All questionnaires were available in English or Chinese.
After reading the study description and the exclusion criteria, persons who met the inclusion criteria and denied having the exclusion criteria were eligible to participate. Qualified respondents were then directed to complete the online survey instruments. Participants who completed all questionnaires on the WeChat app each received a red-envelope of RMB 20 (E-gift card) as a reward.
The Institutional Review Board of the University where the investigators were employed approved all research methods. The study was conducted from April 8–21, 2021. The survey included participant demographic characteristics, the Multidimensional Scale of Perceived Social Support (MSPSS), questions about Chinese American respondents’ perceived double threat and COVID-19 racial discrimination suffered during the outbreak, and the Generalized Anxiety Disorder Scale (GAD-7).
Participant Demographic Characteristics
The demographic survey items included participants’ gender, age, nativity, years in the United States, education, occupation, marital status, and current residence locations.
Multidimensional Scale of Perceived Social Support Scale (MSPSS)
Zimet et al. [36] developed a self-administered 12-item measure of perceived adequacy of social support in three areas: family (Fam), friends (Fri), and significant others (SO). Each MSPSS item had a 7-point Likert scale response, ranging from ‘very strongly disagree’ (1) to ‘very strongly agree’ (7). When summed, the total MSPSS score ranged from 12 to 84. Based on scoring on a similar study of U.S. young adults [20], a mean score of 5 or above on each subscale was regarded as strong support, while scores below 5 were referred to as low support.
The MSPSS has been translated and used to assess support in a variety of environments and populations [37]. There are two Chinese versions of the MSPSS such as a traditional Chinese version of MSPSS (MSPSS-C) and a simplified Chinese language (MSPSS-SCV). The MSPSS-C was first established by Chou [38] with a sample of Chinese adolescents in Hong Kong. Later Guan et al. [39] translated the MSPSS-C into the MSPSS-SCV and validated it with a sample of Malaysian university students. This study used both the MSPSS (English version) and the MSPSS-C (Traditional Chinese version).
Both the MSPSS-C and MSPSS-SCV have good reliability and validity [38,39]. The Cronbach’s alpha coefficients of the MSPSS for recent studies ranged from 0.72 to 0.94 [40,41]. In particular, Cronbach’s alpha coefficients of the MSPSS-C of family support, friend support, and significant other support subscales among a previous Chinese sample were 0.88, 0.89, and 0.87 [42]. In our study, Cronbach’s alpha coefficients of the family support, friend support, and significant other support subscales were 0.85, 0.88, and 0.84, respectively.
Double Threat Situations
Since the outbreak of the novel coronavirus (COVID-19) pandemic, Chinese Americans have experience threats associated with COVID-19 and live in fear of contracting COVID-19 [43]. Tavernise et al. [44] described the double threat from COVID-19 among Chinese Americans: “Not only are they grappling like everyone else with how to avoid the virus itself, but they are also contending with growing racism in the form of verbal and physical attacks”. Therefore, to validate this statement, this survey included two questions to explore Chinese Americans perceived double threat during the COVID-19 outbreak with 5-point Likert-Type response scales: 1) Are you afraid of the threat of COVID-19? and 2) Are you afraid of the ethnic discrimination threat caused by your Chinese background related to the COVID-19 outbreak? This two-item scale has good reliability, with a Spearman-Brown coefficient of 0.72 [45].
The response scale for these two questions ranged from ‘not afraid at all’ (1) ‘to strongly afraid’ (5). A response of 3 and above to either question indicated the respondent was afraid, so the mean score of 3 was used to differentiate low from high levels of a perceived double threat. To expand on the response to the second question, the study participants were asked to select specific situations where they were afraid during the COVID-19 outbreak. The examples were taken from situations described in the New York Times News and the CNN News [44]: a) when grocery shopping; b) when using public transportation such as buses or subway; c) when their children go outside by themselves, and d) others [please describe]. The participants were able to select any one or more of the three specific situations or add other situations where they felt afraid.
COVID-19 Ethnic Discrimination
As ethnic discrimination related to the COVID-19 outbreak is the key threat that Chinese Americans specifically experienced during the epidemic, so the racism discrimination Chinese Americans perceived caused by their ethnic group was furtherly measured. This survey included an adapted Asian American Racism-Related Stress Inventory (AARRSI) and one open-end question. The 13 items of AARRSI (α = 0.87) were adapted to focus on COVID-19 [46]. The media/online discrimination was explored with items like (a) Some media outlets had presented negative reports, using the term ‘the Chinese’ to blame the COVID-19 outbreak in China; (b) People online cracked jokes about Chinese ethnic (like food) cause of the COVID-19 outbreak; (c) People said rude words to me online related to COVID-19 because of my Chinese ethnic. The in-person discrimination from the community after the COVID-19 outbreak was identified with the adjusted items as (1) Someone was unfriendly or rude to me as of my Chinese ethnicity after the outbreak; (2) I have witnessed people saying mean things about the Chinese related to the COVID-19 outbreak; (3) People have threatened me with violence because of my Chinese ethnicity after the COVID-19 outbreak. The response 5-point Likert-type rating for each item ranged from ‘totally disagree’ (4) to ‘totally agree’ (5). A score below 3 is a low level of perceived ethnic discrimination related to the COVID-19 outbreak.
An open-end question was aimed to furtherly explore specific personal experiences after the above scales. With the question “would you please share your personal experience of ethnic discrimination or attacks due to your Chinese background during the COVID-19 outbreak?”, the study participants described their personal experience of ethnic discrimination during the COVID-19 outbreak.
Generalized Anxiety Disorder Scale (GAD-7)
In 2006, Spitzer et al. [47] developed the Generalized Anxiety Disorder Scale-7 (GAD-7) to access perceived anxiety levels in the previous two weeks. The GAD-7 consists of seven items, each with a 4-point Likert-type response scale (0-not at all to 3-nearly every day). The possible total score on the GAD-7 ranges from 0 to 21 points; the higher the score, the more serious the anxiety, total scores of 0–9 were recoded as lower anxiety, and scores of 10 or higher were recorded as increased anxiety. Spritzer and colleagues [47] reported a Cronbach’s internal consistency reliability score of 0.92 and 0.89 in this study.
The investigators analyzed the data through the IBM Statistical Package for Social Sciences (SPSS) version 27. Descriptive statistical analysis revealed details about the study participants’ demographic characteristics, perceived social support status, double threat situations, COVID-19 racial discrimination, and GAD-7 anxiety level. To explore the significant predictors for high anxiety level GAD-7 scores for Chinese Americans during the COVID-19 pandemic, stepwise logistic regression was conducted. Five predictors of anxiety were introduced into the regression model in stepwise order: three types of social support from family (MSPSS-FAM), friends (MSPSS-FRI), and significant others (MSPSS-SO), and perceived double threat and COVID-19 ethnic discrimination. The level of statistical significance was established a priori at p < 0.05.
3.1 Demographic Characteristics of Participants
Initially, 306 participants met all the study criteria and started the survey. Five respondents’ surveys were discarded due to failure to complete the survey, leaving the final sample size at 301. Study participant characteristics are described in Table 1. Among them, 57.81% were female; 96.01% were foreign-born; 86.38% had undergraduate and higher education degrees; 94.68% were married; 93.02% had well-employed; the average age was 41.67 (SD = 5.89). The participants had lived in the United States for more than 13 years and resided in the Western, Northeast, Southern, and Midwest regions of the United States.
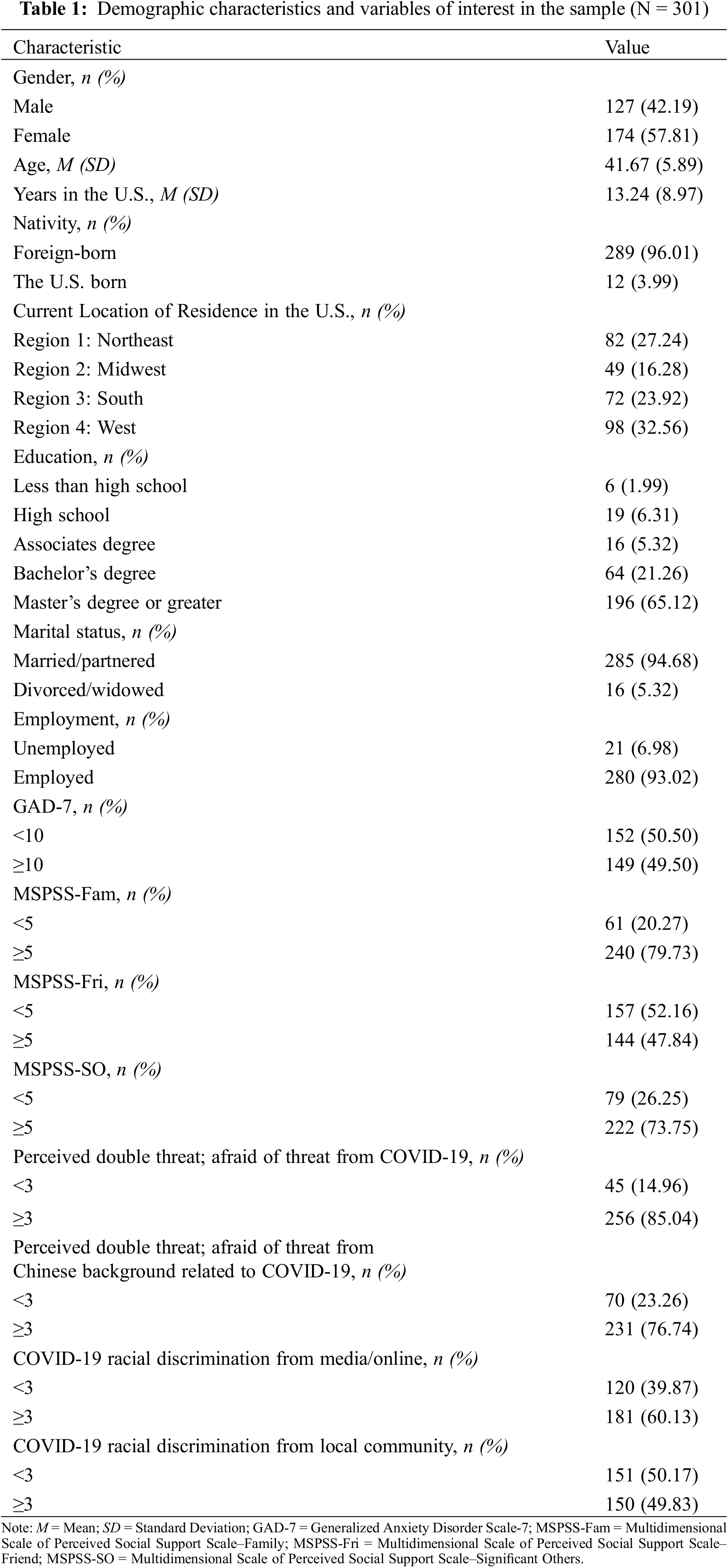
According to the MSPSS mean scores, the study participants reported high levels of social support from family (mean score of the MSPSS-FAM ≥ 5; 79.73%, n = 240) and significant others (mean score of the MSPSS-SO ≥ 5; 73.75%, n = 222), while more than half (52.16%, n = 157) reported low-levels of support from friends (mean score of the MSPSS–FRI < 5). See Table 1.
Perceived Double Threat
This sample of Chinese Americans reported a high level of perceived threats (mean score ≥ 3), both from the COVID-19 virus (85.04%, n = 256) and personal threats due to their Chinese ethnic background (76.74%, n = 231). Besides the virus, the respondents expressed fear in the following situations: letting their children go outside by themselves (75.42%, n = 227), taking public transportation like buses or the subway (69.43%, n = 209), and grocery shopping (51.82%, n = 156). A small portion of the sample (n = 16, 5.32%) added fear of wearing masks in public.
Some mentioned a debate among their Chinese American WeChat groups on whether to wear a mask in public. Wearing the mask outside may draw unwanted attention to their ethnicity, but not wearing one truly was against their desire for self-protection from the coronavirus. “We were afraid of getting physically attacked if we wore one. But we knew all people in China wear masks, and all our families and friends in China reminded us of the importance of the masks, and they also mailed some to the United States for us. But, to wear or not to wear, it’s a question.”
Regarding open-end questions about abuse, nine members (2.99%) of this Chinese Americans sample reported having been yelled at in public. One participant describes the situation this way: “this is the darkest day during my over-20 years of life in the United States when I was yelled at on the street.” Another Chinese American reported his specific experience: “I was followed by a young man when I was out into the parking lot from the supermarket. I just bought some protective gear like goggles and N-95 masks from China and donated them to a local hospital. Then I went shopping for groceries on the way home. This made him feel very bad for days afterward and worried about his safety.” Three American-born Chinese described their feelings as: “this is the very first time I felt like I am not supposed to belong to this country.” “there is a sudden sense of being watched, that is as unsettling as it is unfamiliar.” “it’s especially hard when you grow up here and expect this world to be yours equally”.
Online Media and the Community COVID-19 Racial Discrimination
The high level of media/online and local community discrimination among Chinese Americans is shown in Table 1. About two-thirds of participants (n = 181, 60.13%) reported that they felt media or online discrimination. About half of the respondents reported personal experiences of racial discrimination by the local community (49.83%, n = 150).
The GAD-7 mean anxiety score in this sample was 9.1 (SD = 5.5). Almost half (49.50%, n = 149) of the participants had a mean score ≥ 10, indicating high levels of anxiety. See Table 1 for details.
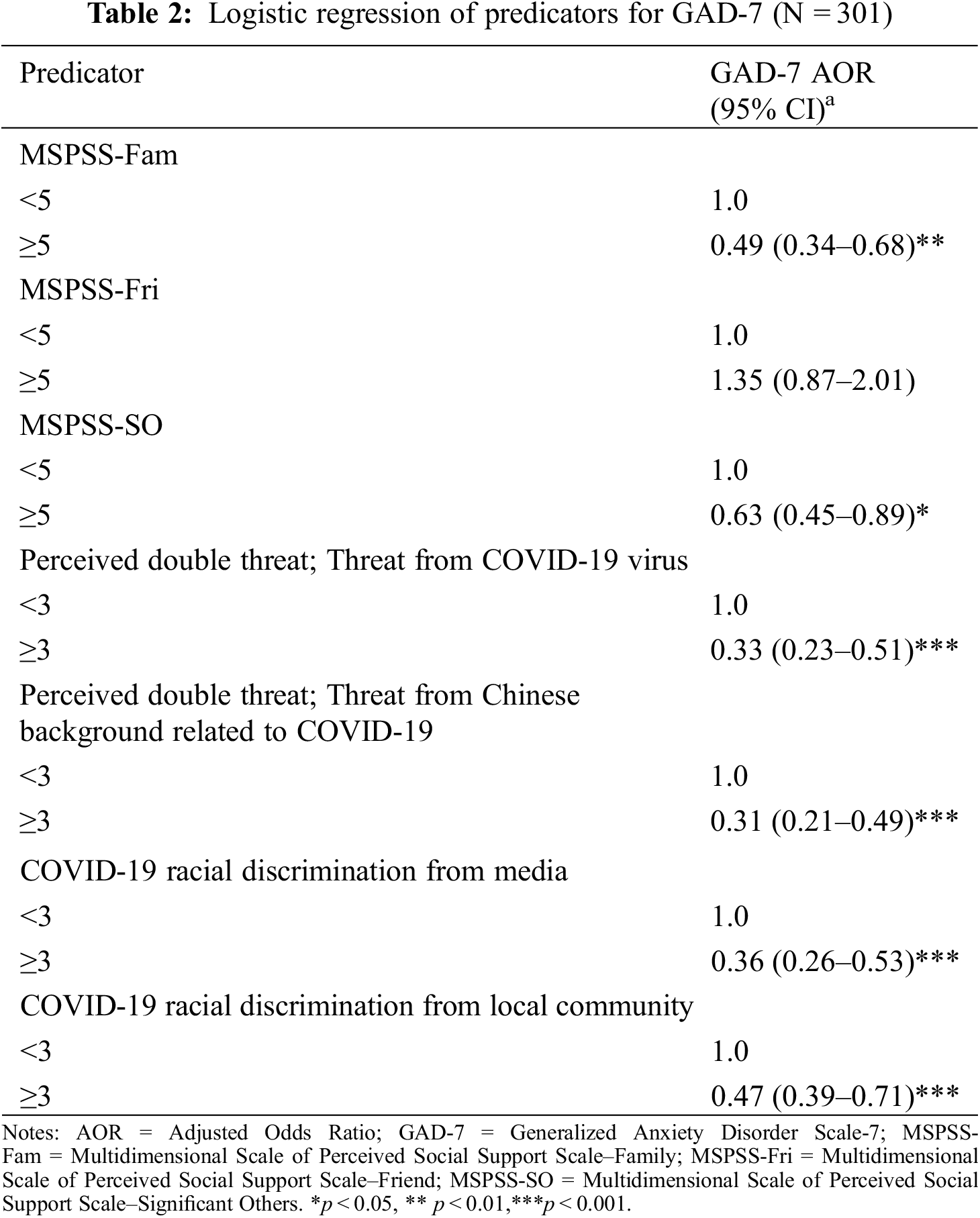
The results of the stepwise logistic regression of high anxiety on the five predictors are detailed in Table 2. The statically significant predictors for the high GAD-7 levels are listed as follows in order of magnitude: general COVID-19 racial discrimination from the local community (OR = 0.47, 95% CI = 0.39–0.71, p < 0.001) and media/online (OR = 0.36, 95% CI = 0.26–0.53, p < 0.001), followed by the perceived personal double threat from the COVID-19 virus (OR = 0.33, 95% CI = 0.23–0.51, p < 0.001) and discrimination due to their Chinese ethnic background (OR = 0.31, 95% CI = 0.21–0.49, p < 0.001), and then low levels of perceived social support from their family (OR = 0.49, 95% CI = 0.34–0.68, p < 0.01), and from others (OR = 0.63, 95% CI = 0.45–0.89, p < 0.05). Social support from friends did not enter the regression model because it was not a significant predictor of anxiety.
Chinese Americans although other population groups have been surveyed about their reactions and behaviors regarding COVID-19 precautions and quarantines, the double threat situations related to the pandemic Chinese Americans experienced and the relations with their mental health have not been explored. Our study explored Chinese Americans’ perceived double threat during the COVID-19 pandemic, racism and discrimination threats from the media/online, and their local communities. The findings provide evidence of the physical and psychological effects of the double threat to Chinese Americans as a result of the COVID-19 pandemic.
Almost half of the 301 Chinese Americans (49.50%, n = 149) survey respondents in our study reported having high levels of anxiety on the GAD-7 Anxiety measure with scores ≥ 10. This proportion of individuals who reported high pandemic anxiety was slightly higher than similar reports from American young adults (45.4%) [20] and much higher than the similar studies conducted before the COVID-19 pandemic. For instance, Spitzer et al. [47] found that 23.0% of United States primary care patients showed high levels of anxiety while Martin’ s [48] research demonstrated the rate of 21.0% in United States college students, and 17.4% of United States non-veteran community college students [49]. The high rates of anxiety among Chinese American participants may be related to their high level of perceived double threat situations, reflecting the overall ongoing distress in the U.S. in weeks after the American government announced COVID-19 closures during the weeks just before the current study period.
This sample of Chinese Americans might have especially suffered in this pandemic due to their race and nationality, combined with the uncertainty of this deadly pandemic. Despite the high levels of anxiety, these Chinese Americans generally received a high level of social support from family and significant others, which was a protective factor for their mental health. The high level of perceived social support might have been the result of previous communication with families and friends living in China. The residents of China already had received information about COVID-19 and practiced with required prevention measures, i.e., masks and quarantining. Reactions of Chinese Americans and other U.S. populations might have been influenced by cultural differences.
Compared to other Americans, Chinese Americans may have more tolerance to staying at home for days, even weeks to follow the government isolation requirements to avoid any possibility of becoming infected. These study findings are consistent with previous study findings that personal recognition of what could be as important as actual social support performance for people under the striving from negative emotions and anxiety during a public health crisis quarantine situation [50,51].
Even with the social support from family and significant others, Chinese Americans still reported high levels of perceived threats both from the virus itself and the racist discrimination, and attacks specifically experienced by them. Most of the participants (85.04%, n = 256) reported a high level of worry about the virus as a health threat, which was lower than the rate of 96.7% reported by the research on Chinese overseas students [46]. This may be explained by the different characteristics of the two study samples. The overseas students might have more fear of this deadly disease since they were studying alone abroad, away from their family and motherland. Further, over three-fourths of the current study participants (76.74%, n = 231) expressed a high level of fear of the ethnic racism threat in forms of discrimination due to their Chinese background. More than half of the participants worried about daily life situations listed here by the magnitude of the fear level: “afraid to let their kids go outside by themselves”, “afraid of taking public transportation like the bus or subway”, and “afraid of grocery shopping”.
The participants also shared their personal and specific experiences of ethnic racism attacks and discrimination like being yelled at in the public, followed in grocery shopping, and the dilemma of wearing or not wearing masks in public causing their ethnic group. Because these ethnic attacks and discriminations occurred in different forms might have led to their high perceived racism threat and lead to increased worries of safety and negative emotional feelings, even their sense of belonging in the United States: “the darkest day during my over-20 years of life in the United States”. This made him feel very bad for several days afterward and he continued to worry about his personal safety.” “it’s especially hard when you grow up here and expect this world to be yours equally”.
These fears of the threat of racial discrimination led groups of Chinese Americans to debate whether to wear a mask in public during the initial periods of the outbreak in their social media groups even among families. They wanted to wear masks for protection, but also had very strong concerns and fear of being labeled as someone who carries an infectious disease, as well as the prejudice and discrimination caused by their ethnic identity. In some instances, there were reports that Asians in the United States have experienced racist attacks while either wearing a protective mask or not wearing one. The prevalent discrimination and stigmatization suffered by Asian populations during the 2003 SARS outbreak negatively affected their mental health conditions and healthcare-seeking behaviors [52]. Our study also found that Chinese Americans’ perceived threat of racial discrimination negatively affected their mental health.
As one of the double threat experienced specifically, the sample of Chinese Americans also reported a perceived high level of COVID-19-related racial discrimination. About two-thirds of participants (n = 181, 60.13%) stated they felt discrimination from the media/online, and almost one-half (49.83%, n = 150) had experienced local community discrimination, which was higher than the CCN report rates of 31% but was a similar rate with the 58.2% (discrimination from media) and higher rate than 31.3% (discrimination from the local community) of the study on Chinese overseas students [27]. These higher rates of perceived discrimination are perhaps caused by the convenience sampling strategy which may recruit similar participants who are in close relationships and faced/talked about the same racist situations, which may strengthen their perception of that. The specific examples of verbal and physical attacks from others reported by the individual respondent and those high rates of perceived discrimination both from media/online and local community confirmed the “double threat” Chinese Americans experienced due to the COVID-19 pandemic. The high rates of double threat perceiving and anxiety levels from our sample may reflect ongoing distress, as we conducted the survey in the weeks following the American government directives for closures. Chinese Americans may have been particularly distressed in managing the threat of racism and discrimination besides the threat of the virus, and the pressure of school or work responsibilities during this time while having no sense of certainty regarding the pandemic’s end.
The high anxiety level and high perceived discrimination from media/online may also be due to the misinformation that can arise easily cause of the fast development of multiple media paths in the Internet Era, resulting in public panic with anxiety, stigmatization, and discrimination, also many other mental health issues. The study of changing perceptions of community risk and how the population viewed protective behaviors on Zika in 2016 documented how media affected health information and behaviors among the public [53]. Investigators found that social media affected attitudes of risk perception while legacy media (TV, radio) affected perceptions of protective behaviors [54]. The media showed a greater impact on the less educated population, which also should be considered by healthcare workers and indicate the need for healthcare workers to contribute the facts on social media, especially concerning the media influence on health attitudes and behaviors, health education, and care-seeking of patients and ethnic groups during the public emergency event.
These study findings support the body of literature on discrimination and stigmatization of specific ethnic groups associated with epidemics of infectious disease. For example, Russian Jewish immigrants from Eastern Europe were stigmatized and discriminated against in 1892 as the cause of typhus and cholera outbreaks [55]. The discrimination against Native Americans occurred in 1993 as the cause of the Hantavirus outbreak, often referred to as the Navajo disease in the United States [52].
Discrimination and stigmatization harm people’s attitudes and behavior toward seeking proper health care, as well as a general public response. Individuals with infectious diseases who believe or perceive they are discriminated against and stigmatized may delay seeking necessary health care or conceal their true situation, which may cause not only a delay in treatment but provide more opportunities to spread infectious diseases to others. The fear of the sick person will be amplified because of misinformation or improper media orientation. The entire population might be biased and stigmatized in some instances bringing about violence against individuals and groups. Mitigation of discrimination and stigmatization should be valued by healthcare professionals when referring to individuals, families, and communities [56]. This mitigation is especially important for the Chinese Americans who have been double threatened during this huge COVID-19 outbreak and uncertainty of international situations, addressing their high risks of stigma should be a concern for the public health of United States citizens.
Many Chinese Americans who lived in the United States for more than 20 years have led peaceful lives. The current double threatening situation facing the COVID-19 pandemic and its consequential racism disruptions have great potential for creating overwhelming feelings of anxiety and fear, and the dread of feeling unable to cope with the shifting situation. The individuals might become more isolated and begin to withdraw from their important healthy relationships, which leads to increased social and/or psychological problems.
Asian researchers concluded after they studied the influence of stigma related to HIV/AIDS, TB, and SARS: “More efforts should be placed in strategically changing the attributions made by the public towards infectious diseases. In so doing the public would develop more acceptable attitudes towards the diseases and the affected individuals. For preventive programs of infectious diseases to be effective, their associated stigma must be actively addressed.” [57]. So, healthcare workers should pay more attention to the ethnic discrimination threat the specific groups faced during the epidemic and some infectious diseases, and the indeed negative psychological influences.
These data were unique because of the timely focus on COVID-19 racial discrimination, while some limitations should be considered. First, generalizability is limited because the participants were recruited from the Western, Northeast, Southern, and Midwest regions of the United States. The situation varies from region to region, this may lead to biased study results. Future studies using more nationally representative Chinese American samples are warranted to increase the generalizability of these findings and to examine regional differences in discrimination experiences [58]. Second, the investigators used self-reporting, which is subject to social desirability bias [59], which was not assessed. Statistical control for social desirability bias and the inclusion of different reporters are recommended for future research. Third, the sample size of the present study is relatively small and may reduce the reliability of our findings. Finally, this study focused on the experiences of Chinese Americans, but other Asian American groups have been targeted by racism during COVID-19. Thus, other Asian Americans should be surveyed and the unique racism experiences and the effects of racism in Asian subgroups compared [58].
There is a long history of racial discrimination and stigmatization of disease. In addition to the normal stressors shared by many people during the COVID-19 pandemic, Chinese Americans must contend with the additional burden of ethnic discrimination, which is associated with worse depression and anxiety. The sense of belonging and social perceptions of Chinese immigrants is closely related to public health problems in Western societies and needs to be addressed at all levels. Our findings call for the attention of healthcare workers to specific racism double threatened situations and high mental health risks that Chinese Americans are experiencing during this pandemic [60], and also call for mental health professionals may consider exploring experiences of direct and indirect ethnic discrimination during the pandemic with Chinese American clients, its effects on their psychological well-being, and ways of coping with this additional stressor. Further research regarding the long-term implications of ethnic discrimination during the pandemic on Asian American well-being and effective coping ways to address this issue are also warranted.
Acknowledgement: Great thanks to Dr. Cheryl L. Brandt, Ph.D., RN, ACNS-BC, CNE (California State University San Bernardino, USA) for the manuscript edition.
Funding Statement: The research was supported by the Project of National Social Science Foundation of China (21BMZ018), the Philosophy and Social Science Project of Yunnan Province (YB2020093).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. World Health Organization (2022). WHO coronavirus disease (COVID-19) dashboard. https://covid19.who.int/ [Google Scholar]
2. He, Q., Fu, Y., Su, Y., Luan, Y. (2020). Understanding Chinese nursing education and practice for developing international nursing partnerships. Journal of Transcultural Nursing, 31(4), 406–412. https://doi.org/10.1177/1043659619872798 [Google Scholar] [PubMed] [CrossRef]
3. He, Q., Li, T., Su, Y., Luan, Y. (2021). Instructive messages and lessons from Chinese countermarching nurses of caring for COVID-19 patients: A qualitative study. Journal of Transcultural Nursing, 32(2), 96–102. https://doi.org/10.1177/1043659620950447 [Google Scholar] [PubMed] [CrossRef]
4. Cao, W., Fang, Z., Hou, G., Han, M., Xu, X. et al. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry, 287, 112934. https://doi.org/10.1016/j.psychres.2020.112934 [Google Scholar] [PubMed] [CrossRef]
5. Li, H. Y., Cao, H., Leung, D., Mak, Y. W. (2020). The psychological impacts of a COVID-19 outbreak on college students in China: A longitudinal study. International Journal of Environmental Research and Public Health, 17(11), 3933. https://doi.org/10.3390/ijerph17113933 [Google Scholar] [PubMed] [CrossRef]
6. World Health Organization (2020). WHO (COVID-19) homepage, China situation. https://covid19.who.int/region/wpro/country/cn [Google Scholar]
7. Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S. et al. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395(10227), 912–920. https://doi.org/10.1016/S0140-6736(20)30460-8 [Google Scholar] [PubMed] [CrossRef]
8. Bressan, V., Mansutti, I., Longhini, J., Moreale, R., Caruzzo, D. et al. (2022). Implications of quarantine among healthcare professionals: Findings from a scoping review. Archives of Environmental & Occupational Health, 77(10), 846–862. https://doi.org/10.1080/19338244.2022.2042171 [Google Scholar] [PubMed] [CrossRef]
9. Kim, H., Hong, J., Cho, I. K., Lee, D., Cho, E. et al. (2022). Psychometric properties of the stress and anxiety to viral epidemics-9 scale among front line nursing professionals working in the COVID-19 inpatients ward. Frontiers in Psychiatry, 13, 934202. https://doi.org/10.3389/fpsyt.2022.934202 [Google Scholar] [PubMed] [CrossRef]
10. Cai, W., Lian, B., Song, X., Hou, T., Deng, G. et al. (2020). A cross-sectional study on mental health among healthcare workers during the outbreak of corona virus disease 2019. Asian Journal of Psychiatry, 51, 102111. https://doi.org/10.1016/j.ajp.2020.102111 [Google Scholar] [PubMed] [CrossRef]
11. Chong, M. Y., Wang, W. C., Hsieh, W. C., Lee, C. Y., Chiu, N. M. et al. (2004). Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. The British Journal of Psychiatry: The Journal of Mental Science, 185, 127–133. https://doi.org/10.1192/bjp.185.2.127 [Google Scholar] [PubMed] [CrossRef]
12. Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J. et al. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e203976–e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 [Google Scholar] [PubMed] [CrossRef]
13. Si, M. Y., Su, X. Y., Jiang, Y., Wang, W. J., Gu, X. F. et al. (2020). Psychological impact of COVID-19 on medical care workers in China. Infectious Diseases of Poverty, 9(1), 1–13. https://doi.org/10.1186/s40249-020-00724-0 [Google Scholar] [PubMed] [CrossRef]
14. Wang, Y., Wang, P. (2019). Perceived stress and psychological distress among Chinese physicians: The mediating role of coping style. Medicine, 98(23), e15950. https://doi.org/10.1097/MD.0000000000015950 [Google Scholar] [PubMed] [CrossRef]
15. Xiang, Y. T., Jin, Y., Wang, Y., Zhang, Q., Zhang, L. et al. (2020). Tribute to health workers in China: A group of respectable population during the outbreak of the COVID-19. International Journal of Biological Sciences, 16(10), 1739–1740. https://doi.org/10.7150/ijbs.45135 [Google Scholar] [PubMed] [CrossRef]
16. Smallwood, N., Willis, K. (2021). Mental health among healthcare workers during the COVID-19 pandemic. Respirology, 26(11), 1016–1017. https://doi.org/10.1111/resp.14143 [Google Scholar] [PubMed] [CrossRef]
17. Nicomedes, C. J. C., Avila, R. M. A. (2020). An analysis on the panic during COVID-19 pandemic through an online form. Journal of Affective Disorders, 276, 14–22. https://doi.org/10.1016/j.jad.2020.06.046 [Google Scholar] [PubMed] [CrossRef]
18. Werneke, U., van der Feltz-Cornelis, C., Löwe, B., Ventriglio, A., Bhugra, D. (2022). Editorial: Outbreak investigation: Mental health in the times of coronavirus (COVID-19). Frontiers in Psychiatry, 13, 854388. https://doi.org/10.3389/fpsyt.2022.854388 [Google Scholar] [PubMed] [CrossRef]
19. Talevi, D., Socci, V., Carai, M., Carnaghi, G., Faleri, S. et al. (2020). Mental health outcomes of the CoViD-19 pandemic. Rivista Di Psichiatria, 55(3), 137–144. https://doi.org/10.1708/3382.33569 [Google Scholar] [PubMed] [CrossRef]
20. Liu, C. H., Zhang, E., Wong, G. T. F., Hyun, S. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for US young adult mental health. Psychiatry Research, 290, 113172. https://doi.org/10.1016/j.psychres.2020.113172 [Google Scholar] [PubMed] [CrossRef]
21. Wood, C. I., Yu, Z., Sealy, D. A., Moss, I., Zigbuo-Wenzler, E. et al. (2022). Mental health impacts of the COVID-19 pandemic on college students. Journal of American College Health. https://doi.org/10.1080/07448481.2022.2040515 [Google Scholar] [PubMed] [CrossRef]
22. Buizza, C., Bazzoli, L., Ghilardi, A. (2022). Changes in college students mental health and lifestyle during the COVID-19 pandemic: A systematic review of longitudinal studies. Adolescent Research Review, 7(4), 537–550. https://doi.org/10.1007/s40894-022-00192-7 [Google Scholar] [PubMed] [CrossRef]
23. Xu, F., Huang, L. (2022). Impacts of stress response and negative emotion on mental health of college students during the COVID-19 outbreak. Frontiers in Psychiatry, 12, 784661. https://doi.org/10.3389/fpsyt.2021.784661 [Google Scholar] [PubMed] [CrossRef]
24. Cohen, Z. P., Cosgrove, K. T., DeVille, D. C., Akeman, E., Singh, M. K. et al. (2021). The impact of COVID-19 on adolescent mental health: Preliminary findings from a longitudinal sample of healthy and at-risk adolescents. Frontiers in Pediatrics, 9, 622608. https://doi.org/10.3389/fped.2021.622608 [Google Scholar] [PubMed] [CrossRef]
25. Borja, M., Jeung, R., Horse, A. Y., Gibson, J., Gowing, S. et al. (2020). Anti-Chinese rhetoric tied to racism against asian Americans stop AAPI hate report. https://caasf.org/2020/06/anti-chinese-rhetoric-tied-to-racism-against-asian-americans-stop-aapi-hate-report/ [Google Scholar]
26. Shoichet, C. E. (2020). 31% of Asian Americans say they’ve been subject to racist slurs or jokes since the coronavirus pandemic began. https://www.cnn.com/2020/07/01/us/coronavirus-discrimination-study/index.html [Google Scholar]
27. Ma, H., Miller, C. (2021). Trapped in a double bind: Chinese overseas student anxiety during the COVID-19 pandemic. Health Communication, 36(13), 1598–1605. https://doi.org/10.1080/10410236.2020.1775439 [Google Scholar] [PubMed] [CrossRef]
28. Zhai, Y., Du, X. (2020). Mental health care for international Chinese students affected by the COVID-19 outbreak. The Lancet Psychiatry, 7(4), e22. https://doi.org/10.1016/S2215-0366(20)30089-4 [Google Scholar] [PubMed] [CrossRef]
29. Bitters, J. (2020). Chinese Americans leverage ties abroad to bring PPE to silicon valley. https://sanjosespotlight.com/chinese-americans-leverage-ties-abroad-to-bring-ppe-to-silicon-valley/ [Google Scholar]
30. Mapp, L. J. (2020). Chinese American groups donate medical supplies to help fight coronavirus. https://www.sandiegouniontribune.com/caregiver/news-for-caregivers/story/2020-04-20/chinese-american-groups-donate-medical-supplies-to-help-fight-coronavirus [Google Scholar]
31. Xinhua Net (2020). Spotlight: Southern California Chinese Americans donate much-needed supplies to U.S. hospitals, first responders. http://www.xinhuanet.com/english/2020-04/12/c_138967815.htm [Google Scholar]
32. He, Q. (2017). Caring for Chinese-American home care patients. Home Healthcare Now, 35(4), 211–214. https://doi.org/10.1097/nhh.0000000000000525 [Google Scholar] [PubMed] [CrossRef]
33. Hooper, K., Batalova, J. (2015). Chinese immigrants in the United States: Migration Policy Institute. https://www.immigrationresearch.org/system/files/Chinese_Immigrants_in_the_United_States.pdf [Google Scholar]
34. Kharpal, A. (2019). Everything you need to know about WeChat—China’s billion-user messaging app. https://www.cnbc.com/2019/02/04/what-is-wechat-china-biggest-messaging-app.html [Google Scholar]
35. Zhang, Q. L., Liu, J. F., Xie, W. P., Cao, H., Chen, Q. (2021). The effect of WeChat on parental care burden, anxiety, and depression in children after CHD surgery during COVID-19 pandemic. Applied Clinical Informatics, 12(4), 768–773. [Google Scholar] [PubMed]
36. Zimet, G. D., Dahlem, N. W., Zimet, S. G., Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. https://doi.org/10.1207/s15327752jpa5201_2 [Google Scholar] [CrossRef]
37. Dambi, J. M., Corten, L., Chiwaridzo, M., Jack, H., Mlambo, T. et al. (2018). A systematic review of the psychometric properties of the cross-cultural translations and adaptations of the multidimensional perceived social support scale (MSPSS). Health and Quality of Life Outcomes, 16(1), 1–19. https://doi.org/10.1186/s12955-018-0912-0 [Google Scholar] [PubMed] [CrossRef]
38. Chou, K. L. (2000). Intimacy and psychosocial adjustment in Hong Kong Chinese adolescents. The Journal of Genetic Psychology, 161(2), 141–151. https://doi.org/10.1080/00221320009596701 [Google Scholar] [PubMed] [CrossRef]
39. Guan, N. C., Seng, L. H., Hway Ann, A. Y., Hui, K. O. (2015). Factorial validity and reliability of the Malaysian simplified Chinese version of multidimensional scale of perceived social support (MSPSS-SCV) among a group of university students. Asia Pacific Journal of Public Health, 27(2), 225–231. https://doi.org/10.1177/1010539513477684 [Google Scholar] [PubMed] [CrossRef]
40. De Maria, M., Vellone, E., Durante, A., Biagioli, V., Matarese, M. (2018). Psychometrics evaluation of the multidimensional scale of perceived social support (MSPSS) in people with chronic disease. Annali Dell’Istituto Superiore di Sanità, 54(4), 308–315. https://doi.org/10.4415/ann_18_04_07 [Google Scholar] [PubMed] [CrossRef]
41. Nearchou, F., Davies, A., Hennessy, E. (2019). Psychometric evaluation of the multi-dimensional scale of perceived social support in young adults with chronic health conditions. Irish Journal of Psychological Medicine, 39(4), 386–390. https://doi.org/10.1017/ipm.2019.54 [Google Scholar] [PubMed] [CrossRef]
42. Wang, Y., Wan, Q., Huang, Z., Huang, L., Kong, F. (2017). Psychometric properties of multi-dimensional scale of perceived social support in Chinese parents of children with cerebral palsy. Frontiers in Psychology, 8, 2020. https://doi.org/10.3389/fpsyg.2017.02020 [Google Scholar] [PubMed] [CrossRef]
43. Haft, S. L., Zhou, Q. (2021). An outbreak of xenophobia: Perceived discrimination and anxiety in Chinese American college students before and during the COVID–19 pandemic. International Journal of Psychology, 56(4), 522–531. [Google Scholar] [PubMed]
44. Tavernise, S., Oppel Jr, R. A. (2020). Spit on, yelled at, attacked: Chinese-Americans fear for their safety. The New York Times, 23. [Google Scholar]
45. Eisinga, R., Te Grotenhuis, M., Pelzer, B. (2013). The reliability of a two-item scale: Pearson, cronbach, or spearman-brown? International Journal of Public Health, 58(4), 637–642. https://doi.org/10.1007/s00038-012-0416-3 [Google Scholar] [PubMed] [CrossRef]
46. Miller, M. J., Kim, J., Chen, G. A., Alvarez, A. N. (2012). Exploratory and confirmatory factor analyses of the asian American racism-related stress inventory. Assessment, 19(1), 53–64. https://doi.org/10.1177/1073191110392497 [Google Scholar] [PubMed] [CrossRef]
47. Spitzer, R. L., Kroenke, K., Williams, J. B., Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092 [Google Scholar] [PubMed] [CrossRef]
48. Martin, R. J., Usdan, S., Cremeens, J., Vail-Smith, K. (2014). Disordered gambling and co-morbidity of psychiatric disorders among college students: An examination of problem drinking, anxiety and depression. Journal of Gambling Studies, 30(2), 321–333. https://doi.org/10.1007/s10899-013-9367-8 [Google Scholar] [PubMed] [CrossRef]
49. Fortney, J. C., Curran, G. M., Hunt, J. B., Cheney, A. M., Lu, L. et al. (2016). Prevalence of probable mental disorders and help-seeking behaviors among veteran and non-veteran community college students. General Hospital Psychiatry, 38, 99–104. https://doi.org/10.1016/j.genhosppsych.2015.09.007 [Google Scholar] [PubMed] [CrossRef]
50. Santini, Z. I., Koyanagi, A. (2021). Loneliness and its association with depressed mood, anxiety symptoms, and sleep problems in Europe during the COVID-19 pandemic. Acta Neuropsychiatrica, 33(3), 160–163. https://doi.org/10.1017/neu.2020.48 [Google Scholar] [PubMed] [CrossRef]
51. Koh, J. X., Liew, T. M. (2022). How loneliness is talked about in social media during COVID-19 pandemic: Text mining of 4,492 twitter feeds. Journal of Psychiatric Research, 145, 317–324. https://doi.org/10.1016/j.jpsychires.2020.11.015 [Google Scholar] [PubMed] [CrossRef]
52. Person, B., Sy, F., Holton, K., Govert, B., Liang, A. (2004). Fear and stigma: The epidemic within the SARS outbreak. Emerging Infectious Diseases, 10(2), 358–363. https://doi.org/10.3201/eid1002.030750 [Google Scholar] [PubMed] [CrossRef]
53. Chan, M. P. S., Winneg, K., Hawkins, L., Farhadloo, M., Jamieson, K. H. et al. (2018). Legacy and social media respectively influence risk perceptions and protective behaviors during emerging health threats: A multi-wave analysis of communications on zika virus cases. Social Science & Medicine, 212, 50–59. https://doi.org/10.1016/j.socscimed.2018.07.007 [Google Scholar] [PubMed] [CrossRef]
54. Hadi, T., MacGregor, J., Mann, L. (2017). Social media monitoring: 2016 zika response in NYC. Health Security, 15(4), 440–444. https://doi.org/10.1089/hs.2017.0031 [Google Scholar] [PubMed] [CrossRef]
55. Raikova, S. V., Zavialov, A. I. (2013). Typhus fever morbidity among the military personnel and civilians in the regions around Volga river during world War I. Voenno-medicinskij Žurnal, 334(7), 56–61. [Google Scholar]
56. Perry, P., Donini-Lenhoff, F. (2010). Stigmatization complicates infectious disease management. Virtual Mentor, 12(3), 225–230. https://doi.org/10.1001/virtualmentor.2010.12.3.mhst1-1003 [Google Scholar] [PubMed] [CrossRef]
57. Mak, W. W., Mo, P. K., Cheung, R. Y., Woo, J., Cheung, F. M. et al. (2006). Comparative stigma of HIV/AIDS, SARS, and tuberculosis in Hong Kong. Social Science & Medicine, 63(7), 1912–1922. https://doi.org/10.1016/j.socscimed.2006.04.016 [Google Scholar] [PubMed] [CrossRef]
58. Gee, G. C., Spencer, M. S., Chen, J., Takeuchi, D. (2007). A nationwide study of discrimination and chronic health conditions among Asian Americans. American Journal of Public Health, 97(7), 1275–1282. https://doi.org/10.2105/AJPH.2006.091827 [Google Scholar] [PubMed] [CrossRef]
59. Krieger, N., Smith, K., Naishadham, D., Hartman, C., Barbeau, E. M. (2005). Experiences of discrimination: Validity and reliability of a self-report measure for population health research on racism and health. Social Science & Medicine, 61(7), 1576–1596. https://doi.org/10.1016/j.socscimed.2005.03.006 [Google Scholar] [PubMed] [CrossRef]
60. Gee, G. C., Ro, M. J., Rimoin, A. W. (2020). Seven reasons to care about racism and COVID-19 and seven things to do to stop it. American Journal of Public Health, 110(7), 954–955. https://doi.org/10.2105/AJPH.2020.305712 [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools