 Open Access
Open Access
ARTICLE
Associations of Domain and Pattern of Sedentary Behaviors with Symptoms of Mental Disorders in Saudi Adults: ‘The Sedentary Behavior Paradox’
Department of Exercise Physiology, College of Sport Sciences and Physical Activity, King Saud University, Riyadh, 80200, Saudi Arabia
* Corresponding Author: Abdullah B. Alansare. Email:
International Journal of Mental Health Promotion 2024, 26(1), 11-20. https://doi.org/10.32604/ijmhp.2023.044656
Received 05 August 2023; Accepted 01 November 2023; Issue published 05 February 2024
Abstract
Emerging evidence suggests the existence of ‘paradoxical’ relationships between domain-specific sedentary behavior (SB) and health outcomes. This study assessed the associations of total and domain-specific SB, by pattern, with symptoms of mental disorders in Saudi adults. Participants (n = 554) completed a web-based survey between January 18th, 2023 and February 5th, 2023. Total SB was measured by using the Sedentary Behavior Questionnaire. Total SB was then partitioned into leisure, occupational, and commuting SB during weekdays and on weekend days. Symptoms of mental disorders including symptoms of depression, anxiety, and stress were evaluated by using the DASS-21 questionnaire. Adjusted linear regressions estimated associations of SB with these symptoms of mental disorders. Mann-Whitney tests compared these symptoms between Saudi adults who accumulated excessive total SB (≥8 hours/day) and those who did not. The results showed that higher total and leisure SB was associated with unfavorable symptoms of depression, anxiety, and stress (p < 0.05 for all). Paradoxically, greater occupational SB on weekend days and commuting SB in weekdays favorably associated with depressive symptoms (p < 0.05 for all). Saudi adults who accumulated excessive total SB had worse symptoms of mental disorders (p < 0.05 for all). In summary, these findings provide evidence for the existence of the ‘Paradoxical Sedentary Behavior’ regarding depression. All SB is not created equal. Interventions that aim at improving mental health should target not only excessive total SB, but also total and domain-specific SB during the week and in weekdays and on weekend days while using individualized strategies.Keywords
Mental disorders such as depression, anxiety, and certain types of stress are clinically significant psychological or behavioral disturbances that occur in individuals, and it is prevalent worldwide [1–3]. A robust meta-analysis estimated that mental disorders are attributed to 14.3% of global mortality (i.e., ~8 million deaths per year) [4]. Furthermore, it is projected that the global economic burden of mental disorders will be 16.3 trillion US dollars between 2011 and 2030 [5]. Hence, efforts to reduce mental disorders and its repercussions are critical to preserve lives lost and global economy.
Of particular interest is the pervasiveness of mental disorders in Saudi adults. A national investigation discovered that 34% of Saudi adults have been diagnosed with mental disorders during their lives [6]. This means that 2 out of 5 Saudi adults have been diagnosed with a mental disorder such as depression and anxiety [6]. Shockingly, 80% of these diagnosed individuals do not receive treatment [6]. Several factors have been suggested to impede access to the treatments of mental disorders for Saudi adults, including high treatment cost, stigma associated with mental disorders, and low perceived need [7–9]. As such, strategies to overcome these barriers, as well as early prevention of mental disorders and its risk factors are indispensable to reducing the economic and health burdens of mental disorders in Saudi Arabia.
Lifestyle modifications have been proposed as a potential effective strategy to prevent and reduce the risk of mental disorders. For instance, sedentary behavior (SB), which is defined as any activity that occurs while seated, laying, or reclining and has low energy expenditure [10], has emerged as a significant risk factor for several chronic diseases, including mental disorders, independent of physical inactivity [11,12]. For instance, accumulating excessive SB (≥8 hours/day) increases the risk of depression by 20% [13]. Importantly, the majority of the existing research examined these associations by measuring total SB or SB in front of screens only [11]. Whether the correlations observed differ by other domain-specific SB (e.g., other leisure SB, occupational SB, commuting SB) and patterns of SB (e.g., weekdays vs. weekend days) have been overlooked, especially in Saudi adults. This knowledge gap is of clinical significance because growing evidence suggests ‘paradoxical’ relationships between various domain-specific activities (e.g., leisure vs. occupational) and major risk factors for chronic disease [14–17]. For example, leisure SB have been shown to have detrimental associations, whereas occupational SB has tended to have beneficial correlations with these risk factors [15–17]. As such, clarification of the correlations between domain-specific SB and mental disorders is essential to boost advocacy efforts for mental disorders and maximize its benefits in Saudi adults.
Therefore, the primary aim of this study was to evaluate the associations of total and domain-specific (i.e., leisure, occupational, and commuting) SB and its patterns with symptoms of mental disorders, including depression, anxiety, and stress, in Saudi adults. Based on previous research that found leisure SB to be detrimental and occupational SB to be beneficial for health outcomes [15–17], it was hypothesized that total SB would be detrimentally associated with these psychological indicators, and that these relationships would be stronger for leisure SB compared to other domain-specific SB. A secondary aim of this study was to examine the relationships between excessive total SB (≥8 hours/day) and these symptoms of mental disorders. In comparison with a previous study that revealed increased risk for mental disorders among those who accumulate excessive total SB [13], it was hypothesized that Saudi adults who accumulate excessive total SB per day would have worse symptoms of depression, anxiety, and stress compared to those who do not.
This anonymous, cross-sectional, web-based study targeted Saudi adults. The decision to use the web-based method was to: 1) ease the reach to more adults from various Saudi regions, 2) overcome the cultural challenges to access Saudi females, and 3) surmount the probable research fatigue (i.e., avoid participation) and/or COVID-19 phobia following COVID-19 outbreak [18,19]. As such, the results of this study may be more generalizable to the Saudi adult population. Data was collected between January 18, 2023 and February 05, 2023. Microsoft online survey creator (Microsoft Forms) was utilized to design a structured questionnaire. The link to this questionnaire was shared through the most popular social media platforms by adults in Saudi Arabia (i.e., Twitter, Instagram, Snap Chat, and WhatsApp) [20].
The structure web-based questionnaire consisted of electronic informed consent, measurements of potential confounders (i.e., demographic, anthropometric, and socioeconomical variables), SB assessments, and evaluations of psychological states. Details of these measurements are as follows.
All participants self-reported their age (years), biological sex (i.e., female or male), the region of Saudi Arabia where they currently live (i.e., central, western, eastern, southern, northern, or did not report), current smoking status (i.e., current smoker or not a current smoker), if they have been diagnosed with a chronic disease (i.e., yes or no), and if they have been diagnosed with a psychological disease (i.e., yes or no).
All participants also self-reported their body’s height in centimeters (cm) and weight in kilograms (kg) according to their last measurements. Body mass index (BMI) was then calculated using these measures as follows: BMI = body’s weight (kg)/body’s height (meter squared (m2)). Thereafter, the BMI score was utilized to classify the participants into the following categories: 1) obese (BMI > 30 kg/m2), 2) overweight (BMI between 25 and 29.9 kg/m2), 3) healthy weight (BMI between 18.5 and 24.9 kg/m2), and 4) underweight (BMI < 18.5 kg/m2).
Furthermore, other important potential confounders were reported by all participants including their marriage status (i.e., single, married, divorced, or widower), if they had children (i.e., yes or no), their highest earned degree (i.e., high school or less, diploma, bachelor, Master’s, or PhD), their present occupation (i.e., governmental sector, private sector, currently unemployed, retired, or student), and their current monthly income in Saudi Riyals (i.e., less than 5,000, 5,000 to 10,000, 11,000 to 15,000, 16,000 to 20,000, more than 20,000, or did not repot).
Sedentary behavior assessments
Total and domain-specific (i.e., leisure, occupational, and commuting) SB were assessed by using the Arabic version of the Sedentary Behavior Questionnaire (SBQ) [21,22]. This instrument includes questions about time spent (hours/day) in nine different SBs during a weekday, and then repeats the same questions to measure time spent (hours/day) in these SB on a weekend day (i.e., a total of 18 questions). These nine different SBs are listed as follows: 1) watching TV, 2) playing computer or video games, 3) sitting and listening to music, 4) sitting and talking on the phone, 5) doing paperwork or computer work (office work, emails, paying bills, etc.), 6) sitting and reading a book or magazine, 7) playing a musical instrument, 8) doing artwork or crafts, and 9) siting and driving a car, bus, or train [21]. Data from these questions were used to calculate total, leisure, occupational, and commuting SB during a weekday or on a weekend day [23] as described in the Suppl. Table S1.
The Arabic, short version of the DASS-21 questionnaire was utilized to evaluate the current psychological states in Saudi adults [24,25]. This instrument is a valid and reliable tool that assesses three negative emotional states including depression, anxiety, and stress [24,26]. This questionnaire consists of 21 items of which a set of seven items are used to measure one psychological state [26]. In other words, each psychological state is evaluated by seven relevant items. Each item can be scored from 0 to 3 points, and the sum of these items is then multiplied by 2 to acquire the total score for each scale (i.e., the score for each scale ranges from 0 to 14) [25,26]. As indicated in the psychometric properties paper for the DASS-21, the reason for multiplying the total score by 2 is to make the results comparable to the original long-version DASS (DASS-42) [27]. The total score for each scale can then be used to classify individuals for each psychological symptom, into conventional severity labels as follows: normal, mild, moderate, severe, or extremely severe symptoms [26]. The depression scale measures characteristics such as self-disparaging, pessimistic about the future, or unable to experience enjoyment or satisfaction. Whereas the anxiety scale measures characteristics such as apprehensive, shaky, or worried about performance. The stress scale, on the other hand, measures characteristics such as tense, touchy, or easily startled.
Raosoft calculator was utilized, as follows, to determine the sample size needed for this study. First, the current Saudi population was reported to be 35,013,424. Using the power of 80% and confidence level of 95% with a margin of error of 5%, at least 385 adults were required to represent the Saudi population. Still, a higher sample size was attained to enhance the generalizability of the study’s conclusions.
The demographic, anthropometric, and socioeconomical variables as well as total SB for the participants were reported as means and standard deviations or frequencies and percentages, as appropriate. To check for potential outliers, the first quartile, median, the third quartile, and interquartile range were calculated. Afterward, the lower (the first quartile − [1.5 × interquartile range]) and upper (the third quartile + [1.5 × interquartile range]) fences were determined [28]. Any points that were below or above the calculated lower and upper fences were carefully checked and omitted if they were not reasonable.
Then, multiple linear regression models were constructed to assess the associations of total and domain-specific SB with depression, anxiety, and stress as follows. First, these relationships were assessed in unadjusted models (i.e., Model 1). Model 2 then assessed these associations while adjusting for potential confounders including demographic (i.e., age, sex, current smoking status, having chronic diagnosed disease), anthropometric (i.e., age, BMI), and socioeconomical (i.e., marriage status, having children, current degree, occupations, and monthly income). For the associations with domain-specific SB, further simultaneous adjustment for leisure, occupational, and commuting SB was performed. To evaluate the effect sizes for these associations, Cohen’s d was calculated (β/the standard deviation of the dependent variable), and the magnitude of the relationships was determined as small (d = 0.2), medium (d = 0.5), or large (d = 0.8).
Lastly, Mann-Whitney tests compared depression, anxiety, and stress scores between Saudi adults accumulating vs. not accumulating excessive total SB. To evaluate the magnitude of the differences, the rank-biserial correlation (rB) was used as follows: large if rB = .5, medium if rB = .3, and small if rB = .1. Significant level was set as p-value < 0.05 for all statistical tests. All statistical analyses were performed by using JASP software (JASP 0.15 Version).
Participants (n = 3) who did not report their height and/or weight, participants who had unreasonable BMI that was below or above the fences of outliers (n = 4) were excluded from the present analyses. Furthermore, participants (n = 1) who reported total SB of >24 hours/day were also excluded from the current analyses. The exclusion of these participants (n = 8) was to avoid the effects of outliers or potential problematic influential points. Moreover, participants (n = 48) who reported being diagnosed with psychological disorders (e.g., depression, bipolar) were omitted from the present analyses. Therefore, the total number of omitted participants from the current analyses was n = 56.
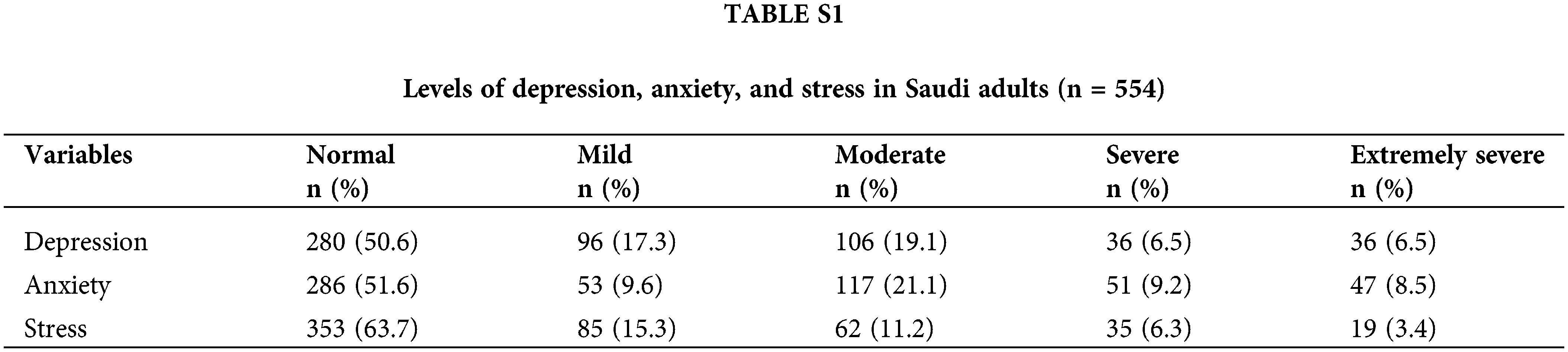
Table 1 displays the general characteristics of the included participants (n = 554). On average, they were 38.5 years old. More than half of these participants were male, married, non-smokers with overweight or obesity but free from reported chronic diseases. They also tended to be highly educated, working in the governmental sector, and from western region of Saudi Arabia. Importantly, approximately 40% of these participants accumulated excessive total SB (≥8 hours/day). Lastly, the majority of the participants were classified into normal severity categories for depression, anxiety, and stress symptoms (Suppl. Table S1).
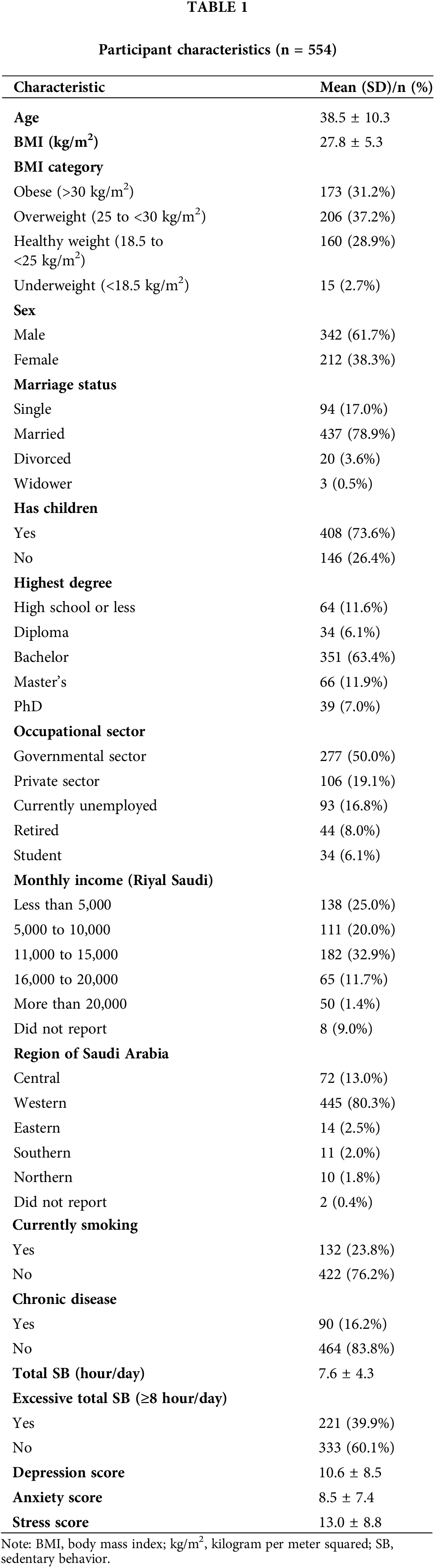
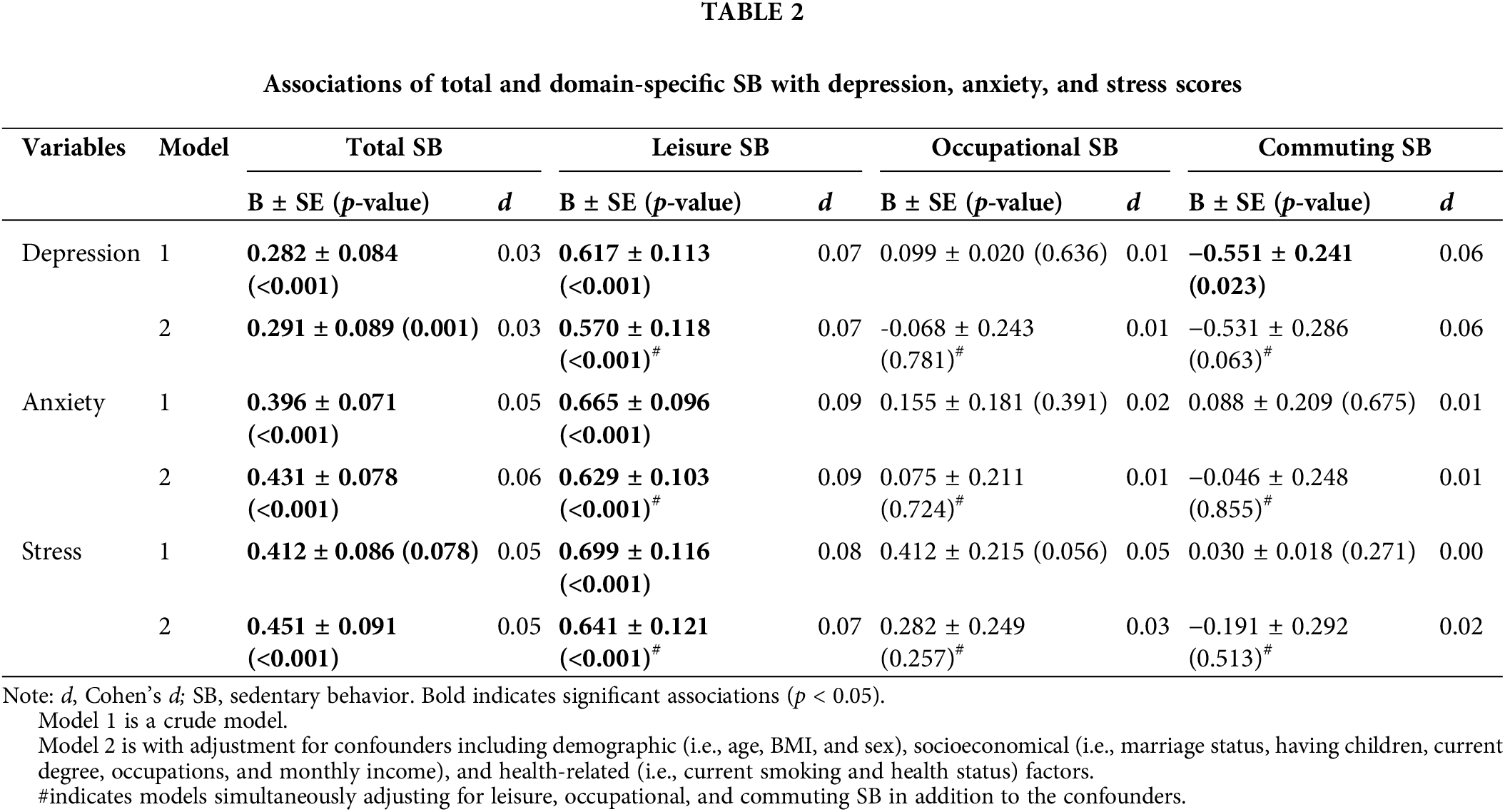
Table 2 presents the associations of total and domain-specific SB with depression, anxiety, and stress scores in Saudi adults. As it was hypothesized for the primary aim, adjusted models found that higher total and leisure SB were detrimentally associated with higher depression, anxiety, and stress scores (p < 0.001 for all). Yet, these relationships observed appeared slightly stronger for leisure SB as compared to total SB. On the other hand, adjusted models revealed that higher occupational or commuting SB did not associate with any of these psychological indicators (p > 0.05 for all). Noteworthy, the Cohen’s d values showed that the magnitude of these effects were trivial (d = 0.03 to 0.09).
When the patterns of total and domain-specific SB were considered (i.e., weekdays or weekend days separately), several interesting ‘paradoxical’ associations emerged (Table 3). During weekdays, adjusted models revealed that only higher leisure SB was significantly correlated with higher anxiety and stress scores (p < 0.05 for both). Paradoxically, higher commuting SB was significantly associated with lower depression score (p = 0.005). No other relationships were observed during weekdays. On weekend days, adjusted models found that higher total and leisure SB were associated with higher anxiety score (p < 0.05 for both). In contrast, higher occupational SB was related to lower depression score (p = 0.025). No other associations were detected on weekend days. Importantly, though the relationships observed were statistically significant, Cohen’s d indicated that the magnitudes of these effects ranged from trivial to small (d = 0.03 to 0.14).
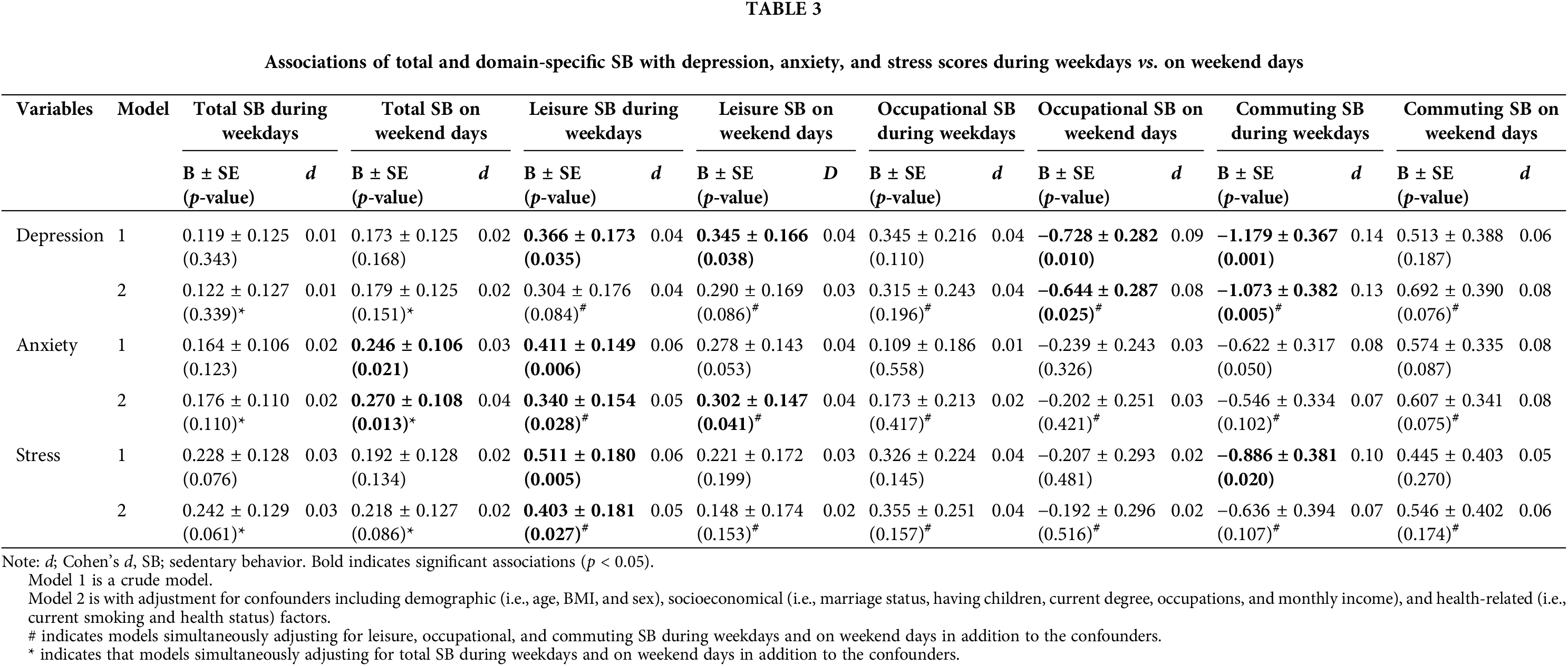
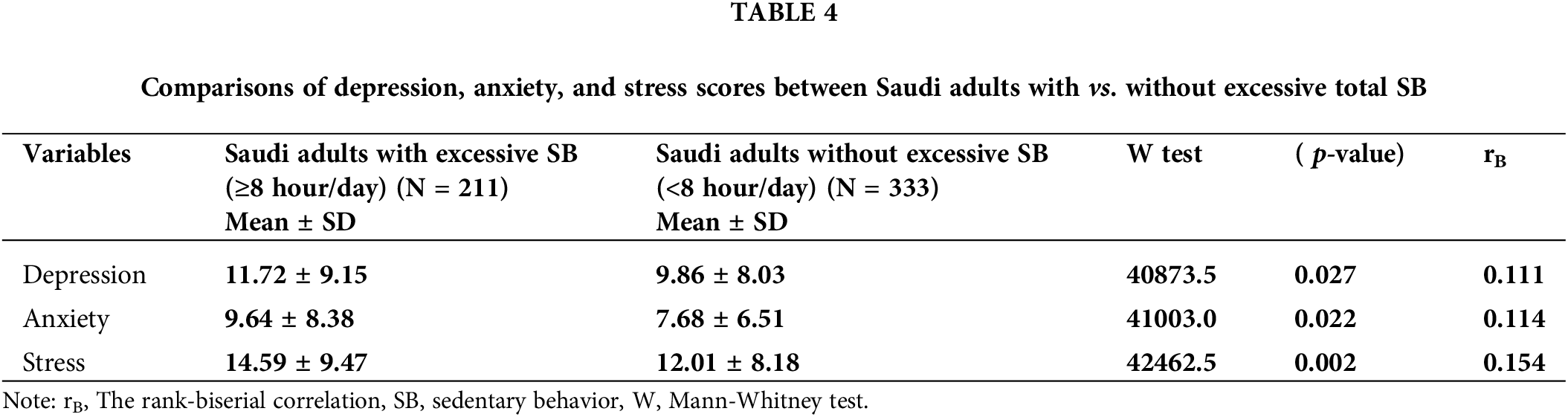
Table 4 displays the differences in depression, anxiety, and stress scores according to total SB level (i.e., accumulating vs. not accumulating excessive total SB). As it was hypothesized for the secondary aim, Saudi adults who engaged in excessive total daily SB had significantly worse depression, anxiety, and stress scores compared to those who did not (p < 0.05). The rank-biserial correlation indicated that these differences ranged from small to mild magnitudes (rB = 0.11 to 0.15).
This study was the first to uniquely examine the associations of the domain-specific patterns of SB with symptoms of mental disorders in Saudi adults. Higher amounts of total and leisure SB were deleteriously associated with symptoms of depression, anxiety, and stress in Saudi adults. Though high total SB unfavorably correlated to these symptoms, high leisure SB had stronger associations. The current novel findings suggest the existence of ‘the Sedentary Behavior Paradox’ with regards to mental disorders, specifically with depression, in adults. Total and leisure SB may be detrimental, while occupational and commuting SB may be beneficial for the symptoms of depression, particularly when the pattern (i.e., weekdays vs. weekend days) of SB is taken into consideration. Remarkably, the present results also found statistically significant relationships between excessive total SB and these symptoms of mental disorders. Specifically, Saudi adults (2 out of 5 individuals) who accumulated excessive total SB (≥8 hours/day) had significantly worse symptoms of depression, anxiety, and stress compared to those who did not accumulate excessive total SB.
Associations of SB with the symptoms of depression
A recent overview of systematic reviews proficiently synthesized the literature on the associations of SB with depression in American, European, and Australian adults [29]. It was demonstrated that high total SB and TV watching adversely correlated with depression and symptoms of depression, while high internet- and computer-based SB had favorable associations [29]. These findings suggest that the correlations between SB and depressive symptoms appear to be context-dependent. Further adding to this evidence, the present study observed that the associations of SB with symptoms of depression may also be domain- and pattern-dependent in a more complex fashion. It was determined that only high total and leisure SB had significant unfavorable associations with the depressive symptoms in Saudi adults. Nonetheless, when the pattern (i.e., weekdays and weekend days) of SB was considered, these associations were slightly attenuated and occupational SB on weekend days and commuting SB during weekdays were significantly associated with favorable depressive symptoms.
Although well-defined explanations for the paradoxical associations observed between domain-specific SB and symptoms of depression are not yet established, a few theoretical mechanisms were speculated. First, time spent in leisure SB is likely to displace time spent in moderate to vigorous intensity physical activity, which is an activity that mainly occurs during leisure time and has noticeable benefits for depression and depression symptoms [30,31]. Furthermore, leisure SB is likely to be prolonged bouts [16] and comprise socially isolated behaviors (e.g., TV watching, playing video games), which may promote negative emotions such as depression [32]. On the other hand, mentally active SB such as work-related tasks while sedentary or driving a car may prevent or delay the onset of depression by promoting the awareness of autonomy and achievement and social interactions [33]. In agreement with other health outcomes [15,16], there is accumulating evidence that suggests the existence of ‘paradoxical’ relationships between SB and depression which may be context-, domain-, and pattern-dependent. As such, lifestyle interventions should be carefully constructed, and personalized strategies may be warranted to address the impacts of SB on depression in adults.
Associations of SB with the symptoms of anxiety
A handful of studies have evaluated the associations of SB with anxiety in adults. The results of these studies were recently summarized in a systematic review and meta-analysis [34]. It was demonstrated that total SB correlated to the risk of anxiety in adults (OR = 1.42 (95% CI: 1.25, 1.61)). Importantly, the detrimental relationships observed were stronger for total sitting time as compared to TV watching (a common leisure SB) or screen time (OR = 1.61, 1.46, and 1.37, respectively) [34]. Adding to these findings, the present study detected significant linear and deleterious correlations only between total and leisure SB with the symptoms of anxiety in Saudi adults. When the pattern (i.e., weekdays vs. weekend days) of SB was taken into consideration, total SB on weekend days and leisure SB both during weekdays and on weekend days were adversely associated with the anxiety symptoms. In contrast to depression, the accrued evidence does not support the existence of the ‘paradoxical’ relationships between SB and anxiety in adults. Instead, SB generally appears to have unfavorable associations with anxiety. Therefore, lifestyle interventions to reduce anxiety in adults should target all forms of SB, but more attention should be given to total and leisure SB to maximize the benefits.
Associations of SB with symptoms of stress
A recent systematic review which included twenty-six studies also consolidated the literature on the correlations between SB (i.e., total SB, sitting time, TV watching, and computer use) and stress in American, European, Australian, or south Korean adults [35]. The best synthesized evidence suggested either insufficient evidence or strong evidence for no relationships between different SBs and indicators of stress [35]. In contrast, the current study observed significant associations of total and leisure SB with the symptoms of stress in Saudi adults. These correlations were stronger for leisure SB compared to total SB, particularly during weekdays.
The discrepancies between the present and previous investigations on the associations of SB with stress and its symptoms may be explained by the following: 1) differences in the instruments used to measure SB (e.g., single- or multiple-item questionnaires or accelerometers), 2) utilized stress indicators (e.g., single-, 21-, 51-item self-report tools or hair or salivary cortisol), or 3) samples characteristics (e.g., young or middle-age adults, only females or mix sexes) [35]. For example, studies that used a single-item instrument (e.g., the Short Version of International Physical Activity Questionnaire) likely underestimated SB compared to studies that employed objective tools (e.g., accelerometers) or a multiple-items instrument (e.g., the SBQ) [36] leading to underestimation of the associations between SB and stress. Likewise, whereas studies which utilized objective devices (e.g., accelerometer) captured overall SB [35,36], studies that used self-reported questionnaires (e.g., the SBQ) estimated only several types of SB [35,36], potentially contributing to different conclusions of the associations between SB and stress. Thus, further studies that examine the role of domain and pattern of SB with different stress indicators in a variety of populations while considering such limitations are warranted to acquire more thorough conclusions about the correlations between SB and stress in adults.
Associations of excessive total SB with depression, anxiety, and stress
Previous reports have revealed that the economic burden of excessive total SB (≥8 hours/day) on Finnish and Canadian economy to be 1.47 and 1.62 billion US dollars/year, respectively [37,38]. Of particular relevance, a recent systematic review and meta-analysis also found that individuals who accumulated ≥8 hours/day of total SB had a 20% higher risk of depression [13]. In line with these reports, the present study detected statistically significant differences in the symptoms of depression, anxiety, and stress when comparing Saudi adults who accumulated vs. did not accumulate ≥8 hours/day of total SB. Together, the existing evidence indicates the aggravated negative impacts of excessive total SB on the economy as well as physical and mental health [37–40]. Therefore, evidence-based interventions that aim at reducing excessive total SB are encouraged not only to preserve the economy, but also to protect adult physical and mental health.
Both mental disorders and SB are ubiquitous in Saudi Arabia [6,41]. As a result, advocates for developing best practices and public recommendations to combat mental disorders and SB have been growing [6,41,42]. Though much advancement regarding mental disorder has been engendered in Saudi Arabia, much work remains, particularly in terms of the associations of SB with mental disorders. To this end, the current study sheds light into this important perspective. Saudi adults who accumulate higher total and leisure SB may have higher symptoms of depression, anxiety, and stress. Yet, accumulating higher occupational or commuting SB may reduce the depressive symptoms. As such, these findings support governmental endeavors to decrease SB [41] and propose Saudi physiatrists, psychological researchers, and interventionists to target not only excessive total SB, but also total and domain-specific SB during the week and weekdays and on weekend days while using personalized strategies to improve mental health in Saudi adults.
The present study has several noteworthy strengths. It was the first investigation to assess the role of SB domain and pattern in the associations of SB with the symptoms of depression, anxiety, and stress in Saudi adults. Moreover, the present study provided novel evidence for the existence of the ‘paradoxical’ correlations between SB and depression. In addition, to maximize the reach to a variety of Saudi populations such as females and individuals from different regions of Saudi Arabia, the sample recruitment was performed by using the most common social media platforms in Saudi Arabia [20]. Hence, the results of this study are more generalizable to all Saudi adults.
Still, several limitations should be considered when interpreting the present results. Though the web-based research is valid, recommended, and has many advantages [43], it is also prone to a few disadvantages, including self-selection or response biases [44]. Thus, more robust methods for data collection are warranted. Furthermore, a self-report tool (i.e., the SBQ) was utilized in the current study to measure SB. Although such instruments capture in-depth details of SB that are usually challenging to obtain by objective instruments alone, it is also prone to systematic, random, or reporting errors that can result in underestimation of SB [45]. Future research should use both subjective and objective tools to draw more comprehensive conclusions. Additionally, the current version of the SBQ does not capture modern SB such as time spent using a smartphone for social media use or internet browsing. These types of SB have profound impacts on mental health [46]. Furthermore, the items utilized to estimate domain-specific SB could overlap. For example, sitting and talking on the phone or reading a book could be a large part of one's workday and/or leisure time. As such, future studies should consider developing new tools or updating the existing instruments to address such limitations. This study also did not measure or control for physical activity level, which is known to affect mental health disorders [47]. Adjusting for physical activity could have obscured or attenuated these associations. Lastly, even though this study revealed significant associations of SB with the symptoms of mental disorders, the calculated effect sizes (i.e., rB and d) suggested that these relationships were small to moderate (ranged from 0.00 to 0.15). In other words, SB may have limited effects on these mental disorders and may be less meaningful as compared to other risk factors such as physical activity and employment status [48].
The current study uniquely investigated the relationships between domain and pattern of SB with symptoms of mental health disorders in Saudi adults. Total and leisure SB was consistently found to be adversely associated with depressive, anxiety, and stress symptoms. Once the pattern (i.e., weekdays vs. weekend days) of SB was considered, occupational and commuting SB was found to be beneficially associated with depressive symptoms in Saudi adults. These results provide evidence for the existence of a ‘Sedentary Behavior Paradox’ regarding depression. As a result, physiatrists, researchers, and interventionists should bear in mind that all SBs are not created equal. Importantly, reducing excessive total SB (≥8 hours/day) may preserve Saudi economy as well as physical and mental health.
Acknowledgement: The author would like to thank Researchers Supporting Project Number (RSPD2023R587), King Saud University, Riyadh, Saudi Arabia.
Funding Statement: The author received no specific funding for this study.
Author Contributions: The author confirms contribution to the paper as follows: study conception and design: A.A.; data collection: A.A.; analysis and interpretation of results: A.A.; draft manuscript preparation: A.A. The author reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Data is available upon requesting.
Ethics Approval: The procedure of this study was reviewed and approved by Institutional Review Board at King Saud University (No. KSU-HE-23-075). Electronic consent was provided by all participants.
Conflicts of Interest: The author declares that he has no conflicts of interest to report regarding the present study.
References
1. Knudsen AK, Øverland S, Aakvaag HF, Harvey SB, Hotopf M, Mykletun A. Common mental disorders and disability pension award: Seven year follow-up of the HUSK study. J Psychosom Res. 2010;69(1):59–67. doi:https://doi.org/10.1016/j.jpsychores.2010.03.007. [Google Scholar] [PubMed] [CrossRef]
2. Black DW, Grant JE. DSM-5® guidebook: The essential companion to the diagnostic and statistical manual of mental disorders. The United States: American Psychiatric Pub; 2014. [Google Scholar]
3. Spitzer RL, Endicott J. Medical and mental disorder: Proposed definition and criteria. Ann Med Psychol. 2018;176(7):656–65. doi:https://doi.org/10.1016/j.amp.2018.07.004. [Google Scholar] [CrossRef]
4. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–41. doi:https://doi.org/10.1001/jamapsychiatry.2014.2502. [Google Scholar] [PubMed] [CrossRef]
5. Bloom DE, Cafiero E, Jané-Llopis E, Abrahams-Gessel S, Bloom LR, et al. The global economic burden of noncommunicable diseases. PGDA Working Papers 8712. Program Glob Demogr Aging. 2012. [Google Scholar]
6. Al-Subaie AS, Al-Habeeb A, Altwaijri YA. Overview of the Saudi national mental health survey. Int J Methods Psychiatr Res. 2020;29(3):e1835. doi:https://doi.org/10.1002/mpr.1835. [Google Scholar] [PubMed] [CrossRef]
7. Alattar N, Felton A, Stickley T. Mental health and stigma in Saudi Arabia: A scoping review. Ment Health Rev. 2021;26(2):180–96. doi:https://doi.org/10.1108/MHRJ-08-2020-0055. [Google Scholar] [CrossRef]
8. Qureshi NA, Al-Habeeb AA, Koenig HG. Mental health system in Saudi Arabia: An overview. Neuropsychiatr Dis Treat. 2013:1121–35. doi:https://doi.org/10.2147/NDT.S48782. [Google Scholar] [PubMed] [CrossRef]
9. Alangari AS, Knox SS, Kristjansson AL, Wen S, Innes KE, Bilal L, et al. Barriers to mental health treatment in the Saudi National Mental Health Survey. Int J Environ Res Public Health. 2020;17(11):3877. doi:https://doi.org/10.3390/ijerph17113877. [Google Scholar] [PubMed] [CrossRef]
10. Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary behavior research network (SBRN)–terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1):1–17. doi:https://doi.org/10.1186/s12966-017-0525-8. [Google Scholar] [PubMed] [CrossRef]
11. Rodriguez-Ayllon M, Estévez-López F, Cadenas-Sanchez C, Gracia-Marco L, Lubans DR, Ortega FB, et al. Physical activity, sedentary behaviour and mental health in young people: A review of reviews. Adolesc Health Wellbeing Curr Strategies Future Trends Germany. 2019;35–73. doi:https://doi.org/10.1007/978-3-030-25816-0. [Google Scholar] [CrossRef]
12. Ekelund U, Brown WJ, Steene-Johannessen J, Fagerland MW, Owen N, Powell KE, et al. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. 2019;53(14):886–94. doi:https://doi.org/10.1136/bjsports-2017-098963. [Google Scholar] [PubMed] [CrossRef]
13. Zhou Q, Guo C, Yang X, He N. Dose-response association of total sedentary behaviour and television watching with risk of depression in adults: A systematic review and meta-analysis. J Affect Disord. 2023;324:652–659. doi:https://doi.org/10.1016/j.jad.2022.12.098. [Google Scholar] [PubMed] [CrossRef]
14. Holtermann A, Krause N, van der Beek AJ, Straker L. The physical activity paradox: Six reasons why occupational physical activity (OPA) does not confer the cardiovascular health benefits that leisure time physical activity does. Br J Sports Med. 2017;52(3):1–2. doi:https://doi.org/10.1136/bjsports-2017-097965. [Google Scholar] [PubMed] [CrossRef]
15. Alansare AB, Gibbs BB, Catov JM, Jennings JR, Kline CE, Nagle E, et al. Association of physical activity and sedentary time with cardio-autonomic regulation in women. J Womens Health. 2022;31(4):600–8. doi:https://doi.org/10.1089/jwh.2021.0243. [Google Scholar] [PubMed] [CrossRef]
16. Alansare AB, Paley JL, Quinn TD, Gibbs BB. Paradoxical associations of occupational and non-occupational sedentary behavior with cardiovascular disease risk measures in desk workers. J Occup Environ Med. 2023;65(7):e506–13. doi:https://doi.org/10.1097/JOM.0000000000002873. [Google Scholar] [PubMed] [CrossRef]
17. Hallgren M, Owen N, Vancampfort D, Nguyen TT, Dunstan DW, Wallin P, et al. Associations of sedentary behavior in leisure and occupational contexts with symptoms of depression and anxiety. Prev Med. 2020;133(2):106021. doi:https://doi.org/10.1016/j.ypmed.2020.106021. [Google Scholar] [PubMed] [CrossRef]
18. Patel SS, Webster RK, Greenberg N, Weston D, Brooks SK. Research fatigue in COVID-19 pandemic and post-disaster research: Causes, consequences and recommendations. Disaster Prev Manage. 2020;29(4):445–55. doi:https://doi.org/10.1108/DPM-05-2020-0164. [Google Scholar] [PubMed] [CrossRef]
19. Arpaci I, Karataş K, Baloğlu M. The development and initial tests for the psychometric properties of the COVID-19 Phobia Scale (C19P-S). Pers Individ Differ. 2020;164(6):110108. doi:https://doi.org/10.1016/j.paid.2020.110108. [Google Scholar] [PubMed] [CrossRef]
20. Alkhaldi R, Alsaffar D, Alkhaldi T, Sari Al B, Almaymuni H, Alnaim N, et al. Sentiment analysis for cruises in Saudi Arabia on social media platforms using machine learning algorithms. J Big Data. 2022;9(1):1–28. doi:https://doi.org/10.1186/s40537-022-00568-5. [Google Scholar] [PubMed] [CrossRef]
21. Rosenberg DE, Norman GJ, Wagner N, Patrick K, Calfas KJ, Sallis JF. Reliability and validity of the sedentary behavior questionnaire (SBQ) for adults. J Phys Act Health. 2010;7(6):697–705. doi:https://doi.org/10.1123/jpah.7.6.697. [Google Scholar] [PubMed] [CrossRef]
22. Alahmadi MA, Almasoud KH, Aljahani AH, Alzaman NS, Nozha OMA, Alahmadi OM, et al. Validity and reliability of the Arabic sedentary behavior questionnaire among university students aged between 18–30 years old. BMC Public Health. 2023;23(1):1–11. doi:https://doi.org/10.1186/s12889-023-15030-1. [Google Scholar] [PubMed] [CrossRef]
23. Bakker EA, Hopman MT, Lee DC, Verbeek AL, Thijssen DH, Eijsvogels TM. Correlates of total and domain-specific sedentary behavior: A cross-sectional study in dutch adults. BMC Public Health. 2020;20(1):1–10. doi:https://doi.org/10.1186/s12889-020-8316-6. [Google Scholar] [PubMed] [CrossRef]
24. Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. Australia: Sydney Psychology Foundation; 1995. [Google Scholar]
25. Ali AM, Ahmed A, Sharaf A, Kawakami N, Abdeldayem SM, Green J. The Arabic version of the depression anxiety stress Scale-21: Cumulative scaling and discriminant-validation testing. Asian J Psychiatr. 2017;30(6):56–8. doi:https://doi.org/10.1016/j.ajp.2017.07.018. [Google Scholar] [PubMed] [CrossRef]
26. Osman A, Wong JL, Bagge CL, Freedenthal S, Gutierrez PM, Lozano G. The Depression Anxiety Stress Scales-21 (DASS-21Further examination of dimensions, scale reliability, and correlates. J Clin Psychol. 2012;68(12):1322–38. doi:https://doi.org/10.1002/jclp.21908. [Google Scholar] [PubMed] [CrossRef]
27. Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol Assess. 1998;10(2):176–81. doi:https://doi.org/10.1037/1040-3590.10.2.176. [Google Scholar] [CrossRef]
28. Kwak SK, Kim JH. Statistical data preparation: management of missing values and outliers. Korean J Anesthesiol. 2017;70(4):407–11. doi:https://doi.org/10.4097/kjae.2017.70.4.407. [Google Scholar] [PubMed] [CrossRef]
29. Saunders TJ, McIsaac T, Douillette K, Gaulton N, Hunter S, Rhodes RE, et al. Sedentary behaviour and health in adults: An overview of systematic reviews. Appl Physiol Nutr Metab. 2020;45(10):S197–S217. doi:https://doi.org/10.1139/apnm-2020-0272. [Google Scholar] [PubMed] [CrossRef]
30. Hallgren M, Owen N, Stubbs B, Nguyen TTD, Vancampfort D, Lundin A, et al. Cross-sectional and prospective relationships of passive and mentally active sedentary behaviours and physical activity with depression. BJPsych. 2020;217(2):413–19. doi:https://doi.org/10.1192/bjp.2019.60. [Google Scholar] [PubMed] [CrossRef]
31. Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. J Psychiatr Res. 2016;77(5):42–51. doi:https://doi.org/10.1016/j.jpsychires.2016.02.023. [Google Scholar] [PubMed] [CrossRef]
32. Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychol Aging. 2006;21(1):140–51. doi:https://doi.org/10.1037/0882-7974.21.1.140. [Google Scholar] [PubMed] [CrossRef]
33. Hallgren M, Dunstan DW, Owen N. Passive versus mentally active sedentary behaviors and depression. Exerc Sport Sci Rev. 2020;48(1):20–7. doi:https://doi.org/10.1249/JES.0000000000000211. [Google Scholar] [PubMed] [CrossRef]
34. Allen MS, Walter EE, Swann C. Sedentary behaviour and risk of anxiety: A systematic review and meta-analysis. J Affect Disord. 2019;242(5):5–13. doi:https://doi.org/10.1016/j.jad.2018.08.081. [Google Scholar] [PubMed] [CrossRef]
35. Teychenne M, Stephens LD, Costigan SA, Olstad DL, Stubbs B, Turner AI. The association between sedentary behaviour and indicators of stress: A systematic review. BMC Public Health. 2019;19(1):1–15. doi:https://doi.org/10.1186/s12889-019-7717-x. [Google Scholar] [PubMed] [CrossRef]
36. Prince SA, Cardilli L, Reed JL, Saunders TJ, Kite C, Douillette K, et al. A comparison of self-reported and device measured sedentary behaviour in adults: A systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2020;17:1–17. doi:https://doi.org/10.1186/s12966-020-00938-3. [Google Scholar] [PubMed] [CrossRef]
37. Kolu P, Kari JT, Raitanen J, Sievänen H, Tokola K, Havas E, et al. Economic burden of low physical activity and high sedentary behaviour in Finland. J Epidemiol Community Health. 2022;76(7):677–84. doi:https://doi.org/10.1136/jech-2021-217998. [Google Scholar] [PubMed] [CrossRef]
38. Chaput JP, Janssen I, Lang JJ, Sampasa-Kanyinga H. Economic burden of excessive sedentary behaviour in Canada. Can J Public Health. 2023;114(2):165–74. doi:https://doi.org/10.17269/s41997-022-00729-2. [Google Scholar] [PubMed] [CrossRef]
39. Li S, Lear SA, Rangarajan S, Hu B, Yin L, Bangdiwala SI, et al. Association of sitting time with mortality and cardiovascular events in high-income, middle-income, and low-income countries. JAMA Cardiol. 2022;7(8):796–807. doi:https://doi.org/10.1001/jamacardio.2022.1581. [Google Scholar] [PubMed] [CrossRef]
40. Joundi RA, Patten SB, Williams JV, Smith EE. Association between excess leisure sedentary time and risk of stroke in young individuals. Stroke. 2021;52(11):3562–68. doi:https://doi.org/10.1161/STROKEAHA.121.034985. [Google Scholar] [PubMed] [CrossRef]
41. Alfawaz RA, Aljuraiban GS, AlMarzooqi MA, Alghannam AF, BaHammam AS, Dobia AM, et al. The recommended amount of physical activity, sedentary behavior, and sleep duration for healthy Saudis: A joint consensus statement of the Saudi Public Health Authority. Ann Thorac Med. 2021;16(3):239–44. doi:https://doi.org/10.4103/atm.atm_33_21. [Google Scholar] [PubMed] [CrossRef]
42. Koenig HG, Al Zaben F, Sehlo MG, Khalifa DA, Al Ahwal MS, Qureshi NA, et al. Mental health care in Saudi Arabia: Past, present and future. OJPsych. 2014;4(2):45045. doi:https://doi.org/10.4236/ojpsych.2014.42016. [Google Scholar] [CrossRef]
43. Ramsey SR, Thompson KL, McKenzie M, Rosenbaum A. Psychological research in the internet age: The quality of web-based data. Comput Hum Behav. 2016;58(2):354–60. doi:https://doi.org/10.1016/j.chb.2015.12.049. [Google Scholar] [CrossRef]
44. Andrade C. The limitations of online surveys. Indian J Psychol Med. 2020;42(6):575–76. doi:https://doi.org/10.1177/0253717620957496. [Google Scholar] [PubMed] [CrossRef]
45. Healy GN, Clark BK, Winkler EA, Gardiner PA, Brown WJ, Matthews CE. Measurement of adults’ sedentary time in population-based studies. Am J Prev Med. 2011;41(2):216–27. doi:https://doi.org/10.1016/j.amepre.2011.05.005. [Google Scholar] [PubMed] [CrossRef]
46. Abi-Jaoude E, Naylor KT, Pignatiello A. Smartphones, social media use and youth mental health. Can Med Assoc J. 2020;192(6):E136–41. doi:https://doi.org/10.1503/cmaj.190434. [Google Scholar] [PubMed] [CrossRef]
47. Kandola A, Ashdown-Franks G, Hendrikse J, Sabiston CM, Stubbs B. Physical activity and depression: Towards understanding the antidepressant mechanisms of physical activity. Neurosci Biobehav Rev. 2019;107(4):525–39. doi:https://doi.org/10.1016/j.neubiorev.2019.09.040. [Google Scholar] [PubMed] [CrossRef]
48. Shim R, Koplan C, Langheim FJ, Manseau MW, Powers RA, Compton MT. The social determinants of mental health: An overview and call to action. Psychiatr Ann. 2014;44(1):22–6. doi:https://doi.org/10.3928/00485713-20140108-04. [Google Scholar] [CrossRef]
Supplementary Materials
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools