 Open Access
Open Access
ARTICLE
Associations of Physical Activity and Sedentary Behavior with Internalizing Problems among Youth with Chronic Pain
1 Department of Physical Education, Inner Mongolia Normal University, Hohhot, 010022, China
2 Body-Brain-Mind Laboratory, School of Psychology, Shenzhen University, Shenzhen, 518060, China
3 Department of Physical Education, Shanghai Jiao Tong University, Shanghai, 200240, China
4 Center for Epidemiological Research in Nutrition and Health, Department of Nutrition, School of Public Health, Universidade de São Paulo, São Paulo, 01246-904, Brazil
5 Research Group Degenerative and Chronic Diseases, Movement, Faculty of Health Sciences, University of Potsdam, Potsdam, 14476, Germany
6 Health and Rehabilitation Sciences, Health Sciences University, Bournemouth, BH5 2DF, UK
7 Department of Psychiatry, University of Oxford, Oxford, OX3 7JX, UK
* Corresponding Author: Yanxia Chen. Email:
(This article belongs to the Special Issue: Enhancing Mental Health through Physical Activity: Exploring Resilience Across Populations and Life Stages)
International Journal of Mental Health Promotion 2025, 27(2), 97-110. https://doi.org/10.32604/ijmhp.2025.061237
Received 20 November 2024; Accepted 16 January 2025; Issue published 03 March 2025
Abstract
Background: Taking actions to maintain a healthy lifestyle, including regular engagement in physical activity (PA) and reducing sedentary behavior (SB), may protect against the development of internalizing problems among healthy youth. However, it remains unclear whether such associations exist among youth with chronic pain who often report symptoms of depression and anxiety. To this end, we aimed to investigate the associations between independent and combined PA and/or SB patterns with indicators of internalizing problems in this vulnerable population. Methods: Data used in this cross-sectional study were retrieved from the U.S. National Survey of Children’s Health for the years 2021–2022. Specifically, caregiver proxy reports on sociodemgraphic factors and lifestyle behaviors of 4735 U.S. children and adolescents (referring to youth) aged 6–17 years were collected. We examined independent and combined patterns of PA and SB as exposures, with internalizing problems serving as outcomes of interest. Logistic regressions were used to examine the independent and combined associations of PA and/or SB patterns with anxiety and depression symptoms among youth with chronic pain while adjusting for covariates including age, sex, ethnicity, primary caregivers’ education level, overweight status, and household federal poverty level. Results: Overall, our results indicated that PA was negatively associated with anxiety and depressive symptoms. Specifically, youth with chronic pain who engaged in at least 60–minute PA for 1–3 days, 4–6 days, or every day reported significantly lower likelihood of experiencing symptoms of anxiety (OR = 0.71, 95% CI: 0.60–0.84; OR = 0.44, 95% CI: 0.36–0.53; OR = 0.50, 95% CI: 0.40–0.63, respectively; all p-value < 0.001) and depression (OR = 0.63, 95% CI: 0.53–0.75; OR = 0.38, 95% CI: 0.31–0.47; OR = 0.46, 95% CI: 0.36–0.59, respectively; all p-value < 0.001) symptoms compared to those with 0 days. Conversely, SB (operationalized via the proxy screen time) was positively associated with anxiety and depression symptoms. Youth with chronic pain who reported 4 or more hours of daily screen time had significantly higher odds of experiencing symptoms of anxiety (OR = 2.17, 95% CI: 1.52–3.09, p < 0.001) and depression (OR = 2.30, 95% CI: 1.48–3.59, p < 0.001). Furthermore, youth with chronic pain who engaged in higher PA levels and reported lower SB levels had a lower likelihood of experiencing symptoms of anxiety (OR = 0.68, 95% CI: 0.52–0.87, p = 0.003) and depression (OR = 0.49, 95% CI: 0.34–0.70, p < 0.001) symptoms compared to those with lower PA levels and higher SB levels. Conclusions: Higher PA levels and lower SB levels were associated with a reduced likelihood of developing anxiety and depression symptoms, which are indicative of internalizing problems, among youth with chronic pain. Future public health actions in this vulnerable population should prioritize intervention programs that promote PA engagement to reduce SB levels.Keywords
Chronic pain is defined as an ongoing unpleasant sensory and emotional experience lasting 3 months or more months, typically associated with or caused by muscle-related injuries [1,2]. Chronic pain such as back pain and headache, is a common health condition among various age groups, including but not limited to children and adolescents (referred to in the rest of this manuscript as “youth”) which affects physical, psychological, and social function [3–5]. It is estimated that worldwide ~21% of youth experience chronic pain, with headache and musculoskeletal (e.g., back or body) pain accounting for most cases [6]. Furthermore, accumulating evidence suggests that in youth anxiety and depressive symptoms (commonly referred to as internalizing problems), often occur concomitantly with chronic pain [7].
Such comorbidities or co-existing health issues may be linked to an increased likelihood of functional limitations in daily life [8]. Previous studies have shown that youth with chronic pain are more susceptible to developing internalizing problems [9], and these issues may persist into adulthood if left untreated [10]. A recent seminal meta-analytical review containing 79 studies (pooled sample size = 12,614 youth with chronic pain) indicated that the overall prevalence of anxiety and depression had reached ~35% and ~12%, respectively [11]. Furthermore, youth with chronic pain were observed to be 3 times more likely to report anxiety and depressive symptoms relative to healthy controls [11]. Against this background, it is critical to deepen an understanding of the factors that influence internalizing problems in this vulnerable population, especially concerning the role of modifiable lifestyle factors such as physical activity (PA) and sedentary behaviors (SB) [12].
Regular engagement in PA may have the potential to protect against the development of anxiety and depressive symptoms in youth [13–17]. For example, a meta-analysis conducted by Schuch and colleagues including 49 prospective studies (N = 266,939) indicated that higher levels of PA can protect against the development of depression in youths (adjusted OR = 0.90) [18]. Furthermore, recent reviews also provide evidence that PA intervention programs as an alternative or adjunct treatment for anxiety and depressive symptoms can effectively alleviate internalizing problems in youths [16,19,20]. In contrast, SB is defined as any waking behaviors (e.g., sitting, reclining, or lying posture) with an energy expenditure that has reached at least 1.5 metabolic equivalents [21] and has attracted great attention from the research community due to its close relation to a variety of health outcomes including indicators of internalizing problems [22–26]. Previous studies in youth showed negative associations of SB (indicated by proxy via screen-based activities) with indicators of internalizing problems (e.g., increased risk of developing anxiety and depressive symptoms) [27–30]. Notably, the associations of PA and/or screen-based SB with indicators of internalizing problems have rarely been investigated among youth with chronic pain.
The findings of a previous study suggest that individuals with knee osteoarthritis (noted musculoskeletal disorder) were more likely to report catastrophizing thinking which increased the likelihood of physical inactivity and SB [31]. Thus, chronic pain, to some extent, seems to be more likely to limit PA engagement [32], and this may exacerbate anxiety and depressive symptoms in youth [33,34]. PA and SB are two independent but interrelated lifestyle behaviors [35]. However, there is limited evidence regarding how PA and SB jointly contribute to internalizing problems in youth with chronic pain. Such an outstanding research question may preclude researchers and health professionals from making nuanced and evidence-based recommendations for this vulnerable population concerning the potential benefits of PA for mental health. To address this research gap, it is essential to investigate the associations of PA and SB with indicators of internalizing problems among youth with chronic pain. Thus, this study aimed to investigate the associations of PA and SB with depression and anxiety among youth with chronic pain. Given that accumulating evidence indicates the beneficial association of PA with depression and/or anxiety among youth with different health conditions [36], while its associations with SB are less clear due to mixed findings in previous studies, we investigated both associations between independent and combined PA and SB patterns with indicators of internalizing problems among youth with chronic pain.
2.1 Study Design and Participants
Similar to previous research [12], in this cross-sectional study, publicly accessible data from the 2021–2022 National Survey of Children’s Health (NSCH) (https://www.childhealthdata.org/) (accessed on 15 January 2025) was used. The original data was collected using web- or paper-based surveys querying parents or primary caregivers of children aged between 0–17 years who were randomly selected from households across all 50 U.S. states and the District of Columbia between 2021 and 2022. A total of 104,995 complete responses were received in the NSCH survey. Ethical approval for this survey was granted by the U.S. Department of Health and Human Services.
Considering that caregivers of children aged 0–5 years were not surveyed about school safety and related outcomes, this analysis focuses on children and adolescents aged 6–17 years who experience chronic pain. The eligibility of children and adolescents was determined via the following single-item question responded to by either a parent or primary caregiver: “Does this child have any repeated or chronic pain, including headaches or other back or body pain?”, with a binary response (Yes vs. No). Only children and adolescents for whom their parents or primary caregivers responded with “yes” were deemed eligible for inclusion in this study.
2.2.1 Assessment of Movement Behaviors
Consistent with previous research [37], PA and SB were assessed via self-reports. More specifically, PA was assessed by querying the parents or primary caregivers with the following question: “During the past week, on how many days did this child exercise, play a sport, or participate in physical activity for at least 60 minute?” This single-item question was answered with 4 options (e.g., 0 days, 1–3 days, 4–6 days, or every day). SB was assessed using the following question: “On most weekdays, about how much time did this child usually spend in front of a TV, computer, cell phone, or other electronic device watching programs, playing video games, accessing the internet, or using social media, not including schoolwork?” Response options were less than 1 h a day, 1 h a day, 2 h a day, 3 h a day, and 4 or more hours a day.
As per PA and SB guidelines, only youth who were physically active every day of the week were classified as being “active” (being coded as 1 vs. 0 = failed to meet PA guidelines) [38]. Less than 1 h a day, 1 h a day and 2 h a day were considered “sedentary” (coded as 1 vs. 0 = failed to meet SB guidelines) [39]. Youth who met the combined PA + SB guidelines were coded as 1 (vs. 0 = failed to meet the combined guidelines) [38].
2.2.2 Assessment of Internalizing Problems
As in previous studies [39,40], depressive symptoms were assessed by the following question: “Has a doctor or other healthcare provider ever told you that your child has depression?” Answers included: 1 (do not have the condition), 2 (ever told, but no current condition), and 3 (currently have the condition). For our analysis, depression was coded as 1 when the parents or primary caregivers responded that their child “currently has the condition”. Anxiety was assessed by asking parents: “Has a doctor or other healthcare provider ever told you that your child has anxiety problems?” Answers included: 1 (do not have the condition), 2 (ever told, but no current condition), and 3 (currently have the condition). Anxiety was coded as 1 when a response was “currently has the condition”. Higher scores reflect greater levels of anxiety and/or depression, respectively.
Based on a previous study [40], we considered age (younger group = 6–13 years old vs. Older group = 14–17 years old), sex (male vs. female), ethnicity (Hispanic, white, black, Asian, and other/multi-racial), education level of primary caregivers (less than high school, high school degree or General Educational Development (GED), some college or technical school, and college degree or higher), overweight status (yes vs. no), and household federal poverty level (FPL) (0%–199% FPF, 200%–299% FPL, 300%–399% FPL, and 400% FPL or greater) as covariates.
The statistical analysis was performed using Stata software (StataCorp (2017). Stata Statistical Software: Release 15. StataCorp LLC, 2017). Regarding descriptive statistics, categorical variables were provided as percentages, while continuous variables were provided as means with standard deviations (SDs). Logistic regression models were used to assess the relationships between movement behaviors (PA and/or SB) and internalizing problems (i.e., depression and anxiety), adjusting for age, sex, ethnicity, primary caregivers’ education level, overweight status, and household FPL. A p-value of less than 0.05 was considered statistically significant.
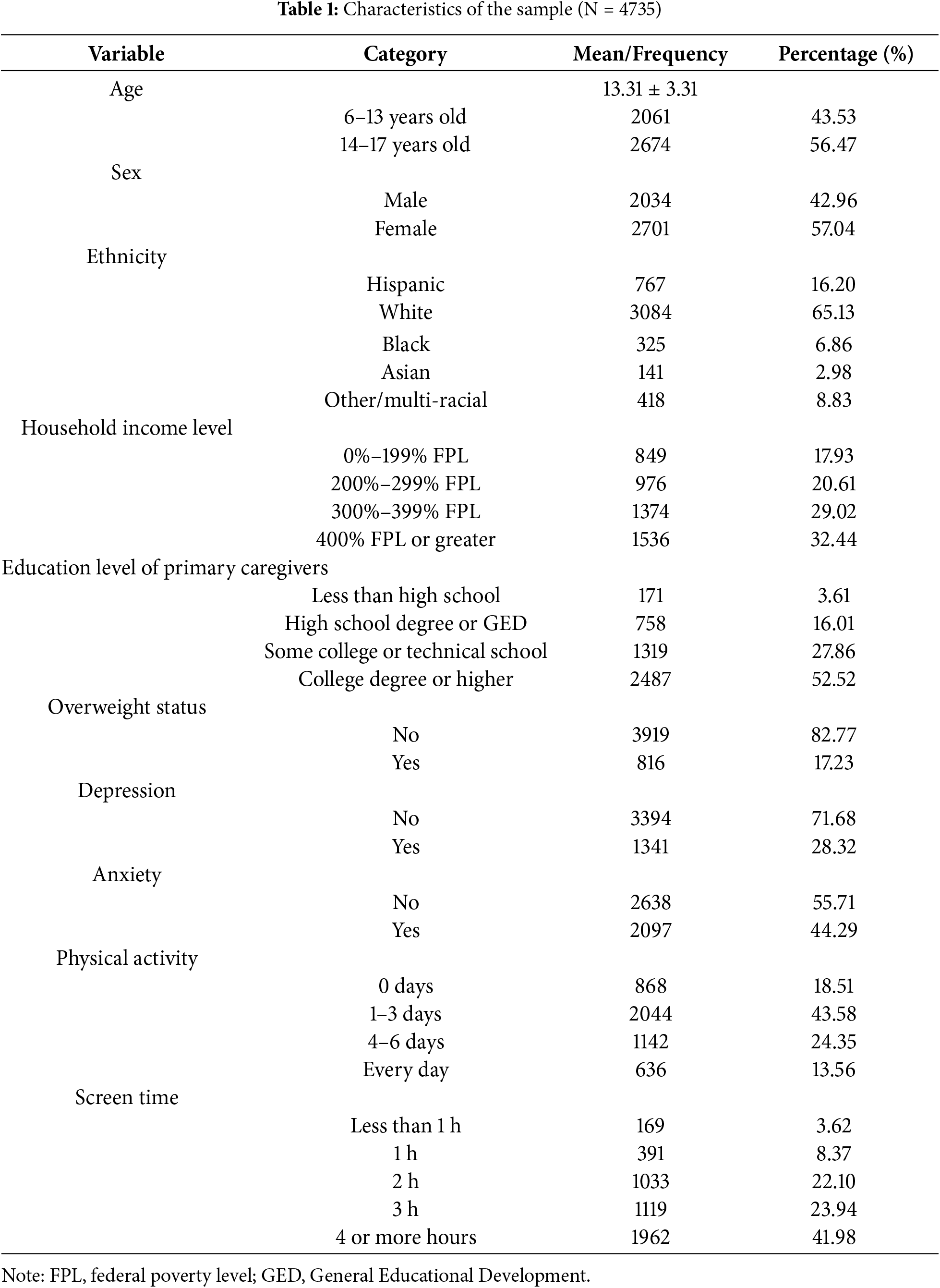
Table 1 presents the descriptive characteristics of the sample. This study included 4735 youth who have chronic pain with a mean age of 13.31 (±3.31) years. Among these participants, 42.96% were male. The majority of the sample were White (65.13%) and reported a household income level of 400% FPL or greater (32.44%). Additionally, more than half of the primary caregivers had a college degree or higher education level (52.52%). Around one-fifth (17.23%) of youth were categorized as overweight. In terms of mental health, 28.32% of youth reported symptoms of depression, and 44.29% were reported to have anxiety. PA levels varied with 18.51% of the sample did not engage in PA, whereas 13.56% engaged in PA every day. Screen time as a proxy of SB was high in this cohort, with 41.98% of participants spending four or more hours on screen time per day.
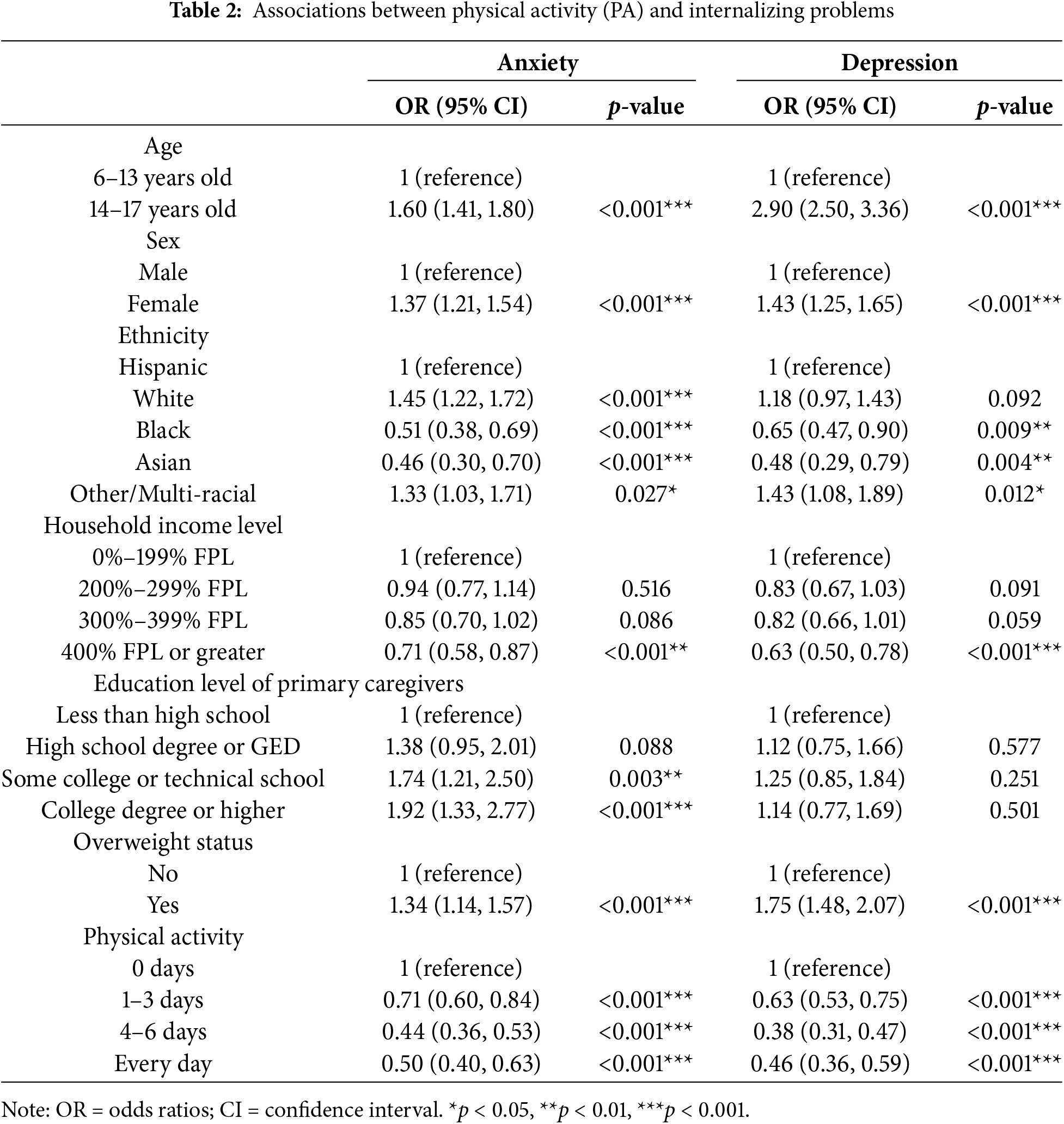
3.1 Associations between Physical Activity and Internalizing Problems
As shown in Table 2, negative associations between PA and internalizing problems are observed (all OR < 1). Compared with youth who did not engage in PA, those who engaged in at least 60-minute PA for 1–3 days, 4–6 days, or every day had a significantly lower likelihood of experiencing symptoms of anxiety (OR = 0.71, 95% CI: 0.60–0.84; OR = 0.44, 95% CI: 0.36–0.53; OR = 0.50, 95% CI: 0.40–0.63, respectively; all p-value < 0.001). Additionally, youth who engaged in at least 60-minute PA on 1–3 days, 4–6 days, or every day showed a significantly lower likelihood of reporting symptoms of depression (OR = 0.63, 95% CI: 0.53–0.75; OR = 0.38, 95% CI: 0.31–0.47; OR = 0.46, 95% CI: 0.36–0.59, respectively; all p-value < 0.001).
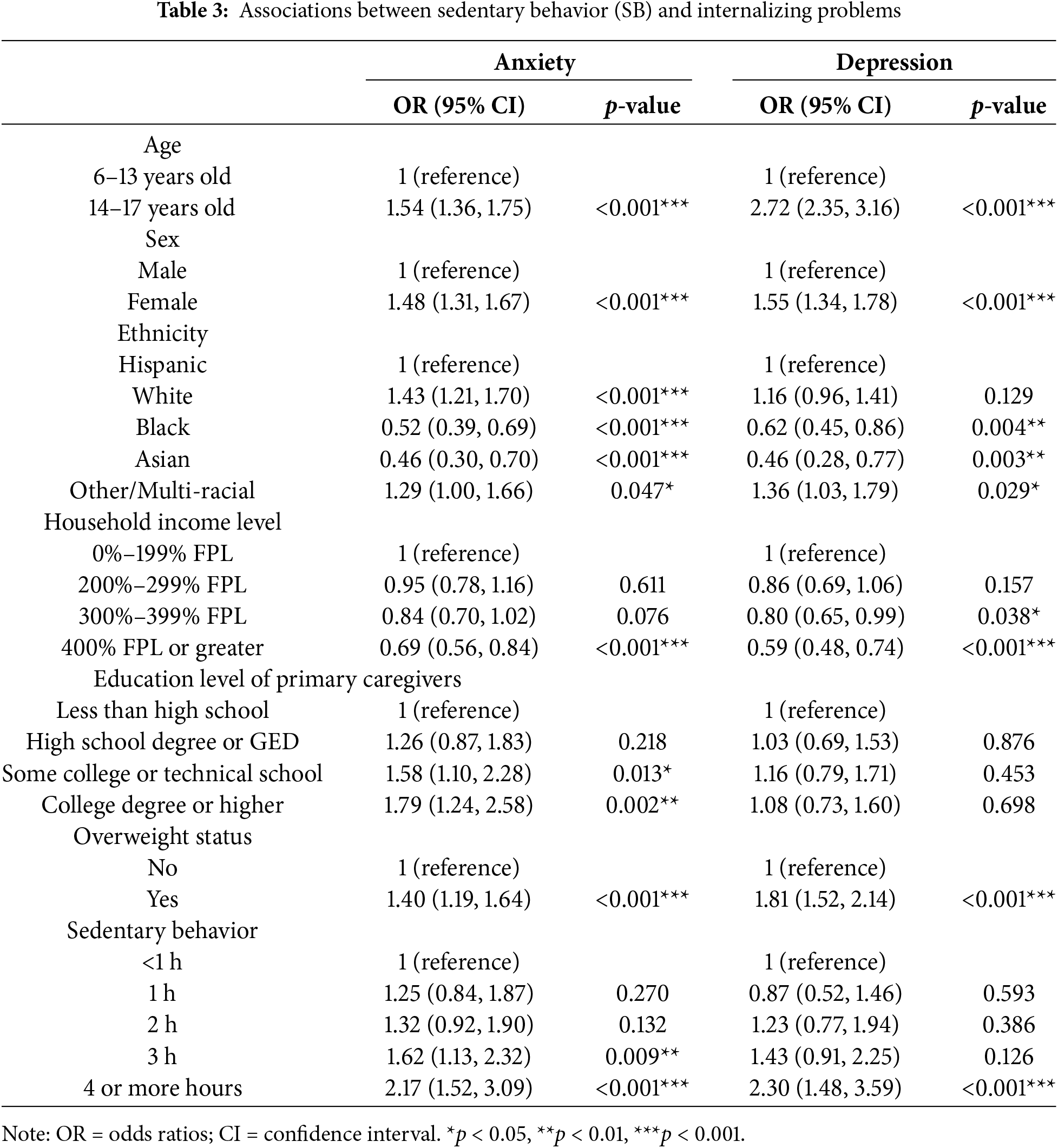
3.2 Associations between Sedentary Behavior and Internalizing Problems
Positive associations between SB and internalizing problems were observed (see Table 3). Youth who spend four or more hours on screen time per day had a significantly higher likelihood of experiencing anxiety (OR = 2.17, 95% CI: 1.52–3.09, p < 0.001) and depressive symptoms (OR = 2.30, 95% CI: 1.48–3.59, p < 0.001) compared to those with less than one hour of screen time. Additionally, youth who spend three hours on screen time had a higher likelihood of reporting anxiety (OR = 1.62, 95% CI: 1.13–2.32, p = 0.009).
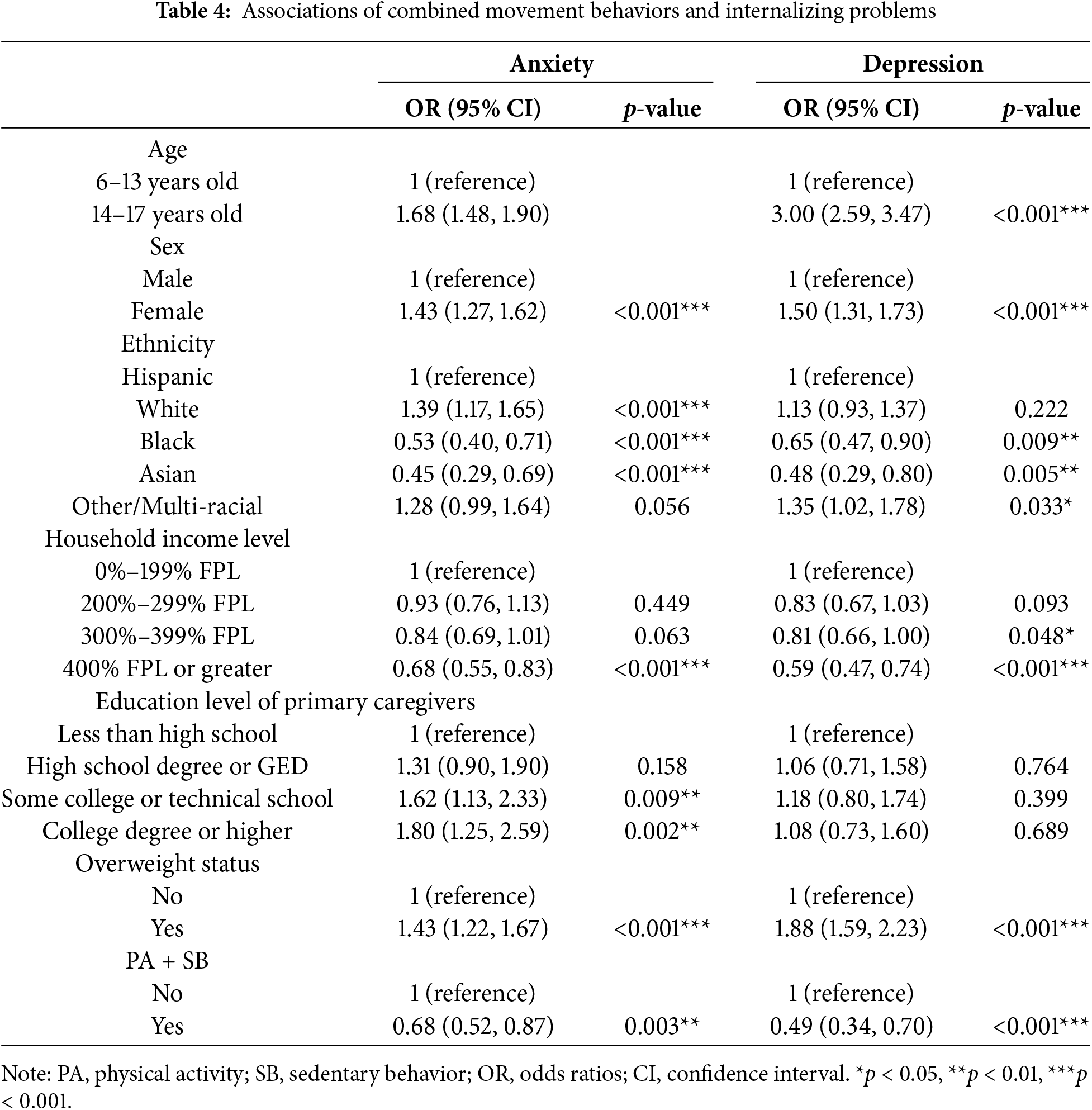
3.3 Associations of Combined Movement Behaviors and Internalizing Problems
Results for the associations between meeting PA + SB guidelines and internalizing problems are presented in Table 4. Youth who met the combined PA + SB guidelines had significantly lower odds of experiencing anxiety and depressive symptoms relative to those youth who did not meet the combined guidelines. Specifically, youth who met the PA + SB guidelines had 32% lower likelihood of reporting anxiety (OR = 0.68, 95% CI: 0.52–0.87, p = 0.003) and a 51% lower likelihood of reporting depressive symptoms (OR = 0.49, 95% CI: 0.34–0.70, p < 0.001) as compared to those who did not meet the combined recommendations on PA and SB.
The present study investigated the independent and combined associations of PA and/or SB with internalizing problems (i.e., depressive symptoms and anxiety) among youth with chronic pain. Our findings provide evidence that both more time spent on PA and less time spent on SB are associated with a lower likelihood of reporting symptoms of depression and anxiety in this vulnerable population.
In particular, our findings indicate that higher PA levels are associated with a reduced likelihood of reporting anxiety and depressive symptoms among youth with chronic pain. These findings align with previous research on children and adolescents suggesting that PA has a positive effect on internalizing problems [30,41]. More specifically, comparable to our study, PA was associated with a lower likelihood of developing symptoms of depression and anxiety, with stronger associations observed with higher PA [42]. These findings suggest a dose-response relationship in which higher PA may yield a greater mental health benefits. The positive effects of PA on mental health are likely to be mediated by complex neurobiological mechanisms [43] including but not limited to exercise-induced changes in endorphin release [44], the human dopaminergic system [45], peripheral brain-derived neurotrophic factor (BDNF) concentrations [46], and structural changes to brain regions associated with depression such as the hippocampus, and the prefrontal and anterior cingulate cortices [47]. Undertaking PA also offers opportunities for social interaction [48], which may serve as a protective factor against these mental health issues [48,49], especially in children and adolescents who are at a critical stage of social development [50,51]. Concerning SB, our results showing that more screen time (proxy of SB) is associated with a higher risk of developing symptoms of depression and anxiety. These findings align with those of previous studies that have reported prolonged screen time as a risk factor for internalizing problems in youth [13,52] potentially driven by mechanisms related to higher rates of inflammation [53] and a reduction in social interaction [54].
From an integrated perspective, youth with chronic pain who met the recommendations on PA + SB had a lower risk of experiencing depression and anxiety, suggesting an synergistic and positive effect. This aligns with findings from a previous study on youth with chronic pain, indicating that adherence to the combined (PA and SB) guidelines is associated with reduced severity of depressive symptoms [12]. Furthermore, our findings are partially supported by a previous meta-analysis [28] indicating that engaging in PA and reducing the time spent on SB may be beneficial for youth mental health. Collectively, our findings highlight the importance of addressing both movement behaviors in interventions aimed at improving mental health among youth with chronic pain. In particular, such interventions should not only target the PA promotion but also the reduction of time spent sedentary, particularly of screen-based SB which is prevalent in youth. Parents, caregivers, and schools can promote enjoyable (supportive) and convenient types of PA that accommodate the pain-related limitations of this vulnerable population. These strategies, in turn, may be effective in promoting overall mental health for youth with chronic pain.
Although the findings of this study add to the growing body of evidence documenting the positive influence of specific lifestyle patterns (i.e., high PA levels and low SB levels) on mental health in youth with chronic pain, it is important to acknowledge several limitations. Firstly, the cross-sectional design prevents testing whether the observed associations between these variables are causal. Thus, prospective and intervention studies are warranted to elucidate the underlying causal mechanisms of our observations. Second, the assessment of movement behaviors (e.g., PA and SB) relies on self-reported measures which could be influenced by recall bias and social desirability bias [55,56]. Thus, future studies should utilize objective assessment methods (e.g., accelerometers) to obtain more accurate data on PA and SB, thereby enhancing the reliability and robustness of the findings. Third, the survey did not consider the PA intensity that is differentially linked to mental health outcomes [57,58]. To address this limitation, future research should investigate whether the associations between PA and mental health among youth with chronic pain vary as a function of the PA intensity [59]. Fourth, although the NSCH survey question about chronic pain was specific to recurrent and chronic pain, the chronicity of pain was not evaluated, which requires further investigation with a longitudinal design. Fifth, the severity of symptoms of depression and anxiety was not assessed, which has precluded us from concluding whether youth with a specific severity level are more responsive to the influence of lifestyle behaviors (e.g., PA and SB), especially whether youth with higher levels of depression and anxiety benefit to a greater extent from a healthier lifestyle (e.g., more PA and less SB) [60,61].
Our findings suggest that higher PA levels and lower SB levels are protective factors against the development of anxiety and depressive symptoms (i.e., indicators of internalizing problems) among youth with chronic physical pain. However, future interventional studies are required to investigate whether increasing regular PA levels and reducing SB levels can reduce the prevalence of depressive symptoms and anxiety among this vulnerable population.
Acknowledgement: We thank the anonymous reviewers for their constructive feedback that greatly helped us improve the overall quality of this manuscript.
Funding Statement: This study was supported by Shenzhen Educational Research Funding (zdzb2014), Shenzhen Science and Technology Innovation Commission Foundation (202307313000096), Social Science Foundation from China’s Ministry of Education (23YJA880093), China Postdoctoral Science Foundation (2022M711174), National Center for Mental Health Foundation (Z014), Research Excellence Scholarships of Shenzhen University (ZYZD2305), Research Funding for Society of Sport Science (PT2023030), and Natural Science Foundation of Shenzhen University (000311).
Author Contributions: Lingling Yu: Writing—review & editing, Writing—original draft, Formal analysis, Conceptualization. Yanxia Chen: Writing—review & editing, Writing—original draft, Formal analysis. Jinming Li: Writing—review & editing. André O. Werneck: Writing—review & editing, Conceptualization. Fabian Herold: Writing—review & editing, Visualization, Validation. Alyx Taylor: Writing—review & editing, Visualization, Validation. Benjamin Tari: Writing—review & editing, Methodology, Conceptualization. Liye Zou: Writing—review & editing, Conceptualization. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data can be obtained through the website: https://www.childhealthdata.org/ (accessed on 15 January 2025).
Ethics Approval: Not applicable.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
References
1. Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976–82. doi:10.1097/j.pain.0000000000001939. [Google Scholar] [PubMed] [CrossRef]
2. Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019;160(1):19–27. doi:10.1097/j.pain.0000000000001384. [Google Scholar] [PubMed] [CrossRef]
3. Groenewald CB, Tham SW, Palermo TM. Impaired school functioning in children with chronic pain. Clin J Pain. 2020;36(9):693–9. doi:10.1097/ajp.0000000000000850. [Google Scholar] [PubMed] [CrossRef]
4. Forgeron PA, King S, Stinson JN, McGrath PJ, MacDonald AJ, Chambers CT. Social functioning and peer relationships in children and adolescents with chronic pain: a systematic review. Pain Res Manage. 2010;15(1):27–41. doi:10.1155/2010/820407. [Google Scholar] [PubMed] [CrossRef]
5. Wilson AC, Palermo TM. Physical activity and function in adolescents with chronic pain: a controlled study using actigraphy. J Pain. 2012;13(2):121–30. doi:10.1016/j.jpain.2011.08.008. [Google Scholar] [PubMed] [CrossRef]
6. Chambers CT, Dol J, Tutelman PR, Langley CL, Parker JA, Cormier BT, et al. The prevalence of chronic pain in children and adolescents: a systematic review update and meta-analysis. Pain. 2024;165(10):2215–34. doi:10.1097/j.pain.0000000000003267. [Google Scholar] [PubMed] [CrossRef]
7. Wrona SK, Melnyk BM, Hoying J. Chronic pain and mental health co-morbidity in adolescents: an urgent call for assessment and evidence-based intervention. Pain Manage Nurs. 2021;22(3):252–9. doi:10.1016/j.pmn.2020.12.004. [Google Scholar] [PubMed] [CrossRef]
8. Bateman S, Jordan A, Noel M, Loades M, Caes L. The impact of co-occurring chronic pain and mental health symptoms on adolescent functioning, a cross-sectional survey. BMC Psychol. 2024;12(1):629. doi:10.1186/s40359-024-02126-5. [Google Scholar] [PubMed] [CrossRef]
9. Falla K, Kuziek J, Mahnaz SR, Noel M, Ronksley PE, Orr SL. Anxiety and depressive symptoms and disorders in children and adolescents with migraine: a systematic review and meta-analysis. JAMA Pediatr. 2022;176(12):1176–87. doi:10.1001/jamapediatrics.2022.3940. [Google Scholar] [PubMed] [CrossRef]
10. Noel M, Groenewald CB, Beals-Erickson SE, Gebert JT, Palermo TM. Chronic pain in adolescence and internalizing mental health disorders. Pain. 2016;157(6):1333–8. doi:10.1097/j.pain.0000000000000522. [Google Scholar] [PubMed] [CrossRef]
11. Dudeney J, Aaron RV, Hathway T, Bhattiprolu K, Bisby MA, McGill LS, et al. Anxiety and depression in youth with chronic pain: a systematic review and meta-analysis. JAMA Pediatr. 2024;178(11):1114–23. doi:10.1001/jamapediatrics.2024.3039. [Google Scholar] [PubMed] [CrossRef]
12. Chen Y, Hou M, Herold F, Wang K, Werneck AO, Van Damme T, et al. Linking 24-hour movement behavior guidelines to academic engagement and social-emotional functioning among youth with chronic pain. Ment Health Phys Act. 2024;27:100614. doi:10.1016/j.mhpa.2024.100614. [Google Scholar] [CrossRef]
13. Zhang Y, Chen S, Wang C, Zhang X, Zou L, Chi X, et al. Does more sedentary time associate with higher risks for sleep disorder among adolescents? A pooled analysis. Front Pediatr. 2021;9:603177. doi:10.3389/fped.2021.603177. [Google Scholar] [PubMed] [CrossRef]
14. Taylor A, Kong C, Zhang Z, Herold F, Ludyga S, Healy S, et al. Associations of meeting 24-h movement behavior guidelines with cognitive difficulty and social relationships in children and adolescents with attention deficit/hyperactive disorder. Child Adolesc Psychiatry Ment Health. 2023;17(1):42. [Google Scholar] [PubMed]
15. Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R, et al. Association between physical activity and risk of depression: a systematic review and meta-analysis. JAMA Psychiatr. 2022;79(6):550–9. doi:10.1001/jamapsychiatry.2022.0609. [Google Scholar] [PubMed] [CrossRef]
16. Singh B, Olds T, Curtis R, Dumuid D, Virgara R, Watson A, et al. Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews. Br J Sports Med. 2023;57(18):1203–9. doi:10.1136/bjsports-2022-106195. [Google Scholar] [PubMed] [CrossRef]
17. Kandola A, Lewis G, Osborn DPJ, Stubbs B, Hayes JF. Device-measured sedentary behaviour and anxiety symptoms during adolescence: a 6-year prospective cohort study. Psychol Med. 2022;52(14):2962–71. doi:10.1017/s0033291720004948. [Google Scholar] [PubMed] [CrossRef]
18. Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatr. 2018;175(7):631–48. doi:10.1176/appi.ajp.2018.17111194. [Google Scholar] [PubMed] [CrossRef]
19. Li J, Zhou X, Huang Z, Shao T. Effect of exercise intervention on depression in children and adolescents: a systematic review and network meta-analysis. BMC Public Health. 2023;23(1):1918. doi:10.1186/s12889-023-16824-z. [Google Scholar] [PubMed] [CrossRef]
20. Yu Q, Wong KK, Lei OK, Nie J, Shi Q, Zou L, et al. Comparative effectiveness of multiple exercise interventions in the treatment of mental health disorders: a systematic review and network meta-analysis. Sports Med Open. 2022;8(1):135. doi:10.1186/s40798-022-00529-5. [Google Scholar] [PubMed] [CrossRef]
21. Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary Behavior Research Network (SBRN)—Terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1):75. doi:10.1186/s12966-017-0525-8. [Google Scholar] [PubMed] [CrossRef]
22. Hallgren M, Nguyen TT, Owen N, Vancampfort D, Dunstan DW, Wallin P, et al. Associations of sedentary behavior in leisure and occupational contexts with symptoms of depression and anxiety. Prev Med. 2020;133:106021. doi:10.1016/j.ypmed.2020.106021. [Google Scholar] [PubMed] [CrossRef]
23. Hallgren M, Dunstan DW, Owen N. Passive versus mentally active sedentary behaviors and depression. Exerc Sport Sci Rev. 2020;48(1):20–7. doi:10.1249/jes.0000000000000211. [Google Scholar] [PubMed] [CrossRef]
24. Ringin E, Dunstan DW, McIntyre RS, Owen N, Berk M, Rossell SL, et al. Differential associations of mentally-active and passive sedentary behaviours and physical activity with putative cognitive decline in healthy individuals and those with bipolar disorder: findings from the UK Biobank cohort. Ment Health Phys Act. 2023;24:100514. doi:10.1016/j.mhpa.2023.100514. [Google Scholar] [CrossRef]
25. Zou L, Herold F, Cheval B, Wheeler MJ, Pindus DM, Erickson KI, et al. Sedentary behavior and lifespan brain health. Trends Cogn Sci. 2024;28(4):369–82. doi:10.1016/j.tics.2024.02.003. [Google Scholar] [PubMed] [CrossRef]
26. Yu Q, Zhang Z, Ludyga S, Erickson KI, Cheval B, Hou M, et al. Effects of physical exercise breaks on executive function in a simulated classroom setting: uncovering a window into the brain. Adv Sci. 2024;12:1341. doi:10.1002/advs.202406631. [Google Scholar] [PubMed] [CrossRef]
27. Zhang J, Yang SX, Wang L, Han LH, Wu XY. The influence of sedentary behaviour on mental health among children and adolescents: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2022;306:90–114. doi:10.1016/j.jad.2022.03.018. [Google Scholar] [PubMed] [CrossRef]
28. Rodriguez-Ayllon M, Cadenas-Sánchez C, Estévez-López F, Muñoz NE, Mora-Gonzalez J, Migueles JH, et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med. 2019;49(9):1383–410. doi:10.1007/s40279-019-01099-5. [Google Scholar] [PubMed] [CrossRef]
29. Hayward J, Jacka FN, Skouteris H, Millar L, Strugnell C, Swinburn BA, et al. Lifestyle factors and adolescent depressive symptomatology: associations and effect sizes of diet, physical activity and sedentary behaviour. Aust N Z J Psychiat. 2016;50(11):1064–73. doi:10.1177/0004867416671596. [Google Scholar] [PubMed] [CrossRef]
30. Sampasa-Kanyinga H, Colman I, Goldfield GS, Janssen I, Wang J, Podinic I, et al. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: a systematic review. Int J Behav Nutr Phys Act. 2020;17(1):72. doi:10.1186/s12966-020-00976-x. [Google Scholar] [PubMed] [CrossRef]
31. Zhaoyang R, Martire LM, Darnall BD. Daily pain catastrophizing predicts less physical activity and more sedentary behavior in older adults with osteoarthritis. Pain. 2020;161(11):2603–10. doi:10.1097/j.pain.0000000000001959. [Google Scholar] [PubMed] [CrossRef]
32. Perruchoud C, Buchser E, Johanek LM, Aminian K, Paraschiv-Ionescu A, Taylor RS. Assessment of physical activity of patients with chronic pain. Neuromod: Technol Neural Interface. 2014;17(Suppl 1):42–7. doi:10.1111/ner.12036. [Google Scholar] [PubMed] [CrossRef]
33. Bélair M-A, Kohen DE, Kingsbury M, Colman I. Relationship between leisure time physical activity, sedentary behaviour and symptoms of depression and anxiety: evidence from a population-based sample of Canadian adolescents. BMJ Open. 2018;8(10):e021119. doi:10.1136/bmjopen-2017-021119. [Google Scholar] [PubMed] [CrossRef]
34. Malmborg JS, Roswall J, Almquist-Tangen G, Dahlgren J, Alm B, Bergman S. Associations between pain, health, and lifestyle factors in 10-year-old boys and girls from a Swedish birth cohort. BMC Pediatr. 2023;23(1):328. doi:10.1186/s12887-023-04139-2. [Google Scholar] [PubMed] [CrossRef]
35. Falck RS, Davis JC, Li L, Stamatakis E, Liu-Ambrose T. Preventing the ‘24-hour Babel’: the need for a consensus on a consistent terminology scheme for physical activity, sedentary behaviour and sleep. Br J Sports Med. 2022;56(7):367–8. doi:10.1136/bjsports-2021-104487. [Google Scholar] [PubMed] [CrossRef]
36. Korczak DJ, Madigan S, Colasanto M. Children’s physical activity and depression: a meta-analysis. Pediatrics. 2017;139(4):e20162266. doi:10.1542/peds.2016-2266. [Google Scholar] [PubMed] [CrossRef]
37. Brown DMY, Kwan MYW. Movement behaviors and mental wellbeing: a cross-sectional isotemporal substitution analysis of canadian adolescents. Front Behav Neurosci. 2021;15:736587. doi:10.3389/fnbeh.2021.736587. [Google Scholar] [PubMed] [CrossRef]
38. Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62. doi:10.1136/bjsports-2020-102955. [Google Scholar] [PubMed] [CrossRef]
39. Hou M, Herold F, Werneck AO, Teychenne M, Paoli AGD, Taylor A, et al. Associations of 24-hour movement behaviors with externalizing and internalizing problems among children and adolescents prescribed with eyeglasses/contact lenses. Int J Clin Health Psychol. 2024;24(1):100435. doi:10.1016/j.ijchp.2023.100435. [Google Scholar] [PubMed] [CrossRef]
40. Gao Y, Yu Q, Schuch FB, Herold F, Hossain MM, Ludyga S, et al. Meeting 24-h movement behavior guidelines is linked to academic engagement, psychological functioning, and cognitive difficulties in youth with internalizing problems. J Affect Disord. 2024;349:176–86. doi:10.1016/j.jad.2024.01.017. [Google Scholar] [PubMed] [CrossRef]
41. Recchia F, Bernal JDK, Fong DY, Wong SHS, Chung PK, Chan DKC, et al. Physical activity interventions to alleviate depressive symptoms in children and adolescents: a systematic review and meta-analysis. JAMA Pediatr. 2023;177(2):132–40. doi:10.1001/jamapediatrics.2022.5090. [Google Scholar] [PubMed] [CrossRef]
42. Rothon C, Edwards P, Bhui K, Viner RM, Taylor S, Stansfeld SA. Physical activity and depressive symptoms in adolescents: a prospective study. BMC Med. 2010;8:32. doi:10.1186/1741-7015-8-32. [Google Scholar] [PubMed] [CrossRef]
43. Herring MP, Meyer JD. Resistance exercise for anxiety and depression: efficacy and plausible mechanisms. Trends Mol Med. 2024;30(3):204–6. doi:10.1016/j.molmed.2023.11.016. [Google Scholar] [PubMed] [CrossRef]
44. Bender T, Nagy G, Barna I, Tefner I, Kádas E, Géher P. The effect of physical therapy on beta-endorphin levels. Eur J Appl Physiol. 2007;100(4):371–82. doi:10.1007/s00421-007-0469-9. [Google Scholar] [PubMed] [CrossRef]
45. Hou M, Herold F, Zhang Z, Ando S, Cheval B, Ludyga S, et al. Human dopaminergic system in the exercise-cognition link. Trends Mol Med. 2024;30(8):708–12. doi:10.1016/j.molmed.2024.04.011. [Google Scholar] [PubMed] [CrossRef]
46. Molendijk ML, Spinhoven P, Polak M, Bus BA, Penninx BW, Elzinga BM. Serum BDNF concentrations as peripheral manifestations of depression: evidence from a systematic review and meta-analyses on 179 associations (N = 9484). Mol Psychiat. 2014;19(7):791–800. doi:10.1038/mp.2013.105. [Google Scholar] [PubMed] [CrossRef]
47. Deslandes A, Moraes H, Ferreira C, Veiga H, Silveira H, Mouta R, et al. Exercise and mental health: many reasons to move. Neuropsychobiology. 2009;59(4):191–8. doi:10.1159/000223730. [Google Scholar] [PubMed] [CrossRef]
48. Ludyga S, Schilling R, Colledge F, Brand S, Pühse U, Gerber M. Association between cardiorespiratory fitness and social cognition in healthy adults. Scand J Med Sci Sports. 2020;30(9):1722–8. doi:10.1111/sms.13730. [Google Scholar] [PubMed] [CrossRef]
49. Ludyga S, Ishihara T, Kamijo K. The nervous system as a pathway for exercise to improve social cognition. Exerc Sport Sci Rev. 2022;50(4):203–12. doi:10.1249/JES.0000000000000300. [Google Scholar] [PubMed] [CrossRef]
50. Simpson A, Teague S, Kramer B, Lin A, Thornton AL, Budden T, et al. Physical activity interventions for the promotion of mental health outcomes in at-risk children and adolescents: a systematic review. Health Psychol Rev. 2024;18(4):899–933. doi:10.1080/17437199.2024.2391787. [Google Scholar] [PubMed] [CrossRef]
51. Liu C, Liang X, Yang Y, Liu R, Arbour-Nicitopoulos K, Sit CH. Mechanisms linking physical activity with mental health in children and adolescents with neurodevelopmental disorders: a systematic review. Am J Prev Med. 2024;67(4):592–605. doi:10.1016/j.amepre.2024.05.022. [Google Scholar] [PubMed] [CrossRef]
52. Suchert V, Hanewinkel R, Isensee B. Sedentary behavior and indicators of mental health in school-aged children and adolescents: a systematic review. Prev Med. 2015;76:48–57. doi:10.1016/j.ypmed.2015.03.026. [Google Scholar] [PubMed] [CrossRef]
53. Endrighi R, Steptoe A, Hamer M. The effect of experimentally induced sedentariness on mood and psychobiological responses to mental stress. Br J Psychiat. 2016;208(3):245–51. doi:10.1192/bjp.bp.114.150755. [Google Scholar] [PubMed] [CrossRef]
54. Marks J, de la Haye K, Barnett LM, Allender S. Friendship network characteristics are associated with physical activity and sedentary behavior in early adolescence. PLoS One. 2015;10(12):e0145344. doi:10.1371/journal.pone.0145344. [Google Scholar] [PubMed] [CrossRef]
55. Nigg CR, Fuchs R, Gerber M, Jekauc D, Koch T, Krell-Roesch J, et al. Assessing physical activity through questionnaires—a consensus of best practices and future directions. Psychol Sport Exerc. 2020;50:101715. doi:10.1016/j.psychsport.2020.101715. [Google Scholar] [CrossRef]
56. Prince SA, Cardilli L, Reed JL, Saunders TJ, Kite C, Douillette K, et al. A comparison of self-reported and device measured sedentary behaviour in adults: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2020;17(1):31. doi:10.1186/s12966-020-00938-3. [Google Scholar] [PubMed] [CrossRef]
57. Pascoe MC, Bailey AP, Craike M, Carter T, Patten RK, Stepto NK, et al. Poor reporting of physical activity and exercise interventions in youth mental health trials: a brief report. Early Interv Psychiat. 2020;15(5):1414–22. doi:10.1111/eip.13045. [Google Scholar] [PubMed] [CrossRef]
58. Yan W, Wang Y, Yuan Y, Farid M, Zhang P, Peng K. Timing matters: a longitudinal study examining the effects of physical activity intensity and timing on adolescents’ mental health outcomes. J Youth Adolesc. 2024;53(10):2320–31. doi:10.1007/s10964-024-02011-9. [Google Scholar] [PubMed] [CrossRef]
59. Noetel M, Sanders T, Gallardo-Gómez D, Taylor P, Del Pozo Cruz B, Van den Hoek D, et al. Effect of exercise for depression: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2024;385:q1024. doi:10.1136/bmj-2023-075847. [Google Scholar] [PubMed] [CrossRef]
60. Murri MB, Ekkekakis P, Magagnoli M, Zampogna D, Cattedra S, Capobianco L, et al. Physical exercise in major depression: reducing the mortality gap while improving clinical outcomes. Front Psychiat. 2019;9:762. doi:10.3389/fpsyt.2018.00762. [Google Scholar] [PubMed] [CrossRef]
61. Cody R, Beck J, Brand S, Donath L, Eckert A, Faude O, et al. Depression severity and psychosocial determinants of physical activity behavior in in-patients with major depressive disorders. Psychol Sport Exerc. 2022;63:102294. doi:10.1016/j.psychsport.2022.102294. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools