 Open Access
Open Access
REVIEW
Caregiver Burden of Children with Attention Deficit/Hyperactivity Disorder (ADHD): A Systematic Review
1 Nursing College, Palestine Polytechnique University, Hebron, P720, Palestine
2 School of Leadership and Advanced Nursing Practice, College of Nursing and Health Professions, The University of Southern Mississippi, Hattiesburg, MS 39406-0001, USA
* Corresponding Author: Nadia Amro. Email:
International Journal of Mental Health Promotion 2025, 27(5), 637-648. https://doi.org/10.32604/ijmhp.2025.060988
Received 14 November 2024; Accepted 14 April 2025; Issue published 05 June 2025
Abstract
Background: Raising a child with attention deficit hyperactivity disorder (ADHD) is a key challenge for the primary caregiver. This systematic review aims to identify major burdens facing the primary caregiver of a child with ADHD. Methods: The electronic databases CINAHL, PubMed, and Google Scholar were searched for studies published in English from 2017 to 2022 assessing the challenges facing caregivers of a child with ADHD. The Johns Hopkins Nursing Evidence-Based Practice Model was used to assess quality and risk of bias of studies identified for inclusion. Articles were synthesized by evaluating principal themes of burden to caregivers, stress of caregivers, and effectiveness of intervention programs. Results: Eleven articles were included in this review and included a total of 2426 participants. Findings revealed that caregivers of children with ADHD have a poor quality of life and high stress levels. Supportive parenting programs can be effective for improved coping and adaptation mechanisms with children with ADHD. However, few interventional studies were identified, increasing potential for bias. No meta-analysis was conducted. Conclusion: Caregivers of children with ADHD can benefit from strategies to improve their quality of life and reduce their stress levels. Targeted parenting programs can make a positive difference in the well-being of caregivers and children with ADHD. Additional research is needed to address the evidence-based effectiveness of parenting support programs.Keywords
Supplementary Material
Supplementary Material FileAttention deficit hyperactivity disorder (ADHD) is the most common childhood neurodevelopmental disorder and among the most prevalent chronic health conditions affecting school-age children [1]. An analysis by the National Health Interview Survey (NHIS) determined the prevalence of ADHD diagnoses increased from 1997 to 2016 in US children from 6.1% to 10.2% [2]. A similar prevalence rate was observed in the US during the years 2017 to 2022 [3]. As recognition has increased, the impact attributed to the condition has also, contributed to a global burden of increase in disability-adjusted life years (DALYs) across 204 countries from 1990 to 2019 [4].
According to the National Institute for Health and Care Excellence, the diagnosis of ADHD should only be completed by a psychosocial assessment by a pediatrician, psychiatrist, or qualified healthcare professional. It also should include a full clinical evaluation and review of the child’s symptoms, including the presence of social, educational, and psychological impairments in the different domains of the child’s everyday life and settings, and not solely on rating scales. A positive diagnosis should meet the criteria in Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the International Classification of Diseases (ICD-10) [5].
The impulsivity and inattention of the child can make parenting unusually difficult, and parents may blame high stress levels on their children’s behavior, unmet support needs, and stigma surrounding the condition [6,7]. Treatment approaches include pharmacological options, psychological interventions for behavior modification, and school accommodations for learning and academic support [8].
For a caregiver, responsibility for a child with ADHD means a life full of challenges. These may include difficulties in the environment, inattention, increased distractibility, and decreased self-inhibitory capacity, in addition to motor overactivity and restlessness [9]. Children with an ADHD diagnosis commonly experience academic underachievement, low self-esteem, and poor interpersonal relationships with family and friends, and may commonly be diagnosed with other behavioral, emotional, language, and learning disorders [5]. Approximately 40%–50% of children with ADHD persist with varying symptoms into adulthood, frequently leading to significant unemployment as well as increased risk of antisocial behaviors including substance abuse, difficulty sustaining social relationships, and problems with the law [10]. However, limited attention has been given to caregivers of children with ADHD and how the burden of coordinating care may impact their quality of life. Having a child with ADHD can put parents in a demanding situation [11]. Parents caring for children with ADHD face diverse challenges, including but not limited to managing their economic burden meeting the time and resources needs of their children, in addition to psychological problems, lack of support, and stigma from the community [12]. ADHD symptoms and behaviors impact the child’s social and academic life affect parents and thereby influence family functioning as a whole [13]. Further, several barriers can hinder the effective parenting of children with ADHD, such as the burden of care which can cause depression symptoms among caregivers [14]. Parenting stress potentiates adverse childhood experiences as it influences the child’s mental and behavioral outcomes, which in turn can be mitigated by family resilience [15]. In comparison to mothers of children with average development, mothers of children with ADHD reported significantly lower HRQoL (Health-Related Quality of Life) Mothers of Children with ADHD sought more help and used more indirect methods and coping strategies compared to mothers of children.
Several studies have discussed the effectiveness of positive parenting strategies to overcome the challenges facing children with ADHD’s mothers. Positive parenting training has shown a significant impact on enhancing executive functions and impulsivity in children with ADHD [16]. Findings of a randomized control trial in Sweden showed improved parenting behavior and competence in addition to decreased parenting stress in a post-test behavioral management training of mothers of children with ADHD [17]. Similarly, Chesterfield et al. [18] reported less dysfunctional parenting and less disruptive child behavior after six months of follow-up post-intervention. These studies were consistent with a meta-analysis that recommended the adoption of effective parenting programs as a part of the ADHD intervention plan [19].
Despite these findings, further research is needed about the burden of the caregiver experience for children with ADHD. Exploring the nature and characteristics of this challenge can provide further insight into the development of effective management of ADHD treatment and parenting programs. Additional examination of the literature is needed to evaluate the impact of the experiences of caregivers and address this gap. This systematic review aims to identify major burdens facing primary caregivers of a child with ADHD.
The systematic review study aims to explore the most frequent challenges facing the caregiver of a child with ADHD according to the guidelines of PRISMA (see the supplementary material) [20]. The search was designed and conducted by two PhD-prepared nurse scientists who collaborated to identify potential articles. The lead author, who has five years of nursing experience and two years of clinical experience working with children and families experiencing ADHD, personally reviewed all the articles and made a final determination regarding inclusion.
In accordance with PRISMA guidelines, a literature search was conducted utilizing the databases CINAHL, PubMed, and Google Scholar. The relevant search terms utilized included (“ADHD” AND “caregiver burden”) OR (mothers AND child with ADHD) OR (attention deficit disorder with) hyperactivity”[MeSH Terms] OR (“attention”[All Fields] AND “deficit”[All Fields] AND “disorder”[All Fields] AND “hyperactivity”[All Fields]) OR “attention deficit disorder with hyperactivity”[All Fields] OR “ADHD”[All Fields]) AND (“child”[MeSH Terms] OR “child”[All Fields] OR “children”[All Fields] OR “children’s”[All Fields] OR “children”[All Fields] OR “child’s”[All Fields]) AND (“mothers”[All Fields] OR “mothered”[All Fields] OR “mothers”[MeSH Terms] OR “caregiver”[All Fields] OR “mother”[All Fields] OR “mothering”[All Fields]).
The search was limited to English peer-reviewed research articles published in academic journals. The goal of the review was to focus on the most recent five-year period, and the search was limited to articles from 2017 onward. Inclusion criteria required the focus of the research to include children only specifically diagnosed with ADHD with their primary caregivers. Research findings focused on children with ADHD combined with other conditions such as autism or mental disorders, such as patients co-diagnosed with autism, were excluded, to avoid confounding. Additional criteria limited inclusion to articles that were primary data-driven studies, thus review and opinion articles were excluded. The articles were assessed using the Johns Hopkins Nursing Evidence-Based Practice Model to evaluate the quality and strength of evidence in healthcare research [21]. The Johns Hopkins Evidence-based Practice for Nurses and Healthcare model was developed to evaluate the quality and strength of evidence in healthcare research. It is commonly used to assess the validity and reliability of studies, assess bias, and determine the level of evidence supporting healthcare practices. This model categorizes Level I research as Experimental, Level II as Quasi-experimental, and Level III as Non-Experimental concurrently evaluates the quality and risk of bias of each study according to its type, as High, Good, or Low.
Because this systematic review was not a meta-analysis, no data conversions, subgroup analyses, effect measures, confidence interval calculations, or sensitivity analyses were conducted.
The search generated 558 articles. Duplicate articles were removed (n = 14) and articles not relevant to the research question (n = 496) were marked as ineligible based on a review of the abstract. Of the remaining 48 abstracts reviewed, more than half (n = 28) were excluded as they were not specific to the condition of ADHD in children and their caregivers, for example, if the analysis incorporated a comorbid condition. Twenty articles were sought for retrieval. Four of them were not retrieved. The remaining articles (n = 16) were assessed for eligibility. Three of these were excluded as they were conducted in a systematic review design, and two articles were excluded on the basis of relevance. Based on these exclusion criteria the final sample size was reduced to 11 articles. See PRISMA diagram (Fig. 1).
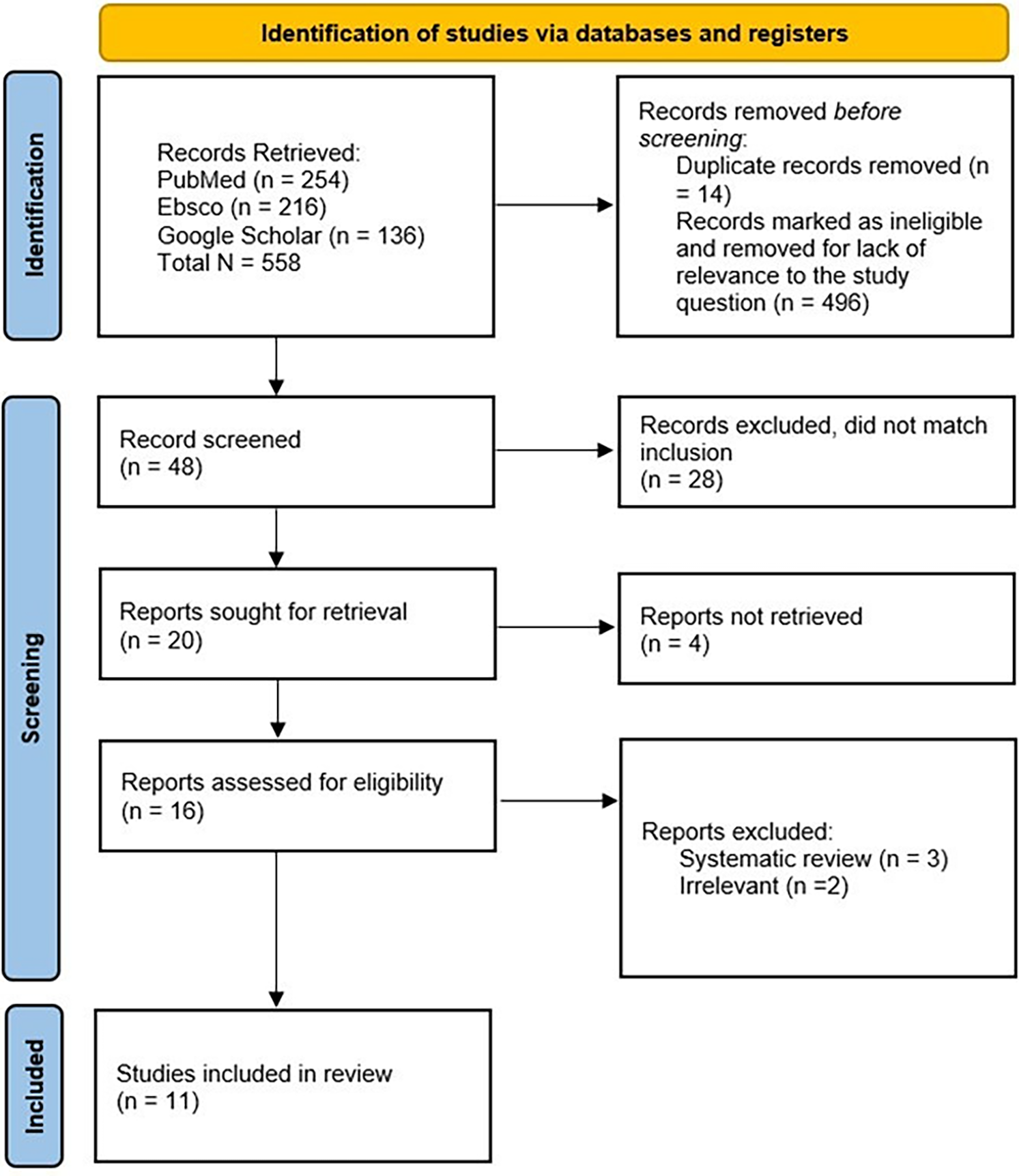
Figure 1: PRISMA diagram
As a result of the search process, 11 articles were included in the qualitative analysis. All 11 articles were confirmed to be High or Good in quality, using reasonable research procedures to develop scientific evidence based on recommendations consistent with findings [21]. In terms of strength of evidence, a single Level I article was conducted in a randomized control trial design [22], this experimental study examined parenting support programs. Another article of Level II was conducted in a quasi-experimental design to assess the effect of the resiliency program used on the level of care burden or stress [23].
The rest of the studies were descriptive in nature and observational. Three of the articles [13,24,25] were conducted in a qualitative design at Level III. The remaining articles were of Level IV and framed by a quantitative design [26–31].
The sampling strategies used in these investigations were most frequently convenience sampling, such as in the cross-sectional studies. The single randomized control study blindly assigned participants to each condition [22]. Three qualitative studies relied on purposive sampling [13,24,25].
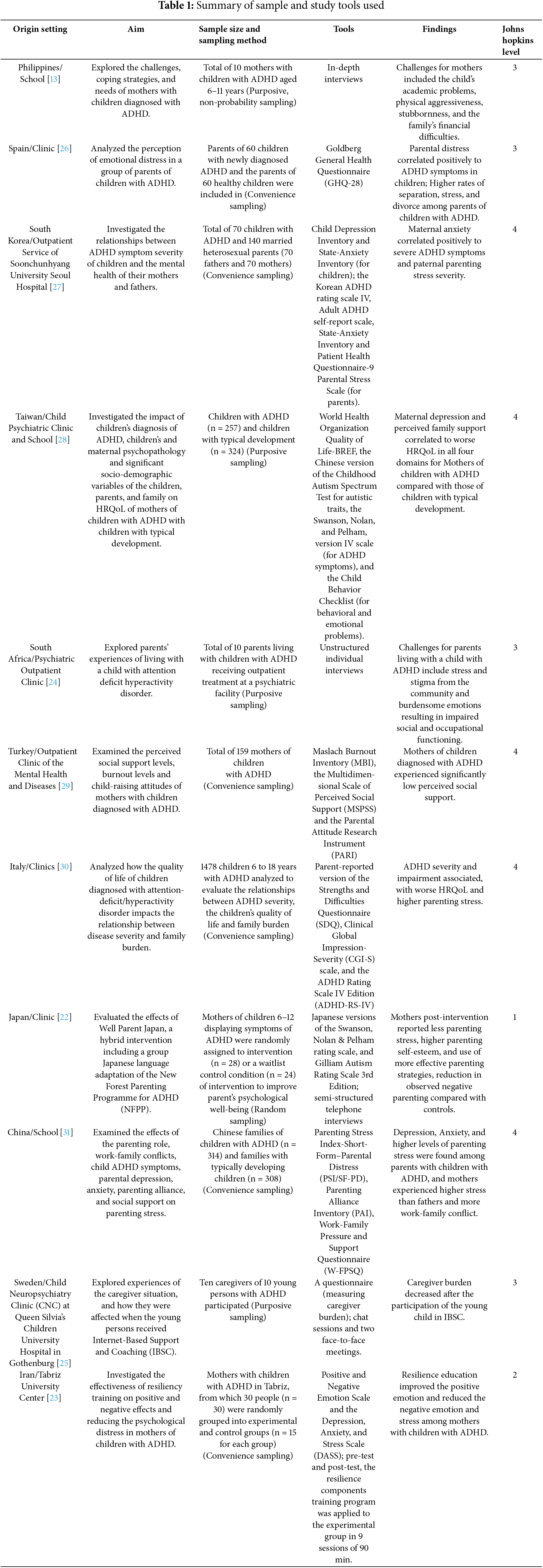
The investigations included a total of 2426 participants. Each article in the review represented research conducted in a different country or region: China, Mainland China, Taiwan, South Africa, Turkey, Iran, Japan, Philippines, Spain, Italy, Sweden, and South Korea. The settings where the identified studies were conducted included psychiatric outpatient clinics [24,25,28,29], as well as a hospital or a medical center [26]. Another two studies were conducted at a university campus [22,23]. One study was conducted using an online questionnaire [30]. One study was performed in a primary school [13]. One other study was conducted in mixed settings of both a school and a hospital [31].
Several different methods and surveys were used in the data collection. In-depth interviews were used for qualitative study designs [13,24,25]. Several tools are used in quantitative study design to explore the caregiver challenges and difficulties, including the Goldberg General Health Questionnaire (GHQ-28) [26], the Korean ADHD rating scale-IV, Adult ADHD self-report scale State-Anxiety Inventory and Parental Stress Scale [27], the World Health Organization Quality of Life-BREF, Maslach Burnout Inventory (MBI) [28], the Multidimensional Scale of Perceived Social Support (MSPSS), Parental Attitude Research Instrument (PARI), Parent-reported version of the Strengths and Difficulties Questionnaire (SDQ), the Clinical Global Impression-Severity (CGI-S) scale of ADHD Rating Scale IV Edition (ADHD-RS-IV) [29], the Parenting Stress Index-Short-Form-Parental Distress (PSI/SF-PD) [23], and the Parenting Alliance Inventory (PAI) [31].
The samples in six studies incorporated both the mother and father of the children with ADHD [22,24,26,27,30,31]. The other five studies (45%) recruited only mothers in their samples [13,23,25,28,29]. No investigations included in the review had primary caregivers other than mothers or fathers. For a complete summary of articles, see Table 1.
The majority of the observational and descriptive studies described the most common challenges of a caregiver in raising a child with ADHD. Dimensions that were influenced included social, psychological, and physical burdens in their lives as all of them concluded that the caregiver of a child with ADHD had emotional stress [25,31] and negative emotions [23]. Low social support and burnout [24,29]. Another finding across studies was the poor quality of life for the mother in addition to poor academic achievement for the ADHD-diagnosed child [13,27,30,31].
As a result of their research, both studies from Liang et al. [28] and Si et al. [31] concluded that stress is higher in the caregivers of a child with ADHD than among caregivers of a typically developing child. Further, several studies [26,31] correlated increased maternal stress to the severity of ADHD symptoms. Similarly, the study from [30] showed that parental stress was related to parental perception of low quality of life for their children with ADHD and not related to the severity of the symptoms.
3.4 Effectiveness of Intervention Programs
Two studies [22,23] examined the positive influence of implementing intervention programs for the parents of a child with ADHD for improving parenting practices and skills in raising a child with ADHD in addition to improved self-esteem for the parent. Tabatabaei and Chalabainloo [23] found that resiliency training decreased psychological distress and increased the positive effect for the mother of a child with ADHD. On the other hand, the burden of care was not significantly improved, and another study [25], found no common trajectory in change or improvement in the burden of care post (IBSC) an Internet-Based Support and Coaching program for children. This investigation was limited to 10 caregivers and their children, however, limiting generalizability.
This systematic review study found strong support that caregivers of children with ADHD experience increased burdens managing the challenges of their children’s condition. These burdens included feelings of stress, physical demands, and poor quality of life. The most pronounced findings were related to the deteriorating psychological status of the caregivers and the increased burden of care while having a child with ADHD [13,24,26,27,29–31]. In general, the caregiver’s well-being and mental health are considered to affect the child’s well-being [15]. Several papers specifically focused on the mother as the primary person and the capstone for effective family function and support. In these articles, she is perceived as the person who will mainly manage to overcome conflicts and achieve balance for the child [13,23,25,28,29]. Consequently, the mother and child’s well-being are interrelated, and the severity of maternal stress has specifically been associated with a child with more complicated ADHD symptoms [27]. At the same time, Uddin et al. [15] noted the influence of parental stress on the child’s behavioral outcome and adverse child experience, which could reinforce the relationship.
Another consistent finding was the poor quality of life for a mother of a child with ADHD [28], specifically leading to burnout. Polat and Karakas [29] found that mothers of children with ADHD experienced greater burnout displaying negative child-raising attitudes. Three studies correlated this decrease in quality of life to the severity of the child’s symptoms [26,30,32]. This work was consistent with Si et al. [31] who found that parents of children with ADHD reported much more parenting stress compared to parents without children with the condition. In addition to stress, the child’s condition appeared to foster feelings of stigma, and social dysfunction [24]. This was similar to the study of Leitch et al. [7] who found parental stress related to child behavior and social stigma.
The caregiver of a child with ADHD needs extensive support programs to ease the burden of care and learn coping strategies. Tabatabaei and Chalabainloo [7,23] conducted an effective resiliency program found to decrease the negative mother’s affect and promote positive emotions. This was in line with the demonstrated effectiveness of family resiliency on the improvement of a child’s adverse experiences with ADHD as a cause of parenting stress. Studies [15,22] found that less parenting stress, higher self-esteem, and more effective parenting strategies were the major outcomes in a randomized controlled trial of applied techniques to increase psychological well-being and gain the confidence of parents in their abilities to make changes when compared to the control group. Additionally, it was found that positive parenting training has a considerable influence on improving executive functioning and impulsivity in children with ADHD [16]. Similarly, Yusuf et al. [19] showed improvement in family functional attitude after the adoption of the triple parenting program as a part of the ADHD intervention plan.
The results of this systematic review demonstrated the necessity of identifying the burdens experienced by the caregivers of children with ADHD. This information has the potential to increase the sensitivity of healthcare providers to provide support that will enable caregivers to offer better care and understanding to their children with the condition. Further research will aid in the change and improvement in the quality of clinical care for children with ADHD and guide the inclusion of their primary caregiver or parents as an integral part of the intervention and treatment plan. This evidence calls for the incorporation of parenting programs, support groups, and education for parents of children with the condition to deliver social and functional strategies and coping mechanisms, especially for those experiencing burnout.
Despite this systematic review, there is still a knowledge gap in addressing several aspects of the burden for ADHD caregivers. For example, more research is needed specifically on the roles of other caregivers, such as grandparents. Furthermore, it is possible that the search strategy prioritized mothers as caregivers for the child with ADHD, as this was only explored in six articles of the 11 articles.
A third recommendation regards the need for randomized control trials to study to investigate the effectiveness of parenting programs on the improvement of parental attitudes and behavior in caring for a child with ADHD. Although outside the main focus of the investigation, this finding provides guidance regarding the type of intervention that should be emphasized in follow-up studies to provide support for caregivers.
This research spotlights special needs and supports the caregiver and the child with ADHD to promote an atmosphere of understanding and positive adaptation strategies and bridge a new step forward in incorporating mental health and behavioral well-being.
One limitation of this systematic review is that it was not registered prospectively, which may be considered to reduce the potential for bias. Thus, a recommendation would be to register prospectively for a follow-up examination as further research becomes available. This important and quickly developing topic merits further examination. Besides, at this time, a limited sample of articles are available on the topic of caregivers of children specifically with ADHD. Many of the articles initially identified by the keywords did not meet inclusion criteria, as they included children with comorbid disorders rather than concentrating on children with ADHD specifically. Additionally, the quality of the articles varied considerably, including in the sampling methodology.
This systematic review study adds supportive evidence that caregivers of a child with ADHD may experience a burden of care associated with their role. The findings of this study indicate more research is needed to investigate and address the burden and negative effects experienced by both caregivers of children with ADHD. These efforts can help promote a positive quality of life for both caregivers and children with ADHD.
Acknowledgement: Not applicable.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: Nadia Amro initiated the concept and design of the study. Nadia Amro and Lila de Tantillo contributed to the manuscript preparation, manuscript editing and manuscript review. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval: Not applicable.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
Supplementary Materials: The supplementary material is available online at https://www.techscience.com/doi/10.32604/ijmhp.2025.060988/s1.
References
1. American Academy of Pediatrics, Subcommittee on Attention-Deficit/Hyperactivity Disorder, & Steering Committee on Quality Improvement and Management. ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007–22. doi:10.1542/peds.2011-2654. [Google Scholar] [CrossRef]
2. Xu G, Strathearn L, Liu B, Yang B, Bao W. Twenty-year trends in diagnosed attention-deficit/hyperactivity disorder among US children and adolescents, 1997–2016. JAMA Netw Open. 2018;1(4):e181471. doi:10.1001/jamanetworkopen.2018.1471. [Google Scholar] [PubMed] [CrossRef]
3. Li Y, Yan X, Li Q, Li Q, Xu G, Lu J, et al. Prevalence and trends in diagnosed ADHD Among US Children and Adolescents, 2017–2022. JAMA Netw Open. 2023;6(10):e2336872. doi:10.1001/jamanetworkopen.2023.36872. [Google Scholar] [PubMed] [CrossRef]
4. Cortese S, Song M, Farhat LC, Yon DK, Lee SW, Kim MS, et al. Incidence, prevalence, and global burden of ADHD from 1990 to 2019 across 204 countries: data, with critical re-analysis, from the Global Burden of Disease study. Mol Psychiatry. 2023;28(11):4823–30. doi:10.1038/s41380-023-02228-3. [Google Scholar] [PubMed] [CrossRef]
5. Dalrymple RA, Maxwell LM, Russell S, Duthie J. NICE guideline review: attention deficit hyperactivity disorder: diagnosis and management (NG87). Arch Dis Childhood-Educ Pract. 2020;105(5):289–93. doi:10.1136/archdischild-2019-316928. [Google Scholar] [PubMed] [CrossRef]
6. Adeosun II, Ogun O, Adegbohun A, Ijarogbe G, Fatiregun O. The burden on caregivers of children with attention-deficit hyperactivity disorder in Lagos Nigeria: prevalence and correlates. J Educ Soc Behav Sci. 2017;22(1):1–7. doi:10.9734/jesbs/2017/35582. [Google Scholar] [CrossRef]
7. Leitch S, Sciberras E, Post B, Gerner B, Rinehart N, Nicholson JM, et al. Experience of stress in parents of children with ADHD: a qualitative study. Int J Qualit Stud Health Well-Being. 2019;14(1):1–12. doi:10.1080/17482631.2019.1690091. [Google Scholar] [PubMed] [CrossRef]
8. Fabiano GA, Schatz NK, Aloe AM, Pelham WE Jr, Smyth AC, Zhao X, et al. Comprehensive meta-analysis of attention-deficit/hyperactivity disorder psychosocial treatments investigated within between group studies. Rev Educ Res. 2021;91(5):718–60. doi:10.3102/00346543211025092. [Google Scholar] [CrossRef]
9. Riddle MA, Yershova K, Lazzaretto D, Paykina N, Yenokyan G, Greenhill L, et al. The preschool attention-deficit/hyperactivity disorder treatment study (PATS) 6-year follow-up. J Am Acad Child Adolesc Psychiatry. 2013;52(3):264–78.e2. doi:10.1097/01.chi.0000235074.86919.dc. [Google Scholar] [CrossRef]
10. Kliegman MR. Nelson textbook of pediatrics, 2-volume set. Elsevier; 2016. [Google Scholar]
11. Moen ØL, Hall-Lord ML, Hedelin B. Contending and adapting every day: norwegian parents’ lived experience of having a child with ADHD. J Fam Nurs. 2011;17(4):441–62. doi:10.1177/1074840711423924. [Google Scholar] [PubMed] [CrossRef]
12. Ching’oma CD, Mkoka DA, Ambikile JS, Iseselo MK. Experiences and challenges of parents caring for children with attention-deficit hyperactivity disorder: a qualitative study in Dar es salaam, Tanzania. PLos One. 2022;17(8):e0267773. doi:10.1371/journal.pone.0267773. [Google Scholar] [PubMed] [CrossRef]
13. Balagan MMB, Tarroja MC. Challenges, coping strategies, and needs of mothers with children with attention deficit hyperactivity disorder: implications for intervention. Open J Soc Sci. 2021;8(12):24–35. doi:10.4236/jss.2020.812003. [Google Scholar] [CrossRef]
14. del-Pino-Casado R, Rodriguez Cardosa M, López-Martínez C, Orgeta V. The association between subjective caregiver burden and depressive symptoms in carers of older relatives: a systematic review and meta-analysis. PLoS One. 2019;14(5):e0217648. doi:10.1371/journal.pone.0217648. [Google Scholar] [PubMed] [CrossRef]
15. Uddin J, Alharbi N, Uddin H, Hossain MB, Hatipoğlu SS, Long DL, et al. Parenting stress and family resilience affect the association of adverse childhood experiences with children’s mental health and attention-deficit/hyperactivity disorder. J Affect Disord. 2020;272:104–9. doi:10.1016/j.jad.2020.03.132. [Google Scholar] [PubMed] [CrossRef]
16. Jalilvand M, Bagheri F, Nikmanesh Z. The influence of positive parenting training on improving behavioral function and impulsivity in children suffering from attention-deficit/hyperactivity disorder. Int J Med Toxicol Forens Med. 2022;12(1):35740. doi:10.32598/ijmtfm.v12i1.35740. [Google Scholar] [CrossRef]
17. Stattin H, Enebrink P, Özdemir M, Giannotta F. A national evaluation of parenting programs in Sweden: the short-term effects using an RCT effectiveness design. J Consult Clin Psychol. 2015;83(6):1069. doi:10.1037/a0039328. [Google Scholar] [PubMed] [CrossRef]
18. Chesterfield JA, Porzig-Drummond R, Stevenson RJ, Stevenson CS. Evaluating a brief behavioral parenting program for parents of school-aged children with ADHD. Parenting. 2021;21(3):216–40. doi:10.1080/15295192.2020.1777783. [Google Scholar] [CrossRef]
19. Yusuf Ö, Gonka Ö, Pekcanlar Aynur A. The effects of the triple P-positive parenting programme on parenting, family functioning and symptoms of attention-deficit/hyperactivity disorder. A randomized controlled trial. Psychiatry Clin Psychopharmacol. 2019;29(4):665–73. doi:10.1080/24750573.2018.1542189. [Google Scholar] [CrossRef]
20. Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA, 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi:10.1136/bmj.n160. [Google Scholar] [PubMed] [CrossRef]
21. Dang D, Dearholt SL, Bissett K, Ascenzi J, Whalen M. Johns Hopkins evidence-based practice for nurses and healthcare professionals: model and guidelines. 4th edition. Sigma Theta Tau International Honor Society of Nursing; 2022. [Google Scholar]
22. Shimabukuro S, Daley D, Thompson M, Laver-Bradbury C, Lovern K, Tripp G. Supporting Japanese mothers of children at risk for attention deficit hyperactivity disorder (ADHDa small scale randomized control trial of well parent Japan. J Child Fam Stud. 2020;29(6):1604–16. [Google Scholar]
23. Tabatabaei SM, Chalabainloo G. The effectiveness of resilience training on positive and negative affect and reduction of psychological distress in mothers of children with attention deficit hyperactivity disorder. J Arak Univ Med Sci. 2020;23(4):438–49. [Google Scholar]
24. Mofokeng M, van der Wath AE. Challenges experienced by parents living with a child with attention deficit hyperactivity disorder. J Child Adoles Ment Health. 2017;29(2):137–45. doi:10.2989/17280583.2017.1364253. [Google Scholar] [PubMed] [CrossRef]
25. Söderqvist H, Kajsa E, Ahlström BH, Wentz E. The caregivers’ perspectives of burden before and after an internet-based intervention of young persons with ADHD or autism spectrum disorder. Scand J Occup Ther. 2017;24(5):383–92. doi:10.1080/11038128.2016.1267258. [Google Scholar] [PubMed] [CrossRef]
26. Insa I, Alda JA, Chamorro M, Espadas M, Huguet A. Difference in psychic distress lived by parents with ADHD children and parents with healthy children: focus on gender differences. J Attent Disord. 2021;25(3):332–9. doi:10.1177/1087054718790010. [Google Scholar] [PubMed] [CrossRef]
27. Lee YJ, Kim J. Effect of maternal anxiety on parenting stress of fathers of children with ADHD. J Korean Med Sci. 2022;37(11):e89. doi:10.3346/jkms.2022.37.e89. [Google Scholar] [PubMed] [CrossRef]
28. Liang SHY, Lee Y-C, Kelsen BA, Chen VC-H. Health-related quality of life in mothers of children with attention deficit hyperactivity disorder in Taiwan: the roles of child, parent, and family characteristics. Res Dev Disabil. 2021;113(2):103944. doi:10.1016/j.ridd.2021.103944. [Google Scholar] [PubMed] [CrossRef]
29. Polat H, Karakas SA. An examination of the perceived social support, burnout levels and child-raising attitudes of mothers of children diagnosed with attention deficit hyperactivity disorder in Turkey. Int J Caring Sci. 2019;12(2):1165–74. doi:10.3138/9781442673038-003. [Google Scholar] [CrossRef]
30. Rocco I, Bonati M, Corso B, Minicuci N. Quality of life improvement in children with attention-deficit hyperactivity disorder reduces family’s strain: a structural equation model approach. Child Care Health Dev. 2021;47(5):667–74. doi:10.1111/cch.12874. [Google Scholar] [PubMed] [CrossRef]
31. Si Y, Ma JL, Zhang J. Factors influencing parenting stress among Chinese families of children with attention-deficit/hyperactivity disorder. Child Youth Serv Rev. 2020;116:105148. doi: 10.1016/j.childyouth.2020.105148. [Google Scholar] [CrossRef]
32. Coghill D, Hodgkins P. Health-related quality of life of children with attention-deficit/hyperactivity disorder versus children with diabetes and healthy controls. Eur Child Adoles Psychiatry. 2016;25:261–71. [Google Scholar] [PubMed]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools