 Open Access
Open Access
ARTICLE
Generalized Anxiety Disorder Prevalence and Related Risk Factors among Females with Polycystic Ovarian Syndrome in Jazan Region, Saudi Arabia
1 Family and Community Medicine Department, Faculty of Medicine, Jazan University, Jazan, 45142, Saudi Arabia
2 Internal Medicine Department, Faculty of Medicine, Jazan University, Jazan, 45142, Saudi Arabia
3 Faculty of Medicine, Jazan University, Jazan, 45142, Saudi Arabia
* Corresponding Author: Ahmad Y. Alqassim. Email:
International Journal of Mental Health Promotion 2025, 27(5), 701-716. https://doi.org/10.32604/ijmhp.2025.062924
Received 31 December 2024; Accepted 11 April 2025; Issue published 05 June 2025
Abstract
Background: Polycystic ovarian syndrome (PCOS), a common endocrine disorder in reproductive-aged women, has substantial physical and psychological impacts. While the physical manifestations of PCOS are well established, the psychological burden, especially anxiety, is understudied in Saudi Arabia. This study aimed to assess the prevalence of generalized anxiety disorder among females with PCOS compared to those without PCOS, and to identify the clinical and sociodemographic factors associated with anxiety in the Jazan region of Saudi Arabia. Methods: A cross-sectional study was conducted between January and March 2023 using an Arabic self-administered online questionnaire distributed via social media platforms. The study recruited 410 reproductive-age females (≥18 years) from the Jazan region using convenience sampling. The questionnaire encompassed socio-demographic characteristics, economic indicators, medical history, PCOS symptoms, and the validated Generalized Anxiety Disorder-7 (GAD-7) assessment tool. Results: The prevalence of PCOS in the study population was 22.44%. Women with PCOS showed significantly higher anxiety levels compared to controls without PCOS (32.61% vs. 22.33%). Biochemical hyperandrogenism was the strongest predictor of anxiety (OR = 4.179). Menstrual irregularities demonstrated a dose-dependent relationship with anxiety risk, wherein participants with 2–3 months and ≥3 months of amenorrhea had 2.5- and 3.3-times higher odds of anxiety compared to those with regular cycles (OR = 2.451 and 3.314). Other PCOS-related dermatological manifestations were also associated with increased anxiety, including hirsutism (OR = 1.745), alopecia (OR = 2.285) and acne (OR = 1.723). Marital status was a significant factor, with divorced/widowed females having 4.4-fold higher anxiety odds compared to single females (OR = 4.371). Conclusion: PCOS presents a significant psychological burden in Saudi women, with anxiety prevalence higher than the general population. The robust associations between PCOS manifestations and anxiety emphasize the need for integrated healthcare approaches that address both endocrine and mental health aspects. Routine psychological screening and support services should be incorporated into PCOS management protocols.Keywords
Polycystic ovarian syndrome (PCOS) is among the most common endocrine disorders, affecting approximately 8%–13% of reproductive-age women globally, and up to 70% of cases are undiagnosed [1]. The condition is characterized by hormonal imbalances that manifest through multiple reproductive and metabolic disturbances. Despite the widespread use of Rotterdam Consensus criteria, the lack of standardized diagnostic guidelines makes determining PCOS prevalence challenging [2–5]. The Rotterdam criteria, established in 2003, requires at least two of three symptoms for PCOS diagnosis: polycystic ovaries, hyperandrogenism, and irregular menstrual cycles [5,6]. Recent epidemiological studies have revealed varying prevalence rates across different geographical regions, 37.9% increase since 1990 in the Middle East and North Africa region [7], 6.2% (using NIH criteria) to 19.5% (using Rotterdam criteria) in European countries [8], and 5.2% in the United States [9]. The prevalence estimates vary significantly based on diagnostic criteria used and populations studied, with rates being 4–5 fold higher in the US compared to the UK [9]. In Saudi Arabia, epidemiological data remain limited, with only two notable studies conducted in Madinah, reporting substantially higher prevalence rates of 53.7% and 32.5% compared to global estimates [10,11].
Women face elevated risks of mental health conditions, as evidenced by two previous studies reporting high rates of mental illnesses among women. The physiological and societal challenges women experience during pregnancy, childbirth, and daily life can significantly contribute to mental health vulnerabilities [12,13]. However, Jazan region, Saudi Arabia’s developing area, presents unique healthcare challenges due to its diverse geography of islands, highlands, and coastal villages. Almalki and Ashdown’s research revealed that despite having a college education, about half of the young Saudi women in rural areas remain unemployed, living in middle-income households. While most report good health, their rural location and regional infrastructure limitations significantly impact healthcare accessibility, including reproductive health services [14]. These findings highlight the importance of investigating women-specific health conditions and their correlation with anxiety disorders, such as PCOS and its association with mental health in females.
The clinical manifestations of PCOS encompass a broad spectrum of physical and psychological symptoms that significantly impact patients’ quality of life [15]. These manifestations include hirsutism, obesity, acne, and various metabolic disturbances, which often lead to decreased self-esteem and increased risk of mental health disorders [16,17]. Global studies examining mental health effects in PCOS patients have consistently identified anxiety as a predominant psychological comorbidity, with prevalence rates 38.6% in PCOS patients compared to control populations [18], and a standardized mean difference of 0.63 higher than controls [19]. Anxiety is particularly elevated among those presenting with visible symptoms, with studies showing significant associations between anxiety and infertility and alopecia [18], and especially pronounced effects in Chinese populations with a pooled effect size of 0.97 [19]. The psychological burden appears to be further compounded by socioeconomic factors. In Saudi Arabia, mental health research in PCOS remains nascent, with only two significant studies conducted in Riyadh: a case-control study demonstrating a doubled risk of anxiety among PCOS patients, and a cross-sectional study reporting anxiety in 40% of affected individuals [20,21]. Moreover, in consistent with international findings, these investigations have identified significant associations between unemployment and low income with anxiety in PCOS patients [20,22,23].
The psychological impact of appearance-altering health conditions, particularly PCOS, extends beyond mere cosmetic concerns to fundamentally affect women’s self-concept and emotional well-being. PCOS emerges as a particularly challenging condition due to its multiple effects on physical appearance, including dermatological manifestations, weight changes, and hormonal imbalances that affect skin health [23]. Current research demonstrates that body image concerns and appearance-related anxiety are especially pronounced among adolescent girls and young women, largely attributed to pervasive sociocultural pressures and media-driven beauty standards [24]. These societal expectations create a complex psychological burden, studies indicate that appearance-based social prejudices can impact various aspects of daily life, from interpersonal relationships to professional opportunities. Women with PCOS who struggle to meet these culturally imposed beauty standards frequently experience a cascade of psychological consequences, including heightened anxiety regarding social evaluation, persistent body image dissatisfaction, and disrupted sleep patterns, potentially creating a cycle of physical and psychological distress [25].
Health conditions that alter physical appearance, particularly PCOS, can significantly impact women’s self-esteem. PCOS represents a major physiological disorder affecting women’s physical appearance and skin health worldwide [26]. Body image and physical appearance significantly influence self-esteem among adolescent girls and young women, primarily shaped by societal and media influences. Society has established and maintained specific beauty standards that create preferential treatment for physically attractive people [27]. When women don’t meet societal beauty standards, they often experience negative emotional consequences. These include anxiety about others’ judgments and personal body dissatisfaction, which can extend to affecting their sleep quality [28].
Despite the extensive international research on PCOS and its psychological comorbidities, there remains a critical knowledge gap in understanding the mental health burden among Saudi women with PCOS, particularly in the Jazan region. To our knowledge, this study addresses this critical research gap by providing the first assessment of generalized anxiety disorder among Jazan females with PCOS in Saudi Arabia, specifically investigating the associations between distinct PCOS manifestations and anxiety levels.
This research aims to establish baseline epidemiological data and identify potential risk factors that may inform targeted interventions for this vulnerable population. The findings will not only enhance our understanding of the psychological burden of PCOS in this geographical and cultural context but also contribute to the development of culturally appropriate screening and management strategies for anxiety in women with PCOS in the Jazan region. While several studies have documented the prevalence of anxiety in PCOS patients across different global populations, regional data from Saudi Arabia has been limited, with most studies focusing primarily on the endocrine and metabolic aspects of the syndrome. We hypothesized that women experiencing polycystic ovary syndrome symptoms would demonstrate significantly higher prevalence of generalized anxiety disorder compared to unaffected women.
A cross-sectional analytical study was conducted between 01 January 2023 and 31 March 2023, in the Jazan region of Saudi Arabia. Jazan, situated in the southwestern part of Saudi Arabia with an estimated population of 1.5 million [29], represents a unique geographical and demographic setting with distinct cultural characteristics. The region extends along the Red Sea coast and includes both urban and rural populations distributed across 16 governorates. The study employed a web-based methodology, which was considered appropriate given the cultural context, geographical spread, and the sensitive nature of the health conditions being studied. The sampling frame comprised females of reproductive age (18–55 years) residing in the Jazan region. Participants were recruited through a structured social media distribution strategy using social media platforms commonly used in the region. This recruitment strategy was chosen based on the high social media penetration rate in Saudi Arabia (approximately 95% among the target age group) [26].
The sample size was calculated using the formula n = Z2P(1-P)/d2, where Z = 1.96 (95% confidence level), P = 32.5% (estimated PCOS prevalence from previous Saudi studies [13], and d = 5% (margin of error), with a design effect of 1.2. This yielded a minimum required sample size of 374 participants, increased by 10% to 410 to account for potential non-response. A convenience sampling technique was employed through social media platforms, primarily WhatsApp, targeting females of reproductive age in the Jazan region. The recruitment strategy incorporated both urban (59.76%) and rural (40.24%) areas to enhance representativeness. Systematic distribution was implemented through community WhatsApp groups and other social media platforms, with structured reminder messages to optimize response rates. The final achieved sample of 410 participants met the calculated size requirement, with participants completing all mandatory questions, including the Generalized Anxiety Disorder-7 (GAD-7) assessment tool and PCOS diagnostic criteria questions. Despite the limitations of non-probability sampling, this approach provided a pragmatic method for accessing the target population while maintaining methodological rigor within the cultural and logistical constraints of the study setting.
2.3 Data Collection and Measurements
All data were gathered from a self-administered online questionnaire of multiple variables including a screening tool for generalized anxiety. The data collected was categorized into three parts: socioeconomic and demographic, medical history, and variables related to PCOS. Socio-economic data included age, marital status, income status, and others. Variables related to medical history included the presence of chronic diseases, psychiatric history, usage of medications, and family history. Variables related to PCOS included diagnosis status; and symptoms experienced by the patient, such as hirsutism, irregular menses, infertility, and acne. Meanwhile, to assess anxiety, we utilized the Arabic version of the GAD-7 questionnaire, a widely validated screening tool. This validated scale has demonstrated high reliability in Saudi populations (Cronbach’s α = 0.763) [30]. The scale comprises seven items measuring anxiety frequency on a 4-point Likert scale (0 = never to 3 = nearly every day), with total scores ranging from 0–21. Higher scores indicate more severe anxiety-related functional impairment. Participants were classified as: not anxious (0–4), mildly anxious (5–9), moderately anxious (10–14), or severely anxious (15–21). Following studies’ validated methodology, we employed a cut-off score of ≥10 to indicate the presence of generalized anxiety disorder [31,32].
This study was approved by the Standing Committee for Scientific Research at Jazan University (Reference No. REC-44/06/458) on 02 January 2022, under the protocol number HAPO-10-Z-001. The study was conducted in accordance with the Declaration of Helsinki. All participants provided informed consent before participation. Participants didn’t participate until they gave full approval. We did ensure a sufficient level of confidentiality when handling the participants’ data. The participants’ privacy was upheld, and their data was used only with their consent for scientific purposes.
The unit of measurement in our study is the female population in the Jazan region. We gathered our data by asking these women to complete the online questionnaire. We analyzed the results of 410 participants of reproductive age. The data was analyzed through three processes: firstly, we gave a full description of the data set of numbers, prevalence, frequencies, percentages, and standard error of the sample of variables in the study. Secondly, we tested the distribution of each of the predictor variables among the dependent variables separately by using bivariate analysis (chi-square test) or crosstabs procedure. Thirdly, we used regression analysis to analyze the data, logistic regression for the binary data and multivariate linear regression for continuous data. Finally, alongside using the regression model to study the relationship coefficients and 95% confidence intervals (CIs) were obtained. Stata software, Version 16 (Stata Corp., TX, USA) was used for the data analysis. All tests are two-sided, and a p-value < 0.05 is statistically significant.
The study population comprised 410 female participants, predominantly aged 18–25 years (46.1%), single (50.24%), and Saudi nationals (99.02%) as shown in Table 1. Most participants resided in urban areas (60.49%) and held bachelor’s degrees or higher (81.71%), with nearly half (49.76%) reporting monthly incomes below 5000 Saudi Riyal (SR). Among the participants, physician-confirmed PCOS diagnoses were present in 22.44%, with the most prevalent associated symptoms being hair loss (66.59%), acne (32.20%), and hirsutism (19.02%). Anthropometric measurements indicated that 42.19% of participants were overweight or obese, while 20.24% reported chronic diseases, and 25.12% had a history of miscarriage or infertility. Regarding menstrual patterns, irregularities were reported in 19.27% of participants, with 12.20% experiencing two-month amenorrhea and 7.07% reporting amenorrhea lasting three months or longer. Laboratory-confirmed elevated testosterone levels were present in 5.12% of participants, while documented insulin resistance was reported in 10.73% of the study population.
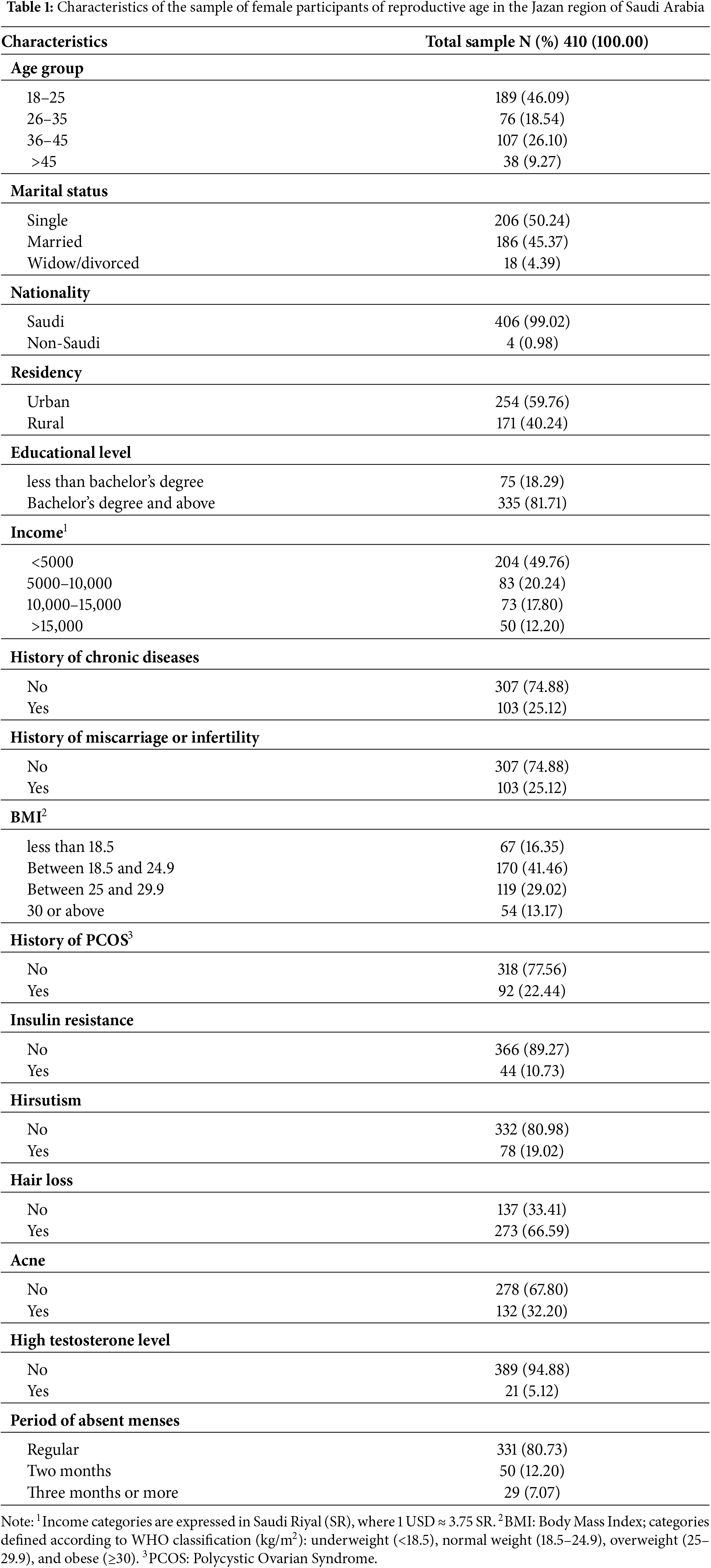
Table 2 presents the distribution of anxiety among participants, revealing several significant associations (p < 0.05). Age analysis showed the highest anxiety prevalence in the 18–25 age group (32.28%). Marital status significantly influenced anxiety levels, with divorced/widowed participants showing the highest prevalence (38.89%), followed by single participants (32.04%). Socioeconomic analysis revealed significantly higher anxiety rates among those with monthly incomes below 5000 SR (36.27%), with notably lower rates in higher income brackets (14.46% for 5000–10,000 SR, 17.81% for 10,000–15,000 SR, and 18.00% for >15,000 SR). PCOS-related manifestations demonstrated strong associations with anxiety: women with PCOS had higher anxiety prevalence (32.61% vs. 22.33%, p = 0.044), with particularly strong associations observed in those with hirsutism (44.87% vs. 19.88%, p < 0.001), hair loss (32.60% vs. 12.76%, p < 0.001), acne (38.64% vs. 17.99%, p < 0.001), and elevated testosterone levels (61.90% vs. 22.62%, p < 0.001). Additionally, insulin resistance showed a significant association with anxiety (45.45% vs. 22.13%, p < 0.001). Menstrual irregularity showed a progressive relationship with anxiety, increasing from 22.66% in those with regular cycles to 40.00% in those with two-month amenorrhea, and 44.83% in those with three or more months of amenorrhea (p = 0.002).
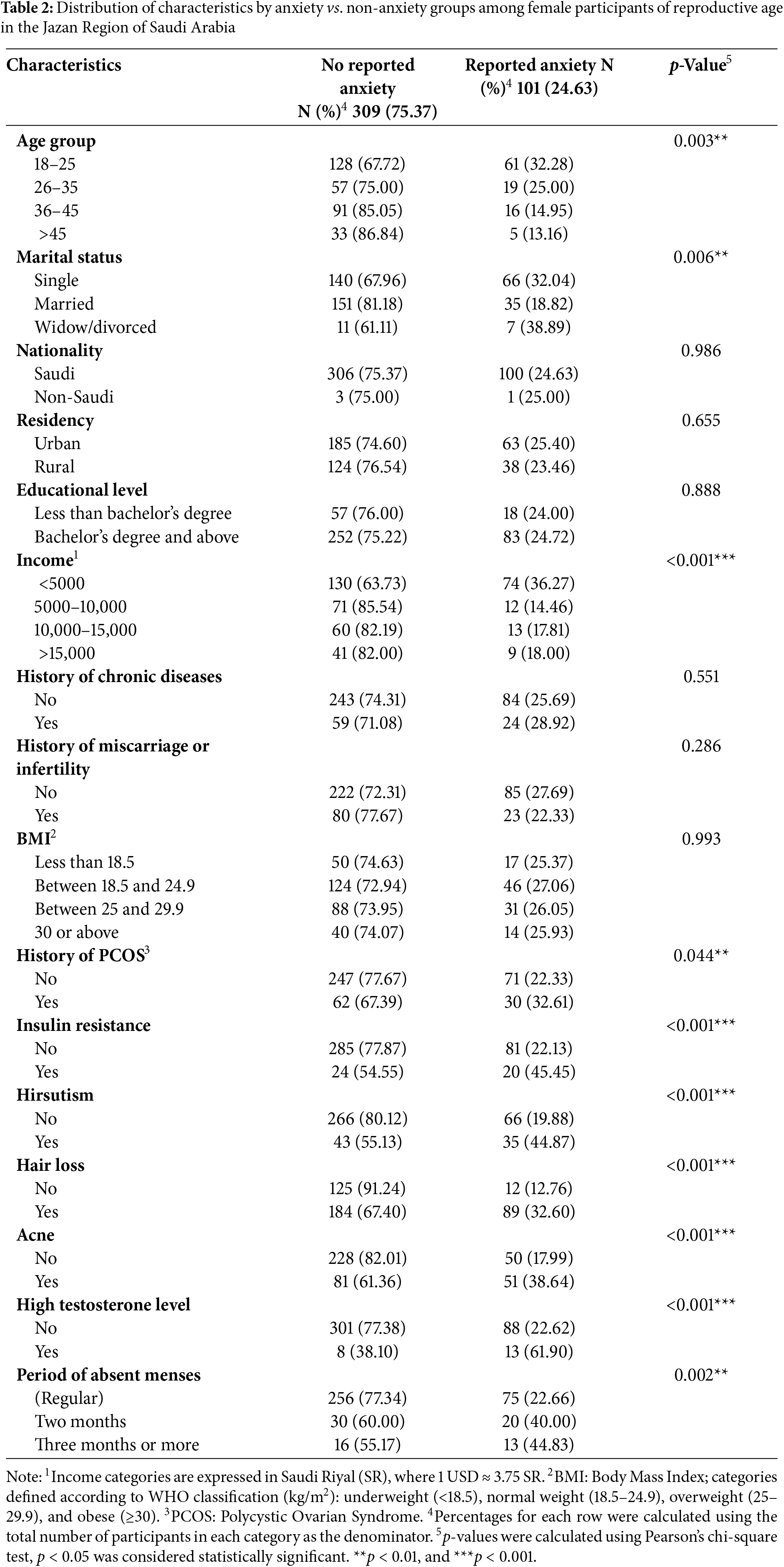
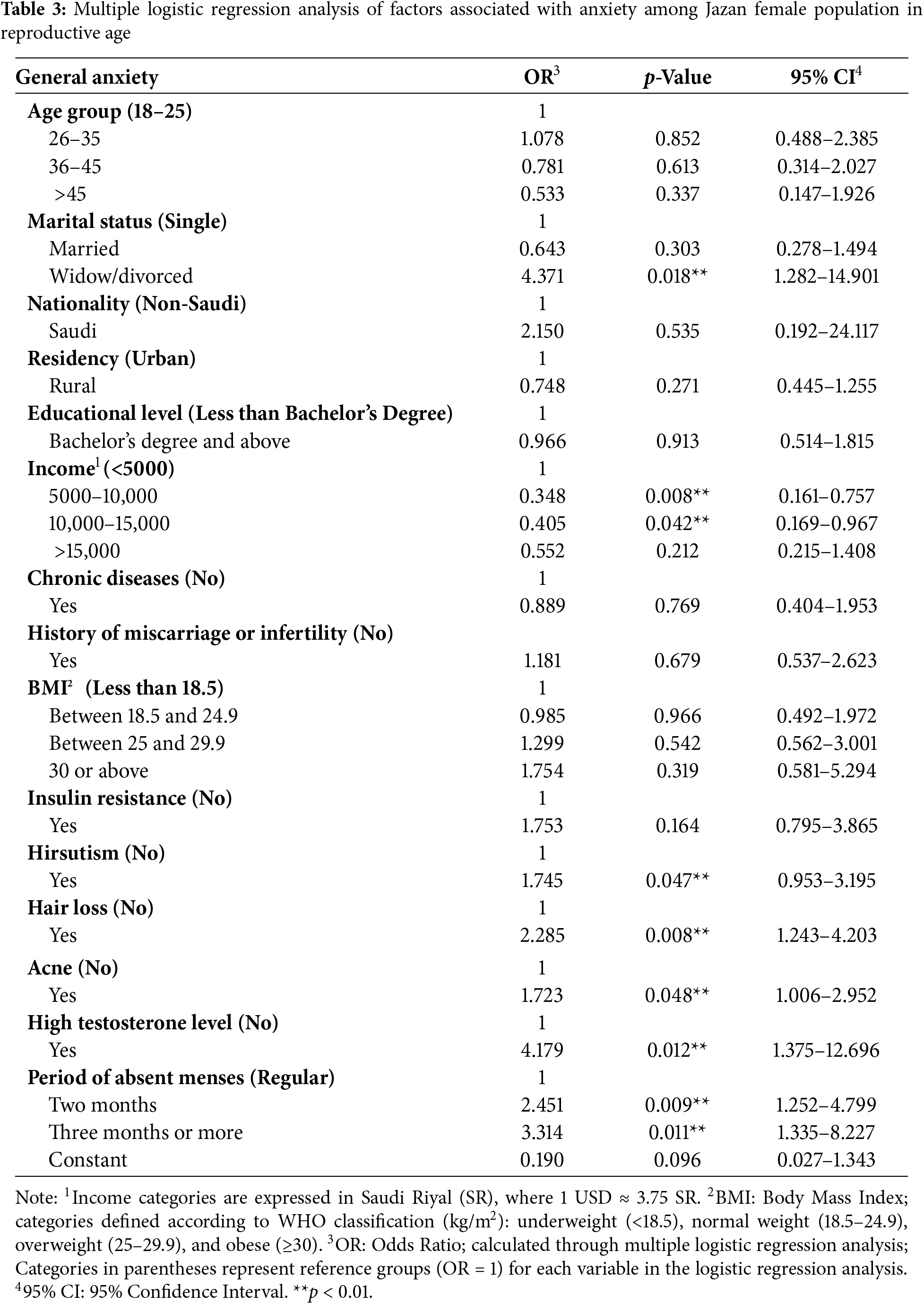
Table 3 presents multiple logistic regression analysis revealing several significant predictors of anxiety among females in the Jazan region. Marital status emerged as a significant factor, with divorced/widowed females showing 4.4-fold higher odds of anxiety compared to single females (OR = 4.371, 95% CI: 1.282–14.901, p = 0.018). Income levels demonstrated an inverse relationship with anxiety, where participants in the 5000–10,000 SR and 10,000–15,000 SR brackets showed significantly reduced anxiety risk (OR = 0.348, p = 0.008; OR = 0.405, p = 0.042, respectively) compared to those earning <5000 SR. Regarding clinical manifestations, PCOS-related manifestations showed strong associations with anxiety: hair loss (OR = 2.285, p = 0.008), hirsutism (OR = 1.745, p = 0.047), and acne (OR = 1.723, p = 0.048) all significantly increased anxiety odds. The highest risk was associated with elevated testosterone levels (OR = 4.179, p = 0.012) while menstrual irregularities showed a progressive increase in anxiety risk, where participants with 2-month and ≥3-month amenorrhea showed significantly higher odds of anxiety (OR = 2.451, p = 0.009; OR = 3.314, p = 0.011, respectively) compared to those with regular cycles.
This cross-sectional study revealed significant associations between PCOS and generalized anxiety disorder among reproductive-age women in Jazan region, with PCOS patients showing markedly higher anxiety prevalence (32.61%) compared to non-PCOS women (22.33%, p = 0.044). This prevalence rate falls within the range reported in the international literature, though with significant regional variations. Our findings are comparable to Indian studies that reported prevalence rates of 15% and 38.6% [18,33], but higher than rates reported in other Gulf countries such as Oman (67% vs. 60%) [34]. The observed prevalence is also lower than findings from Bangladesh (88%) [35], and slightly below a previous Saudi study that reported a 40% prevalence [21]. Recent Saudi studies have documented similar patterns of psychological burden, with a new study from Al-Ahsa reporting that 30.5% of PCOS patients experienced extremely severe depression and 39.2% had extreme anxiety [36]. Additionally, two case-control studies from Riyadh demonstrated significantly higher odds of anxiety in PCOS patients compared to controls (OR = 2.056 and OR = 2.127, respectively) [37,38]. While our results align with the meta-analysis findings from U.S. studies that consistently showed higher anxiety rates in PCOS patients compared to controls [22], the varying prevalence rates likely reflect differences in sociocultural contexts, healthcare systems, and assessment methodologies used across studies. This variation is evident even within Saudi Arabia, where rates of anxiety in PCOS patients range from 32.61% in our Jazan cohort to 65.9%–67.85% in Riyadh studies [37,38], highlighting the importance of considering regional sociocultural factors in psychological assessment and care.
The elevated anxiety risk in PCOS patients may be attributed to both physiological factors and psychosocial stressors, particularly in conservative societies where appearance-related concerns and fertility expectations create an additional psychological burden [25]. These sociocultural influences become especially evident when examining specific demographic and clinical predictors of anxiety in our population.
Our analysis revealed significant associations between psychosocial factors and anxiety risk, with marital status and socioeconomic position emerging as key determinants. Divorced/widowed women demonstrated notably higher anxiety rates (38.89%) compared to married (18.82%) or single women (32.04%, p = 0.006), while lower income (<5000 SR) was significantly associated with increased anxiety risk (36.27%, p < 0.001). These findings align with a recent Eastern Saudi study [36] that reported higher anxiety prevalence among divorced PCOS patients, particularly in conservative regions where divorce carries significant social stigma. The Jazan region’s traditional social fabric, where marriage and fertility are highly valued, may amplify psychological distress among divorced women with PCOS. Similarly, an Omani study [39] attributed elevated anxiety in divorced PCOS patients to social pressure and criticism regarding infertility, often leading to marital discord. The socioeconomic gradient in anxiety risk observed in our study (36.27% in low-income vs. 18.00% in high-income groups) mirrors international trends, with recent meta-analyses reporting 2.5-fold higher anxiety risk among PCOS patients from lower socioeconomic backgrounds [21]. This association likely reflects both reduced access to healthcare resources and increased psychological burden from managing PCOS symptoms with limited financial means, particularly in Jazan’s rural communities, where healthcare access may be constrained. These findings underscore the need for targeted psychological support for vulnerable PCOS patients, especially those facing both social and economic challenges.
Regarding the association between PCOS symptoms (hirsutism, alopecia, acne, and other manifestations) and developing anxiety symptoms, our data showed that women with these symptoms demonstrated higher rates of anxiety compared to those without these clinical features. Regarding our second objective, examining PCOS symptoms and anxiety, our data showed that women with these symptoms had higher anxiety rates. Qualitative research has shown that women with hirsutism report diminished feminine identity, reducing their quality of life [40] Our study found females with hirsutism were 1.7 times more likely to develop anxiety than unaffected females, aligning with previous research that attributes this relationship to anxiety-provoking social encounters and feelings of shame [41]. The continuous self-monitoring of facial hair perpetuates anxiety and can contribute to social phobias [42].
The analysis of appearance-altering PCOS manifestations revealed significant psychological impacts, with alopecia demonstrating a particularly strong association with anxiety (OR = 2.285, 95% CI: 1.243–4.203, p = 0.008). This relationship remained robust after adjusting for demographic and clinical variables, suggesting an independent contribution to psychological distress. This finding aligns with US and Indian studies reporting associations between hair loss and increased anxiety in PCOS patients [18,43], demonstrating similar associations (OR = 2.1, 95% CI: 1.8–2.5). The psychological burden of alopecia appears particularly pronounced in cultural contexts where feminine identity is closely tied to hair appearance [44]. Similarly, our analysis identified acne as an independent predictor of anxiety (OR = 1.723, 95% CI: 1.006–2.952, p = 0.048), with affected individuals showing significantly higher anxiety prevalence compared to those without acne. This association aligns with recent systematic reviews [40,45] and regional studies [46] that consistently demonstrate the psychological impact of PCOS-related dermatological manifestations. Barry et al. [46] proposed a comprehensive model explaining these associations, where appearance-related symptoms trigger a cascade of psychological responses, including diminished self-esteem, increased social anxiety, and body image dissatisfaction, particularly in societies with a strong emphasis on physical appearance.
Analysis of endocrine parameters revealed a striking association between elevated testosterone levels and anxiety risk in our cohort (OR = 4.179, 95% CI: 1.375–12.696, p = 0.012). This robust relationship suggests that women with biochemically confirmed hyperandrogenism experience significantly higher rates of anxiety compared to those with normal testosterone levels (61.90% vs. 22.62%, p < 0.001). These findings align with recent meta-analyses [43] showing similar associations in PCOS populations (pooled OR = 3.82, 95% CI: 2.14–6.81) and observations in the general female population [47,48]. The biological plausibility of this association is supported by emerging neurobiological evidence suggesting that androgens modulate anxiety-related neural circuits through both genomic and non-genomic pathways [48]. Furthermore, the hyperandrogenic state in PCOS is associated with increased sympathetic tone, potentially amplifying anxiety susceptibility through autonomic dysregulation [49]. While two Turkish studies reported contrasting results [50,51], these discrepancies likely reflect methodological heterogeneity rather than true biological differences, as these studies were limited by small sample sizes (n < 100), lack of matched controls, and variations in testosterone measurement techniques [51]. Our findings contribute to the growing body of evidence supporting the role of androgens in anxiety pathogenesis, particularly in PCOS populations.
Menstrual irregularity emerged as a significant predictor of anxiety in our PCOS cohort, demonstrating a dose-dependent relationship with symptom severity. Women experiencing two-month amenorrhea showed significantly increased anxiety risk (OR = 2.451, 95% CI: 1.252–4.799, p = 0.009), while those with prolonged amenorrhea (≥3 months) demonstrated even higher odds (OR = 3.314, 95% CI: 1.335–8.227, p = 0.011) compared to those with regular cycles [18]. This progressive association suggests that the chronicity of menstrual dysfunction may play a crucial role in anxiety development. Recent meta-analyses have reported similar patterns, with longer durations of amenorrhea correlating with increased psychological distress (pooled effect size = 0.42, p < 0.001) [20]. The relationship between menstrual irregularity and anxiety appears particularly pronounced in Gulf region populations, where fertility concerns carry significant sociocultural implications [20]. A comprehensive review of Gulf Cooperation Council countries revealed comparable associations between menstrual dysfunction and anxiety disorders (OR range: 2.1–3.8), suggesting that shared cultural values and healthcare systems may influence the psychological impact of PCOS manifestations in this region.
Our findings underscore the importance of integrating psychological care into standardized PCOS management protocols, given the high prevalence of anxiety symptoms (32.61%) in our cohort. In alignment with Saudi Arabia’s Vision 2030 healthcare transformation agenda [52,53], we propose key policies for improved care delivery: mandatory GAD-7 screening during PCOS diagnosis and follow-ups, particularly for patients with multiple phenotypic manifestations; establishment of specialized PCOS clinics combining endocrine, gynecological, and mental health services; and mandatory mental health competency training for healthcare providers. This comprehensive model emphasizes both clinician education and patient psychoeducation regarding the bidirectional relationship between PCOS symptoms and psychological well-being [54].
For future research, we recommend investigating how cultural expectations and fertility pressures impact anxiety levels among women with PCOS in the Jazan region. Prospective cohort studies should focus on establishing temporal relationships between PCOS manifestations and anxiety development [55]. Additionally, randomized controlled trials evaluating integrated treatment approaches are needed to determine optimal strategies for addressing both endocrine and psychological aspects of PCOS.
Several methodological constraints warrant careful interpretation of our findings. First, while online survey methodology enabled a broad geographical reach, potential selection bias may exist due to differential internet accessibility across socioeconomic strata. This digital divide could especially affect representation from rural regions, where internet penetration remains variable. Second, the convenience sampling strategy, although following standardized protocols, introduces limitations as it may not be representative of the target population. This non-probability sampling method can limit the generalizability of research findings since participants are selected based on ease of access rather than random selection, potentially overrepresenting individuals with higher health literacy and psychological awareness. Third, the cross-sectional design inherently limits causal inference regarding the temporal relationship between PCOS manifestations and anxiety development. Additionally, the reliance on self-reported symptoms, although validated through standardized instruments (GAD-7), may be affected by recall bias. Future longitudinal studies with probability-based sampling methods and objective clinical assessments would address these limitations.
This study identified biochemical hyperandrogenism as the strongest predictor of anxiety risk in Saudi women with PCOS, underscoring the need for greater awareness and proactive screening for mental health issues in patients presenting with androgenic manifestations. Longitudinal research is warranted to elucidate temporal relationships between specific PCOS features and anxiety onset. Randomized controlled trials are recommended to evaluate integrated treatment protocols addressing both hormonal and psychological aspects of PCOS. The significant associations between endocrine dysfunction and anxiety prevalence shown here highlight the necessity of incorporating routine psychological assessment and management into standard PCOS care to improve both physical and mental health outcomes in this high-risk population. These locally relevant findings can inform regional clinical practice transformation efforts aimed at providing holistic PCOS care.
Acknowledgement: We would like to thank the participants who contributed their time and informationto this study. Special thanks to the medical staff at Jazan University for their support during data collection.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: Abdullah A. Alharbi; data collection: Fatimah H. Al Ghazwi, Seba Y. Muzaiiadi, Joud N. Refaei, Revan A. Arishi, Bashaer A. Al Rajhi, Fatima A. Aqili, Saleha M. Ayoub; analysis and interpretation of results: Abdullah A. Alharbi, Ahmad Y. Alqassim, Mohammed A. Muaddi, Mohammad A. Jareebi; draft manuscript preparation: Abdullah A. Alharbi, Ahmad A. Alharbi, Nada M. Makein. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data that support the findings of this study are available from the corresponding author, Ahmad Y. Alqassim, upon reasonable request.
Ethics Approval: This study was approved by the Standing Committee for Scientific Research at Jazan University (Reference No. REC-44/06/458) on 02 January 2022, under the protocol number HAPO-10-Z-001. The study was conducted in accordance with the Declaration of Helsinki. All participants provided informed consent before participation.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
References
1. WHO. Polycystic ovary syndrome [cited 2025 Apr 1]. Available from: https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome. [Google Scholar]
2. Cussons AJ, Stuckey BGA, Walsh JP, Burke V, Norman RJ. Polycystic ovarian syndrome: marked differences between endocrinologists and gynaecologists in diagnosis and management. Clin Endocrinol. 2005;62(3):289–95. doi:10.1111/j.1365-2265.2004.02208.x. [Google Scholar] [PubMed] [CrossRef]
3. Balen A, Michelmore K. What is polycystic ovary syndrome? Are national views important? Hum Reprod. 2002;17(9):2219–27. doi:10.1093/humrep/17.9.2219. [Google Scholar] [PubMed] [CrossRef]
4. Moran L, Gibson-Helm M, Teede H, Deeks A. Polycystic ovary syndrome: a biopsychosocial understanding in young women to improve knowledge and treatment options. J Psychosom Obstet Gynaecol. 2010;31(1):24–31. doi:10.3109/01674820903477593. [Google Scholar] [PubMed] [CrossRef]
5. Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010;8:41. doi:10.1186/1741-7015-8-41. [Google Scholar] [PubMed] [CrossRef]
6. The Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004;19(1):41–7. doi:10.1093/humrep/deh098. [Google Scholar] [PubMed] [CrossRef]
7. Motlagh AK, Nejadghaderi SA, Alizadeh M, Sanaie S, Sullman MJM, Kolahi AA, et al. Burden of polycystic ovary syndrome in the Middle East and North Africa region, 1990–2019. Sci Rep. 2022;12(1):7039. doi:10.1038/s41598-022-11006-0. [Google Scholar] [PubMed] [CrossRef]
8. Chiaffarino F, Cipriani S, Dalmartello M, Ricci E, Esposito G, Fedele F, et al. Prevalence of polycystic ovary syndrome in European countries and USA: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2022;279:159–70. doi:10.1016/j.ejogrb.2022.10.020. [Google Scholar] [PubMed] [CrossRef]
9. Yu O, Christ JP, Schulze-Rath R, Covey J, Kelley A, Grafton J, et al. Incidence, prevalence, and trends in polycystic ovary syndrome diagnosis: a United States population-based study from 2006 to 2019. Am J Obstet Gynecol. 2023;229(1):39.e1–12. doi:10.1016/j.ajog.2023.04.010. [Google Scholar] [PubMed] [CrossRef]
10. Guraya SS. Prevalence and ultrasound features of polycystic ovaries in young unmarried Saudi females. J Microsc Ultrastruct. 2013;1(1–2):30–4. doi:10.1016/j.jmau.2013.06.002. [Google Scholar] [CrossRef]
11. Alraddadi SM, Borzangi KA, Almuher EM, Albaik AF, Aljawad LA, Shaqroon AA, et al. Prevalence of poly-cystic ovarian syndrome with associated risk factors and impact on well-being among women in reproductive aged (18–45) years in Al-Madinah 2017. World J Pharm Res. 2018;7(4):231–47. [Google Scholar]
12. Neyazi A, Padhi BK, Mohammadi AQ, Ahmadi M, Erfan A, Bashiri B, et al. Depression, anxiety and quality of life of Afghan women living in urban areas under the Taliban government: a cross-sectional study. BMJ Open. 2023;13(8):e071939. doi:10.1136/bmjopen-2023-071939. [Google Scholar] [PubMed] [CrossRef]
13. Neyazi A, Mohammadi AQ, Razaqi N, Rahimi BA, Sifat S, Rahimy N, et al. Health survey on anxiety, depression, and stress in Afghanistan: a large-scale cross-sectional study amid ongoing challenges. Discov Ment Health. 2024;4(1):38. doi:10.1007/s44192-024-00090-5. [Google Scholar] [PubMed] [CrossRef]
14. Almalki SA, Ashdown BK. Women’s access to healthcare services in the Jazan region of the KSA. J Taibah Univ Med Sci. 2024;19(4):766–74. doi:10.1016/j.jtumed.2024.07.001. [Google Scholar] [PubMed] [CrossRef]
15. Almhmoud H, Alatassi L, Baddoura M, Sandouk J, Alkayali MZ, Najjar H, et al. Polycystic ovary syndrome and its multidimensional impacts on women’s mental health: a narrative review. Medicine. 2024;103(25):e38647. doi:10.1097/MD.0000000000038647. [Google Scholar] [PubMed] [CrossRef]
16. Begum RF, Vellapandian C, Mohan S. Examining symptom and quality of life in polycystic ovarian syndrome: a web-based cross-sectional study. Future Sci OA. 2024;10(1):2430878. doi:10.1080/20565623.2024.2430878. [Google Scholar] [PubMed] [CrossRef]
17. Stańczak NA, Grywalska E, Dudzińska E. The latest reports and treatment methods on polycystic ovary syndrome. Ann Med. 2024;56(1):2357737. doi:10.1080/07853890.2024.2357737. [Google Scholar] [PubMed] [CrossRef]
18. Chaudhari AP, Mazumdar K, Mehta PD. Anxiety, depression, and quality of life in women with polycystic ovarian syndrome. Indian J Psychol Med. 2018;40(3):239–46. doi:10.4103/IJPSYM.IJPSYM_561_17. [Google Scholar] [PubMed] [CrossRef]
19. Yin X, Ji Y, Chan CLW, Chan CHY. The mental health of women with polycystic ovary syndrome: a systematic review and meta-analysis. Arch Womens Ment Health. 2021;24(1):11–27. doi:10.1007/s00737-020-01043-x. [Google Scholar] [PubMed] [CrossRef]
20. Asdaq SMB, Jomah S, Hasan R, Al-Baroudi D, Alharbi M, Alsubaie S, et al. Impact of polycystic ovary syndrome on eating behavior, depression and health related quality of life: a cross-sectional study in Riyadh. Saudi J Biol Sci. 2020;27(12):3342–7. doi:10.1016/j.sjbs.2020.08.039. [Google Scholar] [PubMed] [CrossRef]
21. Almeshari WK, Alsubaie AK, Alanazi RI, Almalki YA, Masud N, Mahmoud SH. Depressive and anxiety symptom assessment in adults with polycystic ovarian syndrome. Depress Res Treat. 2021;2021:6652133. doi:10.1155/2021/6652133. [Google Scholar] [PubMed] [CrossRef]
22. Dokras A, Clifton S, Futterweit W, Wild R. Increased prevalence of anxiety symptoms in women with polycystic ovary syndrome: systematic review and meta-analysis. Fertil Steril. 2012;97(1):225–30.e2. doi:10.1016/j.fertnstert.2011.10.022. [Google Scholar] [PubMed] [CrossRef]
23. Azhar A, Abid F, Rehman R. Polycystic ovary syndrome, subfertility and vitamin D deficiency. J Coll Physicians Surg Pak. 2020;30(5):545–6. doi:10.29271/jcpsp.2020.05.545. [Google Scholar] [PubMed] [CrossRef]
24. Mushtaq A, Bibi A, Kausar N. Increased risk of infertility, marital maladjustment and psychological morbidity in PCOS patients of southern punjab, Pakistan. Pakistan J Zool. 2023;55(4):1501–2000. doi:10.17582/journal.pjz/20210919130943. [Google Scholar] [CrossRef]
25. Nasiri AF, Ramezani TF, Simbar M, Montazeri A, Mohammadpour TRA. The experience of women affected by polycystic ovary syndrome: a qualitative study from Iran. Int J Endocrinol Metab. 2014;12(2):e13612. doi:10.5812/ijem.13612. [Google Scholar] [PubMed] [CrossRef]
26. Statista [Internet]. Social media usage in Saudi Arabia—statistics & facts. [cited 2025 Apr 1]. Available from: https://www.statista.com/topics/9947/social-media-usage-in-saudi-arabia/#topicOverview. [Google Scholar]
27. Stojcic I, Dong X, Ren X. Body image and sociocultural predictors of body image dissatisfaction in Croatian and Chinese women. Front Psychol. 2020;11:731. doi:10.3389/fpsyg.2020.00731. [Google Scholar] [PubMed] [CrossRef]
28. Azizi KM, Amirjani S, Asemi Z, Taghavi SA, Allan H, Kamalnadian SN, et al. The impact of depression, self-esteem, and body image on sleep quality in patients with PCOS: a cross-sectional study. Sleep Breath. 2020;24(3):1027–34. doi:10.1007/s11325-019-01946-9. [Google Scholar] [PubMed] [CrossRef]
29. Statistics GAf [Internet]. Saudi Census 2022. [cited 2025 Apr 1]. Available from: https://portal.saudicensus.sa/portal/public/1/15/101464?type=TABLE. [Google Scholar]
30. AlHadi AN, AlAteeq DA, Al-Sharif E, Bawazeer HM, Alanazi H, AlShomrani AT, et al. An Arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. Ann Gen Psychiatry. 2017;16:32. doi:10.1186/s12991-017-0155-1. [Google Scholar] [PubMed] [CrossRef]
31. Alhalafi AH. Prevalence of anxiety and depression during the coronavirus disease 2019 pandemic in Riyadh, Saudi Arabia: a web-based cross-sectional survey. J Pharm Res Int. 2020:65–73. doi:10.9734/jpri/2020/v32i2730857. [Google Scholar] [CrossRef]
32. Alharbi AA, Alqassim AY, Muaddi MA, Makeen AM, Hagawi AM, Shaabi LA, et al. Generalized anxiety disorder symptoms during COVID-19 pandemic in Jazan, Saudi Arabia. Heliyon. 2022;8(5):e09424. doi:10.1016/j.heliyon.2022.e09424. [Google Scholar] [PubMed] [CrossRef]
33. Hussain A, Chandel RK, Ganie MA, Dar MA, Rather YH, Wani ZA, et al. Prevalence of psychiatric disorders in patients with a diagnosis of polycystic ovary syndrome in Kashmir. Indian J Psychol Med. 2015;37(1):66–70. doi:10.4103/0253-7176.150822. [Google Scholar] [PubMed] [CrossRef]
34. Sulaiman MA, Al-Farsi YM, Al-Khaduri MM, Waly MI, Saleh J, Al-Adawi S. Psychological burden among women with polycystic ovarian syndrome in Oman: a case-control study. Int J Womens Health. 2017;9:897–904. doi:10.2147/IJWH.S145383. [Google Scholar] [PubMed] [CrossRef]
35. Hasan M, Sultana S, Sohan M, Parvin S, Rahman MA, Hossain MJ, et al. Prevalence and associated risk factors for mental health problems among patients with polycystic ovary syndrome in Bangladesh: a nationwide cross-Sectional study. PLoS One. 2022;17(6):e0270102. doi:10.1371/journal.pone.0270102. [Google Scholar] [PubMed] [CrossRef]
36. Alnaeem L, Alnasser M, AlAli Y, Almarri F, Al Sultan AA, Almuhaysin FA, et al. Depression and anxiety in patients with polycystic ovary syndrome: a cross-sectional study in Saudi Arabia. Cureus. 2024;16(1):e51530. doi:10.7759/cureus.51530. [Google Scholar] [PubMed] [CrossRef]
37. Asdaq SMB, Yasmin F. Risk of psychological burden in polycystic ovary syndrome: a case control study in Riyadh, Saudi Arabia. J Affect Disord. 2020;274:205–9. doi:10.1016/j.jad.2020.05.086. [Google Scholar] [PubMed] [CrossRef]
38. Alamri AS, Alhomrani M, Alsanie WF, Almuqbil M, Alqarni KM, Alshehri SM, et al. Role of polycystic ovarian syndrome in developing psychological burden in Saudi Arabian females: a case control study. Front Public Health. 2022;10:999813. doi:10.3389/fpubh.2022.999813. [Google Scholar] [PubMed] [CrossRef]
39. ALSumri H, Szatkowski L, Gibson J, Fiaschi L, Bains M. Psychosocial impacts of infertility among Omani women with polycystic ovarian syndrome: a qualitative study. Int J Fertil Steril. 2023;17(2):107–14. doi:10.22074/ijfs.2022.550111.1310. [Google Scholar] [PubMed] [CrossRef]
40. Farideh ZZ, Mohammad MN, Nasrin A, Fedyeh H, Davoud H. Psychological signs in patients with polycystic ovary syndrome. J Fam Reprod Health. 2012;6(4):145–51. [Google Scholar]
41. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Washington, DC, USA: American Psychiatric Association; 2013. [Google Scholar]
42. Lipton MG, Sherr L, Elford J, Rustin MHA, Clayton WJ. Women living with facial hair: the psychological and behavioral burden. J Psychosom Res. 2006;61(2):161–8. doi:10.1016/j.jpsychores.2006.01.016. [Google Scholar] [PubMed] [CrossRef]
43. Cooney LG, Lee I, Sammel MD, Dokras A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2017;32(5):1075–91. doi:10.1093/humrep/dex044. [Google Scholar] [PubMed] [CrossRef]
44. Bazarganipour F, Ziaei S, Montazeri A, Foroozanfard F, Kazemnejad A, Faghihzadeh S. Psychological investigation in patients with polycystic ovary syndrome. Health Qual Life Outcomes. 2013;11:141. doi:10.1186/1477-7525-11-141. [Google Scholar] [PubMed] [CrossRef]
45. Molla A, Alrizqi H, Alharbi E, Alsubhi A, Alrizqi S, Shahada O. Assessment of anxiety and depression in patients with acne vulgaris in Medina: a case-control study. Clin Cosmet Investig Dermatol. 2021;14:999–1007. doi:10.2147/CCID.S302311. [Google Scholar] [PubMed] [CrossRef]
46. Barry JA, Hardiman PJ, Saxby BK, Kuczmierczyk A. Testosterone and mood dysfunction in women with polycystic ovarian syndrome compared to subfertile controls. J Psychosom Obstet Gynaecol. 2011;32(2):104–11. doi:10.3109/0167482X.2011.568129. [Google Scholar] [PubMed] [CrossRef]
47. Donbaloğlu Z, Tuhan H, Çoban Ö.G, Kızılay DÖ., İsmailoğlu E, Önder A, et al. Hyperandrogenism correlates with psychological symptoms in adolescents with polycystic ovary syndrome. Clin Pediatr Endocrinol. 2022;31(2):68–76. doi:10.1297/cpe.2022-0010. [Google Scholar] [PubMed] [CrossRef]
48. Stanikova D, Luck T, Pabst A, Bae YJ, Hinz A, Glaesmer H, et al. Associations between anxiety, body mass index, and sex hormones in women. Front Psychiatry. 2019;10:479. doi:10.3389/fpsyt.2019.00479. [Google Scholar] [PubMed] [CrossRef]
49. Kirthika SV, Paul J, Sudhakar S, Selvam PS, Priya VS. Correlation between hormonal level and depression in subjects with polycystic ovarian syndrome. Drug Invent Today. 2019;12(3):393. [Google Scholar]
50. Besenek M, Gurlek B. Hyperandrogenism in polycystic ovary syndrome affects psychological well-being of adolescents. J Obstet Gynaecol Res. 2021;47(1):137–46. doi:10.1111/jog.14444. [Google Scholar] [PubMed] [CrossRef]
51. Annagür BB, Tazegül A, Uguz F, Kerimoglu ÖS, Tekinarslan E, Celik Ç. Biological correlates of major depression and generalized anxiety disorder in women with polycystic ovary syndrome. J Psychosom Res. 2013;74(3):244–7. doi:10.1016/j.jpsychores.2013.01.002. [Google Scholar] [PubMed] [CrossRef]
52. Saudi Ministry of Health (MOH). Healthcare Transformation Strategy. Department: Vision Realization Office (VRO). 2016. [cited 2025 Apr 1]. p. 1–64. Available from: https://www.moh.gov.sa/en/Ministry/vro/Documents/Healthcare-Transformation-Strategy.pdf. [Google Scholar]
53. Mani ZA, Goniewicz K. Transforming healthcare in Saudi Arabia: a comprehensive evaluation of vision 2030’s impact. Sustainability. 2024;16(8):3277. doi:10.3390/su16083277. [Google Scholar] [CrossRef]
54. Brutocao C, Zaiem F, Alsawas M, Morrow AS, Murad MH, Javed A. Psychiatric disorders in women with polycystic ovary syndrome: a systematic review and meta-analysis. Endocrine. 2018;62(2):318–25. doi:10.1007/s12020-018-1692-3. [Google Scholar] [PubMed] [CrossRef]
55. Dokras A, Stener-Victorin E, Yildiz BO, Li R, Ottey S, Shah D, et al. Androgen excess-polycystic ovary syndrome society: position statement on depression, anxiety, quality of life, and eating disorders in polycystic ovary syndrome. Fertil Steril. 2018;109(5):888–99. doi:10.1016/j.fertnstert.2018.01.038. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools