 Open Access
Open Access
ARTICLE
Longitudinal Associations of Loneliness with Mental and Physical Health in Ageing Adults in South Africa
1 Department of Health Education and Behavioral Sciences, Faculty of Public Health, Mahidol University, Bangkok, 10400, Thailand
2 Department of Psychology, University of the Free State, Bloemfontein, 9300, South Africa
3 Department of Psychology, College of Medical and Health Science, Asia University, Taichung, 41354, Taiwan
* Corresponding Author: Karl Peltzer. Email:
International Journal of Mental Health Promotion 2025, 27(5), 625-635. https://doi.org/10.32604/ijmhp.2025.063801
Received 24 January 2025; Accepted 30 April 2025; Issue published 05 June 2025
Abstract
Objectives: Few studies have investigated longitudinal associations of loneliness with health outcomes in Africa. This study aimed to assess the longitudinal associations between loneliness and mental and physical health among aging adults in South Africa. Methods: Data from the 7-year longitudinal Health and Ageing in Africa (HAALSI) study conducted in South Africa were used in the analysis (analytic sample: n = 3707, aged 40 years and older). Loneliness was measured with one question. Longitudinal relationships between loneliness and each health outcome were estimated using Generalized Estimating Equations analysis (GEE), hazard ratios (HRs) (95% CI) were used to determine the relationship between loneliness and 7-year mortality in the entire sample, and correlations between incident health outcomes and loneliness were evaluated using logistic regressions. Results: The prevalence of loneliness was 12.1% in 2015, 16.9% in 2019, and 16.3% in 2022. Multivariable analysis showed that loneliness was positively associated with the prevalence and/or incidence of four poor mental health indicators (e.g., poor sleep quality,AOR = 1.53, 95% CI: 1.30–1.80), four physical ill-health indicators (e.g., incident kidney disease, AOR = 2.50, 95% CI: 1.41–4.42), mortality (Hazard Ratio = 1.20, 95% CI = 1.04–1.39), and three poor behavioral health indicators (e.g., current tobacco use, AOR = 1.21, 95% CI = 1.04–1.42). Conclusion: The study discovered that several outcomes related to mental, physical, and behavioral health were associated with loneliness. Enhancing the detection and management of loneliness could lower mental and physical illness in aging adults in South Africa.Keywords
Loneliness is prevalent in all populations, including those who are older adults [1]. In higher resourced countries, 28.5% of older adults reported loneliness [1], while lower or similar proportions were shown in lower resourced countries, e.g., ranging from 9.9% in South Africa [2], 21.7% in Thailand [3] to 33.8% in India [4]. Numerous detrimental health effects have been linked to loneliness [5]. For instance, loneliness has been found associated with poor mental health, such as mental health symptoms [6], depression [7], anxiety [8], poor life satisfaction [9], sleep problems [10], and poor cognitive function [11]. Associations of loneliness with poor physical health include cardiovascular disease [12], diabetes [13], hypertension [14], functional disability [13], poor perceived health status [13], and mortality [15]. Moreover, current tobacco use [10], problem alcohol use [16], food insecurity [17], underweight [9], and obesity [18] are behavioural risk factors that have been linked to loneliness.
Most research on loneliness and its negative effects on the health of older people is conducted in wealthier countries; however, there is a dearth of longitudinal data on these connections in African countries such as South Africa. Therefore, from 2015 to 2022, the study’s goal was to assess the long-term connections between loneliness and the behavioral, mental, and physical health outcomes of older South Africans.
The longitudinal data from three consecutive waves (2015, 2019, and 2022) of the “Health and Ageing in Africa: A Longitudinal Study of an The International Network for the Demographic Evaluation of Populations and Their Health (INDEPTH) Community in South Africa (HAALSI)” in the “INDEPTH Health and Demographic Surveillance System site of Agincourt” were analyzed [19]. Of 5059 participants at baseline, 1114 died, 185 refused, 42 were not found, and 11 were incomplete, leaving an analytic sample of 3707 participants with complete measurements at all 3 waves. The study protocol “Health and Aging in Africa: A Longitudinal Study in South Africa (HAALSI)” was approved by the “University of the Witwatersrand Human Research Ethics Committee (Ref. M141159), the Harvard T.H. Chan School of Public Health, Office of Human Research Administration (Ref. C13–1608–02), and the Mpumalanga Provincial Research and Ethics Committee”. Participants gave written informed consent.
In wave 1 of the CES-D-8, the Center for Epidemiologic Studies Depression (CES-D) Scale item “Much of the time in the past week, you felt lonely” (Yes/No) was used to assess loneliness, and in waves 2 and 3 the CES-D-20 item “In the past week, how often did you experience feeling lonely?” defined as “almost always (5–7 days), often (3–4 days) or sometimes (1–2 days) = 1” and “very rarely (less than one day) or none” = 0 [20].
Mental Health Outcomes
Depressive mood was assessed the CES-D-8 item in waves 1 “Much of the time in the past week, you felt depressed.” (Yes/No) and the CES-D-20 item in waves 2 and 3, “In the past week, how often did you feel depressed?” defined as “almost always (5–7 days), often (3–4 days) or sometimes (1–2 days)” = 1 and “very rarely (less than one day) or none” = 0 [20].
The question “All things considered, how satisfied are you with your life as a whole these days?” was the source of poor life satisfaction (scores < 7). On a scale of 0 to 10, 10 represents satisfaction, and 0 represents dissatisfaction.
The following question was used to determine poor sleep quality (defined as “very bad, or fairly bad” = 1 and “fairly good, or very good” = 0): “Over the past 4 weeks, how would you evaluate your sleep quality overall? Would you say it is very good, fairly good, fairly bad, or very bad?” [21].
Symptoms of post-traumatic stress disorder (PTSD) were measured using a “7-item PTSD symptom scale” and PTSD was “defined as ≥4 scores” [22].
Using a brief cognitive function assessment that was adapted from the US Health and Retirement Study, cognitive impairment was calculated as the 10th percentile of the total score in each study wave. The first trial in waves 2 and 3 of the test covered “episodic memory (immediate and delayed recall of a 10-word list)” (0–20 points) and four items on orientation (0–4) [23].
Physical Health Consequences
“Bad or very bad” (as opposed to “very good, good, or moderate”) was the definition of poor self-rated health state. Diabetes was “classified with fasting glucose (defined as >8 h without eating) >7 mmol/L(126 mg/dL) or non-fasting glucose level >11.0 mmol/L (200 mg/dL); reported ever being diagnosed with diabetes; or if use of medication is reported at the time of interview” [19]. Cardiovascular disease (angina, heart attack, stroke, and/or heart failure) and kidney disease were evaluated using a self-reported diagnostic [19]. Hypertension was defined as follows: “if systolic blood pressure was greater than or equal to 140 mmHg or diastolic blood pressure was 90 mmHg or higher, or if the use of antihypertensive medication was reported at the time of the interview” [19]. Having trouble with “bathing, dressing, eating, getting in/out of bed, using the toilet, or walking” is referred to as an Activities of Daily Living (ADL) disability [24].
Lifestyle Outcomes
Present-day tobacco use was assessed with questions on “smokeless tobacco and/or smoking” [19]. Heavy alcohol use “such as beer, wine, spirits, fermented cider, thothotho, or traditional beer” was classified as past 12-month intake of “6 or more drinks in a single morning, afternoon, or night” (“one drink should be considered equal to 1 shot or 1 tot of a strong alcoholic drink like spirits, or 1 full glass of a light alcoholic drink like beer.”) [25].
Food insecurity was defined in wave 1 as any past year (3 items) food insecurity and in waves 2 and 3 as any past month (3–5 items) food insecurity, e.g., “In the past month, were you hungry but didn’t eat because you couldn’t afford enough food?” [23,25].
According to WHO criteria (underweight: <18.5 kg/m2 and obesity: ≥30 kg/m2), the measured Body Mass Index (BMI) was classified [26].
Mortality
Survival and exposure to death are used to calculate mortality. The question of whether the interviewee perished in the 2015 wave or lived through the 2017 and 2020 waves was used to gauge their survival status.
The study’s covariates included the following: sex (male or female), age group (40–59 and 60 years or older), education (“none or 0 years = 1 and any educational level or 1 or more years = 0”), household size (alone = 1 and ≥2 = 0), country of origin (“South Africa = 1 and Mozambique or others = 0”), marital status (“widowed = 1, and currently married or living with partner, divorced or separated/deserted, or single or never married = 0”), and wealth status based on household assets (“low = lowest, low or middle = 1and high = high or highest = 0”) [19,23].
The three study waves’ changes in sample proportions were evaluated using chi-square testing. Initially, longitudinal relationships between loneliness and each health outcome at waves 1, 2, and 3 (unadjusted and adjusted [if significant in unadjusted analysis] for social and health determinants) were estimated using Generalized Estimating Equations analysis (GEE). Second, hazard ratios (HRs) (95% CI) were used to determine the relationship between loneliness and 7-year mortality in the entire sample. Third, correlations between incident health outcomes (in wave 2 and/or wave 3 and not having the condition at baseline) and loneliness were evaluated using logistic regressions.
Inverse likelihood of censoring weights that jointly accounted for the probabilities of study drop-out and mortality over the follow-up period were created using the probabilities of mortality in the whole baseline sample and drop-out among the surviving baseline sample. These weights were included in every model. Covariates included previously identified variables, such as living alone [27], widowhood, sex, education, wealth status, and mental, physical, and behavioural health indicators [5,7,14,15,28]. Based on the statistics of Variation Inflation Factors (VIFs), collinearity was not found. For statistical computations, StataSE 15.0 (College Station, TX, USA) was used; p < 0.05 was regarded as significant, and missing values were deleted (mostly because of proxy respondents).
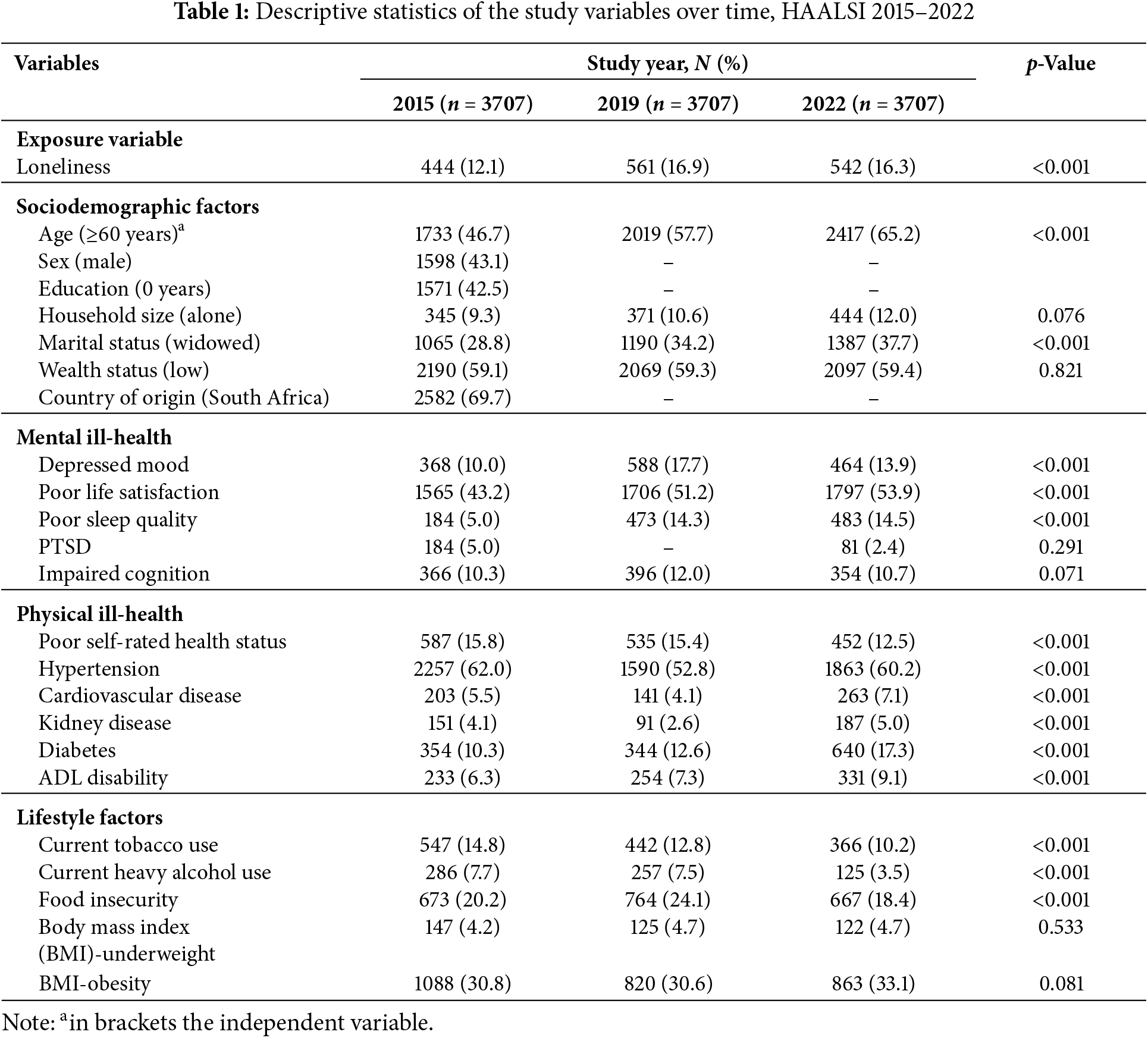
Participants’ descriptives across the three study waves (2015, 2019, and 2022) are found in Table 1. The prevalence of widows increased from 28.8% in 2015 to 37.7% in 2022. The prevalence of loneliness was 12.1% in 2015, 16.9% in 2019, and 16.3% in 2022. Significant differences were found for poor sleep quality, poor life satisfaction and depressed mood, and three lifestyle factors. The prevalence of diabetes, ADL disability, cardiovascular disease, and kidney disease significantly increased, and poor self-rated health and hypertension decreased from 2015 to 2022 (see Table 1).
3.1 Loneliness and Health Outcomes
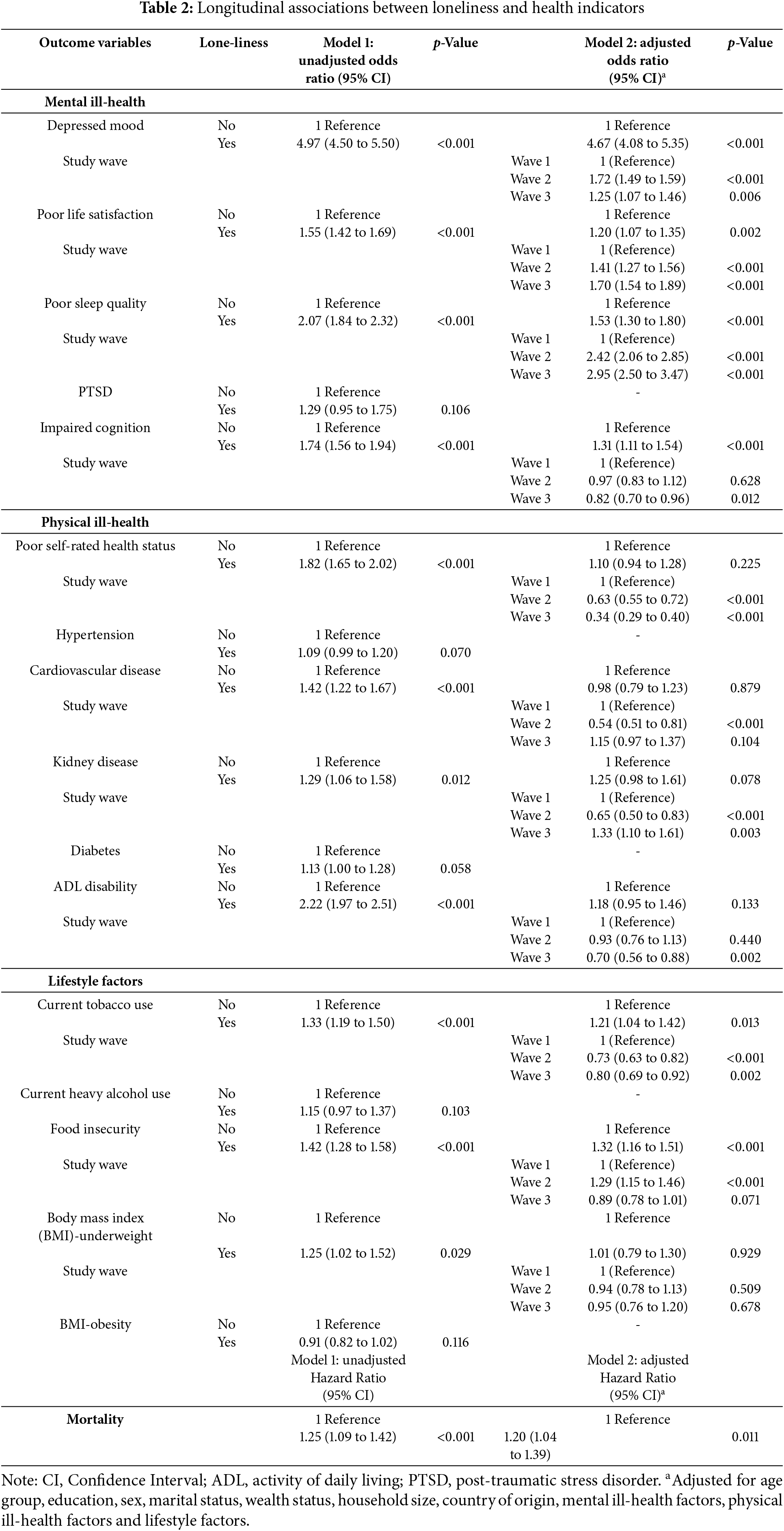
In the adjusted GEE logistic regression model, loneliness was positively associated with mental health problems (depressed mood, low life satisfaction, poor sleep quality, and impaired cognition) and lifestyle factors (current tobacco use and food insecurity). Loneliness raised death risks in adjusted Cox proportional hazards analysis (Table 2).
3.2 Loneliness and Incident Health Outcomes
ADL disability, cardiovascular disease, kidney disease, incident depressed mood, incident poor sleep quality, incident poor self-rated health status, incident current tobacco use, incident current heavy alcohol use, and incident food insecurity were all positively correlated with the degree of loneliness exposure in adjusted logistic regression (see Table 3).
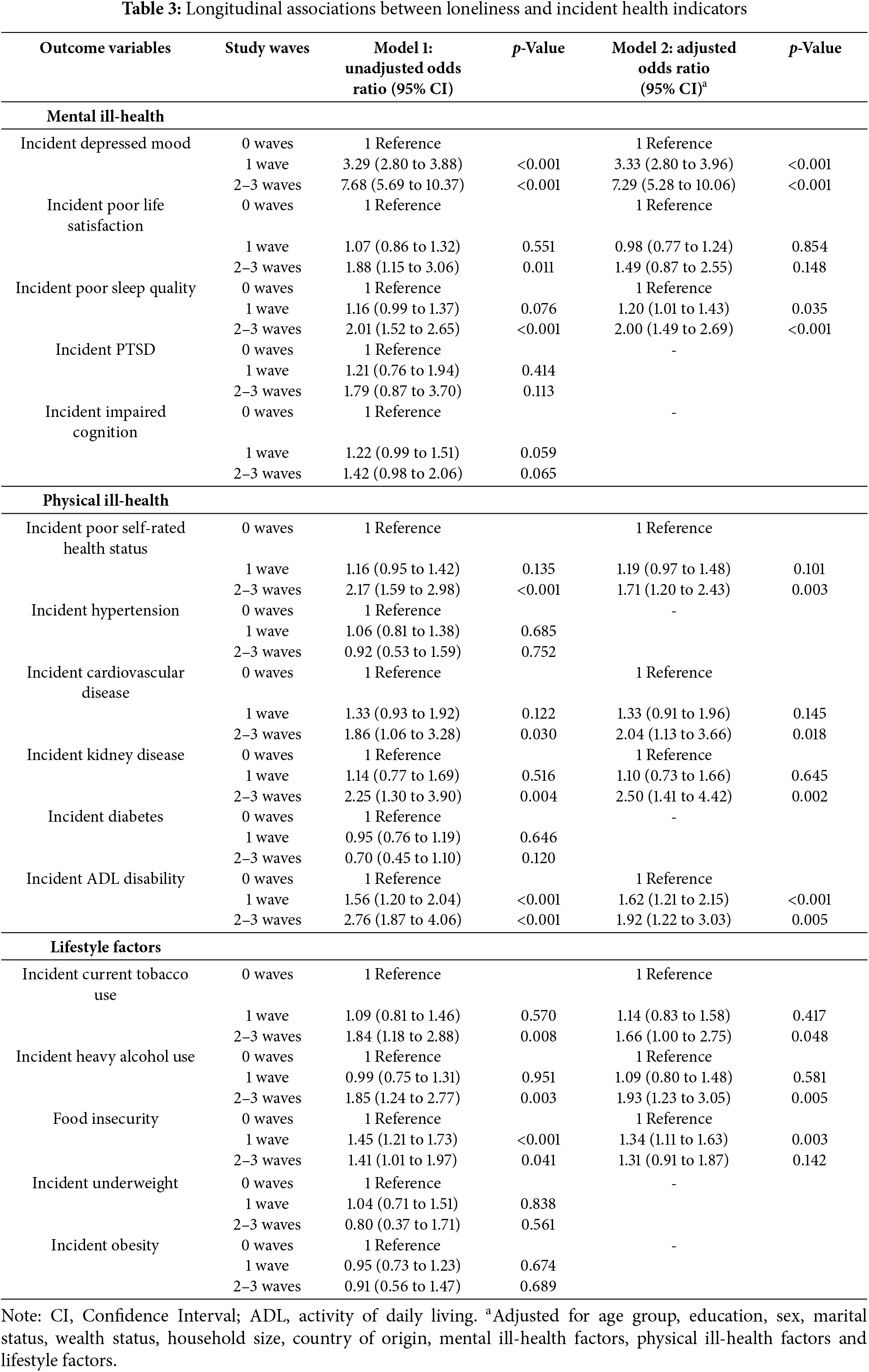
The purpose of the study was to estimate associations between loneliness and various health outcomes among ageing adults from 2015 to 2022 in South Africa. Results show that loneliness increased the odds of poor life satisfaction, (incident) depressed mood, incident poor self-rated health status, (incident) poor sleep quality, impaired cognition, incident cardiovascular disease, incident ADL disability, incident kidney disease, (incident) current tobacco use, (incident) food insecurity, and incident current heavy alcohol use.
In line with former findings [6,7,9–11], the study found that with loneliness, poor mental health (low mood, dissatisfaction with life, bad sleep, and cognitive impairment) increased. However, contrary to a prior study, we did not discover a correlation between loneliness and PTSD [8]. This may be because PTSD was only assessed in waves 1 and 3, and was very low (2.4%) in wave 3. Because loneliness is associated with depressive symptoms, the study reported significant odds ratios (4.67) for the connection between loneliness and depressed mood [13]. Loneliness, but not other depressive symptoms, was linked to an elevated risk of depressed mood in one study [29].
Consistent with previous research [12–14,16], this study showed that being lonely was associated with cardiovascular disease, poor self-rated health status, kidney disease, ADL disability, and mortality. The study did not find a correlation between loneliness and diabetes or hypertension, in contrast to some earlier research [13,14]. Neurobiological mechanisms that result in cardiovascular stress reactions and inflammation are among the mechanisms that explain how loneliness affects poor physical health [10]. Additionally, people who experience loneliness may not engage in as many health-promoting behaviours as others, such as physical inactivity and malnutrition, which can increase the risk of physical disease [30].
In terms of behavioral health outcomes, the study found positive associations between loneliness and food insecurity, current heavy alcohol use, and current tobacco use, which is consistent with previous research [10,16,17]. It is possible that aging adults try to cope with their loneliness by engaging in substance use (tobacco and/or alcohol) [16,31]. Older adults with loneliness may be less inclined to engage in food securing activities and reinforce the experience of being insecure of food [17]. Contrary to a few studies [18,19], this investigation did not find a significant association between being lonely and obesity, and only in unadjusted analysis a positive association with being underweight.
This study also has several limitations. Although some variables were assessed with objective measures, other items were evaluated by self-report, which may result in answers that are skewed. Our exposure variable “loneliness” was measured with a single CES-D item that “performs similarly to other loneliness measures” [32] and correlates highly with multiple-item loneliness measures [33]. Furthermore, some variables, such as physical inactivity, that are known to influence loneliness [9,34] were not assessed in all waves of the study. Since this study was only conducted one district in South Africa, findings cannot be generalized to the whole of South Africa.
Results show that loneliness is positively associated with poor mental health (low mood, dissatisfaction with life, bad sleep, and cognitive impairment), poor physical health (poor self-rated health status, cardiovascular disease, kidney disease, ADL disability and mortality), and poor behavioural health (current heavy drinking, current tobacco use, and food insecurity).
Acknowledgement: The author wants to thank the following for their help and support: HAALSI (Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa) is sponsored by the National Institute on Aging (grant number 5P01AG041710-05) and is conducted by the Harvard Center for Population and Development Studies in Partnership with Witwatersrand University. The Agincourt HDSS was supported by the Wellcome Trust, UK (058893/Z/99/A, 069683/Z/02/Z, 085477/Z/08/Z and 085477/B/08/Z), the University of the Witwatersrand and South African Medical Research Council.
Funding Statement: HAALSI (Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa) is sponsored by the National Institute on Aging (grant number 5P01AG041710-05) and is conducted by the Harvard Center for Population and Development Studies in Partnership with Witwatersrand University. The Agincourt HDSS was supported by the Wellcome Trust, UK (058893/Z/99/A, 069683/Z/02/Z, 085477/Z/08/Z and085477/B/08/Z), the University of the Witwatersrand and South African Medical Research Council.
Availability of Data and Materials: The datasets generated and/or analyzed during the current study are available at “Harvard Center for Population and Development Studies, 2023”, “HAALSI Wave 3 Survey”, doi:10.7910/DVN/F5YHML, Harvard Dataverse.
Ethics Approval: The study protocol “Health and Aging in Africa: A Longitudinal Study in South Africa (HAALSI)” was approved by the “University of the Witwatersrand Human Research Ethics Committee (Ref. M141159), the Harvard T.H. Chan School of Public Health, Office of Human Research Administration (Ref. C13–1608–02), and the Mpumalanga Provincial Research and Ethics Committee”.
Informed Consent: Participants gave written informed consent.
Conflicts of Interest: The author declares no conflicts of interest to report regarding the present study.
Abbreviations
| ADL | Activities of Daily Living |
| BMI | Body Mass Index |
| CES-D | Center for Epidemiologic Studies Depression Scale |
| HAALSI | Health and Aging in Africa: A Longitudinal Study in South Africa |
| INDEPTH | The International Network for the Demographic Evaluation of Populations and Their Health |
| PTSD | Posttraumatic Stress Disorder |
References
1. Chawla K, Kunonga TP, Stow D, Barker R, Craig D, Hanratty B. Prevalence of loneliness amongst older people in high-income countries: a systematic review and meta-analysis. PLoS One. 2021;16(7):e0255088. doi:10.1371/journal.pone.0255088. [Google Scholar] [PubMed] [CrossRef]
2. Phaswana-Mafuya N, Peltzer K. Prevalence of loneliness and associated factors among older adults in South Africa. Glob J Health Sci. 2017;9(12):1–8. doi:10.5539/gjhs.v9n12p1. [Google Scholar] [CrossRef]
3. Pengpid S, Peltzer K. Prevalence and associated factors of incident and persistent loneliness among middle-aged and older adults in Thailand. BMC Psychol. 2023;11(1):70. doi:10.1186/s40359-023-01115-4. [Google Scholar] [PubMed] [CrossRef]
4. Pengpid S, Peltzer K. Prevalence and correlates of loneliness among a nationally representative population-based sample of middle-aged and older adults in India. Int J Disabil Hum Dev. 2022;21(2):151–8. [Google Scholar]
5. Park C, Majeed A, Gill H, Tamura J, Ho RC, Mansur RB, et al. The effect of loneliness on distinct health outcomes: a comprehensive review and meta-analysis. Psychiatry Res. 2020;294(5):113514. doi:10.1016/j.psychres.2020.113514. [Google Scholar] [PubMed] [CrossRef]
6. Pearce E, Birken M, Pais S, Tamworth M, Ng Y, Wang J, et al. Associations between constructs related to social relationships and mental health conditions and symptoms: an umbrella review. BMC Psychiatry. 2023;23(1):652. doi:10.1186/s12888-023-05069-0. [Google Scholar] [PubMed] [CrossRef]
7. Giacco D. Loneliness and mood disorders: consequence, cause and/or unholy alliance? Curr Opin Psychiatry. 2023;36(1):47–53. doi:10.1097/YCO.0000000000000832. [Google Scholar] [PubMed] [CrossRef]
8. Gabarrell-Pascuet A, García-Mieres H, Giné-Vázquez I, Moneta MV, Koyanagi A, Haro JM, et al. The association of social support and loneliness with symptoms of depression, anxiety, and posttraumatic stress during the COVID-19 pandemic: a meta-analysis. Int J Environ Res Public Health. 2023;20(4):2765. doi:10.3390/ijerph20042765. [Google Scholar] [PubMed] [CrossRef]
9. Pengpid S, Peltzer K. Associations of loneliness with poor physical health, poor mental health and health risk behaviours among a nationally representative community-dwelling sample of middle-aged and older adults in India. Int J Geriatr Psychiatry. 2021;36(11):1722–31. doi:10.1002/gps.5592. [Google Scholar] [PubMed] [CrossRef]
10. Cacioppo S, Capitanio JP, Cacioppo JT. Toward a neurology of loneliness. Psychol Bull. 2014;140(6):1464–504. doi:10.1037/a0037618. [Google Scholar] [PubMed] [CrossRef]
11. Harrington KD, Vasan S, Kang JE, Sliwinski MJ, Lim MH. Loneliness and cognitive function in older adults without dementia: a systematic review and meta-analysis. J Alzheimers Dis. 2023;91(4):1243–59. doi:10.3233/JAD-220832. [Google Scholar] [PubMed] [CrossRef]
12. Teshale AB, Htun HL, Owen A, Gasevic D, Phyo AZZ, Fancourt D, et al. The role of social determinants of health in cardiovascular diseases: an umbrella review. J Am Heart Assoc. 2023;12(13):e029765. doi:10.1161/JAHA.123.029765. [Google Scholar] [PubMed] [CrossRef]
13. Richard A, Rohrmann S, Vandeleur CL, Schmid M, Barth J, Eichholzer M. Loneliness is adversely associated with physical and mental health and lifestyle factors: results from a Swiss national survey. PLoS One. 2017;12(7):e0181442. doi:10.1371/journal.pone.0181442. [Google Scholar] [PubMed] [CrossRef]
14. Petitte T, Mallow J, Barnes E, Petrone A, Barr T, Theeke L. A systematic review of loneliness and common chronic physical conditions in adults. Open Psychol J. 2015;8(Suppl 2):113–32. doi:10.2174/1874350101508010113. [Google Scholar] [PubMed] [CrossRef]
15. Wang F, Gao Y, Han Z, Yu Y, Long Z, Jiang X, et al. A systematic review and meta-analysis of 90 cohort studies of social isolation, loneliness and mortality. Nat Hum Behav. 2023;7(8):1307–19. doi:10.1038/s41562-023-01617-6. [Google Scholar] [PubMed] [CrossRef]
16. Stickley A, Koyanagi A, Leinsalu M, Ferlander S, Sabawoon W, McKee M. Loneliness and health in Eastern Europe: findings from Moscow. Russia Public Health. 2015;129(4):403–10. doi:10.1016/j.puhe.2014.12.021. [Google Scholar] [PubMed] [CrossRef]
17. Gonyea JG, O’Donnell AE, Curley A, Trieu V. Food insecurity and loneliness amongst older urban subsidised housing residents: the importance of social connectedness. Health Soc Care Community. 2022;30(6):e5959–67. doi:10.1111/hsc.14027. [Google Scholar] [PubMed] [CrossRef]
18. Lauder W, Mummery K, Jones M, Caperchione C. A comparison of health behaviours in lonely and non-lonely populations. Psychol Health Med. 2006;11(2):233–45. doi:10.1080/13548500500266607. [Google Scholar] [PubMed] [CrossRef]
19. Gómez-Olivé FX, Montana L, Wagner RG, Kabudula CW, Rohr JK, Kahn K, et al. Cohort profile: health and ageing in Africa: a longitudinal study of an INDEPTH community in South Africa (HAALSI). Int J Epidemiol. 2018;47(3):689–90. doi:10.1093/ije/dyx247. [Google Scholar] [PubMed] [CrossRef]
20. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi:10.1177/014662167700100306. [Google Scholar] [CrossRef]
21. Buysse DJ, Reynolds CF3rd, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4. [Google Scholar] [PubMed] [CrossRef]
22. Breslau N, Peterson EL, Kessler RC, Schultz LR. Short screening scale for DSM-IV posttraumatic stress disorder. Am J Psychiatry. 1999;156(6):908–11. doi:10.1176/ajp.156.6.908. [Google Scholar] [PubMed] [CrossRef]
23. Pengpid S, Peltzer K. Associations of history of intimate partner violence with mental ill-health and lifestyle factors in middle-aged and older men and women in South Africa. Arch Gerontol Geriatr. 2024;118(2):105286. doi:10.1016/j.archger.2023.105286. [Google Scholar] [PubMed] [CrossRef]
24. Katz S, Ford AB, Heiple KG, Newill VA. Studies of illness in the aged: recovery after fracture of the hip. J Gerontol. 1964;19(3):285–93. doi:10.1093/geronj/19.3.285. [Google Scholar] [PubMed] [CrossRef]
25. Berkman LF. Health and Aging in Africa: a Longitudinal Study of an INDEPTH Community in South Africa [HAALSI]: Agincourt, South Africa, 2015-2022 (ICPSR 36633) [Internet]. [cited 2024 May 2]. Available from: https://www.icpsr.umich.edu/web/NACDA/studies/36633. [Google Scholar]
26. World Health Organization (WHO). Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1–253. [Google Scholar]
27. Wei K, Liu Y, Yang J, Gu N, Cao X, Zhao X, et al. Living arrangement modifies the associations of loneliness with adverse health outcomes in older adults: evidence from the CLHLS. BMC Geriatr. 2022;22(1):59. doi:10.1186/s12877-021-02742-5. [Google Scholar] [PubMed] [CrossRef]
28. Mann F, Wang J, Pearce E, Ma R, Schlief M, Lloyd-Evans B, et al. Loneliness and the onset of new mental health problems in the general population. Soc Psychiatry Psychiatr Epidemiol. 2022;57(11):2161–78. doi:10.1007/s00127-022-02261-7. [Google Scholar] [PubMed] [CrossRef]
29. von Känel R, Weilenmann S, Spiller TR. Loneliness is associated with depressive affect, but not with most other symptoms of depression in community-dwelling individuals: a network analysis. Int J Environ Res Public Health. 2021;18(5):2408. doi:10.3390/ijerph18052408. [Google Scholar] [PubMed] [CrossRef]
30. Ong AD, Uchino BN, Wethington E. Loneliness and health in older adults: a mini-review and synthesis. Gerontology. 2016;62(4):443–9. doi:10.1159/000441651. [Google Scholar] [PubMed] [CrossRef]
31. deWall CN, Pond RS. Loneliness and smoking: the costs of the desire to reconnect. Self Identity. 2011;10(3):375–85. doi:10.1080/15298868.2010.524404. [Google Scholar] [CrossRef]
32. Newmyer L, Verdery AM, Margolis R, Pessin L. Measuring older adult loneliness across countries. J Gerontol B Psychol Sci Soc Sci. 2021;76(7):1408–14. doi:10.1093/geronb/gbaa109. [Google Scholar] [PubMed] [CrossRef]
33. Mund M, Maes M, Drewke PM, Gutzeit A, Jaki I, Qualter P. Would the real loneliness please stand up? The validity of loneliness scores and the reliability of single-item scores. Assessment. 2023;30(4):1226–48. doi:10.1177/10731911221077227. [Google Scholar] [PubMed] [CrossRef]
34. Hawkley LC, Cacioppo JT. Loneliness and pathways to disease. Brain Behav Immun. 2003;17(Suppl 1):S98–105. doi:10.1016/S0889-1591(02)00073-9. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools