 Open Access
Open Access
ARTICLE
IoMT-Based Smart Healthcare of Elderly People Using Deep Extreme Learning Machine
1 School of Information Technology, Skyline University College, University City Sharjah, 1797, Sharjah, UAE
2 College of Computing and Informatics, Saudi Electronic University, Riyadh, 11673, Saudi Arabia
3 Center for Cyber Security, Faculty of Information Science and Technology, University Kebangsaan Malaysia (UKM), 43600, Bangi, Selangor, Malaysia
4 Center for Cyber-Physical Systems, Khalifa University, 127788, Abu Dhabi, UAE
* Corresponding Author: Hussam Al Hamadi. Email:
Computers, Materials & Continua 2023, 76(1), 19-33. https://doi.org/10.32604/cmc.2023.032775
Received 29 May 2022; Accepted 12 July 2022; Issue published 08 June 2023
Abstract
The Internet of Medical Things (IoMT) enables digital devices to gather, infer, and broadcast health data via the cloud platform. The phenomenal growth of the IoMT is fueled by many factors, including the widespread and growing availability of wearables and the ever-decreasing cost of sensor-based technology. There is a growing interest in providing solutions for elderly people living assistance in a world where the population is rising rapidly. The IoMT is a novel reality transforming our daily lives. It can renovate modern healthcare by delivering a more personalized, protective, and collaborative approach to care. However, the current healthcare system for outdoor senior citizens faces new challenges. Traditional healthcare systems are inefficient and lack user-friendly technologies and interfaces appropriate for elderly people in an outdoor environment. Hence, in this research work, a IoMT based Smart Healthcare of Elderly people using Deep Extreme Learning Machine (SH-EDELM) is proposed to monitor the senior citizens’ healthcare. The performance of the proposed SH-EDELM technique gives better results in terms of 0.9301 accuracy and 0.0699 miss rate, respectively.Keywords
Elderly people care is a big challenge for current Health Care Systems (HCSs). According to the “Council for Economic Planning and Development (CEPD) 2012’s elderly people population growth trends and age structure”, the population comprises persons over 65. In 2011, elderly people over 80 accounted for 25.1 percent of the total population. In 2020, the number of elderly people in the world will be 0.7 billion. By 2060, the elderly people population will have grown by 41%. Scalable systems are required to meet the unique demands of elderly people in terms of health monitoring and accessibility to healthcare services [1]. As a solution to the HCS needs of elderly individuals, there is an increasing trend in using Information and Communication Technologies (ICTs).
There are many concerns with the existing Health care systems’ capacity to meet the necessities of the older adults in terms of availability and flexibility. Older people’s activities should not be limited to home care but should be considered a broader social monitoring effort. Smart cities play an imperative role in this regard [2]. Advances in ICTs have facilitated the creation of low-cost gadgets to monitor complicated activities and opened new possibilities in developing HCSs. For instance, camera installations for person tracking [3] and Wireless Sensor Network (WSN)-based technologies allow for non-intrusive surveillance [4]. Incorporating e-health sensors in wearable gadgets has expanded the possibility for full-time monitoring applications [5]. Many elderly people oblige ongoing support for daily tasks and health care, often their family and friends. Legal pay services presented by careers or care facilities are exclusive and remain beyond reach for many elderly people on a fixed or restricted budget.
Consequently, the need to improve and implement proficient and economical techniques and structures to offer cost-effective but excellent sanitary care and monitoring for those with limited access to medical facilities, particularly older people, has increased. The IoT is a new technology that links various devices, including sensors, actuators, devices, computers, and mobile telephones. It creates a smart system that can interact with other devices and people [6,7]. The IoT is a network of intelligent devices that can organize and share information, data, and assets, make decisions, and respond to opinions [8]. It enables communication between human-to-human, human-to-things, and things-to-things by giving each item a distinct personality [9]. One of the most prevalent reasons for injury and death among older people is falling. In non-injurious cases, around 47 percent of people who fall need help. SHs equipped with cameras can detect falls of elderly people and provide an alarm to the caregiver.
1.1 Multi-Sensor Information Fusion
Various wearable physiological sensors are attached to the human body (through skin electrodes, elastic bands, or smart clothing). These sensors can be used in various healthcare applications, such as cardiovascular and other chronic illness prevention, early diagnosis and monitoring, elderly people’s assistance at home (Fall Detection (FD)), physical Activity Recognition (AR), etc.
The wearable devices gather, process, and send sensed data streams remotely with limited processing power and storage capacity capabilities. These devices may capture data prone to errors, impacting signal processing and pattern identification. Fusing data from multiple sensors effectively extracts valuable data from noisy data, error-affected sensor readings, data loss or variation, and other problems. With the growing complexity of the wearable network, data fusion from multiple, possibly varied sensor sources have become a non-trivial job that directly influences the performance of the AR application.
Individual sensors are frequently insufficient to offer accurate data; this is where multi-sensor data fusion can play an imperative role. Employing numerous homogenous sensors offers redundancy, which increases the system’s fault tolerance even if a sensor fails. Increased dimensionality of the measuring environment (for example, monitoring heart rate with both ECG and photo Plethysmography (PPG) sensors) substantially improves resilience against external interferences [10,11]. When separate measurements of the same feature are fused, the precision of the resultant value is better than that of a single sensor. Multi-sensor Fusion (MSF) improves resistance against data source interferences while capturing features of the target application field.
MSF is generally classified into three categories grounded on the level of thought of data processing: data-level fusion, feature-level fusion, and decision-level fusion. Data fusion techniques can be centralized, distributed, or hybrid, dependent on the processing level. The centralized approach uses a fusion center to do the processing. The distributed technique uses each sensor to perform separate processing on the data and communicate the findings to a “Fusion Node (FN)” for global analysis. Data acquisition and preprocessing are generally made in a distributed manner in hybrid data fusion. However, a central node is still involved in information fusion from dispersed sources and conducting decision-level computing. Sensor data can be immediately fused if the system includes many homogenous sensors monitoring the same physical phenomenon. On the other hand, data from various causes cannot be merged directly, necessitating the feature or decision-level fusion procedures.
Machine Learning (ML), a form of AI, processes and determines patterns in massive datasets to aid decision-making. ML enables the systems to improve them from experience without being explicitly programmed [12,13]. It also allows the machines or software to analyze, predict and sort vast amounts of data. Every time the ML algorithm searches through the data and discovers new patterns, it modifies the model. This method allows for learning and produces progressively accurate results [14,15]. Smart HCSs that use machine learning are a progressive way to provide continuous and comprehensive tracking, reduce care efforts, and assist with better decision-making for elderly people. ML can be used to address complex health problems and give exact results [16,17]. The performance of ML algorithms depends on creating an accurate and multidimensional data collection. Multiple sensors communicate real-time data in smart HCSs, producing massive data for ML.
Many healthcare systems have been developed for monitoring elderly people’s health to provide them better healthcare, and a few of them are described as that Smart Home technologies. These systems help older people, and they can interact with healthcare service providers in an emergency. “AGAPE (Allocation and Group Awareness Pervasive Environment)” is the HCS for people who live far away from a hospital [18]. When the AGAPE notices abnormalities in the data collected through the on-body sensors, it searches for and contacts local caregiver groups. AGAPE finds the patient’s profile and sends it to the group when notified. AGAPE communicates and informs different groups around the situation and asks for more aid if required.
In [19] presented a “smartphone-based emergency calling system.” In an emergency, the structure can initiate an automatic call to “Emergency Medical Service (EMS)” or careers through GSM and send them the location details obtained through the integrated GPS. When a pre-set threshold value is exceeded, e.g., room temperature reaches or falls below a pre-set value, the user creates an alert automatically or routinely by the scheme.
In [20] proposed a “Health Smart Home system” for the disabled or elderly people, a combination of wireless healthcare gadgets and “Wireless Sensor Networks (WSNs)” named “Incident Aware System (IAS).” This system predicts potential accidents in a precise house area and can alert elderly people. It incorporates Raspberry Pi boards and servers to gather sensor data and transmit it to smartphones. The system may be set up to call pre-determined numbers for help if necessary [21]. presented a novel system to monitor the elderly people in their homes by posture identification. The foreground region extraction and postures categorization features were input into a “Directed Acyclic Graph Support Vector Machine (DAGSVM)” for improving multi-class classification outcomes. Experiments using a 15-person dataset demonstrate that their FDS performs well, with a fall detection rate of 97.08 percent.
According to research, a Smart Ambient and Wearable Home Monitoring” for the elderly people was introduced by [22]. It employs biological sensors and sensor-based clothing to track health, heart rate, and accelerometers mounted on the floor to detect movement and falls. These sensors are linked in an internet-based system used to monitor older people indoors and outdoors in their everyday lives.
In [23,24] presented an improved FDS [25,26] to monitor elderly people, using smart body sensors to operate via user home networks. The smart sensors, such as temperature and humidity, are incorporated on a single board with the accelerometer sensor, collecting real-time acceleration data by employing an Analog-To-Digital Converter (ADC). This data is then sent to the Microprogrammed Controller Unit (MCU) for further processing. The data collected from these sensors may be stored and further used to differentiate the falls from everyday activities. The experimental result shows that this FDS can obtain a high detection accuracy of 97.5 percent, with sensitivity and specificity of 96.8 percent and 98.1 percent, separately.
In [27,28] presented a robot-assisted living system for elderly and disabled people. They created a “Multi-Sensor Fusion (MSF) [29] based Activity Recognition (AR)” technique that incorporates “Neural Networks (NN) and Hidden Markov Models (HMMs).” They employed two wearable sensors data is fused to identify the activity type. A “fine-grained classification” module employing heuristic perception or HMMs is used to differentiate the activities further. The HMM-based identification method is only utilized for SDAs. They performed tests on a sample wearable sensor system, and the findings show that their method accurately identified the activities 88.1 percent of the time. They only use two sensors for AR; however, more sensors may enhance accuracy and identify a broader range of activities.
In [30,31] introduced a fusion technique for enhancing human action detection using two modality sensors. A collaborative representation classifier analyses FLF and DNLF for action identification. The “Berkeley multimodal human action database” is used to test the proposed fusion architecture. The results show that the presented fusion techniques enhance identification rates by 2% to 23% based on the action performed when each sensor is employed separately.
In [32] proposed an automated in-home Health Care Monitoring (HCM) system to make intelligent decisions regarding older people living alone at home. The different sensors outputs are fused using a “multi-sensor data fusion technique based on Fuzzy Logic (FL)” with a set of rules driven by healthcare guidelines. The performance may be improved even further with more relevant input variables and additional data to expand the rules’ knowledge. The FL fusion approaches provide flexibility, particularly when integrating sensors. The presented system would provide elderly people individuals with continuous in-home HCM. The experimental findings, based on actual data, were accurate and reliable. The FL decision module improves the accuracy of detecting and locating elderly people with difficulty.
In [33] presented a system that considers a participant’s biological and physical profile and numerous wearable sensor node parameter data. The profile is being utilized to assign the individual to a fall risk group. They conducted FD ML studies using public datasets containing wearable sensor node readings. The algorithms were then retrained by feeding into the participant’s risk classification. The tests were performed to see how a participant’s risk classification affected the accuracy of FD. They examined the performance of several algorithms with and without risk category as an input feature to a public data set for FD. They also evaluated the performance of the “Random Forest (RF) and Ordinal Logistic Regression (OLR)” algorithms in terms of risk category forecasting, finding that OLR had a 91.8 percent accuracy. They also found that adding a risk category improves accuracy, with the most significant results from KNN and Decision Tree (DT) [34]. The Initial letter of each notional word in all headings is capitalized.
3 Proposed Multi-Sensor Information-Based Smart Healthcare for Elderly People
Human life expectancy is growing because of medical technology and advances in nutritional sciences. At the same time, more resources are needed to monitor the health of an ageing population. The IoT connects physical things with various health monitoring applications that monitor conditions via biomedical sensing devices. This research has proposed the architecture of multi-sensor information-based smart healthcare monitoring for elderly patients using a Deep Extreme Learning Machine (DELM). This research aims to concentrate on the elderly people population issues that directly affect the socio-economic structure of the nations.
Fig. 1 demonstrates that the proposed SH-EDELM depends on the training and validation phases communicating through the cloud. The training phase consists of three layers: the sensory, preprocessing, and application. The sensory layer gathers the values from two sources containing the same input parameters, which get the values from parameters and pass these values through IoT to store in a device known as a database. The data received through IoT might hold missing or noisy data. So, it is known as raw data. Then the preprocessing layer plays a vital role in handling the missing values by moving average and normalization to mitigate the noisy data. The preprocessed data from both sources is then sent to the Application layer, further separated into two-layer; Prediction and Performance; in prediction, DELM is used to predict Elderly people’s healthcare.

Figure 1: Proposed model for elderly people healthcare (SH-EDELM)
DELM is utilized in the proposed research to encompass the advantages of ELM and deep learning. Furthermore, DELM has been proven to enhance the expected results substantially. Three layers include the input layer, the multiple Hidden Layers (HL), and the output layer in the proposed SH-EDELM model. Where Ɋ [] indicates the inputs, ʯ [] is the output, addition,
When modeling machine learning algorithms for increased predictability and improved training, complete sample data were normalized to fit the [0, 1] interval using the following Eq. (2):
where, i = 1,2,3 … N
Firstly, a training sample is engaged as, [X, S] = xk, sk, (i = 1, 2, . . . , Z), and input sample, as, X = [xk1 xk2 xk3. . . xkz] and a targeted matrix, as, S = [s11 s12 s13. . . s1z]. The training set consists of such training samples. The matrices X and S may be shown in Eqs. (3) and (4), where x and s are input and output matrices, respectively. The ELM randomly adjusts weights between the input and the HL, where vk1 is the kth input node and the HL lth node, as shown in Eq. (5).
Firstly, the ELM casually chose the HL nodes in Eq. (7). ELM, the network activation function g(x), has likewise been selected. The resultant matrix is revealed in Eq. (8). The resulting column vector T is displayed in Eq. (9).
Formerly it can be obtained Eq. (10) by manipulating Eqs. (8) and (9). The consequence of the HL is M besides transposition of N by way of Ƀ, and principles of weight matrix
Now,
The deep learning system has at least four input or output layers that meet its requirements. The neurons of all layers are trained via a deep neural network on a range of limits resulting from the former layer. It enables the deep learning networks to handle large data sets. Deep learning has received a lot of concern due to its efficiency in addressing real-world problems. The proposed approach comprises neurons’ input, hidden, and output layers. The output of the HL is obtained
where the overall inverse of a matrix
In Eq. (13), the parameters
Modernizing the weight matrix
The
The following weight matrix is intended for the 3rd HL, and the end layer results from Eqs. (22) and (23) represents the result of the third HL.
The method of computing the 4 HL of the DELM system has been studied. The cycle idea was utilized to illustrate the DELM process. The parameters of each HL and the results of the DELM network may be recalculated in Eqs. (18) and (22). When HL is expanded, they may reuse and execute the same operation.
The well-known Back-Propagation Algorithm (BPA) contains weight initialization, feed forwarding, backward error propagation, weight update, and bias elements. The activation function of every neuron in the HL is Sigmoid. It makes it possible to compose the sigmoid input function and DELM HL:
opj = calculated output
Eq. (31) illustrates the backpropagation of error, which can be intended by summating the square of the wanted output from the deliberate output divided by 2.
The modification of weight is required to decrease the overall error. Eq. (32) demonstrates the weight change rate for the output layer.
Eq. (33) utilizing the chain rule process:
The value of revolution in weight can be achieved after substituting Eq. (34) as exposed in Eq. (35).
From op to ʧ6
The calculation to regulate suitable weight change to the hidden weight is exposed in the subsequent process. It is multifaceted since the weighted connection can be central to errors at all nodes.
From ʧ6 to ʧ1 or ʧn
Where l = 5, 4, 3, 2,
where
The process of boosting the weight and bias between the output and the HL is presented in Eq. (36).
Eq. (37) appears on how to appraise the weight and bias amongst the input and the HL.
After the prediction layer, the output of the prediction layer will be sent to the performance layer to predict the elderly people’s healthcare basis on accuracy and miss rate whether the learning criteria are met or not. In the case of ‘No,’ the prediction layer will be updated, but in ‘Yes,’ the output will be stored on the cloud database.
In the Validation phase, the stored data onto the cloud will be imported to the DELM approach to determine whether the elderly people’s healthcare monitoring is found or not. In the case of ‘No,’ the process will be discarded, and in the case of ‘Yes,’ the message will be displayed that elderly people’s healthcare monitoring is found.
Elderly people care about a significant challenge for the future smart cities. It signifies a valuable opportunity to develop scalable applications to cover the unique needs of health monitoring and accessibility for people with DELM. This paper presents a complete system based on a multi-sensor approach for assisting elderly people in daily activities. The proposed DELM based elderly people smart healthcare approach is applied to a dataset divided into 70% training and 30% training samples.
Different statistical parameters are calculated by applying the proposed approach to given datasets, such as accuracy, sensitivity, specificity, miss-rate, fallout, Positive Likelihood Ratio (LR+), Likelihood Negative Ration (LR−), Precision and Negative Predictive Value. In contrast, the True Positive Rate (TPR) is expressed as sensitivity, True Negative Rate (TNR) as specificity, False Negative Rate (FNR) as miss-rate, False Positive Rate (FPR) as fallout and Positive Predictive Value (PPV) as precision. The following parameters are resultant of the formulas assumed as follows:
Table 1 displays the proposed system’s health status prediction during the validation phase. During validation, a total of 743 samples were utilized. They are split into 327, 386 positive, and negative samples. It is discovered that 322 samples contain true positives that are accurately forecasted, and no healthcare issue is discovered. While 5 records are mistakenly predicted as negatives, implying a healthcare issue has been discovered. Similarly, 386 samples are picked, with negative indicating the presence of a health issue in which 378 samples are accurately predicted as negative, indicating the presence of a healthcare issue and 8 samples are incorrectly predicted as positive, indicating the absence of a healthcare issue, although healthcare issues do exist.
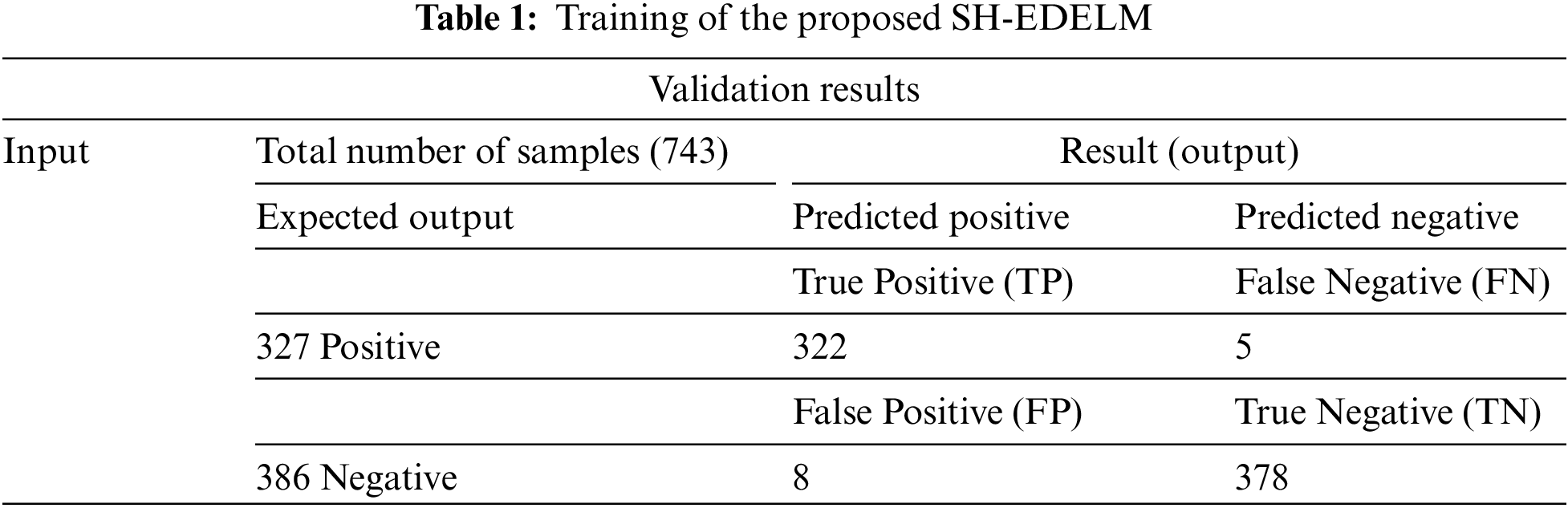
Table 2 shows the proposed SH-EDELM system during the training phase. 186 samples are utilized during training, divided into 73, 113 positive, and negative samples. It was discovered that 65 samples are truly positive, accurately monitored, and found with no healthcare issue. At the same time, 8 records are wrongly predicted as negatives, implying a healthcare issue. 5 samples are incorrectly predicted as positive, indicating the absence of a healthcare issue, although a healthcare issue exists. Similarly, a total of 113 samples are picked, with negative indicating the presence of a healthcare issue, and 108 samples are correctly predicted as negative, indicating the presence of a healthcare issue.

Table 3 shows the performance of the proposed system in terms of accuracy, sensitivity, specificity, miss rate, and precision during the training and validation phase. The proposed system gives 0.9818, 0.9847, 0.9793, 0.0182, and 0.9758 accuracy, sensitivity, specificity, miss rate, and precision during training. And during validation, the model gives 0.9301, 0.8904, 0.9558, 0.0699, and 0.9286 accuracy, sensitivity, specificity, miss rate, and precision, respectively. Furthermore, specific statistical measures of the model are included to forecast values during training, e.g., Fall-out, LR+, LR−, and NPV give the result 0.0207, 45.57, 0.0185, and 0.9869 during validation 0.0442, 20.14, 0.0731, and 0.9310 respectively.
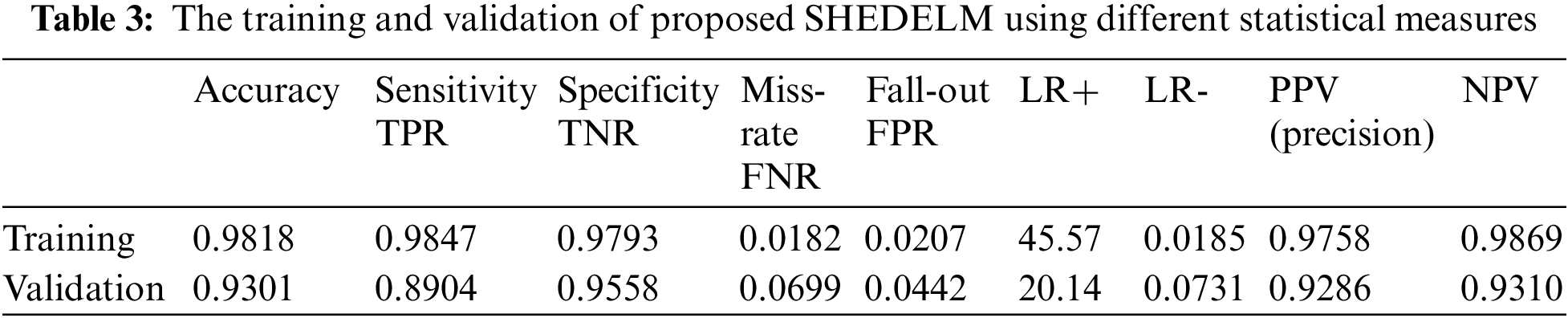
Table 4 compares the previous approaches and the proposed model. The proposed model attained 0.9301 accuracy for monitoring elderly people’s healthcare smartly and efficiently, which is better than the existing approaches.
This research proposes a smart healthcare system for elderly people in emergency scenarios. While reducing the response time in an emergency, the proposed multi-sensor information-based system offers real-time support to older citizens in emergencies with the help of machine learning techniques. Moreover, it can share the information in emergencies with specialists or medical workers to assist in real-time. In this proposed research work, an intelligent multi-sensor fusion-based elderly people healthcare using machine learning is proposed to meet the basic needs of elderly healthcare for getting better treatment. After simulation results, the research conclusions are summarized: the elderly people healthcare service interface of the IoMT has a better accuracy during validation, which gives 0.9301, 0.8904, 0.9558, 0.0699, and 0.9286 accuracy, sensitivity, specificity, miss rate, and precision, respectively
Funding Statement: Self-Funded; no external funding is involved in this study.
Availability of Data and Materials: The data used in this paper can be requested from the corresponding author upon request.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. A. Arcelus, M. H. Jones, R. Goubran and F. Knoefel, “Integration of smart home technologies in a health monitoring system for the elderly,” in 21st Int. Conf. on Advanced Information Networking and Applications Workshop, Niagara Falls, Canada, pp. 820–825, 2013. [Google Scholar]
2. M. N. K. Boulos and N. M. Al-Shorbaji, “On the internet of things, smart cities and the who healthy cities,” International Journal of Health Geographics, vol. 13, no. 1, pp. 1–6, 2014. [Google Scholar]
3. F. Khan, M. A. Khan, S. Abbas, A. Athar, S. Y. Siddiqui et al., “Cloud-based breast cancer prediction empowered with soft computing approaches,” Journal of Healthcare Engineering, vol. 1, no. 2, pp. 1–16, 2020. [Google Scholar]
4. A. Mathur, T. Newe and M. Rao, “Healthcare wsn: Cluster elections and selective forwarding defense,” in 9th Int. Conf. on Next Generation Mobile Applications, Services and Technologies, Cambridge, UK, pp. 341–346, 2015. [Google Scholar]
5. A. Costanzo, A. Faro, D. Giordano and C. Pino, “Mobile cyber-physical systems for health care: Functions, ambient ontology and e-diagnostics,” in 13th IEEE Annual Consumer Communications & Networking Conf., NV, USA, pp. 972–975, 2016. [Google Scholar]
6. A. Bassi and G. Horn, “Internet of things in 2020: A roadmap for the future,” European Commission: Information Society and Media 22, vol. 2, no. 1, pp. 97–114, 2012. [Google Scholar]
7. S. V. Madakam, V. Lake, V. Lake and V. Lake, “Internet of things: A literature review,” Journal of Computer and Communications, vol. 3, no. 5, pp. 164–178, 2015. [Google Scholar]
8. R. Aggarwal and M. L. Das, “Rfid security in the context of internet of things,” in Proc. of the First Int. Conf. on Security of Internet of Things, New York, United States, pp. 51–56, 2012. [Google Scholar]
9. C. Rotariu, A. Pasarica, H. Costin, F. Adochiei and R. Ciobotariu, “Telemedicine system for remote blood pressure and heart rate monitoring,” in E-Health and Bioengineering Conf., Iasi, Romania, pp. 1–4, 2011. [Google Scholar]
10. D. Schuldhaus, H. Leutheuser and B. M. Eskofier, “Towards big data for activity recognition: A novel database fusion strategy,” in Proc. of the 9th Int. Conf. on Body Area Networks, Brussels, Belgium, pp. 97–103, 2014. [Google Scholar]
11. S. Muneer, M. B. Alvi and M. A. Rasool, “Genetic algorithm based intelligent system for estate value estimation,” International Journal of Computational and Innovative Sciences, vol. 1, no. 1, pp. 1–12, 2022. [Google Scholar]
12. D. J. Freitas, T. B. Marcondes, L. H. Nakamura, J. Ueyama, P. H. Gomes et al., “Combining cell phones and wsns for preventing accidents in smart-homes with disabled people,” in 7th Int. Conf. on New Technologies, Mobility and Security, Paris, France, pp. 1–5, 2015. [Google Scholar]
13. M. Yu, A. Rhuma, S. M. Naqvi, L. Wang and J. Chambers, “A posture recognition-based fall detection system for monitoring an elderly person in a smart home environment,” IEEE Transactions on Information Technology in Biomedicine, Shatin, Hong Kong, vol. 16, no. 6, pp. 1274–1286, 2012. [Google Scholar] [PubMed]
14. P. Perego, M. Tarabini, M. Bocciolone and G. Andreoni, “Smarta: Smart ambient and wearable home monitoring for elderly,” in Int. Internet of Things Summit, Washington, DC, pp. 502–507, 2015. [Google Scholar]
15. J. Wang, Z. Zhang, B. Li, S. Lee and R. S. Sherratt, “An enhanced fall detection system for elderly person monitoring using consumer home networks,” IEEE Transactions on Consumer Electronics, vol. 60, no. 1, pp. 23–29, 2014. [Google Scholar]
16. M. Aslam, “Removal of the noise and blurriness using global and local image enhancement equalization techniques,” International Journal of Computational and Innovative Sciences, vol. 1, no. 1, pp. 1–14, 2022. [Google Scholar]
17. Q. Zhang, L. Ren and W. Shi, “Honey: A multimodality fall detection and telecare system,” Telemedicine and E-Health, vol. 19, no. 5, pp. 415–429, 2013. [Google Scholar] [PubMed]
18. S. Abbate, M. Avvenuti, F. Bonatesta, G. Cola, P. Corsini et al., “A smartphone-based fall detection system,” Pervasive and Mobile Computing, vol. 8, no. 6, pp. 883–899, 2012. [Google Scholar]
19. P. Zappi, T. Stiefmeier, E. Farella, D. Roggen, L. Benini et al., “Activity recognition from on-body sensors by classifier fusion: Sensor scalability and robustness,” in 3rd Int. Conf. on Intelligent Sensors, Sensor Networks and Information, Bangalore, India, pp. 281–286, 2007. [Google Scholar]
20. Z. Khan, “Used car price evaluation using three different variants of linear regression,” International Journal of Computational and Innovative Sciences, vol. 1, no. 1, pp. 13–28, 2022. [Google Scholar]
21. L. Gao, A. K. Bourke and J. Nelson, “A system for activity recognition using multi-sensor fusion,” in Annual Int. Conf. of the IEEE Engineering in Medicine and Biology Society, Scotland, UK, pp. 7869–7872, 2011. [Google Scholar]
22. M. Asif, S. Abbas, M. A. Khan, A. Fatima, M. A. Khan et al., “MapReduce based intelligent model for intrusion detection using machine learning technique,” Journal of King Saud University-Computer and Information Sciences, vol. inpress, 2021. [Google Scholar]
23. M. Saleem, S. Abbas, T. M. Ghazal, M. A. Khan, N. Sahawneh et al., “Smart cities: Fusion-based intelligent traffic congestion control system for vehicular networks using machine learning techniques,” Egyptian Informatics Journal, vol. 1, no. 1, pp. 417–426, 2022. [Google Scholar]
24. M. Saleem, M. A. Khan, S. Abbas, M. Asif, M. Hassan et al., “Intelligent fso link for communication in natural disasters empowered with fuzzy inference system,” in Int. Conf. on Electrical, Communication, and Computer Engineering, Istanbul, Turkey, pp. 1–6, 2019. [Google Scholar]
25. A. Rehman, A. Athar, M. A. Khan, S. Abbas, A. Fatima et al., “Modelling, simulation, and optimization of diabetes type II prediction using deep extreme learning machine,” Journal of Ambient Intelligence and Smart Environments, vol. 12, no. 2, pp. 125–138, 2020. [Google Scholar]
26. M. Marschollek, K. H. Wolf, M. Gietzelt, G. Nemitz, H. M. Schwabedissen et al., “Assessing elderly persons’ fall risk using spectral analysis on accelerometric data-a clinical evaluation study,” in 30th Annual Int. Conf. of the IEEE Engineering in Medicine and Biology Society, NW Washington, United States, pp. 3682–3685, 2012. [Google Scholar]
27. C. Wang, S. Lee, J. Ho, Y. Na and S. D. Min, “Detection of optimal activity recognition algorithm for elderly using smartphone,” Advances in Computer Science and Ubiquitous Computing, vol. 5, no. 2, pp. 1013–1018, 2016. [Google Scholar]
28. A. Veeraputhiran and R. Sankararajan, “Feature-based fall detection system for elders using compressed sensing in wvsn,” Wireless Networks, vol. 25, no. 1, pp. 287–301, 2019. [Google Scholar]
29. T. Batool, S. Abbas, Y. Alhwaiti, M. Saleem, M. Ahmad et al., “Intelligent model of the ecosystem for smart cities using artificial neural networks,” Intelligent Automation and Soft Computing, vol. 30, no. 2, pp. 513–525, 2021. [Google Scholar]
30. M. K. Hasan, M. Shafiq, S. Islam, B. Pandey, Y. A. Baker et al., “Lightweight cryptographic algorithms for guessing attack protection in complex internet of things applications,” Complexity, vol. 4, no. 6, pp. 23–36, 2021. [Google Scholar]
31. S. Y. Siddiqui, A. Haider, T. M. Ghazal, M. A. Khan, I. Naseer et al., “IoMT cloud-based intelligent prediction of breast cancer stages empowered with deep learning,” IEEE Access, vol. 12, no. 3, pp. 12–28, 2021. [Google Scholar]
32. T. M. Ghazal, S. Abbas, S. Munir, M. A. Khan, M. Ahmad et al., “Disease detection empowered with transfer learning,” Computers, Materials & Continua, vol. 70, no. 3, pp. 5005–5019, 2022. [Google Scholar]
33. B. Ihnaini, M. A. Khan, T. A. Khan, S. Abbas, M. S. Daoud et al., “A smart healthcare recommendation system for multidisciplinary diabetes patients with data fusion based on deep ensemble learning,” Computational Intelligence and Neuroscience, vol. 8, no. 3, pp. 23–35, 2021. [Google Scholar]
34. S. Y. Siddiqui, S. Abbas, M. A. Khan, I. Naseer, T. Masood et al., “Intelligent decision support system for COVID-19 empowered with deep learning,” Computer Materials & Continua, vol. 66, no. 2, pp. 1719–1732, 2021. [Google Scholar]
35. M. A. Khan, S. Abbas, A. Atta, A. Ditta, H. Alquhayz et al., “Intelligent cloud-based heart disease prediction system empowered with supervised machine learning,” Computer Materials & Continua, vol. 65, no. 1, pp. 139–151, 2020. [Google Scholar]
36. F. Khan, M. A. Khan, S. Abbas, A. Athar, S. Y. Siddiqui et al., “Cloud-based breast cancer prediction empowered with soft computing approaches,” Journal of Healthcare Engineering, vol. 65, no. 1, pp. 139–151, 2020. [Google Scholar]
37. M. F. Khan, T. M. Ghazal, R. A. Said, A. Fatima, S. Abbas et al., “An iomt-enabled smart healthcare model to monitor elderly people using machine learning technique,” Computational Intelligence and Neuroscience, vol. 3, no. 2, pp. 19–30, 2021. [Google Scholar]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF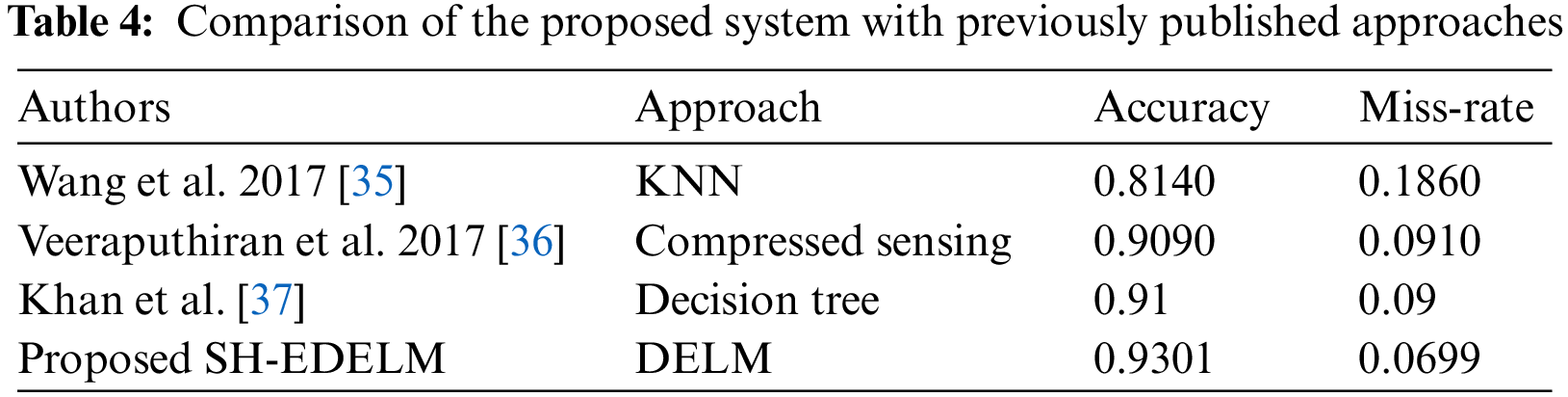
 Downloads
Downloads
 Citation Tools
Citation Tools