 Open Access
Open Access
REVIEW
A Narrative Review of Artificial Intelligence in Medical Diagnostics
Department of Diagnostic and Generalist Medicine, Dokkyo Medical University, Tochigi, 321-0293, Japan
* Corresponding Author: Takanobu Hirosawa. Email:
Computers, Materials & Continua 2025, 83(3), 3919-3944. https://doi.org/10.32604/cmc.2025.063803
Received 24 January 2025; Accepted 16 April 2025; Issue published 19 May 2025
Abstract
Artificial Intelligence (AI) is fundamentally transforming medical diagnostics, driving advancements that enhance accuracy, efficiency, and personalized patient care. This narrative review explores AI integration across various diagnostic domains, emphasizing its role in improving clinical decision-making. The evolution of medical diagnostics from traditional observational methods to sophisticated imaging, laboratory tests, and molecular diagnostics lays the foundation for understanding AI’s impact. Modern diagnostics are inherently complex, influenced by multifactorial disease presentations, patient variability, cognitive biases, and systemic factors like data overload and interdisciplinary collaboration. AI-enhanced clinical decision support systems utilize both knowledge-based and non-knowledge-based approaches, employing machine learning and deep learning algorithms to analyze vast datasets, identify patterns, and generate accurate differential diagnoses. AI’s potential in diagnostics is demonstrated through applications in genomics, predictive analytics, and early disease detection, with successful case studies in oncology, radiology, pathology, ophthalmology, dermatology, gastroenterology, and psychiatry. These applications demonstrate AI’s ability to process complex medical data, facilitate early intervention, and extend specialized care to underserved populations. However, integrating AI into diagnostics faces significant limitations, including technical challenges related to data quality and system integration, regulatory hurdles, ethical concerns about transparency and bias, and risks of misinformation and overreliance. Addressing these challenges requires robust regulatory frameworks, ethical guidelines, and continuous advancements in AI technology. The future of AI in diagnostics promises further innovations in multimodal AI, genomic data integration, and expanding access to high-quality diagnostic services globally. Responsible and ethical implementation of AI will be crucial to fully realize its potential, ensuring AI serves as a powerful ally in achieving diagnostic excellence and improving global health care outcomes. This narrative review emphasizes AI’s pivotal role in shaping the future of medical diagnostics, advocating for sustained investment and collaborative efforts to harness its benefits effectively.Keywords
Abbreviations
| AI | Artificial Intelligence |
| CDSS | Clinical Decision Support Systems |
| EHR | Electronic Health Record |
| EU | European Union |
| CT | Computed Tomography |
| MRI | Magnetic Resonance Imaging |
| PCR | Polymerase Chain Reaction |
| NN | Neural Networks |
| CNN | Convolutional Neural Network |
| NLP | Natural Language Processing |
| LLM | Large Language Model |
Artificial Intelligence (AI) is revolutionizing medical diagnostics, ushering in an era of enhanced precision, efficiency, and personalized patient care [1,2]. This narrative review searches the multifaceted role of AI across various diagnostic domains, highlighting its transformative potential—defined as AI’s ability to fundamentally change diagnostic workflows by automating data analysis, reducing cognitive biases, and enabling predictive analytics in clinical settings.
We begin by examining the foundational principles of medical diagnosis, highlighting their evolution from traditional observational techniques to advanced technological methods. Subsequently, the review explores Clinical Decision Support System (CDSS), detailing their functionalities, classifications, and the seamless integration of AI technologies within these systems. The discussion highlights the essential contribution of AI in enhancing diagnostic accuracy and operational efficiency, thereby supporting health care professionals in delivering high-quality care.
The potential of AI in diagnostics is further illustrated through advancements in specific medical fields, supported by case studies that demonstrate successful AI applications, including their role in telemedicine. These examples highlight AI’s capability to handle complex diagnostic tasks, facilitate early disease detection, and extend specialized care to underserved populations.
However, the adoption of AI in diagnostics is not without challenges. This review critically examines the technical limitations, regulatory hurdles, and ethical considerations associated with AI implementation in health care. Addressing these challenges is crucial for the responsible and effective integration of AI technologies into clinical practice [3].
Looking ahead, the review anticipates future developments in AI-driven diagnostics, including technological innovations, evolving regulatory frameworks, and the changing role of health care professionals in an AI-enhanced health care landscape. Additionally, it explores how AI can bridge global health disparities, ensuring equitable access to advanced diagnostic services worldwide.
2 Introduction to Medical Diagnosis
Accurate medical diagnosis is fundamental to effective patient care, serving as the foundation for all subsequent treatment decisions and management strategies. Diagnostic accuracy directly influences patient outcomes, treatment efficacy, and overall health care quality. However, diagnostic errors remain a significant concern, contributing to preventable harm and adversely affecting patient safety across diverse clinical settings.
2.1 Importance of Medical Diagnosis
Medical diagnosis involves a comprehensive assessment that integrates a patient’s medical history, physical examination findings, and results from various diagnostic investigations. This holistic approach enables health care professionals to identify the underlying cause of a patient’s condition, guiding appropriate and timely interventions. Beyond labeling a disease, a precise diagnosis ensures tailored treatment plans that address the individual’s specific health profile, enhancing the likelihood of successful outcomes and minimizing the risk of adverse effects.
Achieving diagnostic excellence entails adhering to high standards that encompass safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity, as shown in Fig. 1. This multifaceted approach ensures that diagnoses are not only accurate but also delivered in a manner that respects patient preferences and promotes equitable health care access. Diagnostic excellence minimizes errors, reduces unnecessary interventions, and optimizes resource utilization, ultimately leading to improved patient safety and satisfaction.
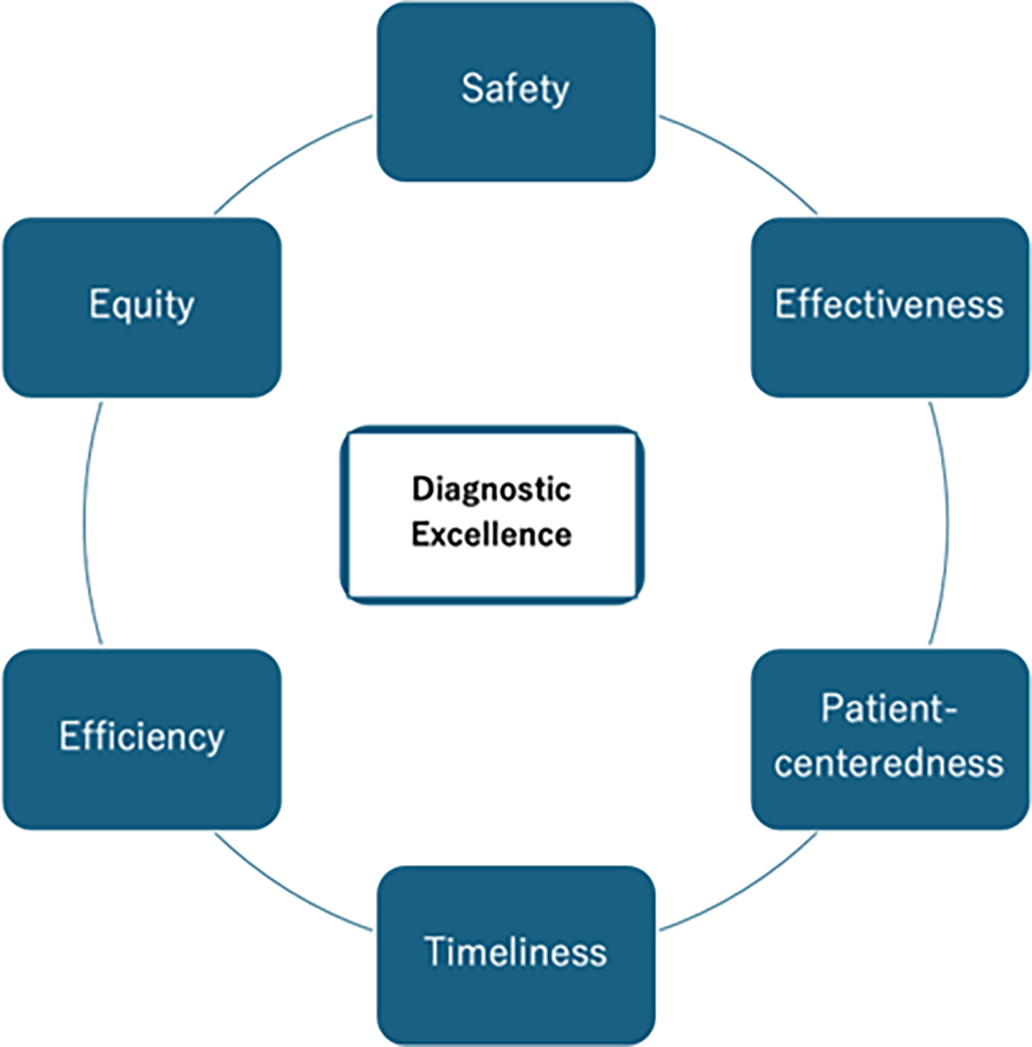
Figure 1: The concept of diagnostic excellence and components
2.3 Challenges in Medical Diagnosis
Despite advancements in medical science and technology, the diagnostic process remains inherently complex due to several factors. A primary challenge is the complexity and variability of diseases, often presenting with overlapping symptoms that complicate differential diagnosis. For example, common symptoms such as fever, fatigue, or pain may be associated with a wide range of differential diagnosis, leading to diagnostic uncertainty. Moreover, individual variations in how diseases manifest further complicate diagnosis, as patients may present atypical or subtle symptoms that do not align neatly with textbook cases. This variability makes differential diagnosis a significant challenge, requiring careful consideration and thorough investigation.
Another obstacle in accurate diagnosis arises from cognitive biases that can affect even experienced health care professionals. Cognitive biases, such as availability bias—where a diagnosis is influenced by recent or impressive cases—and confirmation bias—where evidence is interpreted in ways that support initial hypotheses—can distort clinical judgment. These biases often lead to diagnostic errors, particularly in high-pressure or time-constrained environments, where health care professionals might rely on mental shortcuts rather than exhaustive analysis.
Systemic factors within health care also contribute to diagnostic difficulties. Poor communication between different health care professionals, inefficiencies in workflows, and limited access to essential diagnostic tools or expertise can delay or mislead diagnosis. For example, a lack of proper communication between specialists and primary care providers may result in fragmented care, where important diagnostic details are overlooked. Similarly, health care facilities in resource-limited settings may not have the necessary diagnostic equipment or access to specialist consultation, further exacerbating diagnostic challenges.
Lastly, the sheer volume of clinical data that health care professionals must process represents a significant barrier to effective diagnosis. Modern health care generates a vast amount of information, from electronic health records (EHRs) to medical literature and diagnostic test results. While this data holds valuable insights, it can overwhelm health care professionals, making it difficult to synthesize and interpret the information effectively. Advanced support tools, such as clinical decision support systems, are essential in managing this information overload, providing analytical support that enhances diagnostic accuracy.
2.4 Enhancing Diagnostic Accuracy
Enhancing diagnostic accuracy in health care necessitates a comprehensive and multifaceted approach that tackles both individual and systemic challenges. One of the key elements in this effort is the continuous education and training of health care professionals. Ongoing education programs that focus on critical thinking, evidence-based practice, and the identification of cognitive biases can significantly improve diagnostic skills. Incorporating real-world case studies into education and training programs can provide practical insights, demonstrating how effective diagnostic strategies have led to successful patient outcomes [4]. These examples serve as powerful learning tools, reinforcing the application of theoretical knowledge to clinical practice.
Collaborative practices also play a vital role in enhancing diagnostic accuracy. Multidisciplinary collaboration and structured case discussions allow health care professionals to draw on diverse expertise and perspectives. When specialists from different fields come together to evaluate a case, they can share insights that might not be apparent to a single health care professional. This collective approach reduces the risk of diagnostic oversight, as each participant brings a unique lens to the analysis, leading to more comprehensive and well-rounded evaluations [5–7].
The integration of advanced technology, particularly AI-driven CDSS, is another critical component in improving diagnostic accuracy. These tools assist health care professionals by analyzing vast amounts of patient data, identifying patterns that might not be immediately evident, and generating differential diagnoses. By leveraging machine learning and sophisticated algorithms, AI can process complex datasets, including medical images, lab results, and electronic health records, to provide health care professionals with relevant diagnostic suggestions.
Ultimately, improving diagnostic accuracy is a collective endeavor that requires continuous investment in education, collaboration, and technological innovation.
2.5 Real-World Impact of Diagnostic Excellence
Achieving diagnostic excellence has a profound impact across various areas of health care, enhancing patient outcomes and the effectiveness of medical interventions. In chronic disease management, for example, the early and accurate diagnosis of conditions such as hypertension plays a pivotal role. When hypertension is identified at an early stage, health care professionals initiate timely interventions, including lifestyle modifications and, if necessary, pharmacological treatment. This proactive approach helps to prevent serious complications like ischemic heart disease and stroke.
In the field of oncology, diagnostic excellence is crucial for improving patient survival rates and quality of life. Prompt and accurate diagnosis of cancers, such as breast, lung, and colorectal cancer, allows for early treatment, which significantly improves survival rates and reduces morbidity. Early-stage cancers are often more treatable, and early intervention can prevent the disease from progressing to more advanced stages [8].
Infectious diseases present another area where diagnostic precision is vital, particularly in the care of immunocompromised patients. These patients are more susceptible to infections, and an accurate diagnosis is essential to ensure they receive the correct treatment promptly. By accurately identifying the causative pathogens, health care professionals can administer targeted antibiotic therapies, which help to minimize the use of broad-spectrum antibiotics. This approach, known as antibiotic stewardship, is critical in reducing the risk of antibiotic resistance, a growing global health threat.
As part of diagnostic excellence, patient-centered diagnostic excellence extends beyond clinical accuracy to embrace a comprehensive approach that includes the patient’s perspective. This approach involves valuing the patient’s knowledge alongside the health care professional’s insights. It emphasizes ensuring long-term follow-up with attention to the patient’s reports. Maintaining a balanced approach to diagnostic evaluations helps avoid over-or under-investigation. Enhancing the interpretability of diagnostic information for the patient is crucial. Finally, aligning clinical language with the patient’s understanding fosters a shared framework of care [9].
Diagnostic excellence also plays a key role in the emerging field of precision medicine, where detailed clinical assessments are integrated with advanced diagnostic modalities such as genetic testing, imaging, and biomarker analysis. This approach allows for the creation of personalized treatment plans that are tailored to the unique genetic and molecular profile of each patient. By understanding the specific characteristics of a patient’s condition, health care professionals can choose therapies that are more likely to be effective, enhancing therapeutic outcomes and improving the patient’s quality of life [10].
Overall, medical diagnosis is a critical component of health care that directly impacts patient outcomes and the overall effectiveness of medical interventions. While challenges persist, advancements in education, collaborative practices, and technological support offer promising avenues to enhance diagnostic accuracy and excellence. By striving for continuous improvement in diagnostic processes, the medical community can ensure that patients receive timely, accurate, and personalized care, ultimately elevating the standard of health care delivery.
3 Historical Perspective and Evolution of Diagnostic Methods
The evolution of medical diagnostics reflects the broader advancements in medical science and technology over centuries. From rudimentary observational techniques to sophisticated imaging and molecular diagnostics, each milestone has significantly enhanced the accuracy and efficiency of disease detection and management. Historical diagnostic errors, such as the delayed recognition of life-threatening conditions like dissecting aortic aneurysm and pericardial effusion with tamponade, highlight the importance of technological advancements and mitigating cognitive biases in reducing diagnostic uncertainties [11].
3.1 Early Diagnostic Practices
In ancient and medieval times, diagnosis primarily relied on clinical observations and patient-reported symptoms. Physicians assessed signs such as pulse, respiration, and visible abnormalities to infer underlying conditions. Tools like the stethoscope, introduced in the early 19th century by René Laennec, revolutionized auscultation, allowing for more precise evaluation of cardiac and pulmonary functions.
3.2 Development of Laboratory Diagnostics
The late 19th and early 20th centuries witnessed the emergence of laboratory diagnostics, fundamentally transforming medical practice. The ability to perform biochemical analyses of blood, urine, and other body fluids enabled the identification of metabolic and infectious diseases with greater specificity. For instance, the measurement of blood glucose levels became essential in diagnosing diabetes mellitus, while the detection of bacterial pathogens through cultures advanced the management of infectious diseases. Patient-centered diagnostic innovations, such as point-of-care testing for rapid glucose monitoring, emerged during this era, offering more personalized and immediate diagnostic feedback [12].
3.3 Advancements in Medical Imaging
The discovery of X-rays by Wilhelm Roentgen in 1895 was a groundbreaking development in medical diagnostics, providing a non-invasive means to visualize internal body structures. This innovation paved the way for subsequent imaging technologies such as Computed Tomography (CT) and Magnetic Resonance Imaging (MRI). CT scans offer detailed cross-sectional images of the body, facilitating the diagnosis of complex conditions like malignancy and vascular diseases. MRI utilizes magnetic fields and radio waves to produce high-resolution images of soft tissues, proving invaluable in neurological and musculoskeletal diagnostics.
Ultrasound technology, introduced in the mid-20th century, added another dimension to medical imaging by allowing real-time visualization of soft tissues and fluid-filled structures without ionizing radiation. The portability and safety of ultrasound have made it a staple in various clinical settings, including obstetrics, cardiology, and emergency medicine [13,14].
3.4 Molecular and Genetic Diagnostics
The advent of molecular biology and genetic engineering in the latter half of the 20th century ushered in a new era of diagnostics. Techniques such as Polymerase Chain Reaction (PCR) and DNA sequencing have enabled the precise identification of genetic mutations and infectious agents at the molecular level [15]. Current AI applications in molecular diagnostics include using machine learning to analyze genetic mutations rapidly, aiding in the diagnosis of hereditary diseases and guiding personalized treatment strategies [16]. These advancements have been crucial in diagnosing hereditary disorders, guiding personalized medicine, and managing infectious diseases through targeted therapies [17].
3.5 Integration of Digital Technologies
The late 20th and early 21st centuries have seen the integration of digital technologies into diagnostic practices. EHRs have streamlined the collection and analysis of patient data, enhancing the continuity and coordination of care [18]. Additionally, advancements in computational tools and data analytics have facilitated the development of CDSS, which assists health care professionals in making informed diagnostic and therapeutic decisions based on comprehensive data analysis.
3.6 Contemporary Diagnostic Innovations
Today, diagnostics continue to advance with the incorporation of cutting-edge technologies such as AI, machine learning, and large language models. These innovations promise to further enhance diagnostic accuracy, reduce turnaround times, and enable earlier detection of diseases. AI-driven diagnostic tools, such as deep learning models for analyzing histopathological slides, demonstrate the practical impact of modern diagnostic innovations. For example, AI-powered imaging analysis tools can detect subtle anomalies in radiological images that may be missed by the human eye, while nanotechnology-based sensors offer highly sensitive detection of biomarkers in bodily fluids.
The historical trajectory of medical diagnostics highlights the relentless pursuit of greater accuracy, efficiency, and comprehensiveness in disease detection and management, as shown in Fig. 2. The evolution begins with observational methods, emphasizing early diagnostic practices based on clinical observation and patient-reported symptoms. The next stage is marked by the stethoscope, symbolizing the transition to instrumental diagnostics in the early 19th century. This is followed by the emergence of laboratory diagnostics, which transformed medical practice through biochemical analyses of bodily fluids, enabling specific disease identification. The advancement continues with medical imaging, demonstrating innovations such as X-rays, CT scans, and MRI that provide non-invasive visualization of internal body structures. The introduction of molecular techniques represents the molecular biology revolution, including PCR and genetic sequencing that enhanced precision in diagnostics. The arrow culminates in AI in medicine, reflecting the latest developments in artificial intelligence and machine learning that offer advanced analytical capabilities for earlier and more accurate disease detection. Each technological advancement has built upon previous innovations, collectively transforming diagnostics from basic observational practices to highly sophisticated, multifaceted approaches. Understanding this evolution, including past diagnostic errors and the rise of patient-centered innovations, provides valuable context for appreciating current diagnostic capabilities and anticipating future developments that will continue to shape the landscape of health care.
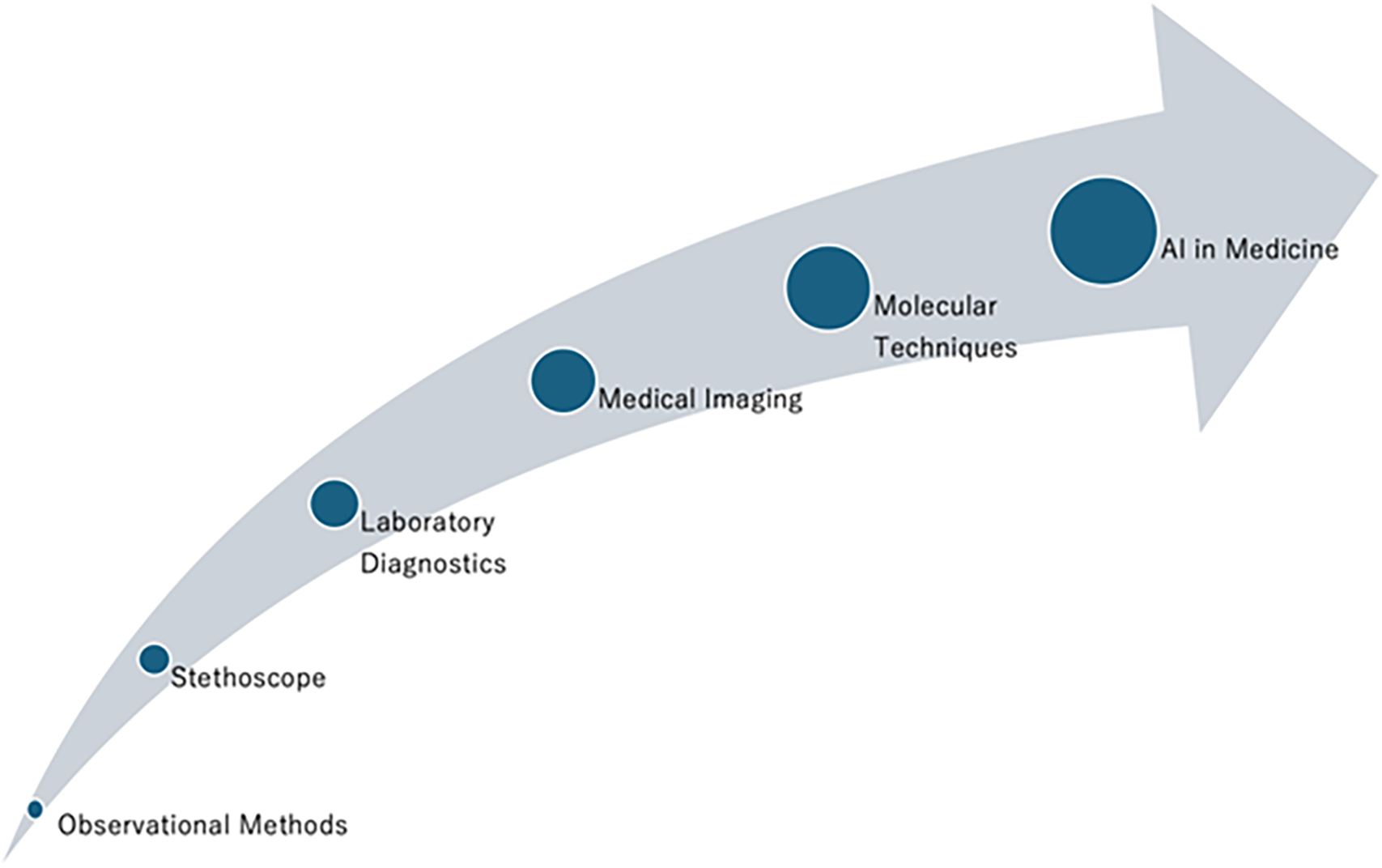
Figure 2: The historical evolution of diagnostic methods
4 The Complexity of Modern Diagnostics
Despite remarkable technological advancements, modern diagnostics remain inherently complex due to the intricate nature of human biology, the multifaceted presentation of diseases, and the dynamic interplay of various physiological systems. This complexity necessitates a nuanced approach to diagnosis, balancing empirical data with clinical intuition to achieve accurate and timely patient assessments.
4.1 Multifactorial Nature of Diseases
Many diseases exhibit a wide spectrum of symptoms that can overlap with other conditions, complicating the diagnostic process. For instance, autoimmune disorders like systemic lupus erythematosus can mimic infectious diseases or malignancies, while cardiovascular diseases may present non-specific symptoms such as fatigue and shortness of breath. This multifactorial nature requires health care professionals to consider a broad differential diagnosis and systematically narrow it down through targeted investigations [19].
Patient-specific factors, including genetics, lifestyle, comorbidities, and environmental exposures, contribute to variability in disease presentation and progression. Personalized medicine emphasizes the need to tailor diagnostic and therapeutic approaches to individual patient profiles. For example, pharmacogenomics examines how genetic variations affect drug metabolism, enabling more precise treatment plans that minimize adverse effects and enhance efficacy [20].
4.3 Cognitive Processes in Diagnosis
Effective diagnosis involves both intuitive and analytical cognitive processes. Heuristic thinking allows health care professionals to make rapid assessments based on pattern recognition and clinical experience, which is particularly valuable in emergency settings. Conversely, analytical thinking involves a deliberate and systematic evaluation of clinical data, laboratory results, and imaging studies to arrive at a comprehensive diagnosis. Balancing these cognitive approaches is essential for managing both common and complex cases [21]. The following Section 4.9 provides a detailed comparison between AI-driven diagnostics and these traditional cognitive processes.
4.4 Cognitive Biases and Diagnostic Errors
Cognitive biases can significantly impact diagnostic accuracy. Biases such as confirmation bias, where health care professionals favor information that supports their initial hypothesis, and availability bias, where recent or memorable cases influence current diagnoses, can lead to diagnostic errors. These biases may result in overlooking critical information or prematurely settling on an incorrect diagnosis [22]. Mitigating cognitive biases involves implementing structured diagnostic protocols, utilizing checklists, and encouraging second opinions. Continuous education and training in cognitive psychology for health care professionals can also enhance awareness and reduce the likelihood of bias-driven errors.
4.5 Systemic and Environmental Factors
The health care system’s structure and resources play a crucial role in the diagnostic process. Factors such as time constraints, workload, access to diagnostic tools, and interdisciplinary collaboration influence diagnostic efficiency and accuracy. Inadequate resources or fragmented care pathways can lead to delays in diagnosis, incomplete evaluations, and increased diagnostic uncertainty.
Enhancing systemic factors involves improving health care infrastructure, investing in advanced diagnostic technologies, and fostering collaborative environments where multidisciplinary teams can contribute their expertise to complex cases.
4.6 Information Overload and Data Integration
The exponential growth of medical knowledge and the availability of extensive patient data present challenges in information management. Health care professionals must efficiently synthesize vast amounts of data from EHRs, laboratory results, imaging studies, and genetic information to form accurate diagnoses. Effective data integration and management systems are essential to prevent information overload and ensure that relevant data informs clinical decision-making.
Advanced informatics tools, including AI-driven data analytics and decision support systems, can aid in managing information overload by highlighting pertinent data, identifying patterns, and suggesting potential diagnoses based on comprehensive data analysis.
4.7 Diagnostic Collaboration and Teamwork
Complex diagnostic scenarios often require the expertise of multiple specialists working collaboratively. Interdisciplinary teams bring diverse perspectives and specialized knowledge, enhancing the diagnostic process through collective reasoning and shared insights [23]. For example, tumor boards, a specific type of case conference, consist of oncologists, surgeons, radiologists, pathologists, nurse specialists, pharmacists, professionals from palliative medicine and mental health, and other specialists who gather to deliberate over cancer cases [24]. Promoting a culture of teamwork and open communication within health care settings is vital for optimizing diagnostic accuracy and ensuring comprehensive patient evaluations.
4.8 Technological Integration and Diagnostic Support
Integrating advanced technologies into the diagnostic workflow can alleviate some complexities by providing enhanced data analysis, visualization, and decision support. Tools such as CDSS, AI-powered imaging analysis, and molecular diagnostics can streamline the diagnostic process, reduce errors, and enable earlier detection of diseases. However, the effective integration of these technologies requires proper training, seamless workflow incorporation, and ongoing evaluation to ensure they complement rather than complicate the diagnostic process.
The complexity of modern diagnostics reflects the intricate interplay between diverse medical knowledge, patient variability, cognitive processes, and systemic factors, as illustrated in Fig. 3. The balance can illustrate a balanced scale metaphorically representing the challenges and corresponding resolutions in modern diagnostics. On the one hand, challenges include complexity, cognitive biases, and systemic and environmental factors. These elements highlight the multifaceted difficulties health care professionals face in diagnostic processes. Conversely, resolutions are presented as diagnostic teams, CDSS, and technological integration, demonstrating strategies to address the identified challenges. The balance of the scale signifies the need for equilibrium between challenges and solutions to optimize diagnostic accuracy and patient outcomes. Addressing these complexities requires a multifaceted approach that encompasses education, cognitive bias mitigation, systemic improvements, effective data management, collaborative practices, and the strategic integration of advanced technologies. By navigating these challenges, health care professionals can enhance diagnostic accuracy, improve patient outcomes, and advance the overall quality of health care delivery.
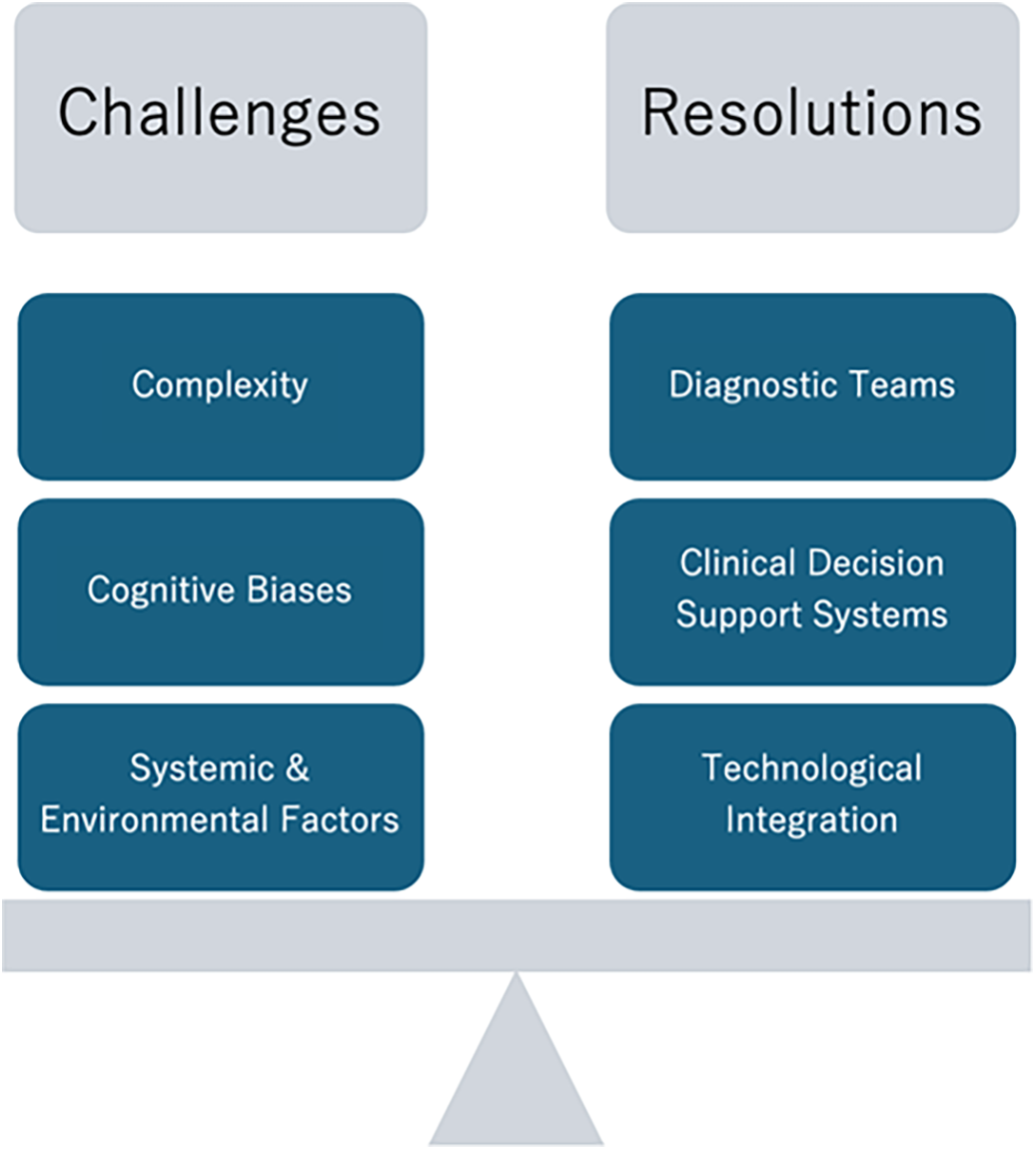
Figure 3: The factors of challenges and resolutions in modern diagnostics
4.9 Differentiating AI-Driven Diagnostics from Traditional Expert-Based Approaches
AI-driven diagnostic methods differ from traditional expert-based approaches, representing a transformative shift in contemporary medical diagnostics. Traditional diagnostic approaches heavily rely on health care professionals’ experience, intuition, and manual data interpretation of clinical data, often involving heuristic and analytical reasoning [21]. Conversely, AI-driven diagnostics utilize sophisticated machine learning algorithms capable of systematically analyzing vast datasets to uncover subtle or complex patterns that might otherwise go unnoticed in routine clinical assessments. This ability to identify nuanced patterns reduces cognitive biases such as confirmation and availability biases, common limitations inherent in human clinical judgment. By providing objective, data-driven insights, AI-driven diagnostics enhance consistency, reproducibility, and reliability of diagnostic outcomes. This systematic approach significantly mitigates variability in clinical practice, contributing to greater diagnostic precision and improved workflow efficiency [25,26].
Importantly, the integration of AI within clinical decision support systems complements rather than replaces human expertise [27]. By merging robust data-driven insights from AI with the clinical judgment and experience of healthcare professionals, diagnostic processes become more accurate, comprehensive, and less prone to errors associated with cognitive biases [28].
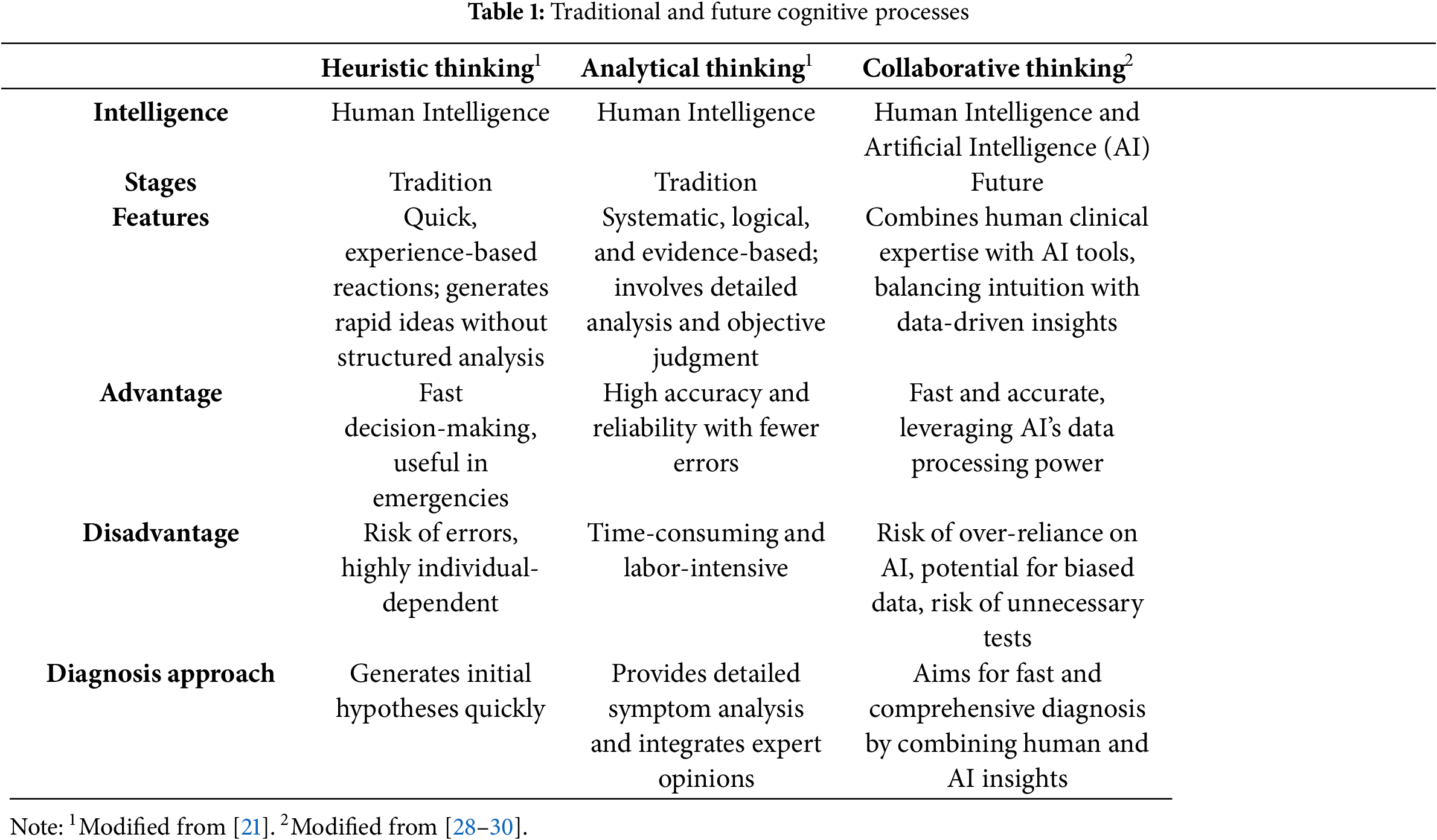
Table 1 summarizes key distinctions between heuristic, analytical, and collaborative diagnostic approaches, underling the complementary strengths of human intuition and AI analytical capabilities. Heuristic thinking emphasizes rapid, experience-based judgments suitable for urgent clinical decisions, while analytical thinking involves meticulous, evidence-based assessments. The collaborative approach combines these human cognitive strengths with AI’s systematic and unbiased analysis, presenting a holistic and highly effective method for achieving diagnostic excellence [29,30].
5 Overview of Diagnostic Clinical Decision Support Systems
CDSS have become essential tools in modern health care, assisting health care professionals by providing evidence-based recommendations and facilitating informed clinical decisions [31]. By integrating patient data with up-to-date medical knowledge, CDSS streamline clinical workflows, allowing health care professionals to deliver high-quality, efficient care.
5.1 Types of Clinical Decision Support Systems
CDSS can be broadly categorized into two types [32]:
• Knowledge-Based Systems: These systems operate on predefined rules and algorithms derived from clinical guidelines and expert knowledge. They function as advanced decision trees, symptom checkers, or differential diagnosis generators. For example, Isabel Pro utilizes a comprehensive database of medical knowledge to assist health care professionals in generating accurate differential diagnoses, thereby improving diagnostic accuracy by approximately 7%–8% [33]. However, real-world instances of knowledge-based CDSS failures, such as the early expert system MYCIN, have highlighted potential pitfalls [34]. While MYCIN demonstrated the potential of rule-based systems in diagnosing bacterial infections and recommending antibiotic treatments, it also revealed limitations, including challenges in accurately handling uncertain data and the need for continuous updates to maintain clinical relevance [35].
• Non-Knowledge-Based Systems: Leveraging artificial intelligence and machine learning, these systems analyze vast amounts of clinical data to identify patterns and make predictions. Unlike knowledge-based systems, they do not rely solely on static rules but can learn and adapt from new data inputs. This dynamic capability allows non-knowledge-based CDSS to provide more flexible and context-aware support in clinical decision-making. However, over-reliance on these systems can pose significant risks, such as when AI-driven tools have generated incorrect differential diagnoses due to biased or incomplete training data, demonstrating the potential dangers of unquestioned trust in AI-generated suggestions [36].
5.2 Integration of AI in Clinical Decision Support
The integration of AI into CDSS represents a transformative shift in health care, significantly enhancing the capabilities and functionality of these systems [37–39]. AI in this context refers to the simulation of human intelligence in machines, allowing them to process vast amounts of data, recognize patterns, and assist in diagnosing diseases. AI-driven systems are designed to learn from data and adapt to new information. This adaptability makes AI particularly valuable in complex medical environments where variability and subtle nuances are commonplace.
One of the key components driving the success of AI in CDSS is generative AI, a subset of AI that can create new data and scenarios based on existing patterns. In diagnostics, generative AI can predict disease outcomes or propose potential treatment paths by analyzing historical data, which is especially useful for simulating clinical scenarios or interpreting unstructured data like clinical notes. This ability to generate insights from data contributes to more personalized and accurate medical care. From unreviewed material, Articulate Medical Intelligence Explorer exhibited standalone performance that exceeded that of unassisted health care professionals (top 10 differentials accuracy 59% vs. 34%, p = 0.04). Comparing the two assisted study arms, the top 10 differentials accuracy was higher for health care professionals assisted by AI, compared to health care professionals without AI assistance (25%, p < 0.01) and health care professionals with Internet search (5%, p = 0.02) for difficult case challenges [40].
Neural networks (NN) play a crucial role in the integration of AI within CDSS [41]. These algorithms are designed to function in a way that mimics the pattern recognition capabilities of the human brain, as shown in Fig. 4. In health care, NNs can analyze complex data sets, such as medical images or patient histories, to detect patterns that may be overlooked by health care professionals. A specialized form of neural networks, known as Convolutional Neural Networks (CNNs), has been particularly effective in processing visual data, such as radiology and pathology images [42,43]. CNNs excel at recognizing spatial patterns and textures, making them ideal for identifying abnormalities in medical images.
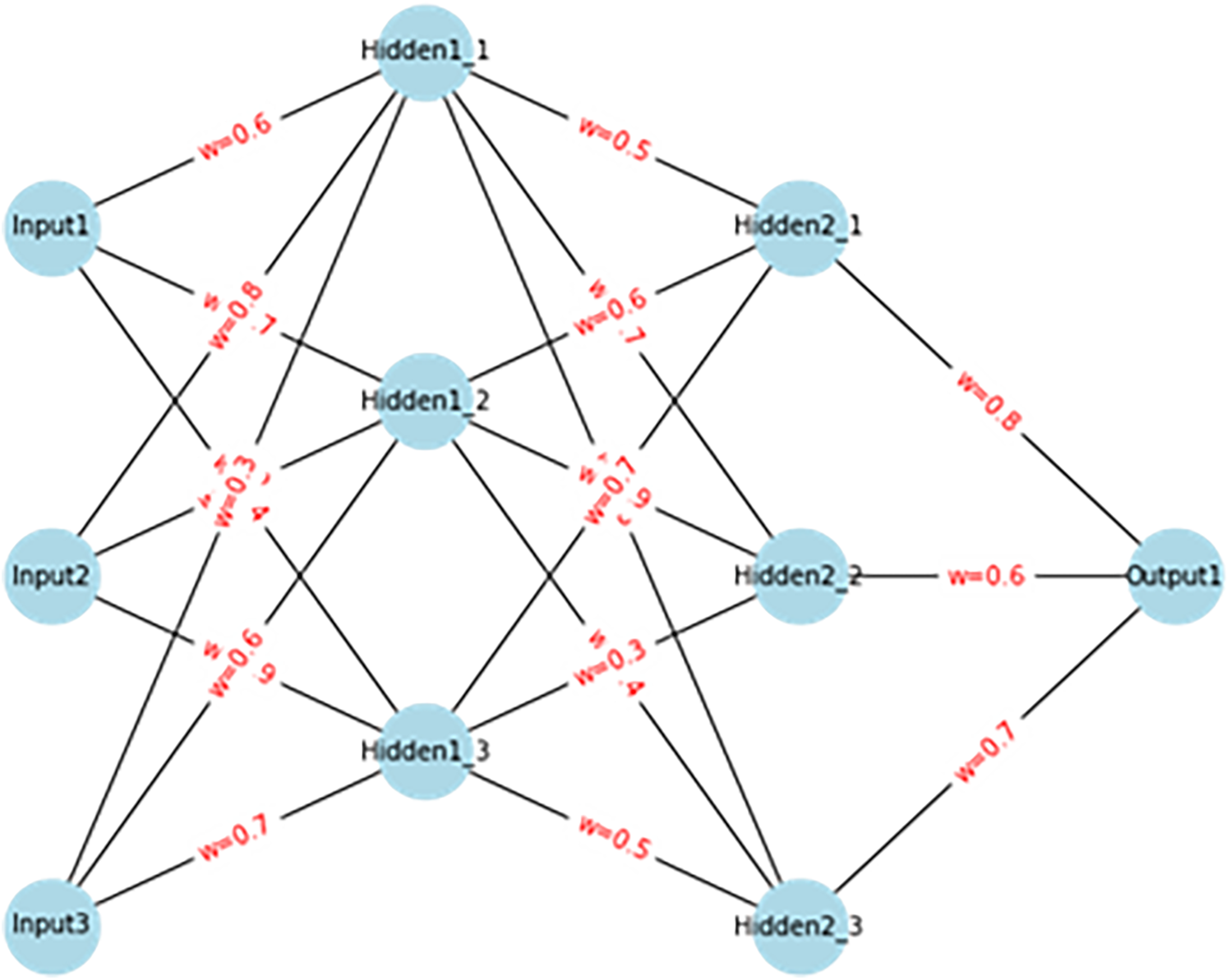
Figure 4: Three-layered neural network with weights
Another critical technology integrated into AI-enhanced CDSS is Natural Language Processing (NLP). NLP allows computers to understand and interpret human language, which is particularly useful for processing unstructured text, such as clinical notes, medical records, and research articles. In health care, NLP can convert this unstructured information into structured data that can be analyzed by AI systems. This enables AI to extract relevant medical insights from vast amounts of written material, thus providing health care professionals with key information that might otherwise be difficult to access or interpret efficiently [44].
Further extending the capabilities of NLP are Large Language Models (LLMs), which are advanced forms of NLP that can understand and generate human-like text. LLMs are trained in large corpora of medical literature, making them adept at tasks such as interpreting clinical notes, summarizing research findings, and even generating diagnostic suggestions. For example, LLMs can help health care professionals interpret complex patient cases by reviewing and synthesizing information from patient records and medical literature, thereby supporting more informed decision-making.
The integration of AI into CDSS marks a significant advancement, enhancing their functionality and effectiveness. AI-powered CDSS utilize complex algorithms, including neural networks and convolutional neural networks, to process and interpret large datasets, such as medical images and EHRs. These systems can identify subtle patterns and correlations that may elude health care professionals, thereby augmenting diagnostic precision and reducing the likelihood of errors.
Generative AI, encompassing technologies like NLP and LLMs such as GPT-4(o), GPT-4.5, Open AI-o1, or Open AI-o3 mini further extends the capabilities of CDSS [45–48]. Generative AI-enabled CDSS can interpret unstructured clinical notes, generate comprehensive diagnostic suggestions, and even simulate patient interactions to enhance clinical reasoning. This integration ensures that CDSS remains current with the latest medical research and clinical guidelines, continuously refining their recommendations based on emerging evidence.
5.3 Benefits of AI-Enhanced Clinical Decision Support
The integration of AI into CDSS has brought about significant improvements in diagnostic practices [49,50]. One of the primary advantages of AI-enhanced CDSS is the enhancement of diagnostic accuracy. AI algorithms can analyze complex datasets with high precision, identifying diagnostic clues that may be overlooked by human observers. This leads to more accurate and timely diagnosis, particularly in fields requiring detailed image analysis such as radiology and pathology, where AI can assist in identifying abnormalities or early signs of disease.
Moreover, AI-driven CDSS contribute to increased efficiency in clinical settings. These systems can process and interpret vast amounts of data rapidly, reducing the time health care professionals spend on simple diagnostic tasks. This efficiency allows health care professionals to focus more on patient care and complex decision-making. By automating routine data analysis, AI enables health care professionals to make quicker decisions, which is crucial in time-sensitive scenarios such as emergency medicine or intensive care.
Another key benefit of AI-enhanced CDSS is their ability to support personalized medicine. By integrating patient-specific data, including genetic information and medical history, AI-enhanced CDSS can tailor diagnostic and treatment recommendations to individual patient profiles. This personalization improves treatment efficacy and minimizes adverse effects. For instance, AI can analyze a patient’s genetic markers to predict how they might respond to a particular drug, thereby guiding health care professionals in choosing the most appropriate therapy.
AI-enhanced CDSS are also characterized by their capacity for continuous learning and adaptation. These systems can learn from new data inputs in real-time, allowing them to stay current with the latest medical advancements and clinical practices. This adaptability is crucial for maintaining the relevance and accuracy of diagnostic support.
In complex diagnostics scenarios, AI-driven CDSS play a critical role by offering comprehensive support. These systems can generate extensive differential diagnoses, suggest additional investigations, and even recommend consultations with specialists when necessary [25]. For example, in cases where a patient presents with ambiguous symptoms that could indicate multiple conditions, an AI-driven CDSS can analyze the available data and provide a prioritized list of possible diagnoses, along with recommendations for further diagnostic steps.
Overall, CDSSs, particularly those enhanced with AI technologies, are revolutionizing the diagnostic landscape in health care. By integrating advanced data analysis, pattern recognition, and continuous learning capabilities, AI-driven CDSS significantly improve diagnostic accuracy, efficiency, and personalization of patient care. As these systems continue to evolve, their role in supporting health care professionals will become increasingly vital, ultimately leading to enhanced patient outcomes and the advancement of medical practice.
6 The Potential of AI in Diagnostics
AI holds immense potential to transform medical diagnostics, offering advancements that enhance accuracy, efficiency, and personalized patient care. By leveraging sophisticated algorithms and vast datasets, AI technologies are reshaping how diseases are detected, analyzed, and managed across various medical disciplines.
AI plays a crucial role in genomics by facilitating the rapid and accurate analysis of complex genetic data. Genomic sequencing generates extensive information about an individual’s genetic makeup, which AI systems can process to identify genetic mutations and markers associated with specific diseases. This capability is fundamental to personalized medicine, enabling tailored treatment plans based on a patient’s unique genetic profile. For instance, AI-driven tools can predict susceptibility to hereditary conditions, guide the selection of targeted therapies, and monitor genetic variations that influence treatment responses [16,51].
Predictive analytics powered by AI utilize historical patient data and machine learning models to forecast future health events. This proactive approach is particularly beneficial in managing chronic diseases, where early prediction of complications can lead to timely interventions. For example, AI systems can monitor diabetic patients to predict hypoglycemic episodes, allowing for preemptive adjustments in insulin dosage [52,53]. Similarly, in cardiology, AI can analyze patterns in patient data to predict the likelihood of heart failure exacerbations, enabling preventative measures that reduce hospital admissions and improve patient quality of life [54,55]. However, not all predictive analytics initiatives have been successful. For example, IBM Watson has faced challenges in practical implementation [56]. This example highlights the complexities of translating predictive analytics into practical clinical settings.
6.3 Efficiency and Early Detection
AI enhances diagnostic efficiency and facilitates early detection of diseases by automating data analysis and identifying subtle anomalies that may be missed by health care professionals. In oncology, AI algorithms analyze imaging data to detect early signs of tumors, significantly improving the chances of successful treatment. In ophthalmology, AI-powered screening tools identify diabetic retinopathy and glaucoma at stages when intervention can prevent vision loss [57,58]. Pathology benefits from AI through the automated analysis of tissue samples, enabling rapid and accurate identification of cancerous cells [59,60]. These applications demonstrate AI’s ability to streamline diagnostic processes, reduce turnaround times, and enable earlier therapeutic interventions, ultimately leading to better patient outcomes.
6.4 Case Studies Demonstrating AI Success
Several real-world applications illustrate the transformative impact of AI in diagnostics across a variety of medical specialties. In oncology, IBM’s Watson for Oncology exemplifies AI’s potential in cancer care. By analyzing extensive medical literature, clinical trial data, and patient records, Watson provides evidence-based treatment recommendations tailored to individual patient profiles. Clinical studies have shown concordance rates as high as 96% between Watson’s suggestions and those of expert oncologists, highlighting AI’s role in enhancing clinical decision-making and supporting more personalized cancer care [61,62].
In the field of radiology, AI algorithms in radiology can rapidly analyze thousands of medical images with high accuracy [63]. For instance, AI systems have demonstrated superior performance in detecting breast cancer in mammograms compared to traditional methods, achieving reduced false positives, improved sensitivity, and nearly a 7% increase in the area under the curve, enabling earlier intervention [64]. Other AI systems have shown strong performance in detecting pulmonary tuberculosis in chest X-rays, achieving 97% accuracy, 99% area under the curve, 92% sensitivity, and 98% specificity on multiclass classification datasets [65,66]. This enhanced accuracy can significantly improve patient outcomes by enabling prompt treatment.
AI has also made significant strides in pathology. AI-driven image analysis in pathology assists in identifying cancerous cells within tissue samples, increasing diagnostic accuracy and consistency. This capability not only speeds up the diagnostic process but also supports pathologists in making more informed treatment decisions [59]. In the milestone CAMELYON16 challenge for whole-slide image classification, the best AI algorithm achieved an impressive area under the curve of 99% (95% CI, 98%–99%), significantly outperforming pathologists in a diagnostic simulation (mean area under the curve, 81% [95% CI, 74%–88%]; p < 0.001) [67].
In ophthalmology, AI tools have been developed to screen retinal diseases, such as diabetic retinopathy and glaucoma. These systems can detect early signs of these retinal diseases, allowing for timely intervention that can prevent irreversible vision loss. For instance, AI has achieved a 91% accuracy rate in classifying bacterial and fungal keratitis and an area under the curve of 91% in differentiating various corneal diseases [68]. These tools are particularly valuable in underserved areas with limited access to specialized ophthalmologists [57,69].
Dermatology has similarly benefited from AI technology, particularly in the analysis of skin lesions. AI-based systems can compare images of lesions against extensive databases to assess the risk of skin cancer. For nonmelanoma skin cancer, AI algorithms applied to all imaging modalities combined achieved an average accuracy of 87%, with the same accuracy observed for dermoscopy. Additionally, AI-based algorithms achieved a higher receiver operating characteristic, more than 80%, in the detection of melanoma, demonstrating robust performance in clinical settings. This preliminary risk assessment helps dermatologists identify suspicious lesions at an early stage, guiding further diagnostic procedures and enabling early treatment that improves patient outcomes [70,71].
The integration of AI in gastrointestinal endoscopy represents another significant advancement. AI algorithms analyze live video feeds to detect abnormalities such as polyps and tumors in real-time, enhancing diagnostic accuracy and reducing the likelihood of missed lesions [72,73]. This capability enhances diagnostic accuracy, reduces the likelihood of missed lesions, and assists gastroenterologists in making immediate decisions during procedures. A systematic analysis demonstrated that the pooled adenoma detection rate was significantly higher in the AI systems with real-time computer-aided polyp detection group than in the control group (37% vs. 25%; p < 0.01), highlighting AI’s role in improving detection rates and supporting gastroenterologists in making immediate decisions during procedures [74].
In psychiatry, studies involving electroencephalogram-based deep learning methods, such as one- or two-dimensional convolutional neural networks, have demonstrated the ability to discriminate depressive patients from healthy controls with approximately 99% accuracy [75]. While AI in psychiatry has shown promise [76,77], its limitations are more pronounced. AI applications that analyze speech patterns and facial expressions to identify mental health conditions often struggle with cultural and linguistic diversity, leading to inconsistent diagnostic outcomes. Addressing these challenges requires more diverse training datasets and collaboration with mental health professionals to refine AI tools for psychiatric use.
Collectively, these case studies demonstrate the diverse applications and benefits of AI across multiple medical fields. Whether through improving the accuracy of cancer detection, enhancing real-time decision-making during procedures, or supporting early intervention in chronic conditions, AI is proving to be an indispensable tool in modern diagnostics. The quantitative evaluation of AI performance in diagnostics is shown as Table 2.
7 The Limitations of AI in Diagnostics
While AI has ushered in transformative advancements in medical diagnostics, several significant limitations must be acknowledged to ensure its effective and ethical integration into clinical practice. One of the foremost challenges lies in the technical complexities associated with AI systems. Despite their ability to process vast datasets, AI algorithms can struggle with the inherent variability and multifaceted nature of medical data. Diseases often present with overlapping symptoms and diverse manifestations, making it difficult for AI to accurately differentiate between similar conditions without extensive and diverse training data.
7.1 Medical Approval and Regulatory Challenges
Regulatory and medical approval processes pose another substantial barrier. The stringent requirements for safety, efficacy, and reliability mean that many AI diagnostic tools face prolonged approval timelines, delaying their availability in clinical settings. Additionally, the rapid pace of AI development can outstrip the ability of regulatory frameworks to keep up, creating gaps in oversight and standardization [78].
Regulatory approaches to AI in diagnostics vary across different countries, reflecting distinct legal, ethical, and cultural considerations. For example, the European Union (EU) has introduced the AI Act, which categorizes AI applications based on risk levels and imposes stringent requirements on high-risk applications, including medical diagnostics. The EU framework emphasizes transparency, accountability, and human oversight, aligning with its broader General Data Protection Regulation to safeguard patient data privacy [79]. In the United States, the Food and Drug Administration has developed a framework for the regulation of AI-based medical devices through its Digital Health Innovation Action Plan [80]. This framework adopts a risk-based approach, focusing on the software as a medical device category and promoting adaptive regulatory practices for continuously learning AI systems.
This expanded discussion of international AI regulations provides a clearer understanding of the regulatory hurdles mentioned earlier in the manuscript and highlights the importance of aligning technological advancements with ethical and legal standards in global health care practices.
7.2 Ethical Concerns and the Risk of AI Tools
Ethical concerns further complicate the deployment of AI in diagnostics [78,81]. Transparency and explainability are critical issues, as many AI models, particularly deep learning systems, operate as “black boxes” with decision-making processes that are not easily interpretable by health care professionals [82,83]. Instead of solely emphasizing transparency, practical methods for enhancing AI explainability should be implemented. These methods include using interpretable models, such as rule-based systems, incorporating visual explanations of AI-generated diagnostics, and providing confidence scores that help health care professionals gauge the reliability of AI outputs [84].
Moreover, data protection and patient privacy are paramount, as AI systems require access to large amounts of sensitive patient data [85]. Ensuring robust data security and addressing biases in training datasets are essential to prevent disparities in diagnostic accuracy across different patient populations.
The risk of misinformation, often referred to as “hallucination,” is another significant limitation [86,87]. AI systems can sometimes generate incorrect or misleading diagnostic suggestions. These errors can arise from biases in training datasets, algorithmic limitations, or external data anomalies. Real-world case studies illustrate how AI hallucinations have led to diagnostic errors, such as neural networks misdiagnosing skin cancers by latching onto confounders like background colors vs. meaningful morphological features [88]. Such cases emphasize the need for robust validation and monitoring mechanisms to detect and correct these errors promptly. Additionally, this highlights the need for continuous monitoring, validation, and updating of AI tools to maintain their reliability and accuracy [89].
Furthermore, the potential for misuse and over-reliance on AI tools presents serious concerns. Health care professionals may become overly dependent on AI recommendations, leading to reduced clinical judgment and delayed diagnoses when AI systems fail or provide inaccurate outputs. This over-reliance can compromise patient care, particularly in critical situations where swift and accurate decision-making is essential [90].
Addressing these limitations requires a multifaceted approach, including the development of more transparent and explainable AI models, rigorous regulatory standards, comprehensive training for health care professionals, and ongoing efforts to ensure data quality and diversity [91]. By acknowledging and proactively addressing these challenges, the medical community can better harness the benefits of AI while mitigating its risks, as shown in Fig. 5.
Figure 5: The concept of potential and limitations of artificial intelligence in medical diagnostics
8 The Future Direction of AI in Diagnostics
The future of AI in medical diagnostics is poised to be shaped by continued technological innovation, evolving regulatory frameworks. This section explores the key areas that will shape the future of AI in medical diagnostics, including technological advancements, ethical considerations, evolving roles of health care professionals, addressing global health disparities, fostering continued innovation and investment, and solutions or guidelines for responsible AI implementation.
The future of AI in medical diagnostics is poised to be shaped by continued technological innovation, evolving regulatory frameworks, and the dynamic interplay between AI systems and health care professionals. As machine learning and deep learning technologies advance, AI models are expected to become increasingly sophisticated, capable of handling more complex and multimodal data. This evolution will enhance their ability to integrate diverse data sources, including genomic information, medical imaging, and EHRs, providing a more comprehensive understanding of patient health.
Multimodal AI, which combines textual and visual data, represents a significant frontier in diagnostic technology. By effectively synthesizing information from various modalities, such as clinical notes and imaging studies, multimodal AI can offer more accurate and context-aware diagnostic insights. This integration is particularly crucial for complex cases where multiple data streams must be considered simultaneously to arrive at an accurate diagnosis [92].
Genomic data integration with AI will further revolutionize diagnostics by enabling personalized medicine approaches. AI systems that analyze genetic information alongside clinical data can identify unique genetic markers associated with specific diseases, allowing for tailored treatment plans that optimize efficacy and minimize adverse effects. This personalized approach not only enhances diagnostic precision but also fosters the development of targeted therapies that address the root causes of diseases at the molecular level [51].
8.2 Ethical Frameworks and Regulation
Ethical frameworks and regulatory standards will play a pivotal role in shaping the future of AI in diagnostics. Given the complexity of ethical considerations, it is essential to establish a multifaceted ethical framework that not only promotes transparency and fairness but also ensures accountability and human oversight in AI-driven decisions. This involves developing ethical guidelines that address issues such as bias mitigation, patient autonomy, and the ethical use of patient data. A more detailed ethical framework could include specific protocols for managing AI-driven clinical errors, guidelines for maintaining patient trust, and strategies for addressing disparities in AI’s diagnostic performance across different demographic groups [93].
Financial and resource barriers are critical factors influencing global AI adoption. Implementing AI solutions in low-resource settings requires strategies that ensure affordability, scalability, and support for infrastructure development. Addressing these barriers involves creating cost-effective AI tools, offering training programs for health care professionals in underserved areas, and establishing international partnerships to share resources and expertise [94]. To implement responsible AI effectively, stakeholders must adopt comprehensive guidelines addressing transparency, ethical use of patient data, continual monitoring for biases, rigorous validation processes, and explicit policies for human-AI collaboration to maintain patient safety and uphold ethical standards [95,96].
8.3 Evolving Role of Health Care Professionals in an AI-Driven World
The role of health care professionals will also evolve in an AI-driven diagnostic landscape. Rather than replacing health care professionals, AI will serve as a powerful decision support tool, augmenting the diagnostic capabilities of health care professionals. Medical education and training programs will need to incorporate AI literacy, equipping health care professionals with the skills to effectively interpret and utilize AI-generated insights. Incorporating case studies of successful AI-human collaboration in diagnostics can highlight the best practices and guide training programs. This collaborative relationship between AI and health care professionals will be essential for optimizing patient care and ensuring that AI tools are used to their fullest potential [97,98].
8.4 Addressing Global Health Disparities
Addressing global health disparities is another critical aspect of the future direction of AI in diagnostics. AI-powered diagnostic tools have the potential to extend specialized medical services to underserved and remote populations, bridging gaps in health care access and equity. By leveraging AI’s capabilities, health care systems can provide high-quality diagnostic services in regions with limited access to medical specialists, thereby improving health outcomes on a global scale [94,99].
Innovative projects, such as mobile diagnostics using AI-powered devices and telemedicine platforms integrated with AI, demonstrate practical solutions for reaching remote communities [100]. These initiatives not only improve diagnostic accuracy but also enhance real-time clinical support in geographically isolated settings.
8.5 Continued Innovation and Investment
Continued innovation and investment in AI research and development will drive the advancement of diagnostic technologies. Collaborative efforts between governments, private sectors, and international health organizations will be essential for funding and implementing AI solutions that can be scaled globally. These partnerships will facilitate the development of AI tools that are adaptable to diverse health care settings and responsive to the evolving needs of populations worldwide [99].
A clearer roadmap for future advancements should focus on establishing measurable goals, such as reducing diagnostic errors by a specific percentage, expanding AI’s use in rural health care, and developing AI models that adapt to regional health care challenges. Additionally, promoting open-source AI initiatives and creating regulatory sandboxes where new AI technologies can be tested in a controlled environment could accelerate innovation while maintaining safety and efficacy standards [83].
Artificial Intelligence has undeniably transformed the landscape of medical diagnostics, offering unprecedented advancements in accuracy, efficiency, and personalized patient care. From enhancing imaging techniques and facilitating genomic analysis to supporting complex clinical decision-making, AI’s role in diagnostics is both profound and far-reaching. The ability of AI systems to process and analyze vast amounts of data with speed and precision addresses some of the longstanding challenges in traditional diagnostic processes, such as human error and the limitations of manual data interpretation.
As AI technologies continue to evolve, their integration into diagnostics promises even greater improvements in early disease detection, tailored treatment strategies, and overall patient outcomes. However, this integration is not without its challenges. In addition to technical limitations, regulatory hurdles, and ethical concerns, there are practical challenges related to the adoption of AI tools in everyday clinical practice. These include the need for clear clinical guidelines, improved interoperability with existing health systems, and strategies to overcome resistance to technological adoption among health care professionals. Addressing these challenges through robust ethical frameworks, stringent regulatory standards, and comprehensive training for health care professionals will be essential for the responsible and effective deployment of AI in clinical settings.
The future of medical diagnostics lies in the seamless collaboration between AI systems and health care professionals, fostering a hybrid approach that leverages the strengths of both. AI will serve as a powerful augmentative tool, enhancing the diagnostic capabilities of health care professionals and enabling more informed and timely decision-making. To ensure practical implementation, a concrete action plan is needed. This should involve establishing standardized protocols for AI integration, promoting interdisciplinary collaboration, and setting measurable goals for evaluating the impact of AI on diagnostic accuracy and patient outcomes.
Moreover, AI’s potential to bridge global health disparities by extending specialized diagnostic services to underserved and remote populations highlights its significance in promoting equitable health care access. By making high-quality diagnostic tools more accessible, AI can play a pivotal role in improving health outcomes on a global scale.
Future research should focus on identifying knowledge gaps related to AI’s diagnostic performance in diverse clinical scenarios, developing adaptive AI systems that learn from real-world clinical data, and exploring the ethical implications of AI-driven diagnostics. Additionally, studies that assess the long-term impact of AI integration on clinical workflows and patient outcomes will provide valuable insights for optimizing these technologies.
In summary, AI’s integration into medical diagnostics represents a transformative shift that holds immense promise for enhancing the quality and accessibility of health care. By continuing to develop and refine AI technologies, addressing associated challenges thoughtfully and ethically, and fostering collaborative relationships between AI and health care professionals, the field of diagnostics can achieve significant advancements. These developments will not only improve patient outcomes but also shape the future of medicine, making health care more personalized, efficient, and equitable for all.
Acknowledgement: This study was made possible using the resources from the Department of Diagnostic and Generalist Medicine, Dokkyo Medical University.
Funding Statement: This research was funded by JSPS KAKENHI (grant number 22K10421).
Author Contributions: The authors confirm contribution to the paper as follows: Conceptualization, Takanobu Hirosawa; methodology, Takanobu Hirosawa; software, Takanobu Hirosawa; validation, Takanobu Hirosawa; formal analysis, Takanobu Hirosawa; investigation, Takanobu Hirosawa; resources, Takanobu Hirosawa; data curation, Takanobu Hirosawa; writing—original draft preparation, Takanobu Hirosawa; writing—review and editing, Takanobu Hirosawa; visualization, Takanobu Hirosawa; supervision, Taro Shimizu; project administration, Takanobu Hirosawa; funding acquisition, Takanobu Hirosawa. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Not applicable.
Ethics Approval: Not applicable.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
References
1. Haug CJ, Drazen JM. Artificial intelligence and machine learning in clinical medicine, 2023. New Engl J Med. 2023;388(13):1201–8. doi:10.1056/NEJMra2302038. [Google Scholar] [PubMed] [CrossRef]
2. Kaul V, Enslin S, Gross SA. History of artificial intelligence in medicine. Gastrointest Endosc. 2020;92(4):807–12. doi:10.1016/j.gie.2020.06.040. [Google Scholar] [PubMed] [CrossRef]
3. Dennehy D, Griva A, Pouloudi N, Dwivedi YK, Mäntymäki M, Pappas IO. Artificial intelligence (AI) and information systems: perspectives to responsible AI. Inf Syst Front. 2023;25(1):1–7. doi:10.1007/s10796-022-10365-3. [Google Scholar] [CrossRef]
4. Li MD, Little BP. Appropriate reliance on artificial intelligence in radiology education. J Am Coll Radiol. 2023;20(11):1126–30. doi:10.1016/j.jacr.2023.04.019. [Google Scholar] [PubMed] [CrossRef]
5. Radcliffe K, Lyson HC, Barr-Walker J, Sarkar U. Collective intelligence in medical decision-making: a systematic scoping review. BMC Med Inform Decis Mak. 2019;19(1):158. doi:10.1186/s12911-019-0882-0. [Google Scholar] [CrossRef]
6. Blanchard MD, Herzog SM, Kämmer JE, Zöller N, Kostopoulou O, Kurvers RHJM. Collective intelligence increases diagnostic accuracy in a general practice setting. Med Decis Making. 2024;44(4):451–62. doi:10.1177/0272989X241241001. [Google Scholar] [PubMed] [CrossRef]
7. Barnett ML, Boddupalli D, Nundy S, Bates DW. Comparative accuracy of diagnosis by collective intelligence of multiple physicians vs individual physicians. JAMA Netw Open. 2019;2(3):e190096. doi:10.1001/jamanetworkopen.2019.0096. [Google Scholar] [PubMed] [CrossRef]
8. Iranmakani S, Mortezazadeh T, Sajadian F, Ghaziani MF, Ghafari A, Khezerloo D, et al. A review of various modalities in breast imaging: technical aspects and clinical outcomes. Egypt J Radiol Nucl Med. 2020;51(1):57. doi:10.1186/s43055-020-00175-5. [Google Scholar] [CrossRef]
9. Berwick DM. Diagnostic excellence through the lens of patient-centeredness. JAMA. 2021;326(21):2127–8. doi:10.1001/jama.2021.19513. [Google Scholar] [PubMed] [CrossRef]
10. Castaneda C, Nalley K, Mannion C, Bhattacharyya P, Blake P, Pecora A, et al. Clinical decision support systems for improving diagnostic accuracy and achieving precision medicine. J Clin Bioinforma. 2015;5(1):4. doi:10.1186/s13336-015-0019-3. [Google Scholar] [PubMed] [CrossRef]
11. Schiff GD, Kim S, Abrams R, Cosby K, Lambert B, Elstein AS, et al. Diagnosing diagnosis errors: lessons from a multi-institutional collaborative project. In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in patient safety: from research to implementation (volume 2: concepts and methodology). Rockville (MDAgency for Healthcare Research and Quality (US); 2005 Feb. [Google Scholar]
12. Lilly CM, Soni AV, Dunlap D, Hafer N, Picard MA, Buchholz B, et al. Advancing point-of-care testing by application of machine learning techniques and artificial intelligence. CHEST. 2025;167(1):152–9. doi:10.1016/j.chest.2024.03.051. [Google Scholar] [PubMed] [CrossRef]
13. Andersen CA, Holden S, Vela J, Rathleff MS, Jensen MB. Point-of-care ultrasound in general practice: a systematic review. Ann Fam Med. 2019;17(1):61–9. doi:10.1370/afm.2330. [Google Scholar] [PubMed] [CrossRef]
14. Popat A, Harikrishnan S, Seby N, Sen U, Patel SK, Mittal L, et al. Utilization of point-of-care ultrasound as an imaging modality in the emergency department: a systematic review and meta-analysis. Cureus. 2024;16(1):e52371. doi:10.7759/cureus.52371. [Google Scholar] [PubMed] [CrossRef]
15. Kubista M, Andrade JM, Bengtsson M, Forootan A, Jonák J, Lind K, et al. The real-time polymerase chain reaction. Mol Aspects Med. 2006;27(2):95–125. doi:10.1016/j.mam.2005.12.007. [Google Scholar] [PubMed] [CrossRef]
16. Dias R, Torkamani A. Artificial intelligence in clinical and genomic diagnostics. Genome Med. 2019;11(1):70. doi:10.1186/s13073-019-0689-8. [Google Scholar] [PubMed] [CrossRef]
17. Ashley EA. Towards precision medicine. Nat Rev Genet. 2016;17(9):507–22. doi:10.1038/nrg.2016.86. [Google Scholar] [PubMed] [CrossRef]
18. Häyrinen K, Saranto K, Nykänen P. Definition, structure, content, use and impacts of electronic health records: a review of the research literature. Int J Med Inform. 2008;77(5):291–304. doi:10.1016/j.ijmedinf.2007.09.001. [Google Scholar] [PubMed] [CrossRef]
19. Cho JH, Gregersen PK. Genomics and the multifactorial nature of human autoimmune disease. New Engl J Med. 2011;365(17):1612–23. doi:10.1056/NEJMra1100030. [Google Scholar] [PubMed] [CrossRef]
20. Pirmohamed M. Pharmacogenetics: past, present and future. Drug Discov Today. 2011;16(19):852–61. doi:10.1016/j.drudis.2011.08.006. [Google Scholar] [PubMed] [CrossRef]
21. Balogh EP, Miller BT, Ball JR. Improving diagnosis in health care. Washington, DC, USA: National Academies Press; 2015. [Google Scholar]
22. Loncharich MF, Robbins RC, Durning SJ, Soh M, Merkebu J. Cognitive biases in internal medicine: a scoping review. Diagnosis. 2023;10(3):205–14. doi:10.1515/dx-2022-0120. [Google Scholar] [PubMed] [CrossRef]
23. Singh H, Connor DM, Dhaliwal G. Five strategies for clinicians to advance diagnostic excellence. BMJ. 2022;376:e068044. doi:10.1136/bmj-2021-068044. [Google Scholar] [PubMed] [CrossRef]
24. Specchia ML, Frisicale EM, Carini E, Di Pilla A, Cappa D, Barbara A, et al. The impact of tumor board on cancer care: evidence from an umbrella review. BMC Health Serv Res. 2020;20(1):73. doi:10.1186/s12913-020-4930-3. [Google Scholar] [PubMed] [CrossRef]
25. Restrepo D, Rodman A, Abdulnour RE. Conversations on reasoning: large language models in diagnosis. J Hosp Med. 2024;19(8):731–5. doi:10.1002/jhm.13378. [Google Scholar] [PubMed] [CrossRef]
26. Zheng N, Liu Z, Ren P, Ma Y, Chen S, Yu S, et al. Hybrid-augmented intelligence: collaboration and cognition. Front Inf Technol Electron Eng. 2017;18(2):153–79. doi:10.1631/FITEE.1700053. [Google Scholar] [CrossRef]
27. Karches KE. Against the iDoctor: why artificial intelligence should not replace physician judgment. Theor Med Bioeth. 2018;39(2):91–110. doi:10.1007/s11017-018-9442-3. [Google Scholar] [PubMed] [CrossRef]
28. Jarrahi MH, Lutz C, Newlands G. Artificial intelligence, human intelligence and hybrid intelligence based on mutual augmentation. Big Data Soc. 2022;9(2):20539517221142824. doi:10.1177/20539517221142824. [Google Scholar] [CrossRef]
29. Hirosawa T, Suzuki T, Shiraishi T, Hayashi A, Fujii Y, Harada T, et al. Adapting artificial intelligence concepts to enhance clinical decision-making: a hybrid intelligence framework. Int J Gen Med. 2024;17:5417–22. doi:10.2147/IJGM.S497753. [Google Scholar] [PubMed] [CrossRef]
30. Bellini V, Badino M, Maffezzoni M, Bezzi F, Bignami E. Evolution of hybrid intelligence and its application in evidence-based medicine: a review. Med Sci Monit. 2023;29:e939366. doi:10.12659/MSM.939366. [Google Scholar] [PubMed] [CrossRef]
31. Bright TJ, Wong A, Dhurjati R, Bristow E, Bastian L, Coeytaux RR, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157(1):29–43. doi:10.7326/0003-4819-157-1-201207030-00450. [Google Scholar] [PubMed] [CrossRef]
32. Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. npj Digital Med. 2020;3(1):17. doi:10.1038/s41746-020-0221-y. [Google Scholar] [PubMed] [CrossRef]
33. Sibbald M, Monteiro S, Sherbino J, LoGiudice A, Friedman C, Norman G. Should electronic differential diagnosis support be used early or late in the diagnostic process? A multicentre experimental study of Isabel. BMJ Qual Saf. 2022;31(6):426–33. doi:10.1136/bmjqs-2021-013493. [Google Scholar] [PubMed] [CrossRef]
34. Yu VL, Buchanan BG, Shortliffe EH, Wraith SM, Davis R, Scott AC, et al. Evaluating the performance of a computer-based consultant. Comput Programs Biomed. 1979;9(1):95–102. doi:10.1016/0010-468X(79)90022-9. [Google Scholar] [PubMed] [CrossRef]
35. Delipetrev B, Tsinaraki C, Kostic U. Historical evolution of artificial intelligence. Luxembourg: Publications Office of the European Union; 2020. [Google Scholar]
36. Saenger JA, Hunger J, Boss A, Richter J. Delayed diagnosis of a transient ischemic attack caused by ChatGPT. Wien Klin Wochenschr. 2024;136(7–8):236–8. doi:10.1007/s00508-024-02329-1. [Google Scholar] [PubMed] [CrossRef]
37. Sai S, Gaur A, Sai R, Chamola V, Guizani M, Rodrigues JJPC. Generative AI for transformative healthcare: a comprehensive study of emerging models, applications, case studies, and limitations. IEEE Access. 2024;12:31078–106. doi:10.1109/ACCESS.2024.3367715. [Google Scholar] [CrossRef]
38. Raiaan MAK, Mukta MSH, Fatema K, Fahad NM, Sakib S, Mim MMJ, et al. A review on large language models: architectures, applications, taxonomies, open issues and challenges. IEEE Access. 2024;12(8):26839–74. doi:10.1109/ACCESS.2024.3365742. [Google Scholar] [CrossRef]
39. Aschenbrenner L. Situational awareness: the decade ahead [Internet]. 2024 [cited 2025 Apr 15]. Available from: https://situational-awareness.ai/wp-content/uploads/2024/06/situationalawareness.pdf. [Google Scholar]
40. Karthikesalingam A, Natarajan P. AMIE: a research AI system for diagnostic medical reasoning and conversations [Internet]. 2024 [cited 2025 Feb 22]. Available from: https://research.google/blog/amie-a-research-ai-system-for-diagnostic-medical-reasoning-and-conversations/. [Google Scholar]
41. Lillicrap TP, Santoro A, Marris L, Akerman CJ, Hinton G. Backpropagation and the brain. Nat Rev Neurosci. 2020;21(6):335–46. doi:10.1038/s41583-020-0277-3. [Google Scholar] [CrossRef]
42. Anwar SM, Majid M, Qayyum A, Awais M, Alnowami M, Khan MK. Medical image analysis using convolutional neural networks: a review. J Med Syst. 2018;42(11):226. doi:10.1007/s10916-018-1088-1. [Google Scholar] [PubMed] [CrossRef]
43. Li Z, Liu F, Yang W, Peng S, Zhou J. A survey of convolutional neural networks: analysis, applications, and prospects. IEEE Trans Neural Netw Learn Syst. 2021;33(12):6999–7019. doi:10.1109/TNNLS.2021.3084827. [Google Scholar] [PubMed] [CrossRef]
44. Zhou B, Yang G, Shi Z, Ma S. Natural language processing for smart healthcare. IEEE Rev Biomed Eng. 2024;17(4):4–18. doi:10.1109/RBME.2022.3210270. [Google Scholar] [PubMed] [CrossRef]
45. OpenAI. GPT-4 technical report. arXiv:2303.08774. 2023. [Google Scholar]
46. Gallifant J, Fiske A, Levites Strekalova YA, Osorio-Valencia JS, Parke R, Mwavu R, et al. Peer review of GPT-4 technical report and systems card. PLoS Digit Health. 2024;3(1):e0000417. doi:10.1371/journal.pdig.0000417. [Google Scholar] [PubMed] [CrossRef]
47. OpenAI. OpenAI o1 system card [Internet]. 2024 [cited 2025 Apr 15]. Available from: https://cdn.openai.com/o1-system-card.pdf. [Google Scholar]
48. OpenAI. OpenAI o3-mini system card [Internet]. 2025 [cited 2025 Apr 15]. Available from: https://cdn.openai.com/o3-mini-system-card-feb10.pdf. [Google Scholar]
49. Alowais SA, Alghamdi SS, Alsuhebany N, Alqahtani T, Alshaya AI, Almohareb SN, et al. Revolutionizing healthcare: the role of artificial intelligence in clinical practice. BMC Med Educ. 2023;23(1):689. doi:10.1186/s12909-023-04698-z. [Google Scholar] [PubMed] [CrossRef]
50. Clusmann J, Kolbinger FR, Muti HS, Carrero ZI, Eckardt J-N, Laleh NG, et al. The future landscape of large language models in medicine. Commun Med. 2023;3(1):141. doi:10.1038/s43856-023-00370-1. [Google Scholar] [PubMed] [CrossRef]
51. Quazi S. Artificial intelligence and machine learning in precision and genomic medicine. Med Oncol. 2022;39(8):120. doi:10.1007/s12032-022-01711-1. [Google Scholar] [PubMed] [CrossRef]
52. Khalifa M, Albadawy M. Artificial intelligence for diabetes: enhancing prevention, diagnosis, and effective management. Comput Methods Programs Biomed Update. 2024;5:100141. [Google Scholar]
53. Heintzman ND. A digital ecosystem of diabetes data and technology: services, systems, and tools enabled by wearables, sensors, and apps. J Diabetes Sci Technol. 2015;10(1):35–41. doi:10.1177/1932296815622453. [Google Scholar] [CrossRef]
54. Pegoraro V, Bidoli C, Dal Mas F, Bert F, Cobianchi L, Zantedeschi M, et al. Cardiology in a digital age: opportunities and challenges for e-health: a literature review. J Clin Med. 2023;12(13):4278. [Google Scholar] [PubMed]
55. Watson X, D’Souza J, Cooper D, Markham R. Artificial intelligence in cardiology: fundamentals and applications. Intern Med J. 2022;52(6):912–20. doi:10.1111/imj.15562. [Google Scholar] [PubMed] [CrossRef]
56. Strickland E. IBM Watson, heal thyself: how IBM overpromised and underdelivered on AI health care. IEEE Spectr. 2019;56(4):24–31. doi:10.1109/MSPEC.2019.8678513. [Google Scholar] [CrossRef]
57. Li Z, Wang L, Wu X, Jiang J, Qiang W, Xie H, et al. Artificial intelligence in ophthalmology: the path to the real-world clinic. Cell Rep Med. 2023;4(7):101095. doi:10.1016/j.xcrm.2023.101095. [Google Scholar] [PubMed] [CrossRef]
58. Balas M, Ing EB. Conversational AI Models for ophthalmic diagnosis: comparison of ChatGPT and the isabel pro differential diagnosis generator. JFO Open Ophthalmol. 2023;1(5):100005. doi:10.1016/j.jfop.2023.100005. [Google Scholar] [CrossRef]
59. Shafi S, Parwani AV. Artificial intelligence in diagnostic pathology. Diagn Pathol. 2023;18(1):109. doi:10.1186/s13000-023-01375-z. [Google Scholar] [PubMed] [CrossRef]
60. Waqas A, Bui MM, Glassy EF, El Naqa I, Borkowski P, Borkowski AA, et al. Revolutionizing digital pathology with the power of generative artificial intelligence and foundation models. Lab Invest. 2023;103(11):100255. doi:10.1016/j.labinv.2023.100255. [Google Scholar] [PubMed] [CrossRef]
61. Zhou J, Zeng Z, Li L. A meta-analysis of Watson for Oncology in clinical application. Sci Rep. 2021;11(1):5792. doi:10.1038/s41598-021-84973-5. [Google Scholar] [CrossRef]
62. Tupasela A, Di Nucci E. Concordance as evidence in the Watson for Oncology decision-support system. AI Soc. 2020;35(4):811–8. doi:10.1007/s00146-020-00945-9. [Google Scholar] [CrossRef]
63. Kelly BS, Judge C, Bollard SM, Clifford SM, Healy GM, Aziz A, et al. Radiology artificial intelligence: a systematic review and evaluation of methods (RAISE). Eur Radiol. 2022;32(11):7998–8007. doi:10.1007/s00330-022-08784-6. [Google Scholar] [PubMed] [CrossRef]
64. Jairam MP, Ha R. A review of artificial intelligence in mammography. Clin Imaging. 2022;88(9855):36–44. doi:10.1016/j.clinimag.2022.05.005. [Google Scholar] [PubMed] [CrossRef]
65. Acharya V, Dhiman G, Prakasha K, Bahadur P, Choraria A, M. S, et al. AI-assisted tuberculosis detection and classification from chest X-rays using a deep learning normalization-free network model. Comput Intell Neurosci. 2022;2022(4):2399428. doi:10.1155/2022/2399428. [Google Scholar] [CrossRef]
66. Santosh KC, Allu S, Rajaraman S, Antani S. Advances in deep learning for tuberculosis screening using chest X-rays: the last 5 years review. J Med Syst. 2022;46(11):82. doi:10.1007/s10916-022-01870-8. [Google Scholar] [PubMed] [CrossRef]
67. Bejnordi BE, Veta M, Van Diest PJ, Van Ginneken B, Karssemeijer N, Litjens G, et al. Diagnostic assessment of deep learning algorithms for detection of lymph node metastases in women with breast cancer. JAMA. 2017;318(22):2199–210. doi:10.1001/jama.2017.14585. [Google Scholar] [PubMed] [CrossRef]
68. Gurnani B, Kaur K, Lalgudi VG, Kundu G, Mimouni M, Liu H, et al. Role of artificial intelligence, machine learning and deep learning models in corneal disorders—a narrative review. J Fr Ophtalmol. 2024;47(7):104242. doi:10.1016/j.jfo.2024.104242. [Google Scholar] [PubMed] [CrossRef]
69. Thirunavukarasu AJ, Mahmood S, Malem A, Foster WP, Sanghera R, Hassan R, et al. Large language models approach expert-level clinical knowledge and reasoning in ophthalmology: a head-to-head cross-sectional study. PLoS Digital Health. 2024;3(4):e0000341. doi:10.1371/journal.pdig.0000341. [Google Scholar] [PubMed] [CrossRef]
70. Foltz EA, Witkowski A, Becker AL, Latour E, Lim JY, Hamilton A, et al. Artificial intelligence applied to non-invasive imaging modalities in identification of nonmelanoma skin cancer: a systematic review. Cancers. 2024;16(3):629. doi:10.3390/cancers16030629. [Google Scholar] [PubMed] [CrossRef]
71. Patel RH, Foltz EA, Witkowski A, Ludzik J. Analysis of artificial intelligence-based approaches applied to non-invasive imaging for early detection of melanoma: a systematic review. Cancers. 2023;15(19):4694. doi:10.3390/cancers15194694. [Google Scholar] [PubMed] [CrossRef]
72. Ali H, Muzammil MA, Dahiya DS, Ali F, Yasin S, Hanif W, et al. Artificial intelligence in gastrointestinal endoscopy: a comprehensive review. Ann Gastroenterol. 2024;37(2):133–41. doi:10.20524/aog.2024.0861. [Google Scholar] [PubMed] [CrossRef]
73. Pannala R, Krishnan K, Melson J, Parsi MA, Schulman AR, Sullivan S, et al. Artificial intelligence in gastrointestinal endoscopy. VideoGIE. 2020;5(12):598–613. doi:10.1016/j.vgie.2020.08.013. [Google Scholar] [PubMed] [CrossRef]
74. Hassan C, Spadaccini M, Iannone A, Maselli R, Jovani M, Chandrasekar VT, et al. Performance of artificial intelligence in colonoscopy for adenoma and polyp detection: a systematic review and meta-analysis. Gastrointest Endosc. 2021;93(1):77–85. doi:10.1016/j.gie.2020.06.059. [Google Scholar] [PubMed] [CrossRef]
75. Saeedi A, Saeedi M, Maghsoudi A, Shalbaf A. Major depressive disorder diagnosis based on effective connectivity in EEG signals: a convolutional neural network and long short-term memory approach. Cogn Neurodyn. 2021;15(2):239–52. doi:10.1007/s11571-020-09619-0. [Google Scholar] [PubMed] [CrossRef]
76. Chen ZS, Kulkarni P, Galatzer-Levy IR, Bigio B, Nasca C, Zhang Y. Modern views of machine learning for precision psychiatry. Patterns. 2022;3(11):100602. doi:10.1016/j.patter.2022.100602. [Google Scholar] [PubMed] [CrossRef]
77. Ray A, Bhardwaj A, Malik YK, Singh S, Gupta R. Artificial intelligence and Psychiatry: an overview. Asian J Psychiatr. 2022;70(1):103021. doi:10.1016/j.ajp.2022.103021. [Google Scholar] [PubMed] [CrossRef]
78. Mennella C, Maniscalco U, De Pietro G, Esposito M. Ethical and regulatory challenges of AI technologies in healthcare: a narrative review. Heliyon. 2024;10(4):e26297. doi:10.1016/j.heliyon.2024.e26297. [Google Scholar] [PubMed] [CrossRef]
79. Forcier MB, Gallois H, Mullan S, Joly Y. Integrating artificial intelligence into health care through data access: can the GDPR act as a beacon for policymakers? J Law Biosci. 2019;6(1):317–35. doi:10.1093/jlb/lsz013. [Google Scholar] [PubMed] [CrossRef]
80. Lievevrouw E, Marelli L, Van Hoyweghen I. The FDA’s standard-making process for medical digital health technologies: co-producing technological and organizational innovation. Biosocieties. 2021;17(3):549–76. doi:10.1057/s41292-021-00232-w. [Google Scholar] [PubMed] [CrossRef]
81. Health Ethics & Governance (HEG) WHO. Ethics and governance of artificial intelligence for health: WHO guidance. Geneva, Switzerland: WHO; 2021. [Google Scholar]
82. Amann J, Blasimme A, Vayena E, Frey D, Madai VI. Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC Med Inform Decis Mak. 2020;20(1):310. doi:10.1186/s12911-020-01332-6. [Google Scholar] [PubMed] [CrossRef]
83. Liesenfeld A, Dingemanse M. Rethinking open source generative AI: open washing and the EU AI Act. In: Proceedings of the 2024 ACM Conference on Fairness, Accountability, and Transparency; 2024; Rio de Janeiro, Brazil. p. 1774–87. [Google Scholar]
84. London AJ. Artificial intelligence and black-box medical decisions: accuracy versus explainability. Hastings Cent Rep. 2019;49(1):15–21. doi:10.1002/hast.973. [Google Scholar] [PubMed] [CrossRef]
85. Pruski M. AI-Enhanced healthcare: not a new paradigm for informed consent. J Bioeth Inq. 2024;21(3):475–89. doi:10.1007/s11673-023-10320-0. [Google Scholar] [PubMed] [CrossRef]
86. Huang L, Yu W, Ma W, Zhong W, Feng Z, Wang H, et al. A survey on hallucination in large language models: principles, taxonomy, challenges, and open questions. ACM Trans Inf Syst. 2025;43(2):42–55. doi:10.1145/3703155. [Google Scholar] [CrossRef]
87. Alkaissi H, McFarlane SI. Artificial hallucinations in ChatGPT: implications in scientific writing. Cureus. 2023;15(2):e35179. doi:10.7759/cureus.35179. [Google Scholar] [PubMed] [CrossRef]
88. Esmaeilzadeh P. Challenges and strategies for wide-scale artificial intelligence (AI) deployment in healthcare practices: a perspective for healthcare organizations. Artif Intell Med. 2024;151(10):102861. doi:10.1016/j.artmed.2024.102861. [Google Scholar] [PubMed] [CrossRef]
89. Taeihagh A. Governance of artificial intelligence. Policy Soc. 2021;40(2):137–57. doi:10.1080/14494035.2021.1928377. [Google Scholar] [CrossRef]
90. Passi S, Vorvoreanu M. Overreliance on AI literature review [Internet]. 2022 [cited 2025 Apr 15]. Available from: https://www.microsoft.com/en-us/research/uploads/prod/2022/06/Aether-Overreliance-on-AI-Review-Final-6.21.22.pdf. [Google Scholar]
91. Abràmoff MD, Tarver ME, Loyo-Berrios N, Trujillo S, Char D, Obermeyer Z, et al. Considerations for addressing bias in artificial intelligence for health equity. npj Digit Med. 2023;6(1):170. doi:10.1038/s41746-023-00913-9. [Google Scholar] [PubMed] [CrossRef]
92. Acosta JN, Falcone GJ, Rajpurkar P, Topol EJ. Multimodal biomedical AI. Nature Med. 2022;28(9):1773–84. doi:10.1038/s41591-022-01981-2. [Google Scholar] [PubMed] [CrossRef]
93. Ashok M, Madan R, Joha A, Sivarajah U. Ethical framework for Artificial Intelligence and Digital technologies. Int J Inf Manag. 2022;62(2):102433. doi:10.1016/j.ijinfomgt.2021.102433. [Google Scholar] [CrossRef]
94. Schwalbe N, Wahl B. Artificial intelligence and the future of global health. The Lancet. 2020;395(10236):1579–86. doi:10.1016/S0140-6736(20)30226-9. [Google Scholar] [PubMed] [CrossRef]
95. Afroogh S, Akbari A, Malone E, Kargar M, Alambeigi H. Trust in AI: progress, challenges, and future directions. Humanities Soc Sci Commun. 2024;11(1):1568. doi:10.1057/s41599-024-04044-8. [Google Scholar] [CrossRef]
96. Nazar M, Alam MM, Yafi E, Su’ud MM. A systematic review of human-computer interaction and explainable artificial intelligence in healthcare with artificial intelligence techniques. IEEE Access. 2021;9:153316–48. doi:10.1109/ACCESS.2021.3127881. [Google Scholar] [CrossRef]
97. Southworth J, Migliaccio K, Glover J, Glover JN, Reed D, McCarty C, et al. Developing a model for AI Across the curriculum: transforming the higher education landscape via innovation in AI literacy. Comput Educ: Artif Intell. 2023;4(1):100127. doi:10.1016/j.caeai.2023.100127. [Google Scholar] [CrossRef]
98. Chen L, Chen P, Lin Z. Artificial intelligence in education: a review. IEEE Access. 2020;8:75264–78. doi:10.1109/ACCESS.2020.2988510. [Google Scholar] [CrossRef]
99. Farlow A, Hoffmann A, Tadesse GA, Mzurikwao D, Beyer R, Akogo D, et al. Rethinking global digital health and AI-for-health innovation challenges. PLoS Glob Public Health. 2023;3(4):e0001844. doi:10.1371/journal.pgph.0001844. [Google Scholar] [PubMed] [CrossRef]
100. D’Amario D, Canonico F, Rodolico D, Borovac JA, Vergallo R, Montone RA, et al. Telemedicine, artificial intelligence and humanisation of clinical pathways in heart failure management: back to the future and beyond. Card Fail Rev. 2020;6:e16. doi:10.15420/cfr.2019.17. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF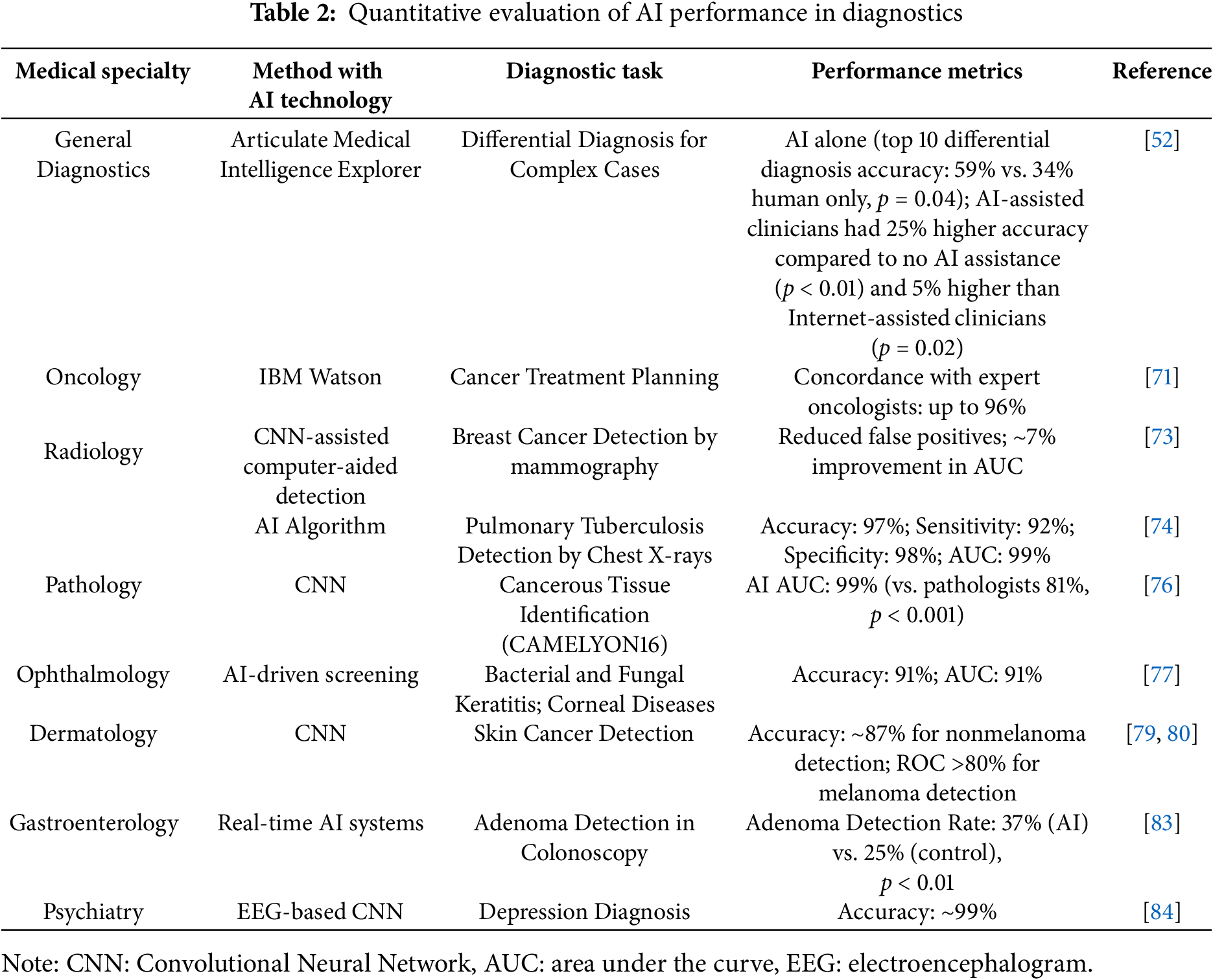
 Downloads
Downloads
 Citation Tools
Citation Tools