 Open Access
Open Access
REVIEW
Effects of Internet-Based Acceptance and Commitment Therapy (IACT) on Adolescents: A Systematic Review and Meta-Analysis
School of Educational Science, Anhui Normal University, Wuhu, 241000, China
* Corresponding Author: Shuanghu Fang. Email:
International Journal of Mental Health Promotion 2023, 25(4), 433-448. https://doi.org/10.32604/ijmhp.2023.025304
Received 04 July 2022; Accepted 24 October 2022; Issue published 01 March 2023
Abstract
Objectives: This study reviewed published randomized controlled trials (RCTs) and evaluated the efficacy of internet-based acceptance and commitment therapy (IACT) on adolescent mental health. Methods: Searches were conducted in PubMed, ProQuest, APA (PsycNET/PsycINFO), and Web of Science from inception to January 2022 to identify RCTs evaluating the effects of IACT on adolescents. The included studies were assessed for quality and risk of bias. This study was performed using the standard mean difference and associated 95% confidence interval of effective measures. Review Manager 5.4 software was adopted to calculate the effect size. Results: Compared to adolescents in control groups, those in the IACT groups showed some improvement in the efficacy of depression symptoms (SMD = −0.24, 95% CI = [−0.44, −0.05], p = 0.01) and had a small but significant effect on reducing experiential avoidance (SMD = −0.24, 95% CI = [−0.46, −0.01], p = 0.04). However, the effect size on anxiety did not reach the threshold (SMD = −0.18, 95% CI = [−0.27, −0.09], p < 0.0001). In addition, there were no significant differences in stress and well-being compared to those of the control group. Compared with universal adolescents, IACT was found to have a more significant therapeutic effect on targeted adolescents. Conclusions: IACT is effective in adolescent mental health interventions, but its clinical reliability and significant efficacy are limited, and more rigorous RCTs are needed in future studies.Keywords
Adolescence is a critical period for emotional and behavioral development, and adolescent mental health has received considerable attention. Many serious mental problems are first identified in childhood or adolescence [1], highlighting the importance of early intervention and adolescent mental health services.
Among behavior therapies, cognitive behavioral therapy can effectively promote mental health [2], and acceptance and commitment therapy (ACT) brings behavior therapy into new territory [3]. As the third wave of behavioral therapy, ACT is a promising approach for transdiagnostic prevention efforts [4]. This therapy has been validated in over 100 randomized controlled trials (RCTs) and is proven to be effective in treating depression, anxiety, substance abuse, eating disorders, stress, smoking, academic concerns, stigma, and self-harm [5]. A recent study indicated that ACT is more effective than treatment as usual (TAU) and untreated groups in improving anxiety, depression, and other mental and behavioral disorders [6].
ACT is based on pragmatism, functional contextualism, and relational frame theory [3]. It can reduce patients’ struggles and frustrating experiences by accepting and noticing their thoughts and behaviors, rather than eliminating negative thoughts and behaviors through thought replacement and cognitive restructuring [7]. Psychological flexibility (PF) is the core of ACT, defined as “fully contacting the present moment as a conscious human being, and based on what the situation affords, changing or persisting in behaviors in the service of chosen values” [8]. It is a protective factor for various psychological problems [9].
Traditional mental health services are usually provided by face-to-face or group counseling, with relatively fixed time, no privacy guarantee, few audience, and low efficiency. Less help-seeking behavior among adolescents may be due to the shame associated with “seeing a therapist” [10]. With the development of the internet, this problem can be addressed by internet-based psychological intervention and prevention programs [11]. A review showed that users generally had a positive attitude toward mental health apps [12]. For young people spending more time online, technology and mobile devices offer a flexible tool and new opportunities to provide mental health services [13]. The COVID-19 pandemic has led to an increase in mantel health problems among adolescents, and the increased levels of stress, depressive thoughts, and anxiety have aroused their interest in online psychotherapy [14,15]. A recent meta-analysis showed that online mental health interventions were effective across different mental health conditions in adolescents [16].
Internet-based acceptance and commitment therapy (IACT) is a novel treatment protocol based on the Internet and ACT. It combines a face-to-face conversation with a mobile application (“app”) between sessions to facilitate ACT and self-acceptance practice, and behavior change [17]. This therapy is delivered primarily through video watching, audio listening, animated presentations, written exercises, and telephone consultation based on ACT. Compared to traditional methods, it has many advantages. For example, its flexibility allows clients to access therapeutic content at any time [18]. In addition, the comparison between face-to-face and web-based interventions shows no differences in effectiveness [19]. A transdiagnostic meta-analysis was conducted to examine the efficacy of IACT in relieving anxiety and depression and improving the life quality and PF of adults [20]. Although there are few meta-analyses on the effectiveness of IACT for adolescents, preliminary results indicated that IACT could increase PF. In recent years, many clinical trials on the effectiveness of IACT in adolescent mental health interventions have been conducted, but related meta-analyses were not performed.
This meta-analysis reviewed published RCTs and evaluated the efficacy of IACT on adolescent mental health. The results can provide clinicians and practitioners with evidence-based research to reduce bias in treatment decisions and guide future research. The current review and meta-analysis aim to address the following questions:
1. What is the efficacy of IACT interventions (compared to control groups) in improving adolescent mental health?
2. What are the risks of bias inherent in the relevant studies?
The systematic review and meta-analysis were performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [21] and Cochrane Handbook for Systematic Reviews of Interventions Version 5.4 [22]. The protocol was registered with the PROSPERO number CRD42022323974.
After the initial scoping searches, relevant studies were searched by key terms in PubMed, ProQuest, APA (PsycNET/PsycINFO), and Web of Science from inception to January 2022. These terms included: (Internet Based Intervention, Internet-Based Interventions, Web-Based Intervention, Web-Based Intervention, Online Intervention, Internet Intervention, Internet-Delivered, Web-Delivered, Mobile Applications, Mobile App, Mobile Apps, App) and (Acceptance and Commitment Therapy, IACT, ACT) and (Adolescents, Adolescence, Teens, Teen, Teenagers, Teenager, Youth, Youths, Adolescents, Female Adolescent, Male Adolescent). Search terms were adjusted for each database, including the use of MeSH terms and Cochrane filters as required. Furthermore, the website of the Association of Contextual Behavioral Science (http://contextualscience.org) was also retrieved. To minimize potential publication bias, unpublished dissertations were searched, and relevant documents were added according to their reference list. Studies were also manually searched based on their reference lists, systematic reviews, and related article features in databases.
2.2.1 Studies were Included Based on the Following Criteria
(a) The study must be an RCT testing the effects of ACT as an intervention before and after the intervention implementation at the group level;
(b) Study participants must be adolescents (including junior high, high school, and college students);
(c) The intervention must be performed using IACT;
(d) The study must have reported pre-test and post-test results of the IACT measurements;
(e) The study must be peer-reviewed.
2.2.2 Studies with Any of the Following Features Were Excluded
(a) Reanalysis of data from previously published studies (including reviews and meta-analyses);
(b) Face-to-face ACT intervention;
(c) Not published in English;
(d) Insufficient data were used to calculate the effect size.
Two researchers with database searching skills and ACT expertise independently screened and cross-checked the literature according to the above criteria. A third reviewer was responsible for resolving any discrepancies.
2.3 Data Extraction and Quality Assessment
After reviewing the full text, the following data were extracted: (a) Participants: country, sample size, age, condition, retention rate; (b) Studies: study design, results, online intervention modalities and duration, intervention content, outcome measurement tools, mean and standard deviation after the experiment (statistical significance is represented by p values, and clinical significance is denoted by effect sizes).
All literature quality was evaluated using the Cochrane Risk of Bias Tool endorsed by the PRISMA guidelines [22]. The tool includes seven parts: (a) “random sequence generation”; (b) “allocation concealment”; (c) “blinding of participants and personnel”; (d) “blinding of outcome assessment”; (e) “incomplete outcome data”; (f) “selective outcome reporting”; (g) “other bias”. The risk of bias in each study was classified as low, high, or unclear based on uniform judgment.
The current meta-analysis was performed using the standard mean difference (SMD) and associated 95% confidence interval (CI) of effective measures and presented in a single forest plot. The effect size of each study was calculated using Hedges’ G [23]. According to Cohen’s theory, 0.2 ⩽ SMD < 0.5 is a small effect, 0.5 ⩽ SMD < 0.8 is a medium effect, and SMD ⩾ 0.8 is a large effect [24]. Heterogeneity between results was examined by the I2 test, and the standard for I2 reflects the proportion of heterogeneity in the total effect size variation. If 0 < I2 < 40, there is low heterogeneity; if 40 < I2 < 60, there is moderate heterogeneity; if 60 < I2 < 75, there is substantial heterogeneity; if 75 < I2 < 100, there is considerable heterogeneity. If heterogeneity existed between study samples, a random effect model was used to evaluate the effect of IACT. Review Manager 5.4 software was adopted to calculate the effect size.
Fig. 1 illustrates the flow diagram from searching to article inclusion based on PRISMA guidelines. A total of 3064 articles were identified through database searching, and 3 articles were found by searching reference lists. After removing duplicates, 489 articles were screened based on title and abstract, of which 440 were excluded for various reasons (e.g., review articles or qualitative research). The eligibility of 49 articles was assessed by reading the full text, and 37 studies were excluded for the reasons listed in Fig. 1. Finally, 12 studies were included that met all criteria.
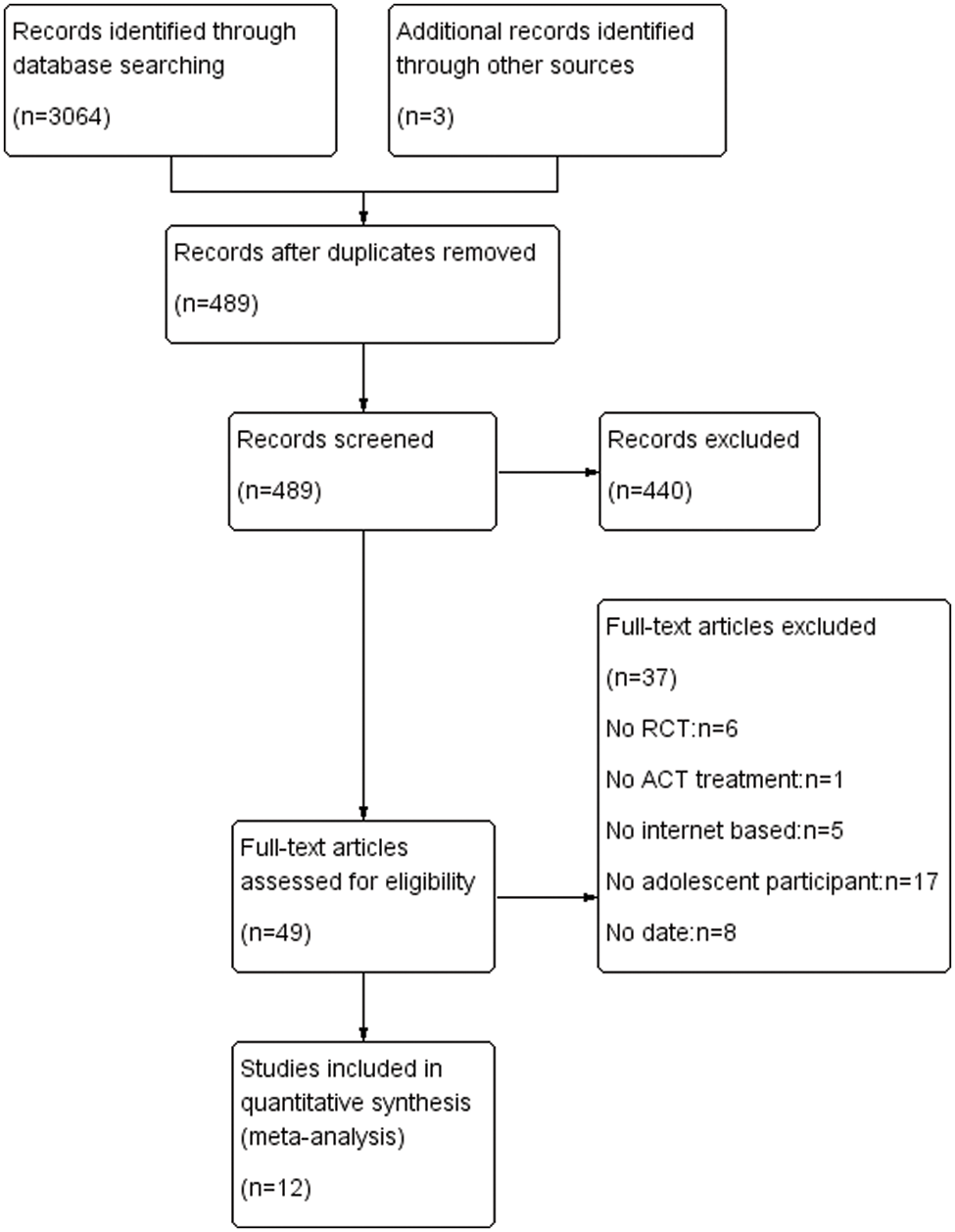
Figure 1: PRISMA flow diagram
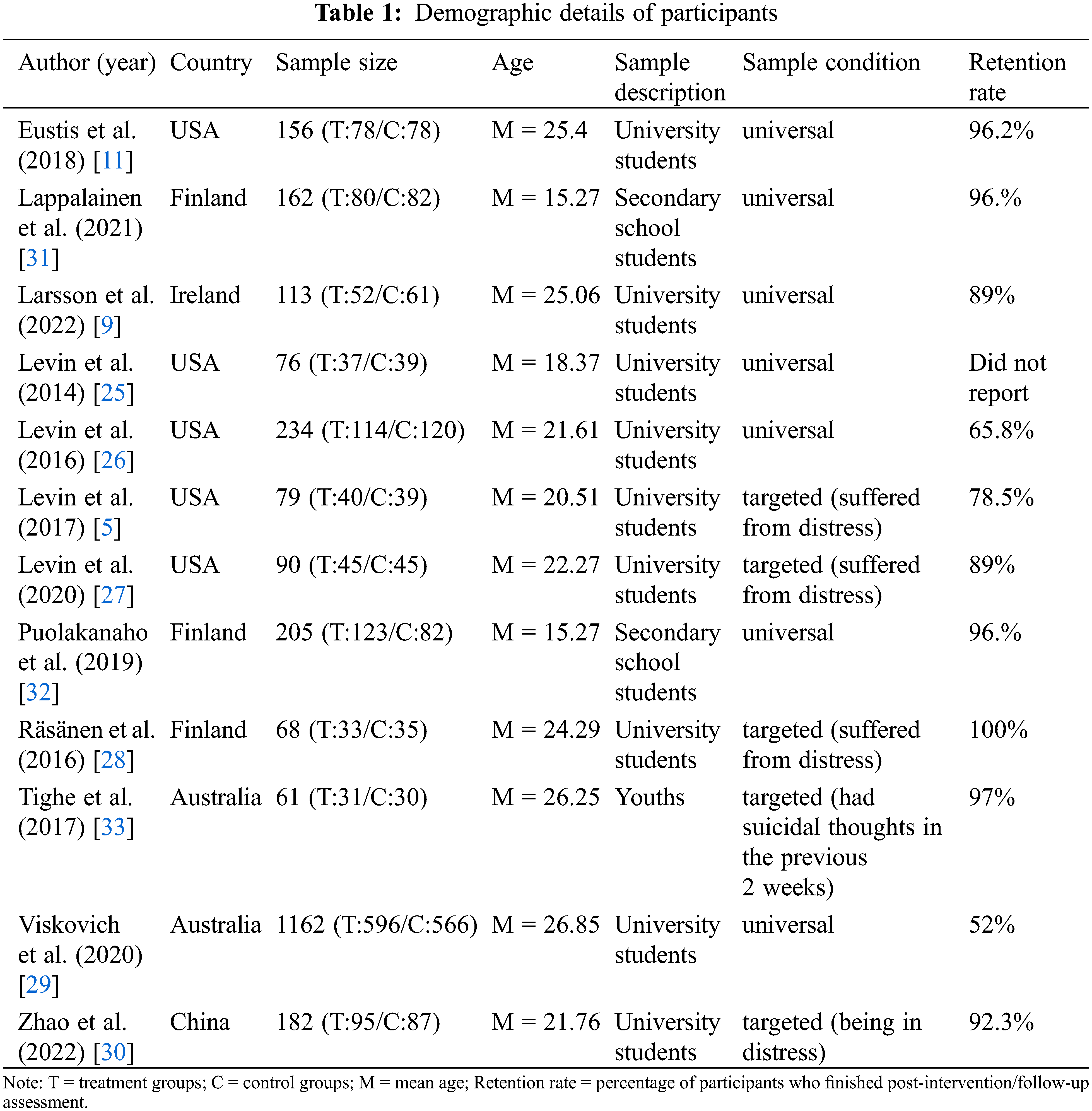
3.2 Sample Characteristics and Demographics
Among the included studies, 2588 adolescents were included, of which 2160 were university students [5,9,11,25–30], 367 were secondary school students [31,32], and 61 were indigenous youths [33]. The mean age ranges from 15.27 to 26.85. A total of 5 included studies were in the targeted screening group (suffered from distress or having suicidal thoughts in the past 2 weeks), and 5 were in the universal screening group. In terms of country, 5 of the included studies were from the United States [5,11,25–27], 2 from Australia [29,33], 3 from Finland [28,31,32], 1 from China [30], and 1 from Ireland [9]. Table 1 illustrates the characteristics of the participants.
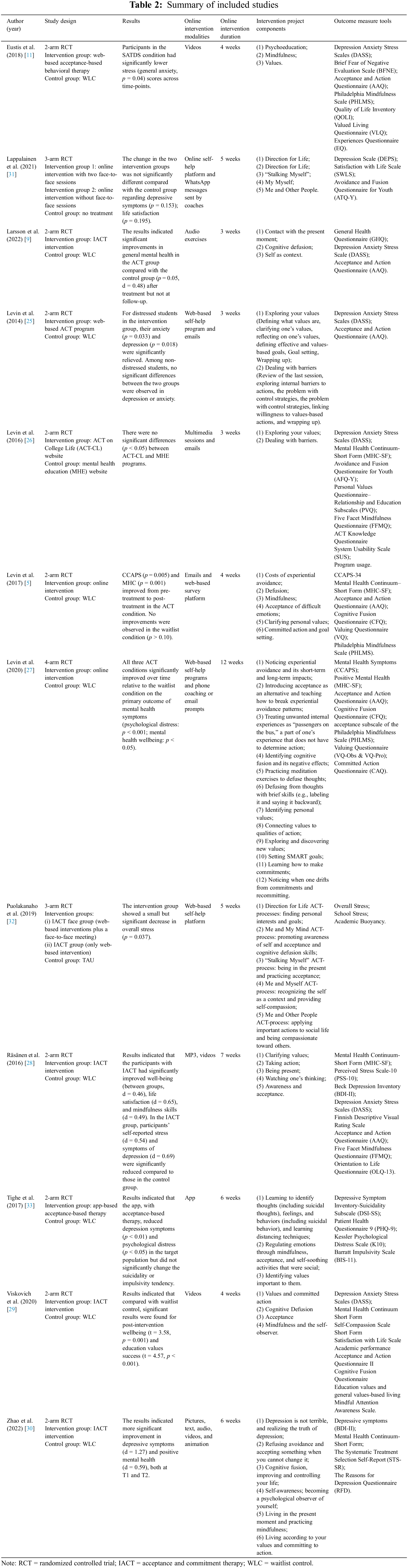
According to the inclusion criteria, all included studies were RCTs, which were divided into 2-arm RCT, 3-arm RCT, and 4-arm RCT based on different research purposes. The experimental group was treated with IACT, while the control group was subject to WLC (waiting list control) or traditional therapy (mental health education).
Online intervention modalities include videos, online self-help platforms and WhatsApp messages from coaches; audio exercises; web-based self-help programs; multimedia sessions; apps; pictures; text; animation; MP3; and Emails. The duration of online intervention was 3 to 12 weeks.
Intervention projects were selected based on the six therapeutic processes of ACT, which include acceptance (embracing internal experiences without altering their form or frequency); cognitive defusion (achieving psychological distance from internal experiences); presence (ongoing, non-judgmental contact with psychological and environmental events as they occur); self-as-context (observing or noticing one’s inner/outer world and taking a flexible perspective); values (choosing valued life directions); and committed action (acting in service of one’s chosen values) [34].
The primary outcome measures were depression (9 studies; n = 2111), anxiety (7 studies; n = 1888), and stress (7 studies; n = 2014); the secondary were well-being (10 studies; n = 2307) and experiential avoidance (6 studies; n = 1654). Table 2 summarizes study characteristics and findings for all included studies.
Five studies were at low risk of selection bias (“allocation concealment”) because the random numbers generated by computers were used [5,26,27,30,33,34]. Three studies also had low risk because the assignment of these RCTs was performed by an independent researcher [28,31] or by the lead investigator using a random number table the conditional assignment of participants [9]. Four studies were considered to have unclear risks due to insufficient information [11,25,29,32]. Details of the literature evaluation are shown in Fig. 2.
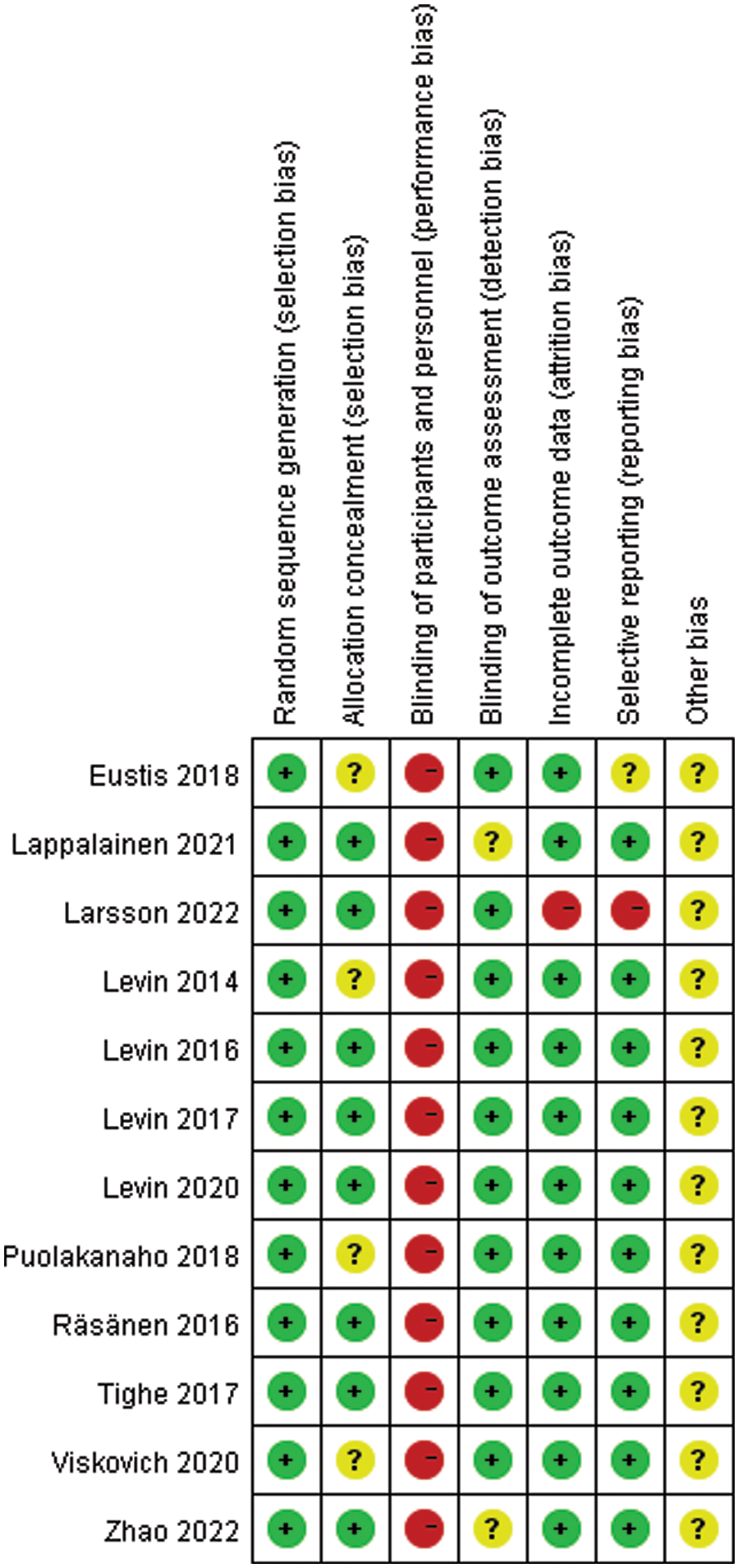
Figure 2: Risk of bias graph
3.5 Effects of IACT on Depression, Anxiety, and Stress
The primary outcome measures were depression, anxiety, and stress. The effects of IACT on depression were investigated in 9 RCTs (N = 2111 participants). According to the evaluation criteria, 9 RCTs revealed that IACT had significant efficacy on depression compared to control groups (SMD = −0.24, 95% CI = [−0.44, −0.05], p = 0.01; Fig. 3). Notably, there was a great heterogeneity (I2 = 71%) among these studies. Based on 7 RCTs (N = 1880 participants), there was no significant improvement in anxiety in IACT group compared to the control groups (SMD = −0.18, 95% CI = [−0.27, −0.09], p < 0.0001; Fig. 3). There was a low heterogeneity among the studies (I2 = 0%). In 7 RCTs (N = 2014 participants), the group with IACT interventions showed a smaller and non-significant effect on stress compared to control groups (SMD = −0.16, 95% CI = [−0.35, 0.03], p = 0.10; Fig. 3). There is great heterogeneity among these studies (I2 = 68%).
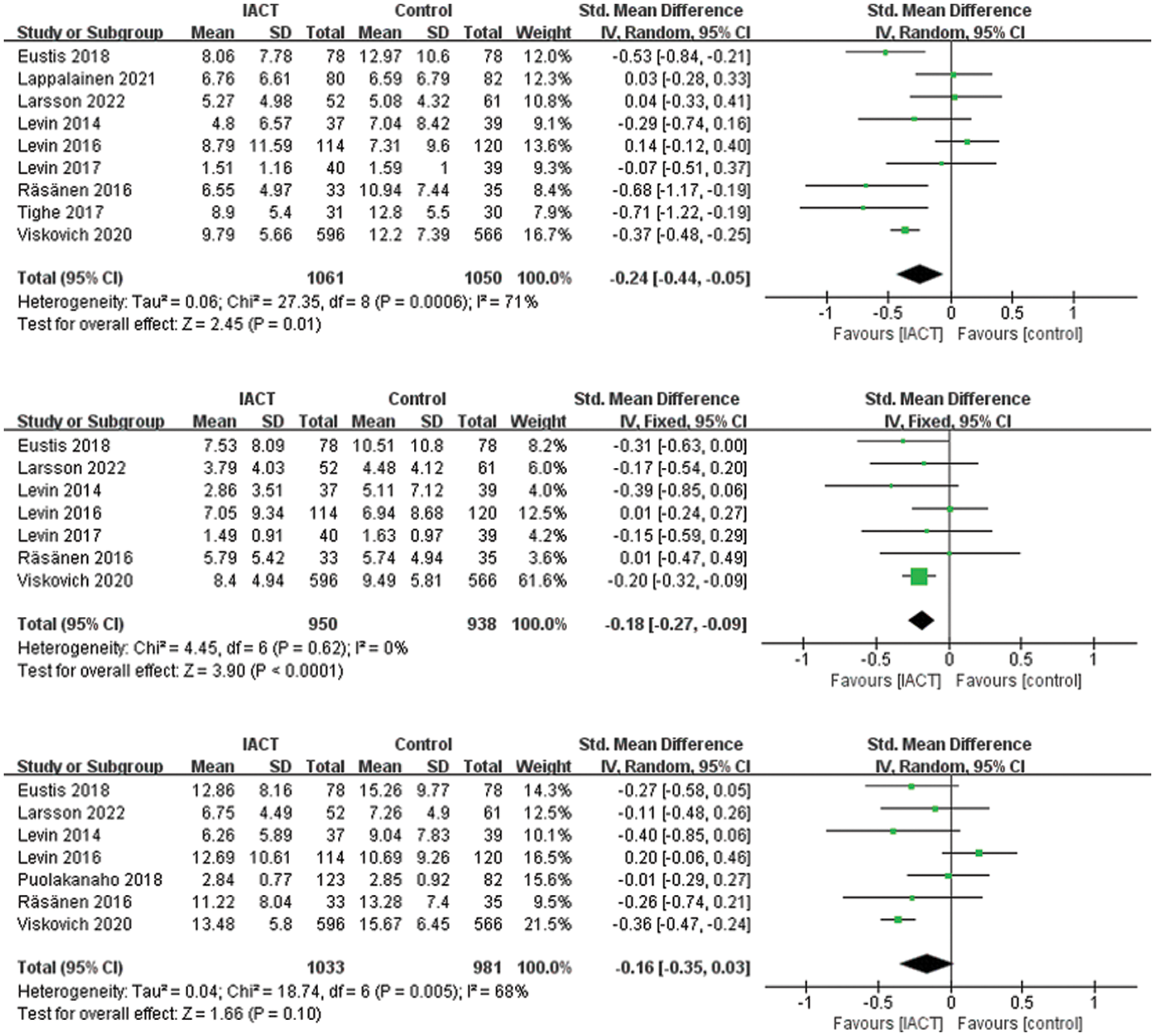
Figure 3: Effects of IACT on depression, anxiety, and stress
Despite insufficient studies on other outcome measures for subgroup analysis, we performed a subgroup analysis of depression outcome measures to assess whether groups with different conditions (universal/targeted) produced different treatment effects. A total of 9 RCTs reported sample conditions of depression outcome measures, including 1903 universal adolescents and 208 targeted adolescents (suffered from distress or having suicidal thoughts in the past 2 weeks). Meta-analysis of the random-effects model showed no significant difference between the universal and targeted groups in improving the efficacy of IACT. However, the therapeutic effect on depression was mainly shown in the targeted group (SMD = −0.47, 95% CI = [−0.89, −0.05], p = 0.03; Fig. 4).
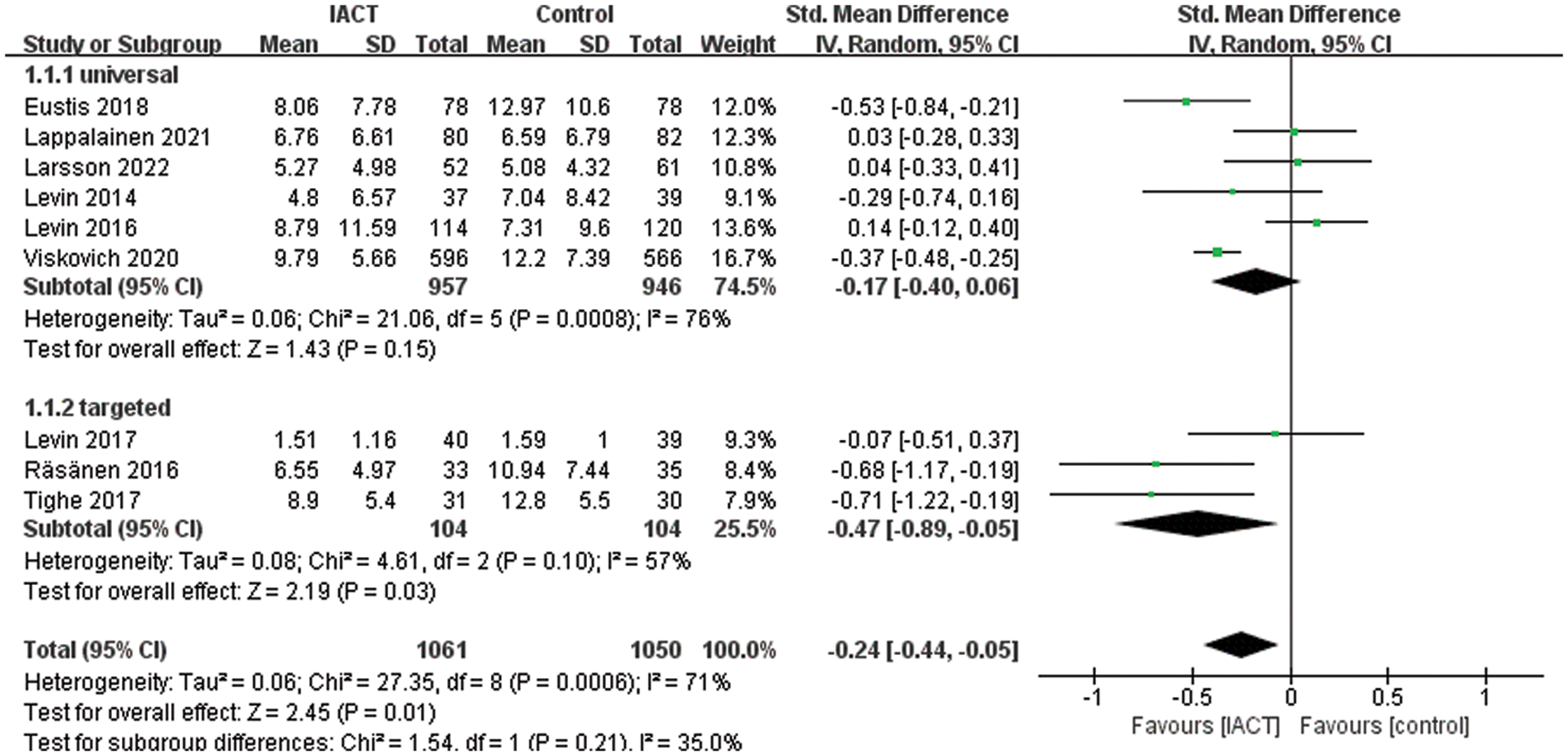
Figure 4: Effects of IACT on depression in different groups
3.6 Effects of IACT on Well-Being
The secondary outcome measure was well-being. A meta-analysis of 10 RCTs (N = 2307 participants) showed that the overall effect of IACT interventions on well-being was not statistically significant (SMD = 0.09, 95% CI = [−0.16, 0.33], p = 0.49; Fig. 5). In addition, this analysis showed the highest degree of heterogeneity among studies (I2 = 84%).
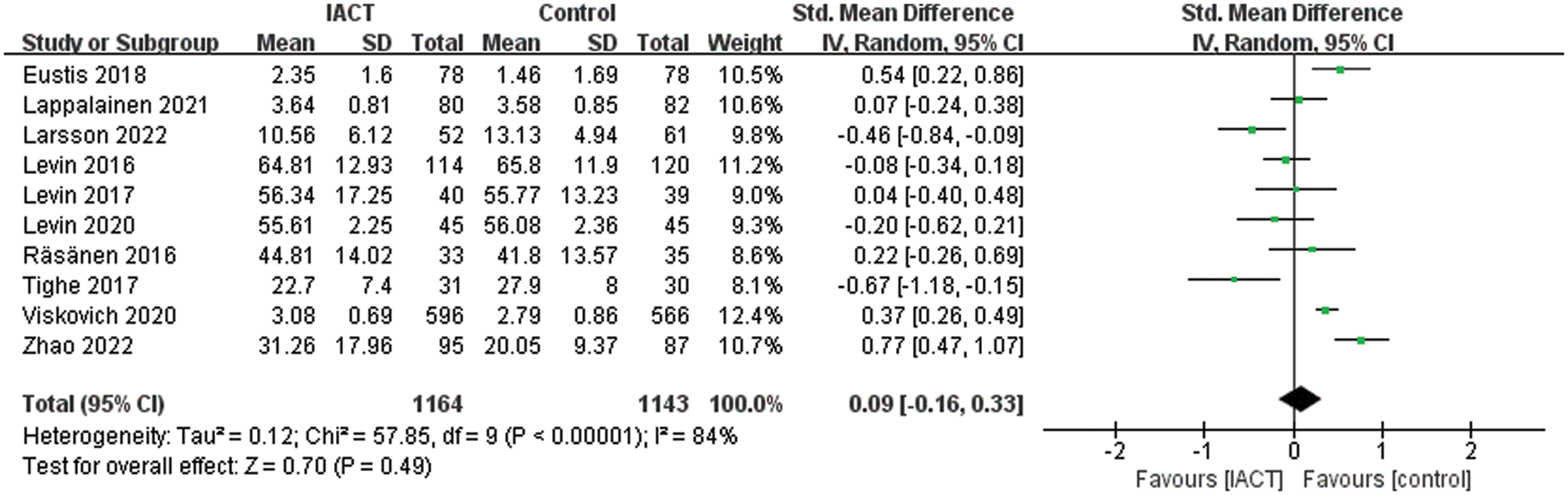
Figure 5: Effects of IACT on well-being
3.7 Effects of IACT on Experiential Avoidance
As mentioned above, a meta-analysis was conducted on the effect of IACT on experiential avoidance. In 6 RCTs (N = 1654 participants), the groups with IACT interventions showed less effect on experiential avoidance than the control groups (SMD = −0.24, 95% CI = [−0.46, −0.01], p = 0.04; Fig. 6). There is a great heterogeneity (I2 = 65%) among studies.
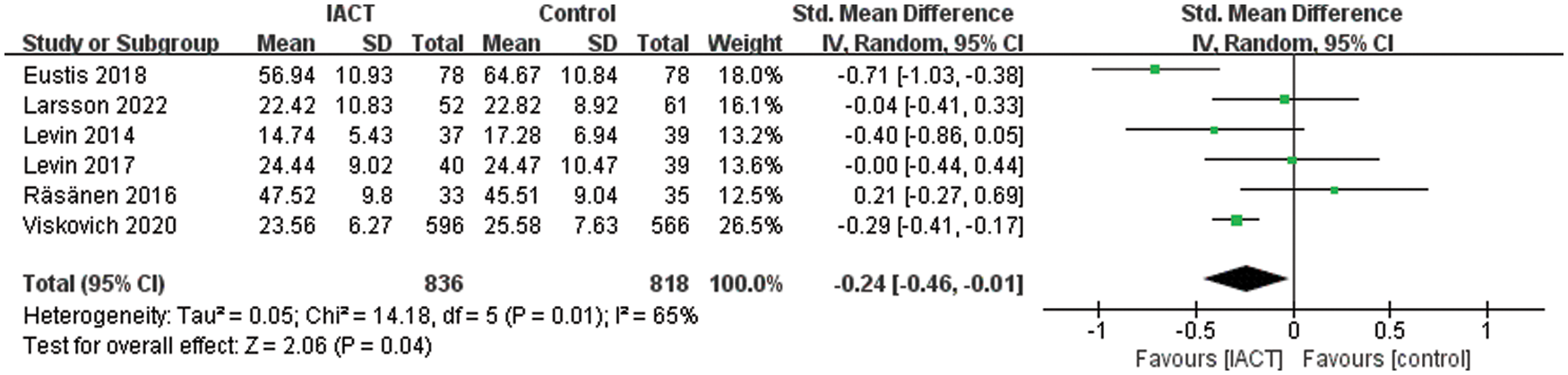
Figure 6: Effects of IACT on experiential avoidance
As far as we know, this is the first meta-analysis regarding the efficacy of IACT in adolescents. IACT is likely to be an effective and popular method for promoting the well-being of adolescents [31]. Although existing RCTs demonstrate the efficacy of IACT, there is no meta-analysis on the application of IACT in adolescents and its development. A transdiagnostic meta-analysis confirmed the effectiveness of IACT in relieving anxiety and depression and improving life quality and PF in adults [20]. However, there was no particular discussion of the adolescent population. In the current study, some of these studies and the latest RCTs were selected. Adolescents were considered as the research objects because they are proficient in internet operation and willing to accept online psychological intervention. The results verified our hypothesis, with a high retention rate for most studies.
The systematic review included 12 studies examined the effects of IACT interventions on the mental health of adolescents. Afterward, meta-analyses were separately conducted for primary and secondary outcome measures using standardized mean deviations. Although there were few studies on the effect of IACT on adolescents, preliminary results suggested that IACT had some efficacy for depression (SMD = −0.24) and a small effect on anxiety (SMD = −0.18), while there were no statistically significant differences in its impact on stress and well-being. These results can be compared with another meta-analysis that examined the role of ACT in improving the well-being of college students [35]. It revealed a significant, small pooled effect size (d = 0.29) of ACT on university students’ well-being. Differences between face-to-face and online interventions may explain this slight difference. Regarding PF, IACT had a small but significant effect on experiential avoidance (SMD = −0.24). Subgroup analysis showed that IACT was more effective in treating targeted adolescents than universal adolescents because of the higher baseline levels of mental health and poorer improvement from psychological interventions. The findings of the present study partially support previous meta-analyses of other populations [20,36–39].
The high heterogeneity in this study may be caused by the differences in the included studies, with the main differences possibly arising from the different measurement instruments. As for the primary outcome indicators, most studies used the DASS to measure depression, anxiety, and stress, and some adopted the DEPS scale, CCAPS scale, HBSC scale, PHQ scale, and BDI scale. Among 12 studies, 5 different indicators were applied to measure well-being. Most studies used the MHC-SF [40], followed by the QOLI scale, SWLS scale, GHQ scale, and K10 scale, reflecting the difference between psychological studies.
The high risk of performance bias for “blinding of participants and personnel” across all studies reflected the universality of psychotherapy research. Blinding of participants and therapists was not feasible in intervention trials of this nature [41]. It is difficult to blind subjects and outcome evaluators based on the nature of online psychological research. In each study, participants were randomly assigned to different conditions, and the “random sequence generation” was assessed as ‘low risk’ in all included studies. Most articles reported all pre-specified outcomes, such as M and SD, which had good psychometric properties and were considered low risk. Only one study was assessed as high risk [9]. Because of the insufficient data, we contacted the authors and obtained the data. In addition, the risk of other biases was assessed as unclear in all studies.
The results of this review suggest that IACT can improve depression, anxiety, and experiential avoidance in adolescents. In addition, subgroup analyses show that IACT is more effective for adolescents with psychological problems. Since the number and quality of included research are limited, the results as mentioned earlier must be supported by more high-quality studies. However, the practical significance of IACT needs to attract more attention because it breaks through the limitations of traditional face-to-face ACT. It can be carried out at any time and space and is worthy of promotion on campus. In future studies, more high-quality RCTs are needed to verify the intervention effect of IACT.
There are still some limitations in this study. First, the number of RCTs included in this study is limited because only adolescents are involved. In addition, the quality of the included studies is low. Because subjects and bureau assessors in all RCTs are not blinded, the risk of implementation and measurement bias is high, partially affecting the credibility of the study results. Finally, the measurement tools in these studies are different, resulting in a high degree of heterogeneity in research findings.
Funding Statement: This study was funded by the Humanities and Social Sciences Key Research Base Project of Anhui Province (SK2017A0278).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Kessler, R. C., Amminger, G. P., Aguilar-Gaxiola, S., Alonso, J., Lee, S. et al. (2007). Age of onset of mental disorders: A review of recent literature. Current Opinion in Psychiatry, 20(4), 359–364. DOI 10.1097/YCO.0b013e32816ebc8c. [Google Scholar] [CrossRef]
2. Smith, J., Newby, J. M., Burston, N., Murphy, M. J., Michael, S. et al. (2017). Help from home for depression: A randomised controlled trial comparing internet-delivered cognitive behaviour therapy with bibliotherapy for depression. Internet Interventions, 9(11), 25–37. DOI 10.1016/j.invent.2017.05.001. [Google Scholar] [CrossRef]
3. Hayes, S. C. (2016). Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies–republished article. Behavior Therapy, 47(6), 869–885. DOI 10.1016/j.beth.2016.11.006. [Google Scholar] [CrossRef]
4. Hart, A. K., Breen, L. J., Beilby, J. M. (2021). Evaluation of an integrated fluency and Acceptance and commitment therapy intervention for adolescents and adults who stutter: Participant perspectives. Journal of Fluency Disorders, 69(5), 105852. DOI 10.1016/j.jfludis.2021.105852. [Google Scholar] [CrossRef]
5. Levin, M. E., Haeger, J. A., Pierce, B. G., Twohig, M. P. (2017). Web-based acceptance and commitment therapy for mental health problems in college students: A randomized controlled trial. Behavior Modification, 41(1), 141–162. DOI 10.1177/0145445516659645. [Google Scholar] [CrossRef]
6. Fang, S., Ding, D. (2020). A meta-analysis of the efficacy of acceptance and commitment therapy for children. Journal of Contextual Behavioral Science, 15(1), 225–234. DOI 10.1016/j.jcbs.2020.01.007. [Google Scholar] [CrossRef]
7. Beilby, J. M., Byrnes, M. L., Yaruss, J. S. (2012). Acceptance and commitment therapy for adults who stutter: Psychosocial adjustment and speech fluency. Journal of Fluency Disorders, 37(4), 289–299. DOI 10.1016/j.jfludis.2012.05.003. [Google Scholar] [CrossRef]
8. Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. DOI 10.1016/j.brat.2005.06.006. [Google Scholar] [CrossRef]
9. Larsson, A., Hartley, S., McHugh, L. (2022). A randomised controlled trial of brief web-based acceptance and commitment therapy on the general mental health, depression, anxiety and stress of college students. Journal of Contextual Behavioral Science, 24(3), 10–17. DOI 10.1016/j.jcbs.2022.02.005. [Google Scholar] [CrossRef]
10. Eisenberg, D., Downs, M. F., Golberstein, E., Zivin, K. (2009). Stigma and help seeking for mental health among college students. Medical Care Research and Review, 66(5), 522–541. DOI 10.1177/1077558709335173. [Google Scholar] [CrossRef]
11. Eustis, E. H., Hayes-Skelton, S. A., Orsillo, S. M., Roemer, L. (2018). Surviving and thriving during stress: A randomized clinical trial comparing a brief web-based therapist-assisted acceptance-based behavioral intervention versus waitlist control for college students. Behavior Therapy, 49(6), 889–903. DOI 10.1016/j.beth.2018.05.009. [Google Scholar] [CrossRef]
12. Chan, A. H. Y., Honey, M. L. L. (2021). User perceptions of mobile digital apps for mental health: Acceptability and usability–An integrative review. Journal of Psychiatric and Mental Health Nursing, 29(1), 147–168. DOI 10.1111/jpm.12744. [Google Scholar] [CrossRef]
13. Edwards-Hart, T., Chester, A. (2010). Online mental health resources for adolescents: Overview of research and theory. Australian Psychologist, 45(3), 223–230. DOI 10.1080/00050060903584954. [Google Scholar] [CrossRef]
14. Eysenbach, G., Fagherazzi, G., Torous, J. (2020). Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. Journal of Medical Internet Research, 22(9), e21279. DOI 10.2196/21279. [Google Scholar] [CrossRef]
15. Babb, S. J., Rufino, K. A., Johnson, R. M. (2021). Assessing the effects of the COVID-19 pandemic on nontraditional students’ mental health and well-being. Adult Education Quarterly, 72(2), 140–157. DOI 10.1177/07417136211027508. [Google Scholar] [CrossRef]
16. Zhou, X., Edirippulige, S., Bai, X., Bambling, M. (2021). Are online mental health interventions for youth effective? A systematic review. Journal of Telemedicine and Telecare, 27(10), 638–666. DOI 10.1177/1357633X211047285. [Google Scholar] [CrossRef]
17. Merwin, R. M., Moskovich, A. A., Babyak, M., Feinglos, M., Honeycutt, L. K. et al. (2021). An open trial of app-assisted acceptance and commitment therapy (iACT) for eating disorders in type 1 diabetes. Journal of Eating Disorders, 9(1), 6. DOI 10.1186/s40337-020-00357-6. [Google Scholar] [CrossRef]
18. Proudfoot, J., Klein, B., Barak, A., Carlbring, P., Cuijpers, P. et al. (2011). Establishing guidelines for executing and reporting internet intervention research. Cognitive Behaviour Therapy, 40(2), 82–97. DOI 10.1080/16506073.2011.573807. [Google Scholar] [CrossRef]
19. Barak, A., Hen, L., Boniel-Nissim, M., Shapira, N. A. (2008). A comprehensive review and a meta-analysis of the effectiveness of internet-based psychotherapeutic interventions. Journal of Technology in Human Services, 26(2–4), 109–160. DOI 10.1080/15228830802094429. [Google Scholar] [CrossRef]
20. Thompson, E. M., Destree, L., Albertella, L., Fontenelle, L. F. (2021). Internet-based acceptance and commitment therapy: A transdiagnostic systematic review and meta-analysis for mental health outcomes. Behavior Therapy, 52(2), 492–507. DOI 10.1016/j.beth.2020.07.002. [Google Scholar] [CrossRef]
21. Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., Altman, D. et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLos Medicine, 6(7), e1000097. DOI 10.1371/journal.pmed.1000097. [Google Scholar] [CrossRef]
22. Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T. et al. (2019). Cochrane handbook for systematic reviews of interventions. 2nd edition. New Jersey: Wiley-Blackwell. [Google Scholar]
23. Hedges, L. V. (1981). Distribution theory for glass’s estimator of effect size and related estimators. Journal of Educational and Behavioral Statistics, 6(2), 107–128. DOI 10.3102/10769986006002107. [Google Scholar] [CrossRef]
24. Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. DOI 10.1037/0033-2909.112.1.155. [Google Scholar] [CrossRef]
25. Levin, M. E., Pistorello, J., Seeley, J. R., Hayes, S. C. (2014). Feasibility of a prototype web-based acceptance and commitment therapy prevention program for college students. Journal of American College Health, 62(1), 20–30. DOI 10.1080/07448481.2013.843533. [Google Scholar] [CrossRef]
26. Levin, M. E., Hayes, S. C., Pistorello, J., Seeley, J. R. (2016). Web-based self-help for preventing mental health problems in universities: Comparing acceptance and commitment training to mental health education. Journal of Clinical Psychology, 72(3), 207–225. DOI 10.1002/jclp.22254. [Google Scholar] [CrossRef]
27. Levin, M. E., Krafft, J., Hicks, E. T., Pierce, B., Twohig, M. P. (2020). A randomized dismantling trial of the open and engaged components of acceptance and commitment therapy in an online intervention for distressed college students. Behaviour Research and Therapy, 126(8), 103557. DOI 10.1016/j.brat.2020.103557. [Google Scholar] [CrossRef]
28. Räsänen, P., Lappalainen, P., Muotka, J., Tolvanen, A., Lappalainen, R. (2016). An online guided ACT intervention for enhancing the psychological wellbeing of university students: A randomized controlled clinical trial. Behaviour Research and Therapy, 78(4), 30–42. DOI 10.1016/j.brat.2016.01.001. [Google Scholar] [CrossRef]
29. Viskovich, S., Pakenham, K. I. (2020). Randomized controlled trial of a web-based acceptance and commitment therapy (ACT) program to promote mental health in university students. Journal of Clinical Psychology, 76(6), 929–951. DOI 10.1002/jclp.22848. [Google Scholar] [CrossRef]
30. Zhao, C., Wampold, B. E., Ren, Z., Zhang, L., Jiang, G. (2022). The efficacy and optimal matching of an Internet-based acceptance and commitment therapy intervention for depressive symptoms among university students: A randomized controlled trial in China. Journal of Clinical Psychology, 78(7), 1354–1375. DOI 10.1002/jclp.23329. [Google Scholar] [CrossRef]
31. Lappalainen, R., Lappalainen, P., Puolakanaho, A., Hirvonen, R., Eklund, K. et al. (2021). The youth compass-the effectiveness of an online acceptance and commitment therapy program to promote adolescent mental health: A randomized controlled trial. Journal of Contextual Behavioral Science, 20(5), 1–12. DOI 10.1016/j.jcbs.2021.01.007. [Google Scholar] [CrossRef]
32. Puolakanaho, A., Lappalainen, R., Lappalainen, P., Muotka, J. S., Hirvonen, R. et al. (2019). Reducing stress and enhancing academic buoyancy among adolescents using a brief web-based program based on acceptance and commitment therapy: A randomized controlled trial. Journal of Youth and Adolescence, 48(2), 287–305. DOI 10.1007/s10964-018-0973-8. [Google Scholar] [CrossRef]
33. Tighe, J., Shand, F., Ridani, R., Mackinnon, A., De La Mata, N. et al. (2017). Ibobbly mobile health intervention for suicide prevention in Australian Indigenous youth: A pilot randomised controlled trial. BMJ Open, 7(1), e013518. DOI 10.1136/bmjopen-2016-013518. [Google Scholar] [CrossRef]
34. Stenhoff, A., Steadman, L., Nevitt, S., Benson, L., White, R. G. (2020). Acceptance and commitment therapy and subjective wellbeing: A systematic review and meta-analyses of randomised controlled trials in adults. Journal of Contextual Behavioral Science, 18(1), 256–272. DOI 10.1016/j.jcbs.2020.08.008. [Google Scholar] [CrossRef]
35. Howell, A. J., Passmore, H. A. (2019). Acceptance and commitment training (ACT) as a positive psychological intervention: A systematic review and initial meta-analysis regarding ACT’s role in well-being promotion among university students. Journal of Happiness Studies, 20(6), 1995–2010. DOI 10.1007/s10902-018-0027-7. [Google Scholar] [CrossRef]
36. Brown, M., Glendenning, A. C., Hoon, A. E., John, A. (2016). Effectiveness of web-delivered acceptance and commitment therapy in relation to mental health and well-being: A systematic review and meta-analysis. Journal of Medical Internet Research, 18(8), e6200. DOI 10.2196/jmir.6200. [Google Scholar] [CrossRef]
37. Hacker, T., Stone, P., MacBeth, A. (2016). Acceptance and commitment therapy-do we know enough? Cumulative and sequential meta-analyses of randomized controlled trials. Journal of Affective Disorders, 190(12), 551–565. DOI 10.1016/j.jad.2015.10.053. [Google Scholar] [CrossRef]
38. Wei, S., Ni, S. F., Xiao, M. Z., Gao, Y. Z., Luo, Q. H. (2018). Effectiveness of internet-delivered acceptance and commitment therapy for improving mental health: A meta-analysis. Journal of Army Medical University, 40(14), 1332–1342. DOI 10.16016/j.1000-5404.201802150. [Google Scholar] [CrossRef]
39. Kelson, J., Rollin, A., Ridout, B., Campbell, A. (2019). Internet-delivered acceptance and commitment therapy for anxiety treatment: Systematic review. Journal of Medical Internet Research, 21(1), e12530. DOI 10.2196/12530. [Google Scholar] [CrossRef]
40. Keyes, C. L. (2002). The mental health continuum: From languishing to flourishing in life. Journal of Health and Social Behavior, 43(2), 207–222. DOI 10.2307/3090197. [Google Scholar] [CrossRef]
41. Munder, T., Barth, J. (2018). Cochrane’s risk of bias tool in the context of psychotherapy outcome research. Psychotherapy Research, 28(3), 347–355. DOI 10.1080/10503307.2017.1411628. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools