 Open Access
Open Access
ARTICLE
Emergency room management of urolithiasis: a sex-based comparison
1 Department of Anesthesiology and Critical Care, School of Medicine, University of New Mexico, Albuquerque, NM 87131, USA
2 Division of Urology, Department of Surgery, School of Medicine, University of New Mexico, Albuquerque, NM 87131, USA
3 Department of Obstetrics and Gynecology, School of Medicine, University of New Mexico, Albuquerque, NM 87131, USA
* Corresponding Author: Frances Alba. Email:
Canadian Journal of Urology 2025, 32(2), 81-88. https://doi.org/10.32604/cju.2025.063415
Received 14 January 2025; Accepted 11 April 2025; Issue published 30 April 2025
Abstract
Introduction: Existing literature has highlighted disparities in acute pain management across racial and sex groups in both emergency department and pre-hospital settings. This study aimed to evaluate prescribing patterns among physicians and advanced practice providers for patients with upper tract urolithiasis in an academic emergency department. Materials and Methods: Retrospective chart review of patients diagnosed with upper tract urolithiasis was performed to evaluate age, sex, race, ethnicity, stone size and location, presence of hydronephrosis, admission status, history of prior nephrolithiasis, medications administered in the emergency department (ED), requests for urology consult or referral, and discharge medications. Results and Conclusions: In this single-center, propensity-matched analysis, we found no significant sex, race, or provider level of training-based differences in prescribing patterns for patients presenting with renal colic secondary to upper urinary tract stones in our academic emergency department.Keywords
Urolithiasis affects up to 11% of adults in the United States, with an estimated incidence of 2054 stones per 100,000 adults annually.1 Severe flank or back pain from renal colic, as well as associated symptoms such as nausea and vomiting, results in a substantial number of emergency department (ED) visits each year.2
Existing literature has highlighted disparities in acute pain management across racial and sex groups in both ED 3–5 and pre-hospital settings.6 Additionally, factors like type of provider licensure have also been shown to influence opioid prescribing rates in both acute and chronic pain contexts.7,8 However, there remains limited research focusing on racial and sex-based differences in pain management strategies in urologic patients, with existing literature on renal colic specifically being equivocal.9,10
Our study sought to use a propensity-based approach to determine whether sex-based differences exist in the treatment of nephrolithiasis within our academic ED, both during the visit and at discharge. Secondary analysis of differences in prescribing patterns by patient ethnicity or by provider license level was also performed. Identifying such disparities is essential to ensuring equitable care, optimizing healthcare spending, minimizing morbidity, and improving pain management strategies for all patients.
After obtaining Institutional Review Board approval, we conducted this single-center retrospective study of patients presenting to an academic ED with a primary diagnosis of nephrolithiasis between January 2022 to November 2023, comparing propensity-matched cohorts of males vs. females. Facility billing data was utilized to identify patients who presented to our ED using International Classification of Diseases 10 codes related to nephrolithiasis, including N200, N201, N202, N209, and N23. Only initial visits were utilized for matching and primary data analysis; however, dates of subsequent visits that were related to stones were recorded to evaluate rates of ED re-presentation.
Inclusion criteria were as follows: (1) ≥18 years of age, (2) presenting to the ED with a primary diagnosis of nephrolithiasis, (3) confirmed diagnosis of nephrolithiasis (via computed tomography or ultrasound imaging). Exclusion criteria were as follows: (1) Lower urinary tract stones within the bladder or urethra as confirmed by imaging, (2) pregnancy as confirmed by patient report or standard of care testing, (3) incarcerated individuals. Only records with complete data were used for matching and final analysis .
The electronic medical record was reviewed, and data were manually extracted on the following categories: age, sex, race, ethnicity, stone size and location, presence of hydronephrosis, admission status, history of prior nephrolithiasis, medications administered in the ED, requests for urology consult or referral, and discharge medications. Radiology reports were reviewed for stone location and size. Study data were collected and managed using REDCap electronic data capture tools hosted at the University of New Mexico. REDCap is a secure, web-based application designed to support data capture for research studies, providing: (1) An intuitive interface for validated data entry, (2) Audit trails for tracking data manipulation and export procedures, (3) Automated export procedure for seamless data downloads to common statistical packages, and (4) Procedures for importing data from external sources.11
Outcomes of interest included proportions of: patients who received opioids in the ED and at discharge, patients discharged with medical expulsive therapy (MET), patients discharged with any prescription for an analgesic, patients who received urology referral or consultation, and patients who re-presented to the ED within 30 days for uncontrolled pain or complications related to the stone.
R statistical software was used for all statistical analyses.12 The “MatchIt” package was used for propensity score matching.13 Matching was performed at a ratio of 1:1 male to female using age, race, ethnicity, history of stones, stone size and location, presence of hydronephrosis, and admission status. Matches were based on greedy nearest-neighbor matching without replacement. We set caliper width at 20% of the standard deviation of the logit of the probability of being in the male group.14
Routine summary statistics were calculated for all outcomes of interest, including means with standard deviations for normally distributed continuous data, medians and interquartile ranges for those not normally distributed, and percentages for binary and categorical data. Wilcoxon-Mann-Whitney, Fisher’s Exact, and Student’s t-test were applied as appropriate. The Holm-Šídák method was used to correct for multiple comparisons. Multiple logistic and linear regression analyses were performed to analyze for effects of ethnicity and provider license level on outcomes of interest. A p-value of less than 0.05 was deemed to be statistically significant.
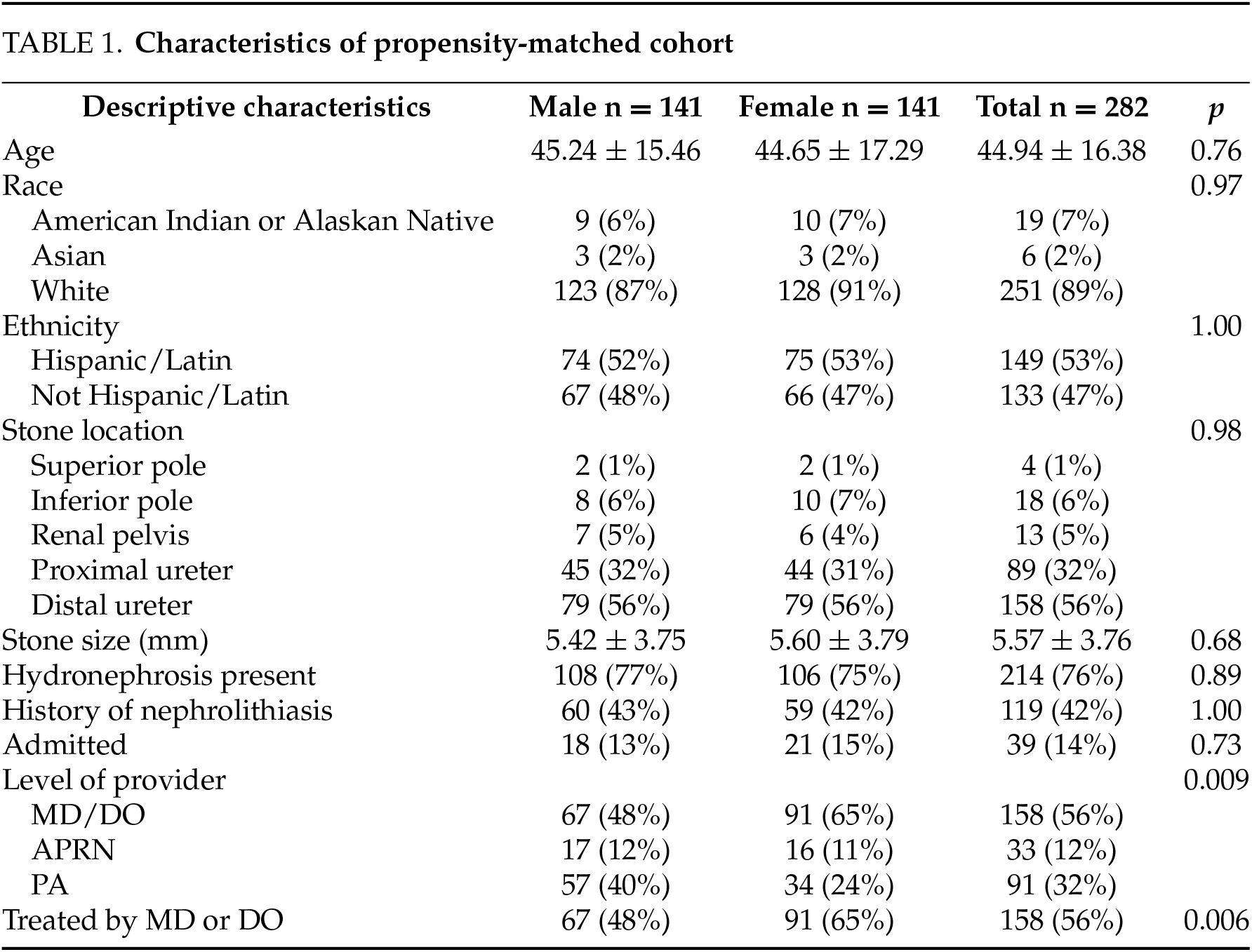
A total of 492 initial encounters were identified. After applying exclusion criteria and filtering for complete records, 338 records remained for matching and subsequent analysis. Propensity score matching yielded 282 total records for analysis (141 male and 141 female). There were no significant differences in baseline characteristics between the two groups (p > 0.05, Table 1) except for practice level of the principal provider (p = 0.009, Table 1) with females being more frequently treated by physicians than males (65% vs. 48% p = 0.006; RR = 1.48 95% CI = 1.13–1.94; Table 1).
After controlling for covariates using our propensity matched approach, there were no statistically significant differences in the proportion of males and females who received opioid analgesia in the ED, or who received a urology consultation or referral (p > 0.05, Table 2). Furthermore, there were no statistically significant differences in the number of opiate, non-opiate, or total analgesic administration counts (p > 0.05, Figure 1).
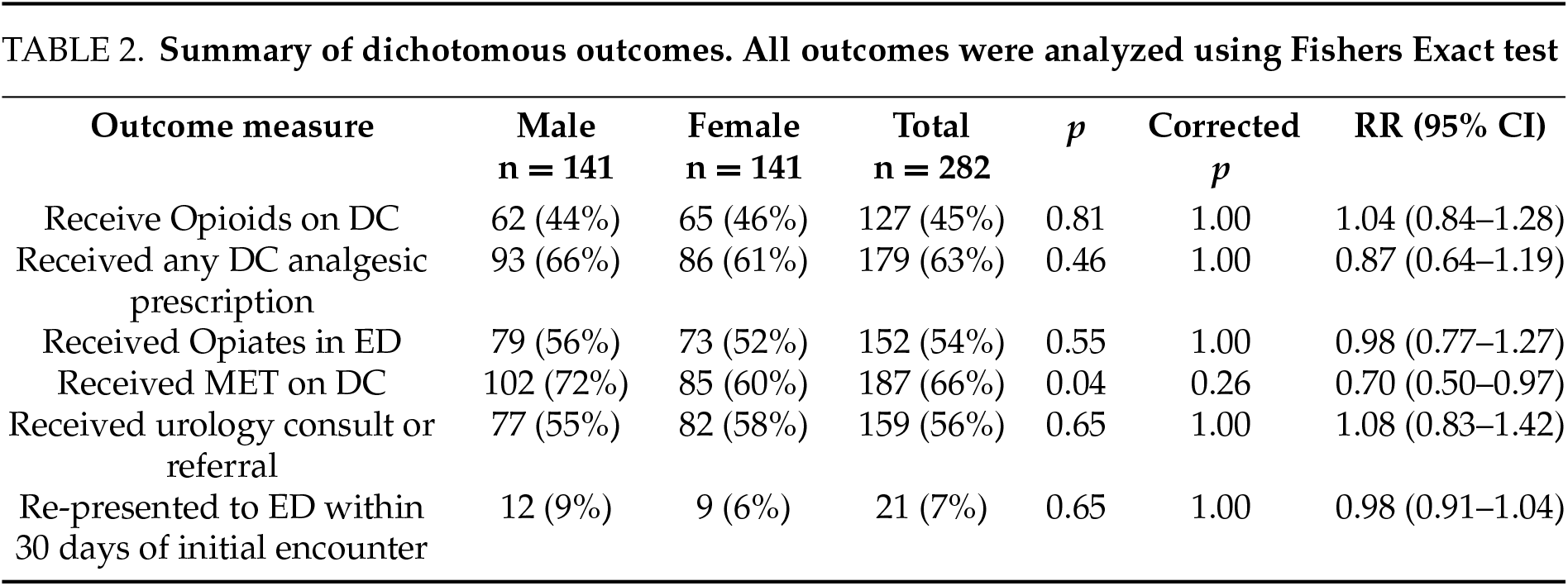

FIGURE 1. Violin plots of continuous outcomes. Diamond represents median. (A) number of opiate tablets prescribed at discharge, (B) total number of analgesic doses received in the ED, (C) number of opioid analgesic doses received in the ED, and (D) number of non-opioid analgesic doses received in the ED. There were no significant differences in any of the observed outcomes using the Wilcoxon-Mann-Whitney test. It should be noted that a smoothing bandwidth of 0.7 was used for plot A for visualization purposes while a bandwidth of 0.3 was used for the remaining plots
On discharge, there were no significant differences in the proportion of males and females who were discharged with a prescription for opioid analgesics or who received a prescription for any type of analgesic medication (p > 0.05, Table 2). On initial analysis, females appeared less likely to receive MET (60% vs. 72% p = 0.04; RR = 0.70, 95% CI = 0.50–0.97), however, after controlling for multiple comparisons, this difference was not statistically significant (p = 0.26, Table 2). Furthermore, there was no significant difference in the quantity of opioid tablets prescribed on discharge (p > 0.05, Figure 1).
Males and females in this cohort exhibited similar likelihood to re-present to the ED within 30 days of initial presentation (p > 0.05, Table 2). Multiple logistic and linear regression analyses revealed no significant effects of race or provider license level on any of the analyzed outcomes when adjusting for patient sex and for interactions of those factors with sex (p > 0.05 for all).
Our propensity-matched analysis identified no statistically significant difference in the prescription management or re-presentation rates of patients managed in our academic emergency department for renal colic secondary to upper urinary tract stones based on patient sex, patient race, or provider level.
Previous literature suggests that sex based differences in pain management exist in certain settings, such as ED15–17 and pre-hospital environments.6 A previously published review on sex-based disparities in pain suggests that much of the evidence on these disparities is anecdotal with few sufficiently powered studies to suggest otherwise.18 Indeed, there are published data to suggest that patient sex or gender does not influence pain management strategies.19–21 The existing literature on sex-based differences in the setting of renal colic is equivocal. Naamany et al. found that, in the context of stones, males were more quickly and more frequently assessed for pain, received more analgesics, and were prescribed opioids at higher rates than females.9 Innes et al. reported similar rates of intravenous ketorolac and opioid administration, with no significant difference in outcomes in the setting of stones, although only physicians were treating patients at this hospital.10 Both studies showed that males underwent computer tomography scans more frequently than females. Our findings suggest that males and females receive comparable management for renal colic secondary to upper urinary tract stones at our institution. Additionally, we found no significant impact of patient ethnicity on prescribing patterns or outcomes. However, our study population was predominantly white, and after propensity score matching, Black and Native Hawaiian/Pacific Islander patients were absent from the analyzed cohort. This is likely due to a relatively small number of these demographic groups being present in the state of New Mexico at 2.8% and 0.2%, respectively.22 Nevertheless, this lack of representation limits our ability to comprehensively assess the effects of race on these findings as previous studies have done6,15,16 underscoring the need for more diverse patient populations in future research.
Approximately 54% of patients in our cohort received an opiate while in the ED and 45% received a prescription for an opiate upon discharge. A report from 2020 by the Centers for Disease Control and Prevention and National Center for Health Statistics described a national ED opiate prescription rate of 14.6% from 2016–2017, with much higher rates for urolithiasis at 49.2%.23 Another report found that 59% and 68% of patients diagnosed with urolithiasis received opiates in the ED and at discharge respectively.24 In this study, the rates of opiate prescriptions, both in the ED and at discharge, are comparable to published literature.
A working paper from the National Bureau of Economic Research found that nurse practitioners at a Veterans Affairs hospital, on average, use more resources and achieve less favorable outcomes, such as 30-day preventable hospitalization.25 However, several systematic reviews of nurse practitioners in emergency and critical care settings came to favorable conclusions, suggesting that nurse practitioners may indeed improve outcomes, decrease wait times, and increase patient satisfaction.26–28 Our analysis fails to suggest that provider license level had any impact on management or outcomes of these patients, as there were no statistically significant differences in prescribing patterns or outcomes between physicians and advanced practice providers. Some literature, however suggests that provider-level characteristics, such as age, may indeed influence prescribing patterns.29 However, the effects of other variables like provider sex and race remain less well-defined.30,31 Unfortunately, as these variables were not available in our dataset, we are unable to evaluate their potential impact on prescribing patterns. Future studies should incorporate these factors to provide a more comprehensive understanding of how both provider and patient characteristics influence treatment decisions and outcomes.
Our analyses initially found a statistically significant difference in the prescribing patterns of MET, with males appearing more likely to receive a prescription than females. This significance disappeared with multiple comparisons correction. Current guidelines on management of ureteral stones suggest that patients with uncomplicated distal ureteral stones should be offered medical expulsive therapy with alpha-blocker medication.32,33 While our primary analysis does not differentiate the rates of MET for a given stone location, our cohort is enriched in distal ureteral stones, and post-hoc analysis found that for distal stones <10 mm in size, 75% of males and 72% of females received a prescription for MET. While these data suggest that males and females at our institution receive similar rates of MET, they may imply that MET is being underutilized, particularly for distal ureteral stones, where literature supports their use.34
Interestingly, only 56% of patients received a consultation or referral to urology. Only 21 (7%) patients re-presented to the ED for renal colic and received intervention. While current guidelines recommend that patients with uncomplicated ureteral stones less than or equal to 10 mm should be offered observation32, it is unclear if the patients not referred to urology were followed for successful trial of passage by another provider. With the rising incidence of stones and shortage of urologists in the United States, retained stones raise the possibility of patients progressing to renal atrophy or xanthogranulomatous pyelonephritis if patients have unidentified failed trials of passage. Future directions could include patient education materials and referral pipelines for patients sent home on trial of passage.
The primary strength of this study lies in its use of a propensity-matched approach for analysis, which helps mitigate potential sources of confounding. However, several limitations should be acknowledged. First, although the propensity-matching method allowed us to control for numerous covariates, inconsistent reporting and documentation of pain scores in our emergency department limited our ability to account for self-reported pain levels. Consequently, we could not assess how variations in pain scores influenced management strategies or clinical outcomes. Moreover, the underrepresentation of certain racial groups further limits our study’s ability to assess potential racial disparities in emergency room management of urolithiasis. Additionally, patients included in our cohort may have sought care at other emergency departments or urgent care centers within the region, potentially contributing to lower rates of re-presentation observed in our data. Furthermore, limiting our study to patients with imaging-confirmed upper-tract stones prevents assessment of management differences in those diagnosed clinically or undiagnosed. This may obscure sex-based disparities in diagnostic timeliness and completeness. Future studies with broader inclusion criteria may reveal additional disparities in this domain. Lastly, the relatively small sample size of our cohort, compared to previously published studies, limits both the statistical power and generalizability of our findings. Future studies with larger, multicenter datasets are needed to validate these results and further explore the impact of self-reported pain on patient outcomes.
In this single-center, propensity-matched analysis, we found no significant sex-based differences in the management or outcomes of patients presenting with renal colic secondary to upper urinary tract stones in our academic emergency department. Our findings align with existing literature suggesting that patient sex does not impact pain management strategies for renal colic. Although males initially appeared more likely to receive medical expulsive therapy (MET), this difference was not statistically significant after adjusting for multiple comparisons. However, our findings did suggest that MET may be underutilized for distal ureteral stones, underscoring the importance of further adherence to guideline-recommended therapies. Future research with larger, multicenter datasets is necessary to support these findings, improve understanding of sex and race-based disparities, and optimize pain management strategies in nephrolithiasis. This work emphasizes the importance of equitable care and the need for consistent guideline implementation to enhance patient outcomes in the ED setting.
Acknowledgement
None.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contributions
Mark Shilling Conceptualization, Methodology, Formal Analysis, Investigation, Data Curation, Writing—Original Draft, Visualization; Lauren Faber: Conceptualization, Methodology, Investigation, Data Curation, Writing—Original Draft; Hoi Doan: Investigation, Data Curation, Writing—Review & Editing; Merry Peckham: Investigation, Data Curation, Writing—Review & Editing; Timothy R. Petersen: Formal Analysis, Visualization, Writing—Review & Editing; Reza Ehsanian: Supervision, Writing—Review & Editing; Frances Alba: Conceptualization, Methodology, Investigation, Writing—Review & Editing, Supervision, Project Administration. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
Raw data can be made available upon reasonable request to the corresponding author.
Ethics Approval
This study was approved by the University of New Mexico Health Sciences Center, Human Research Protections Office, under Institutional Review Board Approval #23-495.
Conflicts of Interest
The authors declare no conflicts of interest to report regarding the present study.
References
1. Hill AJ, Basourakos SP, Lewicki P et al. Incidence of kidney stones in the United States: the continuous national health and nutrition examination survey. J Urol 2022;207(4):851–856. doi:10.1097/JU.0000000000002331. [Google Scholar] [PubMed] [CrossRef]
2. Foster G, Stocks C, Borofsky MS. Emergency department visits and hospital admissions for kidney stone disease, 2009. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MDAgency for Healthcare Research and Quality (US); 2006. [Internet]. [cited 2024 Aug 28]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK100827/. [Google Scholar]
3. Banco D, Chang J, Talmor N et al. Sex and race differences in the evaluation and treatment of young adults presenting to the emergency department with chest pain. J Am Heart Assoc 2022;11(10):e024199. doi:10.1161/JAHA.121.024199. [Google Scholar] [PubMed] [CrossRef]
4. Barr A, Eilat-Tsanani S. Prescribing analgesics for low back pain: is there a gender difference? J Womens Health 2022;31(1):79–83. doi:10.1089/jwh.2021.0039. [Google Scholar] [PubMed] [CrossRef]
5. Chen EH, Shofer FS, Dean AJ et al. Gender disparity in analgesic treatment of emergency department patients with acute abdominal pain. Acad Emerg Med 2008;15(5):414–418. doi:10.1111/j.1553-2712.2008.00100.x. [Google Scholar] [PubMed] [CrossRef]
6. Bradford JM, Cardenas TC, Edwards A et al. Racial and ethnic disparity in prehospital pain management for trauma patients. J Am Coll Surg 2023;236(3):461–467. doi:10.1097/XCS.0000000000000486. [Google Scholar] [PubMed] [CrossRef]
7. Nikpour J, Broome M, Silva S, Allen KD. Influence of primary care provider type on chronic pain management among veterans. J Nurs Regul 2022;13(1):35–44. doi:10.1016/S2155-8256(22)00032-1. [Google Scholar] [PubMed] [CrossRef]
8. Roblin DW, Liu H, Cromwell LF et al. Provider type and management of common visits in primary care. Am J Manag Care 2017;23(4):225–231. [Google Scholar] [PubMed]
9. Naamany E, Reis D, Zuker-Herman R, Drescher M, Glezerman M, Shiber S. Is there gender discrimination in acute renal colic pain management? A retrospective analysis in an emergency department setting. Pain Manag Nurs 2019;20(6):633–638. doi:10.1016/j.pmn.2019.03.004. [Google Scholar] [PubMed] [CrossRef]
10. Innes GD, Scheuermeyer FX, Law MR et al. Sex-related differences in emergency department renal colic management: females have fewer computed tomography scans but similar outcomes. Acad Emerg Med 2016;23(10):1153–1160. doi:10.1111/acem.13041. [Google Scholar] [PubMed] [CrossRef]
11. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377–381. doi:10.1016/j.jbi.2008.08.010. [Google Scholar] [PubMed] [CrossRef]
12. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: r Foundation for Statistical Computing; 2023. [Google Scholar]
13. Ho DE, Imai K, King G, Stuart EA. MatchIt: Nonparametric preprocessing for parametric causal inference. J Stat Softw 2011;42(8):1–28. doi:10.18637/jss.v042.i08. [Google Scholar] [CrossRef]
14. Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 2011;10(2):150–161. doi:10.1002/pst.433. [Google Scholar] [PubMed] [CrossRef]
15. Dickason RM, Chauhan V, Mor A et al. Racial differences in opiate administration for pain relief at an academic emergency department. West J Emerg Med 2015;16(3):372–380. doi:10.5811/westjem.2015.3.23893. [Google Scholar] [PubMed] [CrossRef]
16. Goyal MK, Kuppermann N, Cleary SD, Teach SJ, Chamberlain JM. Racial disparities in pain management of children with appendicitis in emergency departments. JAMA Pediatr 2015;169(11):996–1002. doi:10.1001/jamapediatrics.2015.1915. [Google Scholar] [PubMed] [CrossRef]
17. Guzikevits M, Gordon-Hecker T, Rekhtman D et al. Sex bias in pain management decisions. Proc Nat Acad Sci 2024;121(33):e2401331121. doi:10.1073/pnas.2401331121. [Google Scholar] [PubMed] [CrossRef]
18. Hoffmann DE, Fillingim RB, Veasley C. The woman who cried pain: do sex-based disparities still exist in the experience and treatment of pain? J Law Med Ethics 2022;50(3):519–541. doi:10.1017/jme.2022.91. [Google Scholar] [PubMed] [CrossRef]
19. Siriwardena AN, Asghar Z, Lord B et al. Patient and clinician factors associated with prehospital pain treatment and outcomes: cross sectional study. Am J Emerg Med 2019;37(2):266–271. doi:10.1016/j.ajem.2018.05.041. [Google Scholar] [PubMed] [CrossRef]
20. Safdar B, Heins A, Homel P et al. Impact of physician and patient gender on pain management in the emergency department–a multicenter study. Pain Med 2009;10(2):364–372. doi:10.1111/j.1526-4637.2008.00524.x. [Google Scholar] [PubMed] [CrossRef]
21. Heins JK, Heins A, Grammas M, Costello M, Huang K, Mishra S. Disparities in analgesia and opioid prescribing practices for patients with musculoskeletal pain in the emergency department. J Emerg Nurs 2006;32(3):219–224. doi:10.1016/j.jen.2006.01.010. [Google Scholar] [PubMed] [CrossRef]
22. US. Census Bureau QuickFacts: New Mexico. [Internet]. [cited 2025 Feb 25]. Available from: https://www.census.gov/quickfacts/fact/table/NM/PST045223. [Google Scholar]
23. Rui P, Santo L, Ashman JJ. Trends in opioids prescribed at discharge from emergency departments among adults: United States, 2006–2017. Natl Health Stat Report 2020;135:1–12. [Google Scholar]
24. Wentz AE, Wang RR, Marshall BD, Shireman TI, Liu T, Merchant RC. Variation in opioid analgesia administration and discharge prescribing for emergency department patients with suspected urolithiasis. Am J Emerg Med 2020;38(10):2119. doi:10.1016/j.ajem.2020.07.016. [Google Scholar] [PubMed] [CrossRef]
25. Chan D, Chen Y. The productivity of professions: evidence from the emergency department. Rochester, NY: Social Science Research Network; 2022. [Internet]. [cited 2024 Oct 17]. Available from: https://papers.ssrn.com/abstract=4262592. [Google Scholar]
26. Carter AJE, Chochinov AH. A systematic review of the impact of nurse practitioners on cost, quality of care, satisfaction and wait times in the emergency department. Can J Emerg Med 2007;9(4):286–295. doi:10.1017/S1481803500015189. [Google Scholar] [PubMed] [CrossRef]
27. Jennings N, Clifford S, Fox AR, O’Connell J, Gardner G. The impact of nurse practitioner services on cost, quality of care, satisfaction and waiting times in the emergency department: a systematic review. Int J Nurs Stud 2015;52(1):421–435. doi:10.1016/j.ijnurstu.2014.07.006. [Google Scholar] [PubMed] [CrossRef]
28. Woo BFY, Lee JXY, Tam WWS. The impact of the advanced practice nursing role on quality of care, clinical outcomes, patient satisfaction, and cost in the emergency and critical care settings: a systematic review. Hum Resour Health 2017;15(1):63. doi:10.1186/s12960-017-0237-9. [Google Scholar] [PubMed] [CrossRef]
29. Laurence C.Baker P, Kessler D, Vaska G. The relationship between provider age and opioid prescribing behavior; 2022. [Internet]. [cited 2025 Feb 25]. Available from: https://www.ajmc.com/view/the-relationship-between-provider-age-and-opioid-prescribing-behavior. [Google Scholar]
30. Rambachan A, Joshi M, Auerbach AD, Fang MC. Sex concordance between physicians and patients and discharge opioid prescribing. J Hosp Med 2024;19(7):605–609. doi:10.1002/jhm.13389. [Google Scholar] [PubMed] [CrossRef]
31. Rochon P, Borhani P, Akerman J, Mishra A. Physician variation in opioid prescribing: the importance of sex and gender. BMJ Qual Saf 2022;31(5):331–333. doi:10.1136/bmjqs-2021-013697. [Google Scholar] [PubMed] [CrossRef]
32. Assimos D, Krambeck A, Miller NL et al. Surgical management of stones: American urological association/endourological society guideline, PART I. J Urol 2016;196(4):1153–1160. doi:10.1016/j.juro.2016.05.090. [Google Scholar] [PubMed] [CrossRef]
33. Skolarikos A, Jung H, Neisus A et al. EAU guidelines on urolithiasis. Arnhem, the Netherlands: eAU Guidelines Office; 2024. [Internet]. [cited 2025 Feb 25]. Available from: https://uroweb.org/guidelines/urolithiasis. [Google Scholar]
34. Cui Y, Chen J, Zeng F et al. Tamsulosin as a medical expulsive therapy for ureteral stones: a systematic review and meta-analysis of randomized controlled trials. J Urology 2019;201(5):950–955. doi:10.1097/JU.0000000000000029. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools