 Open Access
Open Access
CASE REPORT
Cryptic torsion: a case report of intra-abdominal supernumerary testicular torsion in a pediatric patient with normal descended testes
1 Department of Urology, Medical College of Wisconsin, Milwaukee, WI 53226, USA
2 Division of Urology, Children’s Hospital of Wisconsin, Milwaukee, WI 53226, USA
* Corresponding Author: Megan G. Paradzinsky. Email:
Canadian Journal of Urology 2025, 32(3), 213-217. https://doi.org/10.32604/cju.2025.063777
Received 23 January 2025; Accepted 16 May 2025; Issue published 27 June 2025
Abstract
Polyorchidism is a rare anomaly of the male urogenital tract characterized by the presence of one or more extra testes. Supernumerary testes can often present with coexistent conditions, including cryptorchidism, inguinal hernia, and torsion. We report a case of a pediatric patient with initial concern for intra-scrotal left testicular torsion on ultrasonography who was ultimately found to have torsion of an intra-abdominal supernumerary testis. He underwent scrotal exploration with bilateral orchiopexy and laparoscopic excision of the torsed gonad. This case highlights a unique presentation of polyorchidism with incongruent descent of an ipsilateral supernumerary testis.Keywords
Supplementary Material
Supplementary Material FilePolyorchidism is a rare anomaly of the male urogenital tract characterized by the presence of one or more extra testes. Triorchidism is the most common type, and a majority of supernumerary testes are located within the scrotum.1 The median age at presentation is 20 years.2 While patients are often asymptomatic, they can present with concomitant conditions, including torsion. We present a case of a torsed supernumerary intra-abdominal testis in a two-year-old boy with normal testes within the scrotum, found incidentally during diagnostic laparoscopy and scrotal exploration. Intraoperative findings were discordant from scrotal ultrasound findings. We describe this patient’s operative management with scrotal exploration with bilateral orchiopexy and laparoscopic excision of the torsed gonad, as well as his postoperative course. This case has been reported in line with the SCARE criteria.3 Institutional Review Board review was not required per the Medical College of Wisconsin Standard Operating Procedure for Case Reports. Informed consent was obtained for this study and accompanying images from the patient’s legal guardian.
Case Report: A two-year-old otherwise healthy male presented to the children’s hospital emergency department with left scrotal swelling. The swelling had been steadily increasing in size for approximately one month. The family had not sought care for this finding before emergency department presentation. In the hours prior to presentation, the swelling was felt to be rapidly worsening, and the patient was noted to be fussier than baseline. There was no associated emesis or fever. On exam, his abdomen was soft, non-distended, and nontender. He had a buried phallus. The left hemiscrotum was enlarged and tense with overlying erythema, and the left testicle was nonpalpable (Figure 1). The right testicle was descended and palpable.

FIGURE 1. Visual genitourinary examination of the patient
Pediatric Surgery was initially consulted due to concern for an incarcerated inguinal hernia. Point-of-care bedside ultrasound of the left inguinal canal was performed by Pediatric Surgery, and the contents appeared consistent with bowel per their read. Bedside reduction was attempted without success; thus, he was taken to the operating room emergently with Pediatric Surgery for hernia reduction and repair. Time from preliminary diagnosis of incarcerated inguinal hernia to case start was approximately two hours. Diagnostic laparoscopy revealed a closed inguinal ring without hernia and a loculated cystic mass just adjacent to the left ring (Figure 2). The cystic mass was 4 cm × 2.7 cm × 2 cm and dusky red-grey in appearance, with brown hemorrhagic material adherent to the external surface. The structure did not have any association with the bowel. At this point, Pediatric Urology was consulted intra-operatively. Formal intra-operative scrotal ultrasound was obtained, which revealed the left testicle located in the left hemiscrotum without blood flow on color Doppler evaluation (Figure 3A). A large lobulated, multiseptated, complex avascular fluid collection was seen in the left inguinal canal without extension into the peritoneal cavity (Figure 3B). The right testis was retractile but appeared normal (Figure 4).
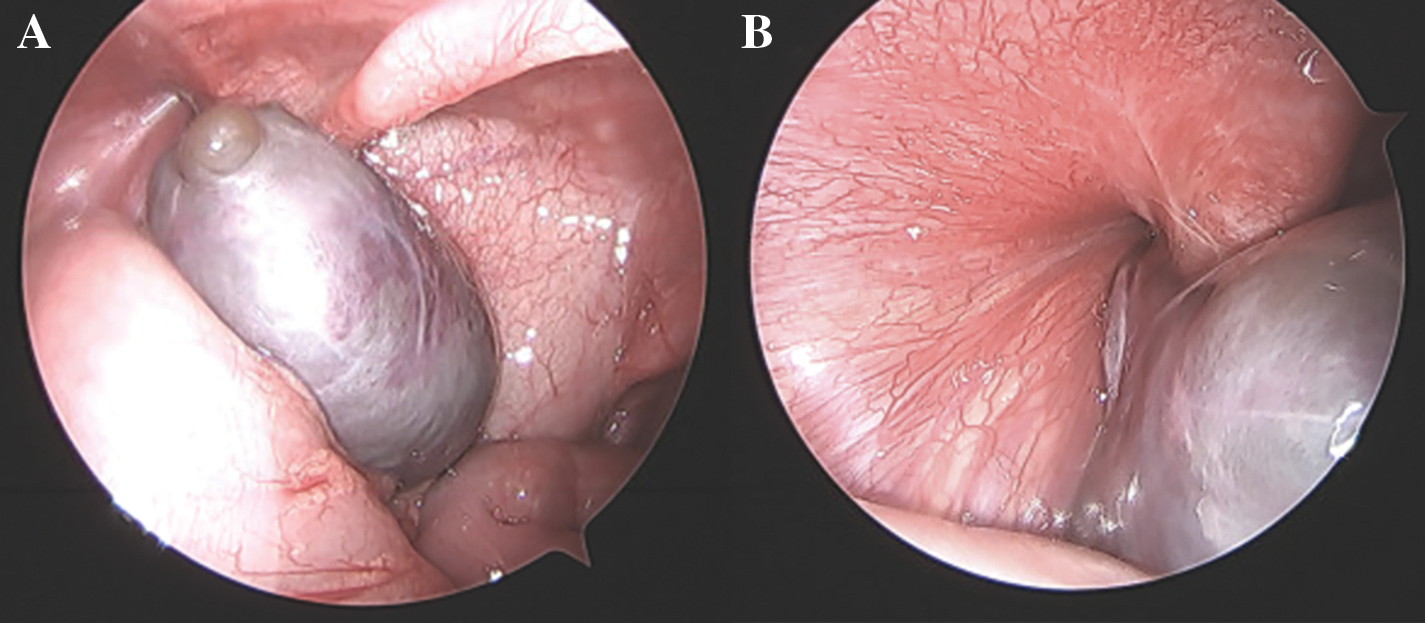
FIGURE 2. Laparoscopic images demonstrating the intra-abdominal findings during surgical exploration. (A) Laparoscopic view of cystic pelvic mass. (B) Laparoscopic view of the adjacent closed left inguinal ring
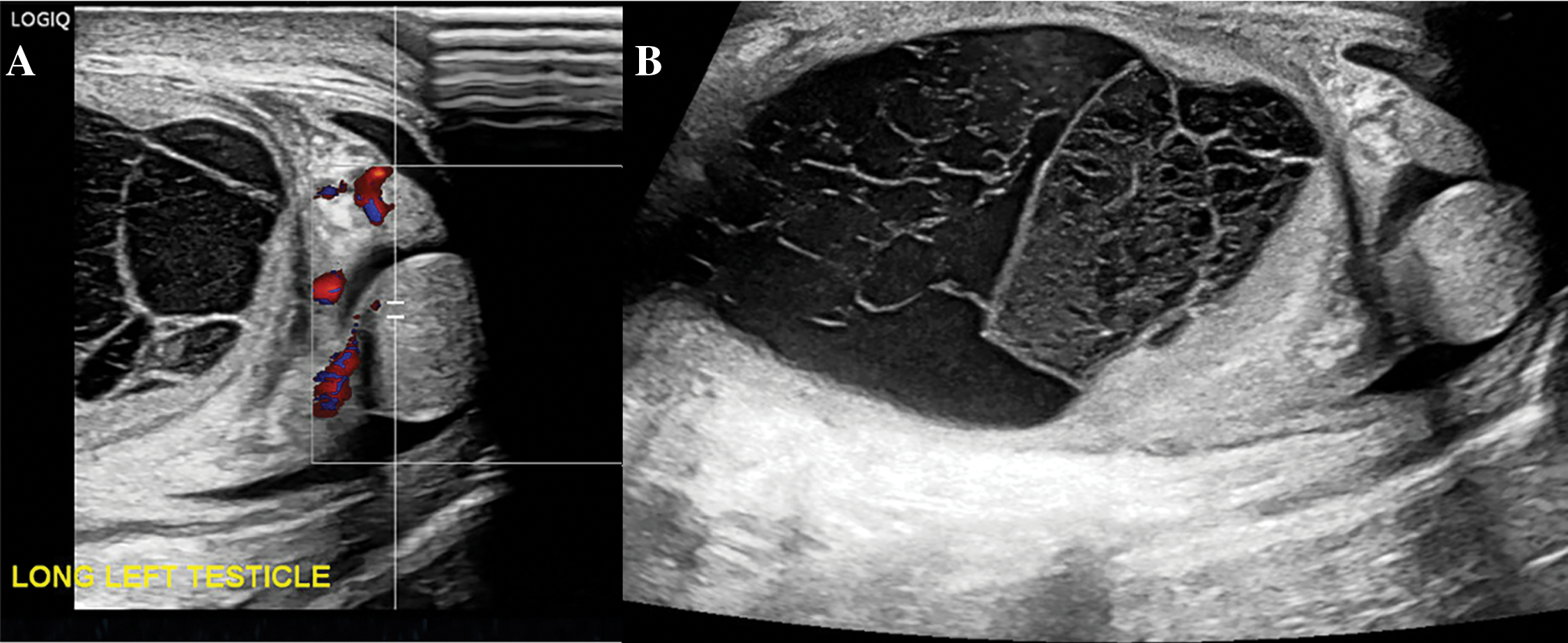
FIGURE 3. Intraoperative formal scrotal ultrasound findings of the left hemiscrotum. (A) Ultrasound with Doppler highlighting left scrotal testis without flow and enlarged hyperemic epididymis. (B) Ultrasound showing a large, multiseptated left hydrocele
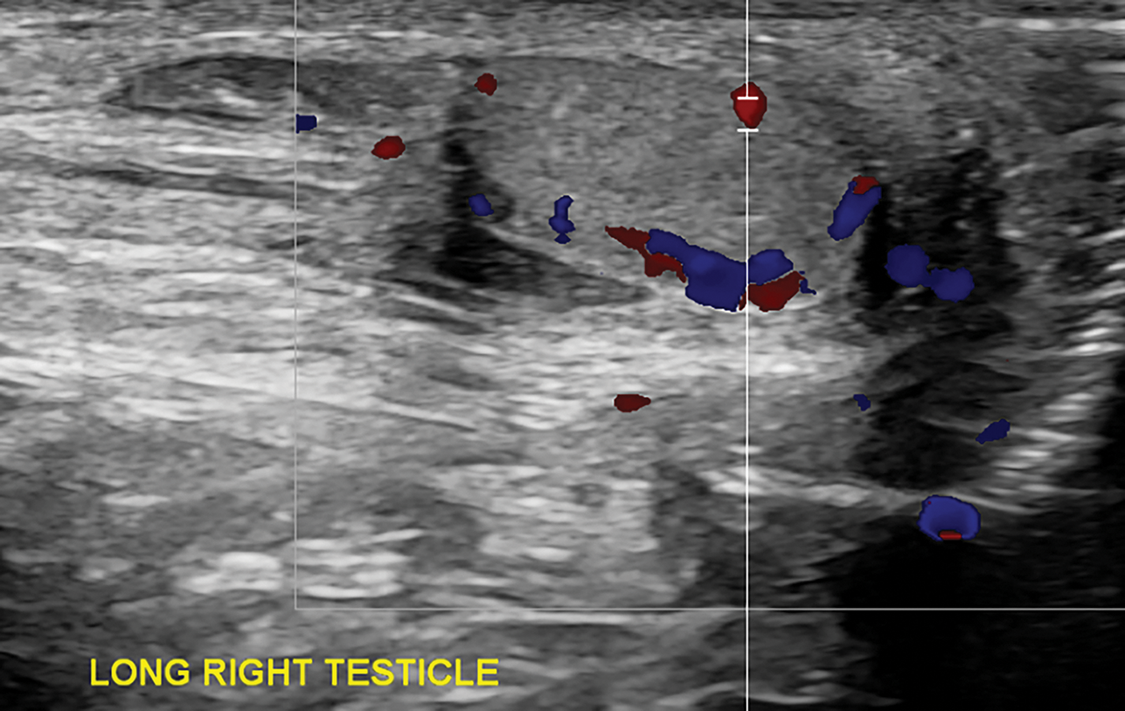
FIGURE 4. Ultrasound with Doppler highlighting the right testis with normal echotexture and blood flow
Given concern for left testicular torsion, the decision was made to perform scrotal exploration and laparoscopic excision of the pelvic mass. When the left testicle was delivered, it was noted to be pink and healthy with normal lie. The gonadal vessels were visualized without torsion, but the dartos and tunica vaginalis were severely thickened. Though he did not have torsion intraoperatively, we elected to perform bilateral orchiopexy given his imaging findings. A ¼-inch Penrose drain was placed through the lateral left scrotum into the prior hydrocele cavity. Repeat laparoscopy revealed the cystic mass was unchanged following scrotal exploration. There appeared to be a twisted stalk leading to the cystic mass. The vessels and thickened tissue going to the mass were ligated with clips and incised. While the mass had the appearance of a torsed gonad with cystic changes, malignancy could not be ruled out. Therefore, the mass was removed via a specimen bag to ensure no spillage of cystic contents.
The patient was admitted to the Pediatric Urology service postoperatively. On postoperative day one, he had increased erythema on scrotal exam and fever to 101°F, and the operating surgeon was concerned for superficial skin infection. He was subsequently started on a seven-day course of oral antibiotics. He otherwise had an uneventful postoperative course with resumption of age-appropriate diet, normal voiding, and return of bowel function and baseline activity. He was discharged on postoperative day two. Penrose drain was removed in the clinic on postoperative day five without complication. Pathology report completed by a pediatric pathologist showed coagulative necrosis of a partially mesothelium-lined fibrovascular wall attached to a ghost-like remnant of necrotic testicular tissue. There was no viable testicular tissue, signs of neoplasia, or intestinal tissue identified. Information regarding immunohistochemical staining was not included in the report. At one-month clinic follow-up with the operating surgeon, the patient had recovered well without residual scrotal swelling.
Polyorchidism is a rare congenital anomaly with fewer than 250 cases reported in the literature.1,2 It originates from the transverse or longitudinal division of the urogenital ridge between the fourth and sixth week of development.4 This embryologic etiology has accordingly influenced classification systems for supernumerary testicles, of which the most comprehensive system proposed by Bergholz et al. classifies the testes based on whether or not they are drained by a ductus deferens and further divides them based on the presence of their own vs. shared epididymis.5 In our case, the undrained supernumerary testis seemed to have consisted of testicular tissue only based on pathology, but the true nature is difficult to determine given the necrotic presentation.
Regarding the location of supernumerary testes, a majority of cases are found in the scrotum, and only 3%–9% of cases are localized to the abdomen.1,2 Approximately 65% of supernumerary testes are noted on the left, as with our case.1,2 The left testis is thought to be more prone to division given its larger size and different vascular topographic anatomy.6 There is not yet an established pattern or understanding of the location of a supernumerary testis about its ipsilateral testis. Many cases describe the testes to be neighbors, but the positioning can be discordant. Bergholz et al. reported in their meta-analysis that of the 12 supernumerary testes found intra-abdominally, only 2 ipsilateral testes were noted in normal scrotal positions.1
Polyorchidism is frequently diagnosed incidentally after presenting with other conditions.2 The concomitant pathologies include ipsilateral inguinal hernia (15%–24% of cases), cryptorchidism (15%–22%), and, less commonly, testicular torsion (7%–15%) and hydrocele (7%–9%).1,2 Testicular malignancy has also been found in cases of polyorchidism, primarily when maldescended.1
Our patient had a unique presentation as he seemed to initially have a possible inguinal hernia vs. intra-scrotal testicular torsion with complex hydrocele on ultrasound, but he was ultimately noted to have a normal descended testis with ipsilateral intra-abdominal supernumerary testicular torsion. We suspect the hydrocele was reactive to his intra-abdominal torsion and resulted in false-positive intra-scrotal torsion on ultrasound. Patients with known polyorchidism have a 280-fold higher absolute risk of torsion compared to the general population, so a high index of suspicion should be maintained if presenting with acute scrotal pain.2 This increased risk is likely because the supernumerary testis has an absent gubernaculum and a longer pedicle.7 Management principles of supernumerary testicular torsion are the same as those of non-complicated testicular torsion with emergent exploration, timely detorsion, and fixation.7,8 Otherwise, there has been a recent push for conservative management with active ultrasound surveillance in asymptomatic cases, even when cryptorchid.9 This differs from other proposed management algorithms, which recommend active surveillance only in cases of scrotal polyorchidism.2,10
Polyorchidism is a rare condition with a high risk of torsion. To our knowledge, this is the first reported case of torsed intra-abdominal supernumerary testis in a patient with bilateral descended testes. Management of non-viable testes with orchiectomy and of all healthy testes with orchiopexy is appropriate.
Acknowledgement
Not applicable.
Funding Statement
The authors received no specific funding for this study.
Author Contributions
The authors confirm contribution to the paper as follows: Conceptualization, Megan G. Paradzinsky, Arya R. Anvar and Travis W. Groth; data curation, Megan G. Paradzinsky; formal analysis, Megan G. Paradzinsky, Mukul Sharda and Arya R. Anvar; investigation, Megan G. Paradzinsky and Travis W. Groth; methodology, Megan G. Paradzinsky and Mukul Sharda; writing—original draft preparation, Megan G. Paradzinsky and Mukul Sharda; writing—review and editing, Megan G. Paradzinsky, Mukul Sharda, Arya R. Anvar and Travis W. Groth; supervision, Travis W. Groth. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
Not applicable.
Ethics Approval
Institutional Review Board review was not required per the Medical College of Wisconsin Standard Operating Procedure for Case Reports.
Informed Consent
Informed consent was obtained for this study and accompanying images from the patient’s legal guardian.
Conflicts of Interest
The authors declare no conflicts of interest to report regarding the present study.
Supplementary Materials
The supplementary material is available online at https://www.techscience.com/doi/10.32604/cju.2025.063777/s1.
References
1. Bergholz R, Wenke K. Polyorchidism: a meta-analysis. J Urol 2009;182(5):2422–2427. doi:10.1016/j.juro.2009.07.063. [Google Scholar] [PubMed] [CrossRef]
2. Balawender K, Wawrzyniak A, Kobos J et al. Polyorchidism: an up-to-date systematic review. J Clin Med 2023;12(2):649. doi:10.3390/jcm12020649. [Google Scholar] [PubMed] [CrossRef]
3. Sohrabi C, Mathew G, Maria N, Kerwan A, Franchi T, Agha RA. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guideline. Int J Surg 2023;109(5):1136–1140. doi:10.1097/JS9.0000000000000373. [Google Scholar] [PubMed] [CrossRef]
4. O’Sullivan DC, Biyani CS, Heal MR. Polyorchidism: causation and management. Postgrad Med J 1995;71(835):317–318. doi:10.1136/pgmj.71.835.317-a. [Google Scholar] [PubMed] [CrossRef]
5. Bergholz R, Koch B, Spieker T, Lohse K. Polyorchidism: a case report and classification. J Pediatr Surg 2007;42(11):1933–1935. doi:10.1016/j.jpedsurg.2007.07.031. [Google Scholar] [PubMed] [CrossRef]
6. Kanbar A, Dabal C, El Khoury J et al. Diagnosis and management of polyorchidism: a case report and literature review. Chen T-C, ed. Case Rep Urol 2023;2023:1–4. doi:10.1155/2023/1620276. [Google Scholar] [PubMed] [CrossRef]
7. Xiaofei L, Benzhang Z. Case report: testicular torsion in unilateral supernumerary testis. Front Pediatr 2022;10:1–3. doi:10.3389/fped.2022.823374. [Google Scholar] [PubMed] [CrossRef]
8. Kealey J, Yao HHI, Grummet J. Acute scrotum–Torsion of the third testicle!. Urol Case Reports 2018;2(3):92–93. doi:10.1016/j.eucr.2018.07.010. [Google Scholar] [PubMed] [CrossRef]
9. Arena L, Szklarz T, Costabel M, Maguiña P, De Carli C. A case of conservative management of intra-abdominal polyorchidism in a child. Urology 2023;176:187–189. doi:10.1016/j.urology.2023.03.005. [Google Scholar] [PubMed] [CrossRef]
10. Sarmiento B, Ellsworth P, Seth A. Inguinal polyorchidism found incidentally during orchiopexy in 9-year-old male: a case report and review of orchiopexy of nonscrotal supernumerary testes. Urology 2023;1–4. doi:10.1016/j.urology.2023.10.017. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools