 Open Access
Open Access
ARTICLE
Quality of life and surgical treatment regret in patients with benign prostatic hypertrophy: a multicenter study
1 Department of Urology, Weill Cornell Medicine, New York City, NY 10021, USA
2 Westchester Medical Center, Department of Urology/Urogynecology, New York Medical College School of Medicine, Valhalla, NY 10595, USA
3 Department of Urology, Northwell Health, Syosset, NY 11791, USA
4 Department of Urology, University of Montreal, Montreal, QC H3C 3J7, Canada
5 Division of Urology, University of Toronto, Toronto, ON M5R 0A3, Canada
* Corresponding Author: Bilal Chughtai. Email:
# These authors contributed equally to this work
Canadian Journal of Urology 2025, 32(3), 219-227. https://doi.org/10.32604/cju.2025.064404
Received 14 February 2025; Accepted 28 May 2025; Issue published 27 June 2025
Abstract
Introduction: Benign prostatic hypertrophy (BPH) is a common condition affecting men later in life, significantly impacting quality of life (QOL). Surgical intervention is often pursued when medical management fails, but patient satisfaction with outcomes varies. Decisional regret can affect perceived success and patient satisfaction post-surgery. This study evaluates the relationship between post-surgical symptoms and decisional regret across BPH procedures. Methods: A prospective, multicenter cohort study included 54 patients undergoing BPH surgery between March 2023 and February 2024. Patients completed the International Prostate Symptom Score-QOL (IPSS-QOL) scale preoperatively and at least three months postoperatively, along with the Decision Regret Scale (DRS). Surgical types included Urolift, Greenlight Laser, Rezum, Aquablation, and transurethral resection of the prostate (TURP). A DRS score of ≥25 indicated significant regret. Changes in IPSS-QOL were correlated with DRS scores (Spearman’s rho), and subgroup comparisons were conducted using Mann-Whitney U tests. Results: The average DRS score was 18.3, with 33% of patients reporting a DRS ≥25. Moderate correlations existed between quality of life (QOL) change (ρ = 0.34, p < 0.05) and total regret score. Minimally invasive surgical treatment (MISTs) patients demonstrated higher regret correlations than TURP. Lack of efficacy (75%), new symptoms (41%), and postoperative complications (25%) were the most common reasons for regret. Conclusion: While BPH surgery generally improves symptoms, a substantial portion of patients experience decisional regret. This underscores the importance of preoperative counseling to establish realistic expectations and reduce regret. Further research should explore strategies to enhance shared decision-making and align patient expectations with possible surgical outcomes.Keywords
Benign Prostatic Hyperplasia (BPH) is a common condition affecting men over the age of 50 and is the fourth overall leading disease in this age cohort; approximately 50% of men in their 60s and 80% of men in their 70s suffer from the disease.1,2 BPH refers to an increased size of the prostate, which may lead to lower urinary tract symptoms (LUTS). LUTS are then classified into either obstructive or irritative symptoms. The severity of LUTS in patients is often measured using the International Prostate Symptom Score (IPSS) with an additional question on quality of life (IPSS-QOL), where higher scores on the IPSS-QOL signify higher symptom severity. This screening measurement is often used to help decide which patients should move forward to surgical management over medical management and monitor outcomes after surgery.1
There is a wide array of surgical interventions for the treatment of symptomatic BPH that differ in advantages, disadvantages, and efficacy. While transurethral resection of the prostate (TURP) is considered the gold standard surgical intervention there are associated complications such as retrograde ejaculation (53–75%), erectile dysfunction (3.4–32%), and urinary retention (3–9%).3,4 For this reason, minimally invasive surgical techniques (MISTs) are favorably considered by many patients. While the current literature reports clinical outcomes of these surgeries, none to date have compared regret from each of them.
There is a strong correlation between BPH symptoms and patient quality of life. German et al. found that men with more severe IPSS scores and larger prostate volumes consistently scored higher on the health-related quality of life (HRQOL), a validated questionnaire on an individual’s perceived physical and mental health.5 The QOL question has also been shown to highly correlate with the HRQOL, even more strongly than the total IPSS score.6
Furthermore, patient QOL is a significant predictor of treatment or decisional regret. Studies have shown that worse functional status, worse postoperative HRQOL scores, and unmet expectations regarding treatment outcomes are substantial predictors of decisional regret.7–9 In this sense, decisional regret represents a combination of patient satisfaction and quality of life, and its minimization is therefore key to the management of BPH and LUTS.
Decisional regret is a measure of distress or remorse after a healthcare decision, and is a complex, negative emotional reflection of a patient’s cognitive processes before and after a decision is made.10 In the case of surgical decision regret, this important metric is a function of continued LUTS leading to a lower QOL, especially if there is a disconnect between their surgical expectations and outcomes.
With patients becoming more involved in their healthcare, and providers increasingly utilizing shared decision-making, there has been reduced decisional conflict, more realistic expectations of outcomes, and improved feelings of support by the physician.11,12
With the increase in a myriad of surgical treatments for BPH, it is valuable to assess the degree of symptom change and decision regret to improve counseling on the risks and complications of these procedures and post-operative expectations. This manuscript aims to evaluate the decisional regret and IPSS-QOL change after surgical intervention for BPH.
This prospective, multi-center, longitudinal cohort study involved telephone interviews conducted by trained research staff members, which included administration of both the IPSS-QOL and Decision Regret Scale (DRS) questionnaires along with an assessment of reasons for decision regret. A retrospective chart review was performed to identify preoperative IPSS-QOL scores for comparison purposes. Patients who either did not complete the full telephone interview or lacked documented preoperative IPSS-QOL scores were excluded from the final results. Consistent with established literature, a DRS score of 25 or greater was considered indicative of high decisional regret.11,12
The study identified 54 male patients with a documented diagnosis of benign prostatic hyperplasia (BPH) who underwent BPH surgery between October 2020 and March 2023. All procedures were performed by experienced urologists at two participating institutions. As part of standard preoperative counseling, patients received comprehensive information about potential complications and the expected variability in symptom relief, which helped establish appropriate expectations and potentially reduce postoperative regret.
Patients were contacted for follow-up at least three months after their surgical procedures to ensure they were beyond the typical recovery period. The postoperative interval ranged from 98 to 922 days, with a mean follow-up time of 344 days (standard deviation ±180 days). The study included various BPH surgical approaches: transurethral resection of the prostate (TURP), Urolift, Greenlight Laser, Water Vapor Therapy (Rezum), and Aquablation.
All participants completed the IPSS-QOL questionnaire preoperatively. At least three months following their surgery, eligible patients received mailed study materials that included background information about the study informed consent documentation, and notification that they would receive a telephone call from the research team. Telephone interviews were conducted no earlier than two weeks after mailing the study materials. During these calls, research staff verified participants’ understanding of the study and obtained verbal informed consent, which had been approved by the respective institutional ethics committees. The telephone interviews consisted of both IPSS-QOL and DRS questionnaires. For patients who scored 25 or higher on the DRS, an additional follow-up call was made to specifically explore their reasons for procedural regret.
Preoperative data collection occurred from October 2020 through March 2023, while postoperative data was gathered from March 2023 to February 2024. All collected data underwent de-identification and aggregation before analysis. The study employed complete case analysis, meaning any participants with missing data points were excluded from the final dataset.
Data analysis was performed using Python version 3.12.3 with the Scipy library (version 1.14.1). Mann-Whitney U tests were used to examine differences among demographic groups, body mass index categories, medication use, and between minimally invasive procedures vs. TURP. Spearman’s rho correlation coefficients were calculated to assess relationships between changes in IPSS, quality of life measures, and IPSS-QOL scores with DRS scores.
The study protocol received approval from two institutional review boards. Study number 17887 was approved by the New York Medical College Institutional Review Board through the General Medical and Behavioral Panel on 24 February 2023. Study number 21-12024199 received approval from the Weill Cornell Medicine Institutional Review Board on 20 February 2023.
Demographic characteristics were similar between patients with and without significant regret (Table 1). The mean (SD) age of patients was 71 (9.02), and an average BMI (SD) of 27.3 (4.16). Our study population was largely healthy with no other significant comorbidities. At baseline, the mean IPSS score (SD) was 17.2 (8.2) and ranged from 0 to 34, with a mean QOL (SD) of 4 (1.6), ranging from 0 to 6. After the procedure, the mean IPSS score was 11 (8.2) ranging from 0 to 31, with a mean QOL (SD) of 2.5 (1.9) ranging from 0 to 6. The mean DRS score was 18.6 (23.7), ranging from 0 to 90. Interestingly, in our analysis of racial demographics, we observed a statistically significant difference in the proportion of self-identified White patients between the regret and no-regret groups (72 vs. 92%, p = 0.046).
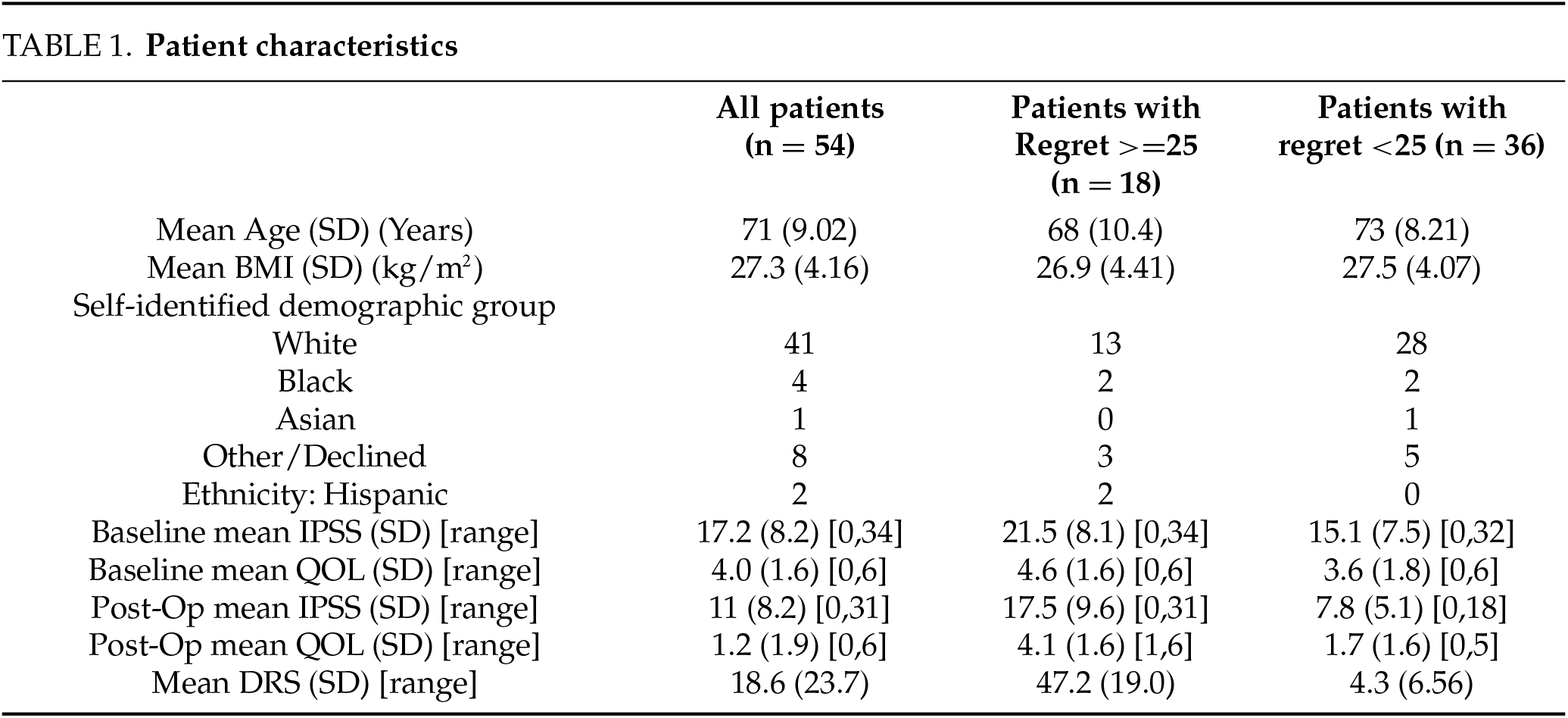
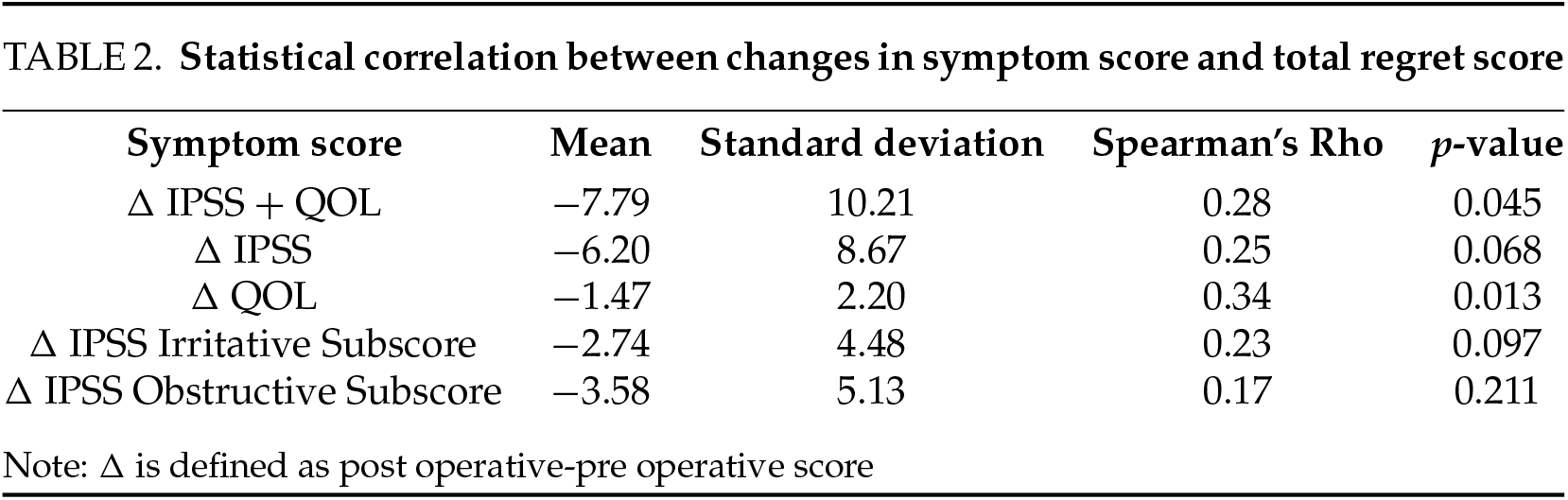
Significant relationships between patient regret and symptom changes were also observed. The mean change in QOL and IPSS-QOL were all seen to vary significantly by DRS with Spearman’s Rho coefficients of 0.28 (p = 0.045), and 0.34 (p = 0.013), respectively (Table 2). However, DRS was not seen to significantly vary with the IPSS score.
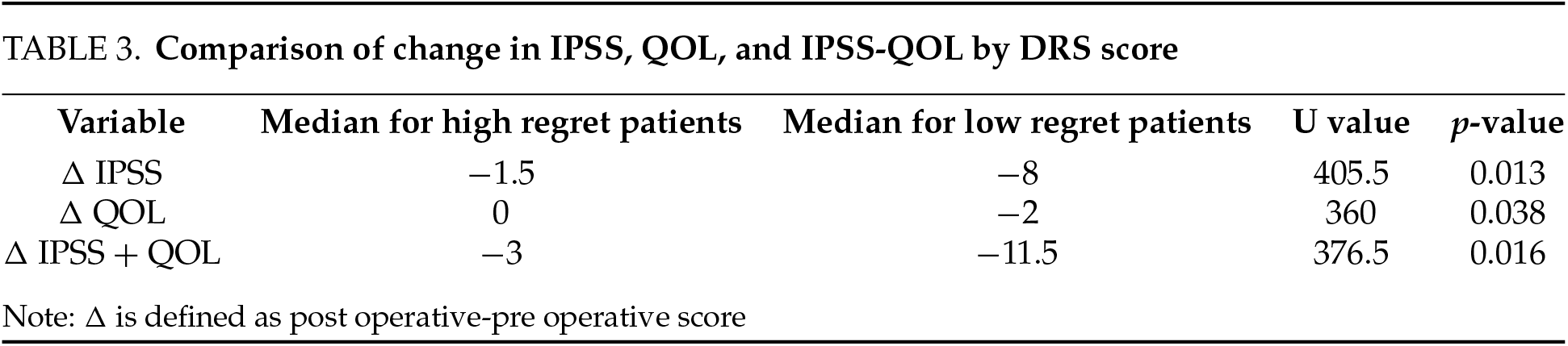
However, when stratified by low vs. high DRS score, we found more statistically significant changes (Table 3). There was a significant difference in the median change in IPSS for high-regret patients (−1.5) when compared to low-regret patients (−8) (p = 0.01). There was also a significant change in the median QOL score for high regret patients (0) vs. low regret patients (−2) (p = 0.04). The change in IPSS-QOL was also statistically significant, with a median of −3 for high regret and of −11.5 for low regret patients (p = 0.02).
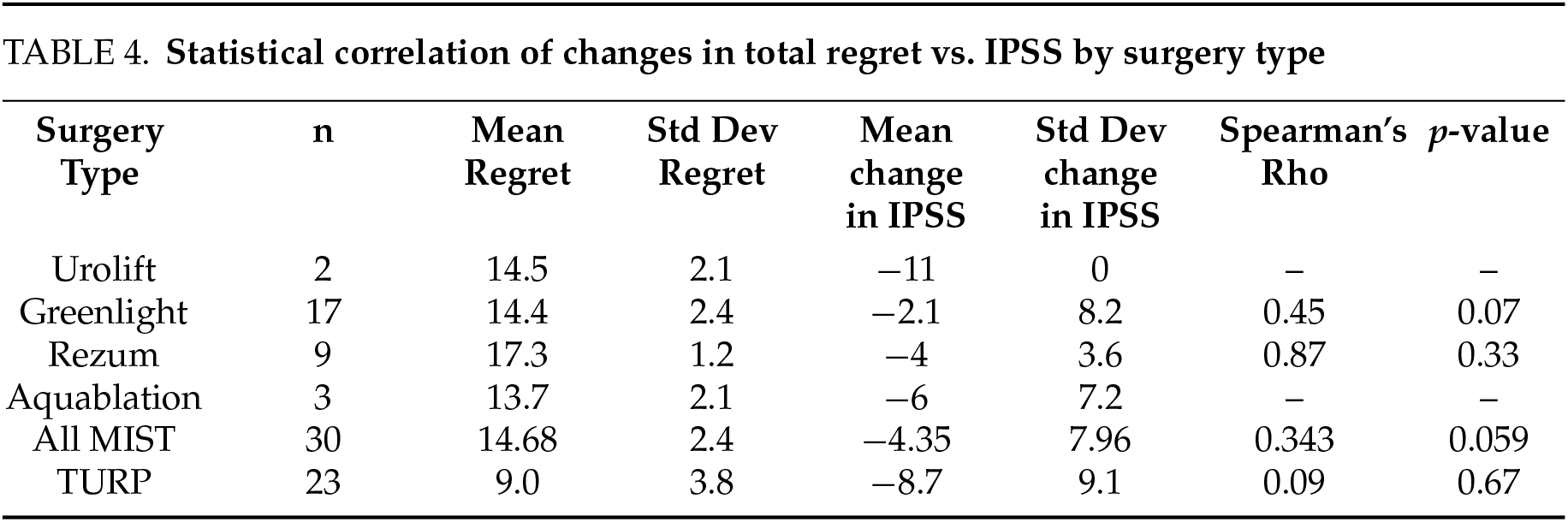
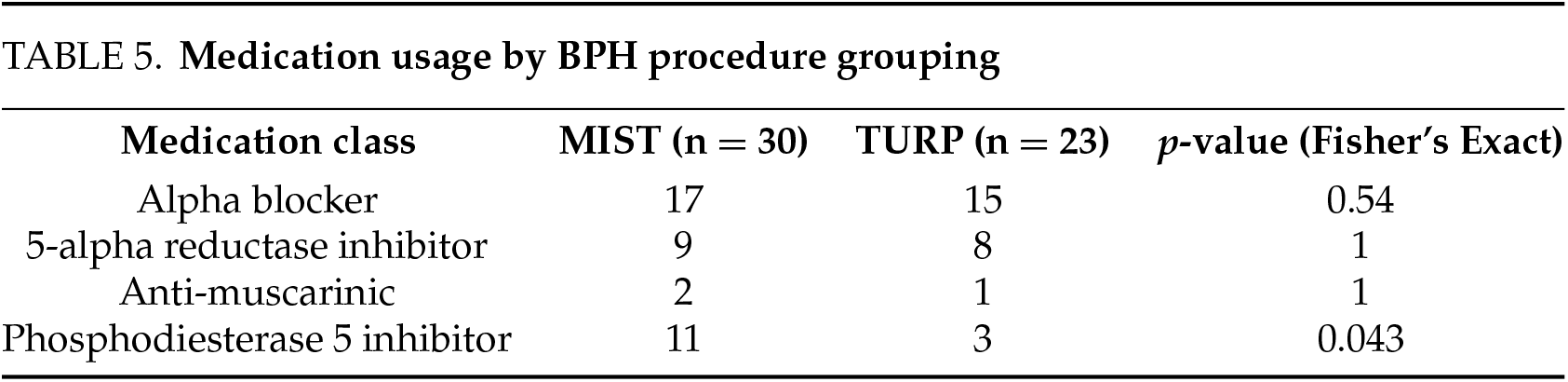
When we examined the average regret score vs. the mean change in IPSS by surgical type, a few trends emerged. There was a large variation of Spearman’s Rho amongst procedures, ranging from a minimum of 0.09 with TURP to a maximum of 0.87 with Rezum. Greenlight also had a relatively high Spearman’s Rho of 0.45. While not a significant correlation, MIST treatments combined had a higher Spearman’s Rho than TURP, with a coefficient of 0.343 (Table 4). Medication usage was broadly similar between MIST and TURP patients with no significant differences in the use of alpha-blockers (57% vs. 65%), 5-alpha reductase inhibitors (30% vs. 35%), or OAB medications (6.7% vs. 4.3%). However, PDE5 inhibitor use was significantly higher in the MIST group (36.7% vs. 13.0%, p = 0.043) (Table 5).
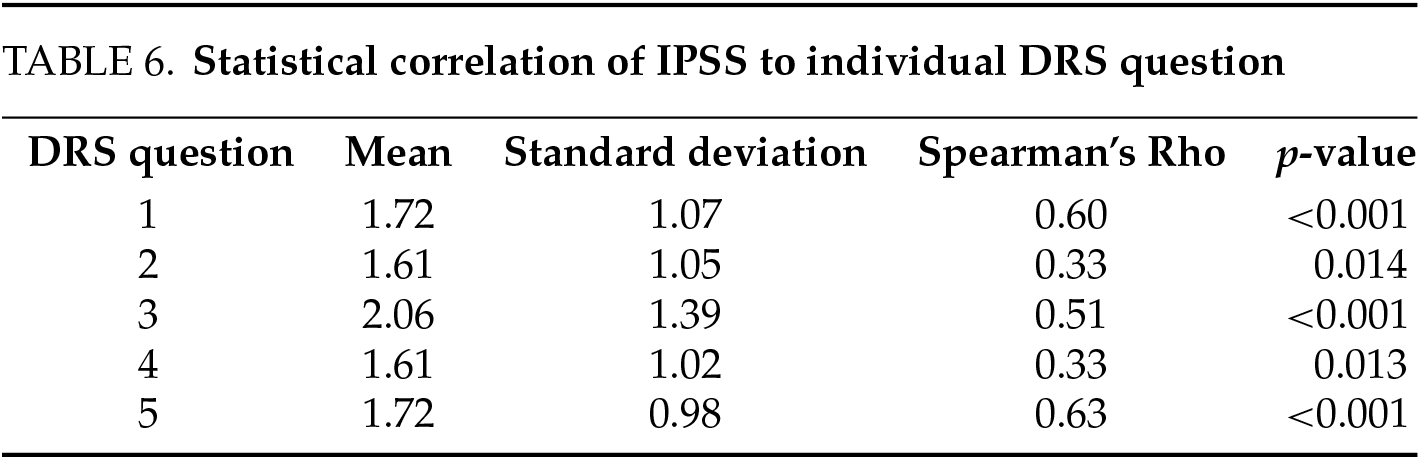
We also analyzed the relationship between each question of the DRS to the IPSS-QOL score. We found all questions had significant correlations, but that questions 1, 3, and 5 correlated most strongly, with Spearman’s Rho coefficients of 0.60, 0.51, and 0.63, respectively. Questions 2 and 4 had weaker but still statistically significant correlations with Spearman’s Rho values of 0.33 and 0.33, respectively (Table 6).
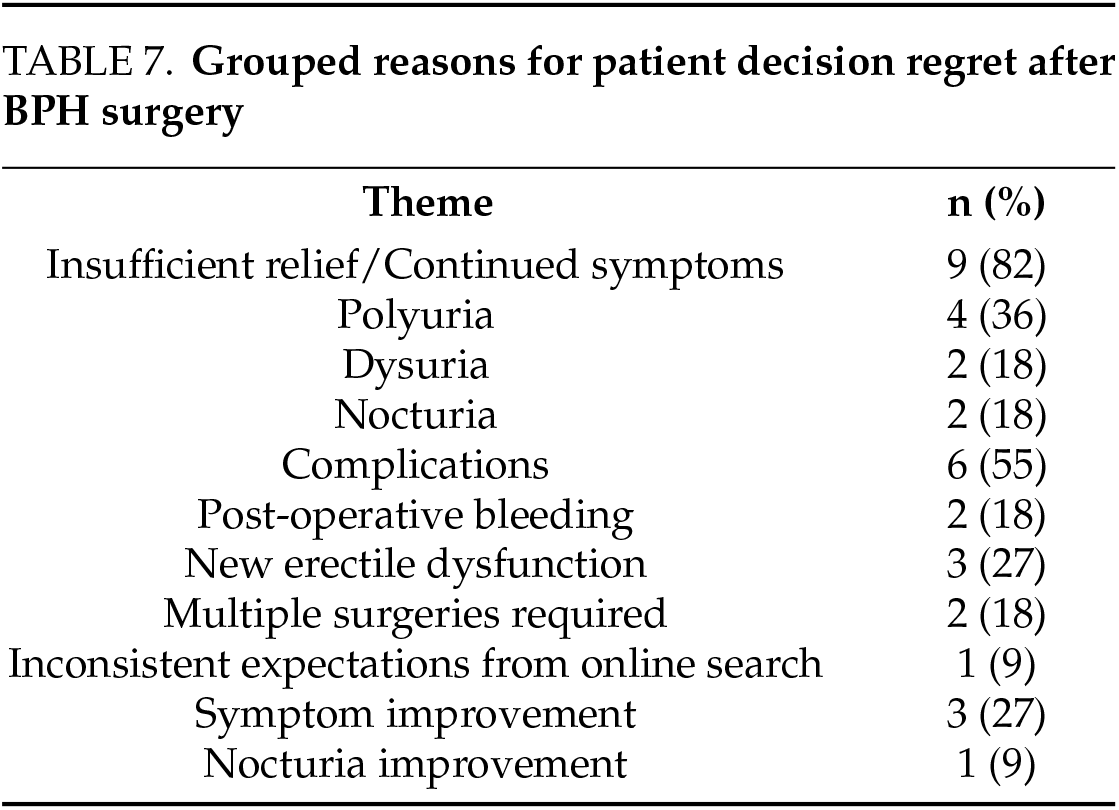
For patients who scored at least 25 on the DRS, we inquired and analyzed the motivations behind regret with follow-up phone calls. Of the 18 patients with significant regret, 11 agreed to talk about their motivations. These interviews were then coded based on recurring themes. The most common reasons for procedural regret were insufficient relief or continued symptoms after surgery (82%), most commonly polyuria (36%), dysuria (18%), and nocturia (18%). 55% of patients had regrets due to complications, including post-operative bleeding (18%), new erectile dysfunction (27%), or the need for multiple surgeries (18%). One patient noted having inconsistent expectations for symptom improvement due to their online searches. Within the regret group, 27% of patients noted some improvement in symptom relief, with one patient specifically mentioning nocturia. These findings highlight the importance of aligning patient expectations with likely outcomes through thorough preoperative counseling, particularly regarding the variability in symptom relief and the potential for post-operative complications.
In addition, we looked at the relationship between the DRS cutoff and the average characteristics of the groups above and below the cutoffs. We saw that the difference in the average of the change in IPSS varied from 1.19 to 6.06 for different values of the DRS. While typically a DR’s cutoff of 25 is used, we only found a difference of 3.31, whereas, for a cutoff of 30, we found a difference of 6.06.
This multicenter study aimed to investigate the relationship between the change in symptoms of BPH, measured by the IPSS-QOL, and postoperative decision regret, measured by the DRS, in patients undergoing various procedures for BPH treatment. Our findings highlight significant correlations between postoperative regret and changes in symptom scores, as well as highlight differences in the relationship between regret and patient symptoms in various BPH surgeries.
In this study, we found statistically significant linear correlations between the IPSS-QOL and QOL scores with DRS. The QOL score had the highest Spearman’s Rho of 0.34, indicating a moderate correlation between the quality of life and decisional regret. The significant correlation between the IPSS-QOL and the DRS suggests that both metrics have validity in the evaluation of BPH patients. This result is consistent with the literature, which has consistently demonstrated that the IPSS score correlates with surgical success in treating benign prostatic hyperplasia. Hackenberg et al. showed that IPSS is a reliable predictor of symptomatic improvement in TURPs.13 Pratsinis et al. found a strong correlation between IPSS changes and patient-reported outcomes such as goal achievement and treatment satisfaction with surgical BPH intervention.14 Perhaps more interestingly, when patients were stratified by regret, we found that patients with lower regret had significantly higher improvements in IPSS and QOL scores, solidifying a link between symptom scores and decisional regret. This is consistent with work done by Lavery et al., who highlighted that baseline urinary and erectile function are significant predictors of postoperative regret.8
The observed difference in the proportion of self-identified White patients between the regret and no-regret groups is notable. While our study did not specifically investigate the underlying reasons for this disparity, cultural, social, or healthcare access factors may influence decisional regret following BPH surgery. For instance, variations in patient expectations, communication with healthcare providers, or support systems across different demographic groups could contribute to differing experiences of regret.15 However, given the limitations of our sample size and the observational nature of our study, these interpretations should be approached with caution. Further research with more diverse and larger cohorts is necessary to explore decisional regret in this context.
We also analyzed decisional regret by the type of BPH surgery. Although sample sizes were limited for individual procedures, several trends emerged. MISTs, when analyzed collectively, showed a stronger correlation between symptom improvement and regret (Spearman’s rho = 0.343, p = 0.059) compared to TURP (rho = 0.09, p = 0.67). This suggests that regret in MISTs may be more tightly linked to the degree of symptomatic relief achieved. Moreover, patients who underwent MISTs reported higher average regret scores (mean 14.7 vs. 9.0 for TURP) and experienced less improvement in IPSS scores (mean ΔIPSS −4.35 vs. −8.7 for TURP).
These findings may reflect the fact that while MISTs are less invasive and often favored for their improved recovery profile, they may lack the same degree of durable symptom resolution as TURP, especially in patients with more advanced disease.16,17 The higher rate of PDE5 inhibitor use among MIST patients may reflect selection patterns favoring these procedures for individuals prioritizing preservation of sexual function, which may also influence expectations and satisfaction with outcomes. However, when MISTs do not achieve sufficient symptom relief, patients may be more likely to experience regret. In contrast, TURP showed greater average improvement in IPSS scores (ΔIPSS = −8.7 vs. −4.35 for MISTs) and lower mean regret (9.0 vs. 14.7), indicating more consistent efficacy in symptom control and a lower likelihood of postoperative regret.16
Thus, patient selection should be closely tailored to both clinical presentation and patient expectations. TURP may be more suitable for patients with higher symptom burden, larger prostate volume, or those seeking more definitive symptom relief, given its greater average improvement in IPSS and lower regret scores. This argument is in agreement with the literature, which found that TURP provides the largest improvement in urinary flow rate and urological symptoms, especially in short-term follow-up.16–18 In contrast, MISTs may be appropriate for patients with less severe symptoms, smaller prostates, or a strong preference for preserving ejaculatory function and minimizing perioperative risk. However, given the observed association between suboptimal symptom improvement and increased regret in MIST recipients, these patients would likely benefit from particularly thorough preoperative counseling to ensure alignment between their expectations and the potential outcomes of treatment.
When analyzing the IPSS score compared to each question of the DRS, we found that questions 1, 3, and 5 had the strongest positive correlations to the IPSS score (Table 6). These questions are all affirmations of the correct decision being made, whereas questions 2 and 4 focus on the harms and regret of a decision. These patients may have been thinking more about their symptoms during questions 1, 3, and 5 than for questions 2 and 4. Furthermore, this analysis underscores the importance of patients having a realistic understanding and expectations of surgical outcomes.
In the analysis of patient regret after surgery, the most common reasons were procedure inefficacy, postoperative complications, new symptoms after surgery, and the necessity of multiple surgeries (Table 7). This result suggests again the importance of setting clear expectations for surgical efficacy as well as fully elucidating the risks and complications of surgical procedures. Our findings are consistent with the literature on surgical regret, which has shown that the discordance between the patient’s preferred and actual outcomes as well as the patient’s perceived understanding of the procedure are major contributors to post-procedural regret.19–21
Traditionally, for the DRS, a cutoff of 25 is used to separate low from high regret.22,23 However, our analysis suggests that 30 may be a superior cutoff for BPH operations, as there was a higher change in the change in IPSS score between the two groups. The maxima at 30 suggests it would be an appropriate threshold for the most powerful dichotomization between a higher and lower regret group. Thus, this threshold may be considered when assessing regret in BPH procedures.
This study has several limitations. First, it relies on self-reported outcomes using the International Prostate Symptom Score (IPSS) and Decision Regret Scale (DRS), which, while validated, are inherently subjective and may be influenced by recall bias and patient interpretation. Preoperative scores were collected during in-person clinical visits, while postoperative scores were obtained via telephone interviews, introducing potential variability in data collection methods. Additionally, the same individual did not consistently administer both pre- and post-operative assessments.
Our analysis was also limited by a lack of urinary flow rates, prostate volume, surgical complication rates, comorbidity indices, or surgeon experience. Furthermore, while our sample size is moderate overall, it becomes limited when broken down by individual procedures, which may reduce the power to detect differences in regret or symptom change across surgical types. The lack of long-term follow-up also limits our ability to assess the durability of symptom control or delayed regret. Finally, we acknowledge that differences in racial composition between regret groups reached statistical significance, but the overall sample size of underrepresented minorities was small and limited meaningful subgroup analysis. These factors underscore the need for future studies with larger, more diverse cohorts and comprehensive clinical data to better define the drivers of decisional regret after BPH surgery.
Surgical treatment for BPH generally leads to improvement in symptoms, but a significant subset of patients experiences decisional regret, particularly in cases of perceived procedure inefficacy or postoperative complications. This is consistent with the observed correlation between increased symptomatic improvement and decreased procedural regret. As patients continually become more involved in their healthcare, shared decision-making, setting of clear expectations, and thorough discussion of potential side effects and complications must be emphasized for any BPH surgery.
Acknowledgement
None.
Funding Statement
The authors received no specific funding for this study.
Author Contributions
Study conception and design; Joshua Winograd, Rebecca Kindler, Alia Codelia-Anjum, Cassidy Lleras, Daniel Ufearo; Data collection; Joshua Winograd, Rebecca Kindler, Alia Codelia-Anjum, Michael A. Diefenbach: Analysis and interpretation of results; Joshua Winograd, Rebecca Kindler, Katharine Kechejian: Draft manuscript preparation; Bilal Chughtai, Dean Elterman, Naeem Bhojani, Siri Drangsholt: Manuscript review and editing; Bilal Chughtai, Dean Elterman, Naeem Bhojani, Michael A. Diefenbach: Clinical insight and supervision. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
The data that support the findings of this study are available from the corresponding author, Bilal Chughtai, upon reasonable request.
Ethics Approval
This study involves human subjects. Study #17887 was approved by the New York Medical College Institutional Review Board by the General Medical and Behavioral Panel on 24 February 2023. Similarly, study #21-12024199 was approved by Weill Cornell Medicine Institutional Review Board on 20 February 2023. Understanding was confirmed of the study and verbal informed consent was obtained with the approval of the respective ethics committees at the institutions conducting them.
Conflicts of Interest
Bilal Chughtai is a consultant for Olympus, Boston Scientific, Femselect, ARMs, Prodeon Medical, Sumitomo, Zenflow, and Teleflex. He is an advisor for Promaxo, Bright Uro, COSM, and Soundable. Dean Elterman is a consultant for Olympus, Boston Scientific, and Procept BioRobotics. Naeem Bhojani is a consultant for Olympus, Boston Scientific, and Procept BioRobotics. The other authors declare no conflicts of interest to report regarding the present study.
References
1. Sandhu JS, Bixler BR, Dahm P et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia (BPHAUA guideline amendment 2023. J Urol 2024;211(1):11–19. doi:10.1097/JU.0000000000003698. [Google Scholar] [PubMed] [CrossRef]
2. Egan KB. The epidemiology of benign prostatic hyperplasia associated with lower urinary tract symptoms: prevalence and incident rates. Urol Clin North Am 2016;43(3):289–297. doi:10.1016/j.ucl.2016.04.001. [Google Scholar] [PubMed] [CrossRef]
3. Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)—incidence, management, and prevention. Eur Urol 2006;50(5):969–979. doi:10.1016/j.eururo.2005.12.042. [Google Scholar] [PubMed] [CrossRef]
4. Teo JS, Lee YM, Ho HSS. An update on transurethral surgery for benign prostatic obstruction. Asian J Urol 2017;4(3):195–198. doi:10.1016/j.ajur.2017.06.006. [Google Scholar] [PubMed] [CrossRef]
5. Girman CJ, Jacobsen SJ, Rhodes T, Guess HA, Roberts RO, Lieber MM. Association of health-related quality of life and benign prostatic enlargement. Eur Urol 1999;35(4):277–284. doi:10.1159/000019861. [Google Scholar] [PubMed] [CrossRef]
6. Hopland-Nechita FV, Andersen JR, Beisland C. IPSS bother question score predicts health-related quality of life better than total IPSS score. World J Urol 2022;40(3):765–772. doi:10.1007/s00345-021-03911-2. [Google Scholar] [PubMed] [CrossRef]
7. Davison BJ, So AI, Goldenberg SL. Quality of life, sexual function and decisional regret at 1 year after surgical treatment for localized prostate cancer. BJU Int 2007;100(4):780–785. doi:10.1111/j.1464-410X.2007.07043.x. [Google Scholar] [PubMed] [CrossRef]
8. Lavery HJ, Levinson AW, Hobbs AR et al. Baseline functional status may predict decisional regret following robotic prostatectomy. J Urol 2012;188(6):2213–2218. doi:10.1016/j.juro.2012.08.016. [Google Scholar] [PubMed] [CrossRef]
9. Wollersheim BM, van Stam MA, Bosch RJLH et al. Unmet expectations in prostate cancer patients and their association with decision regret. J Cancer Surviv 2020;14(5):731–738. doi:10.1007/s11764-020-00888-6. [Google Scholar] [PubMed] [CrossRef]
10. Brehaut JC, O’Connor AM, Wood TJ et al. Validation of a decision regret scale. Med Decis Making 2003;23(4):281–292. doi:10.1177/0272989X03256005. [Google Scholar] [PubMed] [CrossRef]
11. O’Connor AM, Drake ER, Fiset V, Graham ID, Laupacis A, Tugwell P. The Ottawa patient decision aids. Eff Clin Pract 1999;2(4):163–170. [Google Scholar] [PubMed]
12. O’Connor AM, Rostom A, Fiset V et al. Decision aids for patients facing health treatment or screening decisions: systematic review. BMJ 1999;319(7212):731–734. doi:10.1136/bmj.319.7212.731. [Google Scholar] [PubMed] [CrossRef]
13. Hakenberg OW, Pinnock CB, Marshall VR. Does evaluation with the International Prostate Symptom Score predict the outcome of transurethral resection of the prostate? J Urol 1997;158(1):94–99. doi:10.1097/00005392-199707000-00025. [Google Scholar] [PubMed] [CrossRef]
14. Pratsinis M, Müllhaupt G, Güsewell S et al. Comparison of traditional outcome measures and self-assessed goal achievement in patients treated surgically for benign prostatic hyperplasia. World J Urol 2023;41(4):1125–1131. doi:10.1007/s00345-023-04317-y. [Google Scholar] [PubMed] [CrossRef]
15. Antoine SG, Carmichael H, Lloyd GL. The impact of race, ethnicity and insurance status on surgery rates for benign prostatic hyperplasia. Urology 2022;163:44–49. doi:10.1016/j.urology.2021.05.092. [Google Scholar] [PubMed] [CrossRef]
16. Cornu JN, Zantek P, Burtt G et al. Minimally invasive treatments for benign prostatic obstruction: a systematic review and network meta-analysis. Eur Urol 2023;83(6):534–547. doi:10.1016/j.eururo.2023.02.028. [Google Scholar] [PubMed] [CrossRef]
17. Franco JVA, Jung JH, Imamura M et al. Minimally invasive treatments for benign prostatic hyperplasia: a Cochrane network meta-analysis. BJU Int 2022;130(2):142–156. doi:10.1111/bju.15653. [Google Scholar] [PubMed] [CrossRef]
18. Tanneru K, Jazayeri SB, Alam MU et al. An indirect comparison of newer minimally invasive treatments for benign prostatic hyperplasia: a network meta-analysis model. J Endourol 2021;35(4):409–416. doi:10.1089/end.2020.0739. [Google Scholar] [PubMed] [CrossRef]
19. Wilson A, Winner M, Yahanda A, Andreatos N, Ronnekleiv-Kelly S, Pawlik TM. Factors associated with decisional regret among patients undergoing major thoracic and abdominal operations. Surgery 2017;161(4):1058–1066. doi:10.1016/j.surg.2016.10.028. [Google Scholar] [PubMed] [CrossRef]
20. Kinoshita H, Nishigori T, Nakabe T et al. Factors associated with postoperative decisional regret in patients undergoing gastrointestinal cancer surgery: a prospective cohort study. Am Surg 2023;89(12):6070–6077. doi:10.1177/00031348231184197. [Google Scholar] [PubMed] [CrossRef]
21. Janes LA, Lussiez AD, Anderson M, Bamdad MC, Suwanabol PA. Decisional regret among patients undergoing colectomy. Dis Colon Rectum 2022;65(12):1542–1549. doi:10.1097/DCR.0000000000002375. [Google Scholar] [PubMed] [CrossRef]
22. Lipstein EA, Lovell DJ, Denson LA et al. High levels of decisional conflict and decision regret when making decisions about biologics. J Pediatr Gastroenterol Nutr 2016;63(6):e176–e181. doi:10.1097/MPG.0000000000001425. [Google Scholar] [PubMed] [CrossRef]
23. Sheehan J, Sherman KA, Lam T, Boyages J. Association of information satisfaction, psychological distress and monitoring coping style with post-decision regret following breast reconstruction. Psychooncology 2007;16(4):342–351. doi:10.1002/pon.1067. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools