 Open Access
Open Access
ARTICLE
LEGENDS IN UROLOGY
Director,Watanabe Memorial Choumei Research Laboratory Honorary Professor, Kyoto Prefectural University of Medicine (Past-Chairman of Urology) and Meiji University of Integrative Medicine
Canadian Journal of Urology 2025, 32(3), 129-135. https://doi.org/10.32604/cju.2025.068161
Issue published 27 June 2025
Abstract
This article has no abstract.Development and application of Transrectal Ultrasound (TRUS)
Medical ultrasound, developed after World War II, emerged from the application of sonar technology originally used for submarine detection during the 1950s. In the early stages of this development, the concept of transrectal ultrasound (TRUS) was proposed. In 1955, Wild and Reid in the United States developed a basic transrectal scanner, but it could only display the rectal mucosa which lacked diagnostic value.
In 1964, Takahashi and Ouchi in Juntendo University in Tokyo obtained TRUS images by their own scanner, but the tomograms were not enough to recognize the organs.
I graduated from Tohoku University School of Medicine in Sendai, Japan, in 1960, and joined the Department of Urology in 1961 after completing a one-year internship. In the Department, there were several research groups, and in 1966, I was appointed as the leader of the Prostate Group.
At that time, the only diagnostic tool available for prostate examination was rectal palpation, and I was seeking a more precise method of diagnosis. The first idea I had was to use an electric stethoscope to listen to the sound of urine flowing through the urethra from the rectal cavity. I began searching for an expert in electric stethoscopes and found the right person at a research institute located near our hospital—Dr. Motonao Tanaka. Although he had graduated from our university just three years before me, he was already well-known as the world’s first developer of ultrasound cardiac tomography.
In Dr. Tanaka’s laboratory, I discovered a peculiar, stick-like probe he had recently developed for transesophageal ultrasonography. This probe was designed to obtain finer tomograms of the heart than conventional scanning methods that use the body surface. However, since the diameter of the probe was over 2 cm, it could barely be inserted into a dog’s esophagus and was impossible to use in humans. Dr. Tanaka was looking for alternative applications for this device. My initial idea of using an electric stethoscope was quickly abandoned, and we both eagerly agreed to explore the possibility of using the probe for transrectal ultrasound.
The next day, I persuaded one of my patients to undergo a new type of examination and brought him to Dr. Tanaka’s laboratory. The patient was positioned on the examination bed for cystoscopy, and the probe was carefully inserted into the rectum. The images we obtained at that time are shown in Figure 1. In the upper image, the urinary bladder with an inserted balloon and the seminal vesicles behind it are visible, while in the lower image, the prostate with some calculi inside is clearly shown. Without a doubt, this was the first time the prostate had been imaged in a living human body, occurring more than 10 years before the advent of CT. I was deeply impressed by this achievement, considering the potential for future advancements in the technique, which promised to greatly enhance both diagnosis and treatment of prostate diseases.
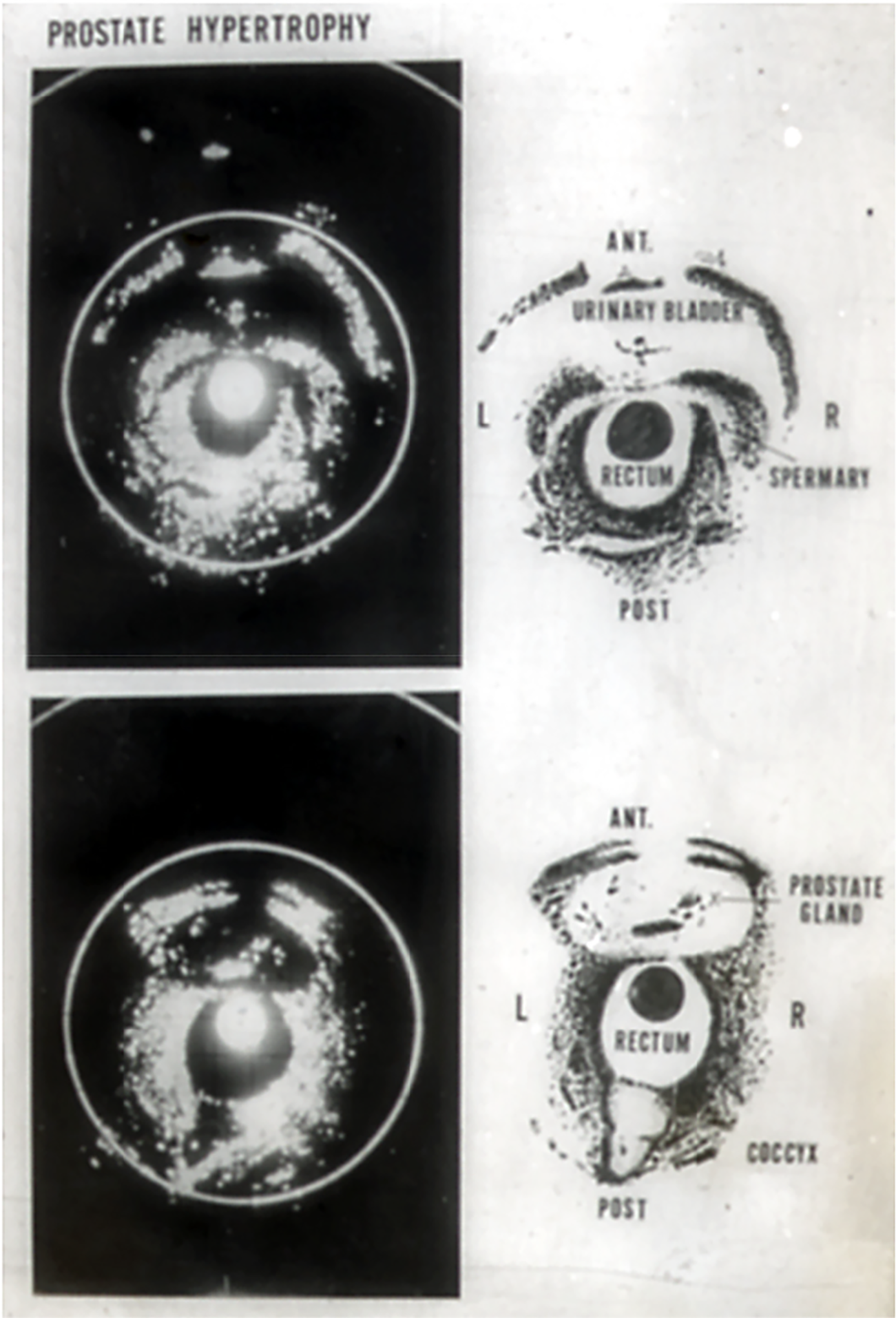
Figure 1: World’s first practical transrectal ultrasonotomogram of the urinary bladder with the seminal vesicles (upper) and the prostate (below) (Watanabe-Tanaka, 1967)
On the following day, I brought another patient for the examination, full of expectation and confidence. However, this time, only disappointing images were obtained, in stark contrast to the beautiful pictures from the previous day. The cause of this failure was later identified as water immersion into the oscillating disc. Despite this setback, I immediately ordered a new machine from the manufacturer, confident that with proper functioning, the equipment would produce the clear, high-quality images we had previously seen.
Soon after, we were able to consistently obtain fine tomograms of the prostate for every patient. However, the procedure was still cumbersome. The patient had to lie on a cystoscopy bed, and the long probe, originally designed for esophageal use, had to be mounted on a tall, unstable tripod. Preparing for the procedure alone took over half an hour. I knew I needed to find a more efficient method.
During this time, I happened to visit the famous Hakone open-air museum. There, I encountered a modern sculpture entitled “Magician’s Chair” (Figure 2) by Kiichi Sumikawa, a renowned artist who was later appointed President of the Tokyo University of the Arts. The sculpture featured a chair with a round protrusion from its seat, and as I observed it, I suddenly realized that my problem could be solved by developing a chair-type scanner, with the probe protruding from the seat.
Figure 2: A modern sculpture: Magician’s chair by Kiichi Sumikawa
Several months later, we completed a prototype of our chair-based scanner (Aloka, Mitaka City, Tokyo, Japan). The chair featured a control stick to adjust the angle of probe insertion, which we believed it was important at the time. To promote this new diagnostic procedure, we planned an advertisement film and invited a young professional model from Tokyo. This marked the first time the machine was used on a woman, and we were able to capture the world’s first ultrasound section of the uterus obtained via intracorporeal scanning. After the introduction of this new machine, the procedure became much more efficient, reducing the time needed for a patient to only 10 min.
Through experience with this apparatus, we realized that the insertion angle of the probe was not as critical for the diagnosis as we had initially thought. This led to the development of a simpler, more refined commercial machine in 1975, which was distributed worldwide. For early investigations on TRUS brought from the USA or Europe, this machine was commonly used. In 2005, we introduced electronic scanning into the machine, allowing for real-time display (Figure 3 New Chair, Figure 4 US).

Figure 3: Commercial chair-type scanner
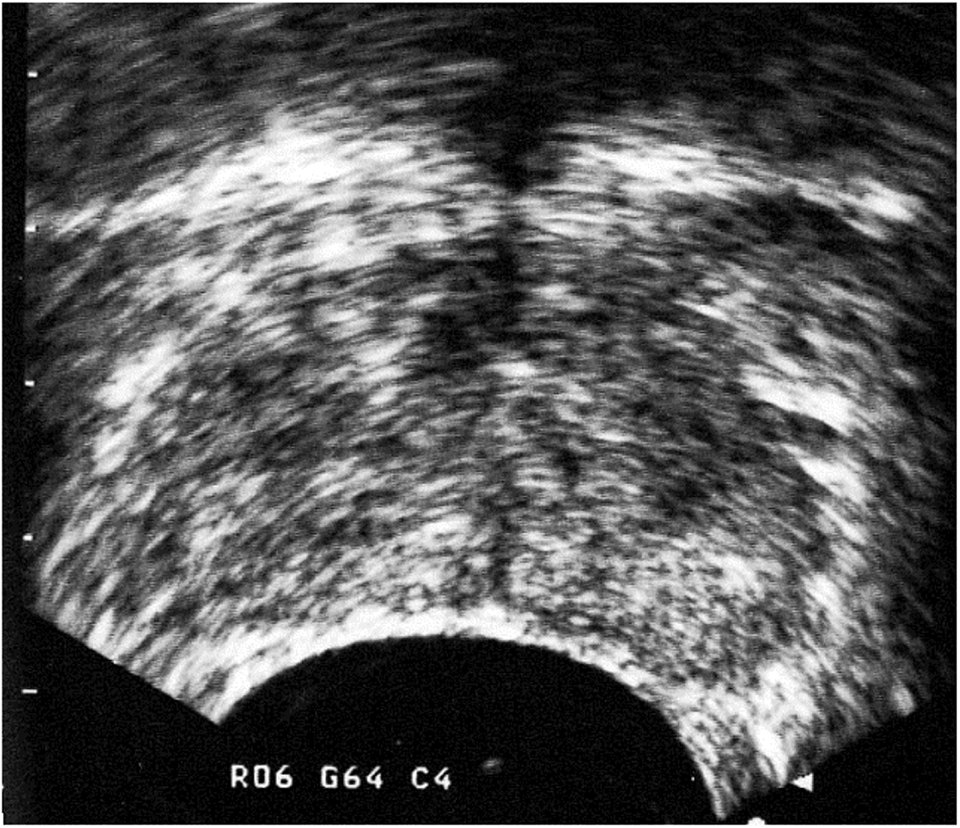
Figure 4: Tomogram of the prostate with very early prostatic cancer, taken by our commercial chair with electronic scanner. A hypoechoic legion was observed in the central part of the left (right on the picture) lobe
The first systematic investigation of TRUS in the U.S. began at Wake Forest University in Winston-Salem. Just two weeks after my publication in Investigative Urology 8:548, 1971, I received a phone call from Dr. King at Wake Forest. A week later, he visited our clinic at Tohoku University and stayed for several weeks to learn the procedure. He then purchased the same machine and began performing the examinations at Wake Forest’s clinic. Dr. King was succeeded by the well-known Dr. Martin I. Resnick, who later became the President of the American Urological Association (AUA). Unfortunately, Dr. Resnick passed away from leukemia in 2007.
I was invited to Wake Forest University in 1975 and subsequently gave lectures at several universities and hospitals across the U.S. during a month-long tour. However, the response I received was largely indifferent, or even negative. The skepticism was especially strong among some of the most prominent professors in the field. This is the thick wall that any pioneer must face. I encountered similar resistance many times, even in Japan.
One memorable experience occurred shortly after my brief lecture on TRUS at the annual meeting of the Japanese Urological Association (JUA). Following the lecture, a well-known professor—often referred to as the No. 1 urologist for prostate issues in Japan—approached the podium and said to me, ‘You, young man! No matter what new device you’ve invented, my finger is much better than that!’
In 1976, I moved to Kyoto Prefectural University of Medicine as the chair of the department. Around this time, the use of TRUS began to spread more widely in the U.S. In line with this trend, the “National Prostate Cancer Project” in Buffalo, established by the U.S. government, organized a special workshop on TRUS in 1985, inviting influential researchers from around the world. This workshop was specifically arranged by Dr. Gerald P. Murphy (1935–2000), a renowned urologist and the President of the project. However, during the workshop, Dr. Murphy was unexpectedly dismissed from the project for reasons unrelated to the event. This incident left a strong impression on me and remains vivid in my memory (Photo, Figure 5).

Figure 5: Attendants to the Workshop for TRUS by NPCP (Buffalo, 1985) Front row from the left: 3rd: Watanabe, 4th: Resnick, 5th: Lee. Rear row from the left: 4th: Pontes, 6th: Bartsch from Germany, 7th: Stamey, 8th: Rifkin. Dr. Murphy could not attend the meeting.
Around this time, the Danish company “Bruel & Kjær” (B&K) began extensively selling machines similar to ours, which made our “Aloka” machine less competitive in the U.S. market. However, the “Aloka” machine still had advantages in the European market.
Later, following the advancements at Wake Forest, Dr. Rifkin, one of the U.S. leaders in TRUS, began using a linear scanner from the Japanese company “Toshiba” and noted that prostate cancer showed a “hyper-echoic pattern” on the ultrasonogram. In contrast, Dr. Fred Lee, another key figure in TRUS, used a “B&K” machine and emphasized that prostate cancer appeared as a “hypo-echoic pattern.” His slogan, “Cancer is black,” became widely recognized during that period. Modern ultrasound machines show that early, small cancerous lesions in the prostate always appear hypoechoic (Figure 4). Dr. Rifkin may have been observing only more advanced cases, which tend to have stronger echo reflections.
A famous urologist, Prof. Thomas A. Stamey (1928–2015) from Stanford University, also attended the workshop in Buffalo. Afterward, he kindly invited me to stay for a few nights at his beautiful house in Palo Alto, where he shared fascinating stories about the field of urology in the U.S. I believe the workshop may have been quite a revelation for him, as it was his first time seeing visible sections of the prostate in such detail.
This workshop marked a turning point for the widespread adoption of TRUS in the U.S. Year by year, the method became a routine examination in many urology clinics across the country, and this trend gradually spread to Europe and, finally, to Japan. Today, it would be rare to find a urology clinic anywhere in the world that does not use TRUS.
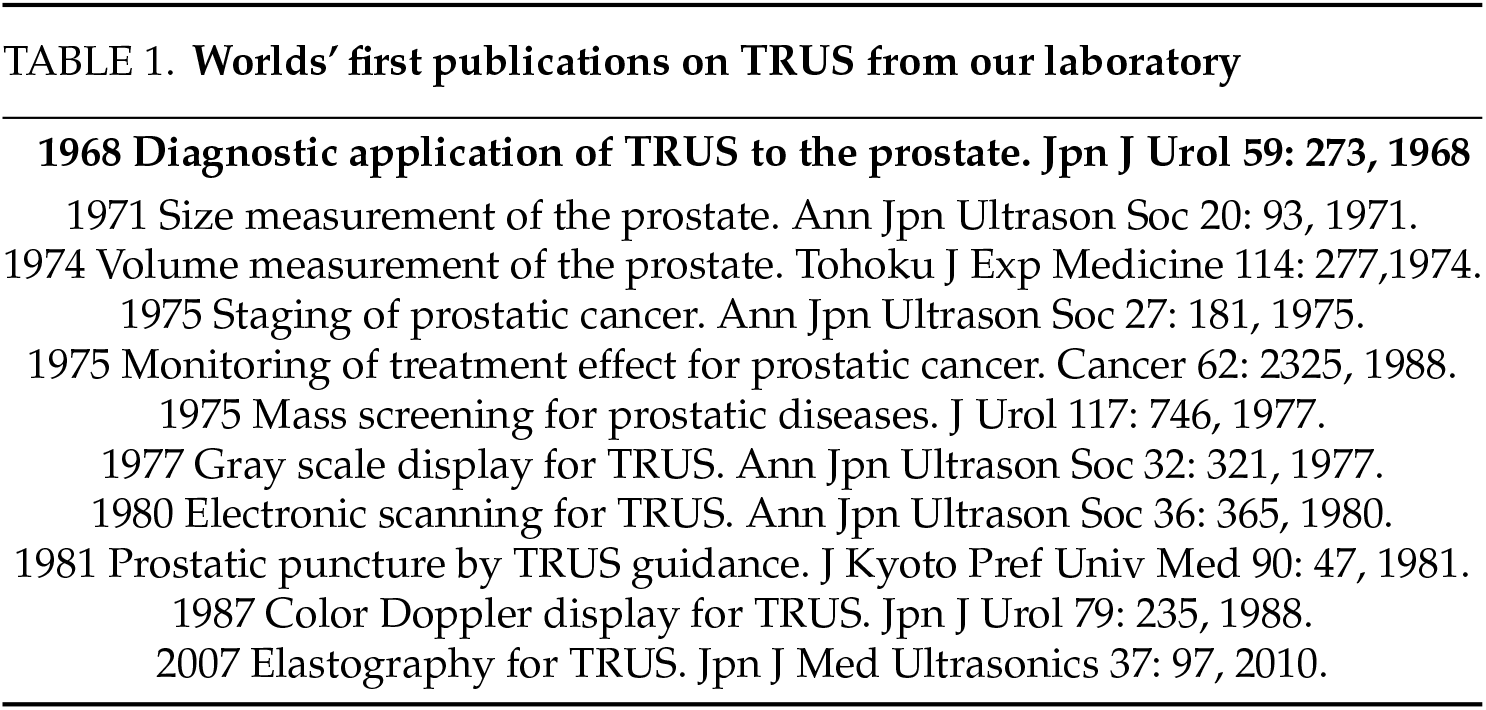
Since then, many studies applying TRUS have been published from our laboratory (Table 1). In recent years, various imaging techniques, such as color Doppler, power Doppler, and elastography, have been integrated into the method. Additionally, numerous endoscopic surgical techniques, using TRUS for guidance and monitoring, have rapidly developed.
In 2004, I moved to Meiji University of Integrative Medicine as Dean of the Third Department of Basic Medicine, Graduate School, and Director of the University Hospital. I became Honorary Professor in 2007. I also served as President of Kyoto Central Nursing School. In 2013, I became the Director of the Watanabi Choumei Research Laboratory. I am currently working for 3 days a week in a medical complex along famous Biwa Lake in an out-patient clinic and dialysis center, which was established by one of my former staff. He offered a small but comfortable research laboratory in the complex for me. The complex is an hour from my house in a small village located on a mountain near Kyoto where I live with my wife, Mizue. She is healthy and keeps our house running perfectly. My daughter, Fumiko, lives in the same village with her husband and works in Kyoto University.
My work brought me several honors of which I am very proud of:
1994–1995 President, Japan Society of Ultrasonics in Medicine (JSUM).
1998–2001 President, Asian Federation for Ultrasound (AFSUMB).
President, World Federation for Utrasound (WFUMB).
1975 Sakaguchi Prize (Japanese Urological Association; Contribution to the development of transrectal ultrasound).
2004 Asahi Cancer Award (“The Asahi Simbun”, Newspaper Publisher; Contribution to the development and advancement of prostate cancer screening).
2008 Special Prize of JSUM (Contribution to the investigation of ultrasound and the advancement of ultrasound medicine for the world).
2017 The Order of the Sacred Treasure, Gold Rays with Ribbon (By the Emperor).
Honorary Memberships in the Japanese Urological Association, American Urological Association, and Medical Ultrasound Societies in Japan, USA, France, Italy, Venezuela, India, Austaraliapacific, Poland, Chile and Taiwan.
TRUS remains a simple, accessible, safe, and cost-effective diagnostic tool for urology, and its further application is anticipated in the future. I have also heard that a set of my early transrectal ultrasound equipment is on display at the Smithsonian Institution in Washington, D.C., although I have not yet had the opportunity to see it in person.
Hiroki Watanabe, MD
Director, Watanabe Memorial Choumei Research Laboratory
Honorary Professor, Kyoto Prefectural University of Medicine (Past-Chairman of Urology) and Meiji University of Integrative Medicine
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools