 Open Access
Open Access
CASE REPORT
Ventral midline approach to penile fracture with bilateral corporal injuries and complete urethral avulsion: a case report
Department of Urology, Northwestern University Feinberg School of Medicine, 676 N. St. Clair Street, Arkes 23, Chicago, IL 60611, USA
* Corresponding Author: Conor B. Driscoll. Email:
Canadian Journal of Urology 2025, 32(4), 345-348. https://doi.org/10.32604/cju.2025.063323
Received 11 January 2025; Accepted 23 April 2025; Issue published 29 August 2025
Abstract
Penile fracture is a rare clinical entity that occurs secondary to direct trauma to an erect penis, most commonly during sexual intercourse. Specifically, increased pressure within the corpus cavernosa results in rupture of the tunica albuginea. Occasionally, these injuries extend to the urethra and very rarely cause a complete urethral avulsion. Emergent exploration improves post-traumatic erectile function, penile curvature, and prevents painful erections. The traditional approach is a subcoronal circumcising incision to allow for adequate visualization. We present an uncircumcised male with bilateral corporal injuries and complete urethral avulsion who underwent a ventral midline approach for successful foreskin preservation.Keywords
Penile fracture results from traumatic disruption of the tunica albuginea of the corpus cavernosum. It is a urologic emergency most commonly seen after injury during sexual intercourse.1 Reports estimate that 3–38% of penile fracture patients present with concomitant urethral injury,2 and there are very few cases in the literature of complete urethral avulsion occurring with a bilateral corporal injury.3,4 Management of penile fractures generally involves prompt surgical exploration to minimize the risk of long-term erectile dysfunction.5 The classic approach involves a subcoronal circumcising incision, complete degloving of the penile shaft, and primary repair of the tunical defect.5 However, this approach may be associated with postoperative wound complications given the extent of dissection, and may be more difficult for patients desiring foreskin preservation. Herein, we present a case of an uncircumcised male with bilateral corporal injuries and complete urethral avulsion who underwent penile exploration via a ventral midline approach to preserve the foreskin.
A 29-year-old man presented to the Emergency Department about 2 h after sustaining a penile injury during sexual intercourse. He had no known past medical history and had no pertinent family or psycho-social history. He reported direct contact with the end of his penis onto his partner’s pelvis, after which he experienced acute penile pain and immediate detumescence. He immediately noticed blood at his urethral meatus and was unable to urinate. On exam, his penis was uncircumcised, mildly diffusely tender and there were scattered ecchymoses most concentrated on the ventral and right lateral shaft with some ventral edema. Although Foley catheterization was attempted, there was significant resistance at the mid penile urethra.
The patient agreed to undergo surgical exploration of his penis, repair of penile fracture(s), and possible urethroplasty. He strongly desired foreskin preservation.
A preoperative retrograde urethrogram (RUG) was performed which demonstrated extravasation at the mid penile urethra (Figure 1a and b). Cystoscopic evaluation demonstrated a circumferential urethral avulsion at the level of the mid-penile urethra.
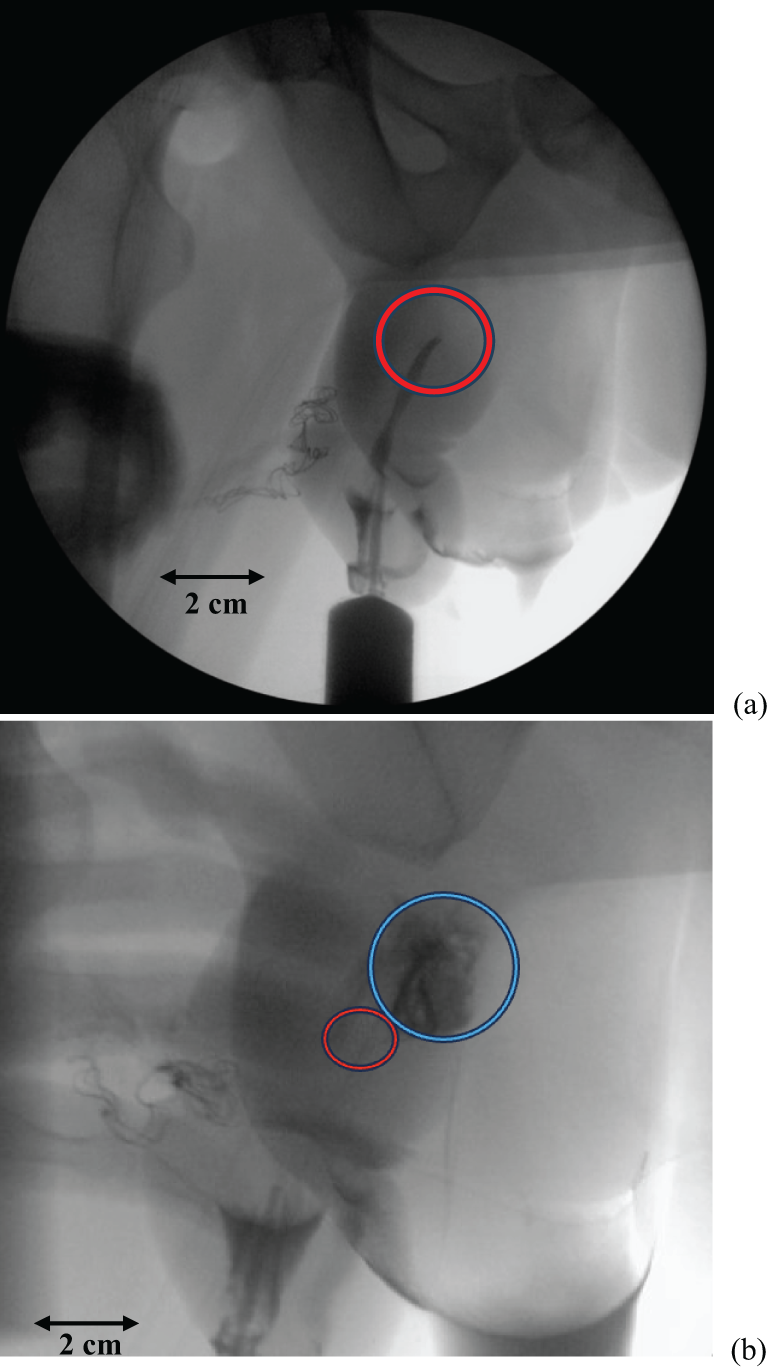
Figure 1: (a) Intra-operative retrograde urethrogram demonstrating an abrupt cutoff to contrast passage in the mid-penile urethra (red circle). (b) Intra-operative retrograde urethrogram demonstrating extravasation of contrast at the mid-penile urethra (blue circle) just proximal to the abrupt cutoff of contrast passage from Figure 1a (red circle)
Intraoperatively, we made a ventral incision along the penile shaft. This provided us with adequate exposure to the injuries. We noted bilateral corporal body injuries with a completely transected penile urethra (Figure 2). The bilateral corporotomies were closed with 3-0 Maxon. Our anastomoses were confirmed to be watertight after injecting normal saline into the corporal bodies. During urethroplasty, care was taken to perform urethrolysis proximally towards the bulbar urethra rather than distally to decrease the risk of postoperative penile curvature. After mobilizing the proximal urethra, we were able to debride the necrotic portions of the proximal and distal urethral segments and perform an excision and primary anastomosis reconstruction using interrupted 5-0 polydioxanone sutures.
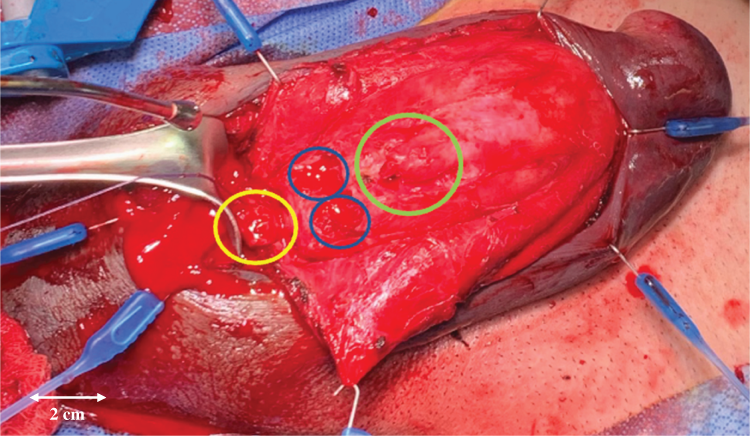
Figure 2: Ventral midline incision with bilateral corporal cavernosa injuries (blue) and complete urethral avulsion with 3 cm gap between distal urethra (green) and proximal urethra (yellow)
Postoperative RUG was performed at 4 weeks post-operatively demonstrated no extravasation, and the Foley catheter was removed (Figure 3).

Figure 3: Office peri-catheter RUG performed at 4 weeks post-operatively demonstrating a healed urethra without extravasation or stricture
On follow-up at 24 months, the patient has noted good erectile function and no evidence of any penile curvature or obstructive urinary symptoms. Additionally, surveillance cystoscopy at 9 months postoperatively demonstrated a healed urethra without evidence of stricture recurrence (Figure 4).
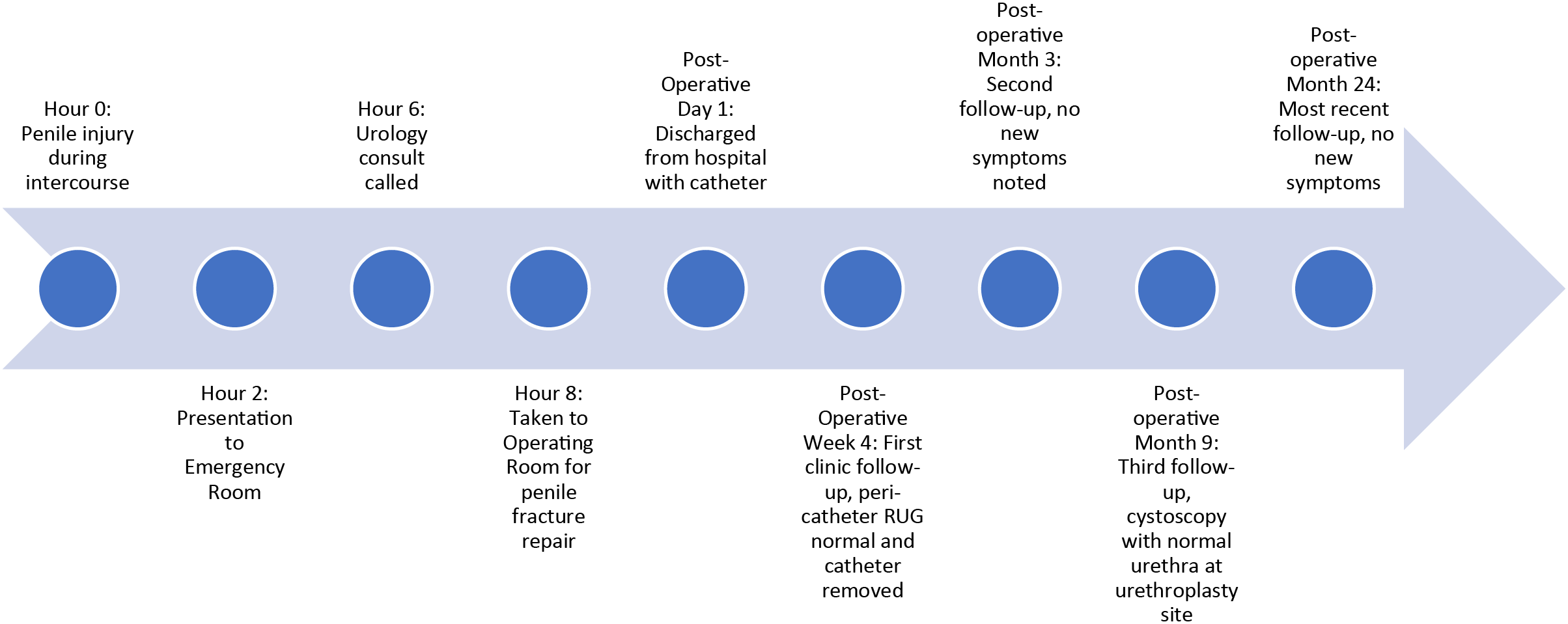
Figure 4: Timeline of clinical care
Penile fracture, defined as traumatic disruption of the tunica albuginea and corpus cavernosum commonly occurs when an erect penis has direct contact with the partner’s pubic symphysis and is a rare clinical entity. It is even rarer for this injury to affect the urethra and yet rarer for the urethral injury to be a complete transection of the urethra, with only 22 cases of complete urethral transection reported as of 2015 and a very small number reported since then.4,6,7 The management of these injuries is emergent surgery, with the best outcomes regarding erectile dysfunction, penile curvature, and painful erection being reported in those patients who receive surgery in less than 12 h from the time of injury.8,9 The classically described incision for this surgery is a subcoronal circumcising incision and penile degloving to the penoscrotal junction. This approach is preferable in circumcised patients or those who consent to circumcision at the time of surgical repair, as it may be difficult to preserve blood flow to the foreskin in a traumatic setting.1 Mazaris et al. (2009) described a case series of 8 patients in Greece from 2002–2006 that underwent penile fracture repairs via a ventral midline incision without immediate or long-term sequelae, providing proof of concept.4 Only one of those patients had a bilateral corporal rupture with concomitant penile urethral avulsion, making our case the second documented case of this approach for a bilateral corporal injury with urethral avulsion. Their manuscript is unclear on the circumcision status of the patient, and they indicate that they performed it for ease of exploration of the base of the corpora. Thus, this case report highlights the utility of a ventral midline approach in an uncircumcised patient desiring to keep his foreskin.
It is notable that this patient presented early enough after his injury that the “eggplant” deformity had not yet formed, but then developed by the time he was taken to the Operating Room. This patient was very invested in maintaining his foreskin, and as such, a ventral midline approach was utilized with success. This approach offered certain advantages over the traditional circumcising approach. With the ventral midline incision, we had immediate clear visualization of all three concomitant injuries, which allowed for expedient confirmation of the extent of the injuries and significantly reduced the operative time. This is important because most penile fractures occur at the base of the corpora, which can be directly accessed via a ventral midline incision but is harder to access with a circumcising incision.4 Furthermore, in cases such as this with a urethral injury, the ventral midline incision allows direct access to the penile urethra for identification and repair. Avoiding circumferential degloving also minimized the dissection of Buck’s fascia and foreskin devascularization, which allowed the patient to maintain his foreskin. At his 4-week post-operative visit, he reported satisfactory erectile function and in-office RUG demonstrated a patent urethra without stenosis or stricture. His surveillance cystoscopy at 9 months demonstrated a normal, healed urethra, and he reported no new urinary symptoms, penile curvature, or erectile dysfunction at his most recent follow-up at 24 months postoperatively.
Our patient here, as well as the single patient described by Mazaris et al., represents the only two cases in the literature to describe a ventral midline surgical approach to a bilateral corporal fracture with urethral avulsion.4 Ours is the first to describe this approach as a means of foreskin preservation per patient request and has good clinical outcomes 2 years post-operatively, which suggests a similar success rate to the traditional circumcising approach. As such, we believe that this surgical approach is useful for uncircumcised patients who suffer a penile fracture and wish to preserve their foreskin. Given that this is a single case report, larger studies with prospective data are necessary to provide additional evidence for this surgical approach.
Abbreviation
| RUG | Retrograde urethrogram |
Acknowledgement
Not applicable.
Funding Statement
Not applicable.
Author Contributions
Conor B. Driscoll: Conceptualization, Methodology, Validation, Formal Analysis, Investigation, Data Curation, Writing—Original Draft, Writing—Review & Editing; Nicole Handa: Investigation, Data Curation, Writing—Review & Editing; Daniel R. Greenberg: Investigation, Data Curation, Writing—Review & Editing; Ziho Lee: Conceptualization, Supervision, Project Administration, Methodology, Validation, Resources, Supervision. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
The patient data in this case report is HIPAA protected and, as such, will not be available unless a written proposal is submitted to the senior author (ziho.lee@nm.org) and the requestor obtains written consent from the patient to access his chart.
Ethics Approval
Northwestern Medicine Institutional Review Board does not require ethical approval for reporting an individual case report that only documents the observations of a patient receiving medical care because there is no intent to test a hypothesis via a systematic data analysis.
Conflicts of Interest
The authors declare no conflicts of interest to report regarding the present study.
References
1. Eke N. Fracture of the penis. Br J Surg 2002;89(5):555–565. doi:10.1046/j.1365-2168.2002.02075.x. [Google Scholar] [PubMed] [CrossRef]
2. Barros R, Ribeiro JGA, da Silva HAM, de Sá FR, Júnior Fosse AM, Favorito LA. Urethral injury in penile fracture: a narrative review. Int Braz J Urol 2020;46(2):152–157. doi:10.1590/S1677-5538.IBJU.2020.99.02. [Google Scholar] [PubMed] [CrossRef]
3. Vagnoni V, Dababneh H, Schiavina R, et al. Sex-related penile fracture with complete urethral rupture: a case report and review of the literature. Arch Ital Urol Androl 2015;87(3):260–261. doi:10.4081/aiua.2015.3.260. [Google Scholar] [PubMed] [CrossRef]
4. Mazaris EM, Livadas K, Chalikopoulos D, Bisas A, Deliveliotis C, Skolarikos A. Penile fractures: immediate surgical approach with a midline ventral incision. BJU Int 2009;104(4):520–523. doi:10.1111/j.1464-410X.2009.08455.x. [Google Scholar] [PubMed] [CrossRef]
5. Zargooshi J. Penile fracture in Kermanshah, Iran: the long-term results of surgical treatment. BJU Int 2002;89(9):890–894. doi:10.1046/j.1464-410x.2002.02745.x. [Google Scholar] [PubMed] [CrossRef]
6. Hanna KF, Jiang J, Burns N, Engelsgjerd JS, Davies JD. A case of traumatic penile fracture with simultaneous rupture of both corpora cavernosa and complete urethral transection. Urol Case Rep 2020;34:101439. doi:10.1016/j.eucr.2020.101439. [Google Scholar] [PubMed] [CrossRef]
7. Mathew J, Parmar K, Chandna A, Kumar S. Penile fracture associated with complete urethra and bilateral corpora cavernosa transection. Ann R Coll Surg Engl 2021;103(3):e88–e90. doi:10.1308/rcsann.2020.7042. [Google Scholar] [PubMed] [CrossRef]
8. Amer T, Wilson R, Chlosta P, et al. Penile fracture: a meta-analysis. Urol Int 2016;96(3):315–329. doi:10.1159/000444884. [Google Scholar] [PubMed] [CrossRef]
9. Ibrahiem EHI, El-Tholoth HS, Mohsen T, Hekal IA, El-Assmy A. Penile fracture: long-term outcome of immediate surgical intervention. Urology 2010;75(1):108–111. doi:10.1016/j.urology.2009.08.057. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools