 Open Access
Open Access
REVIEW
Is the Barthel index a valid tool for patient selection before urological surgery? A systematic review
1 Department of Urology, “Vito Fazzi” Hospital, Lecce, 73100, Italy
2 Department of Radiology, Cittadella della Salute, Azienda Sanitaria Locale di Lecce, Lecce, 73100, Italy
3 Research Unit of Radiology, Department of Medicine and Surgery, Università Campus Biomedico di Roma, Roma, 00128, Italy
4 Department of Urology, Hospital of Bolzano (SABES-ASDAA), Bolzano, 39100, Italy
5 Department of Urology, University of Verona, Azienda Ospedaliera Universitaria Integrata di Verona, Verona, 37126, Italy
6 Dott. Alessandro Tafuri Medical Center, Lecce, 73100, Italy
* Corresponding Author: Alessandro Tafuri. Email:
Canadian Journal of Urology 2025, 32(5), 375-384. https://doi.org/10.32604/cju.2025.066140
Received 31 March 2025; Accepted 25 July 2025; Issue published 30 October 2025
Abstract
Background: The Barthel Index (BI) measures the level of patient independence in activities of daily living. This review aims to summarize current evidence on the use of the BI in urology, highlighting its potential as a tool for assessing patients prior to surgery. Materials and methods: A comprehensive search of PubMed, Scopus, and Web of Science databases was conducted for studies evaluating the BI in patients undergoing urologic surgery, following Systematic Review and Meta-analyses (PRISMA) guidelines. The BI was investigated both as a descriptor of baseline or postoperative health status and a prognostic indicator. A qualitative data synthesis was provided. Results: Overall, nine studies were included (three retrospective, six prospective). Surgical contexts included radical cystectomy (RC) in three studies, kidney transplantation in two, trans-urethral resection/vaporization of the prostate (TURP/TUVRP) in two, with the remainder including several different urological procedures for both oncological and non-oncological diseases. Evidence suggested that the BI reliably reflects functional status pre- and post-operatively, independently predicts major postoperative complications, prolonged hospital stay, higher healthcare costs, and poorer oncologic outcomes in RC patients. Additionally, the BI was associated with postoperative delirium in patients undergoing TURP and predicted the risk of deep vein thrombosis in patients undergoing major urological surgical procedures. Conclusion: The BI is a valid tool for evaluating functional reserve in urologic patients. Its preoperative application can help identify patients at higher risk of adverse outcomes, thereby facilitating personalized treatment planning and optimizing surgical care.Keywords
With the increasing life expectancy of the general population, a growing number of elderly individuals are expected to undergo surgery.1 However, chronological age alone is not always a reliable indicator of a patient’s overall health status, and a thorough assessment should also consider comorbidities, performance status, functional capacity, and cognitive function.2 These aspects are encompassed by the concept of frailty—a multifactorial syndrome characterized by an age-related decline in reserve and function across multiple physiologic systems, leading to heightened vulnerability to stressors.3 As such, a preoperative multidimensional evaluation is recommended, as frail patients undergoing surgery face a higher risk of postoperative complications and mortality.2,4 Indeed, the decision regarding patient fitness for surgery is an important aspect to deal with; identifying frailty is essential for informed decision-making, personalized counseling, and the development of tailored management strategies that may include surgical alternatives.
Several urological malignancies, such as prostate cancer and bladder cancer (BCa), as well as bladder outlet obstruction due to benign prostatic enlargement, represent age-related diseases.5–7 However, nowadays, the widespread use of minimally invasive techniques such as laparoscopy and robotics, together with the advancement in anesthesiologist assistance, allows for to safe candidacy of frail or elderly patients for major surgical procedures.8–10 The routine adoption of multimodal indexes or scales to attempt a more comprehensive patient assessment, as the Charlson Comorbidity Index,11 the American Society of Anesthesiologists’ score,12 the G8 screening questionnaire,13 the Functional Independence Measure,14 the Johns Hopkins Adjusted Clinical Groups frailty-defining diagnoses indicator,15 and the MiniCog,16 among others, is rapidly increasing in surgery and specifically in urology. Indeed, many reports demonstrated less tolerance to medical and surgical therapies and worse outcomes in frail subjects with impaired functioning and cognition, compared to their non-frail counterparts.17–19
The Barthel Index (BI) is a validated tool to assess patient health functional status, through the measurement of the degree of independence in activities of daily living (ADL).20 First developed by Dorothea Barthel in 1955 to monitor advances in patients with neuromuscular and muscular-skeletal disease during inpatients rehabilitation, the BI consists of a scale of 10 items related to self-care (feeding, bathing, grooming, dressing, bowel and bladder control, and toilet use) and mobility (ambulation, bed-to-chair transfers, and stair climbing).20 For each of the 10 considered items, two to four response categories are possible, with a total score ranging from 0 (bedridden and completely dependent patient) to 100 (completely independent patient;20,21 Table 1).
Actually, the BI is largely used for the evaluation of geriatric patients,22 especially in contexts as orthopedics,23,24 and physical medicine.25 Previous reports have shown that lower BI scores are associated with prolonged length of in-hospital stay (LOHS), increased rehospitalization rates, and higher cardiovascular and overall mortality (OM) in patients admitted to emergency departments.26,27 Similarly, the association between the BI and survival has been investigated in surgical contexts other than urology, as general surgery, where patients with hepatocarcinoma, cholangiocarcinoma, or colorectal cancer, with greater functional dependence, had poorer prognosis following surgery.28–30 Conversely, the role of the BI in the urological setting has not been fully explored yet.
The aim of this review is to summarize the state of the art of the use in urology and to provide evidence regarding its potential application for the assessment of patient candidates for surgical procedures.
We used a systematic approach, following the Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) statement32 to search for studies focusing on the use of the BI in patients candidates for urologic surgical procedures. PubMed, Scopus, and Web of Science databases were queried. The string used for the search was as follows: (Barthel Index AND urology) OR (Barthel Index AND urologic surgical procedures). Two paired investigators (Andrea Panunzio and Rossella Orlando) independently screened all titles gathered from the literature review to identify potentially eligible studies and then evaluated abstracts or full-text manuscripts to determine the final included ones. Only original articles were considered, with no restriction on language or study design (prospective or retrospective). Surveys, editorials, and studies focusing on other diseases, treatment types, or non-surgical urological contexts were excluded. All articles were categorized according to level of evidence using the Oxford Level of Evidence Working Group 201133 system (Table 2). All data extracted from the included studies were recorded in an electronic database, including authors, journal, year of publication, country of origin, type of surgery, topic, whether the BI was or not the main variable of interest of the study, patients’ demographics, and main studies’ findings. The BI, both as a descriptor of baseline or postoperative patients’ health status, and as a predictor of perioperative (intraoperative and postoperative complications, LOHS, early readmission) and survival outcomes (cancer-specific mortality [CSM], OM, disease-recurrence [DR]) was investigated. A qualitative data synthesis was provided.
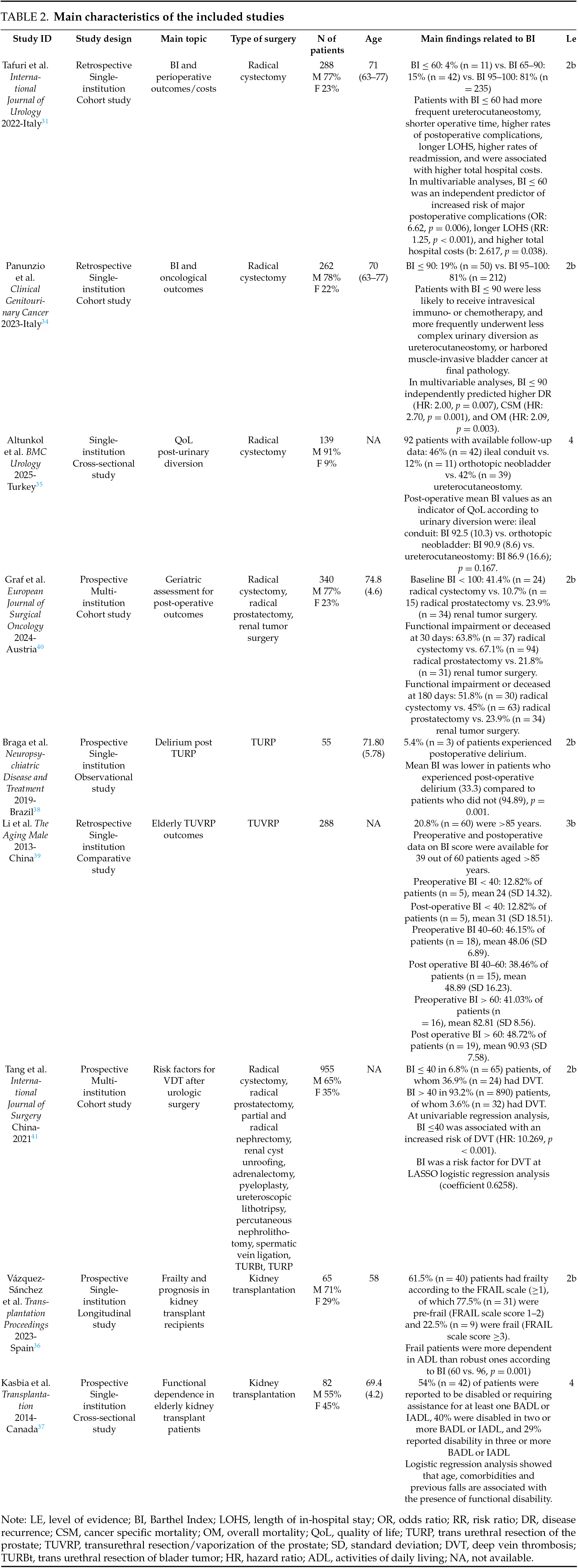
The PRISMA diagram shows the literature research results (Figure 1). We identified 61 records; after excluding duplicates, 45 records remained for screening based on title and abstract. A total of 12 full-text manuscripts were then retrieved and assessed for eligibility, of which three studies focusing on urologic non-surgically treated patients were excluded. Finally, nine records were considered in the current systematic review. Surgical contexts included radical cystectomy (RC) in three studies,31,34,35 kidney transplantation (KT) in two studies,36,37 trans-urethral resection of the prostate (TURP) or trans-urethral vaporization/resection of the prostate (TUVRP) in two studies,38,39 with the remainder including several different urologic surgical procedures performed for both oncological and non-oncological diseases.40,41 The main characteristics of the included studies are summarized in Table 2.
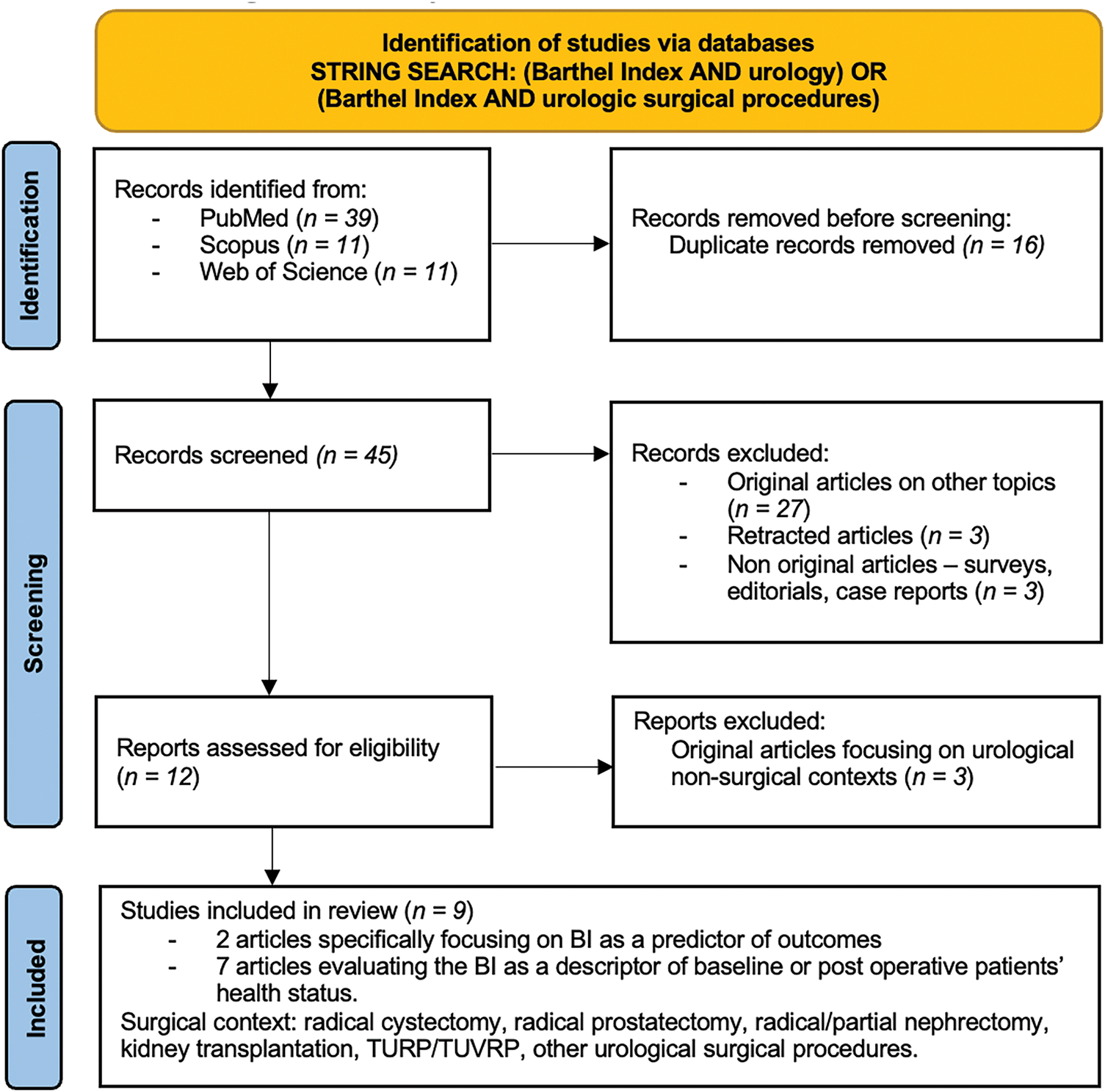
FIGURE 1. The PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) flow diagram
Two studies focused on the BI prognostic value in BCa patients who underwent RC.31,34 Tafuri et al. tested the association between the BI and perioperative outcomes in 288 clinically nonmetastatic BCa patients who underwent RC at a tertiary referral center.31 After having stratified patients according to established risk categories (BI ≤ 60: total/severe dependency in ADL, BI 65–90: moderate dependency in ADL, and BI 95–100: slight dependency/independency in ADL), authors showed that patients with a BI ≤ 60 had more frequent less complex urinary diversion as ureterocutaneostomy, shorter operative time, higher rates of postoperative complications, longer LOHS, higher rates of 90-days readmission, and were associated with higher total costs of hospitalization, compared to patients with BI 65–90 and 95–100. In multivariable analysis, BI ≤ 60 remained an independent predictor of increased risk of major (Clavien Dindo >2) postoperative complications (Odds Ratio: 6.62, p = 0.006), longer LOHS (Risk Ratio: 1.25, p < 0.001), and higher total hospital costs (beta coefficient: 2.617, p = 0.038).31 Panunzio et al. subsequently investigated whether an association between the BI and oncological outcomes also existed in the same patient’s cohort with available follow-up data (n = 262). Authors found that patients with a BI ≤ 90 were less likely to receive intravesical immuno- or chemotherapy, and harbored muscle-invasive BCa at final pathology, compared to patients with a BI of 95–100. In multivariable Cox regression models adjusted for other relevant clinical and pathological confounders, BI ≤ 90 independently predicted higher DR (hazard ratio [HR]: 2.00, p = 0.007), CSM (HR: 2.70, p = 0.001), and OM (HR: 2.09, p = 0.003).34
Other evidence on BI utilization is sparse and comes from included studies where BI was considered as a variable assessed at the initial preoperative patient evaluation or as an indicator of patient health status after surgery. Altunkol et al. used the BI for postoperative functional status assessment as an indicator of quality of life in 92 BCa patients submitted to RC. Based on the type of urinary diversion performed, the mean BI score was 86.9 vs. 90.9 vs. 92.5 in patients with ureterocutaneostomy, orthotopic neobladder and ileal conduit, respectively, with the difference, however, being not statistically significant.35
Graf et al. investigated the accuracy and predictability of geriatric assessment using the Erlangen Index (EI) on persistent functional impairment in ADL measured by the BI following major urological surgery. The EI is derived from the integration of five geriatric assessment tools covering domains of age, mobility, and comorbidities. The authors evaluated a total of 340 patients undergoing RC (n = 58, 17.0%), radical prostatectomy (n = 140, 41.2%), or renal tumor surgery (n = 142, 41.8%). Endpoints were long-term functional deterioration and death at 30- and 180-day. At baseline, 24 (41.4%) patients undergoing RC had a BI < 100 vs. 15 (10.7%) undergoing radical prostatectomy vs. 34 (23.9%) undergoing renal tumor surgery. Overall, ADL impairment as a measure of incomplete recovery after surgery was recorded in 47.6% and 37.4% of cases at 30- and 180-day, respectively. Specifically, according to surgery, radical prostatectomy patients had the highest rate of ADL impairment at 30 days (67.1%), followed by RC (63.8%), and renal tumor surgery (21.8%) patients. Conversely, RC patients had the highest rate of ADL impairment at 180 days (51.8%), followed by radical prostatectomy (45%) and renal tumor surgery (23.9%) patients. The EI showed a good sensitivity for predicting mortality and functional impairment at day 180, highlighting that subjects with poor performance status have a high risk of death or persistent functional deterioration following major oncological urologic surgeries.40
Braga and colleagues explored the incidence and predictors of postoperative delirium within a cohort of 55 healthy elderly patients affected by bladder outlet obstruction due to benign hyperplasia treated with TURP. The authors found that those experiencing post-operative delirium episodes (n = 3) had lower BI score (p < 0.001), suggesting that loss of functional status may be associated with mental health impairment after surgery.38
Li and colleagues investigated independence in ADL in patients aged ≥85 years following TUVRP. Of 39 patients with available follow-up data, 16 had a preoperative BI > 60, which is also maintained after surgery, 18 had a BI between 40 and 60, for whom in 3 cases BI improved to >60, and 5 had a BI <40 for whom in 2 cases BI improved to 40–60. The authors concluded that very elderly patients preserve their functional status after TURVP surgery.39
Tang et al. evaluated data of 955 patients undergoing endoscopic, laparoscopic, and open urologic surgery in order to identify risk factors for the development of deep vein thrombosis, which occurred in 56 cases. At multivariable least absolute shrinkage and selection operator (LASSO) logistic regression analyses, BI < 40, together with other factors such as age, history of deep vein thrombosis, lymph node dissection, perioperative steroid use, Caprini score, D-dimer level, cystectomy, and prostatectomy surgery, represented an independent predictor of high risk of deep vein thrombosis. According to these results, the authors suggested that patients with BI < 40 may require more thromboprophylaxis measures after surgery.41
Vázquez-Sánchez et al. assessed the impact of frailty using the FRAIL scale in 65 KT patients, finding that frailty may impact patients’ ability to perform ADL. Indeed, frail subjects were more dependent in ADL compared with their more robust counterparts, as indicated by lower BI scores (60 vs. 96, p = 0.001).36
Finally, Kasbia et al. evaluated rates of functional disability among 82 elderly patients living with a KT. Functional assessment included the BI for basic self-care tasks (bathing, grooming, dressing, toileting, eating, transferring, and ambulation—BADL), and the Lawton-Brody Scale for the instrumental ADL (shopping, housecleaning, laundry, meal preparation, transportation, telephone use, and management of medications and finances—IADL). Overall, 54% of patients reported being disabled or requiring assistance for at least one BADL or IADL, 40% were disabled in two or more BADL or IADL, and 29% reported disability in three or more BADL or IADL. These results demonstrated a high prevalence of functional dependence in the elderly KT population.37
A comprehensive multidimensional evaluation of patients candidates for surgery is pivotal to identify the most appropriate management in order to avoid complications or adverse events that may impact on quality of life. This concept is of particular interest in elderly or frail subjects, who are even more frequent candidates for surgery.2,42 Despite rarely being routinely assessed, functional health status, measuring patients’ ability to perform ADL, represents an important aspect to evaluate.43 In this review, we summarized the evidence regarding the utility of BI in urology and its potential application as a tool to screen candidates for surgery for frailty.
Overall, nine manuscripts were included, encompassing an overall population of 2474 patients aged >70 years, submitted to several urologic surgical procedures for both oncological and non-oncological diseases. RC represents the most investigated surgical procedure among the included studies. According to international guidelines, RC with bilateral pelvic lymph node dissection and urinary diversion after chemotherapy is the gold-standard treatment for non-metastatic muscle-invasive BCa or recurrent high-risk non-muscle-invasive BCa refractory to previous intravesical therapy.44 Since the incidence of BCa increases with age, RC patients are usually elderly.6,45 Additionally, RC is still burdened by a high risk of complications and mortality related to preexisting comorbidities or the surgical procedure itself, bowel anastomosis, or urinary diversion.44,46,47 Indeed, international guidelines strongly suggest accurately screening candidates for RC for frailty and cognitive impairment, possibly considering geriatric assessment.44 Therefore, it is not surprising that most included reports focused on RC patient cohorts. Two studies, specifically, focused on the BI as a prognostic factor in BCa patients treated with RC, demonstrating worse perioperative outcomes and poor survival in patients with impaired functional health status. Despite the retrospective nature, these findings agree with other contributions, which focused on patients undergoing hepatectomy or hepatic resection for hepatocarcinoma30 or cholangiocarcinoma28 and intestinal resection for colorectal cancer,29 in whom lower BI scores are also associated with poorer prognosis, highlighting the need for alternative strategies or preoperative improvement of autonomy in ADL to provide more favorable outcomes. The BI has also emerged as a predictor of post-operative delirium in patients undergoing TURP and deep vein thrombosis in patients undergoing major urological surgeries. Finally, other contributions, despite not specifically focusing on the BI as the main topic of interest of the research, include it as a preoperative or postoperative variable to evaluate baseline characteristics of surgically treated patients or their health status during the follow-up. These studies demonstrated the reliability of this tool as a descriptor of patients’ functioning before and after surgery, underscoring that more complex surgical procedures, such as RC or KT, are associated with a high prevalence of functional deterioration, significant morbidity, and poorer quality of life.
Taken together, these findings suggest that the BI integration into clinical practice could be of value for the initial assessment of candidates for urologic surgery, especially major oncological surgical procedures. This recommendation is based on the reliability of this tool in describing the patient’s functional reserve and predicting complications and survival. The routine use of the BI should be encouraged for a better selection of patients who are most likely to benefit from surgery or who may require more assistance, due to its important contribution in postoperative and survival risk assessment. Future contributions should explore whether the integration of the BI with other measures of frailty or diminishing reserve and blood tests may improve patient assessment, especially in surgical contexts, as well as the impact of preoperative multidisciplinary rehabilitation programs, including physical exercises, nutrition, and psychological interventions, on perioperative and survival outcomes.
The present systematic review is not devoid of limitations. First, only two studies included in the present review specifically focused on the prognostic role of the BI, with the remainder being heterogeneous for addressing multiple procedures for both the treatment of oncologic and non-oncologic conditions with different outcomes. Second, the evidence base is predominantly composed of intermediate- to low-level studies.
The age of patients candidates for urological surgery is progressively increasing, and a multifactorial preoperative evaluation is needed. The BI is a valid tool to describe a patient’s functional reserve, with important implications in the surgical patient’s pathway. BI use should be encouraged in order to identify subjects at higher risk of adverse outcomes, promoting tailored management and optimizing care.
Acknowledgement
None.
Funding Statement
The authors received no specific funding for this study.
Author Contributions
The authors confirm contribution to the paper as follows: study conception and design: Alessandro Tafuri; data collection: Andrea Panunzio, Rossella Orlando, Giovanni Mazzucato, Floriana Luigina Rizzo, Serena Domenica D’Elia; analysis and interpretation of results: Alessandro Tafuri, Andrea Panunzio; draft manuscript preparation: Alessandro Tafuri, Andrea Panunzio; critical revision: Federico Greco, Antonio Benito Porcaro, Alessandro Antonelli. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
All data analyzed are derived from the published literature and are available in the articles cited within the manuscript. No new data were generated.
Ethics Approval
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest to report regarding the present study.
References
1. Partridge J, Sbai M, Dhesi J. Proactive care of older people undergoing surgery. Aging Clin Exp Res 2018 Mar;30(3):253–257. [Google Scholar]
2. Ethun CG, Bilen MA, Jani AB, Maithel SK, Ogan K, Master VA. Frailty and cancer: implications for oncology surgery, medical oncology, and radiation oncology. CA Cancer J Clin 2017 Sep;67(5):362–377. [Google Scholar]
3. Parikh N, Sharma P. Frailty as a prognostic indicator in the radical cystectomy population: a review. Int Urol Nephrol 2019 Aug;51(8):1281–1290. [Google Scholar]
4. Ornaghi PI, Afferi L, Antonelli A et al. Frailty impact on postoperative complications and early mortality rates in patients undergoing radical cystectomy for bladder cancer: a systematic review. Arab J Urol 2020 Nov 2;19(1):9–23. [Google Scholar]
5. Bell KJL, Del Mar C, Wright G, Dickinson J, Glasziou P. Prevalence of incidental prostate cancer: a systematic review of autopsy studies. Int J Cancer 2015 Oct 1;137(7):1749–1757. [Google Scholar]
6. Fonteyne V, Ost P, Bellmunt J et al. Curative treatment for muscle invasive bladder cancer in elderly patients: a systematic review. Eur Urol 2018;73(1):40–50. [Google Scholar] [PubMed]
7. Patel ND, Parsons JK. Epidemiology and etiology of benign prostatic hyperplasia and bladder outlet obstruction. Indian J Urol 2014 Apr;30(2):170–176. [Google Scholar]
8. Giannarini G, Crestani A, Inferrera A et al. Impact of enhanced recovery after surgery protocols versus standard of care on perioperative outcomes of radical cystectomy: a systematic review and meta-analysis of comparative studies. Minerva Urol Nefrol 2019 Aug;71(4):309–323. [Google Scholar]
9. Suryawanshi CM, Shah B, Khanna S, Ghodki P, Bhati K, Ashok KV. Anaesthetic management of robot-assisted laparoscopic surgery. Indian J Anaesth 2023 Jan;67(1):117–122. [Google Scholar]
10. Reddy K, Gharde P, Tayade H, Patil M, Reddy LS, Surya D. Advancements in robotic surgery: a comprehensive overview of current utilizations and upcoming frontiers. Cureus 2023 Dec;15(12):e50415. [Google Scholar]
11. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40(5):373–383. [Google Scholar] [PubMed]
12. Hendrix JM, Garmon EH. American society of anesthesiologists physical status classification system. In: StatPearls [Internet]. Treasure Island, FL, USA: StatPearls Publishing, 2025. PMID: 28722969. [Google Scholar]
13. G8 geriatric screening tool [Internet]. [cited 2025 Feb 1]. Available from: https://www.mdcalc.com/calc/10426/g8-geriatric-screening-tool. [Google Scholar]
14. Kwon S, Hartzema AG, Duncan PW, Min-Lai S. Disability measures in stroke: relationship among the Barthel Index, the functional independence measure, and the modified rankin scale. Stroke 2004 Apr;35(4):918–923. [Google Scholar]
15. The Johns Hopkins ACG System Excerpt from Technical Reference Guide, 2009 [Internet]. [cited 2025 Feb 1]. Available from: https://www2.gov.bc.ca/assets/gov/health/conducting-health-research/data-access/johns-hopkins-acg-system-technical-reference-guide.pdf. [Google Scholar]
16. Mini-Cog. Quick screening for early dementia detection [Internet]. [cited 2025 Feb 1]. Available from: https://mini-cog.com. [Google Scholar]
17. Michel J, Goel AN, Golla V et al. Predicting short-term outcomes after radical cystectomy based on frailty. Urology 2019;133:25–33. [Google Scholar] [PubMed]
18. Rosiello G, Palumbo C, Knipper S et al. Preoperative frailty predicts adverse short-term postoperative outcomes in patients treated with radical prostatectomy. Prostate Cancer Prostatic Dis 2020 Dec;23:573–580. [Google Scholar]
19. Palumbo C, Knipper S, Pecoraro A et al. Patient frailty predicts worse perioperative outcomes and higher cost after radical cystectomy. Surg Oncol 2020 Mar;32:8–13. [Google Scholar]
20. Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J 1965 Feb;14:61–65. [Google Scholar]
21. Barthel index for activities of daily living (ADL) [Internet]. [cited 2025 Feb 1]. Available from: https://www.mdcalc.com/calc/3912/barthel-index-activities-daily-living-adl. [Google Scholar]
22. Kaur P, Rowland J, Whiting E. The ABCD of the comprehensive geriatric assessment. Med J Aust 2021 Sep 2;215(5):206–207.e1. [Google Scholar]
23. Kammerlander C, Riedmüller P, Gosch M et al. Functional outcome and mortality in geriatric distal femoral fractures. Injury 2012 Jul;43(7):1096–1101. [Google Scholar]
24. Hulsbæk S, Larsen RF, Rosthøj S, Kristensen MT. The Barthel Index and the Cumulated Ambulation Score are superior to the de Morton Mobility Index for the early assessment of outcome in patients with a hip fracture admitted to an acute geriatric ward. Disabil Rehabil 2019;41(11):1351–1359. [Google Scholar]
25. Sainsbury A, Seebass G, Bansal A, Young JB. Reliability of the Barthel Index when used with older people. Age Ageing 2005 May;34(3):228–232. [Google Scholar]
26. Bahrmann A, Benner L, Christ M et al. The Charlson Comorbidity and Barthel Index predict length of hospital stay, mortality, cardiovascular mortality and rehospitalization in unselected older patients admitted to the emergency department. Aging Clin Exp Res 2019 Sep;31(9):1233–1242. [Google Scholar]
27. Ocagli H, Cella N, Stivanello L, Degan M, Canova C. The Barthel index as an indicator of hospital outcomes: a retrospective cross-sectional study with healthcare data from older people. J Adv Nurs 2021 Apr;77(4):1751–1761. [Google Scholar]
28. Mima K, Hayashi H, Yumoto S et al. Disability in perioperative activities of daily living is associated with worse survival outcomes following hepatic resection in patients with intrahepatic cholangiocarcinoma. Hepatol Res 2022 Oct 28;53(2):135–144. [Google Scholar]
29. Mima K, Kosumi K, Miyanari N et al. Impairment of activities of daily living is an independent risk factor for recurrence and mortality following curative resection of stage I–III colorectal cancer. J Gastrointest Surg 2021 Oct;25(10):2628–2636. [Google Scholar]
30. Mima K, Imai K, Kaida T et al. Impairment of perioperative activities of daily living is associated with poor prognosis following hepatectomy for hepatocellular carcinoma. J Surg Oncol 2022 Nov;126(6):995–1002. [Google Scholar]
31. Tafuri A, Panunzio A, Gozzo A et al. Impact of functional impairment and cognitive status on perioperative outcomes and costs after radical cystectomy: the role of Barthel Index. Int J Urol 2022 Dec 28;30(4):366–373. [Google Scholar]
32. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010;8(5):336–341. [Google Scholar] [PubMed]
33. Howick J, Chalmers I, Glasziou P et al. The 2011 oxford CEBM levels of evidence (Introductory Document). Oxford Centre for Evidence-Based Medicine [Internet]. [cited 2025 Feb 1]. Available from: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence. [Google Scholar]
34. Panunzio A, Gozzo A, Mazzucato G et al. Impairment in activities of daily living assessed by the barthel index predicts adverse oncological outcomes after radical cystectomy for bladder cancer. Clin Genitourin Cancer 2023 Dec;21(6):e495–e501.e2. [Google Scholar]
35. Altunkol A, Alma E, Vuruşkan E et al. Health-related quality of life after radical cystectomy for bladder cancer in elderly patients with ileal orthotopic neobladder, ureterocutaneostomy or ileal conduit: cross-sectional study using validated questionnaires. BMC Urol 2025 Mar 10;25(1):46. [Google Scholar]
36. Vázquez-Sánchez T, López V, Schuldt R et al. Importance of frailty in kidney transplant recipients. Transplant Proc 2023 Dec;55(10):2271–2274. [Google Scholar]
37. Kasbia GS, Farragher J, Kim SJ, Famure O, Jassal SV. A cross-sectional study examining the functional independence of elderly individuals with a functioning kidney transplant. Transplantation 2014 Oct 27;98(8):864–870. [Google Scholar]
38. Braga ILS, Castelo-Filho J, de Pinheiro RSB et al. Functional capacity as a predictor of postoperative delirium in transurethral resection of prostate patients in Northeast Brazil. Neuropsychiatr Dis Treat 2019;15:2395–2401. [Google Scholar] [PubMed]
39. Li AH, Zhang Y, Lu HH et al. Living status in patients over 85 years of age after TUVRP. Aging Male 2013 Dec;16(4):191–194. [Google Scholar]
40. Graf S, Lutz J, Koneval L et al. Preoperative geriatric assessment to predict functional outcome after major urologic operations: results from a multicenter study. Eur J Surg Oncol 2024 Dec;50(12):108693. [Google Scholar]
41. Tang G, Qi L, Sun Z et al. Evaluation and analysis of incidence and risk factors of lower extremity venous thrombosis after urologic surgeries: a prospective two-center cohort study using LASSO-logistic regression. Int J Surg 2021 May;89:105948. [Google Scholar]
42. Tafuri A, Marchioni M, Cerrato C et al. Changes in renal function after nephroureterectomy for upper urinary tract carcinoma: analysis of a large multicenter cohort (Radical Nephroureterectomy Outcomes (RaNeO) Research Consortium). World J Urol 2022 Nov;10(11):2771–2779. [Google Scholar]
43. Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK. Prognostic indices for older adults: a systematic review. JAMA 2012 Jan 11;307(2):182–192. [Google Scholar]
44. Witjes JA, Bruins HM, Carrion A et al. EAU guidelines on muscle-invasive and metastatic bladder cancer. Arnhem, The Netherlands: EAU Guidelines Office. [Internet]. [cited 2025 Feb 1]. Available from: https://uroweb.org/guidelines/muscle-invasive-and-metastatic-bladder-cancer. [Google Scholar]
45. Hanna K, Ditillo M, Joseph B. The role of frailty and prehabilitation in surgery. Curr Opin Crit Care 2019;25(6):717–722. [Google Scholar] [PubMed]
46. De Nunzio C, Cindolo L, Leonardo C et al. Analysis of radical cystectomy and urinary diversion complications with the Clavien classification system in an Italian real life cohort. Eur J Surg Oncol 2013 Jul;39(7):792–798. [Google Scholar]
47. Antonelli A, Belotti S, Cristinelli L, De Luca V, Simeone C. Comparison of perioperative morbidity of radical cystectomy with neobladder versus ileal conduit: a matched pair analysis of 170 patients. Clin Genitourin Cancer 2016 Jun;14(3):244–248. [Google Scholar]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF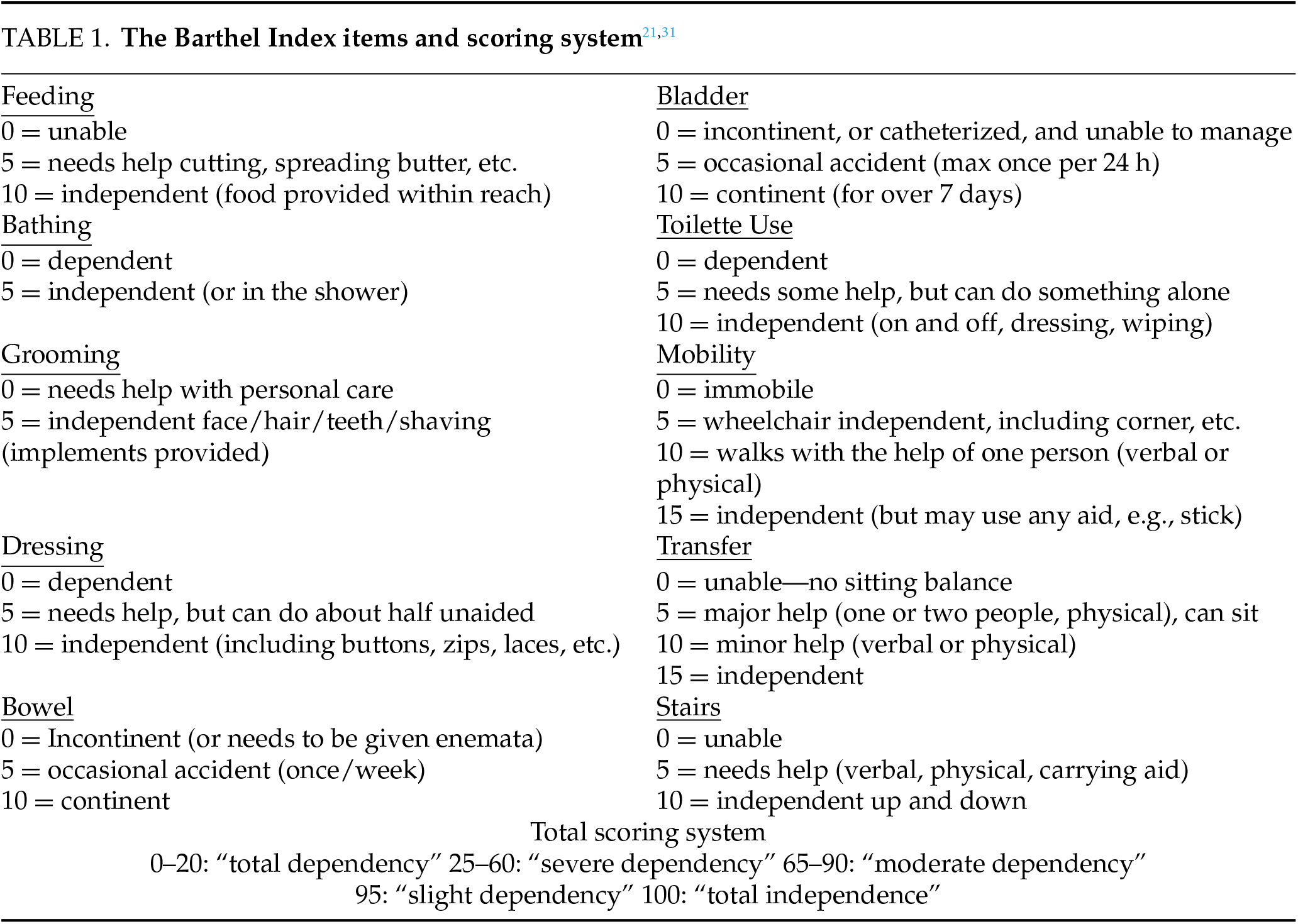
 Downloads
Downloads
 Citation Tools
Citation Tools