 Open Access
Open Access
ARTICLE
Low utilization of intracavernosal injection and penile Doppler ultrasound in the evaluation of erectile dysfunction and Peyronie’s disease
1 Department of Urology, Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA 19107, USA
2 Department of Urology, Jefferson Einstein Philadelphia Hospital, Philadelphia, PA 19141, USA
* Corresponding Author: Paul H. Chung. Email:
Canadian Journal of Urology 2025, 32(6), 589-595. https://doi.org/10.32604/cju.2025.064125
Received 06 February 2025; Accepted 06 August 2025; Issue published 30 December 2025
Abstract
Introduction: Despite the diagnostic value of intracavernosal injections (ICI) and penile Doppler ultrasound (PDUS), there remain barriers to widespread clinical adaptation of these methods. The study aimed to evaluate the practice patterns of utilization of ICI and PDUS in the assessment of erectile dysfunction (ED) and Peyronie’s disease (PD). Methods: Using the TriNetX database (Cambridge, MA, USA), adult (≥18 years) male patients with a diagnosis of ED on oral phosphodiesterase-5 (PDE5) inhibitors were identified. Current Procedural Terminology codes were utilized to identify patients who underwent further evaluation with ICI or PDUS, as well as penile prosthesis placement after PDUS. A second cohort was analyzed, identifying patients with a diagnosis of PD who underwent ICI or PDUS, and those who subsequently underwent PD treatment. Results: Among 104 healthcare organizations, 52,227,262 adult males were screened for ED and PD. 1,689,907 (3.2%) patients had ED and 66,390 (0.1%) patients had PD. Among ED patients, there were 6508 (0.4%) who subsequently went on to receive penile prosthesis. Amongst ED patients, only 23,836 (1.4%) and 8548 (0.5%) patients underwent workup with ICI or PDUS. The number of patients who subsequently received a prosthesis after ICI and PDUS workup was 4680 (19.6%) and 868 (10.1%), respectively. Amongst PD patients, 2960 (4.5%) and 4972 (7.4%) underwent workup with ICI and PDUS, respectively. Conclusion: We recognize that ED and PD are challenging disease processes with complicated diagnostic workup involved. We recommend that providers be knowledgeable about counseling patients and even consider referring motivated patients to high-volume referral centers for definitive treatment.Keywords
Intracavernosal injection (ICI) testing is a valuable tool in the workup of male sexual dysfunction.1,2 ICI testing assesses erectile function, but also enables evaluation of penile deformities, plaques, curvatures or pain. The point of maximum curvature and measurements of erect penile girth and length can also be assessed. Combined with sonography, penile Doppler ultrasound (PDUS) provides a quantitative assessment of penile vasculature as well as inspection of penile pathology, such as fibrosis or plaques and their associated size, density or calcifications.1 Despite the diagnostic value of ICI and PDUS, there remain barriers to the widespread clinical adaptation of these methods. These in-office testing procedures are nuanced and should be performed and interpreted by providers with experience and training. This can also be a logistical challenge due to the need for monitoring patients after ICI injections to ensure full detumescence in the office. The current utilization of pharmacologic agents and PDUS in the evaluation of male sexual dysfunction is not known. In this article, we provide a descriptive analysis of the practice patterns of ICI and PDUS utilization for the assessment of erectile dysfunction (ED) and Peyronie’s disease (PD) using a global registry with the aim of promoting increased utilization of these methods in the workup of male sexual dysfunction. We hypothesize that the utilization of ICI and PDUS for the workup and management of ED and PD remains low.
Data source and study population definition
We accessed the TriNetX research network, a collaborative research enterprise containing real-time data from electronic health records worldwide of over 100 million patients over 100 healthcare organizations at the time of analysis. The TriNetX database constantly updates but reports data coded into the EHRs from up to 20 years prior to the date of analysis only. This database contains data on patient demographics, clinical characteristics, medical diagnoses, procedures and surgeries, and medications. Due to the de-identified nature of this registry, our study was deemed exempt from Institutional Review Board approval or informed consent. For more information, please visit: https://trinetx.com/real-world-resources/case-studies-publications/trinetx-publication-guidelines/ (accessed on 5 August 2025).
Using the TriNetX (https://trinetx.com) database (Cambridge, MA, USA), adult (≥18 years) male patients with a diagnosis of ED (N52) on oral phosphodiesterase-5 (PDE5) inhibitors (e.g., avanafil, sildenafil, vardenafil, and tadalafil) were identified with International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes.3 TriNetX identifies prescriptions using both Veterans Affairs Drug Classification and RxNorm Concept Unique Identifier, part of the Unified Medical Language System.4,5 Current Procedural Terminology (CPT) codes were then utilized to identify patients who underwent further evaluation with ICI of a vasoactive agent (54235) or PDUS (93980, 93981), as well as subsequent penile prosthesis placement (54400, 54401, 54405) after PDUS assessment. A second cohort was analyzed, identifying patients with a diagnosis of PD (N48.6). We then identified patients with curvature who underwent further evaluation with ICI or PDUS, as well as those patients who subsequently underwent intralesional plaque injection (54200), surgical correction including penile plication (54360), penile prosthesis placement (54400, 54401, 54405) or plaque excision ± grafting (54110, 54111, 54112) as a treatment option. A flowchart demonstrating our analysis for the evaluation and management of medically treated ED and PD is shown in Figure 1. Given the de-identified nature of this data, our study was deemed exempt from Institutional Review Board approval. Data was accessed on 11 December 2024.
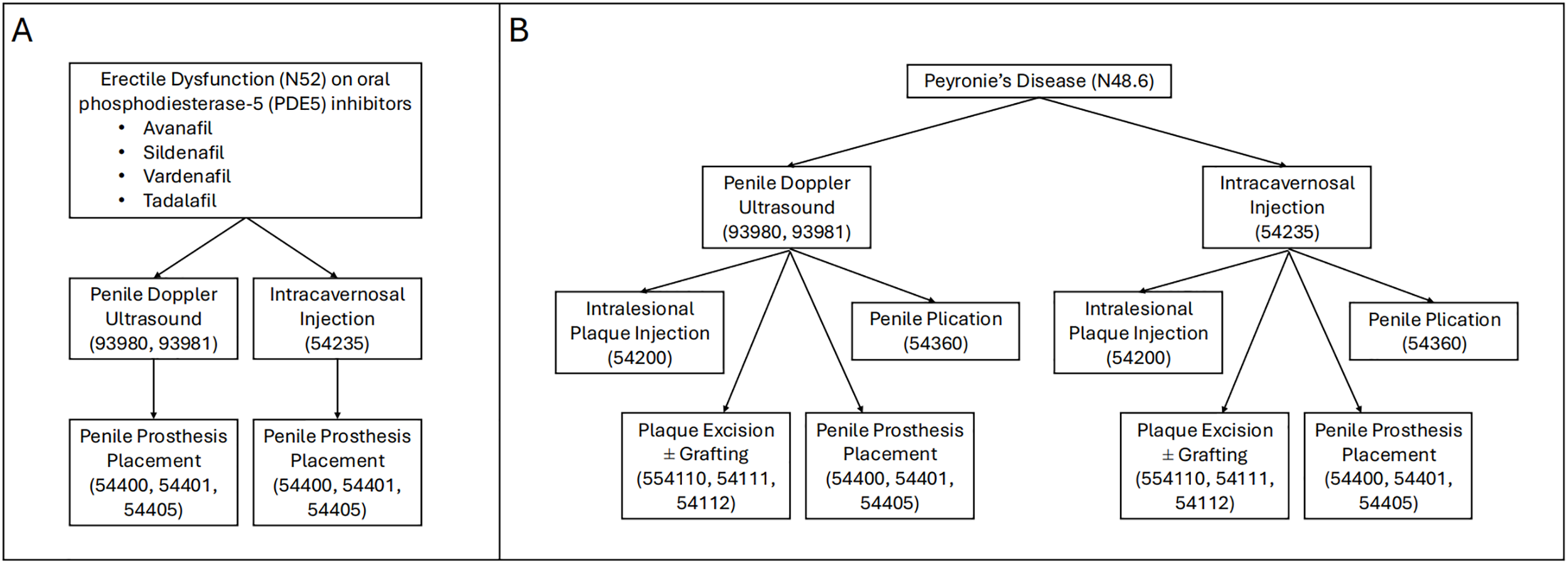
FIGURE 1. Flowchart demonstrating the evaluation and management for medically treated (A) Erectile dysfunction (ED) and (B) Peyronie’s disease (PD)
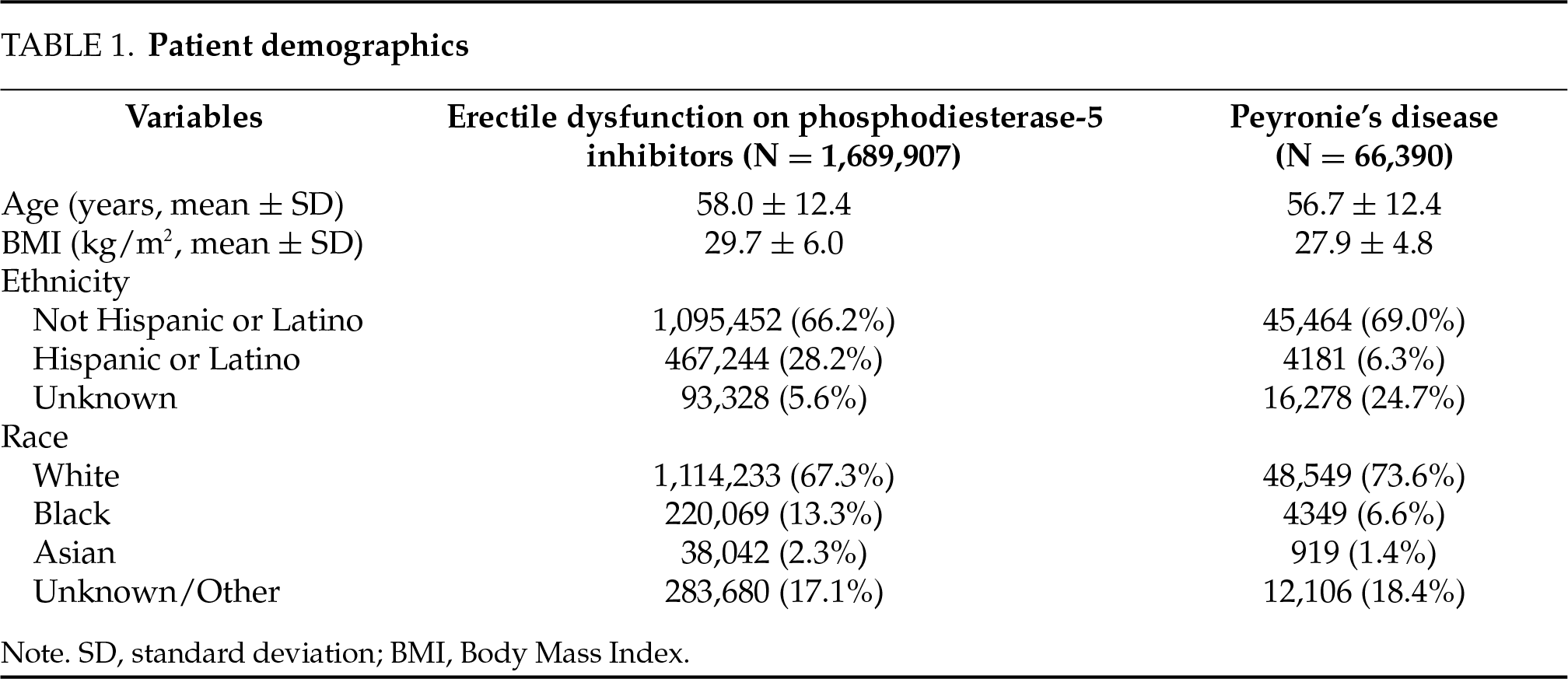
Several demographic a priori determined variables were included. These included age (years), body mass index (kg/m2), ethnicity (not Hispanic or Latino, Hispanic or Latino, Unknown), and race (White, Black, Asian, Unknown/Other). Other covariates included in our analyses were ED on PDE5 inhibitors (yes/no), PD (yes/no), ICI (yes/no), PDUS (yes/no), intralesional plaque injection (yes/no), penile plication (yes/no), penile prosthesis placement (yes/no), and plaque excision ± grafting (yes/no). All data were obtained from the TriNetX database.
All analyses were performed internally via the TriNetX system. Of note, for analyses that resulted in 10 patients or less, TriNetX rounds the value to 10 as part of a patient privacy protection mechanism. For patient demographics, age and BMI were analyzed and presented as continuous variables, while ethnicity and race were analyzed and presented as categorical variables. The remainder of our analyses were primarily descriptive in nature with the results being presented in numbers and percentages.
Patient cohort and clinical characteristics
Among 104 healthcare organizations, 52,227,262 adult males were screened for ED on oral pharmacotherapy and PD. A total of 1,689,907 (3.2%) patients among 98 HCOs had a diagnosis of ED on PDE5 inhibitors, and a total of 66,390 (0.1%) patients among 95 HCOs had a diagnosis of PD. Demographic data for these two separate cohorts are included in Table 1.
ICI and PDUS utilization for ED and PD
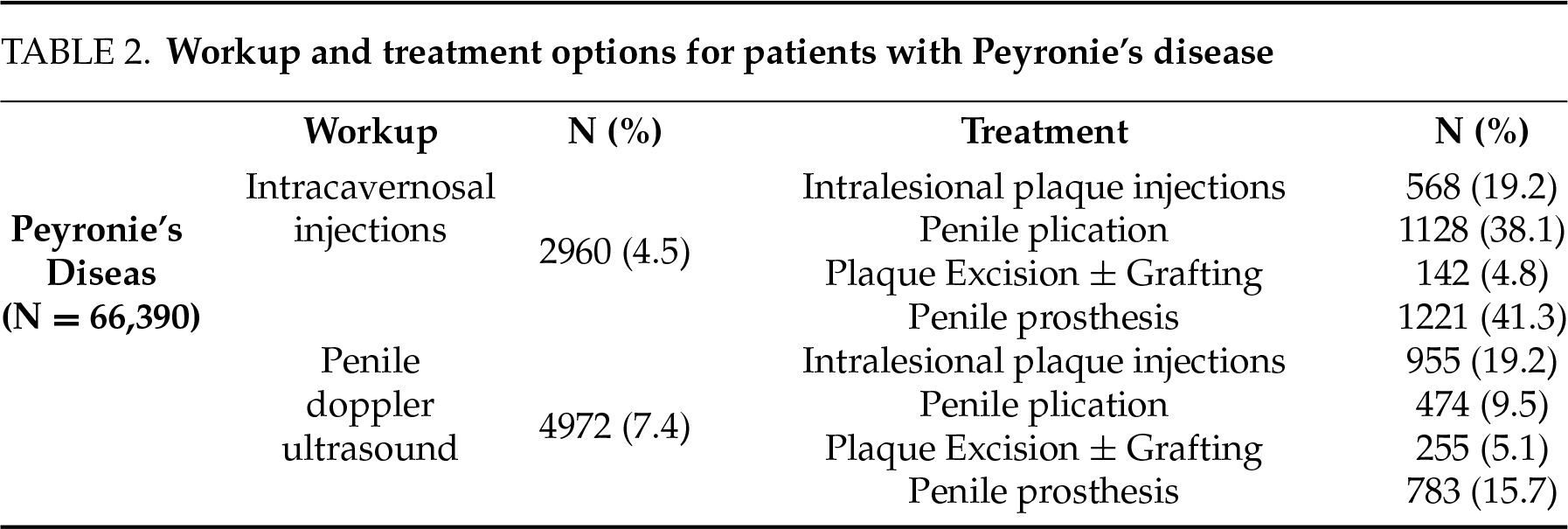
Among patients with a diagnosis of ED on PDE5 inhibitors, there were 6508 (0.4%) who subsequently went on to receive penile prosthesis. Other treatment modalities that were attempted prior to patients receiving penile prosthesis include vacuum erection device, urethral suppositories, and ICI in 21, 292, and 4680 patients, respectively. For patients with ED on PDE5 inhibitors, only 23,836 (1.4%) and 8548 (0.5%) of patients underwent workup with ICI or PDUS. The number of patients who subsequently received a penile prosthesis after ICI and PDUS workup was 4680 (19.6%) and 868 (10.1%), respectively. Details regarding the workup with ICI/PDUS and subsequent management of PD are summarized in Table 2.
Utility of ICI/PDUS for erectile dysfunction
Current guidelines do not provide strong recommendations regarding the utilization of ICI and PDUS. This is because these tests may not be necessary in the early stages of ED. ED can be diagnosed if it fits the definition of “inability to achieve or maintain an erection sufficient for satisfactory sexual activity”. As such, many patients can diagnose this themselves and clinicians can often prescribe accordingly. These specialized workup and diagnostic tests are typically reserved when ED drugs are ineffective. American Urologic Association (AUA)/Sexual Medicine Society of North America (SMSNA) ED guidelines endorse specialized testing comprising ICI and PDUS in select patients.2
Our study suggested that the utilization of PDUS is low, as only 0.5% of adult men with ED on oral therapy underwent evaluation with PDUS. This may be surprising as the reported efficacy of PDE5 inhibitors is 70%.6 The reasoning behind the low usage may be multifactorial. A survey evaluating perceptions of Canadian urology residents and program directors revealed that the majority of programs lack a formal genitourinary imaging curriculum, with the lack of time and educators being primary barriers to increasing imaging training during residency.7 Wide variability exists among practitioners in terms of both penile Doppler ultrasound technique and interpretation. In 2011, the AUA and the American Institute of Ultrasound in Medicine composed guidelines for penile technique to improve the utilization and reliability of diagnostic results.8 A 2018 survey distributed to members of the International Society for Sexual Medicine (ISSM) revealed poor compliance with these guidelines as well as significant heterogeneity in the method of practice.9 This heterogeneity may stem from a lack of training, as the majority of urologists do not have formal instruction in ultrasound technique in residency and/or fellowship training. This gap in training conflicts with AUA/SMSNA ED guidelines, which advise that PDUS should only be utilized by urologists with extensive training in the technique. The issues associated with insurance reimbursement for this diagnostic modality may also limit its widespread use. Both PDUS and ICI testing reimbursement may vary by payer depending on specific plans or policies. Certain carriers may not consider these workups medically necessary unless specific conditions are met. While there have yet to be studies evaluating the specific cost analyses for these diagnostic techniques, a study of patient out-of-pocket costs for guideline-recommended ED treatments demonstrated annual ICI prescriptions to be the second most costly option after intraurethral suppositories.10 Next, PDUS can be a time-consuming or logistically challenging technique that many providers may not have the bandwidth to perform in the clinic. Even in practices in which the radiologist performs the imaging study, many require a urologist to be available to perform the injection, as well as be available should any complications arise, such as prolonged erection. Lastly, the absence of standardized protocols for the use of the vasoactive agent of choice and its associated dosages further complicates its widespread usage.11
Performing ICI routinely prior to penile prosthesis implantation will help identify penile curvature and concealed plaques preoperatively, which can be important as men with these findings require special attention and careful surgical planning owing to associated corporal fibrosis and penile deformity.12,13 Studies have shown that 60–71% of patients have resolution of curvature with prosthesis placement alone, but a subset of patients will require more aggressive dilation, corporal plication, or plaque excision.1,2 While penile prosthesis surgery in men with PD has been shown to be a safe procedure with high patient satisfaction, there is an increased risk of potential complications such as cylinder crossover in cases in which adjuvant procedures are required.14 Another possible complication is urethral injury at the level of the fossa navicularis when the cylinders are forcibly bent during manual modeling.15 Moreover, some authors suggest that intraoperative modelling may increase the risk of mechanical failure.14 Other potential complications with concurrent penile prosthesis placement and PD surgery, such as plaque excision/grafting, include aneurysmal dilation of prosthetic cylinders.16 As such, detailed patient evaluation, including PDUS, especially in men who have been unable to obtain erections for a long duration of time, may benefit from evaluation of penile curvature prior to penile implantation to help manage patient expectations and mitigate potential operative complications.17,18
Utility of ICI/PDUS for Peyronie’s disease
Despite recommendations from the AUA to perform ICI testing with or without PDUS prior to invasive treatment for penile curvature correction, this was rarely performed, as our study showed that only 4.5% of patients with a diagnosis of PD underwent pharmacologic testing.1 It is likely that some of these patients have supplied photos demonstrating curvature or a decision was made to proceed with surgery based on history alone. However, penile autophotography has been found to underestimate the degree of penile curvature compared to ICI testing.19 The risk for error is especially evident in men with concurrent ED, with the potential to impact the planning of treatment strategy.20
Additionally, our study revealed differential utilization of PD surgical techniques depending on patient assessment. Specifically, 38% of men whose PD evaluation included ICI underwent a penile plication procedure as compared to 9% of men whose PD evaluation included PDUS. Although our ability to draw conclusions from this discordance is limited, the findings suggest that additive information from diagnostic ultrasound may influence the decision to proceed with penile plication as opposed to penile excision and grafting. Patients undergoing either penile plication or plaque excision are required to have preserved erectile function, with the deciding factor between the two surgeries determined by the degree of curvature, plaque location and size.21 Information regarding plaque location and burden obtained from imaging evaluation may influence surgeon preference regarding surgical technique.22,23 This insight may help determine the more suitable procedure, and as a result, help to decrease repeat procedures and preventable post-operative morbidity.
Furthermore, a subset of patients presenting with penile curvature and pain may not have plaques palpable on examination.24 Penile ultrasound can provide an objective assessment by identifying plaques confined to the septum or punctate plaques undetectable on exam.25 Plaque calcification has been found to be a poor predictor of the success of collagenase clostridium histolyticum treatment. Importantly, penile ultrasound can also identify concurrent ED and differentiate between vascular and non-vascular etiologies.26 This diagnostic information can aid in patient counseling with the potential to improve patient outcomes and satisfaction.
Certainly, our findings regarding rates of ICI and PDUS utilization must be interpreted in the context of certain limitations, including biases from using a retrospectively maintained database, assumptions regarding the accuracy of the database, as well as potential undercoding of queried ICD/CPT codes. There is also limited data regarding the severity of disease and immediate clinical or surgical outcomes for patients with ED/PD after intervention. Nonetheless, the findings represent the first study to quantify the use of penile injection and ultrasound in the workup of ED and PD, underscoring lower-than-expected use despite society recommendations. This provides insight into the area of practice pattern improvement to increase diagnosis accuracy and patient counseling prior to advancing to corrective procedures. Experts should be diligent in ICI and PDUS in their evaluation of ED and PD to provide the most precise diagnosis, thorough surgical counseling, as well as minimize unexpected scenarios in the operating room. Lastly, we recognize that ED and PD are challenging disease processes with complicated diagnostic workup involved, and we recommend that providers be knowledgeable about counseling their patients and even consider referring motivated patients to high-volume referral centers for definitive treatment. Specifically, these patients may include those with concomitant ED or PD, patients who have failed conservative or medical management, or younger patients.
Utilization of ICI and PDUS for the workup and management of ED and PD remains low. Future research should be focused on analyzing risk factors and specific barriers to the low utilization of these specialized tests, with the goal of overcoming these issues. It should also focus on treatment options that were not readily available in the TriNetX database, such as a vacuum erection device or urethral suppositories for ED or plaque incision for PD, as well as their associated outcomes.
Acknowledgement
Not applicable.
Funding Statement
The authors received no specific funding for this study.
Author Contributions
The authors confirm contribution to the paper as follows: study conception and design: Joon Yau Leong, Paul H. Chung; data collection: Tyler Gaines, Zachary J. Prebay, David Ebbott; analysis and interpretation of results: All authors; draft manuscript preparation: All authors. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
The data that support the findings of this study are available publicly through the TriNetX website.
Ethics Approval
This retrospective study is exempt from informed consent. The data reviewed is a secondary analysis of existing data, does not involve intervention or interaction with human subjects, and is de-identified per the de-identification standard defined in Section §164.514(a) of the HIPAA Privacy Rule. The process by which the data is de-identified is attested to through a formal determination by a qualified expert as defined in Section §164.514(b)(1) of the HIPAA Privacy Rule. This formal determination by a qualified expert refreshed on December 2020.
Conflicts of Interest
The authors declare no conflicts of interest to report regarding the present study.
References
1. Nehra A, Alterowitz R, Culkin DJ et al. Peyronie’s disease: AUA guideline. J Urol 2015 Sep;194(3):745–753. doi:10.1016/j.juro.2015.05.098. [Google Scholar] [PubMed] [CrossRef]
2. Burnett AL, Nehra A, Breau RH et al. Erectile dysfunction: AUA guideline. J Urol 2018 Sep;200(3):633–641. doi:10.1016/j.juro.2018.05.004. [Google Scholar] [PubMed] [CrossRef]
3. World Health Organization (WHO). International statistical classification of diseases and related health problems. 10th ed. Geneva, Switzerland; 2010. [Google Scholar]
4. National Library of Medicine. RxNorm. Bethesda, MD, USA: National Institutes of Health, U.S. Department of Health and Human Services; 2024. [Google Scholar]
5. U.S. Department of Veterans Affairs. VA national drug file. USA: Pharmacy Benefits Management Services; 2017 Jul 26. [Google Scholar]
6. Brock GB, McMahon CG, Chen KK et al. Efficacy and safety of tadalafil for the treatment of erectile dysfunction: results of integrated analyses. J Urol 2002 Oct;168(4 Pt 1):1332–1336. doi:10.1016/s0022-5347(05)64442-4. [Google Scholar] [PubMed] [CrossRef]
7. Bouhadana D, Elbaz S, Di Ioia R et al. Evaluating the perceptions of Canadian urology residents and program directors regarding the current training in genitourinary imaging. Can Urol Assoc J 2023 Aug 29;17(12):418–424. doi:10.5489/cuaj.8430. [Google Scholar] [PubMed] [CrossRef]
8. AIUM practice guideline for the performance of an ultrasound examination in the practice of urology. J Ultrasound Med 2012 Jan;31(1):133–144. doi:10.7863/jum.2012.31.1.133. [Google Scholar] [PubMed] [CrossRef]
9. Butaney M, Thirumavalavan N, Hockenberry MS, Kirby EW, Pastuszak AW, Lipshultz LI. Variability in penile duplex ultrasound international practice patterns, technique, and interpretation: an anonymous survey of ISSM members. Int J Impot Res Oct 2018;30(5):237–242. doi:10.1038/s41443-018-0061-3. [Google Scholar] [PubMed] [CrossRef]
10. Nguyen V, McGovern AM, Rojanasarot S et al. Patient out-of-pocket costs for guideline-recommended treatments for erectile dysfunction: a medicare cost modeling analysis. Int J Impot Res 2025 Jan;37(1):45–50. doi:10.1038/s41443-024-00903-9. [Google Scholar] [PubMed] [CrossRef]
11. Nascimento B, Miranda EP, Terrier JE, Carneiro F, Mulhall JP. A critical analysis of methodology pitfalls in duplex doppler ultrasound in the evaluation of patients with erectile dysfunction: technical and interpretation deficiencies. J Sex Med 2020 Aug;17(8):1416–1422. doi:10.1016/j.jsxm.2020.05.023. [Google Scholar] [PubMed] [CrossRef]
12. Aversa A, Crafa A, Greco EA, Chiefari E, Brunetti A, La Vignera S. The penile duplex ultrasound: how and when to perform it? Andrology 2021 Sep;9(5):1457–1466. doi:10.1111/andr.13029. [Google Scholar] [PubMed] [CrossRef]
13. Varela CG, Yeguas LAM, Rodríguez IC, Vila MDD. Penile doppler ultrasound for erectile dysfunction: technique and interpretation. Am J Roentgenol 2020 May;214(5):1112–1121. doi:10.2214/ajr.19.22141. [Google Scholar] [PubMed] [CrossRef]
14. Garaffa G, Minervini A, Christopher NA, Minhas S, Ralph DJ. The management of residual curvature after penile prosthesis implantation in men with Peyronie’s disease. BJU Int 2011 Oct;108(7):1152–1156. doi:10.1111/j.1464-410X.2010.10023.x. [Google Scholar] [PubMed] [CrossRef]
15. Stember DS, Kohler TS, Morey AF. Management of perforation injuries during and following penile prosthesis surgery. J Sex Med 2015 Nov;12(Supplement_7):456–461. doi:10.1111/jsm.12997. [Google Scholar] [PubMed] [CrossRef]
16. Krakhotkin DV, Ralph DJ, Blecher GA et al. Management of residual penile curvature after penile prosthesis placement. Asian J Androl 2021 Mar–Apr;23(2):129–134. doi:10.4103/aja.aja_62_20. [Google Scholar] [PubMed] [CrossRef]
17. Flores JM, West M, Mulhall JP. Efficient use of penile Doppler ultrasound for investigating men with erectile dysfunction. J Sex Med 2024 Aug;1(8):734–739. doi:10.1093/jsxmed/qdae070. [Google Scholar] [PubMed] [CrossRef]
18. Elgendi K, Zulia N, Beilan J. A review on penile doppler and ultrasonography for erectile dysfunction. Curr Urol Rep 2023 Feb;24(2):69–74. doi:10.1007/s11934-022-01135-4. [Google Scholar] [PubMed] [CrossRef]
19. Wymer K, Ziegelmann M, Savage J, Kohler T, Trost L. Plaque calcification: an important predictor of collagenase clostridium histolyticum treatment outcomes for men with peyronie’s disease. Urology 2018 Sep;119:109–114. doi:10.1016/j.urology.2018.06.003. [Google Scholar] [PubMed] [CrossRef]
20. Traeger M, Leiber-Caspers C, Chierigo F, Cakir OO, Gratzke C, Schlager D. Penile autophotography underestimates the degree of penile curvature in peyronie’s disease. Eur Urol Focus 2023 Jan;9(1):64–68. doi:10.1016/j.euf.2022.10.009. [Google Scholar] [PubMed] [CrossRef]
21. Rybak J, Papagiannopoulos D, Levine L. A retrospective comparative study of traction therapy vs. no traction following tunica albuginea plication or partial excision and grafting for Peyronie’s disease: measured lengths and patient perceptions. J Sex Med 2012 Sep;9(9):2396–2403. doi:10.1111/j.1743-6109.2012.02849.x. [Google Scholar] [PubMed] [CrossRef]
22. Good J, Crist N, Henderson B, Karcher C, Sencaj J, Bernie HL. Inflatable penile prosthesis placement in Peyronie’s disease: a review of surgical considerations, approaches, and maneuvers. Transl Androl Urol 2024 Jan 31;13(1):139–155. doi:10.21037/tau-23-180. [Google Scholar] [PubMed] [CrossRef]
23. Spinozzi L, Droghetti M, Palmisano F et al. Use of soft penile prosthesis in grafting surgery for peyronie’s disease and mild erectile dysfunction: still an option? Arch Esp Urol 2024 Apr;77(3):270–277. doi:10.56434/j.arch.esp.urol.20247703.36. [Google Scholar] [PubMed] [CrossRef]
24. Yafi FA, Hatzichristodoulou G, DeLay KJ, Hellstrom WJ. Review of management options for patients with atypical peyronie’s disease. Sex Med Rev 2017 Apr;5(2):211–221. doi:10.1016/j.sxmr.2016.07.004. [Google Scholar] [PubMed] [CrossRef]
25. Punjani N, Stern N, Brock G. Characterization of septal and punctate scarring in peyronie’s disease. Urology 2018 Aug;118:87–91. doi:10.1016/j.urology.2018.05.014. [Google Scholar] [PubMed] [CrossRef]
26. McCauley JF, Dean RC. Diagnostic utility of penile ultrasound in Peyronie’s disease. World J Urol 2020 Feb;38(2):263–268. doi:10.1007/s00345-019-02928-y. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools