 Open Access
Open Access
CASE REPORT
Brunn’s cyst causing lower urinary tract symptoms in a young adult: A case report with brief review of literature
Department of Urology and Renal Transplant, Vardhman Mahavir Medical College & Safdarjung Hospital, Delhi, 110029, India
* Corresponding Author: Harshdeep Singh. Email:
Canadian Journal of Urology 2025, 32(6), 685-689. https://doi.org/10.32604/cju.2025.064435
Received 16 February 2025; Accepted 01 July 2025; Issue published 30 December 2025
Abstract
Background: Brunn’s cyst is a seldom encountered etiology in a wide spectrum of causative pathologies producing lower urinary tract symptoms (LUTS) in a young male, causing voiding symptoms, with prompt symptom resolution following surgical management. A diagnostic dilemma may arise, as other bladder neck cystic lesions differ in anatomical location, etiology, and the nature of associated LUTS. Case Description: We report a middle-aged male patient with Brunn’s cyst with a brief description of our management strategies and a review of available literature. Conclusions: Brunn’s cyst is a rare but treatable cause of bladder outlet obstruction in young males, with excellent outcomes following transurethral deroofing.Keywords
Supplementary Material
Supplementary Material FileBrunn’s nests are a clump of benign urothelial cells that are trapped in the lamina propria of the bladder, predominantly localized to the bladder neck and trigone regions. Cysts developing from Brunn cells are one of the rarest causes of bladder outlet obstruction in a young healthy male; the first case was elucidated by Israel Franco in 1988.1 Brunn’s nests are congenital formations resulting from the inward folding of normal urothelium into the lamina propria. Brunn’s cysts develop due to inflammation within these nests and can lead to bladder outlet obstruction. We report a 32-year-old gentleman who presented with obstructive lower urinary tract symptoms (LUTS) for 2 years secondary to a Brunn’s cyst, with a brief review of limited published literature.
A 32-year-old male with no comorbidities, and a known case of coronal hypospadias, presented to Safdarjung Hospital, Delhi, with voiding predominant LUTS in the form of straining, poor flow, hesitancy, and a sense of incomplete evacuation. The patient was moderately bothered with an International Prostate Symptom Score (IPSS) of 18. Physical examination was unremarkable except for the coronal hypospadias with a normal digital rectal assessment. Uroflowmetry (UFM) revealed a constrictive pattern with a low maximum flow rate (Qmax) of 3.24 mL/s (Figs. 1A–1B) and significantly high post-void residue (PVR) of 270 mL. Ultrasonographic evaluation revealed a 1.5 × 1.5 cm well-defined cystic lesion at the bladder neck projecting into the bladder base with a prostatic volume of 20 cc and normal upper tracts. Magnetic resonance imaging (MRI) suggested a well-defined multiloculated 16 × 15 mm midline cystic lesion arising from the anterior bladder neck projecting into the prostatic urethra, with a tentative radiological diagnosis of a Brunn’s cyst (Figs. 1C–1E). Other possible differentials considered were the Ectopic or intravesical Ureterocele and the simple bladder wall cysts. Cystoscopic evaluation displayed an isolated occlusive cystic structure seen hanging from the bladder neck at the noon position, protruding into the prostatic urethra and functioning as an obstructive ball valve (Fig. 2A). Both ureteric orifices were normally visualized emitting regular effluxes of urine, with trabeculations seen involving the whole of the bladder. Transurethral deroofing of the cyst revealed a thick-walled cystic lesion with clear intra-cystic fluid as content (Figs. 2B–2D). Per urethral catheter was removed on the first post-operative day, and the patient was discharged on the subsequent day. Histopathology showed urothelial cell nests in glandular patterns, suggestive of Brunn’s nests without dysplasia. Although no intact cyst was retrieved due to transurethral resection, the findings were consistent with Brunn’s cyst. At the 3-month follow-up, obstructive symptoms were resolved, with uroflowmetry showing a Qmax of 19 mL/s (Fig. 1B) with an insignificant post-void residue. The sequence of clinical events, from presentation to follow-up, is outlined chronologically in Table 1.
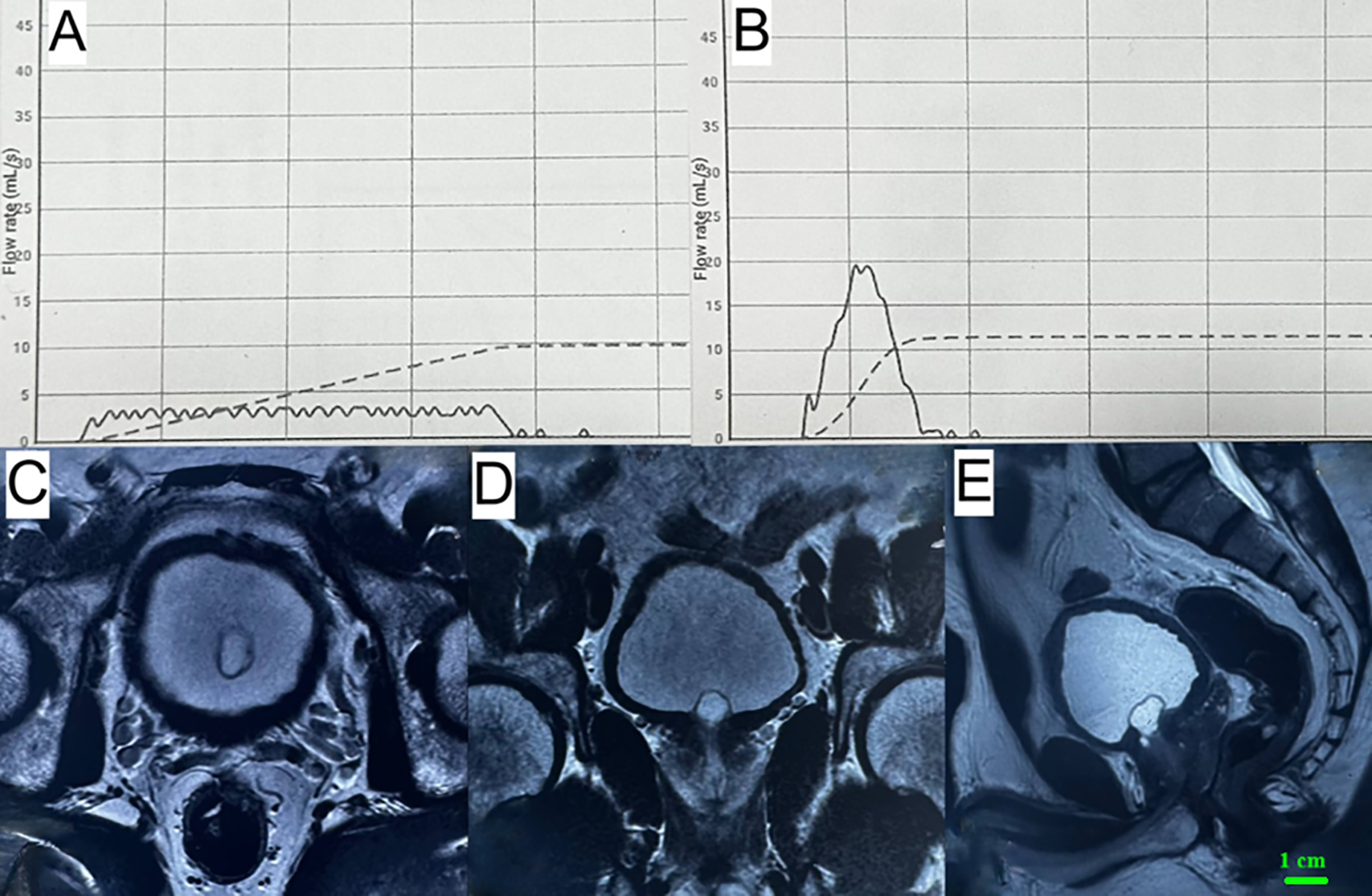
FIGURE 1. Uroflowmetry curves and relevant MRI sections of the patient. (A, B) Pre-Operative and Post-Operative Uroflowmetry Curves. (C–E) MRI Pelvis depicting a cystic lesion at the bladder neck extending to the prostatic urethra, causing evident luminal compromise. (C) Axial, (D) Coronal, and (E) Sagittal
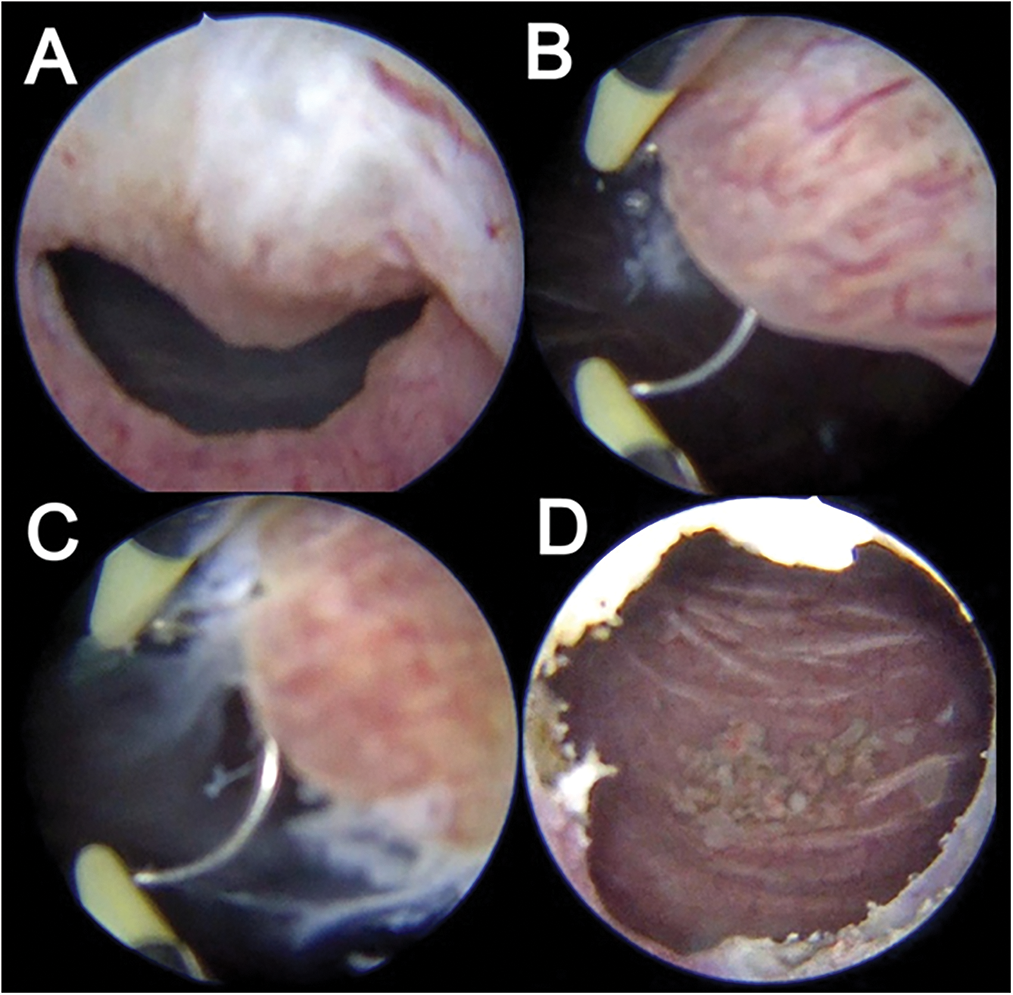
FIGURE 2. Endoscopic findings during resection. (A) Cystoscopic evaluation reveals an occlusive cystic structure seen hanging from the bladder neck at 12 o’clock position, protruding into the prostatic urethra. (B) Depicts images of the deroofing process with Loop cautery. (C) Deroofing of the cyst produces extravasation of clear fluid as cyst content. (D) Post-operative image revealing wide-open bladder neck
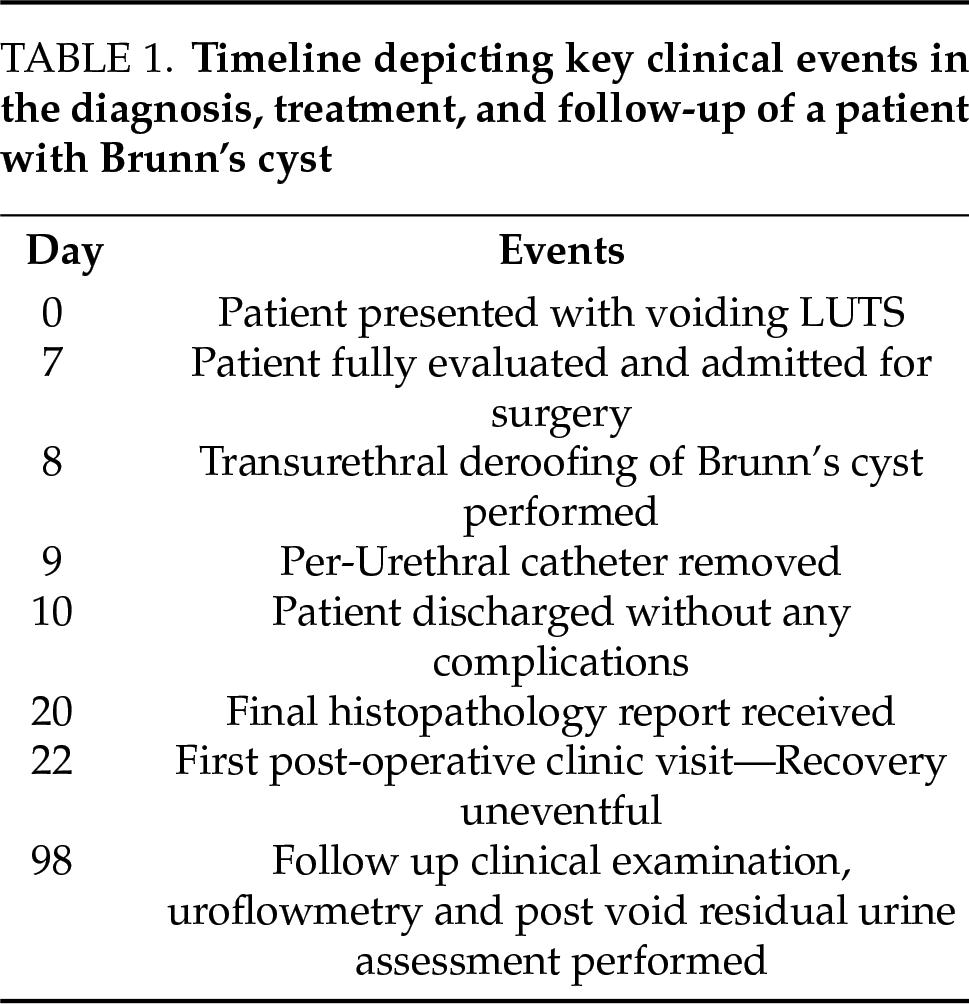
Our case adds to the limited body of literature on bladder neck cysts by highlighting a rare presentation and successful surgical management. A total of eight cases have been reported in the literature, with variable locations of the cyst at the bladder neck (Table 2). The most common site was the noon position,2–4 followed by predominantly left-sided locations between 3 to 6 o’clock and 12 to 3 o’clock,1,5 and right-sided positions between 7 to 11 o’clock.6,7 Based on available previous publications, all patients were male with an average age of 39 years, having at least one symptom of obstructive LUTS (87%). The cysts were mainly located at the noon position with obstructed uroflow curves, revealing a mean Qmax of 7.4 mL/s. All patients were managed surgically with transurethral deroofing and cyst resection, with most having prompt symptom resolution and no recurrence.
Brunn’s nests are thought to be clusters of cells derived from urothelial cells, which become displaced, proliferate, and then form cysts. Our patient demonstrated a similar pathological profile, with
multiple submucosal, cystically dilated von Brunn’s nests and a large cystic structure predominantly lined by denuded epithelium, consistent with a diagnosis of Brunn’s cyst.
It remains unclear why such a cyst has never been reported in females. Various other possible pathologies exist in the differential list of cystic lesions at the bladder neck with ectopic ureteroceles,2 cystitis cystica or glandularis,2 and prostatic cysts,9 forming the major alternatives in the list. Ectopic ureteroceles typically present as cystic formations adjacent to the bladder neck, but the majority are associated with the duplex collecting system and are seen in childhood. Cystitis cystica is characterized by chronic inflammatory changes resulting in cystic lesions, whereas cystitis glandularis represents a form of glandular metaplasia of the urothelium, potentially leading to varying degrees of LUTS. Brunn’s cysts are located at the bladder neck, superior to the prostatic parenchyma, and are commonly associated with LUTS. In contrast, prostatic cysts are mostly incidental to imaging and originate within the prostatic tissue itself. Other causes of LUTS in young males include Diabetes mellitus and generalized anxiety disorders. Diabetic urinary bladder dysfunction, affecting up to 80% of individuals with diabetes, often presents with symptoms like urinary retention and an overactive bladder. LUTS is strongly associated with generalized anxiety, especially in youth, who may face social isolation, teasing, low self-esteem, and psychological distress.5
The mainstay of diagnosing Brunn’s cysts remains ultrasonography and cystoscopic evaluation, with MRI utilized in situations of clinical dilemma. Imaging can effectively differentiate a midline supra prostatic Brunn’s cyst from an intraparenchymal prostatic cyst or a laterally positioned ureterocele near the vesicoureteral junction. Noninvasive alternatives to cystoscopy, such as liquid biopsy using urinary biomarkers, show the potential to distinguish benign from malignant causes. Cystitis cystica can present with inflammatory cells on urine cytology. However, they still need further validation to establish acceptable sensitivity and specificity.10 Transurethral deroofing of the cyst and resection is usually the recognized first line of management. Alternative treatment options include observation in asymptomatic or minimally symptomatic cases, medical management with alpha-adrenergic blockers, transrectal ultrasound (TRUS)-guided aspiration or sclerotherapy for temporary symptom relief, and surgical excision for large or recurrent cysts. In cases where surgical excision is contraindicated or declined by the patient, laser deroofing may be considered a viable alternative. No cases of malignancy have been reported in the follow-up period, implying that long-term follow-up is not necessary, given the benign nature of the disease (Table 2). However, institutional follow-up protocols could be implemented based on symptom questionnaires, uroflowmetry, and imaging. The role of urinary biomarkers represents a future approach to assessing the potential for malignancy. The discussion is constrained by the limited number of reported cases, which restricts the generalizability of observations and limits the ability to establish definitive clinical guidelines. Moreover, the absence of reported cases in females remains unexplained, and the presence of histological ambiguity further complicates diagnosis. Additionally, the lack of standardized follow-up protocols poses a limitation in assessing long-term outcomes.
A Brunn’s cyst, although rare, is an important surgically treatable benign entity in the differential diagnosis of young males presenting with obstructive urinary symptoms. Transurethral deroofing forms the most effective treatment for this entity, with prompt symptom resolution observed post-procedure. The evolution of advanced modalities, such as liquid biopsy for urinary biomarkers, offers a forward-looking perspective on the future of diagnostic trends in urology.
Acknowledgement
None.
Funding Statement
The authors received no specific funding for this study.
Author Contributions
Pawan Vasudeva was the responsible consultant surgeon in charge of the overall care of the patient and on whom the final decision on the patient management rested. Pawan Vasudeva and Harshdeep Singh wrote the first draft of the manuscript. Harshdeep Singh was involved in day-to-day patient care and follow-up. Thiyagarajan Kalaiselvi Aravind provided insight and valuable inputs to the manuscript and was responsible for the typography of the final manuscript draft. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval
As per our national guidelines, ethical clearance is not required for the publication of an anonymous case report; therefore, it was ethical exemption. However, all efforts have been made to ensure the confidentiality of the patient’s details, and informed consent for publication was duly obtained from the patient.
Conflicts of Interest
The authors declare no conflicts of interest to report regarding the present study.
Declaration Statements
This study was conducted under the case report guidelines (CARE), and a completed CARE checklist has been provided (see Supplementary Material for details)
Supplementary Materials
The supplementary material is available online at https://www.techscience.com/doi/10.32604/cju.2025.064435/s1.
List of Abbreviations
| IPSS | International Prostate Symptom Score |
| LUTS | Lower urinary tract symptoms |
| MRI | Magnetic resonance imaging |
| PVR | Post-void residue |
| Qmax | Maximum flow rate |
| TRUS | Transrectal ultrasound |
| UFM | Uroflowmetry |
References
1. Baarimah A, Alsayed A, Yamani A, Aldawsari M, Soliman S. Bladder outlet obstruction secondary to Brunn’s cyst: a rare presentation in young man. Urol Case Rep 2021;38(1):101683. doi:10.1016/j.eucr.2021.101683. [Google Scholar] [PubMed] [CrossRef]
2. Grimsby GM, Tyson MD, Salevitz B, Smith ML, Castle EP. Bladder outlet obstruction secondary to a Brunn’s cyst. Curr Urol 2012;6(1):50–52. doi:10.1159/000338871. [Google Scholar] [PubMed] [CrossRef]
3. Lindner AK, Schachtner G, Aigner F, Biggel S, Horninger W, Pichler R. Brunn’s cyst inducing persistent lower urinary tract symptoms in a young man: a case report. J Endourol Case Rep 2019;5(4):171–173. doi:10.1089/cren.2019.0065. [Google Scholar] [PubMed] [CrossRef]
4. Ren R, McLarty R, Bach PV. Images—A rare case of Brunn’s cyst causing obstructive lower urinary tract symptoms in a young male. Can Urol Assoc J 2020;14(5):E227–8. doi:10.5489/cuaj.6186. [Google Scholar] [PubMed] [CrossRef]
5. Kim D, Cho YM, Song SH. Transurethral resection of an uncommon Brunn’s cyst: a resolution for lower urinary tract symptoms. Urology Video J 2024;22(1):100273. doi:10.1016/j.urolvj.2024.100273. [Google Scholar] [CrossRef]
6. Franco I, Eshghi M, Schutte H, Srinivasan K, Addonizio JC. Bladder neck obstruction secondary to Brunn’s cyst. J Urol 1988;139(1):126–127. doi:10.1016/s0022-5347(17)42316-0. [Google Scholar] [PubMed] [CrossRef]
7. Sailo SL, Sailo L. Brunn’s Cyst: a rare cause of bladder outlet obstruction in a young man. Urol J 2015;12(5):2381. [Google Scholar] [PubMed]
8. Ilyas M, Shafi F, Choh N. Brunn’s cyst: a rare cause of lower urinary tract symptoms. Indian J Urol 2018;34:231–232. [Google Scholar] [PubMed]
9. Chang SG, Hwang IC, Lee JH, Park YK, Lim JW. Infravesical obstruction due to benign intraurethral prostatic cyst. J Korean Med Sci 2003;18(1):125–126. doi:10.3346/jkms.2003.18.1.125. [Google Scholar] [PubMed] [CrossRef]
10. Matuszczak M, Kiljańczyk A, Salagierski M. A liquid biopsy in bladder cancer—The current landscape in urinary biomarkers. Int J Mol Sci 2022;23(15):8597. doi:10.3390/ijms23158597. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF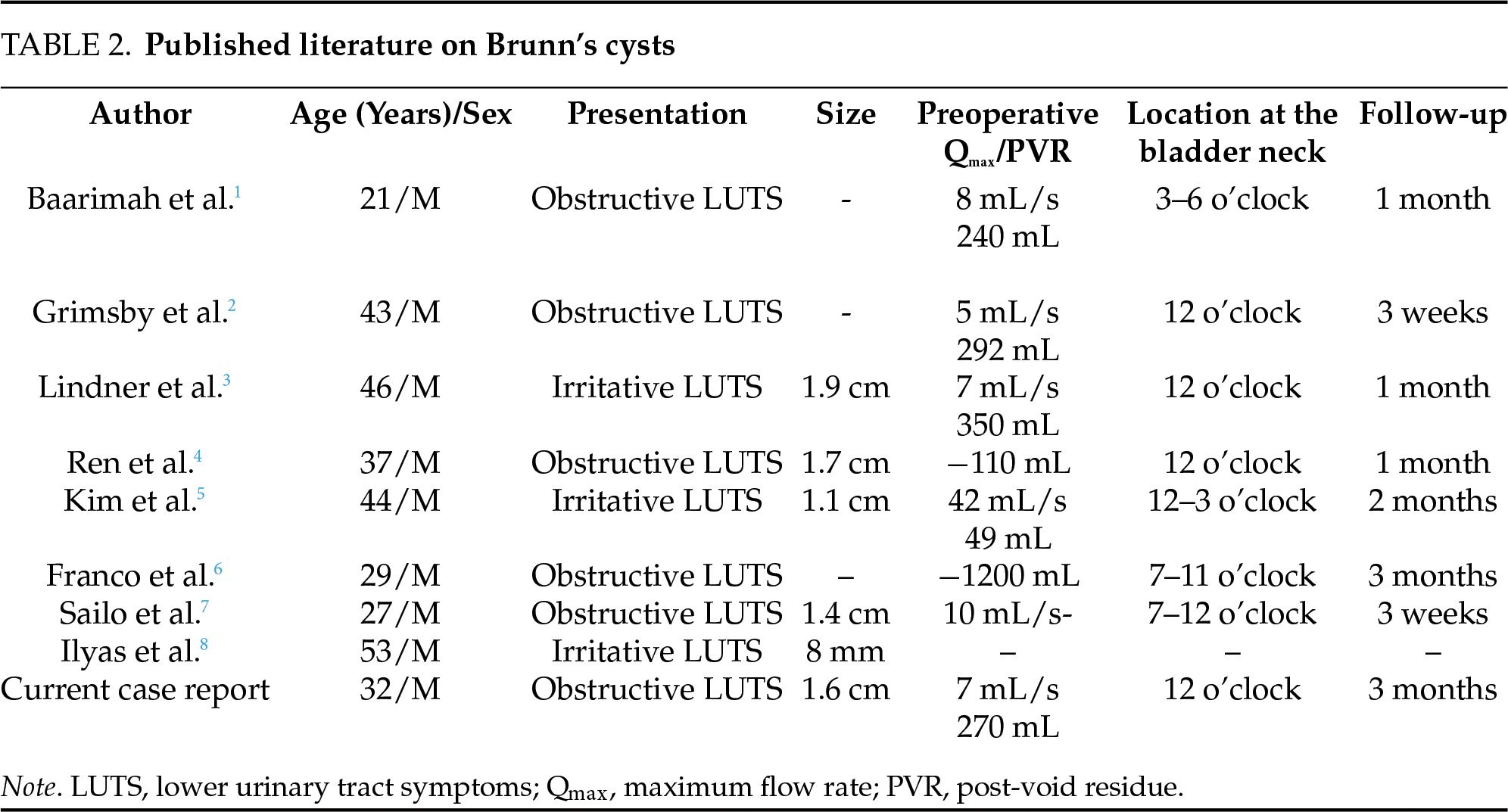
 Downloads
Downloads
 Citation Tools
Citation Tools