 Open Access
Open Access
ARTICLE
The Contribution of BMI, Body Image Inflexibility, and Generalized Anxiety to Symptoms of Eating Disorders and Exercise Dependence in Exercisers
1 Key Laboratory of Adolescent Health Assessment and Exercise Intervention of Ministry of Education, East China Normal University, Shanghai, 200241, China
2 Body-Brain-Mind Laboratory, School of Psychology, Shenzhen University, Shenzhen, 518060, China
3 Research Group Degenerative and Chronic Diseases, Movement, Faculty of Health Sciences Brandenburg, University of Potsdam, Potsdam, 14469, Germany
4 Institute of Health Promotion and Sports Sciences, ELTE Eötvös Loránd University, Budapest, 1053, Hungary
5 School of Rehabilitation, Sport and Psychology, AECC University College, Bournemouth, BH5 2DF, UK
6 School of Medicine and Dentistry, Menzies Health Institute Queensland, Griffith University, Parkland, Gold Coast, QLD, 4222, Australia
* Corresponding Author: Liu Ji. Email:
International Journal of Mental Health Promotion 2022, 24(6), 811-823. https://doi.org/10.32604/ijmhp.2022.024862
Received 10 June 2022; Accepted 10 August 2022; Issue published 28 September 2022
Abstract
1) Background: The common factors which potentially contribute to the development of eating disorders and exercise dependence during early adulthood are still relatively unclear. The present study aimed to examine the role of BMI, body image inflexibility, and generalized anxiety in these two behavioral problems in a sample of college students. 2) Methods: In total, 878 habitual exercisers (58.1% male with BMI = 22.12 ± 2.39; 41.9% female with BMI = 20.55 ± 2.21) with age of 20.09 ± 1.76 years participated in this study. The main outcomes of interest are exercise dependence symptoms, eating disorders symptoms, body image inflexibility, and symptoms of generalized anxiety (as measured by Exercise Dependence Scale-Revised, Eating Disorder Examination-Questionnaire-Short Form, Body Image Acceptance and Action Questionnaire, and Generalized Anxiety Disorder-7, respectively). Pearson correlation, path analysis, and model fit information were tested. 3) Results: After controlling for age, gender, and field of study, lower BMI was linked to more exercise dependence symptoms but this association was not statistically significant, while a greater BMI was significantly associated with a higher risk of developing eating disorders (β = −0.08, p < 0.001). Moreover, higher body image inflexibility significantly and positively contributed to severe exercise dependence (β = 0.26, p < 0.001) as well as abnormal eating attitudes and behaviors (β = 0.74, p < 0.001). Furthermore, generalized anxiety is a significant contributor to exercise dependence symptoms (β = 0.14, p < 0.001) but not eating disorders symptoms. 4) Conclusion: Based on our finding that body image inflexibility is a common risk factor for the development of exercise dependence and eating disorders, the prevention and treatment of these two disorders should involve the improvement of psychological flexibility. In addition, the individual with a higher BMI is more vulnerable to developing eating disorders, while those who have severer generalized anxiety symptoms should be given more attention when screening for exercise dependence.Keywords
Early adulthood (18–29 years) is a unique period of human development from late adolescence to adulthood, in which individuals often start to take more care about their physical appearance (e.g., their body image) [1,2]. Moreover, in this life stage, young adults start to modify their eating and exercise habits [3]. For example, in order to shape their body, some college students attempt to change their physical appearance (appropriate body weight and muscle mass) through extreme behavioral changes such as over-exercising and excessive food restriction [4]. The strongly intertwined behaviors of over-exercising and excessive food restriction [5,6] may increase the risk of developing exercise dependence (EXD) and eating disorders (ED) [7–9]. EXD is a phenomenon that is characterized by uncontrollable excessive engagement in exercise behaviors that negatively affects personal life [10]. For instance, a higher risk of bone fractures and musculoskeletal injuries was found among individuals who engaged in excessive physical exercise [11] while being deprived of the change to do exercise has been associated with withdrawal symptoms (e.g., anxiety and depression), attention deficits and sleep problems in dependent exercisers [10,12]. With regard to ED, it is characterized by severe eating behavior and body image perception disturbances, which affect individual’s body weight and health [13]. Previous investigations into the EXD-ED relationship have mainly focused on levels of comorbidity [14]. However, the shared contributors to developing these two disorders remain largely unknown. To this end, identification of common contributors is urgently needed, so that tailored intervention programs can be designed for these at-risk individuals.
The role of body mass index (BMI) in the development of EXD and ED has been reported in previous studies [15–19]. The evidence concerning a relationship between BMI and EXD is mixed. Some studies observed a negative association between BMI and EXD [15,17], whereas other studies did not reveal such a relationship [20,21]. Regarding ED, the perceived pressure to become thin was increased by the elevated BMI [19]. Those with weight-related pressure and thin-related attitude had a higher risk of developing ED [22–24]. Several studies provided evidence for an association between higher BMI and increased severity of ED symptoms [16,18,19]. In addition, higher BMI has also been linked to greater body dissatisfaction (i.e., a negative attitude towards one’s own physical appearance) and body image inflexibility (BII) (i.e., unwillingness to experience negative appearance-related thoughts and emotions), which reinforce the crucial role of BMI in body perception [25–28].
The body-related attitude was observed as a significant predictor of EXD and ED symptoms [29]. Young adults with BII tend to select physical exercise as one of the readily accessible strategies to change their body image [5,11]. For example, individuals with body image dissatisfaction do regular physical exercise for weight loss and for toning their bodies [30]. This type of exercise motivation can lead to unhealthy exercise behaviours and probably causes feelings of EXD [11]. Body image dissatisfaction often contributes to ED symptoms [31,32]. Since body dissatisfaction, is a widespread phenomenon, which was also called “normative discontent” [33], some authors have started to stress the importance for individuals to develop the ability to adjust the negative feelings about their body and not let them affect their life and well-being by applying body image flexibility [34,35]. Some studies have reported that lower BII (i.e., greater ability to cope with negative appearance-related thoughts and emotions) was associated with better treatment outcomes in interventions dealing with ED [36,37]. Collectively, body-related perception or attitude (e.g., BII) may be predictive of ED and EXD.
Anxiety may be predictive of these co-occurring psychiatric disorders. A relationship between EXD and anxiety level was found among 16-to-68-year-old individuals who exercised for professional purposes and recreation [38]. Dependent exercisers reported withdrawal symptoms (e.g., anxiety and fatigue) when physical exercise was deprived [10]. Furthermore, a recent study by Back et al. [39] aimed to identify psychological risk factors (e.g., obsessive passion, physical appearance, and anxiety) for developing EXD among 330 habitual exercisers recruited from sports clubs, exercise groups, and sport science college students. Results indicated that anxiety was the main predictor of EXD [39]. Likewise, association was also found in ED symptoms and anxiety [40]; lifetime anxiety is common in ED patients [41] and disordered eating women [42]. Some studies indicated that anxiety disorders can precede the onset of ED [43,44]. Concerning generalized anxiety disorders, it was noticed that this type of anxiety is also prevalent in individuals suffering from eating disorders [45,46]. Moreover, in subclinical eating disorders individuals, higher level of generalized anxiety symptoms were observed as compared to individuals who do not suffer from eating disorders [47]. Collectively, this study aimed to determine whether generalized anxiety is an important predictor of developing EXD and ED.
Existing evidence indicates that BMI, BII, and generalized anxiety are independently related to EXD [15,17] and ED [16,18,19]. To date, no studies have comprehensively examined multiple factors including BMI, BII, and generalized anxiety. To fill in this research gap, this study aimed to examine the relative contributions of BMI, BII, and generalized anxiety to symptoms of EXD and ED. We hypothesize that BMI, BII, and generalized anxiety are predictors of both exercise dependence and eating disorder symptoms.
2.1 Participants and Procedure
Participants were recruited from sport universities and sport clubs in universities, from November 28th to December 27th, 2020. Using snowball sampling, the data were collected anonymously through Questionnaire Star via online social media. All participants (N = 1282) had signed their electronic consent before starting questionnaire. To ensure that participants were habitual exercisers, exercise frequency (3 times per week) as a cut-off score was used (recommended by American College of Sports Medicine and American Heart Association) [48]. Participants were excluded if: (i) participants were not university students (n = 82); (ii) participants (n = 322) exercised less than three times a week. Bentler et al. [49] suggested that an adequate sample size should always be 10 times the amount of the free parameters in path analysis. Since the path model consists of 23 free parameters, a total of 230 participant was considered as adequate sample size.
Self-report body weight and height were collected to determine Body Mass Index (kg/m2).
2.2.2 Exercise Dependence Scale-Revised (EDS-R)–Chinese Version (EDS-C)
The EDS-R was used to assess EXD [50]. This scale consists of seven sub-scales: withdrawal effect, continuance, tolerance, lack of control, reduction in other activities, time, and intention effect. Each sub-scale was assessed by three items. Participants responded to each item on a six-point Likert scale ranging from 1 = “never” to 6 = “always”. A total point from 3 to 18 can be obtained for each sub-scale, with higher scores revealing more EXD symptoms. Participants were then classified into three groups: the first was defined as at-risk for exercise dependence (ARED) when they score 15 or higher on at least three sub-scales from the aforementioned 7 sub-scales. The second group is the non-dependent symptomatic (NDS) group which consists of participants who were not classified as ARED but scored larger than seven on more than three sub-scales. The third group consists of participants who are defined as non-dependent-asymptomatic (NDA) because they do not fall into the two aforementioned groups. The scale was translated into Chinese and psychometrically validated [51]. In this study, the total EDS-R score was used for statistical analysis. The reliability of this scale, as reflected by the Cronbach alpha coefficient value, in the present study is 0.94.
2.2.3 Eating Disorder Examination-Questionnaire-Short Form (EDE-QS)
The EDE-QS was used to examine eating attitudes and behaviors in the past seven days [52]. The psychometric properties of the Chinese version of EDE-QS have been investigated in a previous study [53]. This one-dimensional scale contains 12 items examining symptoms of anorexia nervosa, bulimia nervosa, and binge-eating disorder over the past 7 days (e.g., “Has thinking about food, eating or calories made it very difficult to concentrate on things?”). Each item was answered on a four-point Likert scale ranging from 0 to 3. Higher scores indicate greater symptoms of abnormal eating attitudes and behaviors. Cut-off score is 15 for screening purpose [54]. In the present study, the EDE-QS has a value of 0.92 in Cronbach’s alpha coefficient.
2.2.4 Body Image Acceptance and Action Questionnaire (BI-AAQ)
The BI-AAQ was used to measure body image flexibility [35]. In this study, we used the Chinese version of the BI-AAQ provided and validated by He and Colleagues [55]. This one-dimensional scale includes 12 items (e.g., “worrying about my weight makes it difficult for me to live a life that I value”). Each item was answered on a seven-point Likert scale ranging from 1 (“never true”) to 7 (“always true”). A higher score indicates higher body image inflexibility. The BI-AAQ achieved an excellent Cronbach’s alpha coefficient (alpha = 0.96).
2.2.5 Generalized Anxiety Disorder (GAD-7)
The GAD-7 was used to measure generalized anxiety symptoms [56]. In the present study, the validated Chinese version of the GAD-7 was used [57]. This one-dimensional scale includes 7 items (e.g., “not being able to stop or control worrying”). Each item was answered on a four-point Likert scale ranging from 1 (“never”) to 7 (“nearly every day”). A greater score indicates a higher level of anxiety. The Cronbach’s alpha coefficient of GAD-7 in this sample achieved 0.93.
SPSS version 25 (IBM, Chicago, IL) was used to perform data analysis. First, descriptive statistics were calculated for all study variables. Second, the prevalence of people at risk for EXD and probable ED cases were examined, and chi-square analysis was performed to determine difference across different types of disorders (EXD and ED). Third, the Pearson correlation test was conducted to examine possible relationships between all continuous variables. Then, demographics (age, gender, and field of study) being correlated with main outcomes of interest were controlled for further path analysis (95% CI) within Mplus 8.0 [58]; three independent variables (BMI, BII, and generalized anxiety), and two dependent variables (EXD and ED symptoms). Finally, model fit information was calculated. The criteria to determine a good model fit are: a Tucker-Lewis’s Index (TLI) ≥ 0.95; a comparative fit index (CFI) ≥ 0.95; root mean square error approximation (RMSEA) ≤ 0.05 [59]. For all statistical tests, the level of significance was set to α = 0.05.
Participants who were invited to participate in this study were asked to provide their electronic consent through the online survey tool before filling in the questionnaire. All participants who filled out the survey were compensated for their efforts with 5 RMB. The study protocol was approved by the Ethic Committee of Shenzhen University (No. PN-2020-038).
3.1 Descriptive Statistics of Participants
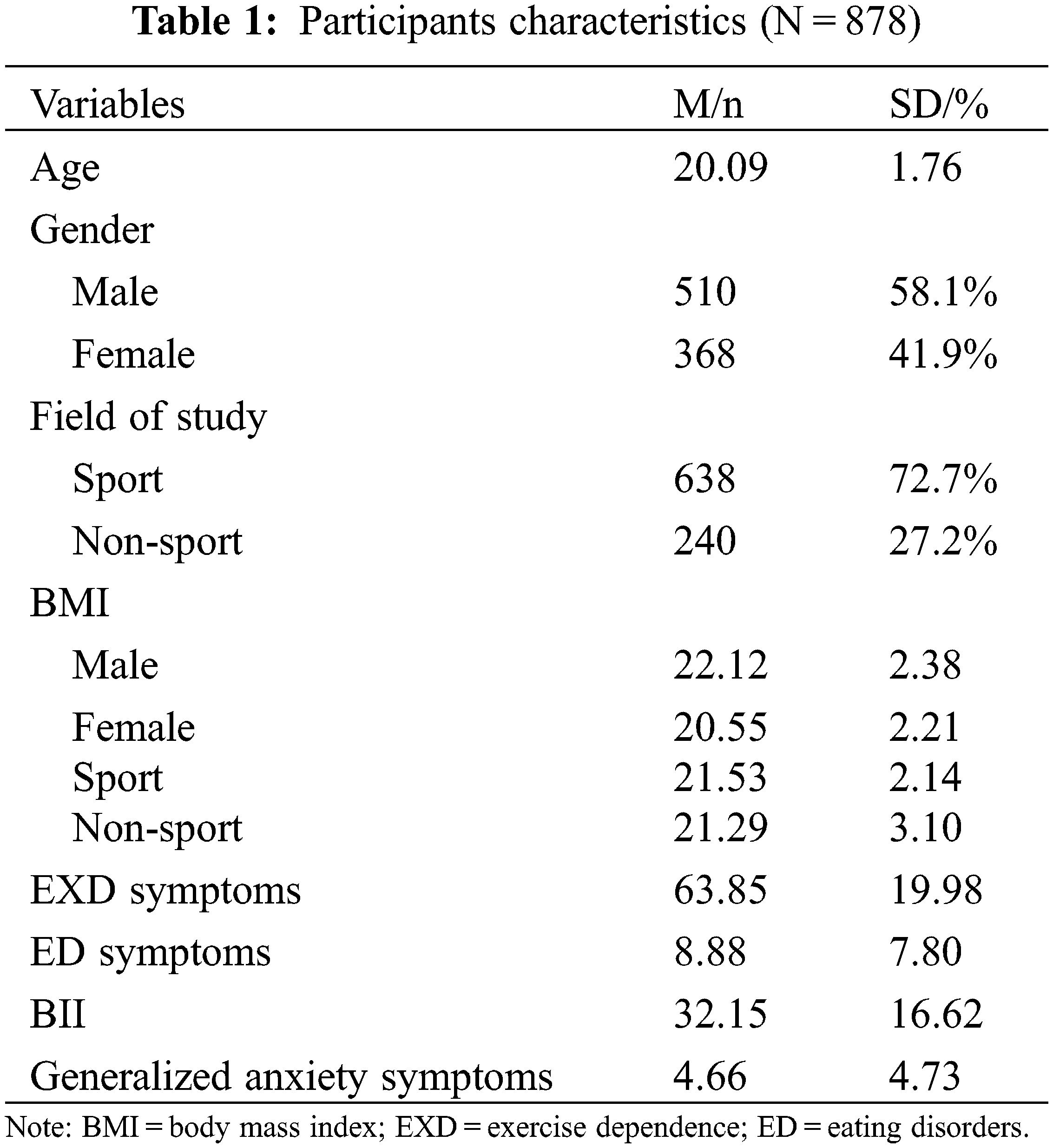
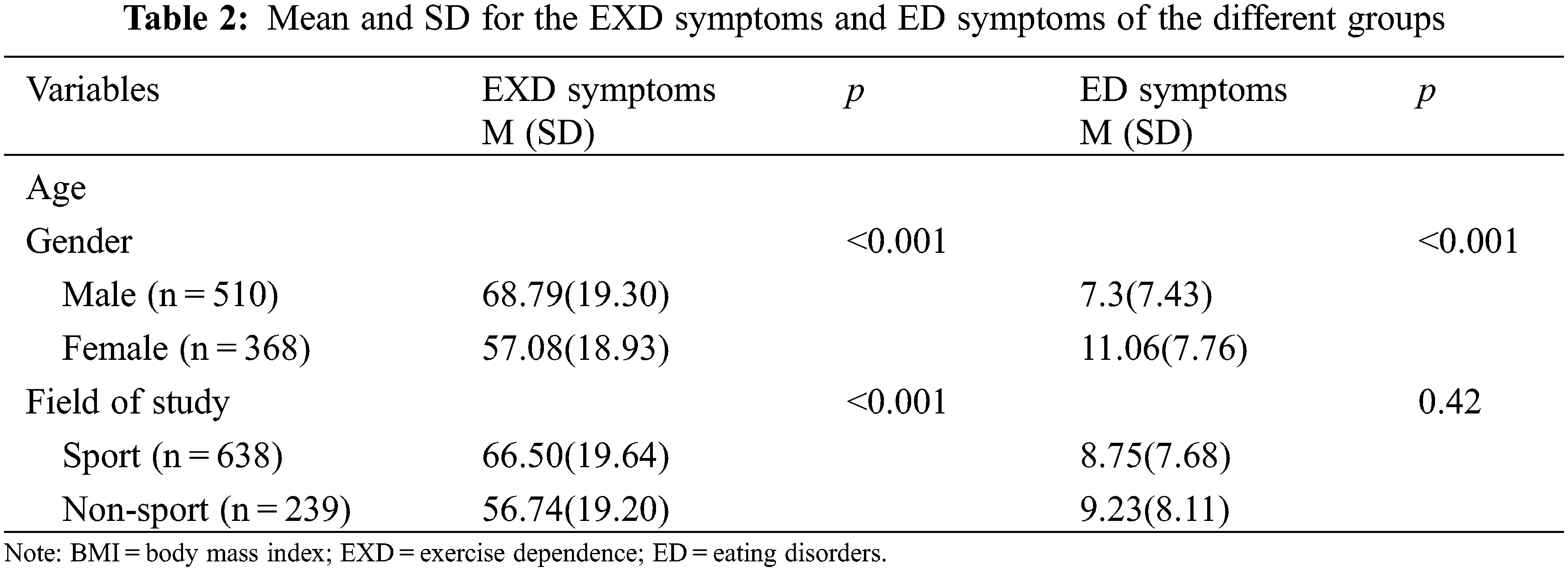
Data from 878 participants were used for statistical analyses (58.1% male). The age of college students ranged from 18 to 25 (M = 20.09, SD = 1.76). The descriptive statistics for demographic data on age, gender, BMI (computed from self-reported height and weight), and field of study, are presented in Table 1. Concerning two dependent variables, males scored significantly higher in EXD symptoms (68.79 vs. 57.08) compared to their female counterparts, whereas females showed significantly higher scores in ED symptoms as compared to male counterparts (see Table 2).
3.2 Prevalence of EXD Symptoms and ED Symptoms, and Group Differences
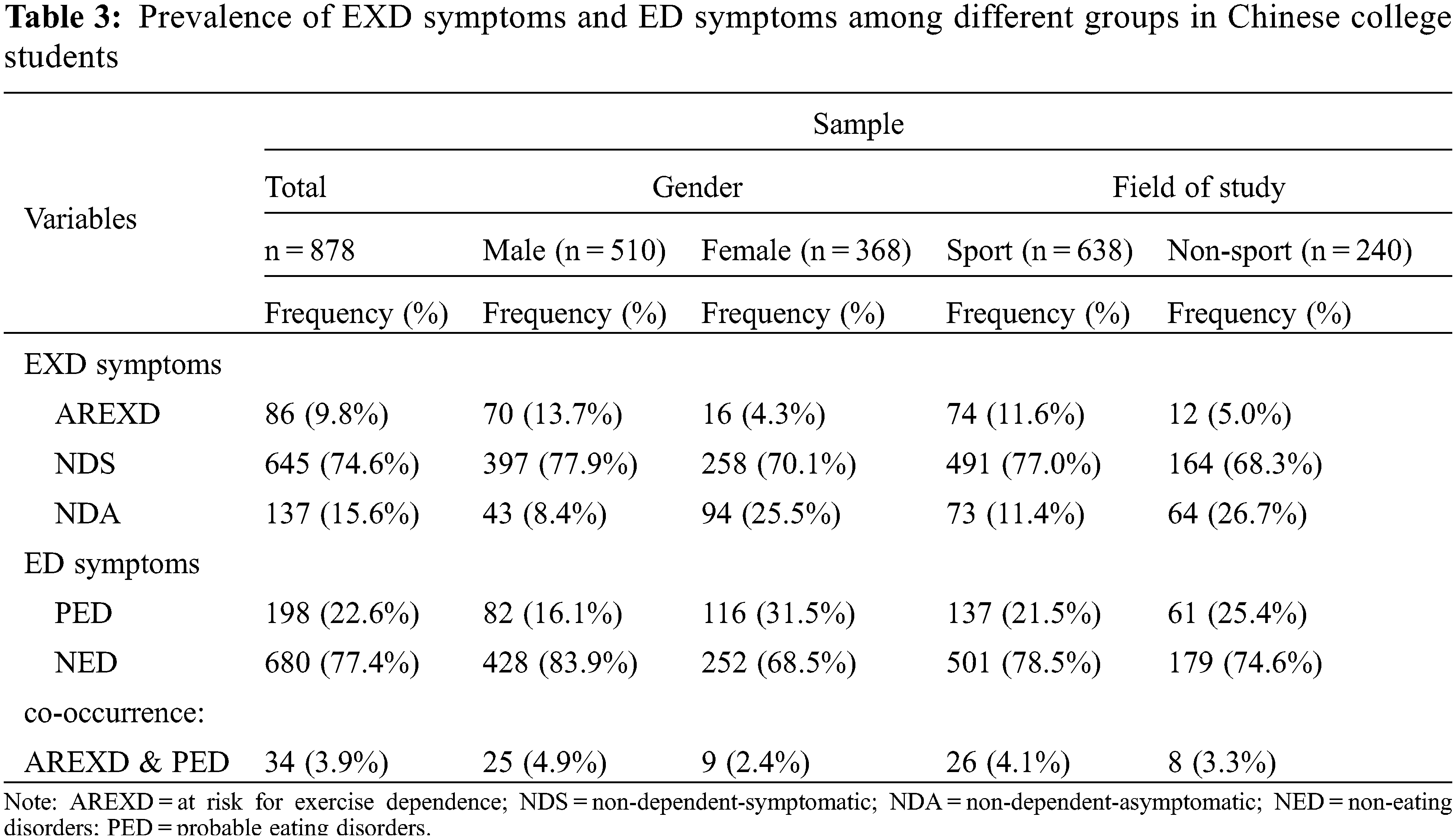
In Table 3, AREXD accounts for 9.8% of the whole sample, while NDS and NDA groups were 74.6% and 15.6%, respectively. Additionally, 22.6% of whole sample were screened as probably having an ED. Concerning the prevalence among different groups, male showed a highest prevalence of ARED and NDS, while non-sport students reported highest prevalence of NDA. Moreover, female showed a highest prevalence of probable ED, while male reported a highest prevalence of non-ED. Results of chi-square analysis showed that ED categories differed by probable ED cases (x2 [2, 878] = 16.67, p = 0.000) in the whole sample and four sub-groups (x2 [2, 510] = 24.35, p = 0.000; x2 [2, 368] = 8.60, p = 0.014; x2 [2, 638] = 13.05, p = 0.001; x2 [2, 240] = 11.28, p = 0.004, for male, female, sport, non-sport group, respectively).
3.3 Correlations Between BMI, BII, Generalized Anxiety Symptoms, EXD Symptoms, and ED Symptoms
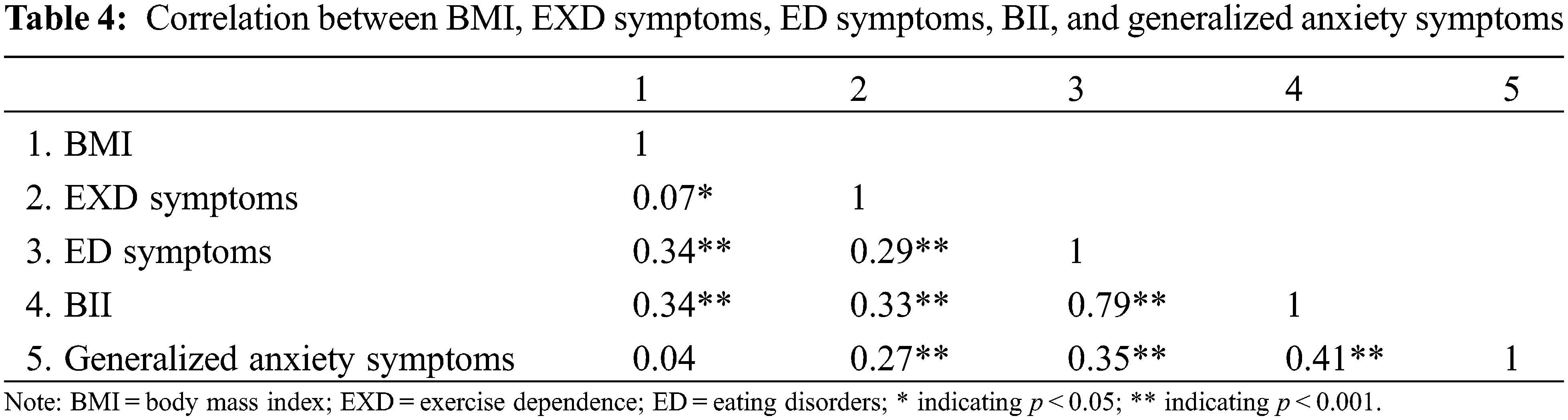
Results from correlation analysis are reported in Table 4. After controlling for age, gender, and field of study, a non-significant anxiety-BMI relationship was observed, whereas other two variables were significantly correlated, with r values ranging from 0.07 to 0.79.
3.4 Results from Path Analysis
Results from the path analysis (see Table 5) in terms of EXD symptoms are presented below: BMI was not a significant predictor with a path coefficient of β = −0.04 (SE = 0.03, p = 0.26), whereas BII with a path coefficient of β = 0.26 (SE = 0.03, p < 0.001) and anxiety with a path coefficient of β = 0.14 (SE = 0.03, p < 0.001) were significantly predictive of EXD symptoms. While looking into ED symptoms, BMI with a path coefficient of β = 0.08 (SE = 0.02, p < 0.001) and BII with a path coefficient of β = 0.74 (SE = 0.02, p < 0.001) were observed as two significant predictors, whereas anxiety was not predictive of ED symptoms with a path coefficient of β = 0.02 (SE = 0.02, p = 0.43). Visual results are presented in Fig. 1. When controlled variables were not included in the model, model fit information showed a good fit (x2(df = 2) = 10.15; TLI = 0.97; CFI = 0.99; RMSEA = 0.03).
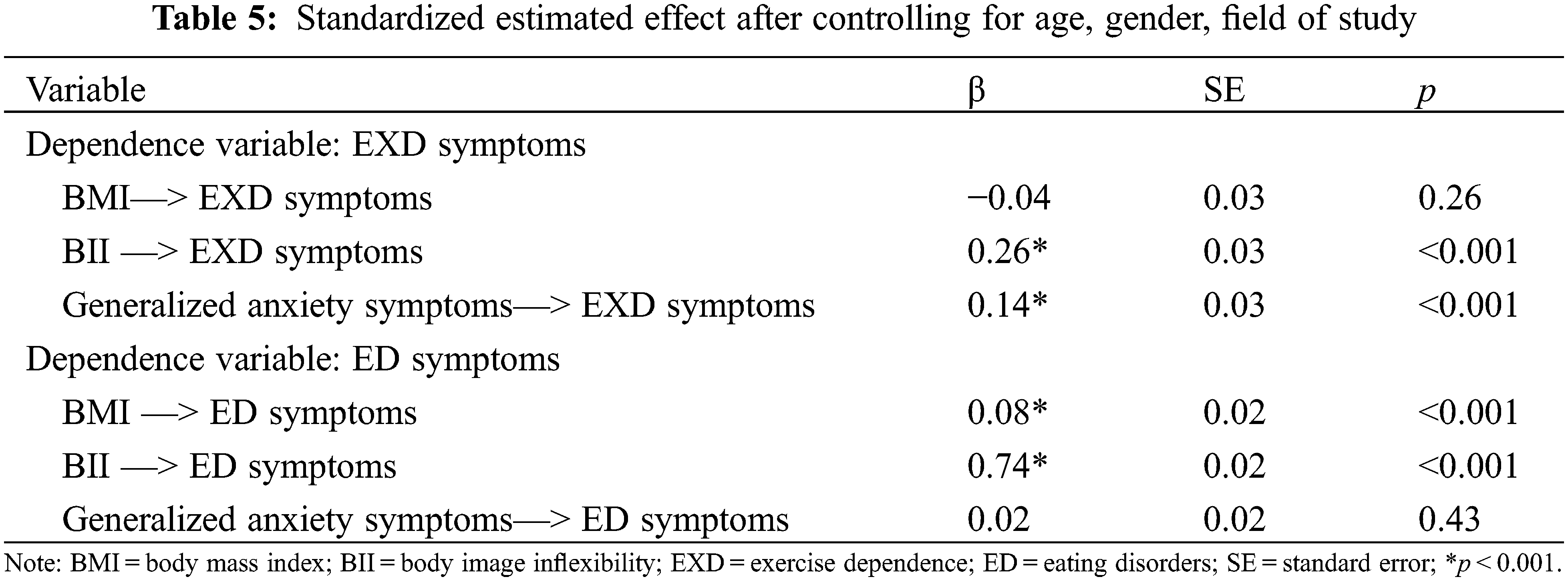
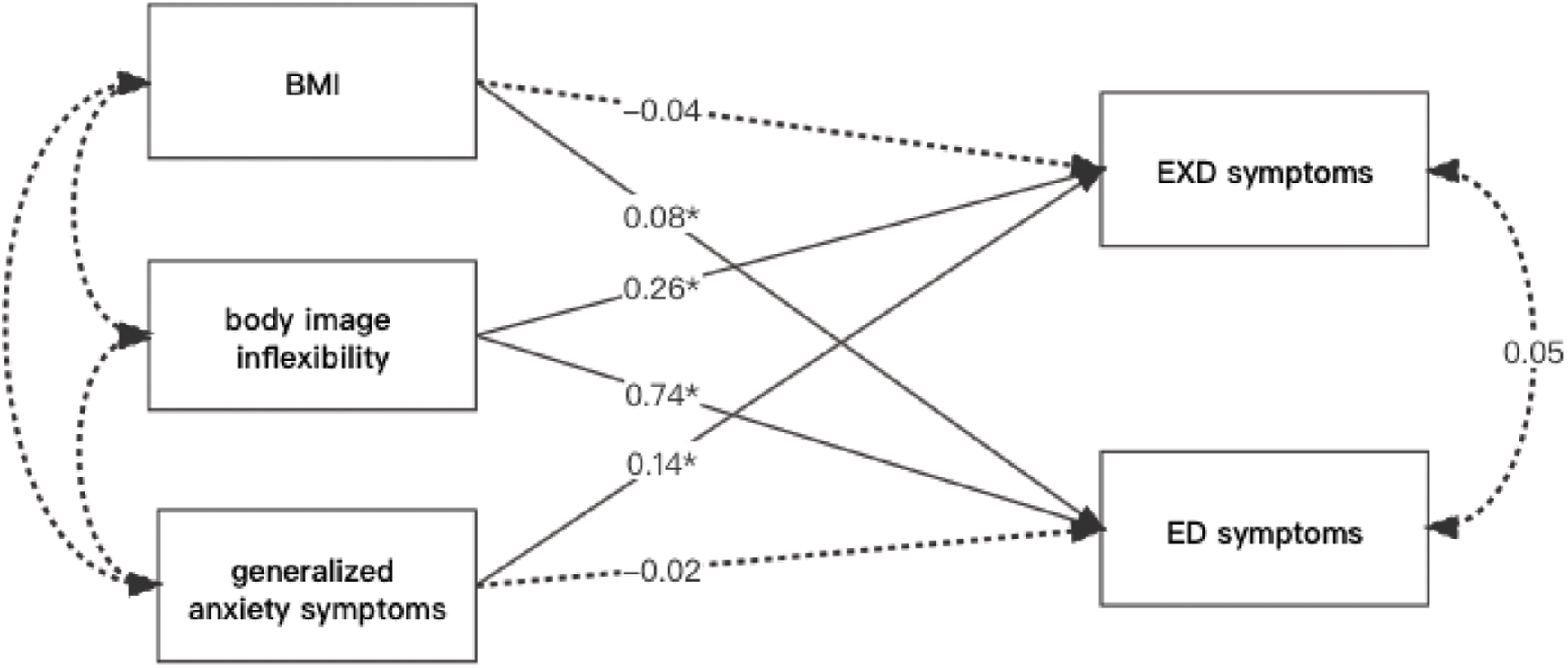
Figure 1: Standardized regression coefficients for associations of BMI, BII, and generalized anxiety symptoms with two disorders (EXD symptoms and ED symptoms) when controlled age, gender, field of study (*p < 0.001)
This study aimed to examine whether BMI, BII, and generalized anxiety were common contributors for the development of EXD and ED in a sample of Chinese university students. Male participants were found to be more likely to develop EXD in comparison to their female counterparts. Female participants tended to have a greater likelihood of developing ED. College students majoring in sports science were more likely to develop EXD in comparison to non-sport participants. These results are in line with previous studies [60,61]. In the present study, the prevalence of ARED was 9.8%, while NDS has the highest proportion 74.6%, which is supported by previous studies of similar age-based samples [50,62]. The prevalence of ED among college students was relatively high in the present study (22.6%), which may be attributed to habitual exercisers paying great attention to their body image to achieve an ideal image through extremely restrictive eating habits [63,64]. The prevalence of co-existing disorders was approximately 4% in the present study. In this context, the prevalence rate for participants who were comorbidity accounted for 17.2% (34 out of 198) in the probable eating disordered sample, which is comparatively lower than the previous studies that ranged from 29% to 80% [65,66].
The findings of our analysis considering important confounders (i.e., age, sex, and field of study) suggest (i) that BII and generalized anxiety are potential risk factors for developing EXD, and (ii) that BMI and BII are predictive of ED symptoms. The findings of the present study are, in general, consistent with observations of previous studies reporting that BMI alone is not a strong predictor of EXD [20,21]. Interestingly, BII was predictive of EXD, suggesting that the perception of their own body (i.e., operationalized by BII) is an important factor relating to EXD. Previous findings indicate that individuals with higher BMI are more likely to experience body image dissatisfaction and BII [25–28,67]. Furthermore, given that physical fitness and physical exercise are, in general, associated with a better perception of their own body image [68,69], body image dissatisfaction and BII might trigger individuals to exercise for weight loss and for toning their bodies (e.g., in obese individuals) [70] or to achieve their “ideal” body image (e.g., in exercise addicted individuals) [11]. Such results may be explained by the fact that in the present study, participants were habitual exercisers with an average BMI of 21 kg/m2 (normal BMI). However, the complex relationship between exercise behavior, body perception (e.g., body image inflexibility), and EXD is not fully understood and further research using high-quality trials is needed to confirm this conclusion [10,71–73].
Our findings are relatively consistent with the previous studies reporting that higher BMI was linked to a higher risk for ED [16,18,19]. Our results also confirmed previous studies’ results that BII is positively associated with ED [35,74]. The finding of our study suggests that individuals with higher BMI have a higher risk of disturbed eating attitudes and behaviors. Furthermore, individuals who had already a low level of BII were more likely to develop ED symptoms. Additionally, in the present study, participants with a higher level of anxiety had a greater probability of developing EXD. These results may be explained by the fact that anxious college students are more likely to consider exercise participation as an effective approach to alleviating anxiety.
5 Contributions of the Current Study
Our findings that provide evidence for a relationship between BII and both EXD symptoms and ED symptoms support the idea that BII plays an important role in the development and thus might also in the prevention of the aforementioned disorders. The results in our study showing statistically significant differences in ED scores and EXD scores of sports students and general students who exercise regularly may inform further mechanistic studies that psychological processes may be associated with EXD as well as ED symptoms in different groups (i.e., athletes vs. general exercisers). Consequently, the findings of the current study contribute to a more nuanced theoretical understanding of EXD and ED.
6 Limitations and Implications
Several limitations need to be acknowledged. Firstly, as all measures rely on self-reports of the participants, they are somewhat prone to measurement error that arises from self-report bias (e.g., as participants provide socially acceptable answers). Furthermore, it should be noted that although BMI is a popular way to measure body composition [75], it has some disadvantages [76]. In particular, BMI is biased because this measure does not take into account the difference between muscle mass and fat mass [77,78], and thus a higher muscle mass, which is, in general, positive for health, will lead to higher BMI scores which are, in general, associated with adverse health outcomes. Secondly, the participants of the present study comprise only university students who were more concerned about their physical appearance as compared to older adults who may be more concerned with their work and family life. Thus, future studies should focus on other cohorts than college students, to test whether our findings can be generalized. In addition, in this study, the number of participants in the non-sport students’ group was relatively small which also challenges the generalizability of the findings. Thirdly, this study focuses on BII as one of the predictors while other possible variables such as self-compassion (i.e., the ability to protect oneself from developing negative body image as well as disturbing eating habits) [79,80], perfectionism personality, and obsessive-compulsive personality disorder (due to their essential role in the development of both exercise dependence [81,82] and eating disorders symptoms) [83,84] were not considered. Finally, the cross-sectional design of this study does not allow the examination of causality and the direction of the pathways. Thus, longitudinal studies are needed to examine causal relationships in the future.
In conclusion, the present study revealed that BII and generalized anxiety are contributing factors to EXD, but not BMI. In addition, BMI and BII can be predictive of ED symptoms. Based on this finding, BMI alone does not appear to be a good predictor of EXD, whereas BII is a joint predictor of EXD symptoms and ED symptoms in this sample of Chinese college students. From a practical point of view, our findings suggest that the prevention and treatment of EXD symptoms and ED symptoms should consider interventions to improve the individual’s attitude towards the perception of their own body by addressing BII.
Funding Statement: The information should be replaced with "This project was supported by China Postdoctoral Science Foundation (No: 2022M711174).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Arnett, J. J. (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469–480. DOI 10.1037/0003-066X.55.5.469. [Google Scholar] [CrossRef]
2. Kuang, J., Zhong, P., Yang, P., Bo, X., Liang Y. et al. (2022). Psychometric evaluation of the inventory of dimensions of emerging adulthood (IDEA) in China. International Journal of Clinical and Health Psychology. DOI 10.1016/j.ijchp.2022.100331. [Google Scholar] [CrossRef]
3. Nelson, M. C., Story, M., Larson, N. I., Neumark-Sztainer, D., Lytle, L. A. (2008). Emerging adulthood and college-aged youth: An overlooked age for weight-related behavior change. Obesity, 16(10), 2205–2211. DOI 10.1038/oby.2008.365. [Google Scholar] [CrossRef]
4. Kevin, T. J. (2001). Body image, eating disorders, and obesity in youth: Assessment, prevention, and treatment. USA: Taylor & Francis. [Google Scholar]
5. Furnham, A., Badmin, N., Sneade, I. (2002). Body image dissatisfaction: Gender differences in eating attitudes, self-esteem, and reasons for exercise. The Journal of Psychology, 136(6), 581–596. DOI 10.1080/00223980209604820. [Google Scholar] [CrossRef]
6. Shroff, H., Reba, L., Thornton, L. M., Tozzi, F., Klump, K. L. et al. (2006). Features associated with excessive exercise in women with eating disorders. International Journal of Eating Disorders, 39(6), 454–461. DOI 10.1002/(ISSN)1098-108X. [Google Scholar] [CrossRef]
7. Dunn, E. C., Larimer, M. E., Neighbors, C. (2002). Alcohol and drug-related negative consequences in college students with bulimia nervosa and binge eating disorder. International Journal of Eating Disorders, 32(2), 171–178. DOI 10.1002/(ISSN)1098-108X. [Google Scholar] [CrossRef]
8. Eisenberg, D., Nicklett, E. J., Roeder, K., Kirz, N. E. (2011). Eating disorder symptoms among college students: Prevalence, persistence, correlates, and treatment-seeking. Journal of American College Health, 59(8), 700–707. DOI 10.1080/07448481.2010.546461. [Google Scholar] [CrossRef]
9. Oberle, C. D., Watkins, R. S., Burkot, A. J. (2018). Orthorexic eating behaviors related to exercise addiction and internal motivations in a sample of university students. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 23(1), 67–74. DOI 10.1007/s40519-017-0470-1. [Google Scholar] [CrossRef]
10. Hausenblas, H. A., Downs, D. S. (2002). Exercise dependence: A systematic review. Psychology of Sport and Exercise, 3(2), 89–123. DOI 10.1016/S1469-0292(00)00015-7. [Google Scholar] [CrossRef]
11. Landolfi, E. (2013). Exercise addiction. Sports Medicine, 43(2), 111–119. DOI 10.1007/s40279-012-0013-x. [Google Scholar] [CrossRef]
12. Bamber, D. J., Cockerill, I. M., Rodgers, S., Carroll, D. (2003). Diagnostic criteria for exercise dependence in women. British Journal of Sports Medicine, 37(5), 393–400. DOI 10.1136/bjsm.37.5.393. [Google Scholar] [CrossRef]
13. Schmidt, U., Adan, R., Bohm, I., Campbell, I. C., Dingemans, A. (2016). Eating disorders: The big issue. The Lancet Psychiatry, 3(4), 313–315. DOI 10.1016/S2215-0366(16)00081-X. [Google Scholar] [CrossRef]
14. Trott, M., Jackson, S. E., Firth, J., Jacob, L., Grabovac, I. (2021). A comparative meta-analysis of the prevalence of exercise addiction in adults with and without indicated eating disorders. Eating and weight disorders-studies on anorexia. Bulimia and Obesity, 26(1), 37–46. [Google Scholar]
15. Allegre, B., Therme, P., Griffiths, M. (2007). Individual factors and the context of physical activity in exercise dependence: A prospective study of ‘ultra-marathoners’. International Journal of Mental Health and Addiction, 5(3), 233–243. DOI 10.1007/s11469-007-9081-9. [Google Scholar] [CrossRef]
16. Kelly, A. C., Vimalakanthan, K., Miller, K. E. (2014). Self-compassion moderates the relationship between body mass index and both eating disorder pathology and body image flexibility. Body Image, 11(4), 446–453. DOI 10.1016/j.bodyim.2014.07.005. [Google Scholar] [CrossRef]
17. Maceri, R. M., Cherup, N. P., Buckworth, J., Hanson, N. J. (2019). Exercise addiction in long distance runners. International Journal of Mental Health and Addiction, 19 (1), 62–71. DOI 10.1007/s11469-019-00122-0. [Google Scholar] [CrossRef]
18. Neumark-Sztainer, D., Falkner, N., Story, M., Perry, C., Hannan, P. J. et al. (2002). Weight-teasing among adolescents: Correlations with weight status and disordered eating behaviors. International Journal of Obesity, 26(1), 123–131. DOI 10.1038/sj.ijo.0801853. [Google Scholar] [CrossRef]
19. Stice, E. (2002). Risk and maintenance factors for eating pathology: A meta-analytic review. Psychological Bulletin, 128(5), 825–848. DOI 10.1037/0033-2909.128.5.825. [Google Scholar] [CrossRef]
20. Mayolas-Pi, C., Simon-Grima, J., Penarrubia-Lozano, C., Munguia-Izquierdo, D., Moliner-Urdiales, D. (2016). Exercise addiction risk and health in male and female amateur endurance cyclists. Journal of Behavioral Addictions, 6(1), 74–83. DOI 10.1556/2006.6.2017.018. [Google Scholar] [CrossRef]
21. Gun, A., Agirbas, O. (2019). The relationship between exercise addiction, physical activity level and body mass index of the students who Are studying at physical education and sports college. Asian Journal of Education and Training, 5(1), 50–55. DOI 10.20448/journal.522. [Google Scholar] [CrossRef]
22. Piran, N., Thompson, S. (2008). A study of the adverse social experiences model to the development of eating disorders. International Journal of Health Promotion and Education, 46(2), 65–71. DOI 10.1080/14635240.2008.10708131. [Google Scholar] [CrossRef]
23. Puhl, R., Suh, Y. (2015). Stigma and eating and weight disorders. Current Psychiatry Reports, 17(3), 1–10. DOI 10.1007/s11920-015-0552-6. [Google Scholar] [CrossRef]
24. Thompson, J. K., Stice, E. (2001). Thin-ideal internalization: Mounting evidence for a new risk factor for body-image disturbance and eating pathology. Current Directions in Psychological Science, 10(5), 181–183. DOI 10.1111/1467-8721.00144. [Google Scholar] [CrossRef]
25. Eidsdottir, S. T., Kristjansson, A. L., Sigfusdottir, I. D., Garber, C. E., Allegrante, J. P. (2014). Association between higher BMI and depressive symptoms in Icelandic adolescents: The mediational function of body image. The European Journal of Public Health, 24(6), 888–892. DOI 10.1093/eurpub/ckt180. [Google Scholar] [CrossRef]
26. Streeter, V. M., Milhausen, R. R., Buchholz, A. C. (2012). Body image, body mass index, and body composition: In young adults. Canadian Journal of Dietetic Practice and Research, 73(2), 78–83. DOI 10.3148/73.2.2012.78. [Google Scholar] [CrossRef]
27. Sujoldžić, A., de Lucia, A. (2007). A cross-cultural study of adolescents–BMI, body image and psychological well-being. Collegium Antropologicum, 31(1), 123–130. [Google Scholar]
28. Wendell, J. W., Masuda, A., Le, J. K. (2012). The role of body image flexibility in the relationship between disordered eating cognitions and disordered eating symptoms among non-clinical college students. Eating Behaviors, 13(3), 240–245. DOI 10.1016/j.eatbeh.2012.03.006. [Google Scholar] [CrossRef]
29. Mendes, A. L., Coimbra, M., Canavarro, M. C., Ferreira, C. (2022). The powerful effect of body image inflexibility on the explanation of eating psychopathology severity. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 27(3), 961–968. DOI 10.1007/s40519-021-01233-1. [Google Scholar] [CrossRef]
30. Liu, H. Y., Chang, C. C., Gill, D. L., Wu, S. C., Lu, F. J. H. (2019). Male weight trainers’ body dissatisfaction and exercise dependence: Mediating role of muscularity drive. Psychological Reports, 122(6), 2137–2154. DOI 10.1177/0033294118805010. [Google Scholar] [CrossRef]
31. Brannan, M. E., Petrie, T. A. (2008). Moderators of the body dissatisfaction-eating disorder symptomatology relationship: Replication and extension. Journal of Counseling Psychology, 55(2), 263–275. DOI 10.1037/0022-0167.55.2.263. [Google Scholar] [CrossRef]
32. Corning, A. F., Krumm, A. J., Smitham, L. A. (2006). Differential social comparison processes in women with and without eating disorder symptoms. Journal of Counseling Psychology, 53(3), 338–349. DOI 10.1037/0022-0167.53.3.338. [Google Scholar] [CrossRef]
33. Rodin, J., Silberstein, L., Striegel-Moore, R. (1984). Women and weight: A normative discontent. In: Nebraska symposium on motivation. USA: University of Nebraska Press. [Google Scholar]
34. Masuda, A., Price, M., Anderson, P. L., Wendell, J. W. (2010). Disordered eating-related cognition and psychological flexibility as predictors of psychological health among college students. Behavior Modification, 34(1), 3–15. DOI 10.1177/0145445509351569. [Google Scholar] [CrossRef]
35. Sandoz, E. K., Smith, B. M., Twohig, M. P., Lensegrav-Benson, T., Quakenbush-Roberts, B. (2013). Assessment of body image flexibility: The body image-acceptance and action questionnaire. Journal of Contextual Behavioral Science, 2(1–2), 39–48. DOI 10.1016/j.jcbs.2013.03.002. [Google Scholar] [CrossRef]
36. Bluett, E., Lee, E. B., Simone, M., Lockhart, G., Twohig, M. P. (2016). The role of body image psychological flexibility on the treatment of eating disorders in a residential facility. Eating Behaviors, 23, 150–155. DOI 10.1016/j.eatbeh.2016.10.002. [Google Scholar] [CrossRef]
37. Lee, E. B., Ong, C. W., Twohig, M. P., Lensegrav-Benson, T., Quakenbush-Roberts, B. (2018). Increasing body image flexibility in a residential eating disorder facility: Correlates with symptom improvement. Eating Disorders, 26(2), 185–199. DOI 10.1080/10640266.2017.1366229. [Google Scholar] [CrossRef]
38. Weinstein, A., Maayan, G., Weinstein, Y. (2015). A study on the relationship between compulsive exercise, depression and anxiety. Journal of Behavioral Addictions, 4(4), 315–318. DOI 10.1556/2006.4.2015.034. [Google Scholar] [CrossRef]
39. Back, J., Josefsson, T., Ivarsson, A., Gustafsson, H. (2019). Psychological risk factors for exercise dependence. International Journal of Sport and Exercise Psychology, 19 (4), 461–472. DOI 10.1080/1612197X.2019.1674902. [Google Scholar] [CrossRef]
40. Rowe, R., Pickles, A., Simonoff, E., Bulik, C. M., Silberg, J. L. (2002). Bulimic symptoms in the virginia twin study of adolescent behavioral development: Correlates, comorbidity, and genetics. Biological Psychiatry, 51(2), 172–182. DOI 10.1016/S0006-3223(01)01257-4. [Google Scholar] [CrossRef]
41. Godart, N., Perdereau, F., Rein, Z., Berthoz, S., Wallier, J. (2007). Comorbidity studies of eating disorders and mood disorders. Critical review of the literature. Journal of Affective Disorders, 97(1–3), 37–49. DOI 10.1016/j.jad.2006.06.023. [Google Scholar] [CrossRef]
42. Gadalla, T., Piran, N. (2008). Psychiatric comorbidity in women with disordered eating behavior: A national study. Women & Health, 48(4), 467–484. DOI 10.1080/03630240802575104. [Google Scholar] [CrossRef]
43. Godart, N. T., Flament, M. F., Curt, F., Perdereau, F., Lang, F. (2003). Anxiety disorders in subjects seeking treatment for eating disorders: A DSM-IV controlled study. Psychiatry Research, 117(3), 245–258. DOI 10.1016/S0165-1781(03)00038-6. [Google Scholar] [CrossRef]
44. Bulik, C. M. (2002). Anxiety, depression and eating disorders. In: Eating disorders and obesity: A comprehensive handbook, vol. 2, no. 1, pp. 193–198. [Google Scholar]
45. Pallister, E., Waller, G. (2008). Anxiety in the eating disorders: Understanding the overlap. Clinical Psychology Review, 28(3), 366–386. DOI 10.1016/j.cpr.2007.07.001. [Google Scholar] [CrossRef]
46. Kaye, W. H., Bulik, C. M., Thornton, L., Barbarich, N., Masters, K. (2004). Comorbidity of anxiety disorders with anorexia and bulimia nervosa. American Journal of Psychiatry, 161(12), 2215–2221. DOI 10.1176/appi.ajp.161.12.2215. [Google Scholar] [CrossRef]
47. Touchette, E., Henegar, A., Godart, N. T., Pryor, L., Falissard, B. (2011). Subclinical eating disorders and their comorbidity with mood and anxiety disorders in adolescent girls. Psychiatry Research, 185(1–2), 185–192. DOI 10.1016/j.psychres.2010.04.005. [Google Scholar] [CrossRef]
48. Haskell, W. L., Lee, I. M., Pate, R. R., Powell, K. E., Blair, S. N. et al. (2007). Physical activity and public health: Updated recommendation for adults from the American college of sports medicine and the American heart association. Circulation, 116(9), 1081–1093. DOI 10.1161/CIRCULATIONAHA.107.185649. [Google Scholar] [CrossRef]
49. Bentler, P. M., Chou, C. P. (1987). Practical issues in structural modeling. Sociological Methods & Research, 16(1), 78–117. DOI 10.1177/0049124187016001004. [Google Scholar] [CrossRef]
50. Downs, D. S., Hausenblas, H. A., Nigg, C. R. (2004). Factorial validity and psychometric examination of the exercise dependence scale-revised. Measurement in Physical Education and Exercise Science, 8(4), 183–201. DOI 10.1207/s15327841mpee0804_1. [Google Scholar] [CrossRef]
51. Yang, P. (2021). Validation of the Chinese version of the exercise dependence scale-revised (EDS-R). International Journal of Mental Health and Addiction, 1–20. DOI 10.1007/s11469-021-00654-4. [Google Scholar] [CrossRef]
52. Gideon, N., Hawkes, N., Mond, J., Saunders, R., Tchanturia, K. et al. (2016). Development and psychometric validation of the EDE-QS, a 12-item short form of the eating disorder examination questionnaire (EDE-Q). PLoS One, 11(5), e0152744. DOI 10.1371/journal.pone.0152744. [Google Scholar] [CrossRef]
53. He, J., Sun, S., Fan, X. (2020). Validation of the 12-item short form of the eating disorder examination questionnaire in the Chinese context: Confirmatory factor analysis and rasch analysis. Eating and Weight Disorders-Studies on Anorexia Bulimia and Obesity, 26 (1), 201–209. DOI 10.1007/s40519-019-00840-3. [Google Scholar] [CrossRef]
54. Prnjak, K., Mitchison, D., Griffiths, S., Mond, J., Gideon, N. et al. (2020). Further development of the 12-item EDE-QS: Identifying a cut-off for screening purposes. BMC Psychiatry, 20(1), 146–146. DOI 10.1186/s12888-020-02565-5. [Google Scholar] [CrossRef]
55. He, J., Cai, Z. H., Chen, X. J., Lu, T., Fan, X. T. (2020). Validation of the Chinese version of the body image acceptance and action questionnaire and the mediating role of body image flexibility in the relationship between body dissatisfaction and psychological distress. Behavior Therapy, 52(3), 539–551. DOI 10.1016/j.beth.2020.07.003. [Google Scholar] [CrossRef]
56. Spitzer, R. L., Kroenke, K., Williams, J. B. W., Lowe, B. (2006). A brief measure for assessing generalized anxiety disorder-The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. DOI 10.1001/archinte.166.10.1092. [Google Scholar] [CrossRef]
57. Wang, Y., Chen, R., Zhang, L. (2018). Reliability and validity of generalized anxiety scale-7 in inpatients in Chinese general hospital. Journal of Clinical Psychiatry, 28, 168–171. [Google Scholar]
58. Muthén, B., Muthén, B. O. (2009). Statistical analysis with latent variables, vol. 123, no. 6. USA: Wiley. [Google Scholar]
59. Kline, R. B. (2015). Principles and practice of structural equation modeling. USA: Guilford Publications. [Google Scholar]
60. Condello, G. (2016). Physical activity and health perception in aging: Do body mass and satisfaction matter? A three-path mediated link. PLoS One, 11(9), e0160805. DOI 10.1371/journal.pone.0160805. [Google Scholar] [CrossRef]
61. Szabo, A., Griffiths, M. D. (2007). Exercise addiction in British sport science students. International Journal of Mental Health and Addiction, 5(1), 25–28. DOI 10.1007/s11469-006-9050-8. [Google Scholar] [CrossRef]
62. Meulemans, S., Pribis, P., Grajales, T., Krivak, G. (2014). Gender differences in exercise dependence and eating disorders in young adults: A path analysis of a conceptual model. Nutrients, 6(11), 4895–4905. DOI 10.3390/nu6114895. [Google Scholar] [CrossRef]
63. Nergiz-Unal, R., Bilgiç, P., Yabancı, N. (2014). High tendency to the substantial concern on body shape and eating disorders risk of the students majoring nutrition or sport sciences. Nutrition Research and Practice, 8(6), 713–718. DOI 10.4162/nrp.2014.8.6.713. [Google Scholar] [CrossRef]
64. Harris, N., Gee, D., D’Acquisto, D., Ogan, D., Pritchett, K. (2015). Eating disorder risk, exercise dependence, and body weight dissatisfaction among female nutrition and exercise science university majors. Journal of Behavioral Addictions, 4(3), 206–209. DOI 10.1556/2006.4.2015.029. [Google Scholar] [CrossRef]
65. Bratland-Sanda, S., Martinsen, E. W., Rosenvinge, J. H., Ro, O., Hoffart, A. et al. (2011). Exercise dependence score in patients with longstanding eating disorders and controls: The importance of affect regulation and physical activity intensity. European Eating Disorders Review, 19(3), 249–255. DOI 10.1002/erv.971. [Google Scholar] [CrossRef]
66. Dalle Grave, R., Calugi, S., Marchesini, G. (2008). Compulsive exercise to control shape or weight in eating disorders: Prevalence, associated features, and treatment outcome. Comprehensive Psychiatry, 49(4), 346–352. DOI 10.1016/j.comppsych.2007.12.007. [Google Scholar] [CrossRef]
67. Hausenblas, H. A., Fallon, E. A. (2002). Relationship among body image, exercise behavior, and exercise dependence symptoms. International Journal of Eating Disorders, 32(2), 179–185. DOI 10.1002/(ISSN)1098-108X. [Google Scholar] [CrossRef]
68. Campbell, A., Hausenblas, H. A. (2009). Effects of exercise interventions on body image: A meta-analysis. Journal of Health Psychology, 14(6), 780–793. DOI 10.1177/1359105309338977. [Google Scholar] [CrossRef]
69. Martin, K. A., Lichtenberger, C. M. (2002). Fitness enhancement and body image change. In: Body image: A handbook of theory, research, and clinical practice, pp. 414–421. USA: Guilford Press. [Google Scholar]
70. McDonald, K., Thompson, J. K. (1992). Eating disturbance, body image dissatisfaction, and reasons for exercising: Gender differences and correlational findings. International Journal of Eating Disorders, 11(3), 289–292. DOI 10.1002/(ISSN)1098-108X. [Google Scholar] [CrossRef]
71. Adams, J. (2009). Understanding exercise dependence. Journal of Contemporary Psychotherapy, 39(4), 231–240. DOI 10.1007/s10879-009-9117-5. [Google Scholar] [CrossRef]
72. Gonçalves Baptista, J., Costa Filho, P. N., Faria Porretti, M., do Espírito-Santo, G., Assis, M., et al. (2019). Exercise dependence: An updated systematic review. Journal of Exercise Physiology Online, 22(5), 105–125. [Google Scholar]
73. Marques, A., Peralta, M., Sarmento, H., Loureiro, V., Gouveia, E. R. et al. (2019). Prevalence of risk for exercise dependence: A systematic review. Sports Medicine, 49(2), 319–330. DOI 10.1007/s40279-018-1011-4. [Google Scholar] [CrossRef]
74. Pellizzer, M. L., Waller, G., Wade, T. D. (2018). Body image flexibility: A predictor and moderator of outcome in transdiagnostic outpatient eating disorder treatment. International Journal of Eating Disorders, 51(4), 368–372. DOI 10.1002/eat.22842. [Google Scholar] [CrossRef]
75. Burniat, W., Cole, T. J., Lissau, I., Poskitt, E. M. (2006). Child and adolescent obesity: Causes and consequences, prevention and management. [Google Scholar]
76. Larsen, J. K., Ouwens, M., Engels, R. C. M. E., Eisinga, R., van Strien, T. (2008). Validity of self-reported weight and height and predictors of weight bias in female college students. Appetite, 50(2–3), 386–389. DOI 10.1016/j.appet.2007.09.002. [Google Scholar] [CrossRef]
77. Kvist, H. (1988). Total and visceral adipose-tissue volumes derived from measurements with computed tomography in adult men and women: Predictive equations. The American Journal of Clinical Nutrition, 48(6), 1351–1361. DOI 10.1093/ajcn/48.6.1351. [Google Scholar] [CrossRef]
78. Baumgartner, R. N., Heymsfield, S. B., Roche, A. F. (1995). Human body composition and the epidemiology of chronic disease. Obesity Research, 3(1), 73–95. DOI 10.1002/j.1550-8528.1995.tb00124.x. [Google Scholar] [CrossRef]
79. Wasylkiw, L., MacKinnon, A. L., MacLellan, A. M. (2012). Exploring the link between self-compassion and body image in university women. Body Image, 9(2), 236–245. DOI 10.1016/j.bodyim.2012.01.007. [Google Scholar] [CrossRef]
80. Ferreira, C., Pinto-Gouveia, J., Duarte, C. (2013). Self-compassion in the face of shame and body image dissatisfaction: Implications for eating disorders. Eating Behaviors, 14(2), 207–210. DOI 10.1016/j.eatbeh.2013.01.005. [Google Scholar] [CrossRef]
81. Hausenblas, H. A., Giacobbi Jr, P. R. (2004). Relationship between exercise dependence symptoms and personality. Personality and Individual Differences, 36(6), 1265–1273. DOI 10.1016/S0191-8869(03)00214-9. [Google Scholar] [CrossRef]
82. Goodwin, H., Haycraft, E., Willis, A. M., Meyer, C. (2011). Compulsive exercise: The role of personality, psychological morbidity, and disordered eating. International Journal of Eating Disorders, 44(7), 655–660. DOI 10.1002/eat.20902. [Google Scholar] [CrossRef]
83. Anderluh, M. B., Tchanturia, K., Rabe-Hesketh, S., Treasure, J. (2003). Childhood obsessive-compulsive personality traits in adult women with eating disorders: Defining a broader eating disorder phenotype. American Journal of Psychiatry, 160(2), 242–247. DOI 10.1176/appi.ajp.160.2.242. [Google Scholar] [CrossRef]
84. Hewitt, P. L., Flett, G. L., Ediger, E. (1995). Perfectionism traits and perfectionistic self-presentation in eating disorder attitudes, characteristics, and symptoms. International Journal of Eating Disorders, 18(4), 317–326. DOI 10.1002/(ISSN)1098-108X. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2022 The Author(s). Published by Tech Science Press.
Copyright © 2022 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools