 Open Access
Open Access
ARTICLE
Medical Students’ Views on Psychiatry in Germany and Italy: Survey
1 Department of Psychiatry, Faculty of Medicine, University of British Columbia, Vancouver, Canada
2 Department of Neuropsychiatry, Tanta University, Tanta, 31511, Egypt
3 Department of Psychiatry, University of Leipzig, Leipzig, 04109, Germany
4 Azienda Ospedaliera Universitaria Pisana Health, Universitaria Pisana, Pisa, 56126, Italy
* Corresponding Author: Andy Man Yeung Tai. Email:
International Journal of Mental Health Promotion 2023, 25(9), 985-993. https://doi.org/10.32604/ijmhp.2023.030087
Received 22 March 2023; Accepted 26 April 2023; Issue published 10 August 2023
Abstract
Objectives: In 2019, the Insititue for Health Metrics and Evaluation reported that 16% of life lost were attributed to mental health. As a result, global shortage of psychiatrists is a pressing issue due to the increasing burden of mental illness. In 2016, a mere 5% of US medical students chose psychiatry as a career, a trend mirrored in Germany and Italy. As the medical students of 2016 have graduated or transitioned into residency in 2023, their attitudes towards psychiatry could have contributed to today’s shortage of psychiatrists. The global mental health burden has only been exacerbated by the COVID-19 pandemic. This study explores the attitudes of German and Italian medical students towards psychiatry, their career aspirations, and the influence of factors such as personal experience and education on their interest in the field. Methods: A cross-sectional survey was conducted among 799 medical students in two European countries in 2016. Participants answered questions about their attitudes towards psychiatry, their psychiatric education, and personal experiences. Inferential analyses were performed using chi-square tests and a significance level of 0.05. Results: The number of years in medical school, personal experiences, and perceived quality of education significantly affected specialty choice and ranking of psychiatry compared to other specialties. Internships, psychiatric placements, and views on psychiatric instructors also played a significant role in choosing psychiatry as a career. Conclusions: Assessing medical students’ attitudes towards psychiatry and the factors that influence their career choices, such as psychiatric education and personal experiences, can inform changes to attract students to the field. Addressing the worldwide shortage of psychiatrists is crucial to reduce the burden of mental health and substance use disorders.Keywords
Supplementary Material
Supplementary Material FileThe global shortage of psychiatrists is a major concern, as nearly half of the world’s population had access to less than one psychiatrist per 100,000 people in 2014 [1]. Even in highly developed European countries psychiatrists are scarce and the availability of psychiatrists differs significantly between countries. This is reflected in the psychiatrists per 100,000 citizens in a country, as reported by the World Health Organization in 2022. As of 2022, there are 5.9 to 48 psychiatrists in European countries per 100,000 citizens [2]. This extensive range of availabilities in psychiatrist results in unmet needs in the field of mental health and reflect the inhomogeneous global landscape of psychiatry. The shortage of psychiatrist is more severe than shortages faced in virtually any other specialty [3]. The enormous demand for psychiatrists, combined with the increasing burden of mental illness worldwide, has increased the number of untreated individuals experiencing mental illness. With estimated 970 million people globally with mental illness in 2019, an estimated number of half of these individuals are treated in first world countries [4]. The COVID-19 pandemic has further worsened this [5]. The demand for psychiatric services is expected to exceed the psychiatrist supply in 2025 by over 15,400 full-time equivalents (FTE) psychiatrists [4]. This shortage of psychiatrists is also described as “the recruitment crisis” [6].
In Europe, the literature suggests that general attitudes towards psychiatry among medical students are positive at the beginning of their medical school training [7]. However, these positive attitudes decline throughout medical school [8,9]. This deterioration has been partially attributed to how psychiatry is presented throughout education. For example, psychiatry is sometimes reported as a “symptom-based pseudo-scientific discipline”, with other fields offered as more scientific, prestigious, or of greater medical significance [10]. Such influence throughout medical school may also result in students not pursuing volunteer opportunities such as internships, research rotations, or clerkships in psychiatry, all of which have been reported to boost students’ interests in particular disciplines [11].
The skepticism towards the discipline’s validity, misrepresentation of patients, unclear responsibilities and treatment outcomes, the stigma associated with mental illness, and its perceived lower status within the medical field and general society are a few reasons for this critical position, which vary across countries and even medical schools [12]. There also exists financial aspects, where salaries in child and adolescent psychiatry are not competitive with other specialties [13]. Cultural factors can also affect personal experience through one’s familial environment and educational background, such as the explicit attitudes of teachers [14].
Moreover, personal experience with mental health among students has been shown to influence their attitudes towards psychiatry in that students exposed to mental health problems seem to have more positive attitudes towards psychiatry [12]. Being more familiar with psychiatry, perhaps through educational or personal experiences with mental health specialists, may contribute to individuals feeling more interested, curious, and comfortable learning about psychiatry and treating psychiatric patients [13]. For instance, having a family member or close friend experiencing health issues could result in individuals being more sympathetic towards psychiatric illness and patients and, therefore, having a more positive outlook on the discipline [15]. It has been reported that having a family member who is a psychiatrist can also attract individuals to the field by serving as a role model and mentor while also lowering the risk of stigma and prejudice [14].
Given the increasing global burden of mental health disorders, especially in youth, combined with the existing shortage of psychiatrists internationally, there is a need to attract more medical students to psychiatry. This would cause a higher demand for education in psychiatry and subsequently catalyze solutions to address. Since positive attitudes towards psychiatry correlates with an increased intention to pursue psychiatry as a career [16], a first step in addressing the recruitment crisis in psychiatry is understanding which factors affect students’ attitudes towards the discipline.
To address this situation and stimulate the discussion in the field, this study aims to ask German and Italian medical students about their attitudes towards psychiatry, their intentions to pursue psychiatry as a career, and the role of different factors such as personal experience and education on their interest in psychiatry. We hypothesize significant associations between German and Italian medical school students’ attitudes towards psychiatry and their educational and personal experiences with psychiatry.
In total, 1131 individuals participated in the survey. However, 332 students (29%) did not complete any questions after the demographic section and were not included in this study. This is hypothesized to be attributed to attrition from the online questionnaire, which is common in literature [17]. After removing this subsample, 799 participants were included in the analyses. Within this primary data set of 799 students, missing data varied at 7.9% (n = 63). Missing data in the primary data set was ignored, as approximately 5% (n = 40) of missing data can be deemed inconsequential [18].
Participant demographics and descriptive statistics
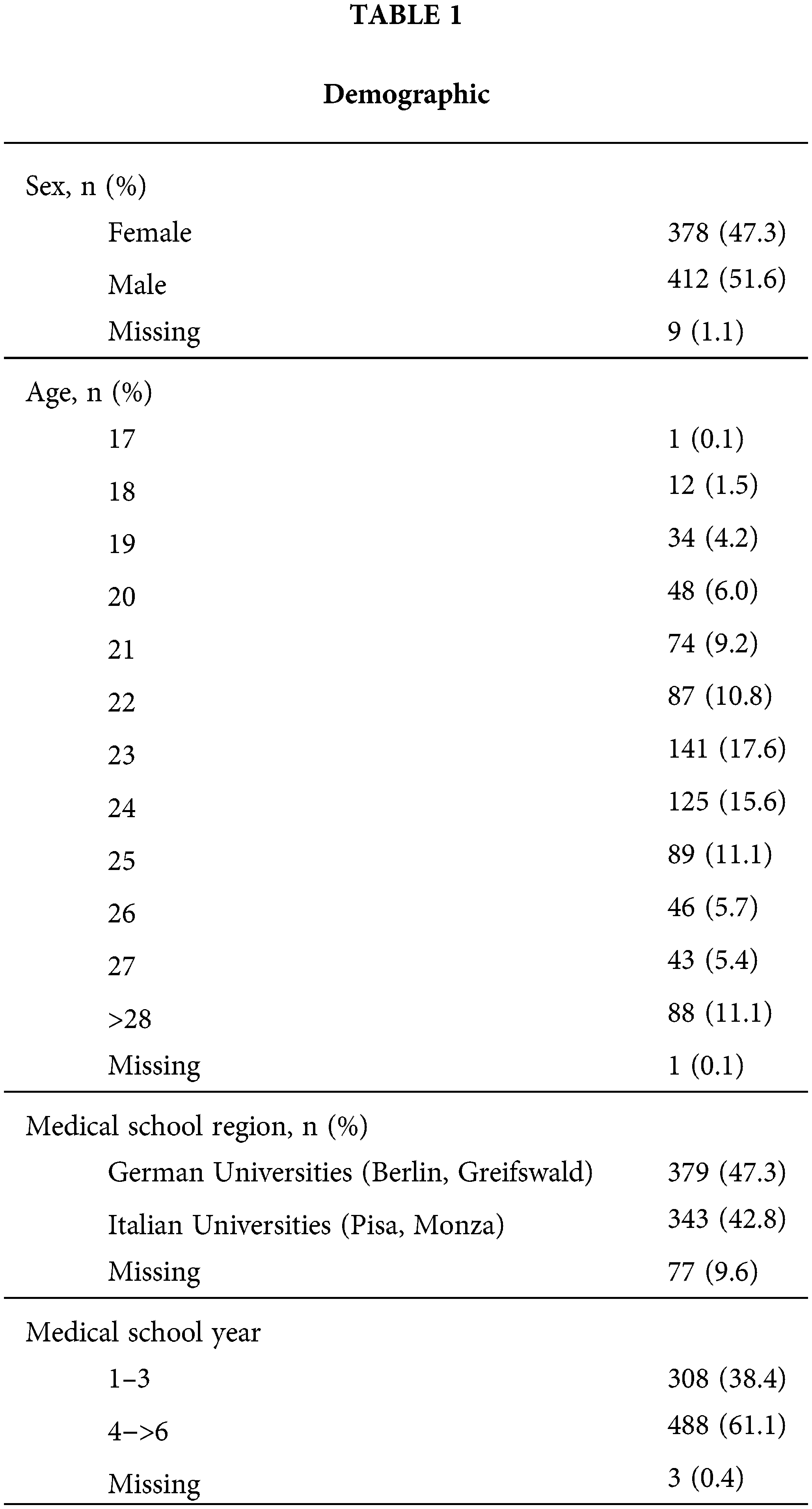
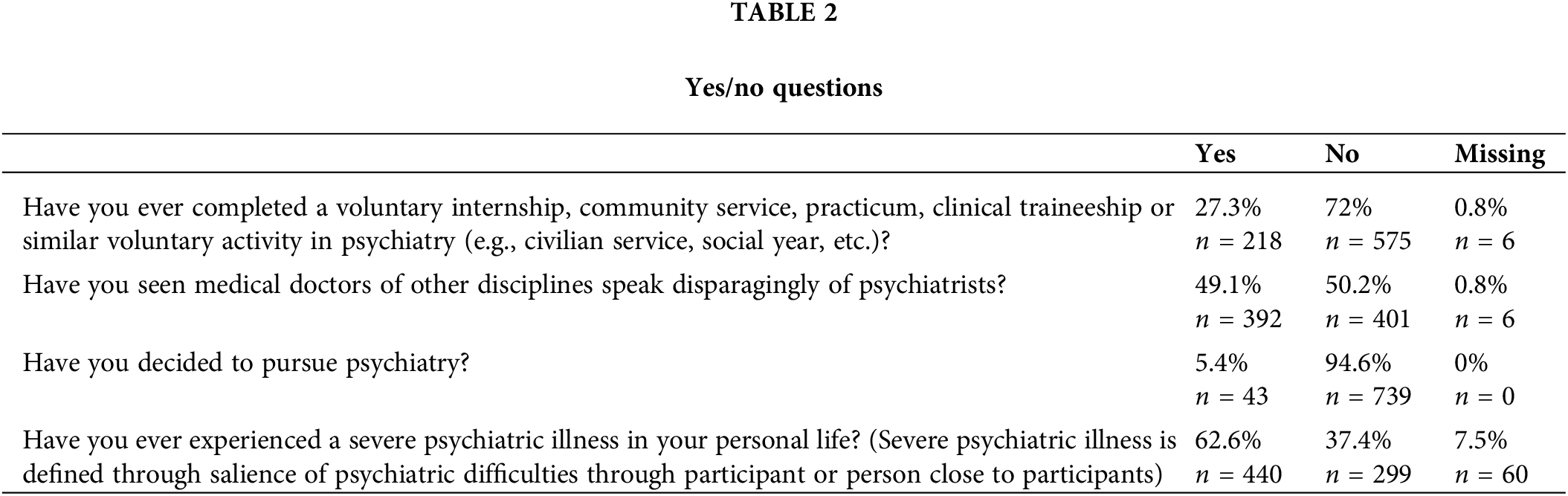
Out of the total 799 participants included, 379 were from Germany (47.3%), 343 from Italy (42.8%), and 77 missing values (9.6%) (Table 1). More than half of the participants were male (n = 412, 51.6%), and the mean age was 23.8 (±3.8). From first to sixth, all academic years were represented in our sample. In the questionnaire shown in Appendix A, students were asked to rank psychiatry among 13 other specialties in question 13. Table 2 shows descriptive statistics of the student population. Table 3 shows student’s answers from Likert style questions. Additional reporting of questions can be seen in Appendix A.
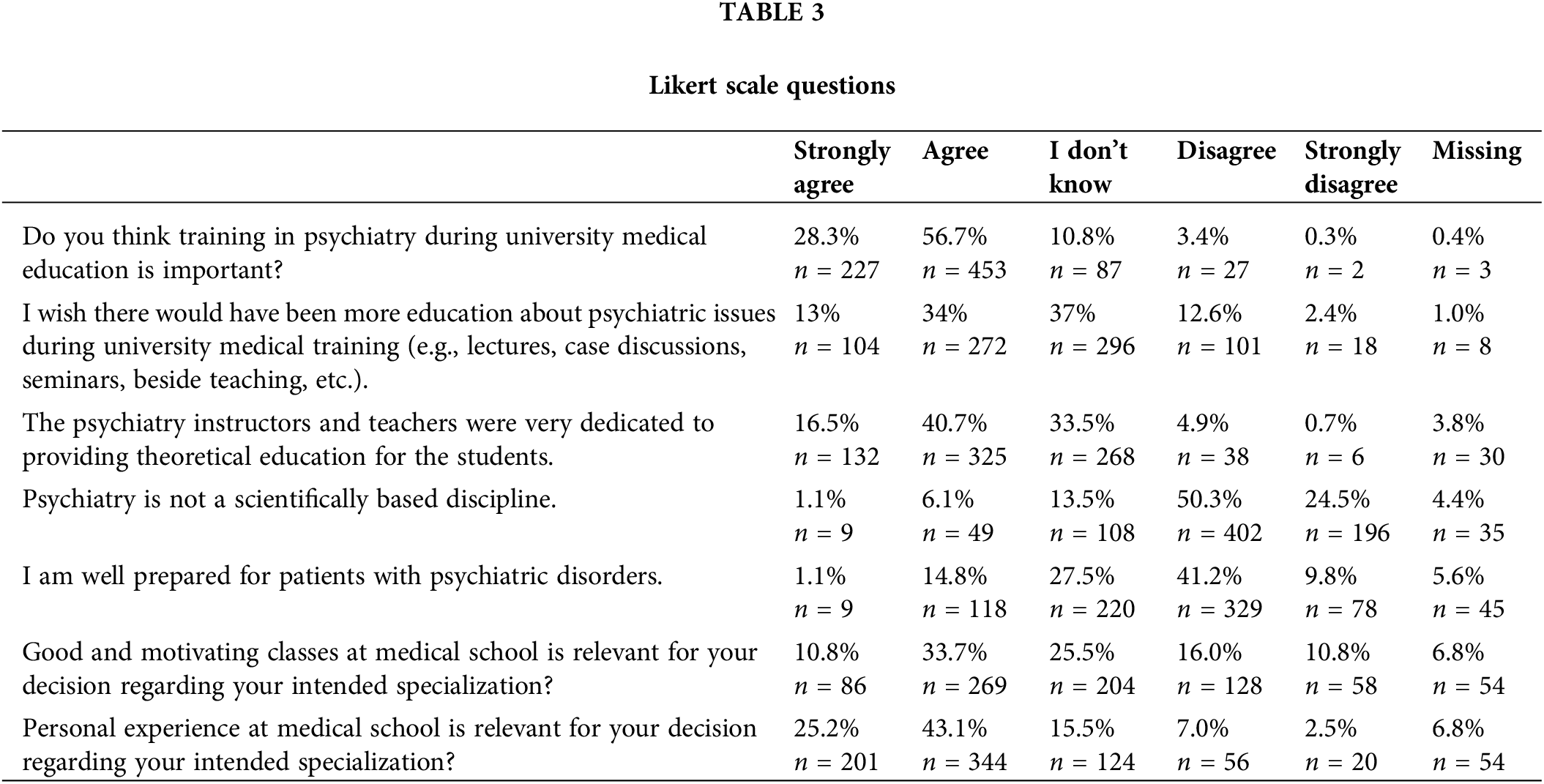
Students’ views on psychiatry as a scientific discipline were significantly positively associated with their ranking and pursuit of psychiatry (Table 4). Students’ opinions on the importance of psychiatric education were also significantly related to their pursuit of psychiatry (Table 4). In addition, their preparedness to deal with psychiatric disorders was significantly associated with the rank and pursuit of psychiatry (Table 4). Almost all (98%, n = 783) of the medical school students pursuing psychiatry found psychiatric training to be essential compared to 85% (n = 679) of medical school students pursuing other specialties (Table 4). There were no significant associations between demographics and the rank of psychiatry (Table 4).
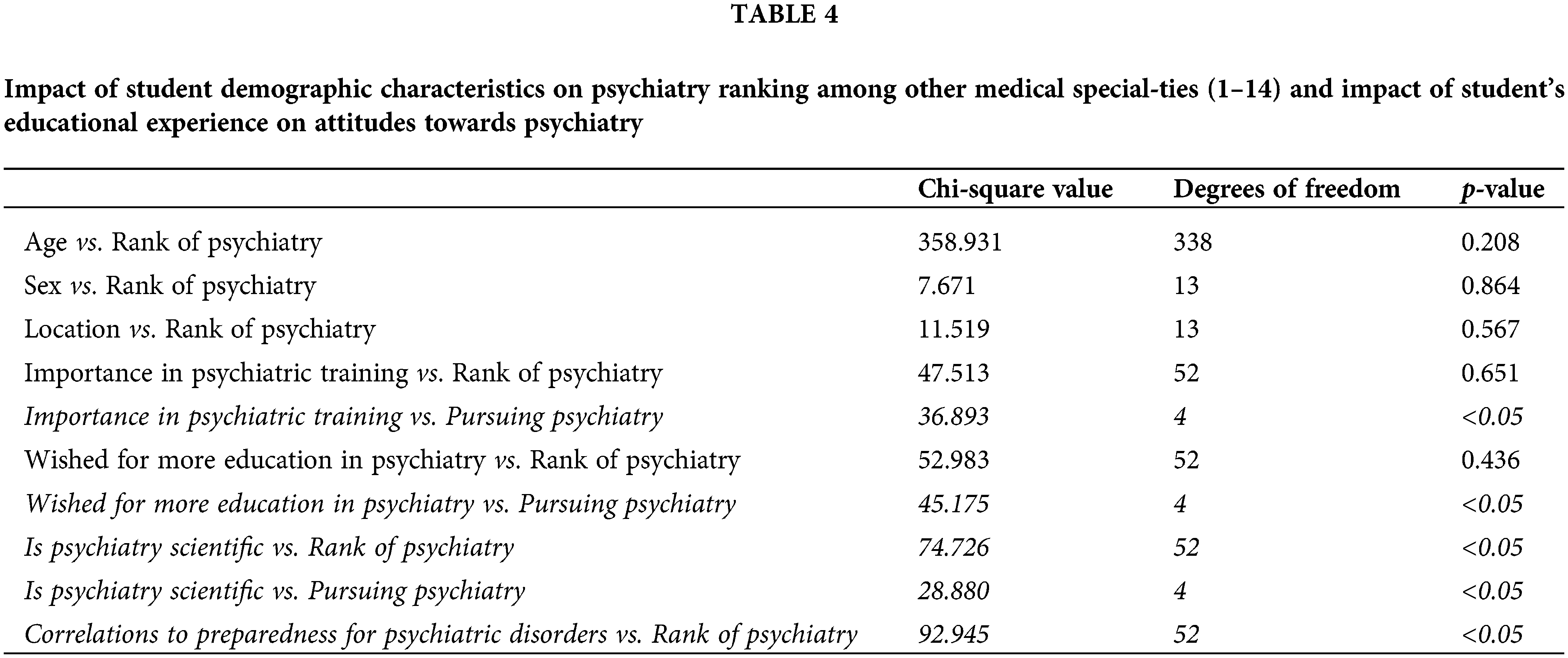
Students who completed voluntary activity in psychiatry were significantly associated with their pursuit of psychiatry (Table 5). As expected, 70% (n = 559) of medical students pursuing psychiatry had completed a psychiatry related voluntary activity, whereas only 25% (n = 200) of medical students pursuing other specialties had completed such activities in psychiatry (Table 5).
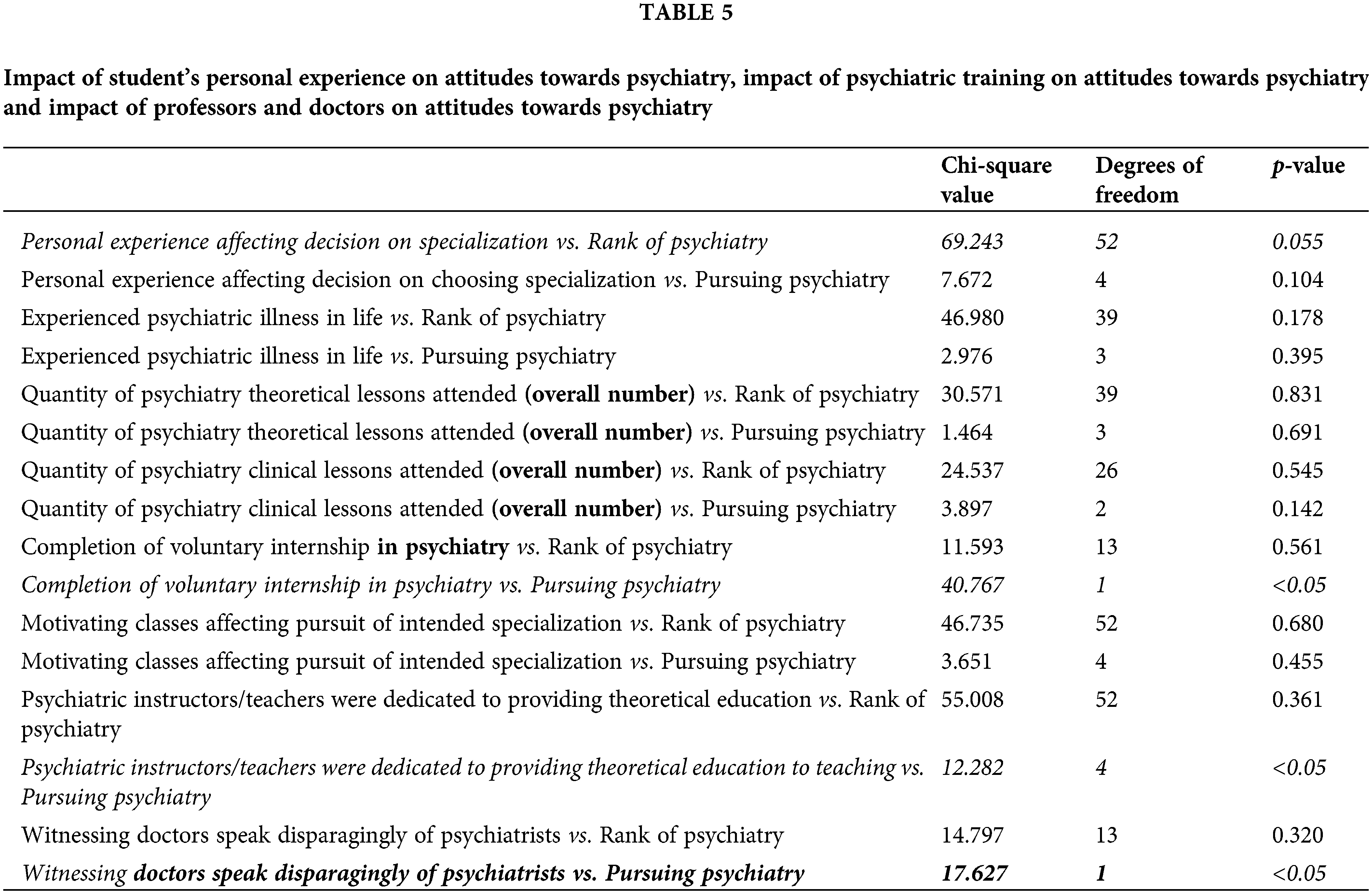
Having a dedicated instructor or teacher was significantly associated with pursuing psychiatry (Table 5). On the flip side, witnessing doctors speak disparagingly of psychiatrists was also significantly associated with one’s pursuit of psychiatry. One-third (34%, n = 272) of medical school students pursuing psychiatry believed their psychiatric instructors were dedicated to providing theoretical education compared to 15% (n = 120) of medical students pursuing other specialties (Table 5). Almost all (81%, n = 647) of medical school students pursuing psychiatry saw doctors speak disparagingly of psychiatrists compared to 48% of medical school students pursuing other specialties (Table 5).
This study sought to assess medical students’ attitudes towards psychiatry and the factors influencing their medical specialization in 2016. The main findings were that students who viewed psychiatry as a scientific discipline and deemed psychiatric education critical, ranked psychiatry higher among their top-choice specializations and reported a greater interest in pursuing psychiatry. Moreover, students’ exposure to psychiatry activities such as internships, community services, practicum, clinical traineeship, and personal experiences with psychiatric illness were also positively associated with their attitudes towards psychiatry and their willingness to pursue it as a specialty.
The results of this study are in line with the currently available literature. A recent survey study also found similar results that showed a correlation between previous experiences, specifically curriculum/education-related and personal experience affecting attitudes towards psychiatry [19]. Furthermore, a recent systematic review published in 2021 on medical students’ attitudes towards psychiatry found that psychiatry as a career choice was rated poorly and found to be unpopular for many students due to beliefs on “the lack” precision, “lack of treatment options”, and “personal prestige”, despite generally positive attitudes toward psychiatry [20,21]. In the general population, there is also a well documented lack of knowledge to identify features of mental illnesses, ignorance about how to access treatment, prejudice against people who have a mental illness, and expectation of discrimination against people diagnosed with mental illness [22].
Factors influencing medical students’ attitudes towards psychiatry
Medical students who grew up in a culture or family environment that perceives psychiatry as irrelevant may believe that psychiatry is emotionally demanding, ineffective, unscientific, and imprecise [23]. Our data suggests that these students are more likely to not pursue psychiatry (Table 4). Furthermore, students who reported that personal experiences affect their specialty choice were significantly associated with their ranking in psychiatry (Table 5). Other authors have also highlighted the critical roles of culture and health politics in shaping attitudes towards psychiatry [16,24]. Specifically, mental illnesses, such as depression, post-traumatic disorders, and suicidality are affected by culture. Family factors, coping methods, mental health stigmatization, and availability of treatment depending on country of origin can all contribute to developing cultural perspectives and views on mental health and psychiatry. Having a family history of psychiatric illness can also increase students’ attitudes towards psychiatry [25].
The importance of increasing exposure to psychiatry-oriented educational opportunities for medical students
In contrast to other medical specialties, the amount of time spent with a patient in psychiatry does not necessarily lead to immediate improvements in health outcomes, a factor that some may find unrewarding or discouraging. In addition, students may have a flawed perception of psychiatrists’ day-to-day activities, such as spending many hours talking to individual patients and providing psychological aid without significant concrete results quickly, which can lead to mental and emotional exhaustion [24]. As a result, Increasing students’ exposure to psychiatry-oriented educational opportunities is an important avenue to explore mental health care systems. In our study, participation in voluntary psychiatric activities was positively associated with the pursuit of psychiatry (Table 5). These results align with the findings of a recent study that reported students having positive attitudes towards psychiatry when completing over a month in psychiatric rotation and having studied psychiatry in college [25]. In addition, this aligned with a recent systematic review that looked at 42 different studies, with trends showing that clerkship improved attitudes towards psychiatry in students [21]. Although students interested in psychiatry might naturally also voluntarily participate in such psychiatric activities as internships and community services to appeal to their curiosity and interest, hands-on and shadowing experiences can significantly impact all students and impact their choice of specialization. Aslam et al. observed that medical students who were directly involved in the care of psychiatric patients were more receptive to psychiatry compared to students who did not receive such experiences [26]. This was also apparent in a recent systematic review, in which 61% of the included studies reported an overall improvement in students’ interest in psychiatry following psychiatry clerkship [27]. Such interactions remove barriers and destigmatize mental health topics through lived experiences, all the while reshaping the student’s perceptions of psychiatry and the day-to-day activities of psychiatrists. These educational experiences can provide valuable and rewarding information to medical students and spark an interest in knowing more about psychiatry [28].
In a recent study including 6213 cancer patients, 23.4% had depression, 17.7% had anxiety, and 9.3% had PTSD [29]. Mental health care and support, along with the basics of psychiatric principles, equip students with the skills necessary when dealing with difficult and complex situations such as a mental health crisis. Medical students who can adequately address mental health symptoms or refer patients to the appropriate mental health specialists are few and far between. Integrating psychiatry teachings with other clinical subjects like general medicine and specialties like dermatology (e.g., the case of OCD/trichotillomania/delusional parasitosis), cardiology (e.g., the point of panic disorder or depression), gastroenterology (e.g., the issue of psychosomatic illness), surgery (e.g., the case of delirium), neurology (e.g., the case of dissociative convulsions), and pediatrics (e.g., the case of OCD/ADHD/dyslexia) could help demonstrate the importance of psychiatry and introduce students to the necessity of acquiring psychiatric skills. Most importantly, this will be to the benefit of patients [29].
The importance of psychiatric education in the medical curriculum
Within the educational setting, the perspectives of professors and physicians hold considerable influence over the proclivities of medical students towards certain specialties. Our research findings have highlighted a positive correlation between the presence of committed instructors and an inclination towards psychiatry among students (Table 5). Conversely, a negative association was observed between instances of derogatory remarks regarding psychiatry made by physicians and the level of interest expressed by students in pursuing the field (Table 5). A recent systematic review found that stigmatizing attitudes towards people with mental disorders are common among physicians in primary care settings, particularly older and more experienced doctors [30]. Stigmatizing attitudes can act as an essential barrier for patients to receive the treatment they need and can also instill stigmatizing attitudes among younger medical students and lead to disinterest in the pursuit of psychiatry as a career choice [31]. Efforts must be invested to increase the quality and quantity of psychiatric education in the medical curriculum to improve students’ impression of psychiatry and their attraction to the field.
The majority of participants acknowledged the necessity of training in psychiatry, with 56.7% agreeing and 28.3% strongly agreeing. However, it is noteworthy that a meager 5.4% expressed an inclination to pursue psychiatry as their chosen specialty. This considerable disparity between the perceived significance of psychiatric training and the actual level of interest in the field is striking. Most of the students in this study acknowledged that their career preferences were influenced by personal encounters, though only a minority (27.4%) had attained proficiency in psychiatry. Prior research has reported that 45% of medical students in the United States were able to anticipate their ultimate specialty preference during their orientation year [32]. Thus, an effective strategy to address the recruitment crisis in psychiatry may entail early integration of psychiatric education into medical curricula.
Addressing the recruitment crisis in psychiatry to tackle the burden of mental illness in Germany and Italy
In 2011, there was a shortage of psychiatrists in Germany with 6% of psychiatric positions remaining unfilled, with a total of 21,289 practicing psychiatrist and 31% of Germans diagnosed with a mental illness [33,34]. Despite the increase in the burden of mental illness due to COVID-19 from 2019 to 2023, the number of psychiatrists has only slightly increased to 23,438 by 2023 compared to over 70,000 of employed physicians in Germany from 2011 to 2021 [35,36]. The situation was even more dire in Italy, where the number of psychiatrists only increased by approximately 1000 from 2011 to 2021 [36]. This scarcity of mental health professionals has likely contributed to the rise in depression, which increased from 5.5% of the total population prior to the COVID-19 pandemic to 17.3% in 2020 [36,37]. The data collected in 2016 sheds light on the growing burden of mental illness. This study contributes to the existing literature by demonstrating the usefulness of previously recorded data in comprehending the current state of mental health in Germany and Italy. Without addressing the recruitment crisis in the psychiatric field, the impact of global mental illness will further strain healthcare infrastructure, even in developed countries. This is of utmost importance, especially considering the significant impact that global crises such as COVID-19 can have on the prevalence of mental illness.
The perception of psychiatry in medicine and medical schools is indicative of its marginalized healthcare and health education status. The discipline of psychiatry contributes to this issue, which ultimately limits its ability to respond appropriately to an increasing burden of disease and mental health’s impact on overall health outcomes. Notably, there is a dearth of long-term studies on medical students’ attitudes throughout their medical training. The systematic evaluation of students’ attitudes towards psychiatry and motivational factors for pursuing psychiatry as a specialty, such as psychiatric education in medical school and personal experience, can inform necessary changes in the recruitment of students to the current mental health and medical education systems.
This study used a self-developed questionnaire and not a validated instrument. Although the study dates back to 2016 there is valuable insight for understanding how the medical students’ opinions have changed about psychiatry throughout the last decade. Additionally, data was only collected in Italy and Germany. Generalizability of this study is therefore limited, even though these countries are representative of European countries in general. Hence, this study primarily reflects German and Italian education systems, socio-economic backgrounds, and mental health care systems. Studies of medical students’ attitudes in various countries should focus on the impact of cultural differences on attitudes towards psychiatry. Despite our findings, the participants’ responses were self-reported and could not be verified. Finally, the cross-sectional design does not allow us to infer causality between education and attitudes towards psychiatry. A longitudinal study surveying students’ attitudes towards psychiatry during the first and last years of medical school would better predict how medical education can directly change one’s attitudes towards psychiatry. This questionnaire fails to capture students that choose to go into psychology majors and skip the expensive, late to fruit and demanding medical schools. This means that students are getting filtered, and “participants” might have been subject to selection bias. As a result, this paper only reflects attitudes towards psychiatry in medical school students in Germany and Italy and not all students in healthcare-related fields. Lastly, psychiatry may be ranked lower because students tend to be pragmatic and may choose specialties that they are less interested in but are more attainable.
In conclusion, there is an evident need to engage medical students more with psychiatry, improve curricula and provide more hands-on clinical experience. Moreover, though curriculums are constructed for students, studies that evaluate students’ attitudes concerning the curriculum are rare. The learners’ voices are primarily neglected in the curriculum design and implementation process. The image of Psychiatry among medical students based on their experience in medical school and the lack of practical experience is not motivating to choose the discipline. The essential factors of this image and the role of Psychiatry and Medicine are reflecting real problems of Psychiatry in healthcare as well as this discipline is presented. This study builds on the existing research on the question of what influences medical students’ perception of psychiatry. It is primarily a challenge for psychiatry to take on this discussion and start research on self-presentation, stigma, and strategies to change it. Improved curricula and an open dialogue among students and faculty would be an essential next step.
This study was a cross-sectional online survey conducted at Charite University Hospital (Germany), Greifswald University (Germany), and Universitaria Pisana (Italy). The questionnaire used in this study was designed through collaboration between the study team and medical students in Germany. The questionnaire was then validated in a meeting of experts through a Delphi survey of participating medical schools. The questionnaire was piloted at Greifswald University before the start of the study. The study was piloted with a small, closed group of students that completed the survey and gave feedback on the study protocol. This study was led by an established collaborative group that had affiliations with these universities. To participate, individuals had to be enrolled in an undergraduate medical program, be fluent in English, and have acces to a computer with an internet connection. Ethal approvalfor this study was obtained from the Behavioural Research Ethics Board at the University of British Columbia (H14-00176).
Participants were medical students enrolled in undergraduate medical education programs at participating universities. A convenience sample of medical students was used through snowball sampling, which began by contacting student council members and leaders within the medical student community of their respective universities. These intermediate students then shared the survey link with their peers via email. Despite the limitations of snowball sampling, such as community bias and non-random participation [38], this method was deemed the best way for maximal recruitment and participation. Furthermore, study advertisements were posted around the university, especially in buildings frequented by medical students.
Data collection started on January 1st, 2016 and ended on September 10th, 2016. Responses were collected electronically using Fluid Surveys and Qualtrics platform. Students completed a consent form before completing the survey. All responses were anonymous, and participation was voluntary. Information was hosted on Canadian databases and was kept confidential through password-protected accounts. To eliminate the possibility of duplicated responses, students were allowed to respond to the survey only once. All data gathered was anonymous. All data was stored and managed according to the data protection guidelines of the University of British Columbia.
The survey consisted of 37 questions with possible responses varying between a 5-point Likert scale (‘strongly agree,’ ‘agree,’ ‘undecided,’ ‘disagree,’ ‘strongly disagree’), a binary scale (‘yes’ or ‘no’) and a ranking scale. The questions were categorized into the following sections: 1. demographic information, 2. personal experience and exposure to mental health, 3. education experience in psychiatry, 4. courses, 5. practical experiences, 6. teachers’ perceived attitudes, 7. Student’s attendance at courses and 8. attitudes towards psychiatry.
Chi-square tests were performed for inferential analyses using a significance level of 0.05. Descriptive and inferential statistical analyses were executed using SPSS version 25, a competent statistical tool [39].
Acknowledgement: The authors would like to express their sincere appreciation to all individuals and organizations who have contributed to the completion of this research. We are grateful to Julie Elsner, Arash Moghadam, Maximilian Meyer, Gurpreet Chopra, Fiona Choi, and Maurice Cabanis for their support and assistance throughout the project. We also thank the reviewers and editors for their valuable feedback and suggestions, which greatly improved the quality of this paper. Our appreciation also goes to the study participants who generously shared their time and insights, without whom this research would not have been possible. Finally, we acknowledge the funding agencies and institutions that supported this research.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contributions to the paper as follows: study conceptions and design: MK. Mostafa, S. Schomerus, GIM. Angelo, K. Michael; data collection: S. Schomerus, GIM. Angelo; analysis and interpretation of results: MYT. Andy. S. Janet; draft manuscript preparations: MYT. Andy. S. Janet. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: This study received ethical approval from the Behavioral Research Ethics Board at the University of British Columbia (H14-00176).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
Supplementary Materials: The supplementary material is available online at https://doi.org/10.32604/ijmhp.2023.030087.
References
1. Satiani A, Niedermier J, Satiani B, Svendsen DP. Projected workforce of psychiatrists in the United States: a population analysis. Psychiatr Serv [Internet]. 2018;69(6):710–3. doi:https://doi.org/10.1176/appi.ps.201700344. [Google Scholar] [PubMed] [CrossRef]
2. Health SB. National projections of supply and demand for selected behavioral health practitioners: 2013–2025. 2013. Available from: https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/behavioral-health-2013-2025.pdf. [Google Scholar]
3. Miller P. Review of physician and advanced practitioner recruiting in-centives. Merrit hawkins. 2017. Available from: https://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Pdf/2017_Physician_Incentive_Review_Merritt_Hawkins.pdf. [Google Scholar]
4. Ferrari A. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry [Internet]. 2022;9(2):137–50. doi:https://doi.org/10.1016/S2215-0366(21)00395-3. [Google Scholar] [PubMed] [CrossRef]
5. Talevi D, Socci V, Carai M, Carnaghi G, Faleri S, Trebbi E, et al. Mental health outcomes of the COVID-19 pandemic. Riv Psichiatr [Internet]. 2020;55(3):137–44. [Google Scholar] [PubMed]
6. Farooq K, Lydall GJ, Malik A, Ndetei DM, Bhugra D. Why medical students choose psychiatry—a 20 country cross-sectional survey. BMC Medical Education [Internet]. 2014;14(1):397. doi:https://doi.org/10.1186/1472-6920-14-12. [Google Scholar] [PubMed] [CrossRef]
7. McParland M, Noble LM, Livingston G, McManus C. The effect of a psychiatric attachment on students’ attitudes to and intention to pursue psychiatry as a career. Med Educ [Internet]. 2003;37(5):447–54. doi:https://doi.org/10.1046/j.1365-2923.2003.01491.x. [Google Scholar] [PubMed] [CrossRef]
8. Farooq K, Lydall G. Psychiatry DB-IR of, 2013 undefined. What attracts medical students to-wards psychiatry? A review of factors before and during medical school. Int Rev Psychiatry [Internet]. 2013;25(4):371–7. [Google Scholar]
9. Mortlock AM, Puzzo I, Taylor S, Kumari V, Young S, Sengupta S, et al. Enrichment activities in the medical school psychiatry programme—could this be a key to engaging medical students in psychiatry? A study from a high secure forensic psychiatric UK hospital. BMC Psychiatry [Internet]. 2017;17(1):444. doi:https://doi.org/10.1186/s12888-017-1236-z. [Google Scholar] [PubMed] [CrossRef]
10. Sloan DI, Browns S, Meagher D, Lane A, Larkin C, Casey P, et al. Attitudes toward psychiatry among Irish final year medical students. Eur Psychiatry [Internet]. 1996;11(8):407–8. doi:https://doi.org/10.1016/S0924-9338(97)82579-5. [Google Scholar] [PubMed] [CrossRef]
11. Lyons Z, Janca A. Impact of a psychiatry clerkship on stigma, attitudes towards psychiatry, and psychiatry as a career choice career choice, professional education and development. BMC Med Educ [Internet]. 2015;15:34. doi:https://doi.org/10.1186/s12909-015-0307-4. [Google Scholar] [PubMed] [CrossRef]
12. Angermeyer M, Dietrich S. Public beliefs about and attitudes to-wards people with mental illness: a review of population studies. Acta Psychiatr Scand [Internet]. 2006;113(3):163–79. [Google Scholar]
13. Eltorai AEM, Eltorai AS, Fuentes C, Durand WM, Daniels AH, Ali S. Financial implications of physician specialty choice. R I Med J [Internet]. 2018;101(8):50–5. [Google Scholar]
14. Kuhnigk O, Strebel B, Schilauske J, Jueptner M. Attitudes of medical students towards psychiatry. Adv Health Sci Educ Theory Pract [Internet]. 2007;12(1):87–101. doi:https://doi.org/10.1007/s10459-005-5045-7. [Google Scholar] [PubMed] [CrossRef]
15. Samari E, Seow E, Chua BY, Ong HL, Abdin E, Chong SA, et al. Stigma towards people with mental disorders: perspectives of nursing students. Arch Psychiatr Nurs [Internet]. 2018;32(6):802–8. doi:https://doi.org/10.1016/j.apnu.2018.06.003. [Google Scholar] [PubMed] [CrossRef]
16. Rajagopal S, Rehill KS, Godfrey E. Psychiatry as a career choice compared with other specialties: a survey of medical students. Psychiatrist [Internet]. 2004;28(12):444–6. doi:https://doi.org/10.1192/pb.28.12.444. [Google Scholar] [CrossRef]
17. Dandurand F, Shultz TR, Onishi KH. Comparing online and lab methods in a problem-solving experiment. Behav Res Methods [Internet]. 2008;40(2):428–34. doi:https://doi.org/10.3758/BRM.40.2.428. [Google Scholar] [PubMed] [CrossRef]
18. Alzahrani A. Assessing the attitudes of medical students towards psychiatry: a new paradigm. Asian J Psychiatr [Internet]. 2019;43(1):17–23. doi:https://doi.org/10.1016/j.ajp.2019.05.005. [Google Scholar] [PubMed] [CrossRef]
19. Warnke I, Gamma A, Buadze M, Schleifer R, Canela C, Strebel B, et al. Predicting medical students’ current attitudes toward psychiatry, interest in psychiatry, and estimated likelihood of working in psychiatry: a cross-sectional study in four European countries. Front Psychiatry [Internet]. 2018;9:49. doi:https://doi.org/10.3389/fpsyt.2018.00049. [Google Scholar] [PubMed] [CrossRef]
20. Bhugra D, Sartorius N, Fiorillo A, Evans-Lacko S, Ventriglio A, Hermans MHM, et al. EPA guidance on how to improve the image of psychiatry and of the psychiatrist. Eur Psychiatry [Internet]. 2015;30(3):23–30. doi:https://doi.org/10.1016/j.eurpsy.2015.02.003. [Google Scholar] [PubMed] [CrossRef]
21. Veliki V. Attitudes towards psychiatry among medical students worldwide: a review. Medicina Academica Mostariensia [Internet]. 2021;33:18–24. [Google Scholar]
22. Aghukwa NC. Attitudes towards psychiatry of undergraduate medical students at Bayero University. Nigeria. South African Journal of Psychiatry [Internet]. 2010;16(4):147–52. doi:https://doi.org/10.4102/sajpsychiatry.v16i4.239. [Google Scholar] [CrossRef]
23. Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am J Public Health [Internet]. 2013;103:777. [Google Scholar]
24. Creed F, Goldberg D. Students’ attitudes towards psychiatry. Med Educ [Internet]. 1987;21(3):227–34. doi:https://doi.org/10.1111/j.1365-2923.1987.tb00695.x. [Google Scholar] [PubMed] [CrossRef]
25. Manriquez PM. Mental health: culture, race, and ethnicity. Washington: Department of Health and Human Services; 2001. [Google Scholar]
26. Aslam M, Taj T, Ali A, Badar N, Saeed F, Abbas M, et al. Psychiatry as a career: a survey of factors affecting students’ interest in Psychiatry as a career. Mcgill J Med [Internet]. 2009;12:7–12. [Google Scholar] [PubMed]
27. Wiesenfeld L, Abbey S, Takahashi SG, Abrahams C. Choosing psychiatry as a career: motivators and deterrents at a critical decision-making juncture. Can J Psychiatry [Internet]. 2014;59(8):450–4. doi:https://doi.org/10.1177/070674371405900808. [Google Scholar] [PubMed] [CrossRef]
28. Goldacre MJ, Turner G, Fazel S, Lambert T. Career choices for psychiatry: national surveys of graduates of 1974–2000 from UK medical schools. Br J Psychiatry [Internet]. 2005;186(2):158–64. doi:https://doi.org/10.1192/bjp.186.2.158. [Google Scholar] [PubMed] [CrossRef]
29. Wang Y, Duan Z, Ma Z, Mao Y, Li X, Wilson A, et al. Epidemiology of mental health prob-lems among patients with cancer during COVID-19 pandemic. Transl Psychiatry [Internet]. 2020;10(1):263. [Google Scholar] [PubMed]
30. Vistorte AOR, Ribeiro WS, Jaen D, Jorge MR, Evans-Lacko S, de Mari JJ. Stigmatizing atti-tudes of primary care professionals towards people with mental disorders: a systematic review. The Int J Psychiatry Med [Internet]. 2018;53(4):317–38. doi:https://doi.org/10.1177/0091217418778620. [Google Scholar] [PubMed] [CrossRef]
31. Kallivayalil RA. The importance of psychiatry in undergraduate medical education in India. Indian J Psychiatry [Internet]. 2012;54(3):208–16. doi:https://doi.org/10.4103/0019-5545.102336. [Google Scholar] [PubMed] [CrossRef]
32. Zeldow PB, Preston RC, Daugherty SR. The decision to enter a medical specialty: timing and stability. Med Educ [Internet]. 1992;26(4):327–32. doi:https://doi.org/10.1111/j.1365-2923.1992.tb00177.x. [Google Scholar] [PubMed] [CrossRef]
33. Grözinger M, Amlacher J, Schneider F. Besetzung ärztlicher stellen in deutschen kliniken für psychiatrie und psychotherapie. Nervenarzt [Internet]. 2011;82(11):1460–8. doi:https://doi.org/10.1007/s00115-010-3193-3. [Google Scholar] [CrossRef]
34. McLean C. A closer look at mental health in germany. The Borgen Project [Internet]. 2021. https://borgenproject.org/mental-health-in-germany/. [Google Scholar]
35. Mauz E, Walther L, Junker S, Kersjes C, Damerow S, Eicher S, et al. Time trends of mental health indicators in Germany’s adult population before and during the COVID-19 pandemic. medRxiv [Internet]. 2022. [Google Scholar]
36. Health Care Resources [Internet]. 2023. https://stats.oecd.org/Index.aspx?&datasetcode=HEALTH_REAC. [Google Scholar]
37. Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet [Internet]. 2021;398(10312):1700–12. doi:https://doi.org/10.1016/S0140-6736(21)02143-7. [Google Scholar] [PubMed] [CrossRef]
38. Choudhry FR, Mani V, Ming LC, Khan TM. Beliefs and perception about mental health issues: a meta-synthesis. Neuropsychiatr Dis Treat [Internet]. 2016;12:2807–18. doi:https://doi.org/10.2147/NDT.S111543. [Google Scholar] [PubMed] [CrossRef]
39. Stehlik-Barry K, Babinec A. Data analysis with IBM SPSS statistics [Internet]. 1st ed. Packt Publishing, Ltd.: Birmingham, UK; 2017. [Google Scholar]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools