 Open Access
Open Access
ARTICLE
Perceived Social Support and Symptoms of Depression and Anxiety among Chinese Adolescents: A Moderated Chain Mediation Model
1 School of Public Health, Suzhou Medical College, Soochow University, Suzhou, 215123, China
2 Department of General Medicine and Big Data Center, The Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou, 215008, China
3 School of Public Health, Peking University, Beijing, 100191, China
4 Graduate School of Interdisciplinary Science and Engineering in Health Systems, Okayama University, Okayama, 700-8530, Japan
* Corresponding Authors: Yi-Bo Wu. Email: ; Tian-Yang Zhang. Email:
(This article belongs to the Special Issue: Mental Health Promotion and Psychosocial Support in Vulnerable Populations: Challenges, Strategies and Interventions)
International Journal of Mental Health Promotion 2025, 27(1), 29-40. https://doi.org/10.32604/ijmhp.2025.057962
Received 01 September 2024; Accepted 16 December 2024; Issue published 31 January 2025
Abstract
Background: Although previous studies indicate that perceived social support might be associated with adolescent psychological problems, the specific mechanism has not been thoroughly discussed. Based on theoretical and empirical research on problematic Internet use (PIU) and sleep quality, this study explored whether they play a mediating role between perceived social support and symptoms of depression and anxiety among adolescents. Furthermore, we investigated whether these relationships varied by place of residence. Methods: A sample of 2115 Chinese adolescents was included, and analyzed data related to perceived social support, PIU, sleep quality, symptoms of depression and anxiety, and sociodemographic variables. Correlation analysis, mediation, and moderation analysis were mainly used. Results: Perceived social support was negatively correlated with depressive symptoms (r = −0.22, p < 0.001) and anxiety symptoms (r = −0.20, p < 0.001) among adolescents. PIU and sleep quality played a chain mediating role in the relationship between perceived social support and symptoms of depression and anxiety in adolescents. Additionally, the place of residence moderated the relationships between perceived social support and PIU and symptoms of depression and anxiety. Perceived social support was a significant negative predictor of PIU and symptoms of depression and anxiety among adolescents in urban areas but not in rural areas. Conclusion: The findings suggest that low levels of perceived social support may lead to more PIU and poorer sleep quality, which may further increase the risk of symptoms of depression and anxiety in adolescents, especially in urban areas.Keywords
Adolescents undergo significant physical and psychological changes and are vulnerable to developing mental health issues [1–3]. A study published in 2019 showed that the aggregate prevalence of depressive symptoms among Chinese children and adolescents stood at 19.85% [4]. Psychological issues are linked to negative outcomes such as substance abuse disorders, poor physical health, and even death by suicide, in addition to affecting adolescents’ academic performance [5]. Moreover, experiencing depression during adolescence can affect the developmental process and potentially elevate the risk of adverse psychological outcomes in adulthood [6,7]. Given the high prevalence and far-reaching consequences of adolescent psychological issues, investigating the factors and underlying processes behind these problems remains crucial.
Notably, the healthy growth of adolescents is widely influenced by various social factors, originating from the family, educational institutions, and the broader community [8]. Perceived social support represents a significant psychological resource for adolescents, deriving from their family, school, and broader social environment. It is closely intertwined with their psychological and behavioral processes. The concept of perceived social support is typically understood to encompass an individual’s subjective assessment and perception that the individuals within their broader social network can receive the necessary support and assistance [9]. An association of perceived social support with mental issues in adolescents is already well corroborated, but the specific mechanisms remain to be further explored and clarified [10,11].
Overall, current research seeks to examine the relevance between perceived social support and symptoms of depression and anxiety among adolescents, focusing on the potential mechanisms underlying this association.
Perceived social support and symptoms of depression and anxiety
The main-effect model of social support points out that help and support from external sources exert important gainful effects on a person’s mental well-being [3]. For instance, teenagers with greater social support may exhibit increased self-esteem and better psychological well-being [12]. Furthermore, a longitudinal study aimed at exploring the impact of social support on psychological health by age and gender suggested that high social support was closely related to greater gains in psychological health among those under the age of 30 [13]. Comparatively, low perception levels of social support are considered to be an important risk factor for adolescent psychological problems [14]. Based on the above theories of social support and past empirical research findings, this study hypothesized that perceived social support negatively predicts adolescent depressive symptoms and anxiety symptoms.
Problematic Internet use as the mediator
For teenagers, the Internet is not only a social and educational tool but also intimately linked to their daily lives [15]. Helpful Internet use can help teenagers obtain information and resources through the Internet to improve efficiency and learning outcomes [16]. Nevertheless, excessive or improper Internet use has caused serious negative effects. Problematic Internet use (PIU) has emerged as an important public health concern, generally defined as uncontrolled people’s Internet use resulting in adverse implications in everyday life. It encompasses two principal characteristics. The first aspect of concern pertains to the utilization of the Internet, which has been characterized as excessive and compulsive, in addition to a preoccupation with the Internet and a perceived loss of control over its use. The second characteristic is the adverse effect that excessive Internet usage can have on an individual. This can manifest in various ways, including ignoring social and interpersonal relationships and failing to meet responsibilities related to health, education, and nutrition (e.g., poor eating and sleeping habits) [17].
PIU has been linked with many psychological problems in adolescents, including higher depressive symptoms, anxiety symptoms, and other negative psychological health outcomes [18]. Huang et al. [19] found a significant association between PIU and an elevated risk of suicidal ideation among adolescents. Noteworthily, teenagers are at a critical stage of their lives and are at higher risk of developing PIU [20]. A recent study reported that 14.9% of Chinese teenagers had PIU [21]. Additionally, researchers have noted that a notable external factor contributing to adolescent PIU may be inadequate social support. Teenagers may resort to support and assistance online when they cannot obtain enough in real life. When the care and support that young people lack in real life is fulfilled through cyberspace, this gratification, in turn, pushes them to utilize the Internet with greater frequency and more time [22]. Empirical findings have confirmed that social support has directly and indirectly implicated in Internet addiction among adolescents [23,24]. In light of the aforementioned empirical evidence, we hypothesized that PIU mediates the relationship between perceived social support and adolescent symptoms of depression and anxiety.
Apart from the PIU mentioned above, sleep also plays a crucial role in cognitive function and mental health during adolescence [25]. Healthy sleep helps to enhance immune function and improve academic performance, which is crucial for the physical and mental health of teenagers [26]. Rather, sleep deprivation can lead to a range of unfavorable consequences [27], including poor concentration, diminished academic performance, and increased risk of mood disorders and suicidal ideation [28]. Furthermore, evidence indicated that sleep deprivation can impair the emotional state and emotional regulation of adolescents, whether the deprivation is chronic or acute [25].
Poor quality of sleep constitutes a considerable hazard factor to the onset of many psychological conditions [29,30]. A cohort study involving individuals aged between 11 and 17 years demonstrated that sleep deprivation at baseline was associated with a more than three-fold increased risk of subsequent major depressive disorder [31]. Importantly, researchers have highlighted that social relationship factors are more influential than developmental factors in shaping adolescent sleep patterns, particularly those about parental, peer, and school relationships, which are crucial in promoting healthy sleep [32]. Moreover, the stress-buffering theory proposes that access to social support can be powerful in buffering the harmful effects of stress on sleep [33]. A study of American high school students demonstrated that adolescents with greater parental support under family pressure slept longer and had fewer nighttime awakenings [34]. In consideration of the above-mentioned theoretical and empirical evidence, this study posits that sleep quality mediates the connection of perceived social support with symptoms of depression and anxiety in adolescents.
PIU and sleep quality as the chain mediator
Within the empirical literature, PIU is closely related to adolescent sleep quality [35,36]. Behavioral symptoms associated with PIU can deleteriously influence an affected individual’s sleep-wake rhythm, which may subsequently give rise to a range of sleep-related issues [37]. A study of students in grades 7 to 9 found that problematic Internet users exhibited a higher propensity for the onset of sleep disorders [38]. A further study indicated that adolescents with Internet addiction were more likely to experience nocturnal sleep deprivation and daytime sleepiness [39]. In addition to its association with decreased sleep quality, PIU has also been linked to increased psychological distress [40]. Teenagers presenting with PIU may be more prone to sleep problems, which can trigger physical and psychological problems. Sleep quality has been shown to mediate the relationship of PIU with physical and psychological symptoms in teenagers [29]. Taken together, a potential mechanism by which perceived social support affects symptoms of depression and anxiety could be through its influence on PIU, as well as on sleep quality.
Place of residence as the moderator
Following the medical model of environmental health, as put forward by Blum, it is evident that socio-environmental exert a pivotal influence on an individual’s physical and mental development [41]. The phenomenon of urbanization represents an exceptional manifestation of the prevailing socioeconomic milieu, exerting a profound implication for mental health and its related fields. In this situation, both personal mental status and the provision of psychological healthcare services are exposed to tremendous shifts and challenges [42]. Urban dwellers may be more susceptible to facing psychological throw-down the gauntlet [43]. A descriptive study on adolescent depression in Huangshi City, China, revealed a higher incidence of depression among urban adolescents compared to rural regions [44]. The process of urbanization may give rise to the emergence and intensification of psychological issues, particularly among those who are most vulnerable [45]. A study found that adolescents in urban settings exhibited more severe Internet addiction than their counterparts [46]. Additionally, the proportion of individuals utilizing the Internet and smartphones is comparatively lower in rural areas [47]. In light of the aforementioned theories and empirical findings, this study attempted to ascertain the part played by urban-rural differences in the correlation between adolescents’ perceived social support, PIU, sleep quality, along symptoms of depression and anxiety.
While the association between perceived social support and adolescent psychological difficulties has been established, the precise mechanisms that underpin this relationship remain to be fully elucidated [10,11]. Based on previous literature, further investigation is warranted into the role of PIU and sleep quality in the nexus between perceived social support levels and mental problems in adolescents. Meanwhile, the question of whether there are discrepancies in these relationships between urban and rural environments deserves particular attention. Furthermore, previous studies have frequently employed involved local or regional samples [12,14]. Given that adolescence is a fragile stage for mental issues, it is crucial to gain an understanding of the specific mechanisms through which perceived social support is associated with psychological issues. This will inform the promotion and advancement of adolescent mental health. Based on a large-scale national survey, this paper aims to explore the role of PIU and sleep quality in the relationship between perceived social support and symptoms of depression and anxiety in adolescents, as well as the possible urban-rural differences in the above relationships. Specifically, the following hypotheses were proposed:
Hypothesis 1: Perceived social support negatively predicts symptoms of depression and anxiety in adolescents.
Hypothesis 2: Perceived social support indirectly predicts symptoms of depression and anxiety in adolescents through PIU and sleep quality and their chain-mediated effects.
Hypothesis 3: Place of residence (urban-rural differences) moderates the relationships between perceived social support and PIU and between perceived social support and symptoms of depression and anxiety.
The data were drawn from the 2022 Psychological and Behavioral Investigation of Chinese Residents (PBICR-2022). Our study has secured all necessary permissions to utilize the data set. Further details regarding the database can be found at the following link: https://www.x-mol.com/groups/pbicr/shujukukaifang (accessed on 15 December 2024). This large-scale cross-sectional survey in 23 provinces, 5 autonomous regions, and 4 municipalities directly under the Central Government in the Chinese mainland was enacted from 20 June to 31 August 2022. Stratified sampling and quota sampling were employed to guarantee the representativeness of the sample. Professional investigators distributed electronic questionnaires to the participants. Details of the survey were previously published [48].
The invitation was extended to permanent residents of Chinese nationality aged 12 and above. Participants needed to be able to comprehend the content of the investigatory questionnaire and capable of completing it independently, or with the assistance of an individual acting in the capacity of an investigator. The research gathered information from 21,916 participants. The present study focused on 12- to 17-year-olds as the research subjects. A total of 21,916 questionnaires were initially screened based on age, and 2178 samples were ultimately obtained. Following the removal of incomplete data and outliers, the final analysis was based on valid data from 2115 participants.
The relevant sociodemographic information included age, gender (male/female), ethnicity (Han/non-Han), place of residence (urban/rural), only-child status (yes/no), and social status. Among them, ethnicity is based on a binary question, where participants answer “Han” or “non-Han”. Place of residence is obtained based on the question of “your permanent residence (urban/rural) in the past three months”. The evaluation of social status is determined by the question “What is your perception of the status of your family in society?”, a 7-level slider question (1 stands for the lowest level, 7 stands for the highest level).
Perceived social support was assessed from three dimensions: family, friends, and significant others using a three-item Perceived Social Support Scale (PSSS). The 7-point Likert scale ranging from “strongly disagree” (1 point) to “strongly agree” (7 points) was used, with overall scores between 3 and 21. Higher scores indicate greater perceived social support [49]. The Chinese version of PSSS has been subjected to a process of validation using a sample of adolescents [3]. The resulting Cronbach’s alpha coefficient value was 0.905.
Symptoms of depression and anxiety
The presence of depressive and anxiety symptoms during the previous two weeks was evaluated through the administration of the 9-item Patient Health Questionnaire (PHQ-9) and the 7-item Generalized Anxiety Disorder Scale (GAD-7), respectively. Scored on the four-point Likert Scale, whereby 0 represents “none at all” and 3 means “almost every day”. Overall scores on the scales range from 0 to 27 (PHQ-9) and 0 to 21 (GAD-7), with higher scores on either scale reflecting a greater severity of corresponding symptoms. A total score below 5 indicates no symptoms of depression or anxiety, while a score of 5 or above indicates varying degrees of symptoms of depression or anxiety. These two scales have been validated as reliable and effective measures in the sample of adolescents [50,51]. Cronbach’s alpha coefficients for PHQ-9 and GAD-7 were recorded at 0.936 and 0.952.
Participants’ PIU was scored using the short-form 6-item Problematic Internet Use Questionnaire (PIUQ-SF6). Each dimension of the scale (compulsion, neglect, and control) is subdivided into two items. A 5-point Likert scale (1 = never, 5 = always/almost always) was used, with an overall score ranging from 6 to 30. Higher scores indicate more severe PIU [52]. The Chinese version of PIUQ-SF6 has been validated in adolescent samples [53]. The Cronbach’s alpha coefficient of the PIUQ-SF6 was 0.919.
The Brief Version of the Pittsburgh Sleep Quality Index (B-PSQI) was used to measure participants’ sleep quality. This scale comprises five dimensions with a total of six items. Since two entries, bedtime and wake time, are applied in the calculation of sleep efficiency, there are five scoring items in the B-PSQI. The total score is expressed as a number between 0 and 15, with lower values denoting a superior quality of sleep [54]. The evidence substantiates the B-PSQI as a reliable instrument for evaluating the sleep quality of adolescents [55]. The Cronbach’s alpha coefficient for this sample was 0.664.
All analyses were carried out in SPSS 26.0 software. The t-test and Chi-square test were performed to compare differences in the presence or absence of symptoms of depression and anxiety. Then, Pearson correlation examined the correlation between the main study variables. Chain mediation analysis and moderated chain mediation analysis were carried out using the PROCESS plug-in models 6 and 92 of SPSS software, respectively. The objective of the subsequent examination, namely the simple slope analysis, was to further investigate the moderating effect of residence. Statistically significant was determined with a p-value < 0.05.
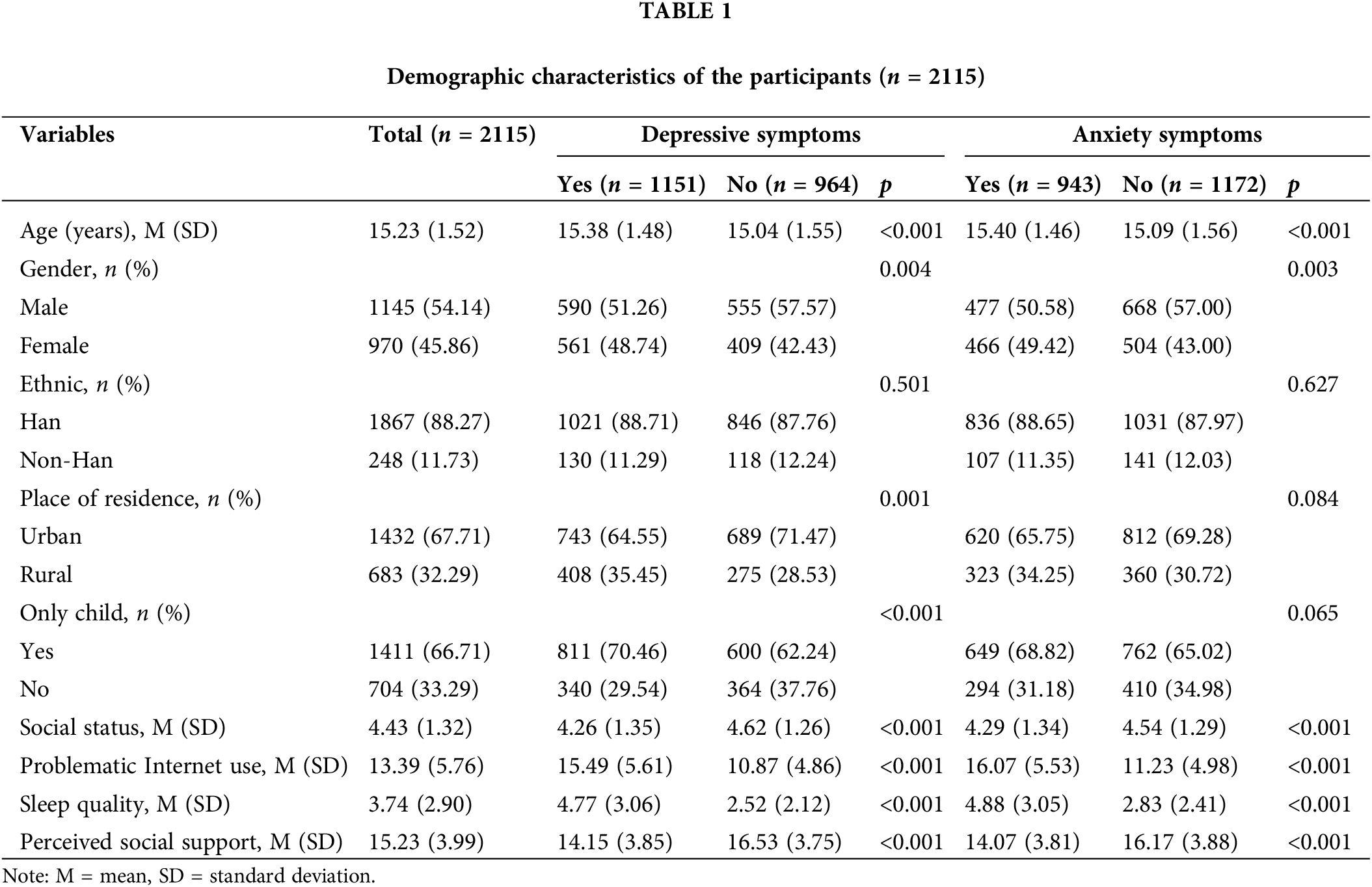
Table 1 shows that 1151 individuals exhibit varying degrees of depressive symptoms, while 943 individuals exhibit varying degrees of anxiety symptoms. Among them, there were significant differences in perceived social support, PIU, and sleep quality scores between adolescents with or without symptoms of depression or anxiety. Adolescents with symptoms of depression or anxiety had higher PIU and sleep quality scores and lower perceived social support scores (both p < 0.001).
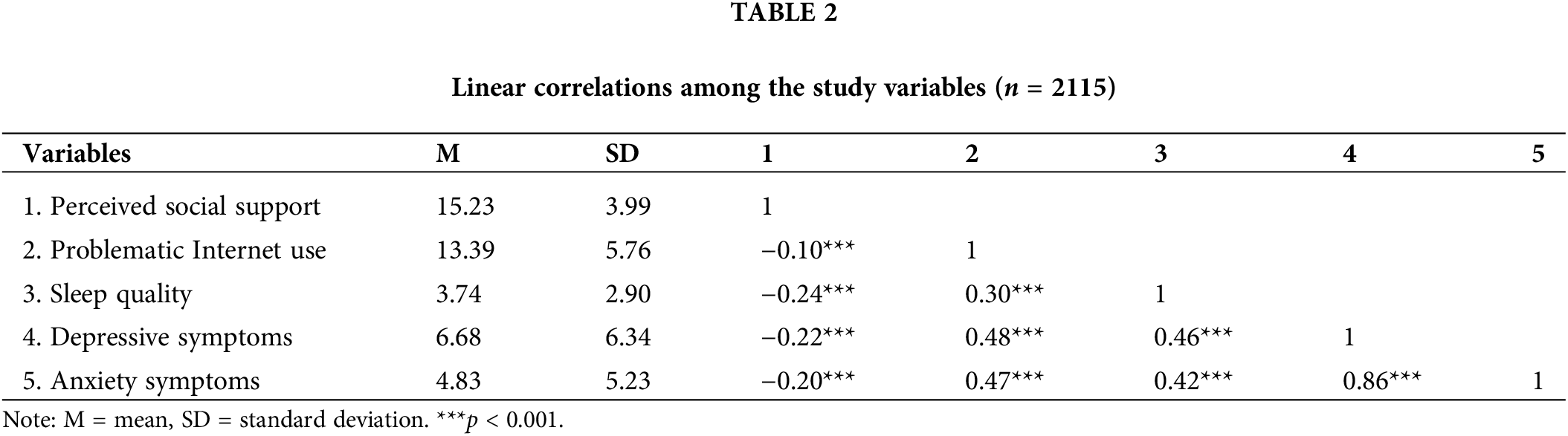
A negative correlation was observed between the perceived social support score and PIU, sleep quality, depressive symptom, and anxiety symptom scores. PIU and sleep quality scores were positively correlated with depressive symptom and anxiety symptom scores. Furthermore, a positive correlation was observed between the PIU score and the sleep quality score (Table 2).
The mediating roles of PIU and sleep quality
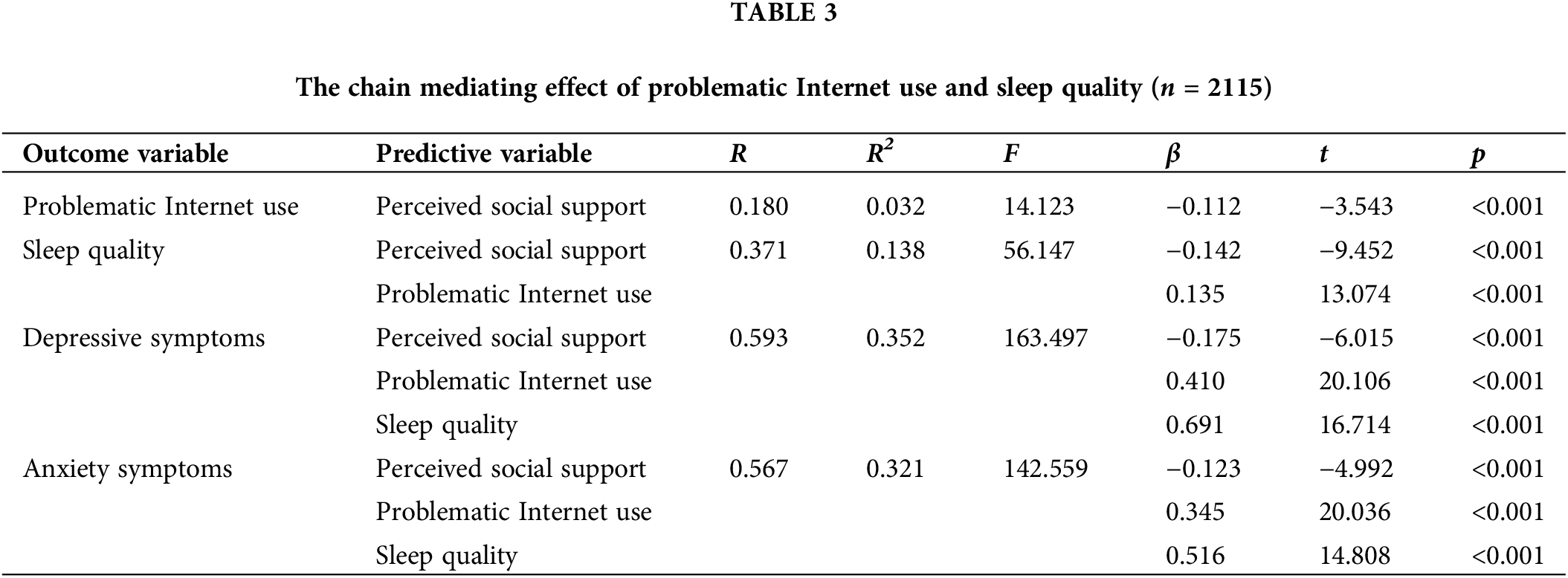
According to the results of univariate analysis, age, gender, one-child status, and social status were included as controlling variables in the mediational models. Results from this analysis revealed that perceived social support significantly negatively predicted symptoms of depression and anxiety (β = −0.330, p < 0.001; β = −0.243, p < 0.001). When PIU and sleep quality were included in the regression equation, the negative prediction of perceived social support for symptoms of depression and anxiety remained significant (β = −0.175, p < 0.001; β = −0.123, p < 0.001). Perceived social support negatively predicted PIU and sleep quality (β = −0.112, p < 0.001; β = −0.142, p < 0.001), and PIU and sleep quality were significant positive predictors of depressive symptoms (β = 0.410, p < 0.001; β = 0.691, p < 0.001) and anxiety symptoms (β = 0.345, p < 0.001; β = 0.516, p < 0.001). Furthermore, PIU had a positive predictive effect on sleep quality (β = 0.135, p < 0.001). See Table 3 for details.
Moderation by place of residence
The overall framework is shown in Figs. 1 and 2. Place of residence was added as a moderating variable. Control variables were identical to the above. The results, as detailed in Table 4, demonstrated that the interaction terms of perceived social support and place of residence were significant in predicting PIU, depressive symptoms, and anxiety symptoms (β = 0.136, p = 0.038; β = 0.143, p = 0.018; β = 0.160, p = 0.002). These suggest that place of residence moderates the relationships between perceived social support and PIU, and perceived social support and symptoms of depression and anxiety. Further simple slope analysis (Figs. 3–5) showed that perceived social support was a significant predictor of both PIU and symptoms of depression and anxiety among urban adolescents (β = −0.158, p < 0.001; β = −0.227, p < 0.001; β = −0.182, p < 0.001), while the results of rural adolescents were not significant (β = −0.022, p = 0.679; β = −0.084, p = 0.086; β = −0.021, p = 0.608).
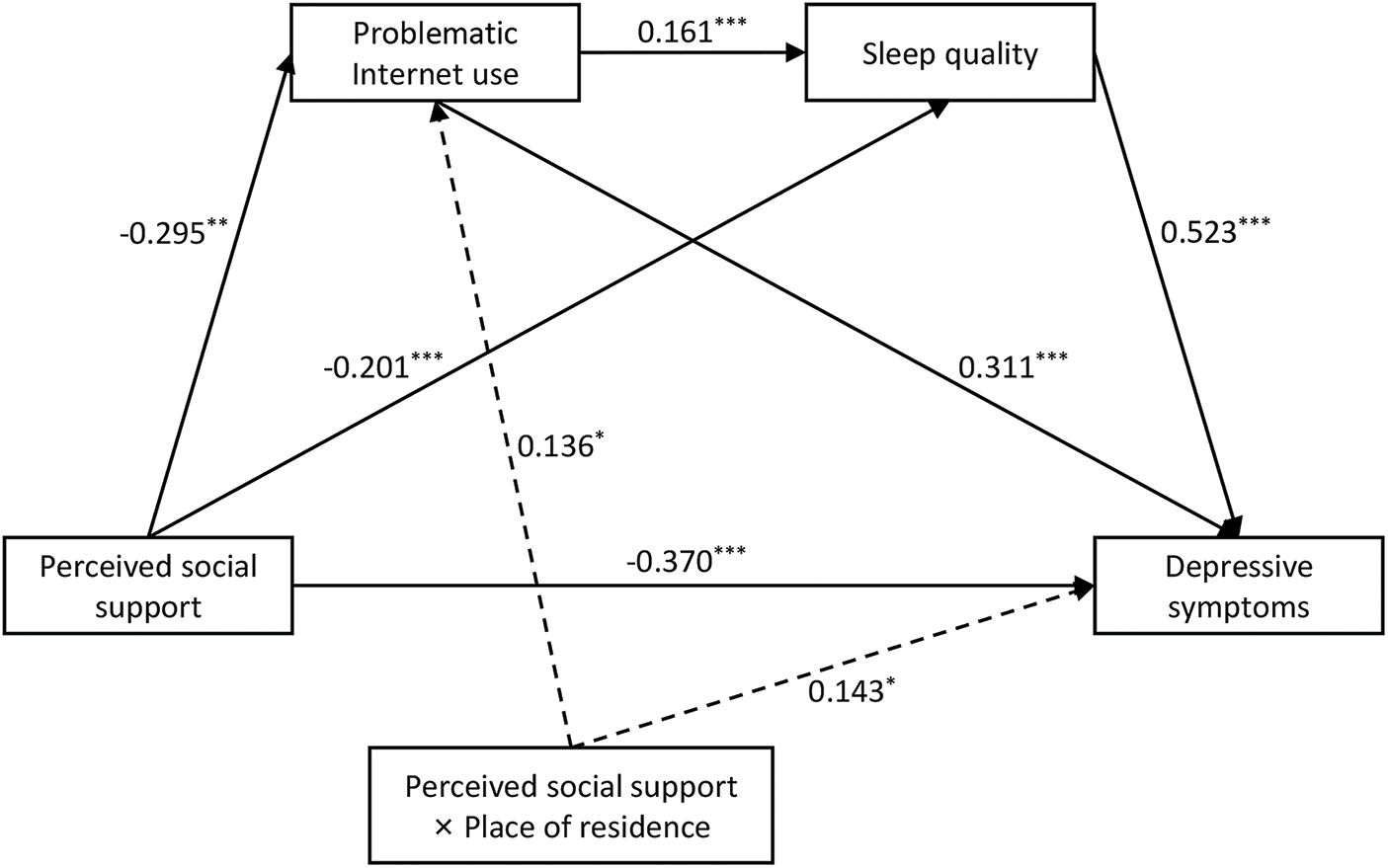
Figure 1: Indirect pathways to perceived social support and depressive symptoms, as well as the moderating role of place of residence.
Note: *p < 0.05, **p < 0.01, ***p < 0.001.
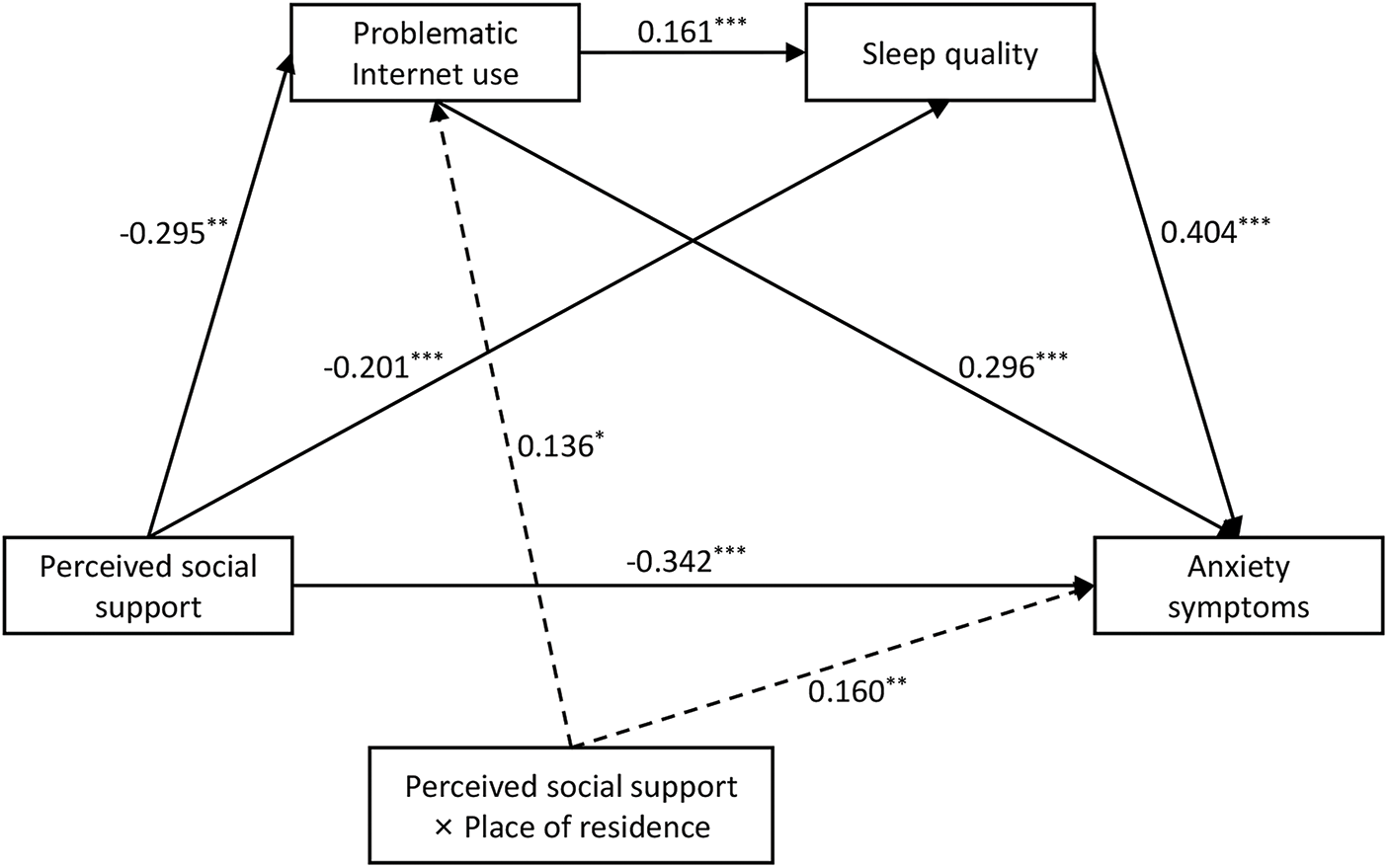
Figure 2: Indirect pathways to perceived social support and anxiety symptoms, as well as the moderating role of place of residence.
Note: *p < 0.05, **p < 0.01, ***p < 0.001.
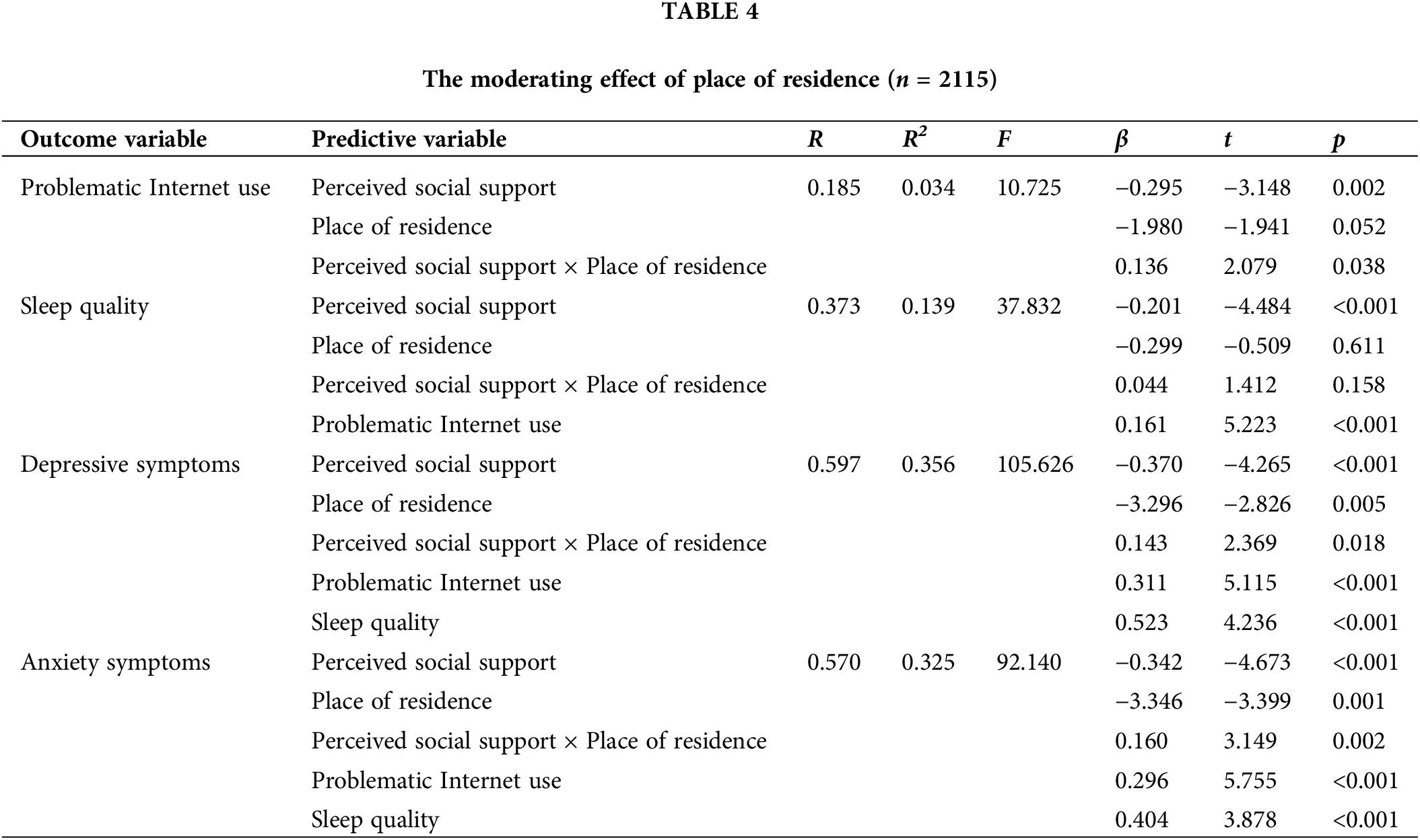
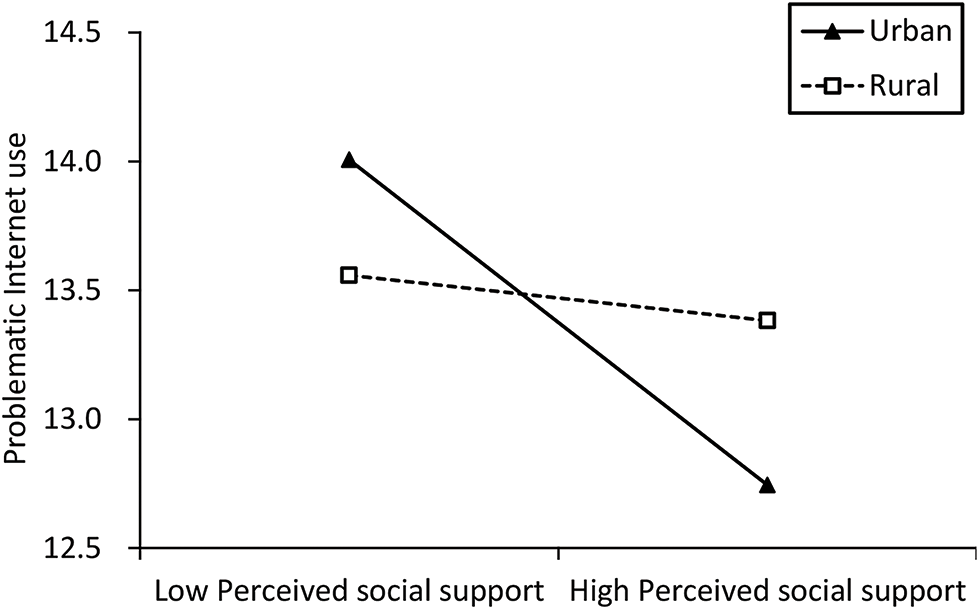
Figure 3: The moderating effect of place of residence on the relationship between perceived social support and problematic Internet use.
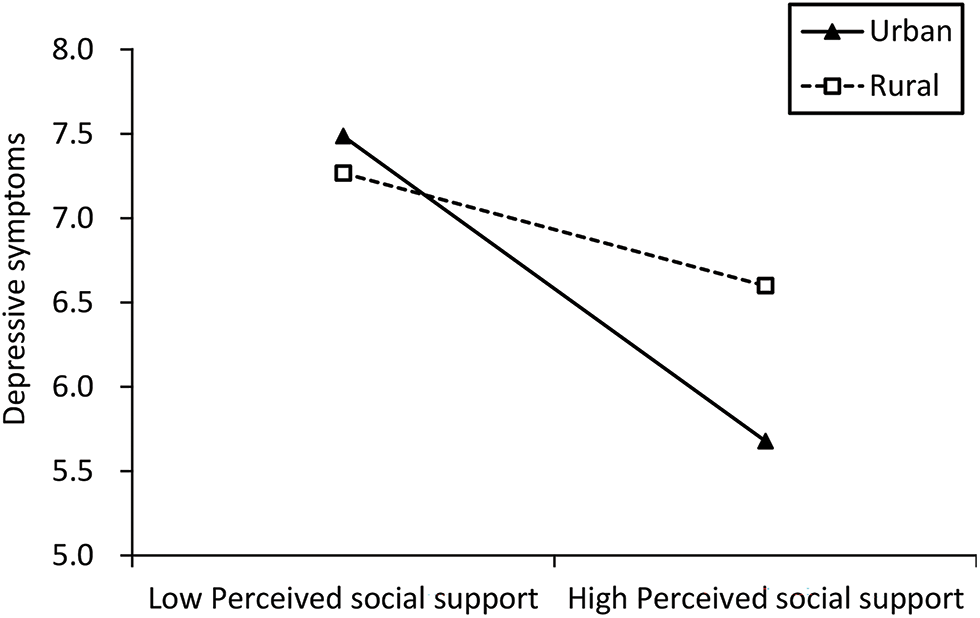
Figure 4: The moderating effect of place of residence on the relationship between perceived social support and depressive symptoms.
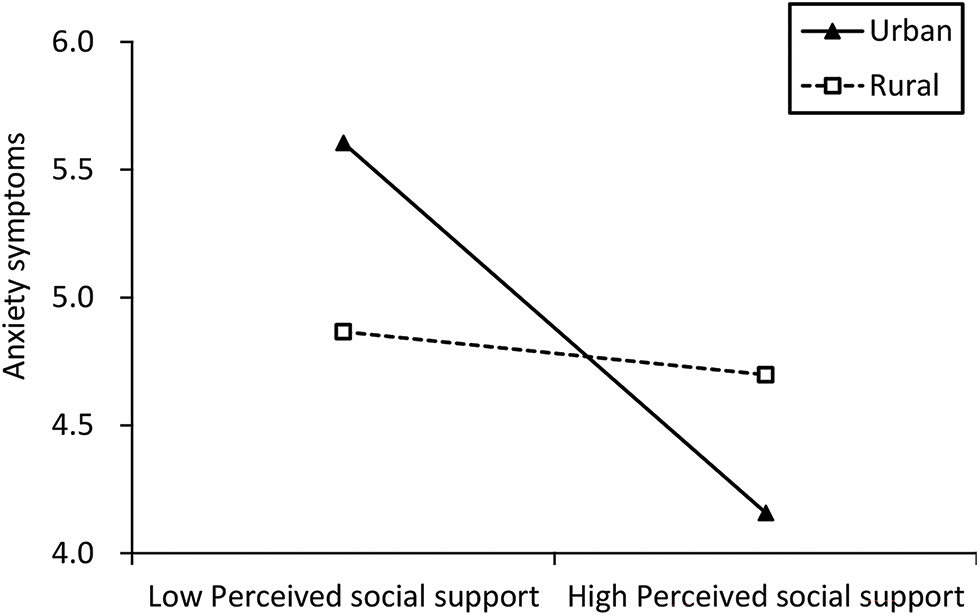
Figure 5: The moderating effect of place of residence on the relationship between perceived social support and anxiety symptoms.
This study investigated the mediating role of PIU and sleep quality in perceived social support and adolescent psychological problems based on a national survey and examined possible urban-rural differences in these relationships in the Chinese context. In the present study, nearly half of the participants reported experiencing varying degrees of symptoms of depression or anxiety. Psychological problems among teenagers cannot be ignored. We found a negative correlation between perceived social support and symptoms of depression and anxiety in adolescents. This finding has been confirmed by several studies [3,14]. In addition, PIU and sleep quality chain mediated the relationship of perceived social support with symptoms of depression and anxiety. Urban-rural differences were also found in the relationships between perceived social support and PIU and perceived social support and symptoms of depression and anxiety. These issues will be the subject of detailed discussion in the next section.
The results indicated that PIU was a mediating factor between perceived social support and depressive and anxiety symptoms. Specifically, when teenagers have low perceived social support, it may lead to more PIU, which in turn is related to symptoms of depression and anxiety. A study involving 1302 Chinese secondary school students showed that mobile phone addicts scored lower levels of social support than nonaddicts but exhibited higher levels of depressive symptoms [56]. This may be attributable to the fact that adolescents who lack sufficient social support from family members and friends are more inclined to utilize the Internet as a medium for fulfilling their social needs [57]. However, improper or excessive use of the Internet is not solely related to bad behaviors such as lack of exercise, and sitting for a long time [58]. In more severe instances, it can also precipitate the development of PIU or Internet addiction [59]. Furthermore, according to the cognitive-behavioral model of PIU [60], low levels of perceived social support can indirectly promote the formation of PIU by affecting individuals’ cognitive processes and behavioral choices. Individuals who lack social support are more likely to seek emotional support through online activities, gradually developing a dependence on and overuse of the Internet [24]. Additionally, excessive or poor Internet use may elevate the likelihood of mental health issues among adolescents. A cross-sectional case-control study of young people in Italy showed that PIU individuals exhibited higher levels of depression, anxiety, and stress, and more feelings of loneliness and boredom than non-PIU individuals [61]. Coping style theory can explain this [62], which refers to the way individuals respond to stressful events, which plays an important mediating role between stress events and health. PIU represents an unhealthy form of coping that may hinder the development of emotional regulation in adolescents [63]. Insufficient emotional regulation means that individuals have difficulty effectively controlling and expressing their emotions, which may lead to inadequate physiological and psychological defense mechanisms to cope with these stressors when facing life challenges, making individuals more susceptible to external stimuli and triggering mental health problems [64]. Furthermore, addictive or inappropriate Internet use has the potential to diminish the ability of adolescents to carry out academic tasks and exacerbate their academic burden [65]. Students are prone to negative emotions when facing academic pressure. These issues not only affect students’ academic performance but may also have long-term negative impacts on their mental health [66].
The mediating role of sleep quality
In alignment with the conclusions reached by Guo et al. [67] regarding the potential mediating mechanism linking social support and negative emotions, sleep quality was another mediator of the relationship between perceived social support and adolescent symptoms of depression and anxiety. Specifically, teenagers with poorer perceptions of social support are more susceptible to having sleep problems, increasing the risk of symptoms of depression and anxiety. One study on parental support and adolescent sleep found that parental support and good parent-child relationships can provide a sense of security for adolescents during difficult times, which is crucial for healthful sleep [34]. From an evolutionary point of view, social support, especially from family and peers, improves and enhances sleep quality by creating a safe and stable environment for adolescents [68]. Additionally, adolescents with suboptimal sleep quality were observed to be more prone to suffer from anxiety symptoms and depressive symptoms. According to a study in the United States, abnormal sleep patterns have been linked to a range of psychiatric disorders [69]. The capacity to regulate emotions is linked to sleep. Insufficient sleep can lead to a decrease in emotional regulation ability, which makes it difficult for individuals to manage their emotions effectively [70], which can easily lead to problems such as large emotional fluctuations and emotional loss of control, thereby triggering mental health issues. The decline in emotional regulation ability can also affect an individual’s cognitive ability and interpersonal relationships, reducing self-satisfaction and happiness [71]. Empirical research supports the above view that sleep restriction can lead to emotional dysregulation in adolescents and decrease their ability to regulate negative emotions [72,73]. In addition, the correlation between sleep problems and psychological disorders is linked to brain dysfunction. Sleep deprivation can result in the dysregulation of dopamine in the limbic and striatal regions of the brain. This, in turn, can disrupt the functionality of the reward processing system and increase susceptibility to psychological problems [74].
The chain mediating role of PIU and sleep quality
Moreover, the obtained results suggested that PIU and sleep quality functioned as a chain mediator. The specific pathways are perceived social support → PIU → sleep quality → symptoms of depression and anxiety. Adolescents who feel they lack social support are far more likely to utilize the Internet to fulfill their psychological needs, which may lead to PIU and poor sleep quality. Previous studies supported these findings that participants with PIU and sleep problems had lower perceived social support scores [75,76]. Additionally, prolonged or poor Internet use is associated with disturbed normal sleep patterns in adolescents [36,38]. One possible explanation is that blue light emitted by electronic devices during use prevents the secretion of melatonin and delays the phase of the biological clock, causing rhythms to be out of sync and, in the long run, leading to disruption of the circadian rhythm and disrupting normal sleep patterns [27]. An 11-month longitudinal study showed that adolescent Internet addiction prospectively predicted circadian rhythm disruption [77]. Another explanation may be that PIU leads to reduced physical activity [29] and sedentary problems [58] that affect sleep quality. In addition, prolonged use of social media before bed can delay falling asleep and reduce sleep time, while habitual delays in falling asleep can lead to changes in circadian rhythms, resulting in persistent sleep difficulties and low mood [78].
The moderating role of place of residence
An interesting finding is that our results indicated that place of residence moderated the relationships between perceived social support and PIU as well as perceived social support and both depressive and anxiety symptoms. Specifically, urban adolescents experiencing low perceived social support may exhibit a heightened propensity for developing PIU and the presentation of depressive symptoms or anxiety symptoms in comparison to their rural counterparts. Such outcomes may be explained, at least in part, by the fact that young people in urban environments encounter greater difficulties [79]. Due to urban overcrowding, lack of green space, environmental pollution, and the pervasive influence of traffic noise, teenagers living in urban areas face greater pressure [42]. Family and school, as the main sources of social networks and social support for adolescents, can alleviate various pressures faced by adolescents [80]. However, urban adolescents experience greater challenges at home and school. Teenagers living in urban areas are more prone to encounter academic apprehension, experience a greater incidence of bullying within school, and exhibit elevated levels of insecurity [81]. Moreover, researchers have found that urban adolescents have more intense conflicts and less cohesion with their parents [82]. All of these factors may contribute to decreased happiness and an elevation in psychological distress [81,83]. Additionally, teenagers tend to use the Internet as a means of mitigating and alleviating perceived stress [84]. Studies have shown that PIU among urban teenagers is a more serious phenomenon than among their rural counterparts [46,85]. A meta-analysis of Chinese adolescents also indicated that urban abode was significantly associated with Internet addiction disorder [86]. Furthermore, as evidenced by the survey findings, Internet users in China continue to be predominantly urban residents [87]. Consequently, adolescents residing in urban areas who lack social support are at higher risk for PIU and psychological distress.
It should be noted that the study has certain limitations. First, cross-sectional studies have an inherent limitation in that they cannot infer causality. Consequently, it is essential to conduct further longitudinal studies to verify causal associations. Second, self-reported scales are susceptible to potential reporting bias, so objective indicators should be considered in the future. Then, perceived social support was measured through a simplified version of the PSSS, and the outcome may be influenced by the emotional state of the individual. Subsequent consideration should be given to using objective indicators and standardized scales with more complete items. Finally, using measures that were not tailored to adolescent samples may not fully reflect their specific needs and characteristics, thereby affecting the effectiveness and applicability of the assessment. In the future, specialized measurement tools for adolescents should be adopted, taking into account their cognitive, physiological, and psychological characteristics, to ensure that the measurement tools can accurately reflect the actual situation of adolescents.
Notwithstanding these constraints, the value and significance of this study are equally noteworthy. This empirical research was set up on a large-scale, cross-sectional investigation conducted in China, which included participants from a wide range of demographic backgrounds, with a wide distribution of participants. Then, we examined the correlation between perceived social support and adolescent symptoms of depression and anxiety through the lens of PIU and sleep quality and further analyzed the distinctive urban-rural differences exerted on the above relationships to provide evidence for enhancing adolescent mental health. In theory, this can facilitate a more nuanced comprehension of adolescent mental health concerns and furnish a scientific foundation for mental health education. In practice, this can assist educators and parents in gaining a deeper comprehension of the psychological requirements of adolescents and prevent and solve psychological problems through the implementation of efficacious support and intervention strategies.
The findings reported by this research not merely validate the hypothesis that perceived social support is inversely correlated with adolescent psychological problems but enhance our comprehension of the mechanism by which perceived social support is linked to symptoms of depression and anxiety in this age demographic. Our findings suggest that reducing PIU and improving sleep quality by increasing perceived social support may contribute to an enhancement of adolescent mental health, particularly in urban areas.
Acknowledgement: We sincerely thank all participants who participated in this study.
Funding Statement: This work was supported by the MOE (Ministry of Education in China) Project of Humanities and Social Sciences (grant number 22YJCZH243) and the Chinese Government Scholarship of China Scholarship Council (grant number 202106920027).
Author Contributions: Le-Qing Jin: Visualization, Formal analysis, Writing—original draft, Writing—review & editing. Chen-Wei Pan: Visualization, Formal analysis, Writing—original draft, Writing—review & editing. Chun-Hua Zhao: Visualization, Formal analysis, Writing—original draft and Writing—review & editing. Dan-Lin Li: Visualization, Formal analysis, Writing—original draft, Writing—review & editing. Yi-Bo Wu: Conceptualization, Visualization, Formal analysis, Writing—original draft, Writing—review & editing. Tian-Yang Zhang: Conceptualization, Visualization, Formal analysis, Writing—original draft; Writing—review & editing, Validation, Funding acquisition. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data that support the findings of this study come from non-public databases. We have obtained permission to use this data.
Ethics Approval: Not applicable.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
References
1. Herpertz-Dahlmann B, Bühren K, Remschmidt H. Growing up is hard: mental disorders in adolescence. Dtsch Arztebl Int. 2013;110(25):432–40. doi:10.3238/arztebl.2013.0432. [Google Scholar] [PubMed] [CrossRef]
2. Li F, Cui Y, Li Y, Guo L, Ke X, Liu J, et al. Prevalence of mental disorders in school children and adolescents in China: diagnostic data from detailed clinical assessments of 17,524 individuals. J Child Psychol Psychiat. 2022;63(1):34–46. doi:10.1111/jcpp.13445. [Google Scholar] [PubMed] [CrossRef]
3. Liu D, Cui Z, Zhang Q, Liu F, Chen H, Wang J, et al. The mediating role of specific coping styles in the relationship between perceived social support and depressive symptoms in adolescents. J Affect Disord. 2023;325(3):647–55. doi:10.1016/j.jad.2023.01.043. [Google Scholar] [PubMed] [CrossRef]
4. Rao WW, Xu DD, Cao XL, Wen SY, Che WI, Ng CH, et al. Prevalence of depressive symptoms in children and adolescents in China: a meta-analysis of observational studies. Psychiat Res. 2019;272:790–6. doi:10.1016/j.psychres.2018.12.133. [Google Scholar] [PubMed] [CrossRef]
5. Garber J, Brunwasser SM, Zerr AA, Schwartz KT, Sova K, Weersing VR. Treatment and prevention of depression and anxiety in youth: test of cross-over effects. Depress Anxiety. 2016;33(10):939–59. doi:10.1002/da.22519. [Google Scholar] [PubMed] [CrossRef]
6. Johnson D, Dupuis G, Piche J, Clayborne Z, Colman I. Adult mental health outcomes of adolescent depression: a systematic review. Depress Anxiety. 2018;35(8):700–16. doi:10.1002/da.22777. [Google Scholar] [PubMed] [CrossRef]
7. Clayborne ZM, Varin M, Colman I. Systematic review and meta-analysis: adolescent depression and long-term psychosocial outcomes. J Am Acad Child Adolesc Psychiat. 2019;58(1):72–9. doi:10.1016/j.jaac.2018.07.896. [Google Scholar] [PubMed] [CrossRef]
8. Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, et al. Adolescence and the social determinants of health. Lancet. 2012;379(9826):1641–52. doi:10.1016/S0140-6736(12)60149-4. [Google Scholar] [PubMed] [CrossRef]
9. Bokhorst CL, Sumter SR, Westenberg PM. Social support from parents, friends, classmates, and teachers in children and adolescents aged 9 to 18 years: who is perceived as most supportive? Soc Dev. 2010;19(2):417–26. doi:10.1111/j.1467-9507.2009.00540.x. [Google Scholar] [CrossRef]
10. Thoits PA. Stress, coping, and social support processes: where are we? What next? J Health Soc Behav. 1995;35:53–79. doi:10.2307/2626957. [Google Scholar] [CrossRef]
11. Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. 2011;52(2):145–61. doi:10.1177/0022146510395592. [Google Scholar] [PubMed] [CrossRef]
12. Poudel A, Gurung B, Khanal GP. Perceived social support and psychological wellbeing among Nepalese adolescents: the mediating role of self-esteem. BMC Psychol. 2020;8(1):43. doi:10.1186/s40359-020-00409-1. [Google Scholar] [PubMed] [CrossRef]
13. Milner A, Krnjacki L, LaMontagne AD. Age and gender differences in the influence of social support on mental health: a longitudinal fixed-effects analysis using 13 annual waves of the HILDA cohort. Public Health. 2016;140:172–8. doi:10.1016/j.puhe.2016.06.029. [Google Scholar] [PubMed] [CrossRef]
14. Väänänen JM, Marttunen M, Helminen M, Kaltiala-Heino R. Low perceived social support predicts later depression but not social phobia in middle adolescence. Health Psychol Behav Med. 2014;2(1):1023–37. doi:10.1080/21642850.2014.966716. [Google Scholar] [PubMed] [CrossRef]
15. Paul B, Bryant JA. Adolescents and the internet. Adolesc Med Clin. 2005;16(2):413–26. doi:10.1016/j.admecli.2005.03.001. [Google Scholar] [PubMed] [CrossRef]
16. Reid Chassiakos YL, Radesky J, Christakis D, Moreno MA, Cross C, Council on Communications and Media, et al. Children and adolescents and digital media. Pediatrics. 2016;138(5):e20162593. doi:10.1542/peds.2016-2593. [Google Scholar] [PubMed] [CrossRef]
17. Spada MM. An overview of problematic internet use. Addict Behav. 2014;39(1):3–6. doi:10.1016/j.addbeh.2013.09.007. [Google Scholar] [PubMed] [CrossRef]
18. Cai Z, Mao P, Wang Z, Wang D, He J, Fan X. Associations between problematic internet use and mental health outcomes of students: a meta-analytic review. Adolesc Res Rev. 2023;8(1):45–62. doi:10.1007/s40894-022-00201-9. [Google Scholar] [PubMed] [CrossRef]
19. Huang Y, Xu L, Mei Y, Wei Z, Wen H, Liu D. Problematic internet use and the risk of suicide ideation in Chinese adolescents: a cross-sectional analysis. Psychiat Res. 2020;290(6):112963. doi:10.1016/j.psychres.2020.112963. [Google Scholar] [PubMed] [CrossRef]
20. Karacic S, Oreskovic S. Internet addiction through the phase of adolescence: a questionnaire study. JMIR Ment Health. 2017;4(2):e11. doi:10.2196/mental.5537. [Google Scholar] [PubMed] [CrossRef]
21. Zhang Y, Wang D, Ma Z, Liu W, Su Y, Wang W, et al. Problematic internet use and suicide ideation among Chinese adolescents: the indirect effects of insomnia, nightmares, and social jetlag. J Affect Disord. 2024;344:347–55. doi:10.1016/j.jad.2023.10.081. [Google Scholar] [PubMed] [CrossRef]
22. Lu X, Zhang M, Zhang J. The relationship between social support and internet addiction among Chinese college freshmen: a mediated moderation model. Front Psychol. 2023;13:1031566. doi:10.3389/fpsyg.2022.1031566. [Google Scholar] [PubMed] [CrossRef]
23. Wu XS, Zhang ZH, Zhao F, Wang WJ, Li YF, Bi L, et al. Prevalence of internet addiction and its association with social support and other related factors among adolescents in China. J Adolesc. 2016;52(1):103–11. doi:10.1016/j.adolescence.2016.07.012. [Google Scholar] [PubMed] [CrossRef]
24. Cui X, Chi X. The relationship between social support and internet addiction among Chinese adolescents during the COVID-19 pandemic: a multiple mediation model of resilience and post-traumatic stress disorder symptoms. Psychol Res Behav Manag. 2021;14:1665–74. doi:10.2147/PRBM.S305510. [Google Scholar] [PubMed] [CrossRef]
25. Tarokh L, Saletin JM, Carskadon MA. Sleep in adolescence: physiology, cognition and mental health. Neurosci Biobehav Rev. 2016;70(952):182–8. doi:10.1016/j.neubiorev.2016.08.008. [Google Scholar] [PubMed] [CrossRef]
26. Agostini A, Centofanti S. Normal sleep in children and adolescence. Child Adolesc Psychiatr Clin N Am. 2021;30(1):1–14. doi:10.1016/j.chc.2020.08.011. [Google Scholar] [PubMed] [CrossRef]
27. Touitou Y, Touitou D, Reinberg A. Disruption of adolescents’ circadian clock: the vicious circle of media use, exposure to light at night, sleep loss and risk behaviors. J Physiol Paris. 2016;110(4):467–79. doi:10.1016/j.jphysparis.2017.05.001. [Google Scholar] [PubMed] [CrossRef]
28. Owens JA, Weiss MR. Insufficient sleep in adolescents: causes and consequences. Minerva Pediatr. 2017;69(4):326–36. doi:10.23736/S0026-4946.17.04914-3. [Google Scholar] [PubMed] [CrossRef]
29. An J, Sun Y, Wan Y, Chen J, Wang X, Tao F. Associations between problematic internet use and adolescents’ physical and psychological symptoms: possible role of sleep quality. J Addict Med. 2014;8(4):282–7. doi:10.1097/ADM.0000000000000026. [Google Scholar] [PubMed] [CrossRef]
30. Xue B, Xue Y, Zheng X, Shi L, Liang P, Dong F, et al. Association of sleep with mental health in Chinese high school students: a cross-sectional study. J Sleep Res. 2022;31(6):e13697. doi:10.1111/jsr.13697. [Google Scholar] [PubMed] [CrossRef]
31. Roberts RE, Duong HT. The prospective association between sleep deprivation and depression among adolescents. Sleep. 2014;37(2):239–44. doi:10.5665/sleep.3388. [Google Scholar] [PubMed] [CrossRef]
32. Maume DJ. Social ties and adolescent sleep disruption. J Health Soc Behav. 2013;54(4):498–515. doi:10.1177/0022146513498512. [Google Scholar] [PubMed] [CrossRef]
33. van Schalkwijk FJ, Blessinga AN, Willemen AM, Van Der Werf YD, Schuengel C. Social support moderates the effects of stress on sleep in adolescents. J Sleep Res. 2015;24(4):407–13. doi:10.1111/jsr.12298. [Google Scholar] [PubMed] [CrossRef]
34. Tsai KM, Dahl RE, Irwin MR, Bower JE, McCreath H, Seeman TE, et al. The roles of parental support and family stress in adolescent sleep. Child Dev. 2018;89(5):1577–88. doi:10.1111/cdev.12917. [Google Scholar] [PubMed] [CrossRef]
35. Islam Z, Hsan K, Islam S, Gozal D, Hossain M. Assessment of sleep quality and its association with problematic internet use among university students: a cross-sectional investigation in Bangladesh. Sleep Sci. 2021;14(S 01):8–15. doi:10.5935/1984-0063.20200069. [Google Scholar] [PubMed] [CrossRef]
36. Kokka I, Mourikis I, Nicolaides NC, Darviri C, Chrousos GP, Kanaka-Gantenbein C, et al. Exploring the effects of problematic internet use on adolescent sleep: a systematic review. Int J Environ Res Public Health. 2021;18(2):760. doi:10.3390/ijerph18020760. [Google Scholar] [PubMed] [CrossRef]
37. Islamie Farsani S, Allahbakhshi K, Valipour AA, Mohammadian-Hafshejani A. Some facts on problematic internet use and sleep disturbance among adolescents. Iran J Public Health. 2016;45(11):1531–2. [Google Scholar] [PubMed]
38. Yang J, Guo Y, Du X, Jiang Y, Wang W, Xiao D, et al. Association between problematic internet use and sleep disturbance among adolescents: the role of the child’s sex. Int J Environ Res Public Health. 2018;15(12):2682. doi:10.3390/ijerph15122682. [Google Scholar] [PubMed] [CrossRef]
39. Tereshchenko S, Kasparov E, Smolnikova M, Shubina M, Gorbacheva N, Moskalenko O. Internet addiction and sleep problems among Russian adolescents: a field school-based study. Int J Environ Res Public Health. 2021;18(19):10397. doi:10.3390/ijerph181910397. [Google Scholar] [PubMed] [CrossRef]
40. Zhou M, Zhu W, Sun X, Huang L. Internet addiction and child physical and mental health: evidence from panel dataset in China. J Affect Disord. 2022;309(1):52–62. doi:10.1016/j.jad.2022.04.115. [Google Scholar] [PubMed] [CrossRef]
41. Liu H, Fan X, Luo H, Zhou Z, Shen C, Hu N, et al. Comparison of depressive symptoms and its influencing factors among the elderly in urban and rural areas: evidence from the China health and retirement longitudinal study (CHARLS). Int J Environ Res Public Health. 2021;18(8):3886. doi:10.3390/ijerph18083886. [Google Scholar] [PubMed] [CrossRef]
42. Okkels N, Kristiansen CB, Munk-Jørgensen P, Sartorius N. Urban mental health: challenges and perspectives. Curr Opin Psychiat. 2018;31(3):258–64. doi:10.1097/YCO.0000000000000413. [Google Scholar] [PubMed] [CrossRef]
43. Liu J, Yang L, Zheng Y, Kang C, Wang X, Shi J, et al. Rural-urban differences in prevalence and correlates of suicidal ideation in adolescent patients with depression in a large sample of Chinese. J Affect Disord. 2023;322(Suppl. 1):118–24. doi:10.1016/j.jad.2022.11.032. [Google Scholar] [PubMed] [CrossRef]
44. Zhang X, Yan Y, Ye Z, Xie J. Descriptive analysis of depression among adolescents in Huangshi, China. BMC Psychiat. 2023;23(1):176. doi:10.1186/s12888-023-04682-3. [Google Scholar] [PubMed] [CrossRef]
45. Lecic-Tosevski D. Is urban living good for mental health? Curr Opin Psychiat. 2019;32(3):204–9. doi:10.1097/YCO.0000000000000489. [Google Scholar] [PubMed] [CrossRef]
46. Stavropoulos V, Alexandraki K, Motti-Stefanidi F. Recognizing internet addiction: prevalence and relationship to academic achievement in adolescents enrolled in urban and rural Greek high schools. J Adolesc. 2013;36(3):565–76. doi:10.1016/j.adolescence.2013.03.008. [Google Scholar] [PubMed] [CrossRef]
47. Zhang X, Lewis S, Firth J, Chen X, Bucci S. Digital mental health in China: a systematic review. Psychol Med. 2021;51(15):2552–70. doi:10.1017/S0033291721003731. [Google Scholar] [PubMed] [CrossRef]
48. Wang Y, Kaierdebieke A, Fan S, Zhang R, Huang M, Li H, et al. Study protocol: a cross-sectional study on psychology and behavior investigation of Chinese residents. PBICR Psychosom Med Res. 2022;4(3):19. doi:10.53388/202219. [Google Scholar] [CrossRef]
49. Miao YF, Dong XX, Li DL, Zhang T, Wu Y, Pan CW. Chronic conditions and depressive symptoms in middle-aged and older Chinese adults: roles of perceived social support and area of residence. J Affect Disord. 2023;340:290–8. doi:10.1016/j.jad.2023.08.045. [Google Scholar] [PubMed] [CrossRef]
50. Fonseca-Pedrero E, Díez-Gómez A, Pérez-Albéniz A, Al-Halabí S, Lucas-Molina B, Debbané M. Youth screening depression: validation of the patient health questionnaire-9 (PHQ-9) in a representative sample of adolescents. Psychiat Res. 2023;328:115486. doi:10.1016/j.psychres.2023.115486. [Google Scholar] [PubMed] [CrossRef]
51. Sun J, Liang K, Chi X, Chen S. Psychometric properties of the generalized anxiety disorder scale-7 item (GAD-7) in a large sample of Chinese adolescents. Healthcare. 2021;9(12):1709. doi:10.3390/healthcare9121709. [Google Scholar] [PubMed] [CrossRef]
52. Dong XX, Li DL, Miao YF, Zhang T, Wu Y, Pan CW. Prevalence of depressive symptoms and associated factors during the COVID-19 pandemic: a national-based study. J Affect Disord. 2023;333:1–9. doi:10.1016/j.jad.2023.04.034. [Google Scholar] [PubMed] [CrossRef]
53. Yu Y, Wu Y, Chen P, Min H, Sun X. Associations between personality and problematic internet use among Chinese adolescents and young adults: a network analysis. J Affect Disord. 2024;365:501–8. doi:10.1016/j.jad.2024.08.069. [Google Scholar] [PubMed] [CrossRef]
54. Sancho-Domingo C, Carballo JL, Coloma-Carmona A, Buysse DJ. Brief version of the Pittsburgh sleep quality index (B-PSQI) and measurement invariance across gender and age in a population-based sample. Psychol Assess. 2021;33(2):111–21. doi:10.1037/pas0000959. [Google Scholar] [PubMed] [CrossRef]
55. Sancho-Domingo C, Carballo JL, Coloma-Carmona A, Buysse DJ. Psychometric adaptation of the Spanish version of the brief Pittsburgh sleep quality index in adolescents. J Pediatr Psychol. 2024;49(8):596–604. doi:10.1093/jpepsy/jsae046. [Google Scholar] [PubMed] [CrossRef]
56. Li M, Jiang X, Ren Y. Mediator effects of positive emotions on social support and depression among adolescents suffering from mobile phone addiction. Psychiat Danub. 2017;29(2):207–13. doi:10.24869/psyd.2017.207. [Google Scholar] [PubMed] [CrossRef]
57. Karaer Y, Akdemir D. Parenting styles, perceived social support and emotion regulation in adolescents with internet addiction. Compr Psychiat. 2019;92:22–7. doi:10.1016/j.comppsych.2019.03.003. [Google Scholar] [PubMed] [CrossRef]
58. Damato TM, Tebar WR, Oliveira CBS, Saraiva BTC, Morelhao PK, Ritti-Dias RM, et al. Relationship of sleep quality with screen-based sedentary time and physical activity in adolescents—the moderating effect of body mass index. Sleep Breath. 2022;26(4):1809–16. doi:10.1007/s11325-021-02519-5. [Google Scholar] [PubMed] [CrossRef]
59. Guo L, Luo M, Wang WX, Huang GL, Xu Y, Gao X, et al. Association between problematic internet use, sleep disturbance, and suicidal behavior in Chinese adolescents. J Behav Addict. 2018;7(4):965–75. doi:10.1556/2006.7.2018.115. [Google Scholar] [PubMed] [CrossRef]
60. Davis RA. A cognitive-behavioral model of pathological internet use. Comput Human Behav. 2001;17(2):187–95. doi:10.1016/S0747-5632(00)00041-8. [Google Scholar] [CrossRef]
61. Orsolini L, Longo G, Volpe U. The mediatory role of the boredom and loneliness dimensions in the development of problematic internet use. Int J Environ Res Public Health. 2023;20(5):4446. doi:10.3390/ijerph20054446. [Google Scholar] [PubMed] [CrossRef]
62. Lazarus RS, Folkman S. Stress appraisal, and coping. New York: Springer Publishing Company; 1984. [Google Scholar]
63. Moritz S, Jahns AK, Schröder J, Berger T, Lincoln TM, Klein JP, et al. More adaptive versus less maladaptive coping: what is more predictive of symptom severity? Development of a new scale to investigate coping profiles across different psychopathological syndromes. J Affect Disord. 2016;191:300–7. doi:10.1016/j.jad.2015.11.027. [Google Scholar] [PubMed] [CrossRef]
64. Adrian M, Jenness JL, Kuehn KS, Smith MR, McLaughlin KA. Emotion regulation processes linking peer victimization to anxiety and depression symptoms in adolescence. Dev Psychopathol. 2019;31(3):999–1009. doi:10.1017/S0954579419000543. [Google Scholar] [PubMed] [CrossRef]
65. Liu S, Zou S, Zhang D, Wang X, Wu X. Problematic internet use and academic engagement during the COVID-19 lockdown: the indirect effects of depression, anxiety, and insomnia in early, middle, and late adolescence. J Affect Disord. 2022;309:9–18. doi:10.1016/j.jad.2022.04.043. [Google Scholar] [PubMed] [CrossRef]
66. Steare T, Gutiérrez Muñoz C, Sullivan A, Lewis G. The association between academic pressure and adolescent mental health problems: a systematic review. J Affect Disord. 2023;339(70):302–17. doi:10.1016/j.jad.2023.07.028. [Google Scholar] [PubMed] [CrossRef]
67. Guo T, Zhang Z, Taylor A, Hall DL, Yeung AS, Kramer AF, et al. Association of social support with negative emotions among Chinese adolescents during omicron-related lockdown of Shenzhen city: the roles of rumination and sleep quality. Front Psychiatry. 2022;13:957382. doi:10.3389/fpsyt.2022.957382. [Google Scholar] [PubMed] [CrossRef]
68. Kent de Grey RG, Uchino BN, Trettevik R, Cronan S, Hogan JN. Social support and sleep: a meta-analysis. Health Psychol. 2018;37(8):787–98. doi:10.1037/hea0000628. [Google Scholar] [PubMed] [CrossRef]
69. Zhang J, Paksarian D, Lamers F, Hickie IB, He J, Merikangas KR. Sleep patterns and mental health correlates in US adolescents. J Pediatr. 2017;182:137–43. doi:10.1016/j.jpeds.2016.11.007. [Google Scholar] [PubMed] [CrossRef]
70. Short MA, Chee MWL. Adolescent sleep restriction effects on cognition and mood. Prog Brain Res. 2019;246(7):55–71. doi:10.1016/bs.pbr.2019.02.008. [Google Scholar] [PubMed] [CrossRef]
71. McLaughlin KA, Hatzenbuehler ML, Mennin DS, Nolen-Hoeksema S. Emotion dysregulation and adolescent psychopathology: a prospective study. Behav Res Ther. 2011;49(9):544–54. doi:10.1016/j.brat.2011.06.003. [Google Scholar] [PubMed] [CrossRef]
72. Baum KT, Desai A, Field J, Miller LE, Rausch J, Beebe DW. Sleep restriction worsens mood and emotion regulation in adolescents. J Child Psychol Psychiat. 2014;55(2):180–90. doi:10.1111/jcpp.12125. [Google Scholar] [PubMed] [CrossRef]
73. Fisher RS, Dattilo TM, Sharkey CM, Traino KA, Espeleta HC, Krietsch KN, et al. Sleep patterns related to emotion dysregulation among adolescents and young adults. J Pediatr Psychol. 2022;47(1):111–20. doi:10.1093/jpepsy/jsab084. [Google Scholar] [PubMed] [CrossRef]
74. Wang W, Du X, Guo Y, Li W, Teopiz KM, Shi J, et al. The associations between sleep situations and mental health among Chinese adolescents: a longitudinal study. Sleep Med. 2021;82(5):71–7. doi:10.1016/j.sleep.2021.03.009. [Google Scholar] [PubMed] [CrossRef]
75. Nowak M, Rachubińska K, Starczewska M, Grochans E. Seeking relationships between internet addiction and depressiveness, daytime sleepiness, as well as perceived social support in young adults. Eur Rev Med Pharmacol Sci. 2022;26(4):1374–81. doi:10.26355/eurrev_202202_28130. [Google Scholar] [PubMed] [CrossRef]
76. Orhon F, Ergin A, Topçu S, Çolak B, Almiş H, Durmaz N, et al. The role of social support on the relationships between internet use and sleep problems in adolescents during COVID-19 pandemic: a multicentre study. Child Adolesc Ment Health. 2023;28(1):117–23. doi:10.1111/camh.12626. [Google Scholar] [PubMed] [CrossRef]
77. Chen YL, Gau SS. Sleep problems and internet addiction among children and adolescents: a longitudinal study. J Sleep Res. 2016;25(4):458–65. doi:10.1111/jsr.12388. [Google Scholar] [PubMed] [CrossRef]
78. Alonzo R, Hussain J, Stranges S, Anderson KK. Interplay between social media use, sleep quality, and mental health in youth: a systematic review. Sleep Med Rev. 2021;56(2):101414. doi:10.1016/j.smrv.2020.101414. [Google Scholar] [PubMed] [CrossRef]
79. Landis D, Gaylord-Harden NK, Malinowski SL, Grant KE, Carleton RA, Ford RE. Urban adolescent stress and hopelessness. J Adolesc. 2007;30(6):1051–70. doi:10.1016/j.adolescence.2007.02.001. [Google Scholar] [PubMed] [CrossRef]
80. Gong Z, Lv Y, Jiao X, Liu J, Sun Y, Qu Q. The relationship between COVID-19-related restrictions and fear of missing out, problematic smartphone use, and mental health in college students: the moderated moderation effect of resilience and social support. Front Public Health. 2022;10:986498. doi:10.3389/fpubh.2022.986498. [Google Scholar] [PubMed] [CrossRef]
81. Boraita RJ, Alsina DA, Ibort EG, Torres JMD. Quality of life related to health and habits: differences between adolescents in rural and urban environments. An Pediatr (Engl Ed). 2022;96(3):196–202. doi:10.1016/j.anpede.2020.11.016. [Google Scholar] [PubMed] [CrossRef]
82. Zhang W, Fuligni AJ. Authority, autonomy, and family relationships among adolescents in urban and rural China. J Res Adolesc. 2006;16(4):527–37. doi:10.1111/j.1532-7795.2006.00506.x. [Google Scholar] [CrossRef]
83. Man X, Liu J, Xue Z. Effects of bullying forms on adolescent mental health and protective factors: a global cross-regional research based on 65 countries. Int J Environ Res Public Health. 2022;19(4):2374. doi:10.3390/ijerph19042374. [Google Scholar] [PubMed] [CrossRef]
84. Shen X, Wang C, Chen C, Wang Y, Wang Z, Zheng Y, et al. Stress and internet addiction: mediated by anxiety and moderated by self-control. Psychol Res Behav Manag. 2023;16:1975–86. doi:10.2147/PRBM.S411412. [Google Scholar] [PubMed] [CrossRef]
85. Ying Ying C, Awaluddin SM, Kuang Kuay L, Siew Man C, Baharudin A, Miaw Yn L, et al. Association of internet addiction with adolescents’ lifestyle: a national school-based survey. Int J Environ Res Public Health. 2020;18(1):168. doi:10.3390/ijerph18010168. [Google Scholar] [PubMed] [CrossRef]
86. Li L, Xu DD, Chai JX, Wang D, Li L, Zhang L, et al. Prevalence of internet addiction disorder in Chinese university students: a comprehensive meta-analysis of observational studies. J Behav Addict. 2018;7(3):610–23. doi:10.1556/2006.7.2018.53. [Google Scholar] [PubMed] [CrossRef]
87. Nie W, Hu M, Ye X. Internet use and rural-urban mental health inequalities: evidence from China. Front Public Health. 2023;11:1107146. doi:10.3389/fpubh.2023.1107146. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools