 Open Access
Open Access
ARTICLE
Association between Mental Distress and Weight-Related Self-Stigma via Problematic Social Media and Smartphone Use among Malaysian University Students: An Application of the Interaction of Person-Affect-Cognition- Execution (I-PACE) Model
1 Department of Nutrition, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Serdang, 43400, Malaysia
2 Department of Family Medicine, E-Da Hospital, I-Shou University, Kaohsiung, 82445, Taiwan
3 Bariatric and Metabolism International Surgery Center, E-Da Hospital, I-Shou University, Kaohsiung, 82445, Taiwan
4 Institute of Environmental Toxin and Emerging Contaminant, Cheng Shiu University, Kaohsiung, 83347, Taiwan
5 Center for Environmental Toxin and Emerging-Contaminant Research, Cheng Shiu University, Kaohsiung, 83347, Taiwan
6 Division of Nutrition, Dietetics and Food Science, School of Health Sciences, IMU University, Bukit Jalil, Kuala Lumpur, 57000, Malaysia
7 Sunway Business School, Sunway University, Selangor, 47500, Malaysia
8 Faculty of Education, Universiti Malaya, Kuala Lumpur, 50603, Malaysia
9 School of Social Sciences, Faculty of Arts, Monash University, Melbourne, VIC 3800, Australia
10 Department of Community Health Nursing, Faculty of Nursing, Universitas Padjadjaran, West Java, 45363, Indonesia
11 Institute of Allied Health Sciences, College of Medicine, National Cheng Kung University, Tainan, 701401, Taiwan
12 Department of Medical Research, E-Da Hospital, I-Shou University, Kaohsiung, 82445, Taiwan
13 International Gaming Research Unit, Psychology Department, Nottingham Trent University, Nottingham, NG1 4FQ, UK
14 Biostatistics Consulting Center, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, 701401, Taiwan
15 School of Nursing, College of Nursing, Kaohsiung Medical University, Kaohsiung, 807378, Taiwan
* Corresponding Authors: Wan Ying Gan. Email: ; Chung-Ying Lin. Email:
# Both authors shared the equal contribution to the co-first authorship
(This article belongs to the Special Issue: Mattering in the Digital Era: Exploring Its Role in Internet Use Patterns and Mental Health Outcomes)
International Journal of Mental Health Promotion 2025, 27(3), 319-331. https://doi.org/10.32604/ijmhp.2025.060049
Received 22 October 2024; Accepted 08 February 2025; Issue published 31 March 2025
Abstract
Background: Weight-related self-stigma (WRSS) is prevalent among individuals with different types of weight status and is associated with a range of negative health outcomes. Social support and coping models explain how individuals may use different coping methods to deal with their mental health needs. Psychological distress (e.g., depression and stress) could lead to overuse of social media and smartphones. When using social media or smartphones, individuals are likely to be exposed to negative comments regarding weight/shape/size posted on the social media. Consequently, individuals who experience problematic social media use (PSMU) or problematic smartphone use (PSPU) may develop WRSS. Therefore, the present study examined the roles of PSMU and PSPU as mediators in the relationship between psychological distress and WRSS. Methods: Using convenience sampling via an online survey, 622 participants with a mean age of 23.70 years (SD = 4.33) completed questions assessing sociodemographic variables, psychological distress, PSMU, PSPU, WRSS, and self-reported weight and height. Results: The hierarchical regression models showed that sex (β = 0.08, p = 0.01), BMI (β = 0.39, p < 0.001), depression (β = 0.21, p = 0.001), stress (β = 0.18, p = 0.01), PSMU (β = 0.09, p = 0.045), and PSPU (β = 0.14, p = 0.001) were significant factors for WRSS. Conclusion: The mediation models showed that both PSMU and PSPU were significant mediators in the relationships between depression and stress with WRSS. The present findings provide some evidence for understanding WRSS and has important implications for developing interventions to reduce its negative impact on individuals’ health and well-being.Keywords
Supplementary Material
Supplementary Material FileAbbreviations
| I-PACE | Interaction of Person-Affect-Cognition-Execution |
| PSMU | Problematic Social Media Use |
| PSPU | Problematic Smartphone Use |
| DASS-21 | Depression, Anxiety, Stress Scale |
| BSMAS | Bergen Social Media Addiction Scale |
| SABAS | Smartphone-Application Based Addiction Scale |
| WSSQ | Weight Self-Stigma Questionnaire |
Weight stigma, also known as weight bias or weight discrimination, is the societally constructed rejection or marginalization of individuals due to negative perceptions of their body weight and size, which can lead to low self-esteem, internalized shame, and decreased motivation to engage in health behaviors [1], eventually resulting in weight gain and difficulty in losing weight [2]. Moreover, there has been increasing evidence showing increased changes in body weight and body mass index, leading to potential increasing public health concerns regarding obesity and being overweight and their related health-risks [3–6].
Weight stigma is highly prevalent among youth, particularly among those with obesity [1,7,8]. The prevalence of weight stigma among adults has been found to be as high as 46.4% in Saudi Arabia [9] and 65.6% in Singapore [10]. Weight stigma has been associated with a range of negative health outcomes including disordered eating [11], food addiction [12], poor mental health [13], and poor quality of life [14].
One cohort who experiences weight-related self-stigma (WRSS, a special type of weight stigma; i.e., individuals who internalize weight stigma to themselves) is university students. They may feel ashamed, embarrassed, and inadequate, leading to psychological distress and decreased self-esteem [15]. This university student population represents a critical demographic for examining WRSS due to the unique challenges they face during this transitional life stage. University students often encounter significant changes in body image perceptions, increased exposure to social media, and increased peer influences, all of which can contribute to the development of negative self-perceptions and weight stigma. In addition, university students are at a critical stage in establishing lifelong health behaviors, making it imperative to understand the psychological impact of weight stigma on their overall well-being. As many students struggle with the pressures of academic life, social comparisons, and emerging adulthood, their experiences may profoundly influence their mental health and future health behaviors [12–14]. Additionally, they may also feel discouraged from engaging in physical activity due to fear of judgment or discrimination [16,17]. This, in turn, can lead to a sedentary lifestyle, which can negatively impact their physical health, such as increasing the risk of non-communicable diseases and obesity. Therefore, understanding the development of WRSS among university students is crucial for developing effective interventions to reduce its negative impacts.
University students often spend significant amounts of time using internet-enabled electronic devices (e.g., smartphones), leading to increased social media use [18]. This behavior was particularly pronounced during the COVID-19 pandemic [19–21], resulting in problematic social media use (PSMU) among this cohort. PSMU (referred to by some scholars in its most extreme form as ‘social media addiction’), is a theorized form of psychological or behavioral dependence on social media platforms. Similarly, problematic smartphone use (PSPU) is another type of behavioral or psychological dependence and is closely related to other forms of problematic digital media use, such as internet addiction disorder [21]. Both PSMU and PSPU have been shown to adversely affect university students by impacting academic performance, social interactions, sleep duration, and promoting sedentary lifestyle [22].
There has been increased interest by researchers in the field of body image to understand the role of PSMU and PSPU in alleviating and exacerbating weight stigma [23]. Social media can be a source of negative weight-related messages (e.g., diet and weight loss advertisements, body shaming, and fat phobia) in which such messages can lead to body dissatisfaction and WRSS across individuals with different types of weight status (including obesity, overweight, normal weight, and underweight) [23,24]. On the other hand, social media can also serve as a positive platform for individuals to promote body appreciation and acceptance [23]. A longitudinal study across different periods of COVID-19 epidemic in China found that PSMU and PSPU were significantly associated with perceived weight stigma among schoolchildren [25]. However, this relationship is unclear among university students.
An important yet underexplored aspect of this relationship is the role of social comparison in social media use. Previous research has shown that upward comparisons, in which individuals compare themselves to those they perceive as more attractive or successful, can be an important driver of negative outcomes such as body dissatisfaction, low self-esteem, and increased WRSS [26,27]. Meta-analyses have found that the effects of social media use on body image and related psychological distress tend to be small, but depend on how individuals engage with social media [28,29]. More specifically, frequent exposure to idealized body images and the tendency to make social comparisons are associated with more negative psychological outcomes [24]. Despite these findings, previous studies have not fully examined the underlying mechanisms that explain the relationship between PSMU, PSPU, and WRSS.
Some theories or frameworks, such as social support and coping models [30] and the Interaction of Person-Affect-Cognition-Execution (I-PACE) model [31] may together explain how psychological distress leads to PSMU and PSPU. The I-PACE model proposes that individuals may develop internet-related addiction (e.g., PSMU and PSPU) due to the interactions between personal factors and functions in affective, cognitive, and executive domains [31]. Additionally, in social support and coping models [30], individuals who have psychological distress may use online activities as a coping method to deal with life stressors and problems. Subsequently, a small proportion of individuals become addicted to online activities because of a lack of control in using online activities as effective coping mechanisms [31]. Therefore, psychological distress can be a risk factor for the development of PSMU and PSPU [21,30]. Individuals who experience psychological distress (e.g., depression, anxiety, and stress) may use social media or smartphones as a coping strategy to alleviate their negative emotions, leading to PSMU and PSPU [21,30]. In sum, the I-PACE model together with social support and coping models suggest that engaging in online activities could be a coping method for individuals to deal with their psychological distress.
Jackson et al. [32] reported a small but significant relationship between depressive symptoms and perceived weight stigma among older adults in England, suggesting that individuals with depression were more likely to perceive weight stigma. Similarly, a recent study demonstrated that depression (OR = 1.68, 95% CI = 1.36–2.09, p < 0.001) was one of the risk factors for weight stigma among Saudi Arabian adults [9]. Therefore, psychological distress may be associated with WRSS. When together considering prior evidence showing the negative impacts of social media use on body image [33], the present study posits that negative emotions such as depression and stress may contribute to the development of WRSS via PSMU or PSPU.
Individuals who experience WRSS are more likely to use social media as one of their coping methods, leading to PSMU and PSPU among some individuals, which further worsens their WRSS [23,24]. However, PSMU and PSPU may further result in WRSS development because young people are likely to be exposed to weight stigma descriptions/environments if they frequently use their smartphones and/or engage in social media use [33]. More specifically, social media (and access social media via smartphone) could be platforms for weight-related teasing and bullying [24,33]. Individuals may use social media to post unreal body images (i.e., editing their true image before posts) to present different types of weight problems (e.g., fat and skinny) [33]. Because young people are at the human development stage where social comparisons are important. They may develop WRSS when reading the social media posts which feature content regarding weight. This may result in a vicious cycle for university students who have weight stigma issues. Moreover, prior research (although not extensive) has shown that WRSS is positively associated with PSMU and PSPU among university students across several Asian countries [34]. Therefore, it is worth investigating the association between psychological distress, PSMU and PSPU to further determine their relationships with WRSS among university students.
Consequently, by applying the social support and coping models, and the I-PACE model, the present study investigated whether PSMU and PSPU mediated the relationship between psychological distress and WRSS among university students. There were two hypotheses in the present study.
Hypothesis 1: PSMU and PSPU would mediate the relationship between depression and WRSS.
Hypothesis 2: PSMU and PSPU would mediate the relationship between stress and WRSS.
2.1 Participant Recruitment Process
A cross-sectional online survey was conducted among Malaysian university students. Participants were recruited through convenience sampling between August and November 2021 using Google Forms via social media platforms including Facebook, WhatsApp, and Instagram. The inclusion criteria for the participating university students included: (1) being Malaysian; (2) being aged 18 years and above; and (3) studying at a university in Malaysia. The exclusion criteria included: (1) being pregnant or lactating; and (2) self-reporting as having chronic diseases such as cardiovascular disease and cancer. Students who agreed to participate in the study were provided with an informed consent form (on the first page of the online survey). They were required to click the option “I agree to participate in the study” to complete the survey. Ethics approval was obtained from the Ethics Committee for Research Involving Human Subjects in Universiti Putra Malaysia (JKEUPM; Reference Number: JKEUPM-2021-455). Ethics approval was obtained by the Ethics Committee for Research Involving Human Subjects in Universiti Putra Malaysia (JKEUPM; Reference Number: JKEUPM-2021-455). This study obtained online informed consent from all participants before data collection and study methods were carried out in accordance with the Declaration of Helsinki.
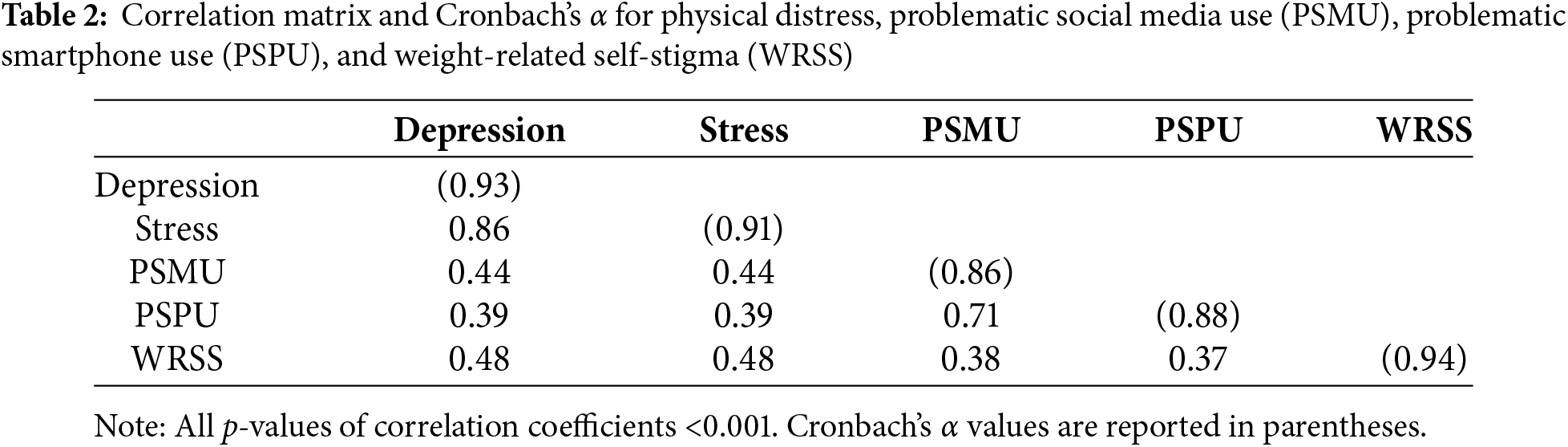
The Depression, Anxiety and Stress Scale (DASS-21) was used to assess two types of psychological distress (i.e., depression and stress) [35]. The DASS-21 has 21 items, and each psychological distress is assessed using seven items on a four-point Likert scale. A higher score on the DASS-21 indicates a higher level of psychological distress. The DASS-21 has been validated with good psychometric properties among Malaysians [36,37]. The internal consistency of the DASS-21 sub-scales in the present study was excellent: α = 0.93 (depression) and 0.91 (stress).
2.2.2 Problematic Social Media Use (PSMU)
The Bergen Social Media Addiction Scale (BSMAS) was used to assess PSMU [38]. The BSMAS has six items assessed using a five-point Likert scale. A higher score on the BSMAS indicates a greater risk of PSMU. The BSMAS has been validated with good psychometric properties among Malaysians [39]. The internal consistency of the BSMAS in the present study was very good: α = 0.86.
2.2.3 Problematic Smartphone Use
The Smartphone-Application Based Addiction Scale (SABAS) was used to assess PSPU [40]. The SABAS has six items assessed using a six-point Likert scale. A higher score on the SABAS indicates a greater risk of PSPU. The SABAS has been validated with good psychometric properties among Malaysians [39]. The internal consistency of the SABAS in the present study was very good: α = 0.88.
2.2.4 Weight-Related Self-Stigma (WRSS)
The Weight Self-Stigma Questionnaire (WSSQ) was used to assess weighted-related self-stigma [41]. The WSSQ has 12 items assessed using a five-point Likert scale. A higher score on the WSSQ indicates a higher level of WRSS. The WSSQ has been validated with good psychometric properties among Malaysians [42]. The internal consistency of the WSSQ in the present study was excellent: α = 0.94.
Some survey items were used to assess the participants’ demographics. More specifically, the participants were asked their age (in years), their sex (male or female), their ethnicity (Malay, Chinese, Indian, or other), their study program level (undergraduate or postgraduate), and their residential status (living in a college dorm, renting a house/room, or living with family members).
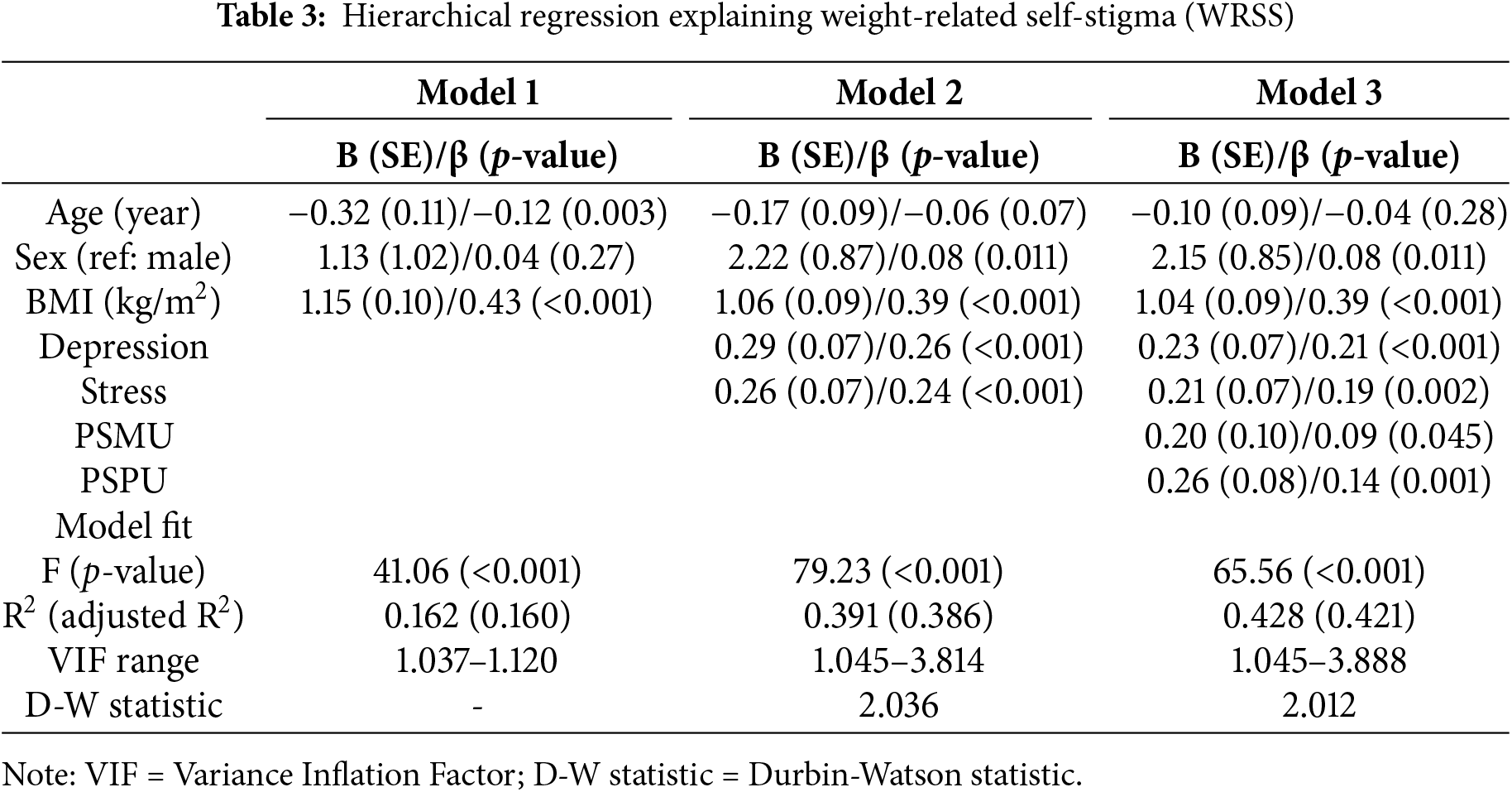
Descriptive statistics including means, standard deviations, frequencies, and percentages were used to summarize the participants’ characteristics. Pearson correlations were used to examine the relationships between the primary variables (i.e., depression, stress, PSMU, PSPU, and WRSS). Hierarchical regression models were then constructed to understand how depression, stress, PSMU, and PSPU were associated with WRSS after controlling for potential confounders. More specifically, there were three models in the hierarchical regression models: Model 1 had the independent variables of age, sex, and BMI; Model 2 added the independent variables of depression and stress; Model 3 further added the independent variables of PSMU and PSPU. Lastly, Hayes’ Process Macro (Model 4) was used to examine the mediation effects of PSMU and PSPU in the association between each type of psychological distress and WRSS. In the mediation models, age and sex were controlled for. All the statistical analyses were conducted using the IBM SPSS 20.0 (IBM Incorp., Armonk, NY, USA).
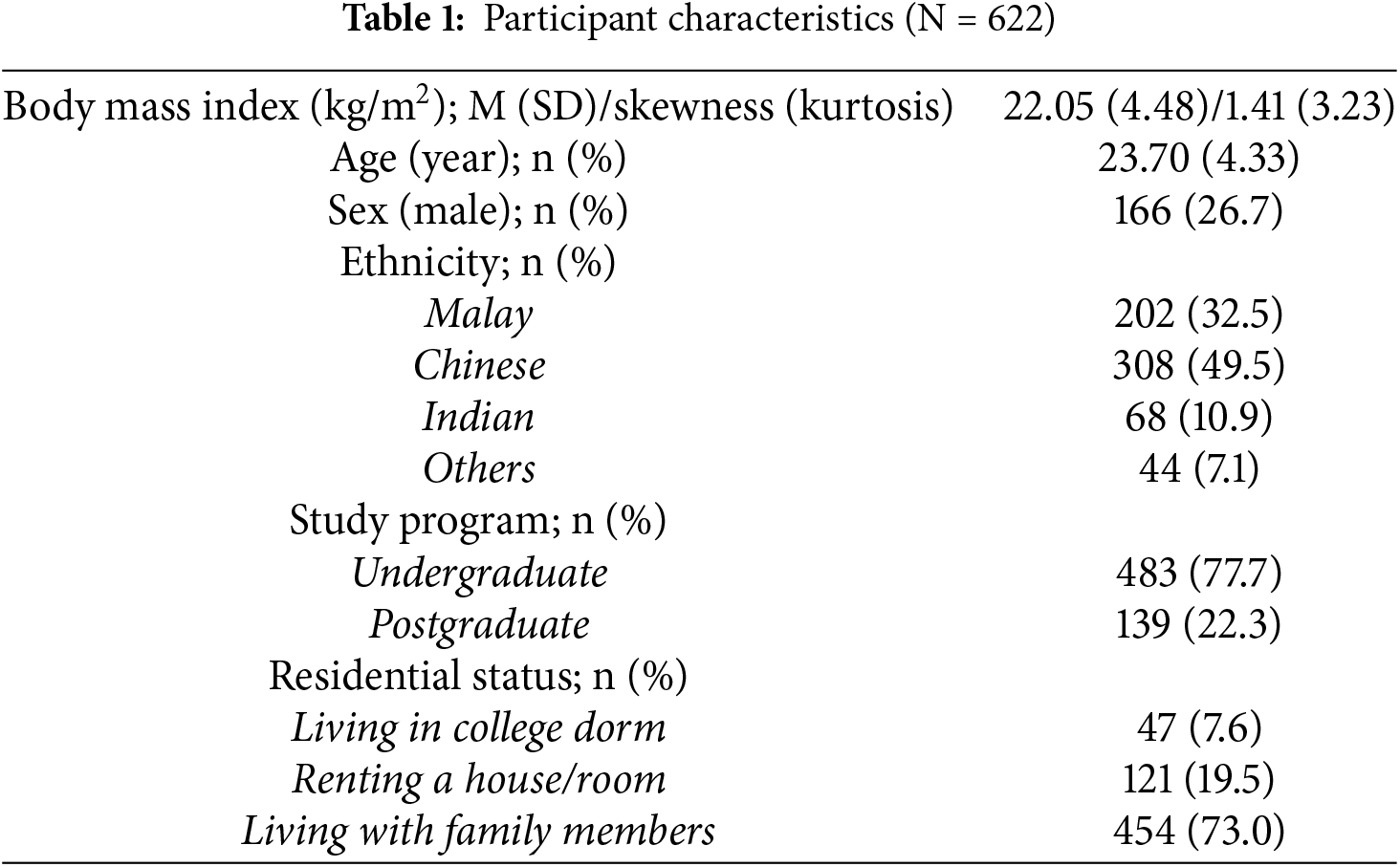
Among the 622 university students (mean age = 23.70 years [SD = 4.33]), the majority were females (n = 456; 73.3%). Nearly half of the participants were ethnic Chinese (n = 308; 49.5%) and nearly one-third were ethnic Malay (n = 202; 32.5%). Over three-quarters of the participants were studying on an undergraduate degree (n = 483; 77.7%). Table 1 summarizes the participants’ characteristics.
The associations between psychological distress, PSMU, PSPU, and WRSS were all significant with moderate to strong magnitudes (r = 0.37 to 0.86; p-values < 0.001) (Table 2). Results of the hierarchical regression models are presented in Table 3. The final model (adjusted R2 = 0.420) showing sex (standardized coefficient [β] = 0.08; p = 0.01), BMI (β = 0.39; p < 0.001), depression (β = 0.21; p = 0.001), stress (β = 0.18; p = 0.01), PSMU (β = 0.09; p = 0.045), and PSPU (β = 0.14; p = 0.001) were significant factors for WRSS. Moreover, the Appendix shows the results of the hierarchical regression models when separately using the two WSSQ factors (i.e., fear of enacted stigma (Table S1) and self-devaluation (Table S2)).
The mediating effects of PSMU and PSPU were then examined in the associations of depression and stress with WRSS. The mediation models showed that both PSMU (indirect effect = 0.05; 95% bootstrapping CI = 0.003, 0.10) and PSPU (indirect effect = 0.06; 95% bootstrapping CI = 0.03, 0.11) were significant mediators in the association between depression and WRSS (Fig. 1a). Both PSMU (indirect effect = 0.06; 95% bootstrapping CI = 0.01, 0.11) and PSPU (indirect effect = 0.06; 95% bootstrapping CI = 0.02, 0.11) were also significant mediators in the association between stress and WRSS (Fig. 1b). The mediation model using anxiety as an independent variable also showed similar results to the mediation model using depression as an independent variable (Fig. S1). Moreover, the Appendix shows the mediation models separately using the two WSSQ factors (i.e., fear of enacted stigma (Fig. S2) and self-devaluation (Fig. S3)) for mediation models using depression and anxiety as independent variables.
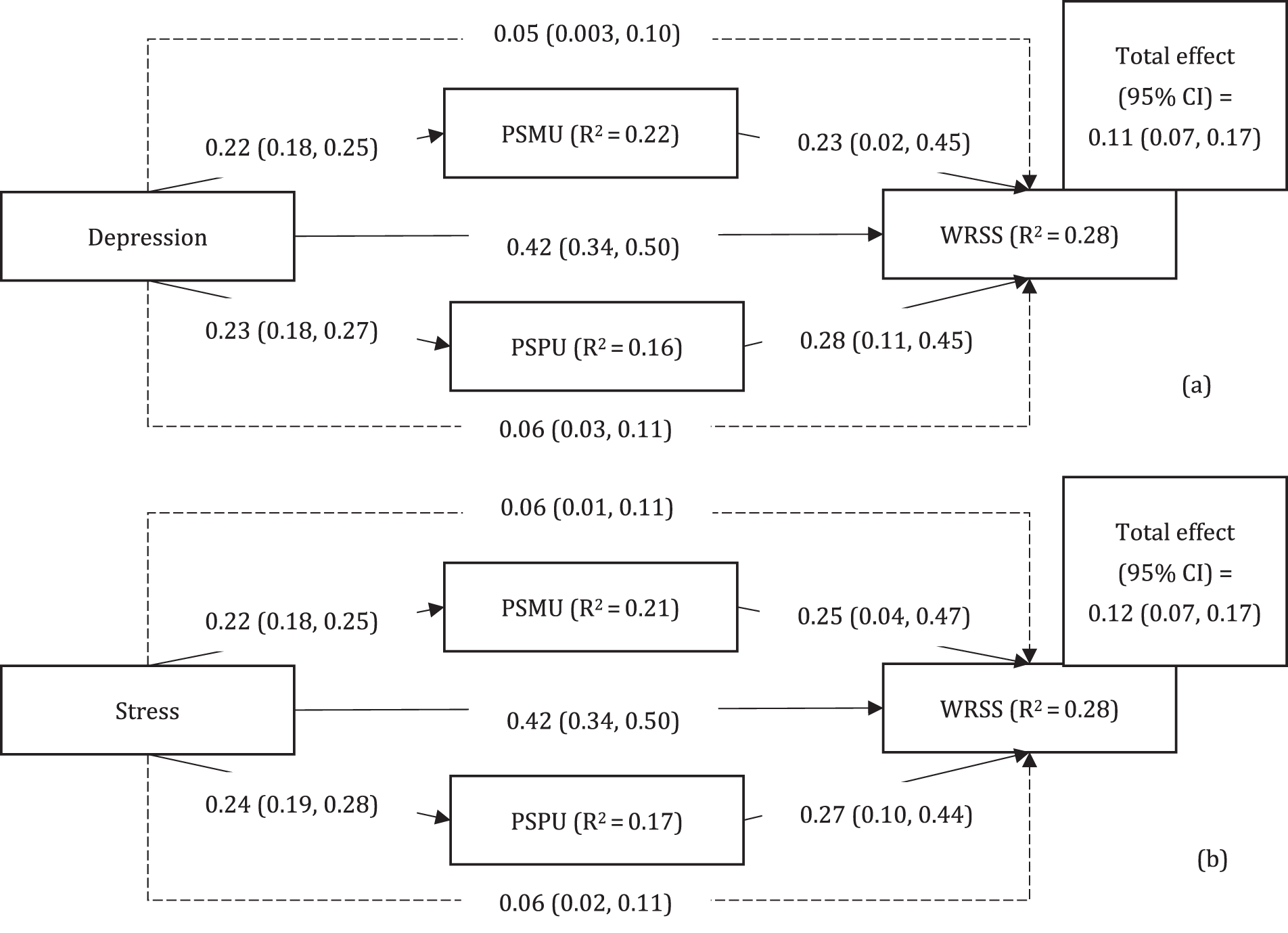
Figure 1: Mediated effects of problematic social media use (PSMU) and problematic smartphone use (PSPU) in the association of depression and stress with weight-related self-stigma (WRSS). Dashed lines indicate indirect effects; solid lines indicate direct effects. Line coefficients are reported in unstandardized coefficients (95% confidenct interval). Age and sex were controlled in the mediated models, which were estimated using 5000 bootstrapping samples
The present study investigated the mediating effects of PSMU and PSPU in the relationship between psychological distress and WRSS among Malaysian university students. The findings supported both Hypotheses 1 and 2. That is, PSMU and PSPU mediated the relationships between depression (Hypothesis 1) and stress (Hypothesis 2) with WRSS.
Social support and coping models, such as those proposed by Barrera [43] and Pearlin [44], primarily emphasize how social resources can buffer against psychological distress, and explains how individuals may use some coping strategies (including some inappropriate coping behaviors) to deal with their psychological distress and maintain self-stigmatizing attitudes. By also considering the I-PACE model, it seems possible that individuals may use PSMU and PSPU to cope with their psychological distress. When individuals develop PSMU and PSPU, they are likely to be exposed to negative comments regarding weight via social media on their smartphones. Here, they may develop WRSS. However, the present study did not collect direct information regarding whether the participants observed negative comments on weight. It is unclear if observing negative comments on weight increases an individual’s WRSS. In this regard, the I-PACE model does not appear to explain the relationship of PSMU and PSPU with WRSS. Therefore, future studies are warranted to identify if the I-PACE model or other untested theories could explain the underlying mechanisms from PSMU and PSPU to WRSS.
The relationship between depression and stress with WRSS may be bidirectional. Evidence has shown that individuals who experience WRSS are at increased risk for developing depression and stress [45,46]. For instance, a longitudinal study in the United States found that pre-pandemic experiences of weight stigma predicted higher levels of stress and depression during the COVID-19 pandemic, even after controlling for BMI and demographic characteristics among young adults [45].
The positive relationships between depression and stress with PSMU and PSPU [21,32,47] and PSMU and PSPU with WRSS [23,24,33] found in the present study were consistent with the evidence accumulated in the existing literature. Chen et al. [48] posited that university students with high levels of psychological distress use smartphones to regulate their negative emotions, eventually decreasing their ability to control smartphone use, and leading to addiction. Moreover, social media algorithms may increase weight bias content and exclude posts from individuals in stigmatized groups, resulting in the perpetuation of harmful weight-related norms, which may worsen WRSS [23].
Findings of the present study have significant implications for the development of interventions aimed at preventing WRSS among university students. The study highlights the importance of addressing PSMU and PSPU in the prevention of WRSS among university students who experience depression and stress. Healthcare professionals should try to prevent PSMU and PSPU among university students to help in the improvement of psychological well-being, and subsequently reduce WRSS. This can be achieved through interventions and programmes that create awareness regarding the health consequences of PSMU and PSPU among university students.
5.1 Limitations and Future Research
The present study has several limitations. First, it was a cross-sectional study, therefore cause and effect relationships between studied variables could not be established. More specifically, WRSS could be a stressor causing students to feel distressed and further develop PSMU and PSPU. However, the present study did not use WRSS as a stressor to examine the mechanism because PSMU and PSPU may cause extensive exposure of weight stigma to university students and result in WRSS. However, the relationship between weight stigma and PSMU/PSPU could be a vicious cycle. Given the aforementioned statement, self-stigma could lead to stress and depression. However, the present study did not test for this direction. Therefore, longitudinal study is needed to determine such relationships. Apart from the use of longitudinal design, future studies should consider applying cross-lagged panel analysis to detect if bidirectional relationships exist.
Second, the present study used a convenience sampling method. Therefore, the results may not be representative for the entire population of university students in Malaysia. Moreover, like university students, other populations (e.g., adolescents who are going through puberty) may also have the issues relating to weight stigma and social media use. However, the present study’s target population was university students. Future studies may want to explore the relationships between PSMU, PSPU, and weight stigma among other age groups such as adolescents.
Third, the data collection comprised an online self-administered questionnaire. This method could impact the accuracy of the data because it solely relies on the willingness of the participants to answer the survey honestly and there might be a high possibility of under-reporting or over-reporting from the participants. Some of the self-report measures (such as height and weight) could be measured more objectively in future studies so that BMI calculations are more accurate—especially in an area examining WRSS. Moreover, the present findings showed that self-reported BMI was relatively normally distributed (skewness < 3 and Kurtosis < 8 according to Kline’s suggestion [49]), indicating that there might not be severe impacts of extreme BMI on the present findings. Nevertheless, it is unclear if BMI had any moderating effects on the present findings. Future studies are therefore warranted to examine the potential moderating effect of BMI in the associations between PSMU/PSPU and WRSS.
Fourth, individuals may also use smartphones to engage in social media activities. Therefore, PSMU (a specific problematic use) and PSPU (generalized problematic use) are not two distinct constructs but clearly overlap. However, given that generalized problematic use may also include many other activities engaged using smartphone (e.g., gaming, gambling, streaming videos and films, web browsing, shopping, taking photographs and selfies), the two constructs were treated differently in the present study. However, caution should be made when interpreting the present study’s findings regarding the potential overlapping features between PSMU and PSPU.
Lastly, there are other variables that were not included in the present study that could have had an impact on the findings, such as participants’ use of social media (e.g., the role of social comparison), protective factors against harmful use of social media (e.g., news or media literacy), and background factors related to weight stigma (e.g., a history of eating disorders). Addressing these variables in future studies may provide a more comprehensive understanding of WRSS among university students.
The present study provides evidence for healthcare providers in understanding the possible development of WRSS among university students. Although some confounding variables were not investigated in the present study, the findings suggest that both PSMU and PSPU mediated the relationships between depression and stress with WRSS. Designing interventions to address PSMU and PSPU may help to prevent WRSS among university students, although the magnitudes of PSMU and PSPU explaining the effects of WRSS in the present study were not strong. Further studies are warranted to confirm these findings by applying longitudinal designs with larger and more representative samples.
Acknowledgement: None.
Funding Statement: This research was supported in part by (received funding from) the Ministry of Science and Technology, Taiwan (MOST 110-2410-H-006-115; MOST 111-2410-H-006-100), the National Science and Technology Council, Taiwan (NSTC 112-2410-H-006-089-SS2), the Higher Education Sprout Project, the Ministry of Education at the Headquarters of University Advancement at the National Cheng Kung University (NCKU), and the 2021 Southeast and South Asia and Taiwan Universities Joint Research Scheme (NCKU 31).
Author Contributions: Conceptualization: Wan Ying Gan, Wei-Leng Chin, Jung-Sheng Chen, Shih-Wei Huang, Kerry S. O’Brien, Iqbal Pramukti, Kamolthip Ruckwongpatr, Mark D. Griffiths, Chung-Ying Lin; Data curation: Wan Ying Gan, Serene En Hui Tung, Ling Jun Lee, Wai Chuen Poon, Yan Li Siaw; Formal analysis: Wei-Leng Chin, Kamolthip Ruckwongpatr, Chung-Ying Lin; Funding acquisition: Wan Ying Gan, Jung-Sheng Chen, Serene En Hui Tung, Yan Li Siaw, Iqbal Pramukti, Chung-Ying Lin; Investigation: Wan Ying Gan, Serene En Hui Tung, Wai Chuen Poon, Yan Li Siaw, Iqbal Pramukti, Kamolthip Ruckwongpatr, Chung-Ying Lin; Methodology: Wan Ying Gan, Jung-Sheng Chen, Kerry S. O’Brien, Kamolthip Ruckwongpatr, Mark D. Griffiths, Chung-Ying Lin; Project administration: Wan Ying Gan, Chung-Ying Lin; Resources: Wan Ying Gan, Jung-Sheng Chen, Shih-Wei Huang, Serence En Hui Tung, Wai Chuen Poon, Iqbal Pramukti, Chung-Ying Lin; Software: Wan Ying Gan, Iqbal Pramukti, Chung-Ying Lin; Supervision: Wan Ying Gan, Chung-Ying Lin; Validation: Jung-Sheng Chen, Shih-Wei Huang, Serene En Hui Tung, Ling Jun Lee, Wai Chuen Poon, Yan Li Siaw, Kerry S. O’Brien, Iqbal Pramukti, Kamolthip Ruckwongpatr, Mark D. Griffiths; Visualization: Chung-Ying Lin; Roles/Writing—original draft: Wan Ying Gan, Wei-Leng Chin, Kamolthip Ruckwongpatr, Chung-Ying Lin; Writing—review & editing: Wei-Leng Chin, Jung-Sheng Chen, Shih-Wei Huang, Serene En Hui Tung, Ling Jun Lee, Wai Chuen Poon, Yan Li Siaw, Kerry S. O’Brien, Iqbal Pramukti, Mark D. Griffiths, Chung-Ying Lin. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval: Ethics approval was obtained by the Ethics Committee for Research Involving Human Subjects in Universiti Putra Malaysia (JKEUPM; Reference Number: JKEUPM-2021-455). This study was obtained online informed consent from all participants before data collection and study methods were carried out in accordance with the Declaration of Helsinki.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
Supplementary Materials: The supplementary material is available online at https://doi.org/10.32604/ijmhp.2025.060049.
References
1. Puhl RM, Lessard LM. Weight stigma in youth: prevalence, consequences, and considerations for clinical practice. Curr Obes Rep. 2020;9(4):402–11. doi:10.1007/s13679-020-00408-8. [Google Scholar] [CrossRef]
2. Tomiyama AJ. Weight stigma is stressful. A review of evidence for the cyclic obesity/weight-based stigma model. Appetite. 2014;82(4):8–15. doi:10.1016/j.appet.2014.06.108. [Google Scholar] [CrossRef]
3. Anderson LN, Yoshida-Montezuma Y, Dewart N, Jalil E, Khattar J, De Rubeis V, et al. Obesity and weight change during the COVID-19 pandemic in children and adults: a systematic review and meta-analysis. Obes Rev. 2023;24(5):e13550. doi:10.1111/obr.13550. [Google Scholar] [CrossRef]
4. Bakaloudi DR, Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Chourdakis M. Impact of the first COVID-19 lockdown on body weight: a combined systematic review and a meta-analysis. Clin Nutr. 2022;41(12):3046–54. doi:10.1016/j.clnu.2021.04.015. [Google Scholar] [CrossRef]
5. Khan MA, Menon P, Govender R, Abu Samra AM, Allaham KK, Nauman J, et al. Systematic review of the effects of pandemic confinements on body weight and their determinants. Br J Nutr. 2022;127(2):298–317. doi:10.1017/S0007114521000921. [Google Scholar] [CrossRef]
6. de Macêdo PFC, Nepomuceno CMM, Dos Santos NS, Queiroz VAO, Pereira EM, Leal LDC, et al. Weight stigma in the COVID-19 pandemic: a scoping review. J Eat Disord. 2022;10(1):44. doi:10.1186/s40337-022-00563-4. [Google Scholar] [CrossRef]
7. Prunty A, Clark MK, Hahn A, Edmonds S, O’Shea A. Enacted weight stigma and weight self stigma prevalence among 3821 adults. Obes Res Clin Pract. 2020;14(5):421–7. doi:10.1016/j.orcp.2020.09.003. [Google Scholar] [CrossRef]
8. Puhl RM, Lessard LM, Himmelstein MS, Foster GD. The roles of experienced and internalized weight stigma in healthcare experiences: perspectives of adults engaged in weight management across six countries. PLoS One. 2021;16(6):e0251566. doi:10.1371/journal.pone.0251566. [Google Scholar] [CrossRef]
9. Althumiri NA, Basyouni MH, AlMousa N, AlJuwaysim MF, Alhamdan AA, Al-Qahtani FS, et al. Exploring weight stigma in Saudi Arabia: a nationwide cross-sectional study. Int J Environ Res Public Health. 2021;18(17):9141. doi:10.3390/ijerph18179141. [Google Scholar] [CrossRef]
10. Chue KM, Foo MY, Chua CME, Toh BC, Ong LWL, Lim CH, et al. Prevalence of perceived weight-based stigmatisation in a multiethnic Asian population. Ann Acad Med Singap. 2022;51(9):583–5. doi:10.47102/annals-acadmedsg. [Google Scholar] [CrossRef]
11. Lee KM, Hunger JM, Tomiyama AJ. Weight stigma and health behaviors: evidence from the eating in America study. Int J Obes. 2021;45(7):1499–1509. doi:10.1038/s41366-021-00814-5. [Google Scholar] [CrossRef]
12. Huang PC, Lee CH, Griffiths MD, O’Brien KS, Lin YC, Gan WY, et al. Sequentially mediated effects of weight-related self-stigma and psychological distress in the association between perceived weight stigma and food addiction among Taiwanese university students: a cross-sectional study. J Eat Disord. 2022;10(1):177. doi:10.1186/s40337-022-00701-y. [Google Scholar] [CrossRef]
13. Warnick JL, Darling KE, West CE, Jones L, Jelalian E. Weight stigma and mental health in youth: a systematic review and meta-analysis. J Pediatr Psychol. 2022;47(3):237–55. doi:10.1093/jpepsy/jsab110. [Google Scholar] [CrossRef]
14. Khodari BH, Shami MO, Shajry RM, Shami JA, Names AA, Alamer AA, et al. The relationship between weight self-stigma and quality of life among youth in the Jazan Region, Saudi Arabia. Cureus. 2021;13(9):e18158. doi:10.7759/cureus.18158. [Google Scholar] [CrossRef]
15. Butt M, Harvey A, Khesroh E, Rigby A, Paul IM. Assessment and impact of paediatric internalized weight bias: a systematic review. Pediatr Obes. 2023;18(7):e13040. doi:10.1111/ijpo.13040. [Google Scholar] [CrossRef]
16. Ajibewa TA, Sonneville KR, Miller AL, Toledo-Corral CM, Robinson LE, Hasson RE. Weight stigma and physical activity avoidance among college-aged students. J Am Coll Health. 2024;72(8):2323–7. doi:10.1080/07448481.2022.2123708. [Google Scholar] [CrossRef]
17. Pearl RL, Wadden TA, Jakicic JM. Is weight stigma associated with physical activity? A systematic review. Obesity. 2021;29(12):1994–2012. doi:10.1002/oby.23274. [Google Scholar] [CrossRef]
18. Stirnberg J, Margraf J, Precht L-M, Brailovskaia J. Problematic smartphone use, depression symptoms, and fear of missing out: can reasons for smartphone use mediate the relationship? A longitudinal approach. J Social Media Res. 2024;1(1):3–13. doi:10.29329/jsomer.3. [Google Scholar] [CrossRef]
19. Sui W, Sui A, Munn J, Irwin JD. Comparing the prevalence of nomophobia and smartphone addiction among university students pre-COVID-19 and during COVID-19. J Am Coll Health. 2024;72(6):1688–91. doi:10.1080/07448481.2022.2087473. [Google Scholar] [CrossRef]
20. Islam MS, Sujan MSH, Tasnim R, Mohona RA, Ferdous MZ, Kamruzzaman S, et al. Problematic smartphone and social media use among Bangladeshi college and university students amid COVID-19: the role of psychological well-being and pandemic related factors. Front Psychiat. 2021;12:647386. doi:10.3389/fpsyt.2021.647386. [Google Scholar] [CrossRef]
21. Mengistu N, Habtamu E, Kassaw C, Madoro D, Molla W, Wudneh A, et al. Problematic smartphone and social media use among undergraduate students during the COVID-19 pandemic: in the case of southern Ethiopia universities. PLoS One. 2023;18(1):e0280724. doi:10.1371/journal.pone.0280724. [Google Scholar] [CrossRef]
22. Kolhar M, Kazi RNA, Alameen A. Effect of social media use on learning, social interactions, and sleep duration among university students. Saudi J Biol Sci. 2021;28(4):2216–22. doi:10.1016/j.sjbs.2021.01.010. [Google Scholar] [CrossRef]
23. Clark O, Lee MM, Jingree ML, O’Dwyer E, Yue Y, Marrero A, et al. Weight stigma and social media: evidence and public health solutions. Front Nutr. 2021;8:739056. doi:10.3389/fnut.2021.739056. [Google Scholar] [CrossRef]
24. Ruckwongpatr K, Chen I-H, Pramukti I, Huang P-C, Latner JD, O’Brien KS et al. Assessing exposure to weight stigma: development and initial validation of the weight stigma exposure inventory (WeSEI). J Eat Disord. 2025;13(1):2. doi:10.1186/s40337-024-01168-9. [Google Scholar] [CrossRef]
25. Fung XCC, Siu AMH, Potenza MN, O’Brien KS, Latner JD, Chen CY, et al. Problematic use of internet-related activities and perceived weight stigma in schoolchildren: a longitudinal study across different epidemic periods of COVID-19 in China. Front Psychiat. 2021;12:675839. doi:10.3389/fpsyt.2021.675839. [Google Scholar] [CrossRef]
26. Midgley C, Thai S, Lockwood P, Kovacheff C, Page-Gould E. When every day is a high school reunion: social media comparisons and self-esteem. J Pers Soc Psychol. 2021;121(2):285–307. doi:10.1037/pspi0000336. [Google Scholar] [CrossRef]
27. Nutter S, Russell-Mayhew S, Saunders JF. Towards a sociocultural model of weight stigma. Eat Weight Disord. 2021;26(3):999–1005. doi:10.1007/s40519-020-00931-6. [Google Scholar] [CrossRef]
28. Godard R, Holtzman S. Are active and passive social media use related to mental health, wellbeing, and social support outcomes? A meta-analysis of 141 studies. J Comput Mediat Commun. 2024;29(1):zmad055. doi:10.1093/jcmc/zmad055. [Google Scholar] [CrossRef]
29. Ahmed O, Walsh EI, Dawel A, Alateeq K, Espinoza Oyarce DA, Cherbuin N. Social media use, mental health and sleep: a systematic review with meta-analyses. J Affect Disord. 2024;367:701–12. doi:10.1016/j.jad.2024.08.193. [Google Scholar] [CrossRef]
30. Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annu Rev Clin Psychol. 2007;3(1):377–401. doi:10.1146/annurev.clinpsy.3.022806.091520. [Google Scholar] [CrossRef]
31. Brand M, Wegmann E, Stark R, Müller A, Wölfling K, Robbins TW, et al. The interaction of person-affect-cognition-execution (I-PACE) model for addictive behaviors: update, generalization to addictive behaviors beyond internet-use disorders, and specification of the process character of addictive behaviors. Neurosci Biobehav Rev. 2019;104(4):1–10. doi:10.1016/j.neubiorev.2019.06.032. [Google Scholar] [CrossRef]
32. Jackson SE, Beeken RJ, Wardle J. Obesity, perceived weight discrimination, and psychological well-being in older adults in England. Obesity. 2015;23(5):1105–11. doi:10.1002/oby.21052. [Google Scholar] [CrossRef]
33. Mazzeo SE, Weinstock M, Vashro TN, Henning T, Derrigo K. Mitigating harms of social media for adolescent body image and eating disorders: a review. Psychol Res Behav Manag. 2024;17:2587–2601. doi:10.2147/PRBM.S410600. [Google Scholar] [CrossRef]
34. Liu W, Chen J-S, Gan WY, Poon WC, Tung SEH, Lee LJ, et al. Associations of problematic internet use, weight-related self-stigma, and nomophobia with physical activity: findings from mainland China, Taiwan, and Malaysia. Int J Environ Res Public Health. 2022;19(19):12135. doi:10.3390/ijerph191912135. [Google Scholar] [CrossRef]
35. Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. 2nd ed. Sydney, NSW, Austrilia: Psychology Foundation of Australia; 1995. [Google Scholar]
36. Ahmad N, Roslan S, Othman S, Abdul Shukor SF, Abu Bakar AY. The validity and reliability of psychometric profile for depression, anxiety and stress scale (DASS21) instrument among Malaysian undergraduate students. Int J Acad Res Bus Soc Sci. 2018;8(6):812–27. doi:10.6007/IJARBSS/v8-i6/4275. [Google Scholar] [CrossRef]
37. Musa R, Maskat R. Psychometric properties of depression anxiety stress scale 21-item (DASS-21) Malay version among a big sample population. Mediterr J Clin Psychol. 2020;8(1):e12269. doi:10.6092/2282-1619/mjcp-2269. [Google Scholar] [CrossRef]
38. Schou Andreassen C, Billieux J, Griffiths MD, Kuss DJ, Demetrovics Z, Mazzoni E, et al. The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: a large-scale cross-sectional study. Psychol Addict Behav. 2016;30(2):252–62. doi:10.1037/adb0000160. [Google Scholar] [CrossRef]
39. Tung SEH, Gan WY, Chen JS, Ruckwongpatr K, Pramukti I, Nadhiroh SR, et al. Internet-related instruments (Bergen Social Media Addiction Scale, Smartphone Application-Based Addiction Scale, Internet Gaming Disorder Scale-Short Form, and Nomophobia Questionnaire) and their associations with distress among Malaysian university students. Healthcare. 2022;10(8):1448. doi:10.3390/healthcare10081448. [Google Scholar] [CrossRef]
40. Csibi S, Griffiths MD, Cook B, Demetrovics Z, Szabo A. The psychometric properties of the Smartphone Application Based Addiction Scale (SABAS). Int J Ment Health Addict. 2018;16(2):393–403. doi:10.1007/s11469-017-9787-2. [Google Scholar] [CrossRef]
41. Lillis J, Luoma JB, Levin ME, Hayes SC. Measuring weight self-stigma: the weight self-stigma questionnaire. Obesity. 2009;18(5):971–6. doi:10.1038/oby.2009.353. [Google Scholar] [CrossRef]
42. Gan WY, Tung SEH, Ruckwongpatr K, Ghavifekr S, Paratthakonkun C, Nurmala I, et al. Evaluation of two weight stigma scales in Malaysian university students: weight self-stigma questionnaire and perceived weight stigma scale. Eat Weight Disord. 2022;27(7):1067–75. doi:10.1007/s40519-022-01398-3. [Google Scholar] [CrossRef]
43. Barrera M. Distinctions between social support concepts, measures, and models. Am J Community Psychol. 1986;14(4):413–45. doi:10.1007/BF00922627. [Google Scholar] [CrossRef]
44. Pearlin LI. The stress process revisited. In: Aneshensel CS, Phelan JC, editors. Handbook of the sociology of mental health. Boston, MA, USA: Springer; 1999. doi:10.1007/0-387-36223-1_19. [Google Scholar] [CrossRef]
45. Puhl RM, Lessard LM, Larson N, Eisenberg ME, Neumark-Stzainer D. Weight stigma as a predictor of distress and maladaptive eating behaviors during COVID-19: longitudinal findings from the EAT study. Ann Behav Med. 2020;54(10):738–46. doi:10.1093/abm/kaaa077. [Google Scholar] [CrossRef]
46. Almutairi BF, Alsaygh KW, Altamimi MM, Alshammari AS, Alsomali AM, Alanazi SM, et al. Internalized weight stigma: prevalence and association with psychiatric disorder among overweight and obese individuals. Cureus. 2021;13(10):e18577. doi:10.7759/cureus.18577. [Google Scholar] [CrossRef]
47. Shanshal SA, Al-Qazaz HK, Saadallah DA, Mohammed SY, Saber QAY, Ali MM, et al. Social media addiction and depression and their predictors among university students. Int J Adolesc Med Health. 2024;36(2):123–32. doi:10.1515/ijamh-2022-0111. [Google Scholar] [CrossRef]
48. Chen H, Ma J, Guan J, Yin L, Shi Z, Zhang Y. The impact of psychological distress on problematic smartphone use among college students: the mediating role of metacognitions about smartphone use. Front Psychol. 2022;13:932838. doi:10.3389/fpsyg.2022.932838. [Google Scholar] [CrossRef]
49. Kline RB. Principles and practice of structural equation modelling. 3rd ed. New York, NY, USA: Guilford Press; 2011. [Google Scholar]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools