 Open Access
Open Access
ARTICLE
Effects of Internet-Based Acceptance and Commitment Therapy on College Students’ Mental Health: A Randomized Controlled Trial
1 School of Educational Science, Anhui Normal University, Wuhu, 241000, China
2 Administration Office, Wuhu University, Wuhu, 241008, China
3 School of Nursing, Wannan Medical College, Wuhu, 241002, China
* Corresponding Author: Shuanghu Fang. Email:
International Journal of Mental Health Promotion 2025, 27(6), 845-861. https://doi.org/10.32604/ijmhp.2025.061476
Received 25 November 2024; Accepted 05 March 2025; Issue published 30 June 2025
Abstract
Objectives: College students face increasing mental health challenges. Although Acceptance and Commitment Therapy (ACT) is effective, the efficacy of Internet-based ACT (iACT) needs further exploration. Methods: This study examines the efficacy of iACT on college students’ mental health through a randomized controlled trial. We recruited 90 college students (19.16 ± 1.02 years old) and randomly divided them into the iACT group, face-to-face ACT group, and control group. The effects of the interventions were evaluated using the comprehensive assessment of ACT processes (CompACT) and the Depression Anxiety Stress Scales (DASS-21). Results: Two-factor repeated measures ANOVA revealed a significant time main effect of iACT. Face-to-face ACT and iACT effectively improved college students’ psychological flexibility [F(2, 83) = 18.78, p < 0.001, η2 = 0.18] and alleviated their negative emotions [F(2, 82) = 41.17, p < 0.001, η2 = 0.36]. Face-to-face ACT exhibited sustained effects on improving participants’ psychological flexibility and alleviating their negative emotions (p < 0.001), while iACT showed no sustained effect on improving participants’ psychological flexibility (p > 0.05). Conclusion: While iACT and face-to-face ACT are effective short-term interventions, face-to-face ACT demonstrates superior sustainability. Integrating guided sessions into iACT may enhance long-term outcomes. These findings advocate for blended interventions to address college students’ mental health needs, particularly in resource-limited settings.Keywords
In recent years, the mental health of college students has become a growing concern and a focus of extensive scholarly investigations [1]. College students frequently face numerous challenges that profoundly impact their mental health. Data from the Healthy Minds Study indicated a 33% surge in college students meeting diagnostic criteria for one or more mental health disorders from 2013 to 2022 [2,3]. Meanwhile, COVID-19 has significantly exacerbated the mental health issues in college students [4–6]. Job loss and income reductions due to the pandemic significantly increased the prevalence of mental disorders such as anxiety, insomnia, boredom, and loneliness [7,8]. A meta-analysis of the mental health problems among Chinese college students revealed the following prevalence rates: 13.7% for anxiety, 20.8% for depression, 4.5% for somatization, 10.8% for suicidal ideation, 16.2% for self-harm, and 2.7% for suicide attempts [9]. Longitudinal research data suggest that Chinese college students’ mental health issues are dynamic processes and that there is heterogeneity among different groups [10–12]. These statistics indicate novel challenges for mental health professionals practicing in higher education institutions. Therefore, it is crucial to explore effective interventions that adequately address the mental health needs of this demographic.
Acceptance and commitment therapy (ACT) represents the “third wave” of Cognitive Behavioral Therapy (CBT) [13,14], which extends beyond the concept of the first two waves of CBT. ACT focuses not on symptom reduction or cognitive restructuring but on modifying individuals’ problem-solving strategies and thought processes [15]. Psychological flexibility (PF) is the primary target and hypothesized change process in ACT, whose theory posits improved symptoms and well-being through increasing PF [16]. The effectiveness of ACT has been validated by over 280 randomized controlled trials (RCTs) involving nearly 33,000 participants [17], and the association between PF and mental health in college students has been extensively examined. A systematic review and three-level meta-analysis examined the effect of ACT on the PF of college students [18]. Previous findings suggest that PF helps to protect against the adverse impacts of the COVID-19 pandemic [19,20].
Different cultural values and beliefs significantly influence individuals’ acceptance and response to psychological therapies. In recent years, there has been growing attention to exploring the applicability of ACT within Chinese cultural and educational contexts. For instance, Fang et al. conducted an RCT to explore the psychological mechanisms of ACT and rational emotive behavior therapy in treating hoarding disorder among Chinese college students [21]. Wang and Fang explored the PF development trajectories of college students using the latent growth model [22]. These studies demonstrated from various perspectives how college students’ mental health interconnects with PF, and ACT has emerged as a prevalent psychological intervention in China.
Internet-based acceptance and commitment therapy (iACT) is a novel treatment protocol based on the Internet and ACT. It typically combines face-to-face sessions with mobile applications to facilitate ACT practice, enhance self-acceptance, and promote behavior change [23]. During the COVID-19 pandemic, iACT has been extensively utilized. Administered primarily through various interactive and remote formats, iACT includes video sessions, audio programs, engaging animated presentations, structured written activities, and personalized telephone consultations, all grounded in the principles of ACT [24]. Previous research has shown that iACT can help increase adolescents’ academic buoyancy and life satisfaction while reducing stress and depression symptoms [25–27]. A transdiagnostic meta-analysis examined the efficacy of iACT in relieving anxiety and depression and improving the life quality and PF of adults [28]. A meta-analysis by Wang & Fang revealed certain efficacy of iACT in enhancing adolescent mental health and PF [24]. However, the effect of Internet-based psychological intervention is relatively limited compared with face-to-face intervention [29], while other studies have further confirmed the effectiveness of these two interventions. Liu et al. compared the intervention effects of iACT and face-to-face ACT on middle school students’ PF, revealing further improved PF in the iACT group [30]. The impact of iACT and face-to-face ACT on Chinese college students remains uncertain, necessitating further RCTs for verification. Hence, this study aims to explore whether iACT can effectively address the prevalent psychological challenges college students face.
This study implemented group psychological counseling interventions based on ACT among college students to compare the effects of iACT and face-to-face ACT on improving their PF. The findings are expected to provide consultation and reference values for the mental health education of college students. The specific research questions are as follows:
First, what is the impact of ACT on PF improvement and negative emotion reduction in college students? Specifically, do ACT and iACT enhance PF and alleviate negative emotions in both intervention groups, and are the differences with the control group significant?
Second, is there a disparity in the efficacy of iACT and face-to-face ACT in enhancing PF and mitigating negative emotions among college students? Specifically, are there statistically significant distinctions between the two intervention groups?
Out of 108 individuals recruited online from a university in Anhui Province, China, 90 were included in this study after evaluation and screening. The sample size was calculated based on the expected effect size of the intervention (Cohen’s d = 0.5) and a power of 80% at an alpha level of 0.05. Using G*Power software, a minimum of 24 participants per group was required. Considering a dropout rate of 15%, we recruited 30 participants per group, totaling 90 participants. The inclusion criteria are (1) students with normal mental assessment results; (2) without previous psychological counseling; (3) able to effectively communicate with researchers either face-to-face or online and participate in group activities punctually. The exclusion criteria include (1) participation in any psychological interventions or psychotherapies that could potentially interfere with the research outcomes; (2) under psychiatric medications; (3) inability to consistently attend group counseling sessions. Randomization was conducted using a centralized randomization system. 90 participants were randomly assigned into three even groups, namely, the face-to-face ACT group (n = 26, 4 dropouts), the iACT group (n = 30), and the control group (n = 30).
All participants provided informed consent for their involvement in this research project. No interim analysis was planned due to the short duration of the study. However, the study would be terminated early if (1) more than 10% of participants in the intervention groups experienced significant worsening of mental health; (2) participation rates fell below 60%; or (3) any ethical violations occurred. The study was approved by the Ethical Committee of Anhui Normal University and performed following the Declaration of Helsinki.
In this study, invalid questionnaires were excluded based on the following criteria. Firstly, for completeness, questionnaires with more than 10% unanswered items, as detected by SPSS 26, are marked for exclusion. Secondly, regarding response consistency, two trained research assistants independently reviewed the questionnaires for obvious contradictions. Finally, considering response time, if a questionnaire is completed in less than half the expected time (estimated by the pre-test to be 15 min), it will be excluded.
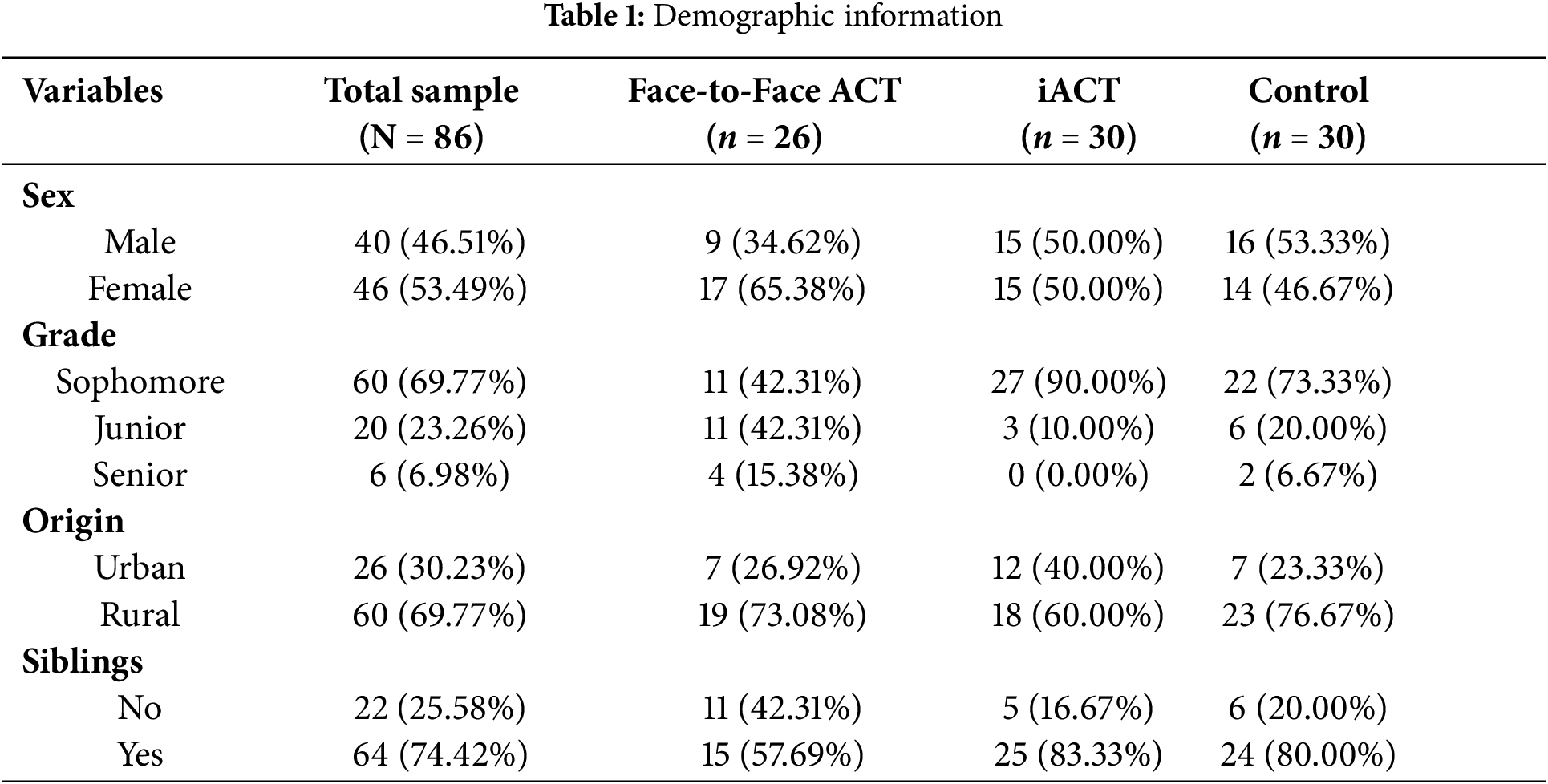
The participants aged 18 to 23 with an average of 19.16 ± 1.02, and the age difference across all groups is not statistically significant. Table 1 presents demographic information of the three groups.
2.2.1 Comprehensive Assessment of ACT Processes (CompACT)
The CompACT questionnaire was used to measure PF, which was developed by combining 11 ACT process assessment tools based on the Delphi method [31]. Fang & Huang revised the Chinese CompACT version into 18 questions in three dimensions: openness (Questions 1 to 6), awareness (Questions 7 to 11), and action (Questions 12 to 18) [32]. The questionnaire is based on a seven-point Likert scale from zero (completely inconsistent) to six (completely consistent), and Questions 1 to 4 and 6 to 11 are reverse-scored. A higher score indicates a higher PF, and vice versa. The Cronbach α coefficients of the three measurements in this study were 0.78, 0.79, and 0.76.
2.2.2 Depression Anxiety Stress Scale (DASS-21)
DASS-21 measures negative emotions such as depression, anxiety, and stress [33]. Its Chinese version comprises 21 items, covering 7 depression factors (items 3, 5, 10, 13, 16, 17, and 21), 7 anxiety factors (items 2, 4, 7, 9, 15, 19, and 20), and 7 stress factors (items 1, 6, 8, 11, 12, 14, and 18). DASS-21 adopts a 4-point scale from 0 (completely inconsistent) to 3 (completely consistent), with a higher total score indicating stronger negative emotional experiences. The Cronbach α coefficients of the three measurements in this study were 0.89, 0.92, and 0.91.
2.2.3 Group Counseling Feedback Form
The effect of group counseling was evaluated using a self-designed group counseling feedback form combined with a questionnaire survey, observations, and interviews.
Based on ACT principles and operational guidelines, a group counseling program centered around the “Get Out of Your Mind and Into Your Life” theme was developed in this study. Distinct intervention methods and strategies have been employed for the face-to-face ACT and iACT groups. During the group counseling sessions, the participants learned how language can contribute to human suffering and learned techniques to overcome the avoidance of negative emotions. They explored their thought processes, embraced inner experiences, and practiced mindfulness. The participants also focused on living in the present and leading a vibrant and meaningful college life. The activities encompassed various forms, such as experiential games, metaphorical storytelling, shared reflections, and mindfulness exercises. The facilitator leading these group counseling activities was certified as a psychological consultant with relevant training in ACT. The specific intervention programs are presented in Table 2.
The face-to-face ACT and iACT groups underwent 7 intervention sessions, while the control group received no intervention. The face-to-face ACT sessions were led by an experienced psychological counselor, assisted by a doctoral student. Both received their training within a structured group psychological counseling classroom setting. The iACT sessions were guided by an adept psychological counselor who delivered video/audio ACT materials via the Internet for self-directed learning/training purposes. Psychological assessments were conducted using Questionnaire Star at T1 (pre-intervention), T2 (post-intervention), and T3 (2 weeks post-intervention). The detailed process is illustrated in Fig. 1.
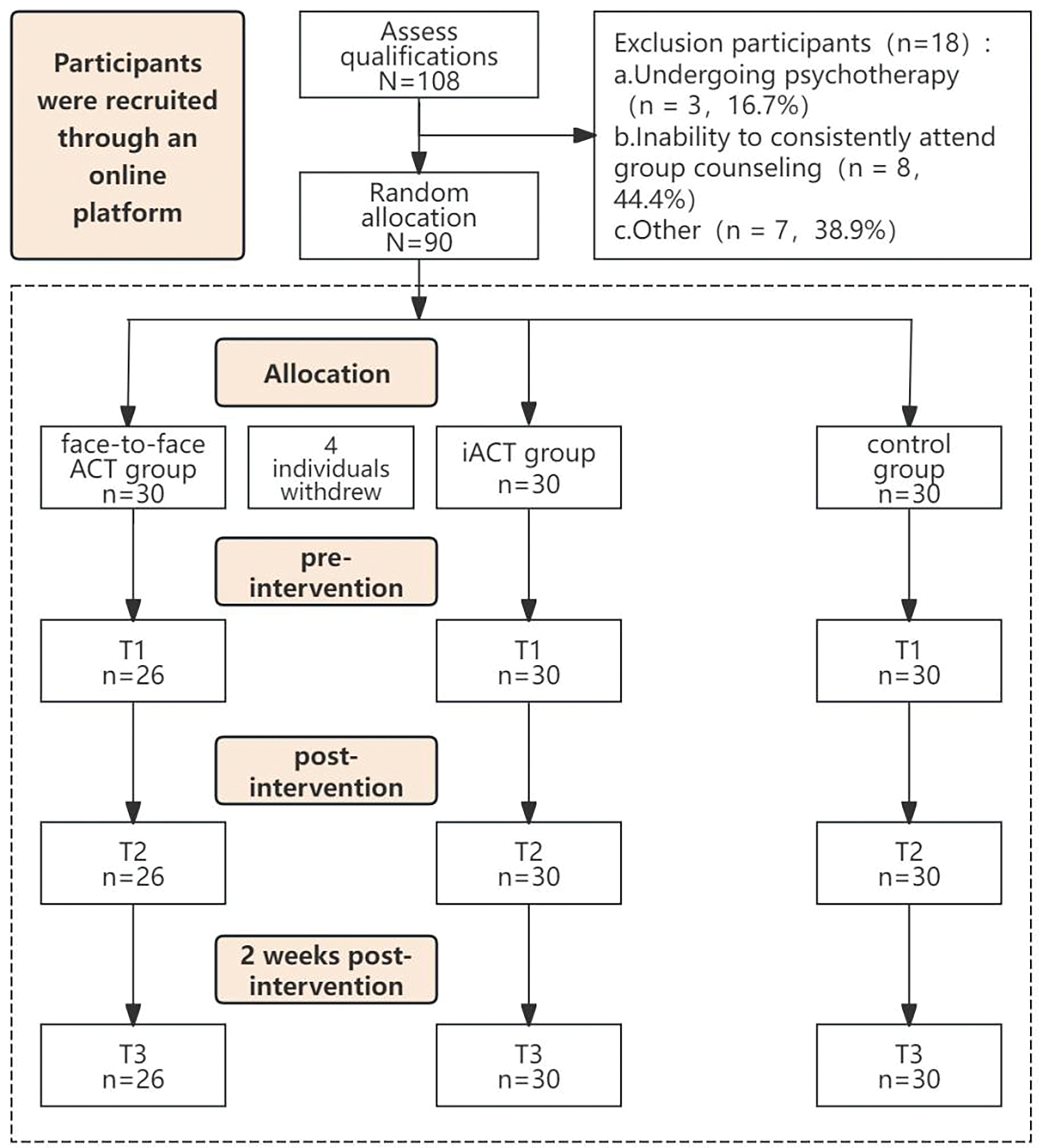
Figure 1: Intervention process
Data analysis was conducted in SPSS 26.0. This study employed a two-factor mixed experimental design with 3 groups (face-to-face ACT, iACT, and control) and 3 time points (T1, T2, and T3). A general linear model was utilized for the two-factor repeated measures Analysis of Variance (ANOVA) to examine the differences in PF and negative emotion scores among college students across the three groups. Effect size bias η2 was used to determine the variance in intervention effects between face-to-face ACT and iACT [35].
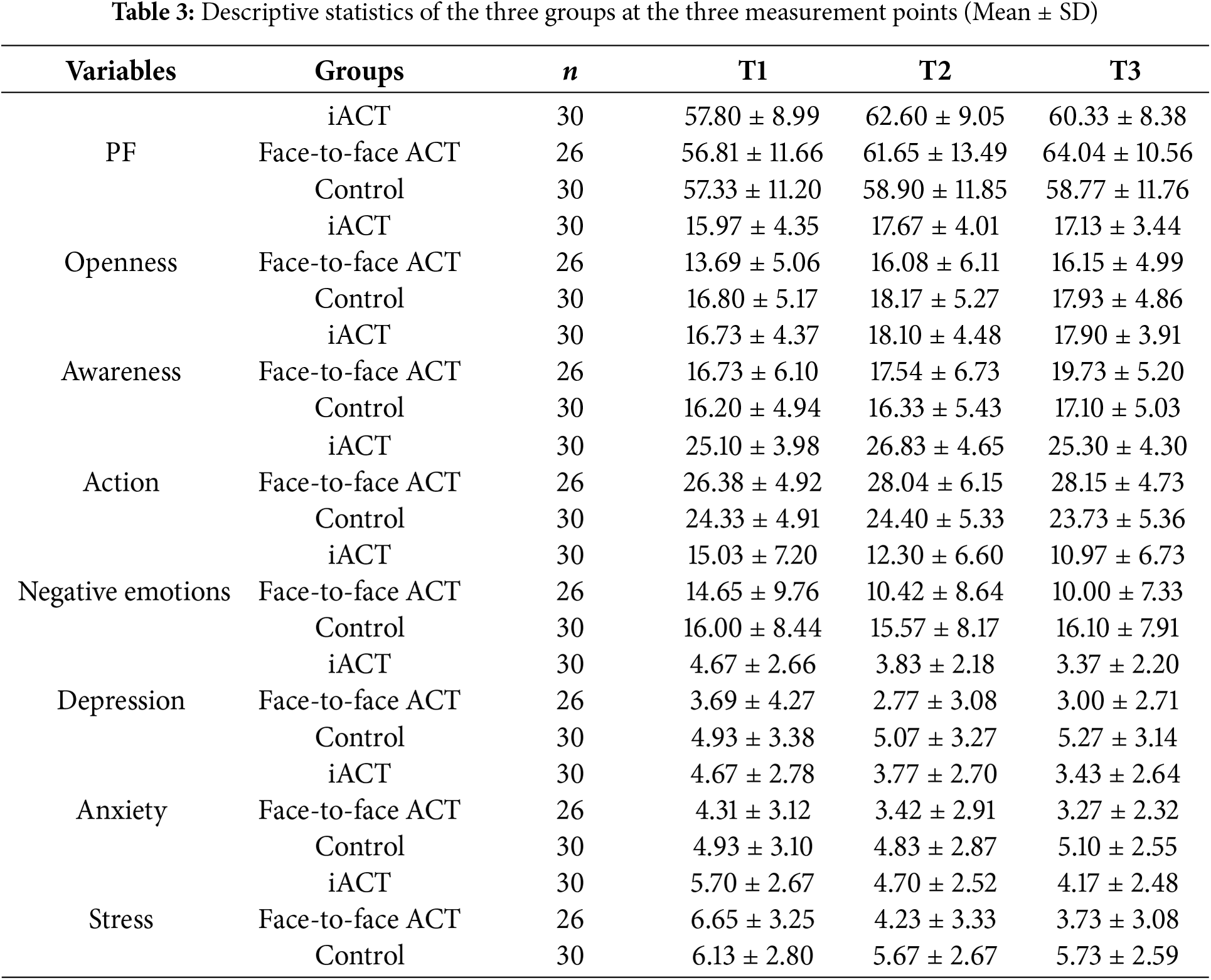
Table 3 displays the descriptive statistical findings for college students in the iACT, face-to-face ACT, and control groups at three measurement points. It presents the overall PF levels and scores on the openness, awareness, and action dimensions, as well as the overall negative emotion levels and scores on the depression, anxiety, and stress dimensions.
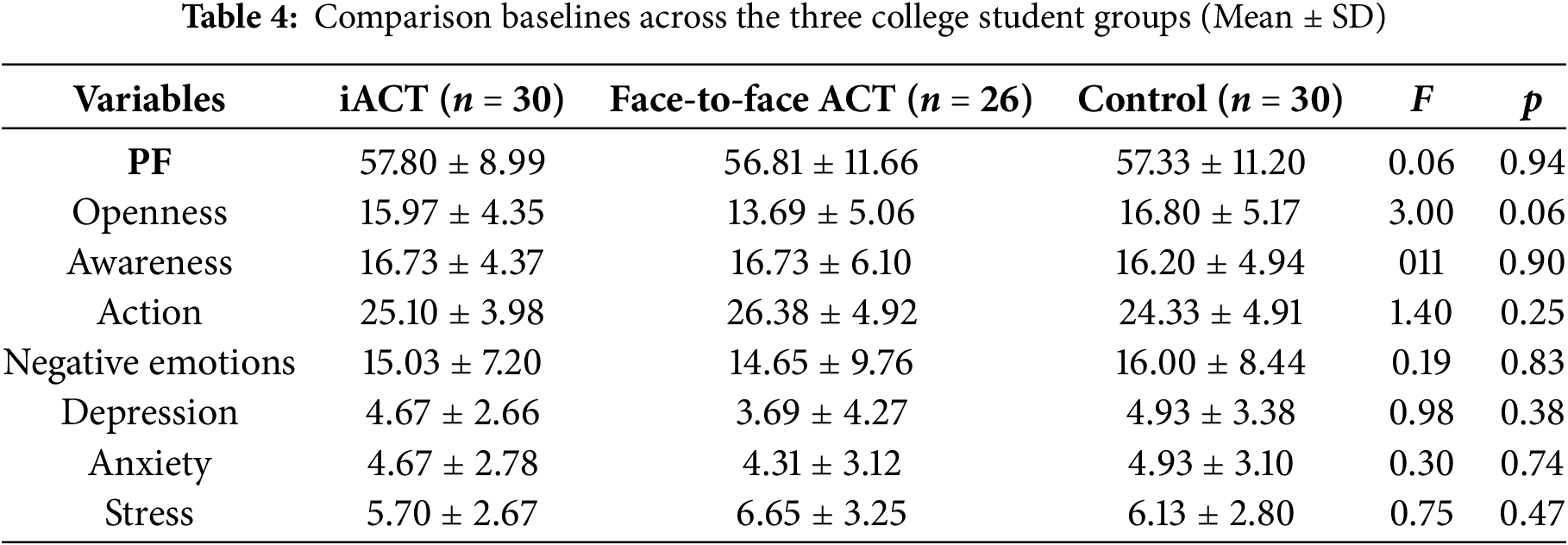
3.2 Comparison Baselines across the Three College Student Groups
An analysis indicates no statistically significant differences in PF and negative emotion scores among the iACT, face-to-face ACT, and control groups of college students prior to interventions. The results are listed in Table 4.
3.3 ACT Efficacy on College Students’ PF
A two-factor repeated measures ANOVA was conducted to examine the impact of iACT and face-to-face ACT on college students’ PF, which aimed to determine the differences among the three groups at the three measurement points. The normal distribution of the data at the three measurement points was confirmed by the Kolmogorov-Smirnov (K-S) test (p > 0.05), allowing for repeated measures ANOVA. Main effect testing with the Greenhouse-Geisser correction revealed a significant time main effect [F(2, 83) = 18.78, p < 0.001, η2 = 0.18], indicating statistically significant differences across measurement points. A significant interaction effect between time and group was also observed [F(2, 83) = 4.03, p < 0.05, η2 = 0.09], suggesting inconsistent changes in PF among the three college student groups. However, no significant group main effect was found through between-subjects effect testing [F(2, 83) = 0.48, p = 0.62] indicating no statistically significant differences among the three groups. The results are presented in Table 5.
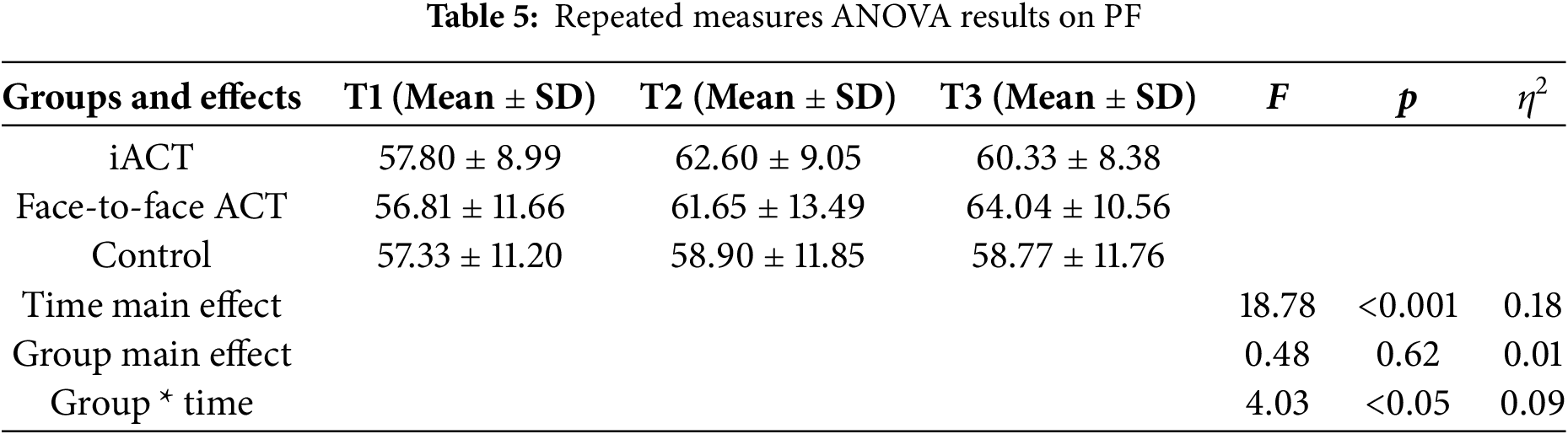
Significant interactions were found between group and time (F(2, 83) = 4.03, p < 0.05). Therefore, the effects were separately analyzed. The simple effect analysis revealed that with measuring time as the independent variable, the intervention group exhibited a significantly higher PF score than the baseline at T2 and T3 (p < 0.001). In contrast, no significant differences were observed in the control group’s PF scores at the three-time points (p > 0.05), suggesting effectively enhanced participant PF by ACT. Furthermore, paired comparison results indicated that face-to-face ACT led to a sustained increase in PF, with significantly higher scores than the baseline at T2 and T3 (p < 0.001), while iACT resulted in an initial improvement but no sustained enhancement over time. The results are shown in Fig. 2.
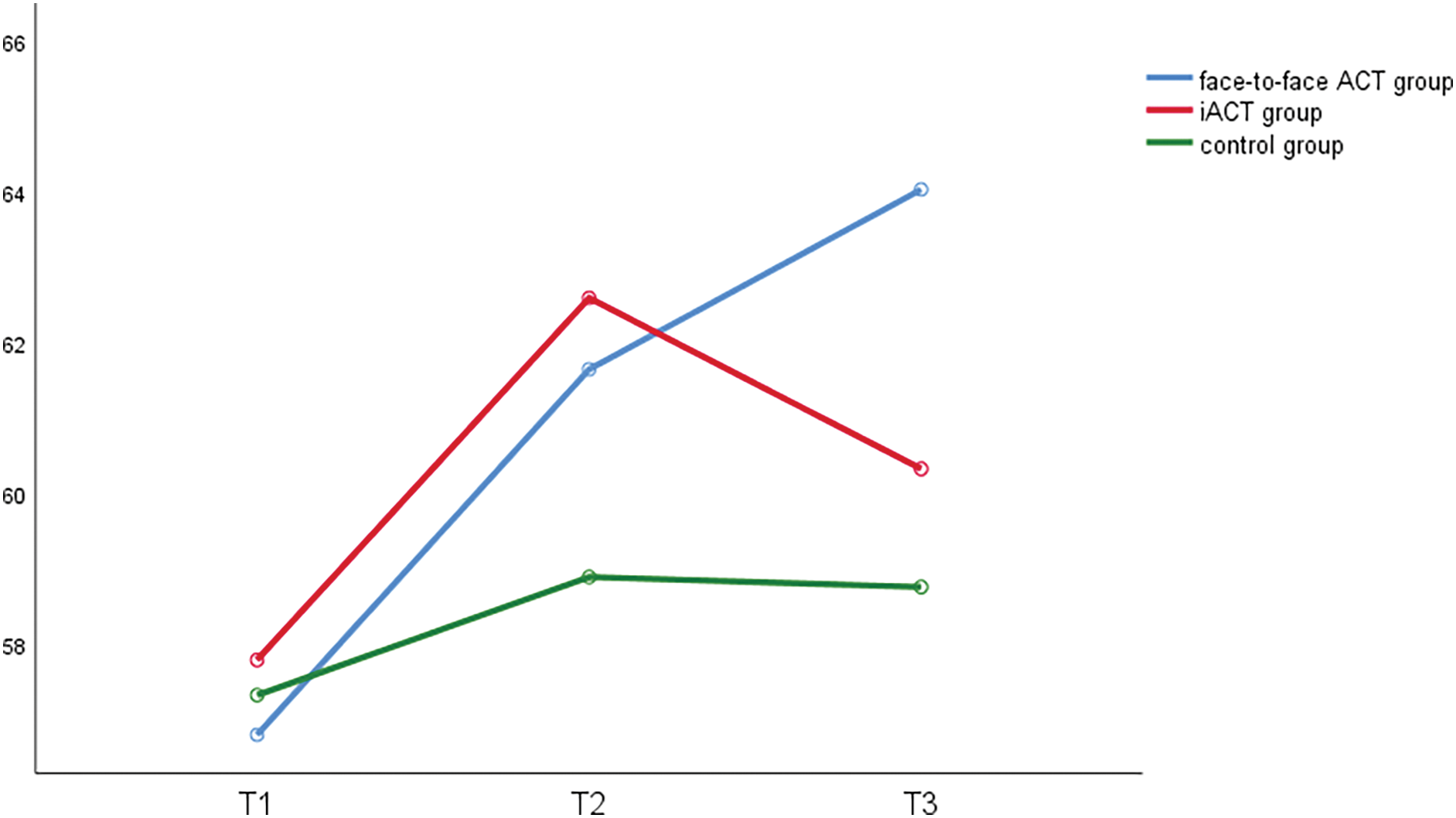
Figure 2: Repeated measures ANOVA results of the three groups on PF scores
3.4 ACT Efficacy on College Students’ Negative Emotions
To examine the effect of iACT and face-to-face ACT on the negative emotions of college students, a two-factor repeated measures ANOVA was conducted. The results showed a significant time main effect [F(2, 82) = 41.17, p < 0.001, η2 = 0.36], indicating statistically significant differences among the three measurements. The interaction effect of time and group was significant [F(2, 82) = 12.32, p < 0.001, η2 = 0.23], indicating that the negative emotions of college students changed differently across the three groups. The intra-group effect test showed no significant group main effect [F(2, 82) = 2.30, p = 0.11, η2 = 0.05], indicating no statistically significant difference among the three groups. The results are listed in Table 6.
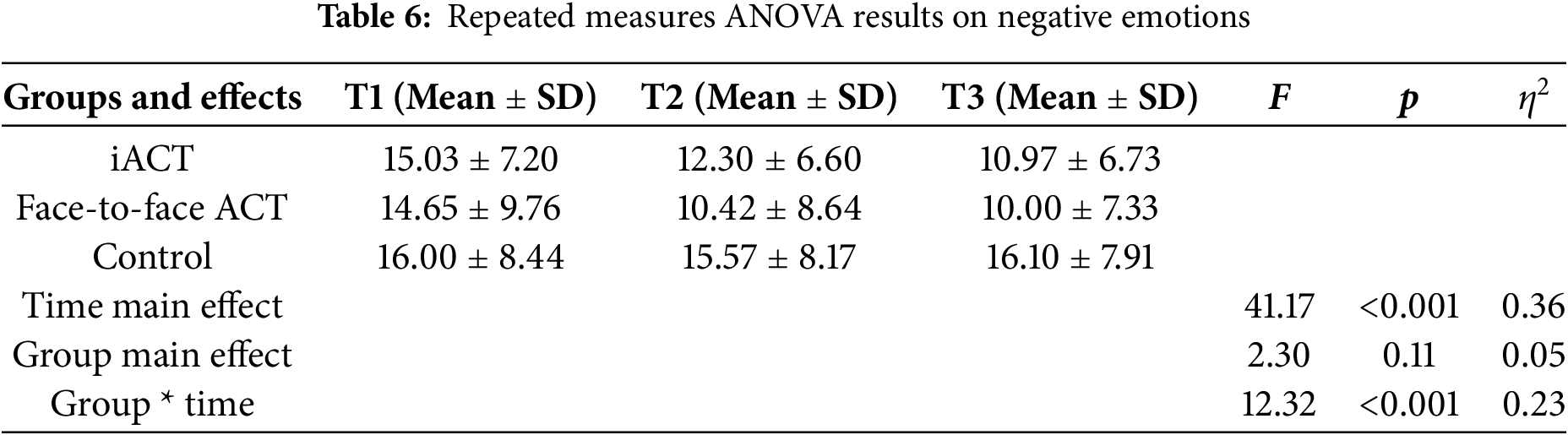
The simple effect analysis revealed that with measuring time as the independent variable, the negative emotion scores of the intervention group were significantly lower than the baseline at T2 and T3 (p < 0.001). In contrast, no significant difference was observed in the negative emotion scores of the control group at the three-time points (p > 0.05), indicating that ACT effectively alleviated participants’ negative emotions. Furthermore, paired comparison results demonstrated that face-to-face ACT led to significantly lower negative emotion scores compared to the baseline at T2 and T3 (p < 0.001), with no significant difference between these two-time points (p > 0.05), indicating the sustainability of face-to-face ACT in alleviating the negative emotions of the participants. The negative emotion scores at T2 and T3 in the iACT group showed a significant decrease compared to the baseline (p < 0.001), with T3 also demonstrating a significantly lower negative emotion score than T2 (p < 0.001). These findings indicated that iACT had a more sustained effect on alleviating negative emotions. The results are shown in Fig. 3.
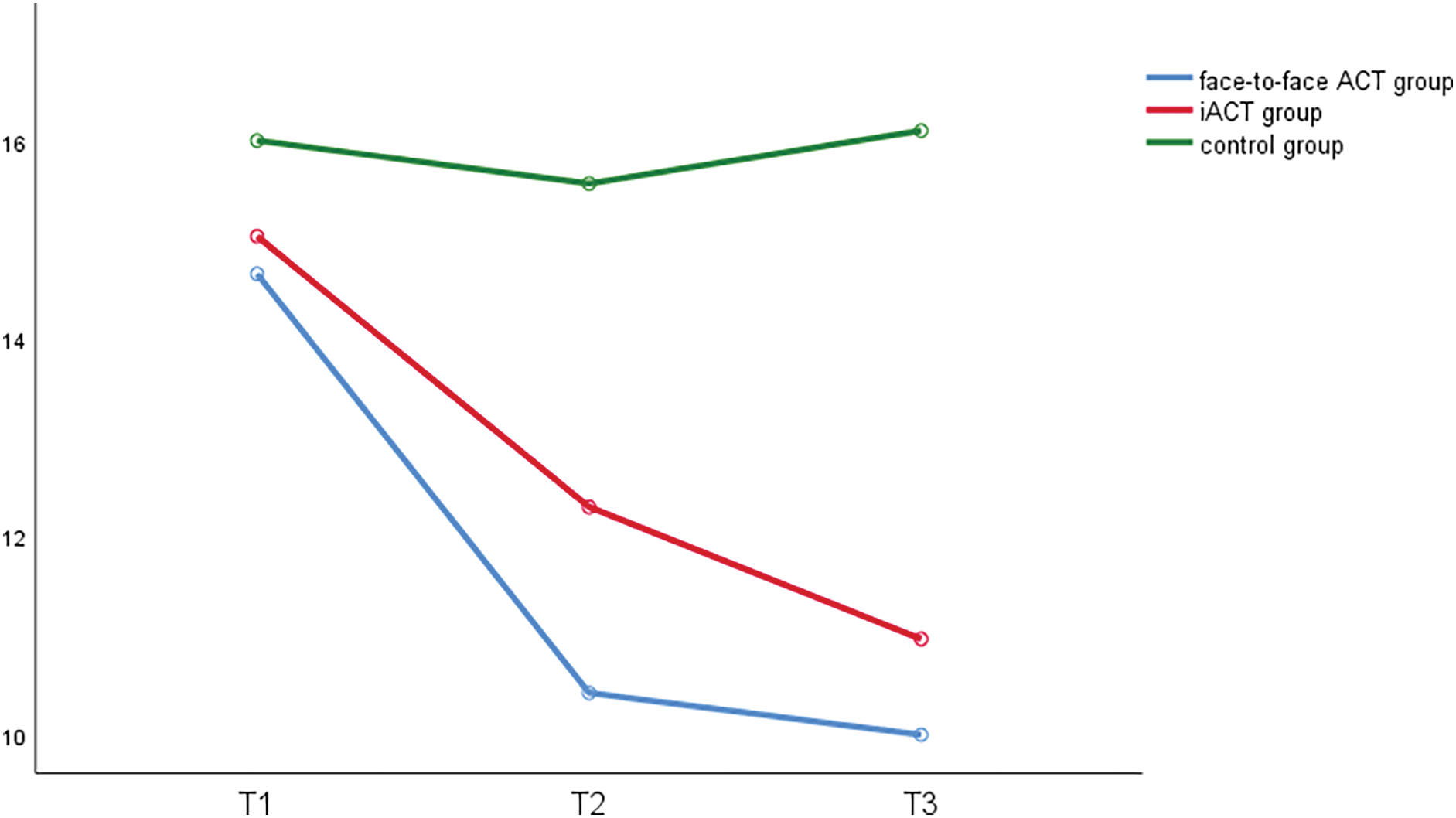
Figure 3: Repeated measures ANOVA results of the three groups on negative emotion scores
3.5 The Efficacy of Group Counseling
This study evaluated the efficacy of group counseling through questionnaires, interviews, and observations. The findings revealed that 8% of the participants demonstrated a strong comprehension of and engagement in group counseling, while 74% were aware of it but had not participated, and 18% had no knowledge of it. Furthermore, 96% of the participants reported that psychological group counseling activities positively impacted their well-being, mood regulation, intellectual enlightenment, psychological knowledge acquisition, and personal development. Additionally, 89% actively engaged in group counseling by expressing their thoughts and emotions sincerely while fostering friendly interactions with other members. During interviews with the participants, many expressed their ability to apply the acquired knowledge from group counseling to their daily lives and highlighted memorable experiences such as “Chinese finger trap” and “mindfully eating an orange”. They emphasized that “mindfulness training” had significantly benefited them.
The primary aim of the RCT in this study was to investigate the efficacy of ACT intervention, specifically concerning its impact on the PF and negative emotions of college students. Meanwhile, the effectiveness of iACT and face-to-face ACT was compared. This section discusses the research findings.
4.1 The Impact of ACT on College Students’ PF
To test the effect of ACT on the PF of college students, this study conducted an RCT on three groups with and without intervention. The results showed that iACT and face-to-face ACT effectively enhanced the PF of college students, consistent with the findings of previous studies [36,37]. ACT primarily improves an individual’s PF through mindfulness, acceptance, cognitive detachment, clarifying values, and behavioral change experiences. It enables individuals to commit to a valuable and meaningful life. The intervention program in this study consists of seven modules, fully covering the six core processes of ACT. The basic knowledge, metaphors, exercises, and mindfulness practices in each module reflect the two ACT processes, namely, the acceptance and mindfulness module and the commitment and action change module. The intervention program significantly enhanced the PF of college students. Additionally, the PF measuring tool in this study (CompACT) is more comprehensive than existing single-dimensional measurement tools, such as AAQ, in assessing the PF improvement in college students. These findings demonstrate the scientificity, completeness, and effectiveness of the ACT intervention program in this study.
4.2 The Impact of ACT on College Students’ Negative Emotions
Data analysis showed that the intervention groups had lower negative emotion scores at T2 and T3 than the baseline. In contrast, the control group had no significant differences in negative emotion scores at the three-time points, indicating that ACT effectively alleviated the participants’ negative emotions. Previous studies have demonstrated PF as a protective factor against the development and progression of various mental problems, including depression and anxiety [38]. As the participants’ PF improved in this study, their negative emotions gradually subsided. Some studies on the PF enhancement mechanisms have shown that the impact of ACT on clinical outcomes is achieved through its effects on PF and its core processes [14]. This study posits that individuals with high PF may accurately discern the reality of negative emotions and utilize cognitive defusion and mindfulness techniques to live in the present moment rather than becoming ensnared by negative emotions. Doing so creates space for their authentic selves and enables them to move toward meaningful actions aligned with their values. As psychologically inflexible college students encounter stimuli triggering depression or other negative emotions, their sensitivity and vigilance toward such stimuli increase, enticing them to unconsciously engage in experiential avoidance and over-generalize to keep themselves from harm. Under the influence of cognitive fusion, negative experiences intensify [39–41]. ACT believes that enhancing PF is the fundamental goal of the intervention while changing symptoms is an “unexpected bonus” naturally arising from increased PF.
Our findings align with the existing literature. For instance, a study demonstrated that iACT interventions yielded significant positive effects on adolescent mental health during the COVID-19 pandemic [27]. Another study revealed that online ACT interventions not only enhanced adolescents’ psychological well-being but also improved their school engagement [20]. We recommend that health and educational authorities promote ACT interventions among college students to assist them in reducing judgments of negative emotions and avoidance behaviors. Additionally, we suggest increasing access to mental health services, particularly in resource-limited areas, by leveraging online platforms and mobile applications to ensure broader student access to support.
4.3 Comparison of iACT and Face-to-Face ACT
This study revealed that iACT and face-to-face ACT effectively enhanced participants’ PF and alleviated their negative emotions. However, some differences were observed between the two interventions. Face-to-face ACT demonstrated sustained effects in improving participants’ PF and alleviating negative emotions, whereas iACT showed no sustained effects in enhancing participants’ PF. ACT has proven to be a highly adaptable intervention that applies to various settings, such as classrooms, psychotherapy offices, or online platforms [42]. Early ACT interventions are primarily implemented face-to-face and yield positive therapeutic outcomes. The effectiveness and lasting effect of face-to-face group psychological counseling were also confirmed in this study. With the continuous IT advancements and the COVID-19 pandemic, iACT has garnered significant attention in recent years. Research has indicated that iACT can enhance mental health [27], reduce anxiety symptoms in adolescents, improve PF skills [20], and notably treat depressive symptoms among college students, particularly those with low mental health baselines [43].
The effectiveness of iACT was validated in a previous systematic review and meta-analysis [24], but the sustainability of iACT in terms of therapeutic effect requires further improvement, which may be due to the absence of iACT guidance. A review by Välimäki et al. [44] on online mental health interventions for adolescents suggested that including face-to-face elements in internet-based psychological interventions may increase the positive impact of online interventions. Some researchers have categorized iACT into two types based on the presence of a guide, and integrating two 45-min face-to-face meetings and weekly coaching messages to encourage participants has produced positive effects [26]. Due to the limited relevant research, we used the conclusions cautiously. The iACT intervention program in this study involved no guidance, with participants primarily engaging in autonomous learning through video, audio, text, and mindfulness training. Our future research aims to delve deeper into guided iACT.
Additionally, this study found that the participant retention rate in Internet-based psychological interventions was relatively high, consistent with the results of the above meta-analysis [24]. The temporal and spatial limitations of face-to-face psychological interventions often cause participants to drop out. In contrast, online psychological interventions are convenient, demanding less time and space, making it easier for active participation.
There are undoubtedly many culture-bound features of ACT [45]. Existing studies have preliminarily demonstrated the effectiveness of iACT and face-to-face ACT in Chinese cultural and educational settings, A study combined iACT with traditional Chinese culture and designed an internet-based self-help ACT for Chinese medical students [46]. This study further provides empirical evidence for the efficacy of iACT and face-to-face ACT within the context of Chinese culture. Future research should focus on expanding cross-cultural and cross-educational studies, which are essential for comprehensively evaluating the applicability of these therapies and establishing a robust foundation for their effective implementation across diverse populations.
Recent studies have demonstrated that AI can substantially enhance the early detection of mental health conditions by analyzing social media posts, smartphone usage patterns, and physiological data from wearable devices [47]. Mental health professionals can benefit from AI-generated insights while maintaining a strong patient-provider relationship [48]. Future research should explore integrating AI with psychological interventions to achieve personalized and precise therapeutic approaches.
Certain limitations remain in this study. One primary limitation is the issue of generalizability. The participant inclusion criteria in this study may result in a sample not fully representing all college students. Moreover, our sample was limited to Chinese college students, which, although pertinent to the Chinese context, restricts the generalizability of our findings. The distinct cultural, social, and educational backgrounds of this population may result in outcomes that are not readily applicable to other college student populations. Future research could use multiple data collection methods and a more diverse sample to improve validity and generalizability. Another limitation is methodological bias. Relying solely on self-reports from college students exposes the research to common method bias, as respondents may be influenced by social desirability or recall issues, potentially distorting variable relationships and undermining validity. The third constraint is blinding, which presents particular difficulties in psychological research. The inability to conceal the interventions from participants and researchers may introduce subjective biases that impact the outcome measures. A nuanced comprehension of these limitations is essential for thoroughly grasping the significance and ramifications of the findings in this study.
This study implemented ACT on college students to validate its efficacy for improving PF and alleviating negative emotions. Additionally, the intervention outcomes between iACT and traditional face-to-face ACT were compared through an RCT. The findings revealed that both formats effectively enhanced participants’ PF and alleviated their negative emotions. However, only face-to-face ACT demonstrated sustained benefits for participants’ PF over time.
Acknowledgement: Thanks for all contributors engaged in this study.
Funding Statement: This study was funded by the Education and Teaching Reform Research Major Project of Anhui Province (2022xqhz023) (2023sx170).
Author Contributions: Jing Wang conducted the analyses and wrote the first manuscript; Jing Wang and Shuanghu Fang conceived the current work; Zihua Li and Shaoyong Ma revised the manuscript and confirmed its final version. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data that support the findings of this study are available on request from the corresponding author upon reasonable request.
Ethics Approval: All the methods were performed following the Declaration of Helsinki. The study was approved by the Ethical Committee of Anhui Normal University (AHNU-ET2022002). Informed consent was obtained from all individual participants included in the study.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
References
1. American College Health Association. The impact of COVID-19 on college students’ wellbeing. [cited 2025 Jan 1]. Available from: https://www.acha.org/documents/ncha/Healthy_Minds_NCHA_COVID_Survey_Report_FINAL.pdf. [Google Scholar]
2. Lipson SK, Zhou S, Abelson S, Heinze J, Jirsa M, Morigney J, et al. Trends in college student mental health and help-seeking by race/ethnicity: findings from the national healthy minds study, 2013–2021. J Affect Disord. 2022;306:138–47. doi:10.1016/j.jad.2022.03.038. [Google Scholar] [PubMed] [CrossRef]
3. Anderson GM, Stanley-Kime KL, Enty LA, Alnarshi M. A DBT-informed, inclusive treatment program for college students with severe mental health issues: outcome analysis of in-person and telehealth services. J Coll Stud Ment Health;2024:1–25. doi:10.1080/28367138.2024.2345833. [Google Scholar] [CrossRef]
4. Salimi N, Gere B, Talley W, Irioogbe B. College students mental health challenges: concerns and considerations in the COVID-19 pandemic. J Coll Stud Psychother. 2023;37(1):39–51. doi:10.1080/87568225.2021.1890298. [Google Scholar] [CrossRef]
5. Wood CI, Yu Z, Sealy DA, Moss I, Zigbuo-Wenzler E, McFadden C, et al. Mental health impacts of the COVID-19 pandemic on college students. J Am Coll Health. 2024;72(2):463–8. doi:10.1080/07448481.2022.2040515. [Google Scholar] [PubMed] [CrossRef]
6. Zamanzadeh A, Eckert M, Corsini N, Adelson P, Sharplin G. Mental health of Australian frontline nurses during the COVID-19 pandemic: results of a large national survey. Health Policy. 2025;151:105214. doi:10.1016/j.healthpol.2024.105214. [Google Scholar] [PubMed] [CrossRef]
7. Zamanzadeh A, Banerjee R, Cavoli T. Job loss and mental disorders: international evidence from the early stages of COVID-19 outbreak. Stress Health. 2024;40(1):e3287. doi:10.1002/smi.3287. [Google Scholar] [PubMed] [CrossRef]
8. Zamanzadeh A, Cavoli T, Ghasemi M, Rokni L. The effect of actual and expected income shocks on mental wellbeing: evidence from three East Asian countries during COVID-19. Econ Hum Biol. 2024;53:101378. doi:10.1016/j.ehb.2024.101378. [Google Scholar] [PubMed] [CrossRef]
9. Yu GL. Chinese students’ mental health problems the detection rate and educational implications. Tsinghua J Educ. 2022;4:20–32. (In Chinese). doi:10.14138/j.1001-4519.2022.04.002013. [Google Scholar] [CrossRef]
10. Liu X, Zhang Y, Cao X. Achievement goal orientations in college students: longitudinal trajectories, related factors, and effects on academic performance. Eur J Psychol Educ. 2024;39(3):2033–55. doi:10.1007/s10212-023-00764-8. [Google Scholar] [CrossRef]
11. Liu X, Zhang Y, Gao W, Cao X. Developmental trajectories of depression, anxiety, and stress among college students: a piecewise growth mixture model analysis. Humanit Soc Sci Commun. 2023;10(1):736. doi:10.1057/s41599-023-02252-2. [Google Scholar] [CrossRef]
12. Cao X, Ji S. Bidirectional relationship between self-rated health and the big five personality traits among Chinese adolescents: a two-wave cross-lagged study. Humanit Soc Sci Commun. 2024;11(1):200. doi:10.1057/s41599-024-02699-x. [Google Scholar] [CrossRef]
13. Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behav Ther. 2004;35(4):639–65. doi:10.1016/S0005-7894(04)80013-3. [Google Scholar] [CrossRef]
14. Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44(1):1–25. doi:10.1016/j.brat.2005.06.006. [Google Scholar] [PubMed] [CrossRef]
15. Harris R. Embracing your demons: an overview of acceptance and commitment therapy. Psychother Aust. 2006;12(4):2–8. [Google Scholar]
16. Ong CW, Sheehan KG, Haaga DAF. Measuring ACT in context: challenges and future directions. J Context Behav Sci. 2023;28:235–47. doi:10.1016/j.jcbs.2023.04.005. [Google Scholar] [CrossRef]
17. Hayes SC. Acceptance and commitment therapy: towards a unified model of behavior change. World Psychiatry. 2019;18(2):226–7. doi:10.1002/wps.20626. [Google Scholar] [PubMed] [CrossRef]
18. Hsu T, Adamowicz JL, Thomas EBK. The effect of acceptance and commitment therapy on the psychological flexibility and inflexibility of undergraduate students: a systematic review and three-level meta-analysis. J Contextual Behav Sci. 2023;30:169–80. doi:10.1016/j.jcbs.2023.10.006. [Google Scholar] [PubMed] [CrossRef]
19. McCracken LM, Badinlou F, Buhrman M, Brocki KC. The role of psychological flexibility in the context of COVID-19: associations with depression, anxiety, and insomnia. J Context Behav Sci. 2021;19:28–35. doi:10.1016/j.jcbs.2020.11.003. [Google Scholar] [CrossRef]
20. Lappalainen P, Lappalainen R, Keinonen K, Kaipainen K, Puolakanaho A, Muotka J, et al. In the shadow of COVID-19: a randomized controlled online ACT trial promoting adolescent psychological flexibility and self-compassion. J Contextual Behav Sci. 2023;27:34–44. doi:10.1016/j.jcbs.2022.12.001. [Google Scholar] [PubMed] [CrossRef]
21. Fang S, Ding D, Zhang R, Huang M. Psychological mechanism of acceptance and commitment therapy and rational emotive behavior therapy for treating hoarding: evidence from randomized controlled trials. Front Public Health. 2023;11:1084467. doi:10.3389/fpubh.2023.1084467. [Google Scholar] [PubMed] [CrossRef]
22. Wang J, Fang S. The developmental trajectory of college students’ psychological flexibility: based on latent growth model. J Context Behav Sci. 2024;32:100765. doi:10.1016/j.jcbs.2024.100765. [Google Scholar] [CrossRef]
23. Merwin RM, Moskovich AA, Babyak M, Feinglos M, Honeycutt LK, Mooney J, et al. An open trial of app-assisted acceptance and commitment therapy (iACT) for eating disorders in type 1 diabetes. J Eat Disord. 2021;9(1):6. doi:10.1186/s40337-020-00357-6. [Google Scholar] [PubMed] [CrossRef]
24. Wang J, Fang S. Effects of Internet-based acceptance and commitment therapy (IACT) on adolescents: a systematic review and meta-analysis. Int J Ment Health Promot. 2023;25(4):433–48. doi:10.32604/ijmhp.2023.025304. [Google Scholar] [CrossRef]
25. Puolakanaho A, Lappalainen R, Lappalainen P, Muotka JS, Hirvonen R, Eklund KM, et al. Reducing stress and enhancing academic buoyancy among adolescents using a brief web-based program based on acceptance and commitment therapy: a randomized controlled trial. J Youth Adolesc. 2019;48(2):287–305. doi:10.1007/s10964-018-0973-8. [Google Scholar] [PubMed] [CrossRef]
26. Lappalainen R, Lappalainen P, Puolakanaho A, Hirvonen R, Eklund K, Ahonen T, et al. The Youth Compass-the effectiveness of an online acceptance and commitment therapy program to promote adolescent mental health: a randomized controlled trial. J Context Behav Sci. 2021;20:1–12. doi:10.1016/j.jcbs.2021.01.007. [Google Scholar] [CrossRef]
27. Hämäläinen T, Lappalainen P, Puolakanaho A, Lappalainen R, Kiuru N. A guided online ACT intervention may increase psychological well-being and support school engagement in adolescents. J Context Behav Sci. 2023;27:152–9. doi:10.1016/j.jcbs.2023.02.002. [Google Scholar] [CrossRef]
28. Thompson EM, Destree L, Albertella L, Fontenelle LF. Internet-based acceptance and commitment therapy: a transdiagnostic systematic review and meta-analysis for mental health outcomes. Behav Ther. 2021;52(2):492–507. doi:10.1016/j.beth.2020.07.002. [Google Scholar] [PubMed] [CrossRef]
29. Cuijpers P, van Straten A, Andersson G. Internet-administered cognitive behavior therapy for health problems: a systematic review. J Behav Med. 2008;31(2):169–77. doi:10.1007/s10865-007-9144-1. [Google Scholar] [PubMed] [CrossRef]
30. Liu ZD, Bai XY, Zhang Y, Wu MX, Liu YH, Zhu ZH, et al. Psychological flexibility training for career adaptability improvement among second-year middle-school students. Chin J Sch Health. 2021;42(3):399–403. (In Chinese). doi:10.16835/j.cnki.1000-9817.2021.03.020. [Google Scholar] [CrossRef]
31. Francis AW, Dawson DL, Golijani-Moghaddam N. The development and validation of the comprehensive assessment of acceptance and commitment therapy processes (CompACT). J Context Behav Sci. 2016;5(3):134–45. doi:10.1016/j.jcbs.2016.05.003. [Google Scholar] [CrossRef]
32. Fang S, Huang M. Revision and reliability and validity evaluation of the Chinese version of comprehensive assessment of acceptance and commitment therapy processes (CompACT) in college students. Chin J Clin Psychol. 2023;1:121–6. (In Chinese). doi:10.16128/j.cnki.1005-3611.2023.01.022. [Google Scholar] [CrossRef]
33. Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. Sydney, NSW, Australia: Psychology Foundation of Australia; 1996. [Google Scholar]
34. Harris R. ACT made simple: an easy-to-read primer on acceptance and commitment therapy. Oakland, CA, USA: New Harbinger Publications; 2009. [Google Scholar]
35. Cohen J. Statistical power analysis for the behavioral sciences. J Am Stat Assoc. 1988;84(363):19–74. [Google Scholar]
36. Gagnon J, Dionne F, Raymond G, Grégoire S. Pilot study of a Web-based acceptance and commitment therapy intervention for university students to reduce academic procrastination. J Am Coll Health. 2019;67(4):374–82. doi:10.1080/07448481.2018.1484361. [Google Scholar] [PubMed] [CrossRef]
37. Küchler AM, Kählke F, Vollbrecht D, Peip K, Ebert DD, Baumeister H. Effectiveness, acceptability, and mechanisms of change of the Internet-based intervention StudiCare mindfulness for college students: a randomized controlled trial. Mindfulness. 2022;13(9):2140–54. doi:10.1007/s12671-022-01949-w. [Google Scholar] [CrossRef]
38. Bond FW, Bunce D. The role of acceptance and job control in mental health, job satisfaction, and work performance. J Appl Psychol. 2003;88(6):1057–67. doi:10.1037/0021-9010.88.6.1057. [Google Scholar] [PubMed] [CrossRef]
39. Bardeen JR, Fergus TA. The interactive effect of cognitive fusion and experiential avoidance on anxiety, depression, stress and posttraumatic stress symptoms. J Context Behav Sci. 2016;5(1):1–6. doi:10.1016/j.jcbs.2016.02.002. [Google Scholar] [CrossRef]
40. Mellick W, Vanwoerden S, Sharp C. Experiential avoidance in the vulnerability to depression among adolescent females. J Affect Disord. 2017;208:497–502. doi:10.1016/j.jad.2016.10.034. [Google Scholar] [PubMed] [CrossRef]
41. Huang M, Jin T, Zhao S. The influence of college students’ psychological inflexibility on depression: the role of ruminative responses and mindfulness. Psychol Res. 2019;5:469–76. (In Chinese). [Google Scholar]
42. Hayes SC, Levin ME, Plumb-Vilardaga J, Villatte JL, Pistorello J. Acceptance and commitment therapy and contextual behavioral science: examining the progress of a distinctive model of behavioral and cognitive therapy. Behav Ther. 2013;44(2):180–98. doi:10.1016/j.beth.2009.08.002. [Google Scholar] [PubMed] [CrossRef]
43. Zhao C, Wampold BE, Ren Z, Zhang L, Jiang G. The efficacy and optimal matching of an Internet-based acceptance and commitment therapy intervention for depressive symptoms among university students: a randomized controlled trial in China. J Clin Psychol. 2022;78(7):1354–75. doi:10.1002/jclp.23329. [Google Scholar] [PubMed] [CrossRef]
44. Välimäki M, Anttila K, Anttila M, Lahti M. Web-based interventions supporting adolescents and young people with depressive symptoms: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2017;5(12):e180. doi:10.2196/mhealth.8624. [Google Scholar] [PubMed] [CrossRef]
45. Hayes SC, King GA. Acceptance and commitment therapy: what the history of ACT and the first 1,000 randomized controlled trials reveal. J Context Behav Sci. 2024;33:100809. doi:10.1016/j.jcbs.2024.100809. [Google Scholar] [CrossRef]
46. Wang D, Lin B, Zhang S, Xu W, Liu X. Effectiveness of an Internet-based self-help acceptance and commitment therapy program on medical students’ mental well-being: follow-up randomized controlled trial. J Med Internet Res. 2024;26:e50664. doi:10.2196/50664. [Google Scholar] [PubMed] [CrossRef]
47. Cao XJ, Liu XQ. Artificial intelligence-assisted psychosis risk screening in adolescents: practices and challenges. World J Psychiatry. 2022;12(10):1287–97. doi:10.5498/wjp.v12.i10.1287. [Google Scholar] [PubMed] [CrossRef]
48. Lee EE, Torous J, De Choudhury M, Depp CA, Graham SA, Kim HC, et al. Artificial intelligence for mental health care: clinical applications, barriers, facilitators, and artificial wisdom. Biol Psychiatry Cogn Neurosci Neuroimag. 2021;6(9):856–64. doi:10.1016/j.bpsc.2021.02.001. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF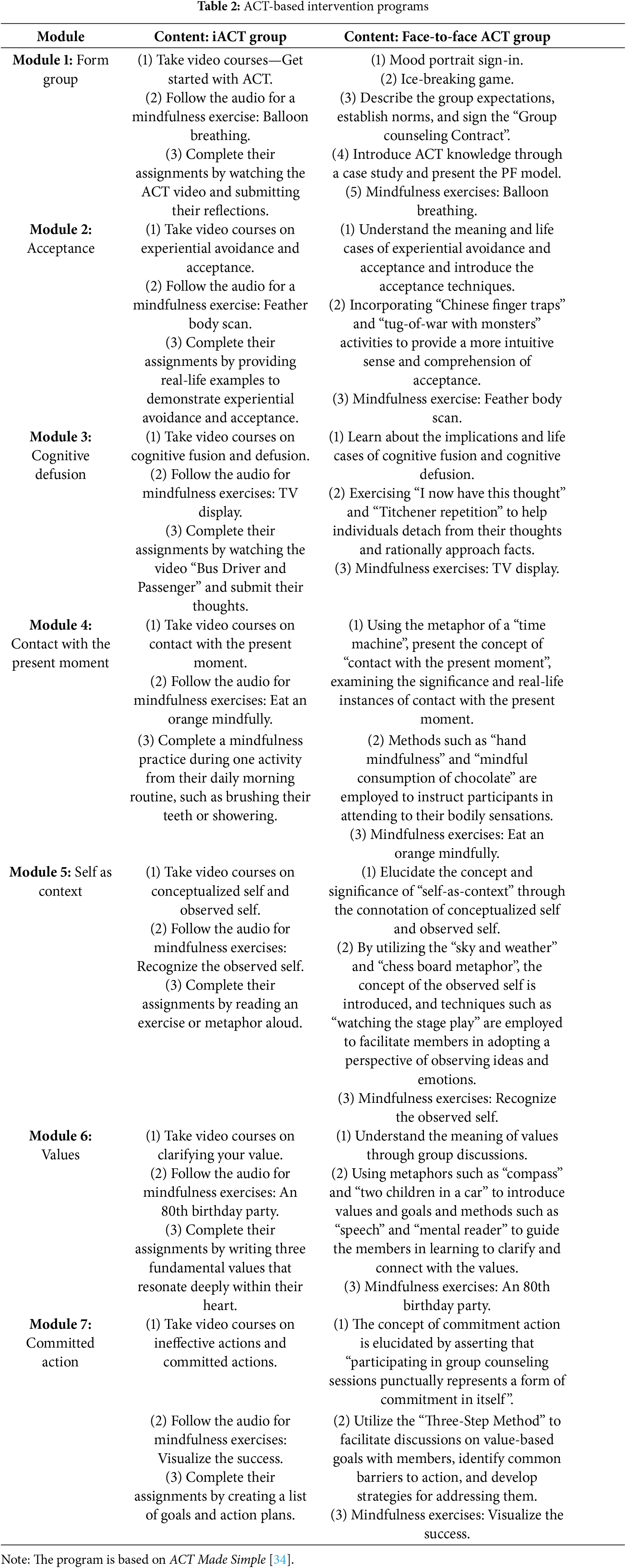
 Downloads
Downloads
 Citation Tools
Citation Tools