 Open Access
Open Access
ARTICLE
Rumination and Coping as Pathways from Stress to Emotional Exhaustion among Hospital Pharmacists
1 Department of Psychiatry, National Clinical Research Center for Mental Disorders, and National Center for Mental Disorders, The Second Xiangya Hospital of Central South University, Changsha, 410011, China
2 Mental Health Institute of Central South University, China National Technology Institute on Mental Disorders, Hunan Technology Institute of Psychiatry, Hunan Key Laboratory of Psychiatry and Mental Health, Hunan Medical Center for Mental Health, Changsha, 410011, China
3 Department of Mathematics, Nazarbayev University, Nur-Sultan, 010000, Kazakhstan
4 Department of Pharmacology and Toxicology, Faculty of Veterinary and Animal Sciences, The Islamia University of Bahawalpur, Bahawalpur, 63100, Pakistan
* Corresponding Author: Erum Rehman. Email:
(This article belongs to the Special Issue: Interdisciplinary Perspectives on Social and Behavioral Determinants of Mental Health: From Theory to Practice)
International Journal of Mental Health Promotion 2025, 27(6), 823-843. https://doi.org/10.32604/ijmhp.2025.063582
Received 18 January 2025; Accepted 21 March 2025; Issue published 30 June 2025
Abstract
Objectives: Emotional exhaustion among healthcare professionals, particularly pharmacists, significantly impacts their well-being and efficacy in patient care. Understanding the psychological mechanisms contributing to emotional exhaustion is essential for developing effective interventions. The present research sought to investigate the potential mediating roles of rumination and coping strategies (adaptive and maladaptive) in the relationship between perceived stress and emotional exhaustion among pharmacists. Methods: A cross-sectional survey was carried out between September 2023 and January 2024 involving 576 pharmacists working in public hospitals in Punjab who met the inclusion criteria and actively participated in the study. We employed the Perceived Stress Scale, the Ruminative Response Scale, the Brief Coping Orientation to Problems Experienced Inventory (COPE), and the Oldenburg Burnout Inventory (OLBI) to assess the hypothesized study model. Path analysis was employed to test the hypothesized mediation model, incorporating simple and chain mediation processes. Results: The findings provided empirical evidence supporting a positive association between perceived stress and emotional exhaustion. Rumination significantly mediated this relationship. Further, both adaptive and maladaptive coping strategies were found to mediate this relationship, with maladaptive coping demonstrating a more substantial impact. Conclusion: The chain mediation model demonstrated that rumination and coping strategies (both maladaptive and adaptive) significantly mediate the relationship between perceived stress and emotional exhaustion among pharmacists. Specifically, rumination was found to be a key mediator, with maladaptive coping strategies having a more substantial impact. These findings provide a deeper understanding of the psychological mechanisms contributing to emotional exhaustion in the pharmacy profession.Keywords
Supplementary Material
Supplementary Material FileEmotional exhaustion, a core component of burnout, is a prevalent issue among healthcare professionals, leading to fatigue, disengagement, and reduced personal achievement [1,2]. It negatively affects individual well-being, patient care, and workplace morale and has been extensively documented across various medical disciplines [3–5]. Public-sector healthcare workers face unique stressors, including limited resources, insufficient managerial support, and rigid organizational structures, which exacerbate emotional exhaustion [6–8]. The consequences include higher absenteeism, increased turnover, and reduced professional efficacy [9,10], highlighting the need to identify and address the underlying causes of emotional exhaustion in the healthcare industry. Perceived stress, defined as an individual’s subjective understanding and reaction to external sources of stress, has been consistently associated with emotional exhaustion [11]. The Transactional Model of Stress and Coping by Lazarus and Folkman [12] provides a framework for understanding this relationship. According to this model, it is not just the stressor itself but an individual’s perception of stress that determines its psychological impact. When stress is persistent, it can evolve into chronic emotional fatigue [13]. Building on this theoretical foundation, we propose the following hypothesis:
Hypothesis I: Perceived stress is positively associated with emotional exhaustion.
Rumination is characterized by the repetitive focus on negative thoughts and emotions, often as an attempt to process stressors or solve problems [14]. While it can sometimes facilitate problem-solving, excessive rumination is associated with anxiety, depression, and post-traumatic stress disorder (PTSD) [15–17]. Research has suggested that individuals who engage in persistent rumination tend to experience heightened emotional distress, as it reinforces negative thought patterns and prolongs stress responses [18,19]. According to the Response Styles Theory (RST), rumination prolongs emotional reactions to stressors, interferes with adaptive coping mechanisms, and ultimately exacerbates psychological distress [20]. Empirical evidence supports this theory, demonstrating that rumination amplifies stress and contributes to emotional fatigue [21]. Understanding its mediating role provides valuable insights into potential cognitive intervention strategies for mitigating stress-induced exhaustion among pharmacists.
Hypothesis II: Rumination mediates the relationship between perceived stress and emotional exhaustion among pharmacists.
1.2 Coping Strategies as Mediators
Coping strategies play a crucial role in determining how individuals manage stress, particularly in relation to burnout and emotional exhaustion [22–24]. These strategies can be broadly categorized into adaptive (active) coping, which involves modifying stressors or cognitive appraisals, and maladaptive (passive) coping, which hinders active problem-solving and contributes to psychological distress [25,26]. Evidence has demonstrated that coping behaviors help explain why individuals exposed to similar stressors may experience varying levels of burnout [27]. Maladaptive strategies such as avoidance, denial, and substance use—have been consistently linked to increased psychological distress and poorer mental health outcomes [28–31]. In contrast, adaptive strategies—such as active coping, planning, and positive reframing—are associated with better stress management and reduced emotional exhaustion [32]. Skinner et al. [33] proposed that coping mechanisms shape the progression from stress to emotional exhaustion, underscoring the need to explore their mediating role in this relationship.
Hypothesis III: Coping styles (maladaptive/adaptive) mediate the relationship between perceived stress and emotional exhaustion.
1.3 Chain Mediation of Rumination and Coping Strategies
The chain mediation concept, beyond traditional mediation, provides a more comprehensive examination of the interrelated pathways linking stress, cognitive processes, and coping behaviors [34,35]. This study explores the impact of initial stress responses, mediated explicitly through rumination, on the selection and efficacy of coping mechanisms, subsequently influencing outcomes such as emotional exhaustion. Hayes [36] advocates for intricate mediation models in psychological research as they afford a more comprehensive comprehension of variables’ sequential and cumulative impacts. This model emphasizes the need for comprehensive interventions targeting cognitive patterns and behavioral responses to stress. Based on this theoretical framework, we have formulated the following hypothesis:
Hypothesis IV: Rumination and coping styles (maladaptive/adaptive) play a chain mediating role between perceived stress and emotional exhaustion.
The present research aims to contribute to the extant scholarly literature by investigating the intricate dynamics of stress, rumination, and adaptive and maladaptive coping mechanisms and their combined effect on emotional exhaustion within the pharmacist profession (Fig. 1). Prior research has extensively examined the individual impacts of stress and coping strategies in various healthcare environments. However, a dearth of studies has delved explicitly into these dynamics among pharmacists, who exclusively manage high-stress responsibilities while fulfilling crucial public health obligations. Besides, this research enhances existing knowledge by introducing a dual mediation model that explains how rumination and coping strategies (adaptive/maladaptive) mediate the link between stress and emotional exhaustion. Punjab, the most densely populated province of Pakistan, comprising approximately 53% of the nation’s populace [37], offers a substantial and varied representation that reflects a wide range of healthcare practices and challenges pharmacists encounter [38,39]. The healthcare system in Pakistan is marked by limited resources and differing levels of service provision, leading to distinct challenges and pressures for healthcare practitioners, including pharmacists [40]. These prevailing conditions in Punjab present an opportune context for investigating the complex interplay of stress, coping strategies, and emotional fatigue. The results derived from this geographic area have the potential to yield a comprehensive understanding of stress management techniques that are relevant on both a regional and global scale, particularly within analogous healthcare environments in emerging economies.
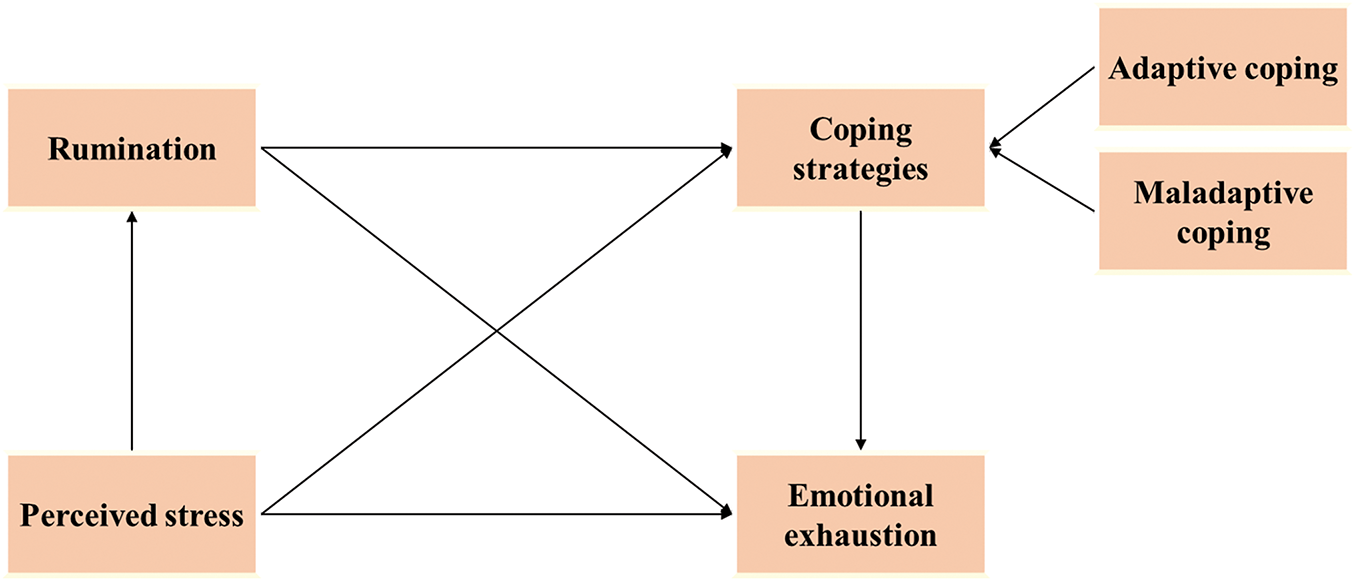
Figure 1: The hypothesized model
Consequently, the principal aim of the present research was to investigate the interconnections between pharmacists’ stress levels and coping strategies and the resulting emotional exhaustion. Additionally, the study sought to examine the potential mediating effects of rumination, adaptive coping, and maladaptive coping in this association. The study’s objectives seek to address existing gaps in the literature and provide practical and clinical frameworks for guiding interventions to mitigate burnout and promote well-being among pharmacists.
2.1 Sample Selection and Participants
The present survey was conducted among 30 public hospitals in Punjab, Pakistan, between September 2023 and January 2024. This targeted demographic encounters distinct occupational stressors such as significant workloads, detailed medication management duties, and direct interactions with patients. These factors differentiate their experience from that of other healthcare professionals and underscore the significance of examining their stress and coping strategies.
A descriptive cross-sectional survey was carried out utilizing stratified sampling across all the public hospitals in Punjab province, Pakistan, wherein each hospital served as a stratum. The sample was drawn from hospital administration records, which contain the list of pharmacists working in these hospitals. Only pharmacists who were registered with the Pakistan Pharmacy Council were eligible to participate in the study. The stratification was intended to achieve a representative sample from a diverse range of hospitals, including those of varying sizes, capacities, and geographic locations in both urban and rural areas of Punjab.
The data collection process involved using a structured questionnaire with validated scales, which was sent through online channels such as professional email lists and hospital intranet systems, as well as in person. This approach was employed to facilitate broad accessibility for pharmacists with differing access levels to digital resources. Fig. 2 illustrates the study design of the paper.
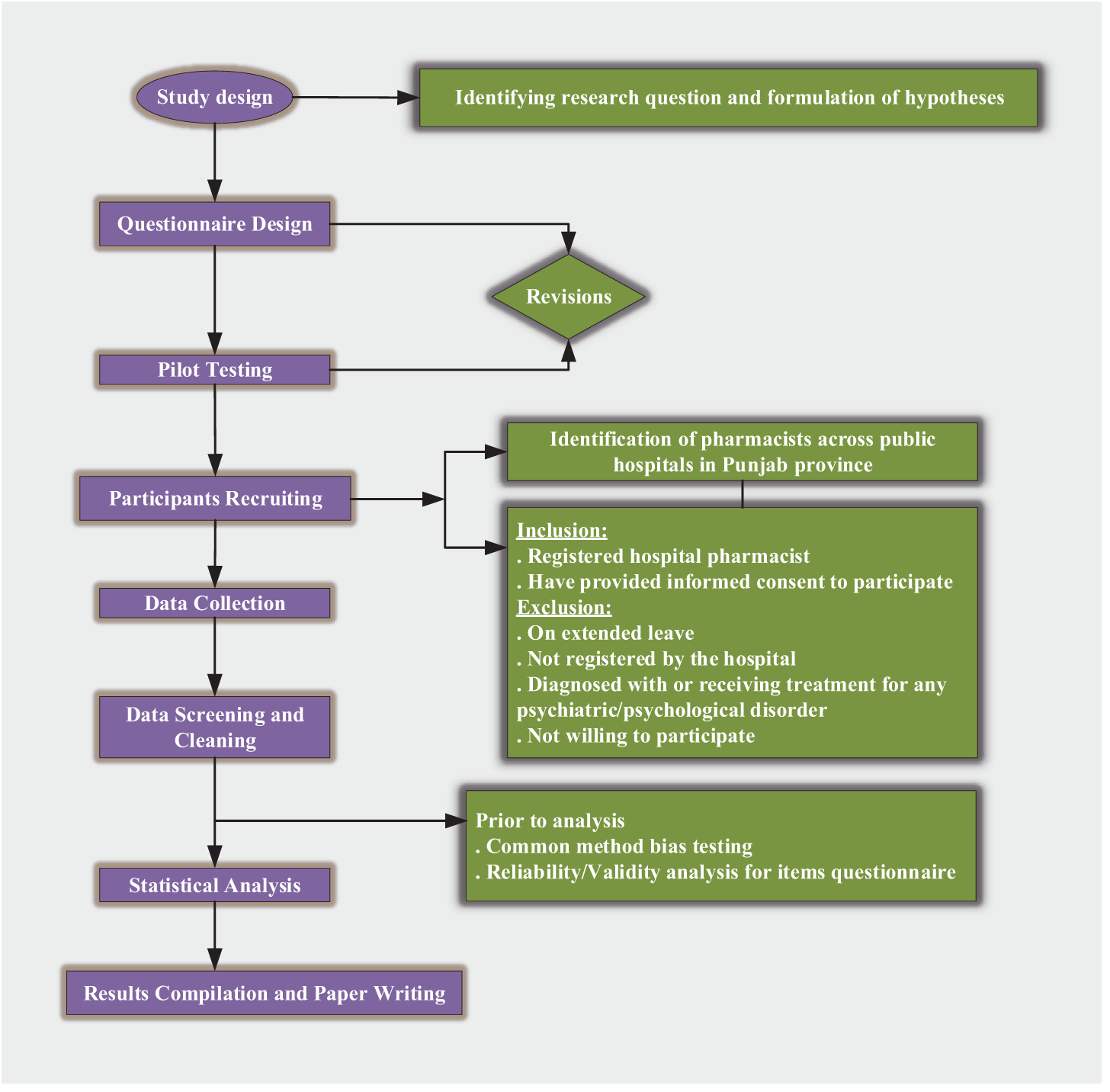
Figure 2: Study design
The questionnaire underwent a pilot test with 35 individuals to ensure its reliability and validity within the context of Pakistani pharmacists. The pilot test aimed to identify potential issues inherent in the survey design, including question clarity, response options, and overall comprehensibility. Based on the feedback, minor adjustments were made to the survey instrument through collaborative discussions between the research team and professional experts. The results of the pilot test are available in Supplementary File.
The sample size was determined using Cochrane’s formula to estimate proportions appropriately within a specified margin of error (5%) and confidence interval (95%). The initial sample size was estimated to be 384; however, to adjust for the design effect resulting from stratification, an effect of 1.5 was employed, a standard practice to mitigate the consequent rise in variance (384 ∗ 1.5 = 576). After accounting for design effects, the estimated sample size was 576. A final sample size of 576 was chosen as a balance between feasibility, manageability, and the need for sufficient statistical power to detect significant relationships within the study’s context.
Inclusion criteria: Registered hospital pharmacists actively participating within the Punjab province and willing to participate by completing an informed consent form.
Exclusion criteria: Those on extended leave (e.g., maternity, sabbatical) or retired, not currently employed by the hospital, diagnosed with or receiving treatment for psychiatric or psychological disorders, and non-consenting during data collection.
2.7.1 Demographic Characteristics
Socio-demographic variables, including age, gender, educational level, marital status, number of Children, ethnicity, year of experience, employment status, shift work, and income level, were reported.
2.7.2 Perceived Stress Scale 10 (PSS-10)
Cohen [41] developed the PSS-10 as a self-reported measure designed to assess individuals’ overall perceived stress levels, delineated into two dimensions: perceived helplessness, reflected in negatively phrased items, and perceived self-efficacy, manifested in positively worded items. Participants were asked to indicate the frequency of their emotions for the previous month using a 5-point Likert scale (Never: 0 to Very often: 4). To obtain the overall scores, the scoring of positive statements was inverted such that a rating of 4 denoted ‘never’ and a rating of 0 represented ‘very often.’ The aggregate score of the PSS-10 spans from 0 to 40, with higher scores indicative of a heightened degree of stress. The PSS-10 scale has been validated in the Urdu version by Mushtaq and Ahmed [42], demonstrating a robust internal consistency coefficient of 0.83. The English version of this measure has been previously validated in the Pakistani community, demonstrating acceptable internal consistency across different demographic groups [43–45]. In this study, the PSS-10 showed high reliability, achieving a Cronbach’s alpha of 0.87 (see Table 1).
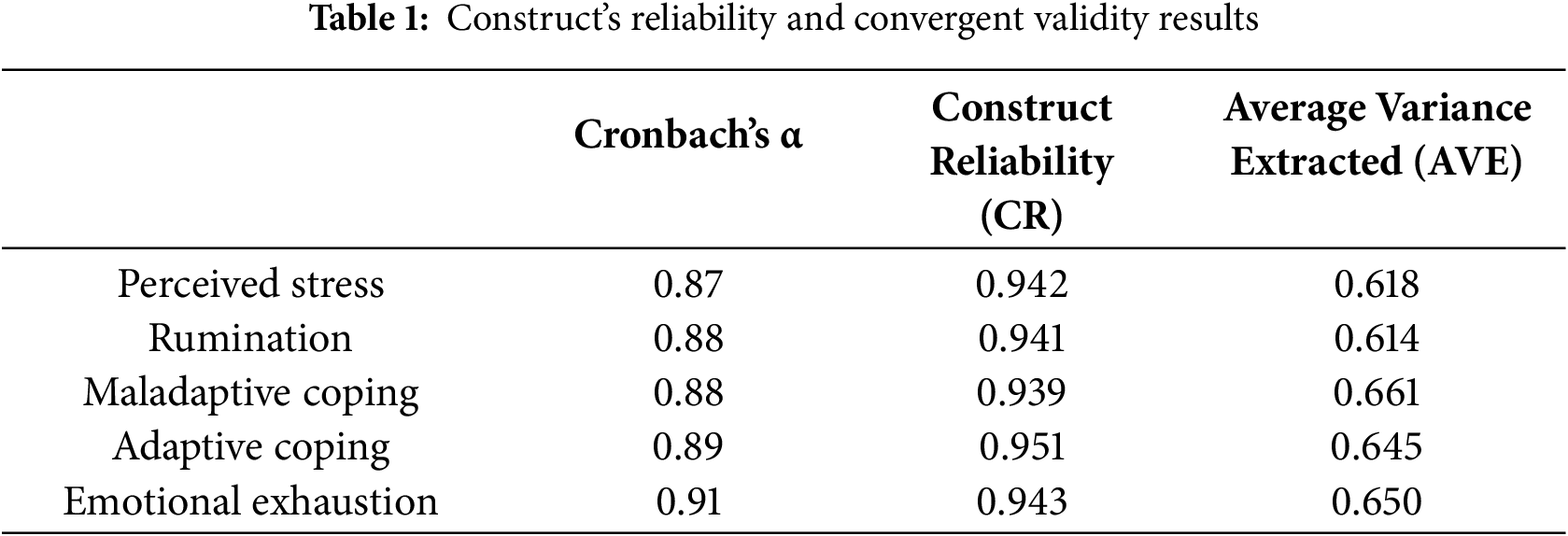
2.7.3 10-Item Ruminative Response Scale (RRS-10)
The RRS-10 is a short form of the comprehensive Response Styles Questionnaire, originally developed to evaluate cognitive patterns and responses associated with depression [20]. However, research has shown that rumination is a transdiagnostic factor relevant across various populations [46], including non-depressed individuals, where it influences psychological well-being and responses to stress [47,48]. The RRS-10 consists of ten items divided into two subscales: Brooding and Reflection. Participants rated their responses on a 4-point Likert scale ranging from 1 (never) to 4 (always), with higher scores indicating a stronger inclination toward rumination. The scale has demonstrated strong internal consistency and test-retest reliability across multiple studies [49–51]. Additionally, the RRS-10 has been validated within the Pakistani population, confirming an acceptable level of reliability for this context [52]. The internal consistency of the RRS-10 was confirmed in this study, with a Cronbach’s alpha coefficient of 0.88 (see Table 1).
The Brief-COPE (Coping Orientation to Problems Experienced Inventory) questionnaire is a validated tool that assesses effective and poor coping strategies in response to a stressful life event [53]. The study participants were evaluated using this 28-item self-reported questionnaire on a 4-point Likert scale (1: I have not been doing at all—4: I have been doing this a lot). Within the stress-coping concept, specific coping strategies are categorized as either primarily adaptive (active coping, planning, positive reframing, acceptance, humor, religion, using emotional support, and using instrumental support) or maladaptive (self-distraction, denial, venting, substance use, behavioral disengagement, and self-blame) [54,55]. Individuals with higher scores in adaptive coping demonstrate an inclination towards utilizing constructive strategies when confronted with adversities. In comparison, those who achieve higher scores in maladaptive coping exhibit a propensity toward embracing unfavorable techniques. This measure has demonstrated strong validity and reliability among the Pakistani population in English and Urdu [56,57]. In this sample, the adaptive coping subscale showed good internal consistency (α = 0.89), while the maladaptive coping subscale achieved a Cronbach’s α of 0.91 (see Table 1).
2.7.5 The Oldenburg Burnout Inventory
The OLBI (Oldenburg Burnout Inventory) is a 16-item validated construct that assesses burnout and consists of two distinct components: exhaustion (8 items) and disengagement (8 items) with positively and negatively phrased items. However, our study primarily focused on the exhaustion component of burnout, broadly regarded as the primary feature of burnout, especially in demanding healthcare settings such as hospital pharmacies. The study participants were instructed to assess the frequency with which they encounter a particular sensation using a rating scale ranging from 1 (indicating strongly disagree) to 4 (indicating strongly agree). The validity of this scale has been thoroughly established in a range of professional fields, with a particular emphasis on its application in healthcare environments [58–60]. This subscale has consistently demonstrated strong reliability across various studies [61–63], signifying its ability to consistently and accurately measure burnout. The scale demonstrated good internal reliability in the current sample, with a reliability estimate of 0.91 (see Table 1).
The study participants were informed that the data collected from these constructs would remain confidential and only accessible to the researchers and their team. Informed consent has been taken from all the participants. The study has been authorized by the Ethics Review Committee (ERC) of the Islamia University of Bahawalpur, Lahore, Pakistan (No. DR/2044).
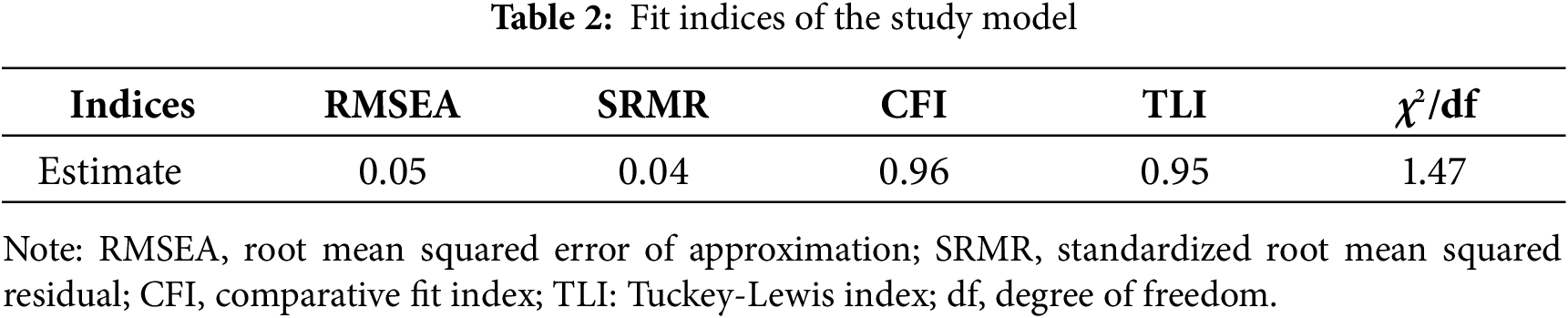
We initially screened the data on the study variables for normality using the Kolmogorov-Smirnov test to confirm their suitability for subsequent parametric analyses. We then performed Harman’s single-factor test to mitigate potential common method bias. The constructs’ reliability was evaluated by Cronbach’s alpha for each construct, ensuring internal consistency. Convergent validity was estimated by analyzing each construct’s average variance extracted (AVE), with values >0.5 considered acceptable. The structural model was evaluated using path analysis via structural equation modeling (SEM), facilitating the estimation of associations between perceived stress, rumination, coping strategies (adaptive and maladaptive), and emotional exhaustion. The model adequacy was assessed using model fit indices:
The method utilized for data collection in the present survey was based on self-reported measures. Therefore, recognizing these methodologies can introduce a CMB, which may impact the study findings. In response to this issue, we employed Harman’s single-factor test method to analyze the potential presence of CMB in the dataset. The Kaiser-Meyer-Olkin (KMO) score, estimated at 0.853 (at p < 0.001), suggests that the data is appropriate for conducting exploratory factor analysis (EFA). The principal component analysis (PCA) performed on the variable measurement items indicated that the initial principal component explained approximately 29.51% of the overall variation, failing to meet the threshold value of 40%. This implies that the deviation of measurement bias did not substantially influence the study outcomes.
A reliability assessment was performed on the hypothesized model, utilizing data obtained by administering questionnaires. The findings revealed that Cronbach’s alpha coefficients of all selected study constructs varied from 0.86 to 0.91, suggesting a satisfactory level of internal consistency. While the construct reliability (CR) values for each construct exceeded 0.7. The AVE values for each construct exceeded the prescribed threshold of 0.5, indicating favorable levels of reliability and validity within the construct (Table 1).
The maximum likelihood method was employed to assess the model parameters. The evaluation of the overall adequacy of the model reveals that all of the indices satisfied the required testing standards. Hence, the model exhibited a robust fit, thus yielding satisfactory outcomes (Table 2).
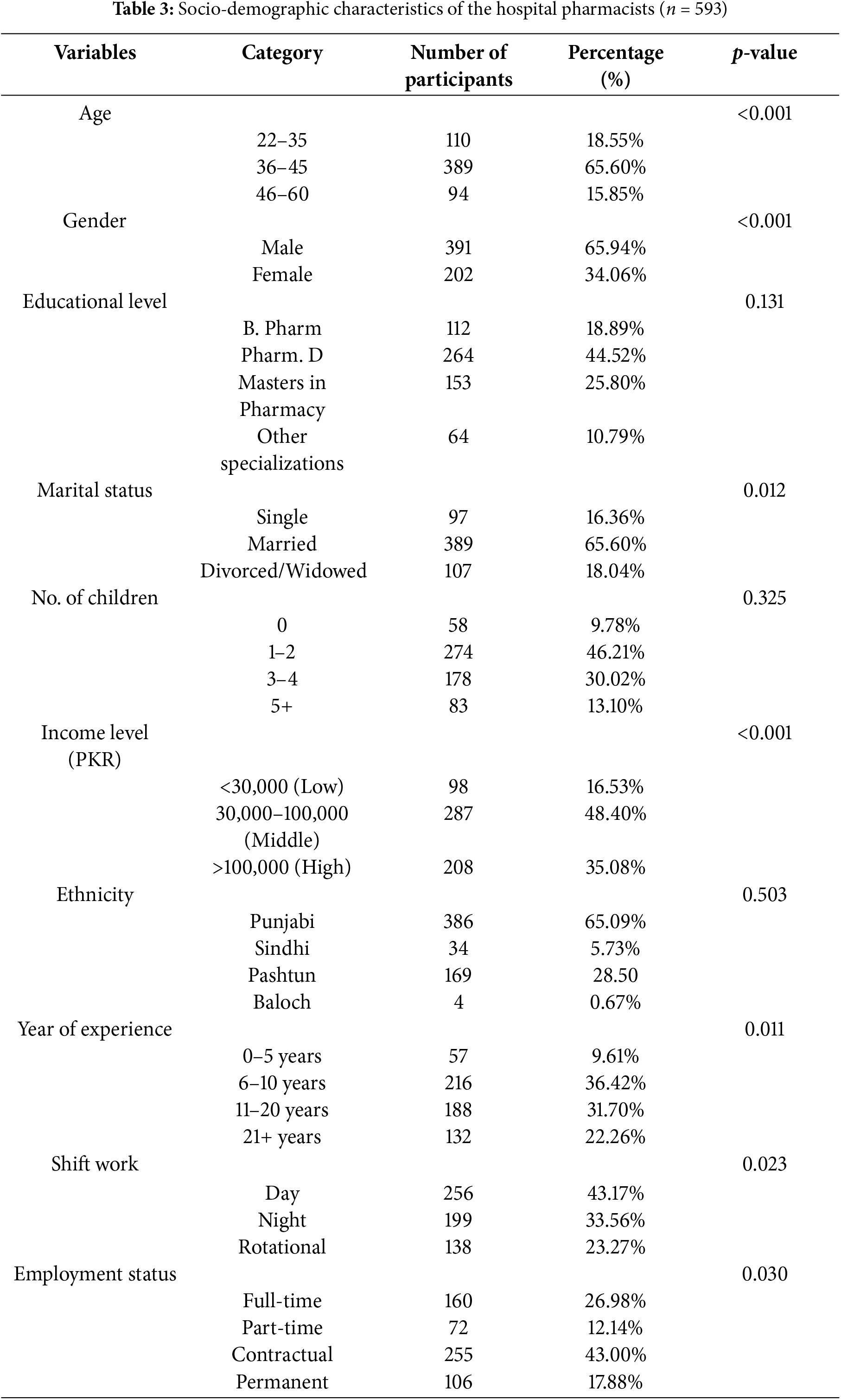
3.3 Socio-Demographic Information
Table 3 exhibits a socio-demographic analysis of 593 hospital pharmacists, indicating a diversified cohort primarily in the mid-career stage, with 66% of individuals falling within the age range of 36 to 45 years with a considerable proportion (66%) of males. There is a diversity in educational levels within the field, with most individuals holding a Doctor of Pharmacy degree (Pharm. D). The attainment of a degree is a significant accomplishment that marks the successful completion of a program of study at an institution of higher education. Most individuals in this demographic are married and have between one and two children, which reflects common family structures within the study population. A significant disparity in income distribution exists, characterized by a pronounced division between individuals in the middle-income bracket and those in the high-income bracket, which may affect economic dynamics. The workforce composition is predominantly Punjabi and Pashtun, with no statistically significant differences evident in these ethnic demographics. The distribution of years of experience indicates a predominantly seasoned workforce, with a considerable proportion possessing more than six years of experience in the field. Diversity in work patterns and employment status exists, giving rise to variations in job security and lifestyle effects. Many individuals are engaged in contractual arrangements or rotational shift schedules. The present demographic overview offers a comprehensive analysis of pharmacists’ professional and personal characteristics, essential for gaining insights into their working conditions and behaviors.
3.4 Bivariate Correlations between Study Constructs
Table 4 illustrates the bivariate correlations among the study variables estimated using Pearson’s correlation coefficient. The findings demonstrated a significant correlation between perceived stress and the utilization of coping strategies (maladaptive: r = 0.323, p < 0.001: adaptive: r = 0.378, p < 0.001), as well as an association with heightened levels of rumination (r = 0.432, p < 0.001) and emotional exhaustion (r = 0.310, p < 0.001). These results suggested that as perceptions of stress increase, so does their tendency to engage in rumination, coping strategy employment, and feelings of burnout. Likewise, there was a significant association between rumination and coping strategies (maladaptive: r = 0.512, p < 0.001: adaptive: r = 0.581, p < 0.001), suggesting that individuals who exhibit higher levels of rumination are more inclined to employ both adaptive and maladaptive coping mechanisms. Additionally, it demonstrates a positive correlation with increased emotional exhaustion (r = 0.459, p < 0.001), thus underscoring its influence on the deterioration of psychological well-being. Simultaneously, the utilization of maladaptive coping strategies is linked to emotional exhaustion (r = 0.452, p < 0.001), indicating that individuals employing these techniques are likely to be experiencing heightened levels of burnout. The observed weak correlation between adaptive coping suggests that individuals have a degree of independence in utilizing these strategies. Although adaptive coping has been shown to have a positive impact, it is also associated with increased emotional exhaustion (r = 0.509, p < 0.001). This suggests that individuals may rely on coping strategies more frequently in situations of high stress or extreme fatigue, even when these strategies are effective.
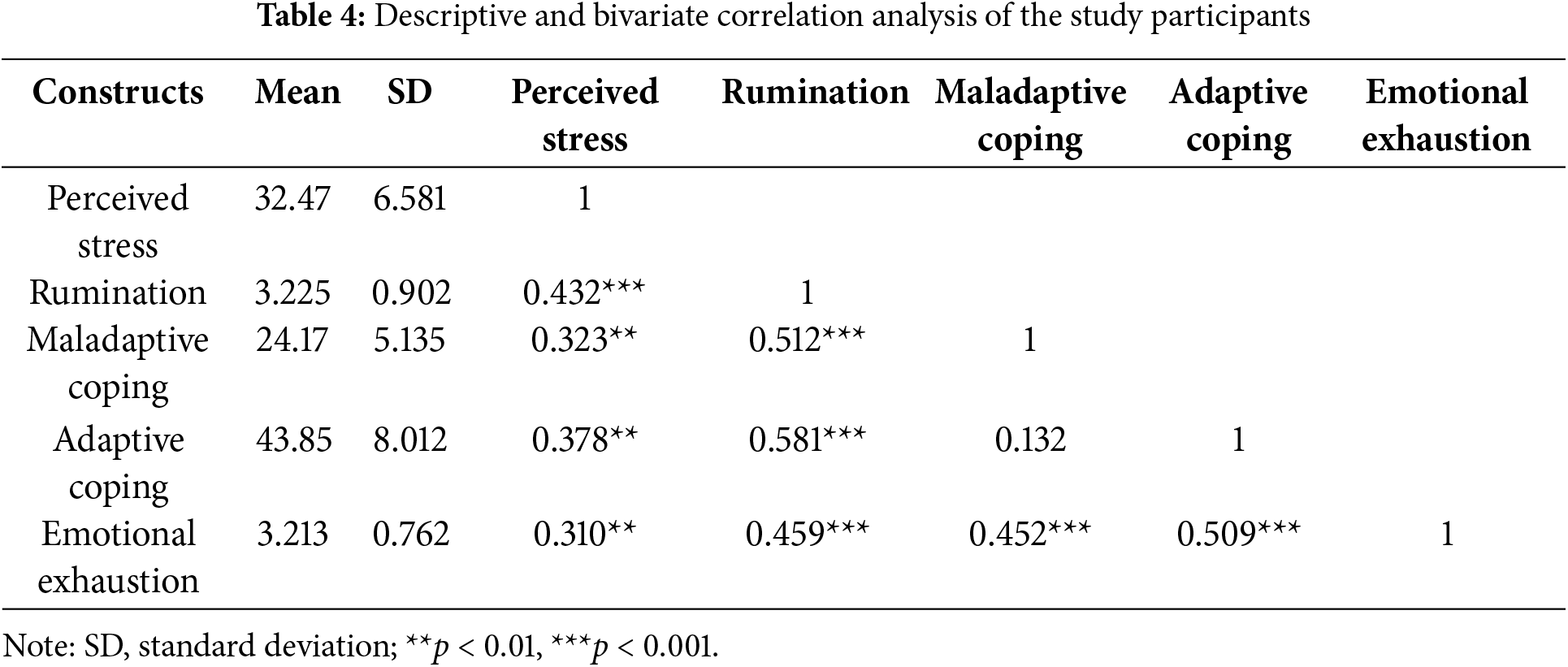
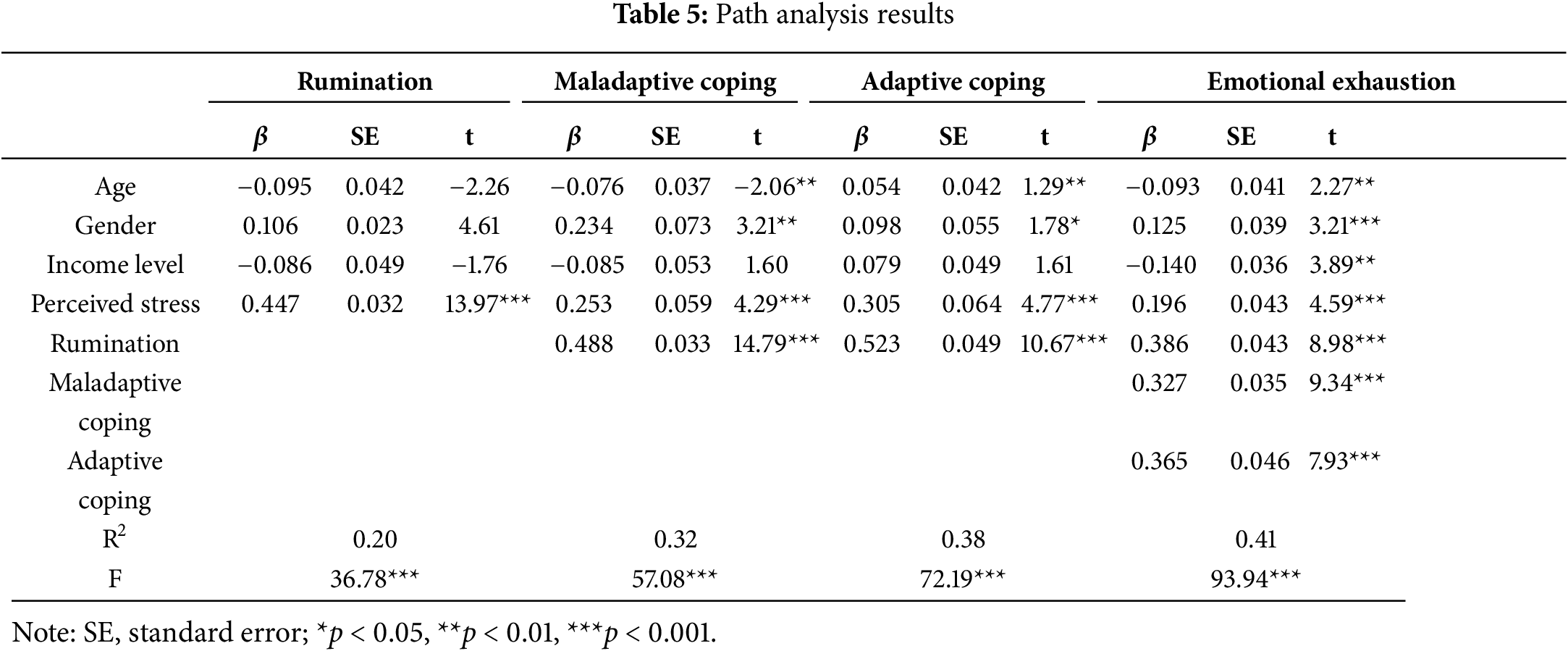
Table 5 demonstrates the results of the path analysis by keeping age, gender, and income level as control variables. The findings indicated that perceived stress has a substantial impact, leading to a significant increase in rumination (β = 0.447), as well as maladaptive (β = 0.253) and adaptive coping (β = 0.305) strategies and emotional exhaustion (β = 0.196). This emphasizes the considerable effect of stress in exacerbating adverse psychological consequences. Despite the implementation of various controls, rumination has been found to enhance maladaptive (β = 0.488) and adaptive coping (β = 0.523) strategies substantially and contribute to emotional exhaustion (β = 0.386), thus underscoring its pivotal role in shaping individual responses to stress. The correlation between maladaptive coping and heightened emotional exhaustion (β = 0.327) suggests that ineffective coping strategies may contribute to the worsening of burnout (emotional exhaustion) associated with stress. Notably, the use of adaptive coping strategies, often perceived as advantageous, is linked to elevated levels of emotional exhaustion (β = 0.365), indicating that employing such strategies may predict responses to heightened underlying stress levels. The statistical models exhibited a moderate to significant explanatory power (R2 = 0.20–0.41), confirming the findings’ strength and reliability, highlighting the necessity of implementing focused interventions to alleviate stress and enhance coping mechanisms among hospital pharmacists.
3.6 Sequential Mediation Analysis Results
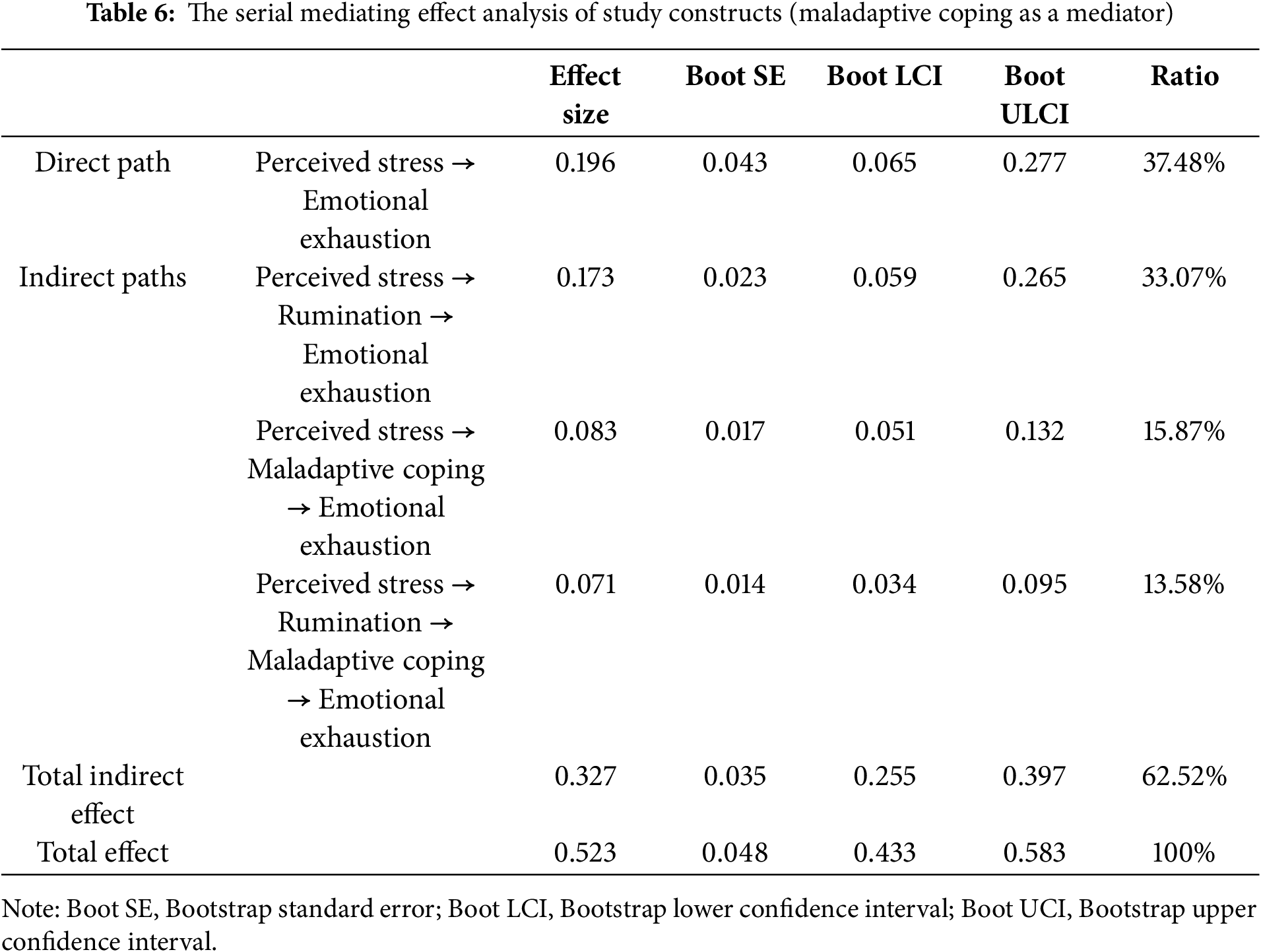
3.6.1 Rumination and Maladaptive Coping as Mediators
Table 6 demonstrates the results of sequential mediation analysis with rumination and maladaptive coping strategies as mediators. The findings indicated a statistically significant direct impact of perceived stress on emotional exhaustion, yielding a direct effect size of 0.196 and explaining 37.48% of the overall effect. The indirect effect of rumination alone is particularly substantial, with an effect size of 0.173, accounting for 33.07% of the total effect. In addition, maladaptive coping alone yields a more modest yet significant effect size of 0.083, comprising 15.87% of the total effect. The results indicated a compounded effect size of 0.071 (13.58% of the total) observed in the serial mediation process involving rumination and maladaptive coping. The cumulative indirect effects make a noteworthy contribution to the overall impact, with an effect size of 0.327, accounting for 62.52% of the total impact. This implies that stress influences emotional exhaustion through mediation via these pathways. The overall effect of stress on emotional exhaustion, accounting for both direct and indirect pathways, is substantial and statistically significant (effect size = 0.523). The confidence intervals for all the indirect and direct effect paths did not include zero, suggesting that the estimated effects were significant. The results indicated a partial mediation in which stress directly affects emotional exhaustion and influences it through sequential mediators, explicitly emphasizing the importance of rumination and maladaptive coping strategies in this mechanism.
3.6.2 Rumination and Adaptive Coping as Mediators
Table 7 displays the mediation effects of rumination and adaptive coping in the relationship between perceived stress and emotional exhaustion (Fig. 3). The findings revealed a significant direct effect of stress, indicated by an effect size of 0.196 (34.69% of the overall effect). This suggests a state of partial mediation, in which stress directly impacts emotional exhaustion while also exerting indirect effects through sequential mediators. The indirect effect via rumination is statistically significant, with an effect size of 0.173, accounting for 30.62% of the total effect. Additionally, adaptive coping demonstrates a significant mediation effect of 0.111, contributing 19.65% to the total effect.
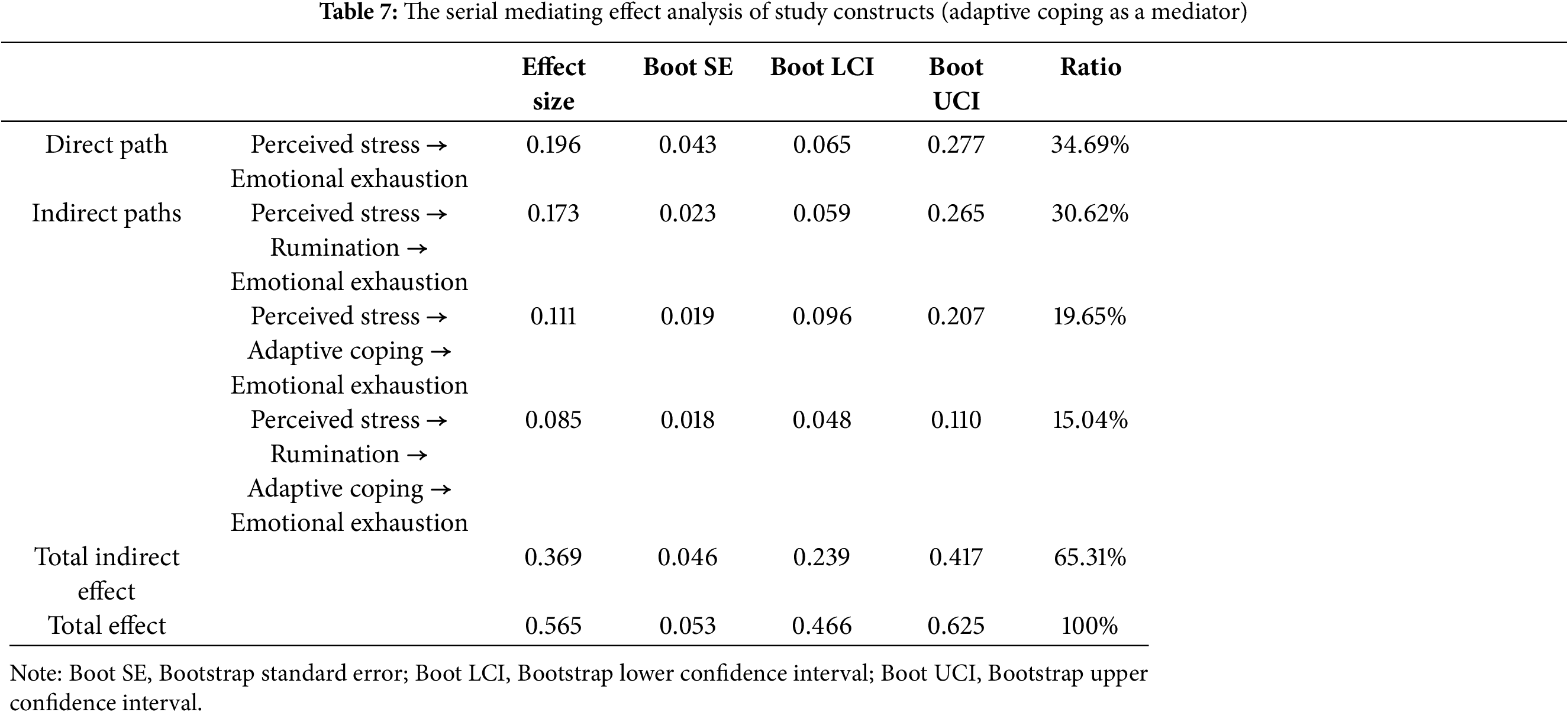
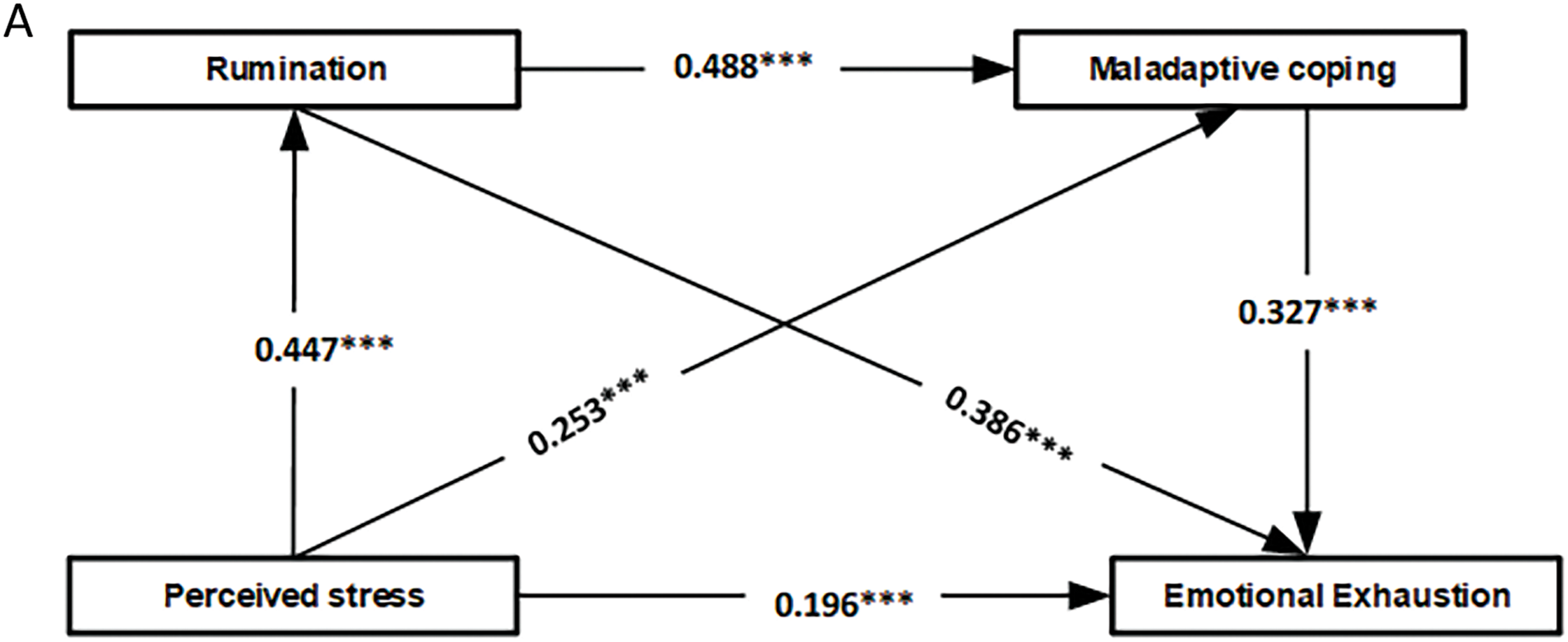
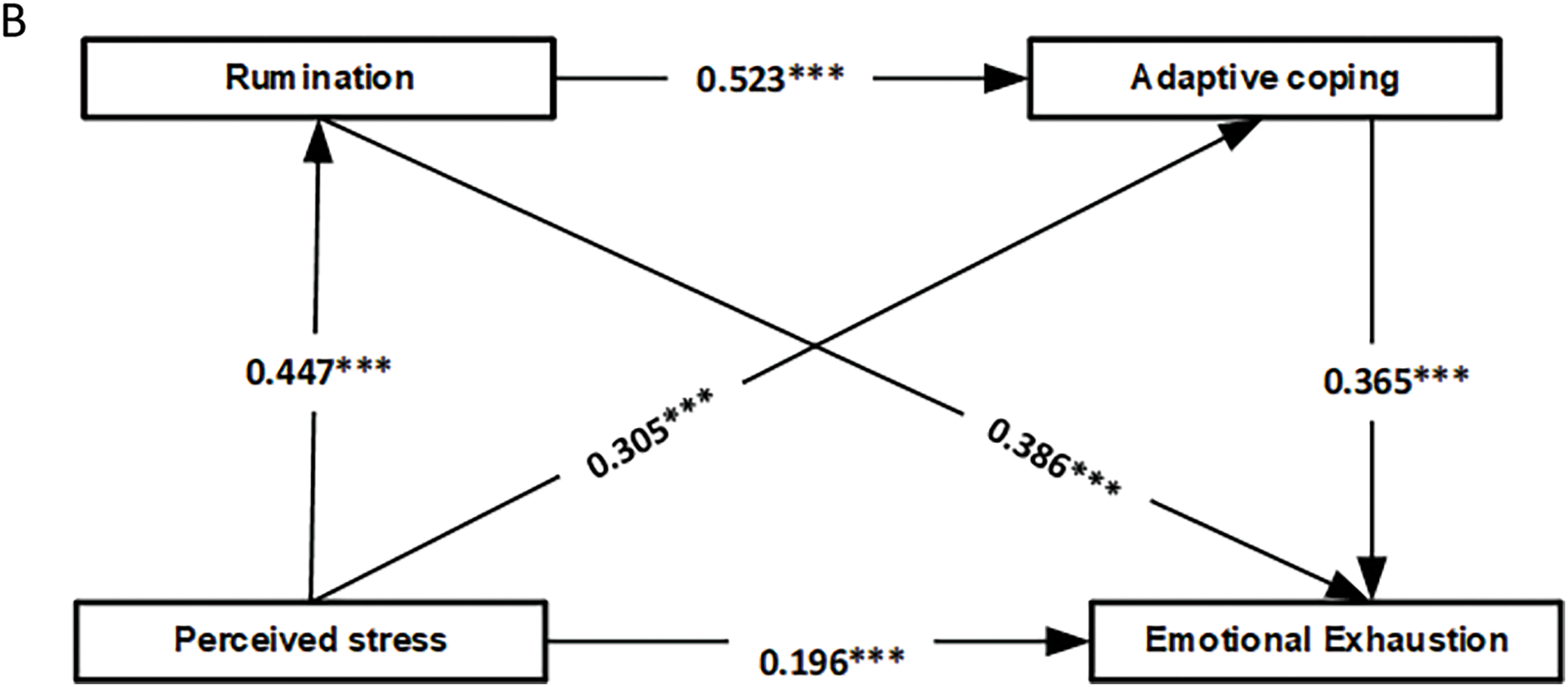
Figure 3: The path mediation model. (A) Maladaptive coping; (B) Adaptive coping. ***p < 0.001
Moreover, the consecutive progression from rumination to adaptive coping demonstrates an effect size of 0.085, explaining 15.04% of the overall effect. The cumulative indirect effects amount to a substantial value of 0.369, accounting for 65.31% of the overall impact, thereby emphasizing the significant contribution of mediated mechanisms. The study findings indicated the direct, substantial impact of stress and emotional exhaustion, with an effect size of 0.565. Furthermore, the confidence intervals consistently exclude zero, providing strong support for the significance of the mediation model.
The present work enhances our comprehension of psychological mechanisms within pharmacy practice by proposing an innovative tripartite mediation model that highlights the functions of stress, rumination, and adaptive and maladaptive coping techniques in developing emotional exhaustion. The results indicated that elevated stress levels were significantly associated with rumination and the adoption of ineffective coping mechanisms, leading to a notable intensification of emotional exhaustion among pharmacists. These findings underscore the negative pattern in which stress not only relates to mental well-being directly but also indirectly aggravates it through maladaptive coping strategies. Contrary to prior research that frequently examined these components separately, our integrated methodology offers a more thorough comprehension of these aspects’ interconnections and mutual influence within the demanding pharmacy practice environment.
The findings of our study supported Hypothesis I by demonstrating a significant positive correlation between perceived stress and emotional exhaustion. The finding was aligned with a substantial body of research that suggested that stress plays a crucial role in the development of burnout, especially in emotional exhaustion among healthcare professionals [64–66]. A cross-sectional study conducted by Durham et al. [65] found that stress, especially in high-pressure settings such as pharmacies, plays a significant role in the depletion of emotional resources, which is consistent with recent research in a similar setting [67]. Furthermore, research conducted in hospital settings, such as the studies conducted by Higuchi et al. [66], Haase [68], and Jones et al. [69], have demonstrated similar patterns, whereby the compounding effects of stress not only hinder day-to-day functioning but also increase the likelihood of experiencing prolonged psychological distress. Furthermore, mounting evidence suggests that sustained high-stress levels can predict the progression of emotional exhaustion over time [64,70,71]. These findings underscore the urgent need for targeted stress management interventions in pharmacy settings, highlighting that reducing workplace stress could significantly alleviate emotional exhaustion among pharmacists.
In addition, our study provided empirical support for Hypothesis II by showing that rumination was a significant mediator in the relationship between perceived stress and emotional exhaustion among study participants. The mediation proposed was aligned with cognitive theories of stress [72], positing that an individual’s cognitive processing of stressors significantly influences their emotional responses. Likewise, researchers have demonstrated that rumination serves to protract the duration of an individual’s emotional stress response while also contributing to the exacerbation of stress-related disorders [73]. In alignment with our findings, Donahue et al. provide additional support that individuals who frequently engaged in ruminative thoughts exhibited elevated levels of emotional exhaustion [74]. This highlighted the maladaptive nature of rumination as a coping mechanism, indicating its propensity to reinforce perceptions of stress. Rumination has been proven to mediate the relationship between work-related stress and burnout over an extended timeframe [75,76], implying that interventions targeting the reduction of rumination may prove effective in alleviating emotional exhaustion. These studies collectively demonstrate the negative association of rumination with mental health and confirm the significance of addressing cognitive processes in stress management programs targeted toward healthcare professionals.
Furthermore, our study’s findings support Hypothesis III, demonstrating that maladaptive and adaptive coping strategies mediate the relationship between perceived stress and emotional exhaustion. The present mediation is aligned with Lazarus and Folkman’s stress and coping theory [12], which emphasizes that the effectiveness of coping mechanisms significantly influences emotional outcomes. Skinner et al. [33] found that maladaptive coping mechanisms, including denial and substance use, intensify stress reactions, resulting in elevated levels of emotional exhaustion. On the other hand, it has been demonstrated that adaptive coping mechanisms, such as problem-solving and positive reframing, can mitigate the effects, as mentioned earlier. However, contextual factors and individual resilience traits may influence their effectiveness [77,78]. Moreover, Folkman and Moskowitz [79] indicated that although adaptive coping strategies may alleviate some immediate stress, they may not consistently diminish long-term emotional fatigue, particularly in ongoing stressors. Our findings suggest that a multifaceted approach is necessary to effectively manage pharmacists’ high-stress levels, as adaptive coping alone may be insufficient. This underscores the importance of comprehensive stress management programs that integrate both proactive and reactive coping strategies to support long-term well-being.
Moreover, our study provided empirical support for Hypothesis IV, demonstrating that rumination and coping styles (both maladaptive and adaptive) function as chain mediators in the relationship between perceived stress and emotional exhaustion among pharmacists. This sequential mediation model extends beyond conventional single-pathway models by illustrating how stress sequentially triggers rumination, which then influences coping behaviors, ultimately leading to emotional exhaustion. This finding aligns with Beck’s cognitive-behavioral stress model [80], which suggests that negative cognitive patterns contribute to maladaptive coping strategies and adverse emotional outcomes. Empirical studies have reinforced this model, showing that rumination increases the use of maladaptive coping mechanisms, particularly avoidance, which, in turn, heightens emotional distress [81,82]. A growing body of research suggests that reducing rumination in healthcare settings can significantly decrease maladaptive coping behaviors and mitigate burnout symptoms [83,84]. These findings highlight the potential effectiveness of cognitive-behavioral interventions in managing these challenges within the healthcare sector. The complex interaction between cognitive processes and coping strategies underscores the need for comprehensive stress management programs to alleviate emotional exhaustion associated with stress effectively.
While adaptive coping strategies are generally associated with psychological resilience and well-being, our findings indicated a significant association between adaptive coping and emotional exhaustion. One possible explanation could be that pharmacists, in an effort to maintain their performance and manage stress, may excessively rely on adaptive coping strategies, leading to cognitive and emotional fatigue. This aligns with research suggesting that even constructive coping mechanisms, when overused, may contribute to burnout and exhaustion in high-demand work environments [85]. Another plausible explanation is that the effectiveness of adaptive coping strategies may depend on contextual factors, such as workload intensity, organizational support, and the availability of recovery time. Prior research has shown mixed findings regarding adaptive coping in stressful professions, with some studies reporting protective effects while others highlight its limitations in highly pressured settings [86]. Future studies should explore the threshold at which adaptive coping becomes counterproductive and how workplace interventions can optimize coping strategies without increasing fatigue.
The results of this study hold significant implications for the design and implementation of specific interventions intended to diminish stress and foster the adoption of more adaptive coping strategies within the pharmacy profession. We propose that training programs for stress management and advancing adaptive coping strategies may yield advantageous outcomes. Furthermore, implementing policy modifications targeting the causes of workplace stress may decrease the utilization of maladaptive coping strategies.
The research emphasizes significant clinical implications for managing stress in pharmacists, underscoring the necessity for personalized stress management interventions, workshops focusing on adaptive coping strategies, and policy modifications to mitigate workplace stressors. Enhancing professional support networks and conducting regular mental health screenings can provide pharmacists additional support in effectively managing stress, ultimately reducing emotional exhaustion. Moreover, it is proposed that public health campaigns can be employed to increase awareness regarding the significance of mental health within the pharmacy profession, fostering an environment that promotes open dialogue and the active pursuit of support, ultimately leading to improvements in the personal well-being of pharmacy professionals and the quality of care provided to patients.
While this study provides valuable insights, several limitations must be considered when interpreting the findings. First, the cross-sectional design restricts the ability to establish causal relationships between the studied variables. Future longitudinal research is recommended to understand the directionality of these associations better. Second, the reliance on self-reported measures introduces the possibility of CMB, as participants’ responses may be influenced by social desirability or recall inaccuracies. While self-reporting is a common practice in psychological research, future studies could enhance data reliability by incorporating objective stress indicators (e.g., cortisol levels, absenteeism rates, or supervisor assessments of emotional exhaustion). Third, the study population was geographically limited to pharmacists working in public hospitals in Punjab, Pakistan, which may limit the generalizability of the findings to pharmacists in private healthcare settings, community pharmacies, or other regions. Different healthcare systems may present unique stressors and coping mechanisms, necessitating further research across diverse settings. Additionally, although stratified sampling ensured representation across various categories of public hospitals, it may not fully capture the heterogeneity of individual pharmacist experiences. Fourth, this study applied the RRS-10, which was originally developed for populations with depression. Its use in a non-depressed sample may affect the applicability of findings. Future studies should validate the scale’s relevance across broader populations. Finally, while the study contributes to understanding the relationship between stress, coping strategies, and emotional exhaustion, limiting the sample to hospital pharmacists may narrow its applicability to the broader pharmacist workforce, including those in clinical laboratories, academia, or retail pharmacy settings. Future research should explore these relationships in diverse professional environments to provide a more comprehensive understanding.
In conclusion, this study highlighted the significant associations between stress, coping mechanisms, and the mental well-being of pharmacists. Our findings provided empirical evidence on the mechanisms through which stress contributes to emotional exhaustion, particularly emphasizing the amplifying role of maladaptive coping strategies such as rumination. These insights underscore the urgent need for targeted interventions aimed at mitigating these effects. Addressing these factors can significantly improve pharmacists’ well-being, ultimately enhancing the quality of care they provide to patients.
Acknowledgement: We would like to express our sincere gratitude to the reviewers and editorial team for their valuable comments and suggestions, which greatly improved the quality of this article. We are also deeply grateful to all the anonymous participants who took part in this research. Their contributions have been invaluable to the successful completion of this study.
Funding Statement: This research was supported by Social Policy Grant through Nazarbayev University, Kazakhstan.
Author Contributions: The authors confirm their contribution to the paper as follows: study conception and design: Shazia Rehman, Erum Rehman, Mehmood Ahmad; data collection: Mehmood Ahmad; analysis and interpretation of results: Shazia Rehman, Erum Rehman, Mehmood Ahmad; draft manuscript preparation: Shazia Rehman, Erum Rehman, Mehmood Ahmad. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The raw data that support the findings of this study are available upon reasonable request from the authors.
Ethics Approval: The study participants were informed that the data collected from these constructs would remain confidential and only accessible to the researchers and their team.
Informed Consent: Informed consent has been taken from all the participants. The study has been authorized by the Ethics Review Committee (ERC) of the Islamia University of Bahawalpur, Lahore, Pakistan (No. DR/2044).
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
Supplementary Materials: The supplementary material is available online at https://www.techscience.com/doi/10.32604/ijmhp.2025.063582/s1.
References
1. López-Cabarcos MÁ, López-Carballeira A, Ferro-Soto C. How to moderate emotional exhaustion among public healthcare professionals? Eur Res Manage Bus Econ. 2021;27(2):100140. [Google Scholar]
2. Sacadura-Leite E, Sousa-Uva A, Ferreira S, Costa PL, Passos AM. Working conditions and high emotional exhaustion among hospital nurses. Rev Bras Med Trab. 2019;17(1):69. [Google Scholar] [PubMed]
3. Sexton JB, Adair KC, Proulx J, Profit J, Cui X, Bae J, et al. Emotional exhaustion among US health care workers before and during the COVID-19 pandemic, 2019–2021. JAMA Netw Open. 2022;5(9):e2232748. doi:10.1001/jamanetworkopen.2022.32748. [Google Scholar] [PubMed] [CrossRef]
4. Cain CL, Taborda-Whitt C, Frazer M, Schellinger S, White KM, Kaasovic J, et al. A mixed methods study of emotional exhaustion: energizing and depleting work within an innovative healthcare team. J Interprof Care. 2017;31(6):714–24. doi:10.1080/13561820.2017.1356809. [Google Scholar] [PubMed] [CrossRef]
5. McFarland DC, Hlubocky F. Therapeutic strategies to tackle burnout and emotional exhaustion in frontline medical staff: narrative review. Psychol Res Behav Manage. 2021;14:1429–36. [Google Scholar] [PubMed]
6. Gilbert S, Laschinger HKS, Leiter M. The mediating effect of burnout on the relationship between structural empowerment and organizational citizenship behaviours. J Nurs Manage. 2010;18(3):339–48. doi:10.1111/j.1365-2834.2010.01074.x. [Google Scholar] [PubMed] [CrossRef]
7. Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15(2):103–11. doi:10.1002/wps.20311. [Google Scholar] [PubMed] [CrossRef]
8. Mintzberg H. The structuring of organizations. Berlin/Heidelberg, Germany: Springer; 1989. [Google Scholar]
9. Chênevert D, Jourdain G, Cole N, Banville B. The role of organisational justice, burnout and commitment in the understanding of absenteeism in the Canadian healthcare sector. J Health Organ Manage. 2013;27(3):350–67. doi:10.1108/jhom-06-2012-0116. [Google Scholar] [PubMed] [CrossRef]
10. Feng Y, Cui J. Emotional exhaustion and emotional contagion: navigating turnover intention of healthcare personnel. J Multidiscip Healthc. 2024;17:1731–42. doi:10.2147/jmdh.s460088. [Google Scholar] [PubMed] [CrossRef]
11. Fiabane E, Dordoni P, Setti I, Cacciatori I, Grossi C, Pistarini C, et al. Emotional dissonance and exhaustion among healthcare professionals: the role of the perceived quality of care. Int J Occup Med Environ Health. 2019;32(6):841–51. doi:10.13075/ijomeh.1896.01388. [Google Scholar] [PubMed] [CrossRef]
12. Lazarus RS, Folkman S. Stress, appraisal, and coping. Berlin/Heidelberg, Germany: Springer; 1984. [Google Scholar]
13. Laubmeier KK, Zakowski SG, Bair JP. The role of spirituality in the psychological adjustment to cancer: a test of the transactional model of stress and coping. Int J Behav Med. 2004;11:48–55. doi:10.1207/s15327558ijbm1101_6. [Google Scholar] [PubMed] [CrossRef]
14. Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspect Psychol Sci. 2008;3(5):400–24. doi:10.1111/j.1745-6924.2008.00088.x. [Google Scholar] [PubMed] [CrossRef]
15. Stoia-Caraballo R, Rye MS, Pan W, Brown Kirschman KJ, Lutz-Zois C, Lyons AM. Negative affect and anger rumination as mediators between forgiveness and sleep quality. J Behav Med. 2008;31:478–88. doi:10.1007/s10865-008-9172-5. [Google Scholar] [PubMed] [CrossRef]
16. McLaughlin KA, Nolen-Hoeksema S. Rumination as a transdiagnostic factor in depression and anxiety. Behav Res Ther. 2011;49(3):186–93. doi:10.1016/j.brat.2010.12.006. [Google Scholar] [PubMed] [CrossRef]
17. Moulds ML, Bisby MA, Wild J, Bryant RA. Rumination in posttraumatic stress disorder: a systematic review. Clin Psychol Rev. 2020;82:101910. doi:10.1016/j.cpr.2020.101910. [Google Scholar] [PubMed] [CrossRef]
18. McEvoy PM, Watson H, Watkins ER, Nathan P. The relationship between worry, rumination, and comorbidity: evidence for repetitive negative thinking as a transdiagnostic construct. J Affect Disord. 2013;151(1):313–20. doi:10.1016/j.jad.2013.06.014. [Google Scholar] [PubMed] [CrossRef]
19. Broderick PC. Mindfulness and coping with dysphoric mood: contrasts with rumination and distraction. Cognit Ther Res. 2005;29:501–10. doi:10.1007/s10608-005-3888-0. [Google Scholar] [CrossRef]
20. Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. J Abnorm Psychol. 1991;100(4):569. doi:10.1037/0021-843x.100.4.569. [Google Scholar] [PubMed] [CrossRef]
21. Vickers KS, Vogeltanz-Holm ND. The effects of rumination and distraction tasks on psychophysiological responses and mood in dysphoric and nondysphoric individuals. Cognit Ther Res. 2003;27:331–48. [Google Scholar]
22. Ding Y, Yang Y, Yang X, Zhang T, Qiu X, He X, et al. The mediating role of coping style in the relationship between psychological capital and burnout among Chinese nurses. PLoS One. 2015;10(4):e0122128. doi:10.1371/journal.pone.0122128. [Google Scholar] [PubMed] [CrossRef]
23. Carmona C, Buunk AP, Peiró JM, Rodríguez I, Bravo MJ. Do social comparison and coping styles play a role in the development of burnout? Cross-sectional and longitudinal findings. J Occup Organ Psychol. 2006;79(1):85–99. doi:10.1348/096317905x40808. [Google Scholar] [CrossRef]
24. Chen J, Li J, Cao B, Wang F, Luo L, Xu J. Mediating effects of self-efficacy, coping, burnout, and social support between job stress and mental health among young Chinese nurses. J Adv Nurs. 2020;76(1):163–73. doi:10.1111/jan.14208. [Google Scholar] [PubMed] [CrossRef]
25. Lou NM, Montreuil T, Feldman LS, Fried GM, Lavoie-Tremblay M, Bhanji F, et al. Nurses’ and physicians’ distress, burnout, and coping strategies during COVID-19: stress and impact on perceived performance and intentions to quit. J Contin Educ Health Prof. 2022;42(1):e44–52. doi:10.1097/ceh.0000000000000365. [Google Scholar] [PubMed] [CrossRef]
26. Stephenson E, DeLongis A. Coping strategies. Wiley Encycl Heal Psychol. 2020;2020:55–60. doi:10.1002/9781119057840.ch50. [Google Scholar] [CrossRef]
27. ALmutairi MN, ElMahalli AA. Burnout and coping methods among emergency medical services professionals. J Multidiscip Healthc. 2020;13:271–9. [Google Scholar] [PubMed]
28. Elliot AJ, Thrash TM, Murayama K. A longitudinal analysis of self-regulation and well-being: avoidance personal goals, avoidance coping, stress generation, and subjective well-being. J Pers. 2011;79(3):643–74. doi:10.1111/j.1467-6494.2011.00694.x. [Google Scholar] [PubMed] [CrossRef]
29. Yusoff MSB. A DEAL-based intervention for the reduction of depression, denial, self-blame and academic stress: a randomized controlled trial. J Taibah Univ Med Sci. 2015;10(1):82–92. doi:10.1016/j.jtumed.2014.08.003. [Google Scholar] [CrossRef]
30. Van Boekel LC, Brouwers EPM, Van Weeghel J, Garretsen HFL. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1–2):23–35. doi:10.1016/j.drugalcdep.2013.02.018. [Google Scholar] [PubMed] [CrossRef]
31. Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267. doi:10.1037/0022-3514.56.2.267. [Google Scholar] [PubMed] [CrossRef]
32. Labrague LJ, McEnroe-Petitte DM, Gloe D, Thomas L, Papathanasiou IV, Tsaras K. A literature review on stress and coping strategies in nursing students. J Ment Health. 2017;26(5):471–80. doi:10.1080/09638237.2016.1244721. [Google Scholar] [PubMed] [CrossRef]
33. Skinner EA, Edge K, Altman J, Sherwood H. Searching for the structure of coping: a review and critique of category systems for classifying ways of coping. Psychol Bull. 2003;129(2):216. doi:10.1037/0033-2909.129.2.216. [Google Scholar] [PubMed] [CrossRef]
34. Teng R, Zhou S, Zheng W, Ma C. Artificial intelligence (AI) awareness and work withdrawal: evaluating chained mediation through negative work-related rumination and emotional exhaustion. Int J Contemp Hosp Manage. 2024;36(7):2311–26. doi:10.1108/ijchm-02-2023-0240. [Google Scholar] [CrossRef]
35. Chen D, Ni Y, Lu J, Wang Y, Qi Q, Zhai H. Examining the impact of perceived stress, anxiety, and resilience on depression among medical staff after COVID-19 quarantine: a chain mediation analysis. Front Public Heal. 2023;11:1250623. doi:10.3389/fpubh.2023.1250623. [Google Scholar] [PubMed] [CrossRef]
36. Hayes AF. Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr. 2009;76(4):408–20. doi:10.1080/03637750903310360. [Google Scholar] [CrossRef]
37. Population Welfare Department, Population Profile Punjab. Govt of Pakistan [Internet]. 2017 [cited 2025 Mar 5]. Available from: https://pwd.punjab.gov.pk/population_profile. [Google Scholar]
38. Hashami MF. Healthcare systems & its challenges in Pakistan. Int J Soc Sci. 2020;9(1):19–23. [Google Scholar]
39. Khattak AF, Rahman AU, Khattak M, Qazi M, Gilani H, Khan A, et al. Toward sustainable healthcare systems: a low and middle-income country’s case for investing in healthcare reforms. Cureus. 2023;9:15–5. doi:10.7759/cureus.39345. [Google Scholar] [PubMed] [CrossRef]
40. Mir AM, Shaikh MS, Rashida G, Mankani N. To serve or to leave: a question faced by public sector healthcare providers in Pakistan. Health Res Policy Syst. 2015;13:85–91. doi:10.1186/s12961-015-0045-4. [Google Scholar] [PubMed] [CrossRef]
41. Cohen S. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Thousand Oaks, CA, USA: Sage Publications, Inc.; 1988. p. 31–67. [Google Scholar]
42. Mushtaq R, Ahmed R. Psychometric properties of Pakistani version of perceived stress scale. Pak J Psychol. 2020;51(1):51–63. [Google Scholar]
43. Shah M, Hasan S, Malik S, Sreeramareddy CT. Perceived stress, sources and severity of stress among medical undergraduates in a Pakistani medical school. BMC Med Educ. 2010;10:1–8. doi:10.1186/1472-6920-10-2. [Google Scholar] [PubMed] [CrossRef]
44. Ikram N, Frost A, LeMasters K, Hagaman A, Baranov V, Gallis J, et al. Adverse childhood experiences and implications of perceived stress, anxiety and cortisol among women in Pakistan: a cross-sectional study. BMJ Open. 2022;12(4):e052280. doi:10.21203/rs.3.rs-403429/v1. [Google Scholar] [CrossRef]
45. Khan A, Ahmed KB. Perceived stress and religious coping among Pakistani-origin emerging muslim adults living in Pakistan and the United States: a cross-cultural view. J Mind Med Sci. 2023;10(2):267–75. [Google Scholar]
46. Luminet O. 10 Measurement of depressive rumination and associated constructs. In: Depressive rumination. New York, NY, USA: Wiley; 2004. 187 p. doi:10.1002/9780470713853.ch10. [Google Scholar] [CrossRef]
47. Piguet C, Desseilles M, Sterpenich V, Cojan Y, Bertschy G, Vuilleumier P. Neural substrates of rumination tendency in non-depressed individuals. Biol Psychol. 2014;103:195–202. doi:10.1016/j.biopsycho.2014.09.005. [Google Scholar] [PubMed] [CrossRef]
48. Topper M, Emmelkamp PMG, Watkins E, Ehring T. Development and assessment of brief versions of the Penn State worry questionnaire and the ruminative response scale. Br J Clin Psychol. 2014;53(4):402–21. doi:10.1111/bjc.12052. [Google Scholar] [PubMed] [CrossRef]
49. Extremera N, Fernández-Berrocal P. Validity and reliability of Spanish versions of the ruminative responses scale-short form and the distraction responses scale in a sample of Spanish high school and college students. Psychol Rep. 2006;98(1):141–50. doi:10.2466/pr0.98.1.141-150. [Google Scholar] [PubMed] [CrossRef]
50. Iqbal A, Khalid S, Batool S. Rumination as predictor of anxiety, depression, stress and affect among people with traumatic amputation in Pakistan. Pak Soc Sci Rev. 2021;5:610–20. [Google Scholar]
51. Syed SMH, Chethiyar SDM, Ibrahim NB. Mediating role of rumination between neuroticism and depression among the married and unmarried nurses of Multan. Ann Soc Sci Perspect. 2021;2(2):299–310. doi:10.52700/assap.v2i2.100. [Google Scholar] [CrossRef]
52. Iqbal A, Khalid S, Bin AS, Tassadaq N, Tariq M, Satti IA. Development and validation of rumination scale for traumatic amputees while utilizing a Pakistani cohort; first part. Rawal Med J. 2022;47(2):342. [Google Scholar]
53. Carver CS. You want to measure coping but your protocol’s too long: consider the brief cope. Int J Behav Med. 1997;4(1):92–100. doi:10.1207/s15327558ijbm0401_6. [Google Scholar] [PubMed] [CrossRef]
54. Moore BC, Biegel DE, McMahon TJ. Maladaptive coping as a mediator of family stress. J Soc Work Pract Addict. 2011;11(1):17–39. doi:10.1080/1533256x.2011.544600. [Google Scholar] [PubMed] [CrossRef]
55. Vanstone DM, Hicks RE. Transitioning to university: coping styles as mediators between adaptive-maladaptive perfectionism and test anxiety. Pers Individ Dif. 2019;141:68–75. doi:10.1016/j.paid.2018.12.026. [Google Scholar] [CrossRef]
56. Nazir A, Mohsin H. Coping styles, aggression and interpersonal conflicts among depressed and non-depressed people. Health Promot Perspect. 2013;3(1):80. [Google Scholar] [PubMed]
57. Shahid N, Malik TA, Hussain A, Ahmed S. Unmet psycho-social needs, coping strategies and psychological distress among people with cancer: evidence from Pakistan. J Pak Med Assoc. 2021;71(5):1373–8. [Google Scholar] [PubMed]
58. Block RI, Bair HL, Carillo JF. Is exhaustion more sensitive than disengagement to burnout in academic anesthesia? A study using the Oldenburg burnout inventory. Psychol Rep. 2020;123(4):1282–96. doi:10.1177/0033294119856560. [Google Scholar] [PubMed] [CrossRef]
59. Le RT, Sifrig B, Chesire D, Hernandez M, Kee-Sampson J, Matteo J, et al. Comparative analysis of radiology trainee burnout using the Maslach burnout inventory and oldenburg burnout inventory. Acad Radiol. 2023;30(5):991–7. doi:10.1016/j.acra.2022.08.016. [Google Scholar] [PubMed] [CrossRef]
60. Hwang S, Kwon KT, Lee SH, Kim S-W, Chang H-H, Kim Y, et al. Correlates of burnout among healthcare workers during the COVID-19 pandemic in South Korea. Sci Rep. 2023;13(1):3360. doi:10.1038/s41598-023-30372-x. [Google Scholar] [PubMed] [CrossRef]
61. Khan A, Yusoff RBM. Psychometric testing of Oldenburg burnout inventory among academic staff in Pakistan. Int Rev Manage Mark. 2016;6(4):683–7. [Google Scholar]
62. Reis C, Tecedeiro M, Pellegrino P, Paiva T, Marôco JP. Psychometric properties of the oldenburg burnout inventory in a portuguese sample of aircraft maintenance technicians. Front Psychol. 2021;12:725099. doi:10.3389/fpsyg.2021.725099. [Google Scholar] [PubMed] [CrossRef]
63. Subburaj A, Vijayadurai J. Translation, validation and psychometric properties of Tamil version of Oldenburg Burnout Inventory (OLBI). Procedia-Soc Behav Sci. 2016;219:724–31. doi:10.1016/j.sbspro.2016.05.067. [Google Scholar] [CrossRef]
64. Zhang J, Rehman S, Addas A, Ahmad J. Influence of work-life balance on mental health among nurses: the mediating role of psychological capital and job satisfaction. Psychol Res Behav Manage. 2024;31(17):4249–62. doi:10.2147/prbm.s497305. [Google Scholar] [PubMed] [CrossRef]
65. Durham ME, Bush PW, Ball AM. Evidence of burnout in health-system pharmacists. Am J Heal Pharm. 2018; 75(23 Supplement 4):S93–100. doi:10.2146/ajhp170818. [Google Scholar] [PubMed] [CrossRef]
66. Higuchi Y, Inagaki M, Koyama T, Kitamura Y, Sendo T, Fujimori M, et al. A cross-sectional study of psychological distress, burnout, and the associated risk factors in hospital pharmacists in Japan. BMC Public Health. 2016;16:1–8. doi:10.1186/s12889-016-3208-5. [Google Scholar] [PubMed] [CrossRef]
67. Dee J, Dhuhaibawi N, Hayden JC. A systematic review and pooled prevalence of burnout in pharmacists. Int J Clin Pharm. 2023;45(5):1027–36. doi:10.1007/s11096-022-01520-6. [Google Scholar] [PubMed] [CrossRef]
68. Haase KK. Addressing burnout in clinical pharmacy: what can we learn from other health care disciplines? J Am Coll Clin Pharm. 2020;3(3):645–54. doi:10.1002/jac5.1189. [Google Scholar] [CrossRef]
69. Jones GM, Roe NA, Louden L, Tubbs CR. Factors associated with burnout among US hospital clinical pharmacy practitioners: results of a nationwide pilot survey. Hosp Pharm. 2017;52(11):742–51. doi:10.1177/0018578717732339. [Google Scholar] [PubMed] [CrossRef]
70. Shanafelt TD, Mungo M, Schmitgen J, Storz KA, Reeves D, Hayes SN, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. 2016;91(4):422–31. doi:10.1016/j.mayocp.2016.02.001. [Google Scholar] [PubMed] [CrossRef]
71. Humer E, Pieh C, Kisler I-M, Schimböck W, Schadenhofer P. A longitudinal study on mental well-being, perceived stress level and job-related meaningfulness of Austrian telephone emergency service counselors during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(6):3166. doi:10.3390/ijerph19063166. [Google Scholar] [PubMed] [CrossRef]
72. Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. J Pers Soc Psychol. 1991;61(1):115–21. doi:10.1037/0022-3514.61.1.115. [Google Scholar] [PubMed] [CrossRef]
73. Nolen-Hoeksema S, Morrow J. Effects of rumination and distraction on naturally occurring depressed mood. Cogn Emot. 1993;7(6):561–70. doi:10.1080/02699939308409206. [Google Scholar] [CrossRef]
74. Donahue EG, Forest J, Vallerand RJ, Lemyre P, Crevier-Braud L, Bergeron É. Passion for work and emotional exhaustion: the mediating role of rumination and recovery. Appl Psychol Health Well-Being. 2012;4(3):341–68. doi:10.1111/j.1758-0854.2012.01078.x. [Google Scholar] [PubMed] [CrossRef]
75. Vandevala T, Pavey L, Chelidoni O, Chang N-F, Creagh-Brown B, Cox A. Psychological rumination and recovery from work in intensive care professionals: associations with stress, burnout, depression and health. J Intensive Care. 2017;5:1–8. doi:10.1186/s40560-017-0209-0. [Google Scholar] [PubMed] [CrossRef]
76. Liu M, Wang N, Wang P, Wu H, Ding X, Zhao F. Negative emotions and job burnout in news media workers: a moderated mediation model of rumination and empathy. J Affect Disord. 2021;279:75–82. doi:10.1016/j.jad.2020.09.123. [Google Scholar] [PubMed] [CrossRef]
77. Smout MF, Simpson SG, Stacey F, Reid C. The influence of maladaptive coping modes, resilience, and job demands on emotional exhaustion in psychologists. Clin Psychol Psychother. 2022;29(1):260–73. doi:10.1002/cpp.2631. [Google Scholar] [PubMed] [CrossRef]
78. Gaudioso F, Turel O, Galimberti C. Explaining work exhaustion from a coping theory perspective: roles of techno-stressors and technology-specific coping strategies. Annu Rev Cybertherapy Telemed. 2015;219:14–20. [Google Scholar]
79. Folkman S, Moskowitz JT. Coping: pitfalls and promise. Annu Rev Psychol. 2004;55:745–74. doi:10.1146/annurev.psych.55.090902.141456. [Google Scholar] [PubMed] [CrossRef]
80. Beck AT. Cognitive therapy and the emotional disorders. London, UK: Penguin; 1979. [Google Scholar]
81. Turliuc MN, Măirean C, Turliuc MD. Rumination and suppression as mediators of the relationship between dysfunctional beliefs and traumatic stress. Int J Stress Manage. 2015;22(3):306–322. doi:10.1037/a0039272. [Google Scholar] [CrossRef]
82. Borders A, Liang CTH. Rumination partially mediates the associations between perceived ethnic discrimination, emotional distress, and aggression. Cult Divers Ethn Minor Psychol. 2011;17(2):125. doi:10.1037/a0023357. [Google Scholar] [PubMed] [CrossRef]
83. Boyes ME, Hasking PA, Martin G. Adverse life experience and psychological distress in adolescence: moderating and mediating effects of emotion regulation and rumination. Stress Health. 2016;32(4):402–10. doi:10.1002/smi.2635. [Google Scholar] [PubMed] [CrossRef]
84. Maresca G, Corallo F, Catanese G, Formica C, Lo Buono V. Coping strategies of healthcare professionals with burnout syndrome: a systematic review. Medicina. 2022 Feb;58(2):327. doi:10.3390/medicina58020327. [Google Scholar] [PubMed] [CrossRef]
85. Sipos D, Goyal R, Zapata T. Addressing burnout in the healthcare workforce: current realities and mitigation strategies. Lancet Reg Health Eur. 2024 Jul;42:100961. doi:10.1016/j.lanepe.2024.100961. [Google Scholar] [PubMed] [CrossRef]
86. Sipos D, Biro AA, Busa F, Freihat O, Tollár J, Pandur AA, et al. Reduced burnout in medical and health science students during the pandemic COVID-19—a follow-up study of a single institution in Hungary. BMC Med Educ. 2023;23(1):893. doi:10.1186/s12909-023-04867-0. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools